PhenytoinInduced Purple Glove Syndrome A Case Report Rebecca
Phenytoin-Induced Purple Glove Syndrome: A Case Report Rebecca Chow, Pharm. D PGY-1 Pharmacy Practice Resident 1
Disclosures Neither the presenter nor the planning committee has received any commercial support associated with this educational activity. 2
Objectives • Identify the early signs of phenytoininduced purple glove syndrome • Describe the prevention and management of purple glove syndrome 3
Outline • Background • Patient Case at RWJUH Somerset • Identification, Management, and Prevention of Purple Glove Syndrome • Conclusion 4
BACKGROUND: PHENYTOIN AND PURPLE GLOVE SYNDROME 5
Phenytoin • Anticonvulsant commonly used intravenously in status epilepticus • Mechanism of Action – Blocks sodium channels to stabilize membrane and decrease seizure activity • Adverse Events – Hypotension, arrhythmias, hepatotoxicity Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. 6
