Phlebotomy Vascular Access Devices and Your Unique Role
Phlebotomy, Vascular Access Devices, and Your Unique Role LYNN HADAWAY, MED, RN-BC, CRNI CE Code (Attendee Use Only): _______________ __
Financial Disclosures 1. Disclosure of Relevant Financial Relationships I have the following financial relationships to disclose: Consultant for: Adhezion Biomedical, Atrion, B Braun, Baxter, BD, 3 m, Elcam, Fresenius Kabi, Linear Health, Pursuit Vascular, Teleflex, VATA, Velano Vascular Speaker’s Bureau for: B Braun, BD, 3 M, Velano Vascular 2. Disclosure of Off-Label and/or investigative Uses - None
Venipuncture ▶ Think about the words we use ▶ What do they mean to patients? ▶ What impressions to they leave with patients?
Fun Things This is a Stick This is Poking
This is Venipuncture! ▶ And it hurts! The Goal-Reduce Venipunctures and Save Veins Don’t forget Phlebotomy
Learning Objectives ▶ Identify anatomical and pathophysiological changes associated with venipuncture and vascular access devices (VAD). ▶ Evaluate clinical practices that increase risk associated with phlebotomy. ▶ Analyze factors associated with unlicensed assistive personnel involved with new technologies for phlebotomy. ▶ Explain techniques and technologies that reduce phlebotomy risks.

Divas or D. I. V. A.

Your Patient’s Experience ▶ DIVA – difficult IV access ▶ clinical condition requiring multiple attempts, special interventions to achieve and maintain peripheral IV access in children (Kuensting, 2009) ▶ At least 2 failed attempts, use of atypical locations, need for USGPIV or intraosseus sites. (Fields, 2014) ▶ 5 risk factors for DIVA in adults – impossible to see or palpate, history of difficulty, unplanned surgery, vein diameter < 2 mm (van Loon, 2016)
Your Patients Experience ▶ Pain ▶ Needle phobia ▶ Anxiety, Fear ▶ Vasovagal Reactions and Syncope
Your Patient’s Experience ▶ ▶ 74% of hospitalized children report IV catheters as worst pain (Kuensting, 2009) Fear, anxiety and DIVA have a significant relationship to 1 st time phlebotomy success in children (Gerceker, 2018) 8% to 16% of adults are DIVAs in ED (Fields, 2014) 59. 3% of highly complex adults are DIVAs (Armenteros. Yegueas, 2017)
Your Patient’s Experience ▶ Pain ▶ ▶ Real procedure pain – under evaluated and under treated ▶ Several methods to manage – local anesthetic, vibration, cold ▶ Many barriers to use – lack of knowledge, denial of pain, no written protocols (Filbet, 2017) Anticipatory distress before procedure begins
Your Patient’s Experience ▶ Needle phobia, AKA Blood-injection-injury phobia ▶ Recognized diagnosis ▶ 10% of people in all medical settings, 1. 6% of general population (Deacon, 2006) ▶ 63% of children have fear of needles; 14% to 38% in adults (Mc. Murtry, 2015) ▶ Significant avoidance of needed healthcare ▶ Becomes a lifelong problem from childhood experiences
Your Patient’s Experience ▶ Vasovagal Reactions and Syncope ▶ Increased heart rate and blood pressure, then suddenly falling ▶ Leads to fainting
Patients Real Cannulation Experience ▶ ▶ ▶ A necessary evil defensive reactions Difficult journey through illness sharing with fellow patients Bad veins trust in clinicians knowledge and skill (Robinson-Reilly, 2015)
Patient Satisfaction ▶ Feelings of being vulnerable ▶ Patients feelings dismissed by clinicians ▶ Need for shared decision-making
Laboratory Services ▶ ▶ “Medical gatekeeper” ▶ Emergent medical interventions ▶ Urgent treatment decisions ▶ Non-emergent decisions All require accurate, timely laboratory data
Laboratory Services ▶ Average number of inpatient phlebotomy venipunctures per day ▶ 1. 38 to 1. 62 per day, up to 20% of patients requiring more than 2 per day ▶ ▶ 777 bed tertiary center (Petrides, 2017) Think Twice, Stick Once program by Internal Medicine residents ▶ 2. 10 punctures per day down to 1. 78 per day (Wheeler, 2016)
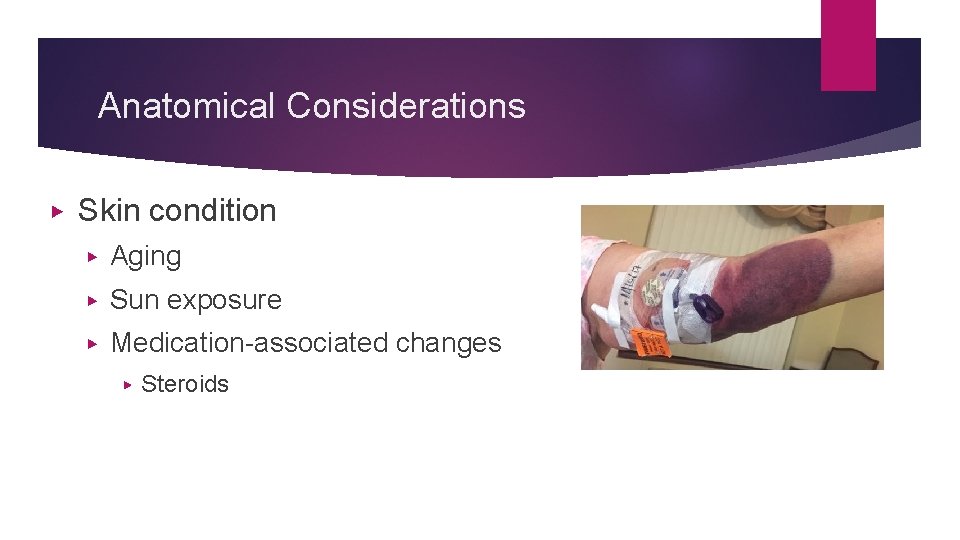
Anatomical Considerations ▶ Skin condition ▶ Aging ▶ Sun exposure ▶ Medication-associated changes ▶ Steroids
Anatomical Considerations ▶ Superficial Veins Visible, elevated above skin surface? ▶ Palpable ▶ ▶ Resilient, elastic ▶ Hard, cord-like from repetitive venipunctures ▶ chronic disease management ▶ Illicit IV drug use Depth in tissue ▶ Venous cross-section area ▶
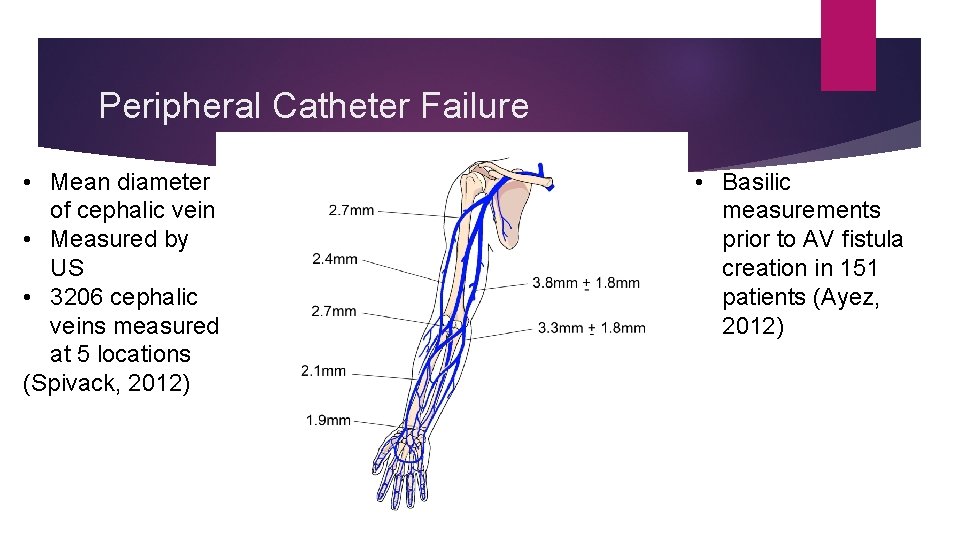
Peripheral Catheter Failure • Mean diameter of cephalic vein • Measured by US • 3206 cephalic veins measured at 5 locations (Spivack, 2012) • Basilic measurements prior to AV fistula creation in 151 patients (Ayez, 2012)
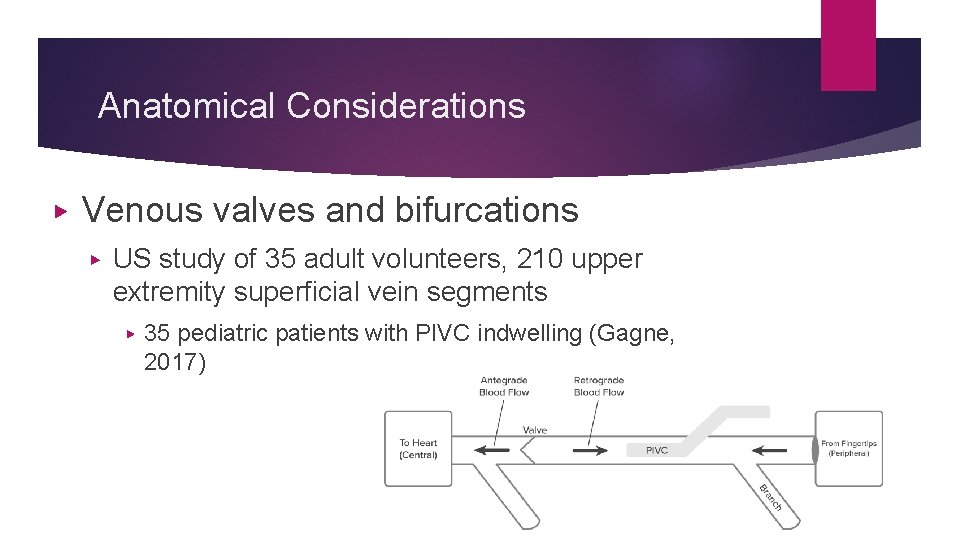
Anatomical Considerations ▶ Venous valves and bifurcations ▶ US study of 35 adult volunteers, 210 upper extremity superficial vein segments ▶ 35 pediatric patients with PIVC indwelling (Gagne, 2017)
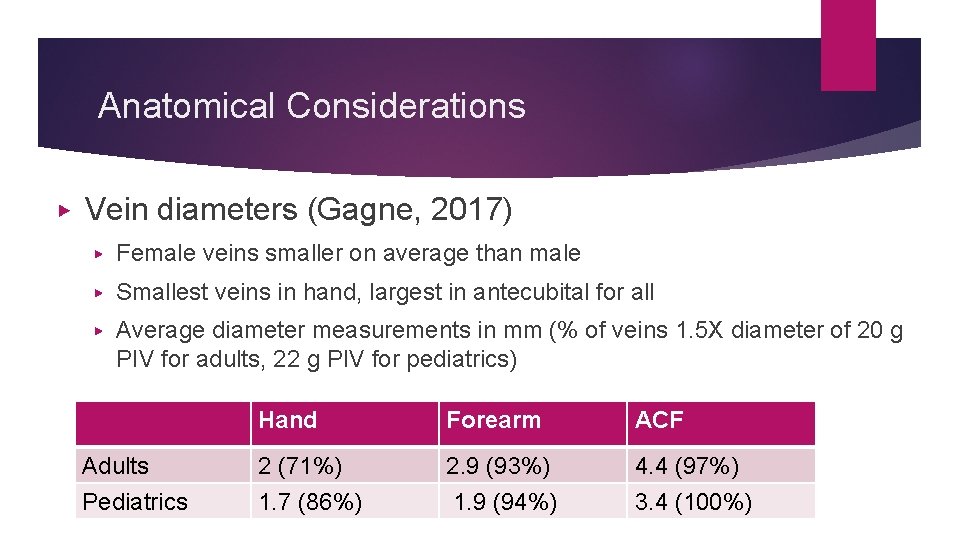
Anatomical Considerations ▶ Vein diameters (Gagne, 2017) ▶ Female veins smaller on average than male ▶ Smallest veins in hand, largest in antecubital for all ▶ Average diameter measurements in mm (% of veins 1. 5 X diameter of 20 g PIV for adults, 22 g PIV for pediatrics) Hand Forearm ACF Adults 2 (71%) 2. 9 (93%) 4. 4 (97%) Pediatrics 1. 7 (86%) 1. 9 (94%) 3. 4 (100%)
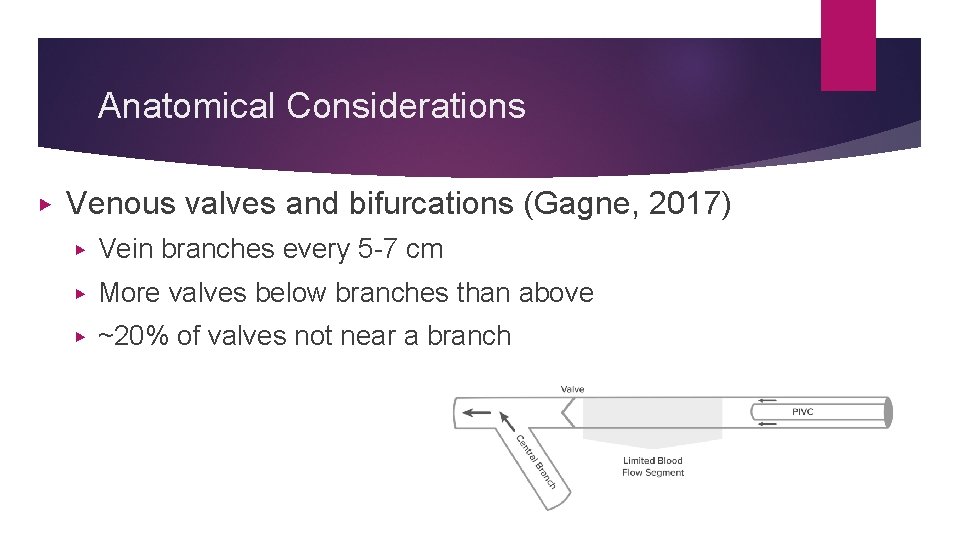
Anatomical Considerations ▶ Venous valves and bifurcations (Gagne, 2017) ▶ Vein branches every 5 -7 cm ▶ More valves below branches than above ▶ ~20% of valves not near a branch
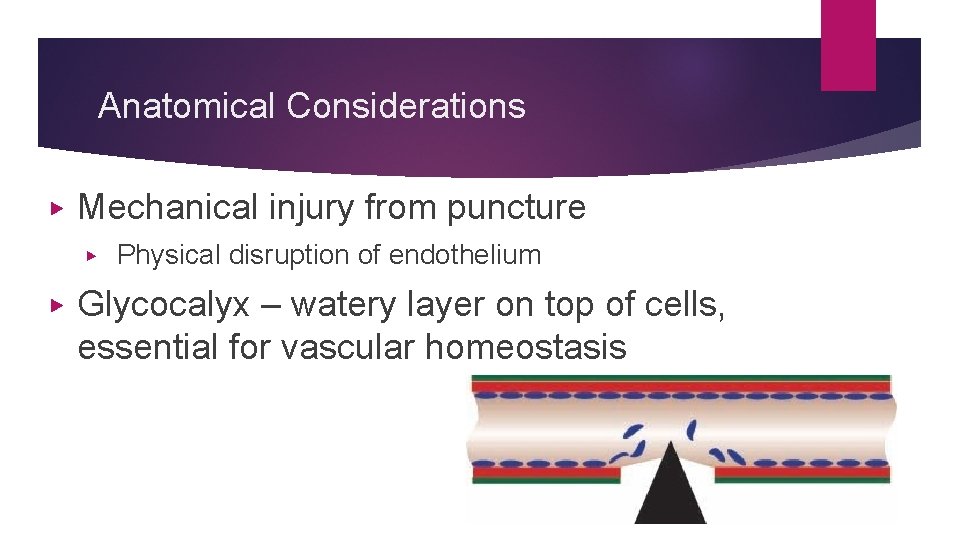
Anatomical Considerations ▶ Mechanical injury from puncture ▶ ▶ Physical disruption of endothelium Glycocalyx – watery layer on top of cells, essential for vascular homeostasis
Pathophysiological Issues ▶ Inflammation!! ▶ Numerous diseases are due to inflammatory processes ▶ ▶ Chronic venous disease can affect upper extremities ▶ ▶ Inflammatory cytokines alter vasoconstricting and vasodilating factors Vein wall weakening and dilation causes incompetent venous valves (Castro. Ferreira, 2018) Least risk – indwelling peripheral catheter or repetitive venpunctures?
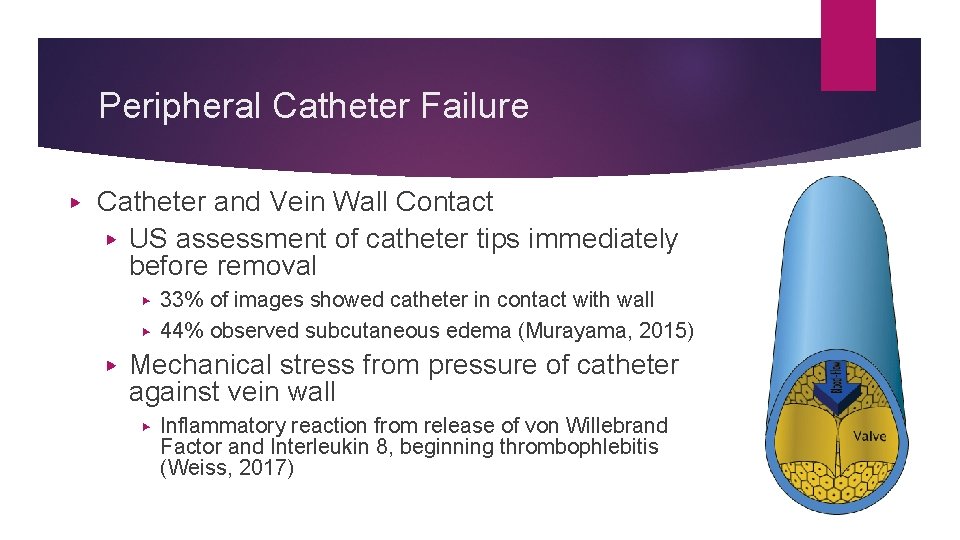
Peripheral Catheter Failure ▶ Catheter and Vein Wall Contact ▶ US assessment of catheter tips immediately before removal 33% of images showed catheter in contact with wall ▶ 44% observed subcutaneous edema (Murayama, 2015) ▶ ▶ Mechanical stress from pressure of catheter against vein wall ▶ Inflammatory reaction from release of von Willebrand Factor and Interleukin 8, beginning thrombophlebitis (Weiss, 2017)
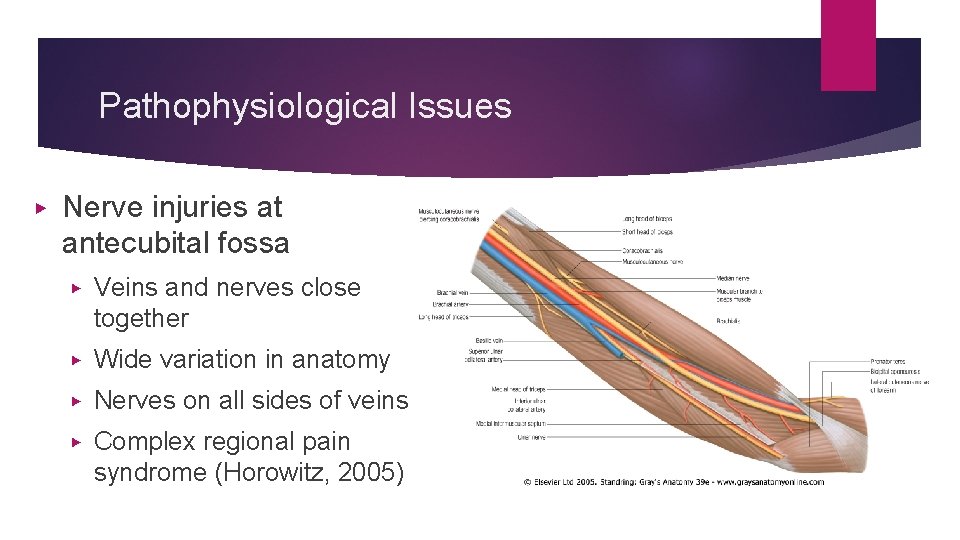
Pathophysiological Issues ▶ Nerve injuries at antecubital fossa ▶ Veins and nerves close together ▶ Wide variation in anatomy ▶ Nerves on all sides of veins ▶ Complex regional pain syndrome (Horowitz, 2005)
Phlebotomy Technique ▶ Needle movement (Fujii, 2013) ▶ Digital recording of procedures showed ▶ ▶ Forward movement of needle tip by additional 6 mm Venipuncture technique ▶ DIVAs ▶ Switching hands ▶ Changing vacuum tubes
Phlebotomy Risks ▶ Pre-analytical phase ▶ The period of time before a body fluid specimen reaches the lab including obtaining, labeling, and transporting specimen to lab (Gorski, 2016) ▶ Most vulnerable period- ▶ ▶ 62% errors before specimen reaches lab ▶ Lack of control by Laboratory Services (Cadamuro, 2018) Practice standardization strongly recommended (Lippi, 2017)
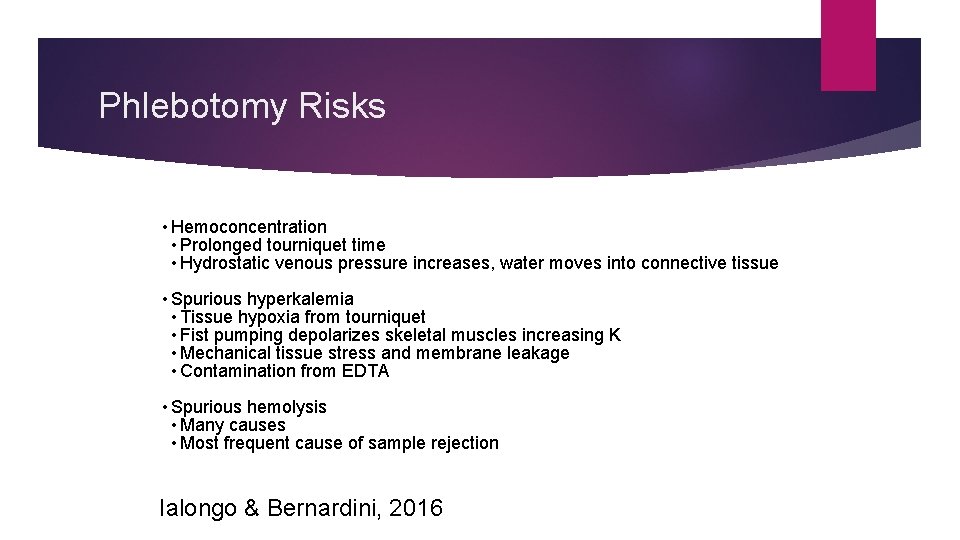
Phlebotomy Risks • Hemoconcentration • Prolonged tourniquet time • Hydrostatic venous pressure increases, water moves into connective tissue • Spurious hyperkalemia • Tissue hypoxia from tourniquet • Fist pumping depolarizes skeletal muscles increasing K • Mechanical tissue stress and membrane leakage • Contamination from EDTA • Spurious hemolysis • Many causes • Most frequent cause of sample rejection Ialongo & Bernardini, 2016
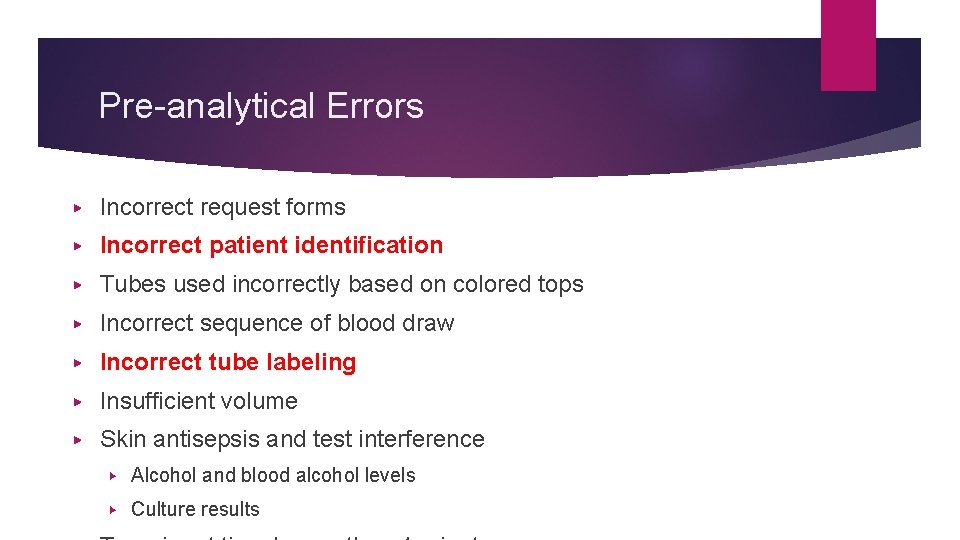
Pre-analytical Errors ▶ Incorrect request forms ▶ Incorrect patient identification ▶ Tubes used incorrectly based on colored tops ▶ Incorrect sequence of blood draw ▶ Incorrect tube labeling ▶ Insufficient volume ▶ Skin antisepsis and test interference ▶ Alcohol and blood alcohol levels ▶ Culture results
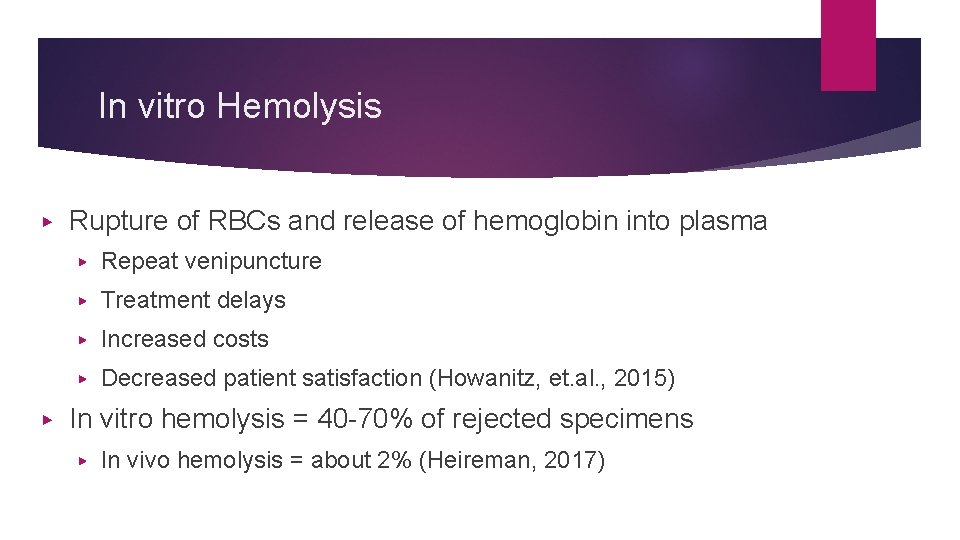
In vitro Hemolysis ▶ ▶ Rupture of RBCs and release of hemoglobin into plasma ▶ Repeat venipuncture ▶ Treatment delays ▶ Increased costs ▶ Decreased patient satisfaction (Howanitz, et. al. , 2015) In vitro hemolysis = 40 -70% of rejected specimens ▶ In vivo hemolysis = about 2% (Heireman, 2017)
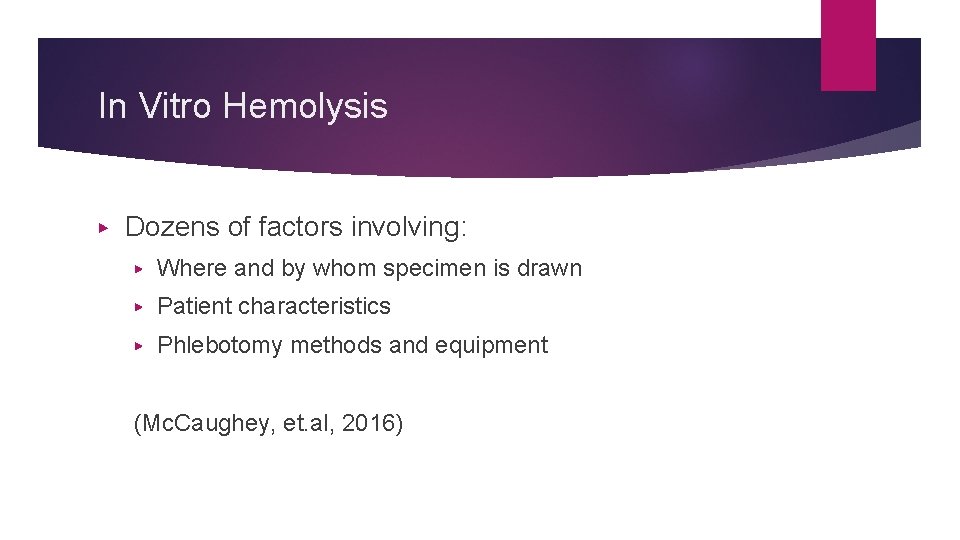
In Vitro Hemolysis ▶ Dozens of factors involving: ▶ Where and by whom specimen is drawn ▶ Patient characteristics ▶ Phlebotomy methods and equipment (Mc. Caughey, et. al, 2016)
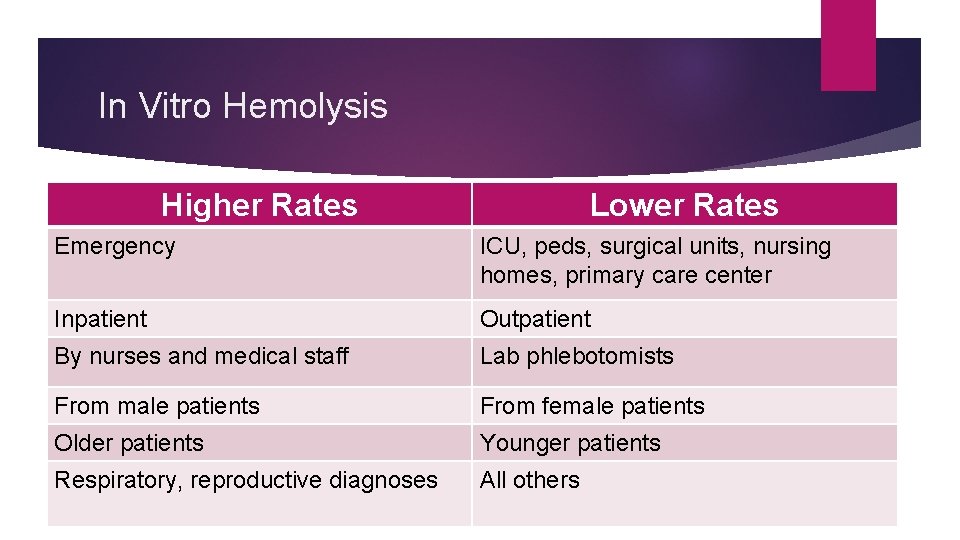
In Vitro Hemolysis Higher Rates Lower Rates Emergency ICU, peds, surgical units, nursing homes, primary care center Inpatient Outpatient By nurses and medical staff Lab phlebotomists From male patients From female patients Older patients Younger patients Respiratory, reproductive diagnoses All others
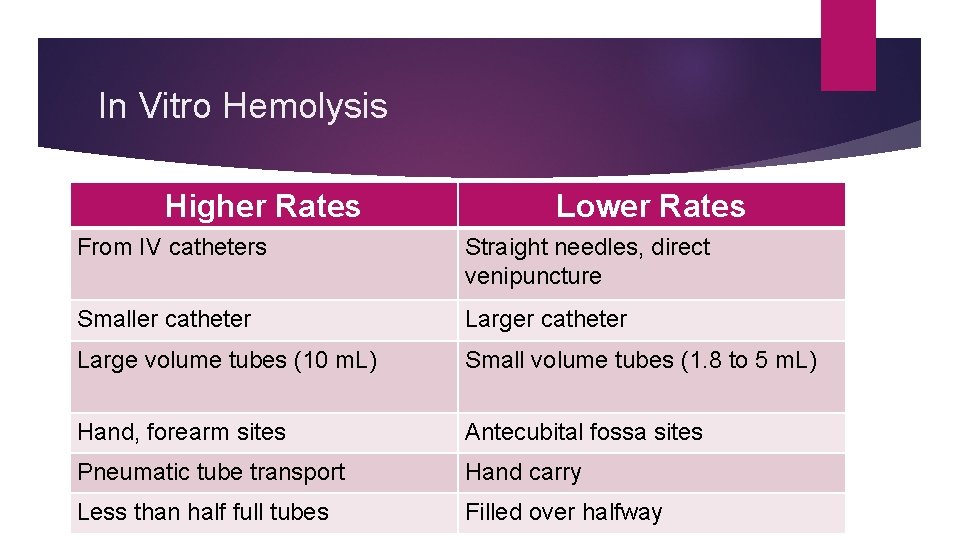
In Vitro Hemolysis Higher Rates Lower Rates From IV catheters Straight needles, direct venipuncture Smaller catheter Large volume tubes (10 m. L) Small volume tubes (1. 8 to 5 m. L) Hand, forearm sites Antecubital fossa sites Pneumatic tube transport Hand carry Less than half full tubes Filled over halfway
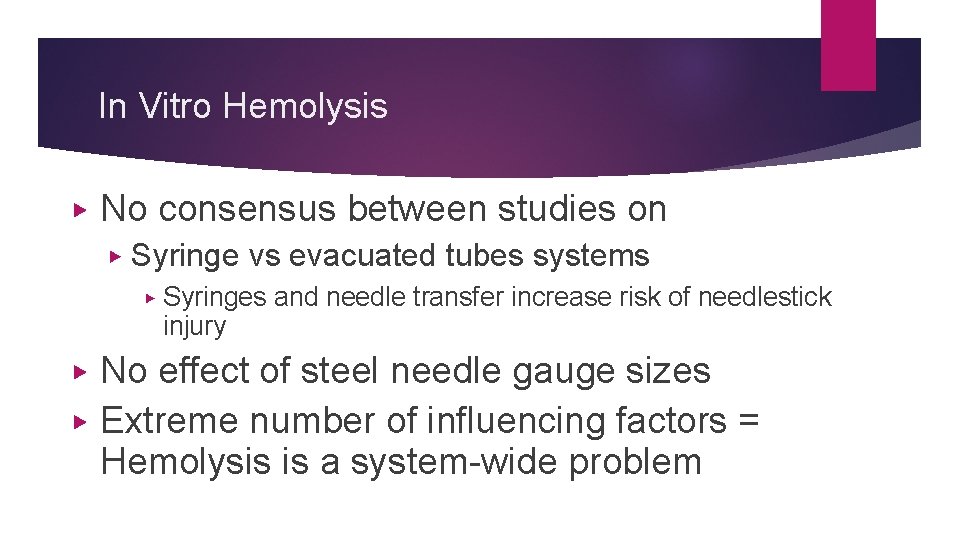
In Vitro Hemolysis ▶ No consensus between studies on ▶ Syringe vs evacuated tubes systems ▶ ▶ ▶ Syringes and needle transfer increase risk of needlestick injury No effect of steel needle gauge sizes Extreme number of influencing factors = Hemolysis is a system-wide problem
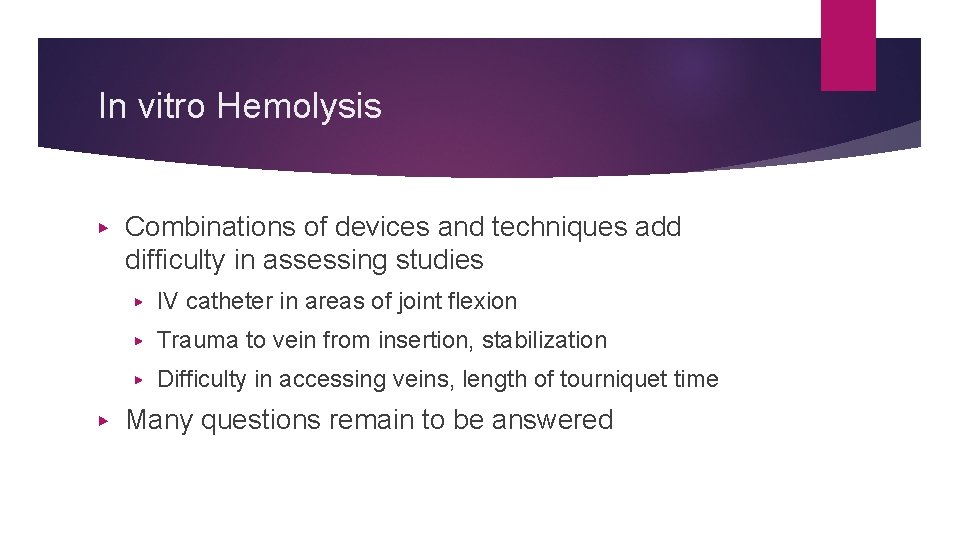
In vitro Hemolysis ▶ ▶ Combinations of devices and techniques add difficulty in assessing studies ▶ IV catheter in areas of joint flexion ▶ Trauma to vein from insertion, stabilization ▶ Difficulty in accessing veins, length of tourniquet time Many questions remain to be answered
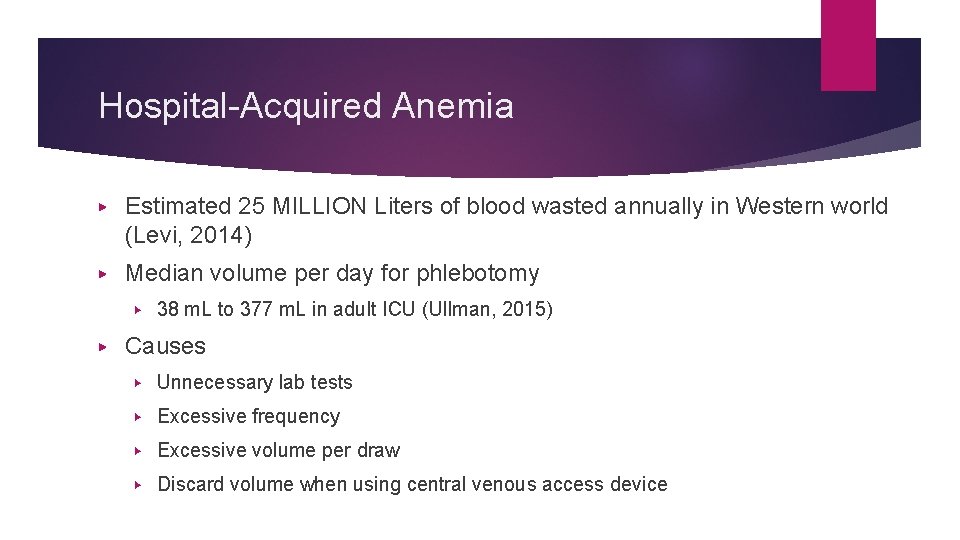
Hospital-Acquired Anemia ▶ Estimated 25 MILLION Liters of blood wasted annually in Western world (Levi, 2014) ▶ Median volume per day for phlebotomy ▶ ▶ 38 m. L to 377 m. L in adult ICU (Ullman, 2015) Causes ▶ Unnecessary lab tests ▶ Excessive frequency ▶ Excessive volume per draw ▶ Discard volume when using central venous access device
Hospital Acquired Anemia ▶ Phlebotomy volume = reduced Hemoglobin and Hematocrit ▶ ▶ Adult and pediatric ICU (Chant, 2006; Ullman, 2016, Steffen, 2017)) General medical units, no admission anemia, no anemia producing conditions (Thavendiranathan, 2005) Preterm neonates (Rosebraugh, 2013) Elderly trauma patients – lower Hemoglobin on admission and discharge, need control of phlebotomy blood loss (Loftus, 2018)
Hospital Acquired Anemia ▶ Choosing Wisely Guidelines, Critical Care Societies Collaborative ▶ Identifies unnecessary phlebotomy as cause of potential harm ▶ Added risk of associated transfusion ▶ Excessive costs (Lutz & Cho, 2016)
Accuracy of Lab Data ▶ Blood cultures ▶ Inadequate skin antisepsis, lack of asepsis ▶ Skin fragments with venipuncture (Rupp, 2017) ▶ Not enough volume collected, 2 bottles with 10 m. L each ▶ reduces sensitivity by 3% for each m. L missed (van Ingen, 2013)
Accuracy of Lab Data ▶ Drug adsorption by intraluminal CVAD walls ▶ Can alter therapeutic drug level monitoring ▶ Coagulation tests ▶ Antibiotics ▶ Immunosuppression drugs
CLABSI and Phlebotomy ▶ Increased hub manipulation = increased risk of CLABSI ▶ Requires risk to benefit assessment for each patient (Gorski, 2016)
CLABSI and Phlebotomy ▶ ▶ No Central Line Blood Draw program ▶ Acute Care unit in large medical center decreased CLABSI rates from 2. 99/1000 catheter days to Zero ▶ From average of 6 draws per day to 1. 4 per day (Williamson, 2017) Increased hub manipulation = increased risk of CLABSI ▶ Risk factor in neutropenic acute leukemia patients (Martinez, 2018)
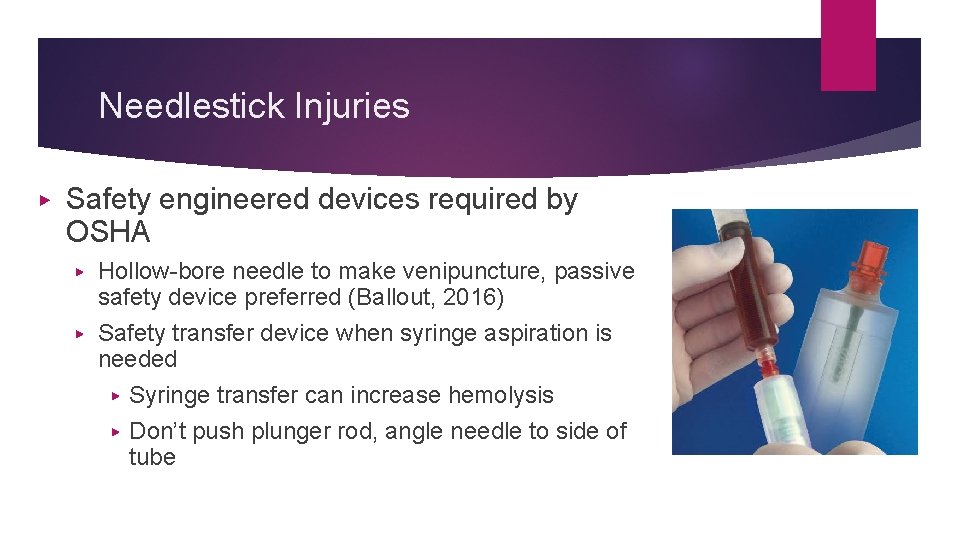
Needlestick Injuries ▶ Safety engineered devices required by OSHA Hollow-bore needle to make venipuncture, passive safety device preferred (Ballout, 2016) ▶ Safety transfer device when syringe aspiration is needed ▶ Syringe transfer can increase hemolysis ▶ Don’t push plunger rod, angle needle to side of tube ▶
Needlestick Injuries ▶ “Review specimen collection systems to identify opportunities to consolidate and eliminate unnecessary punctures, a strategy that is good for both patients and healthcare personnel. ” (CDC, 2008)
Phlebotomy Services ▶ Who is performing phlebotomy? ▶ Facility-based decision ▶ Phlebotomist based in Laboratory Dept ▶ Consistent practices directed by Lab Management ▶ Quality improvement, changes implemented quickly ▶ Nursing unit or department personnel ▶ Inconsistent practices ▶ Shifting personnel costs from Lab to other departments
Phlebotomy Services ▶ Who are decision-makers for ▶ Standardized policy and procedure development ▶ Technology being used ▶ Communicating changes to staff ▶ Job descriptions for all personnel involved with phlebotomy
Who is Phlebotomist? ▶ Job title or assigned role? ▶ Job title for unlicensed personnel in Lab ▶ Assigned role for all others ▶ ▶ Nursing – RN, LP/VN. Unlicensed assistive personnel (UAP) ▶ Licensed independent providers (MD, NP, PA) ▶ Respiratory therapist ▶ Paramedics Pre-analytical errors ▶ Associated with personnel outside of Lab Dept
Scope of Practice Issues ▶ Licensed personnel ▶ ▶ Defined legal scope of practice in state practice acts All unlicensed personnel ▶ No legal scope of practice ▶ May require delegation of tasks from licensed to unlicensed personnel
Phlebotomy Competency ▶ Knowledge acquisition and critical thinking ▶ Anatomy of peripheral veins ▶ Venous site selection ▶ Devices used – design and indications for use ▶ Infection prevention ▶ Complications – nerve injury, infection ▶ Hospital policies and procedures ▶ Classroom or online delivery
Phlebotomy Competency ▶ Psychomotor skills to use devices and employ correct techniques ▶ ▶ Repeated deliberate practice in simulation lab Successful clinical skills observed and measured ▶ Documented by complication of skills checklist or global rating scale
Risk Reduction - Techniques ▶ Bundling daily tests, scheduling together ▶ Documentation of daily blood loss from phlebotomy for all ages ▶ Phlebotomy procedural checklist ▶ Specimen receipt record in lab, focus on turnaround time reduction ▶ Point of care testing (POCT)
Risk Reduction - Techniques ▶ Vacuum tubes versus syringe method Syringe method requires steps to transfer to tubes ▶ Blood exposure ▶ Safety transfer device required ▶ No additives in syringes as in tubes ▶ ▶ Micro-volume testing ▶ Small volume tubes
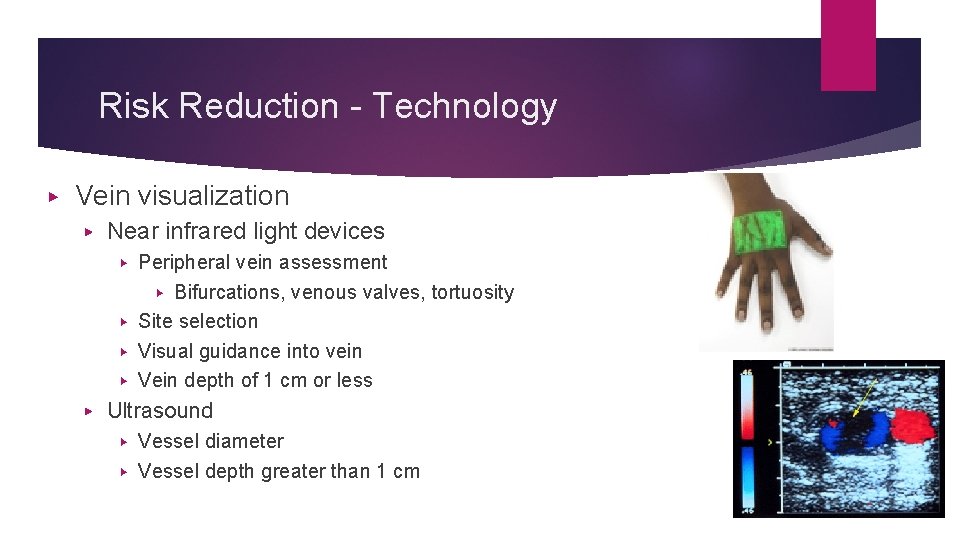
Risk Reduction - Technology ▶ Vein visualization ▶ Near infrared light devices Peripheral vein assessment ▶ Bifurcations, venous valves, tortuosity ▶ Site selection ▶ Visual guidance into vein ▶ Vein depth of 1 cm or less ▶ ▶ Ultrasound Vessel diameter ▶ Vessel depth greater than 1 cm ▶
Risk Reduction - Technology ▶ Administration set devices ▶ Closed system devices for arterial and venous infusions ▶ Eliminates blood waste ▶ More common in critical care ▶ PICU nurse survey – more difficulty with small VAD, lack of education with device (Steffen, 2017)
Risk Reduction - Technology ▶ Catheter-based device ▶ Thin long tube advanced through PIV lumen ▶ Extends beyond catheter tip ▶ Discard volume eliminated ▶ Used by nursing personnel and UAPs through intermittent PIVCs
Risk Reduction - Technology ▶ Flushing before and after with prefilled flush syringes ▶ FDA - Prefilled flush syringe is device, not a drug ▶ Medical device – “does not achieve primary intended purposes through chemical action within or on the body of man or other animals and which is not dependent upon being metabolized for the achievement of any of its primary intended purposes. ” (FDA, 2014)
Risk Reduction - Technology ▶ Catheter-based device studies in healthy volunteers ▶ No hemolysis in study with volunteers (Cadacio, 2017) – 51 paired samples ▶ Flush volume and wait time in 27 subjects ▶ 4 samples from device in PIV of forearm, plus direct venipuncture in opposite arm ▶ Sodium and creatinine values ▶ Results – Flush, 30 -second wait, no waste required (Adams, 2018)
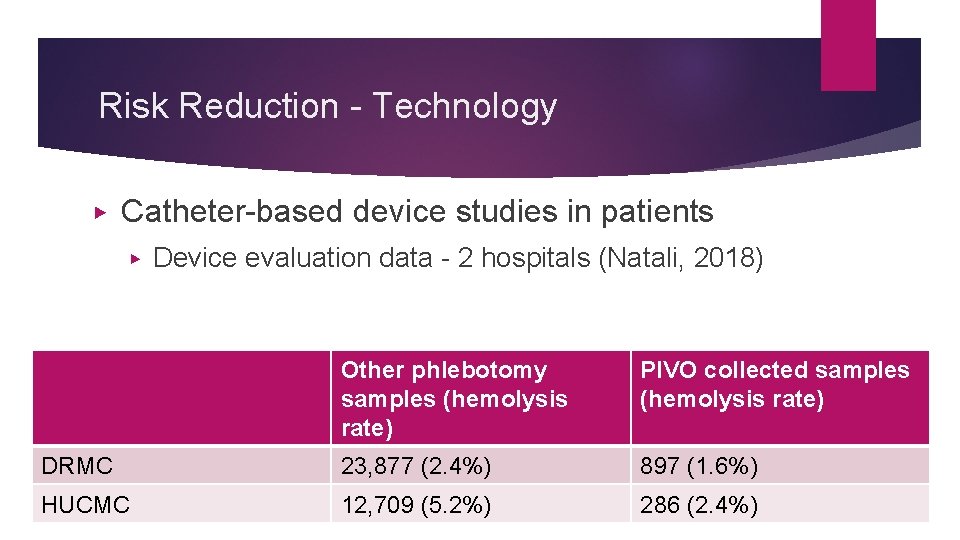
Risk Reduction - Technology ▶ Catheter-based device studies in patients ▶ Device evaluation data - 2 hospitals (Natali, 2018) Other phlebotomy samples (hemolysis rate) PIVO collected samples (hemolysis rate) DRMC 23, 877 (2. 4%) 897 (1. 6%) HUCMC 12, 709 (5. 2%) 286 (2. 4%)
Risk Reduction - Technology ▶ Catheter-based device studies in patients, cont ▶ RCT in 138 GI surgical patients to assess dwell time and reliability of catheter based device (Mulloy, 2018) ▶ Preop insertion of 18 or 20 gauge PIVC ▶ 68 patients (73 PIVC) with daily blood samples drawn through catheter based device; 9. 6% replaced; survival time 2. 77 days ▶ 70 patients, (79 PIVC) with PIVC only; 15. 2% replaced; survival time 2. 75 days ▶ ▶ No statistical difference; intervention group survival rate not inferior to control Blood collection 81% successful in intervention group (62 patients, 126 samples, no hemolysis)
Your Role in Phlebotomy ▶ Focus on pre-analytical phase to reduce errors ▶ ▶ System-wide problem Collaboration with Laboratory Services Accurate test results critical for correct diagnoses and treatment Vein preservation! ▶ Reduce need for CVADs over the life of patient
Your Role in Phlebotomy ▶ Reduce CLABSI rates ▶ Reduce needle use to reduce needlestick injuries ▶ Reduce anemia and risk of blood transfusion ▶ Improve phlebotomy practices by all staff ▶ UAPs regardless of job title and all nursing staff ▶ Education ▶ Competency assessment and validation
- Slides: 63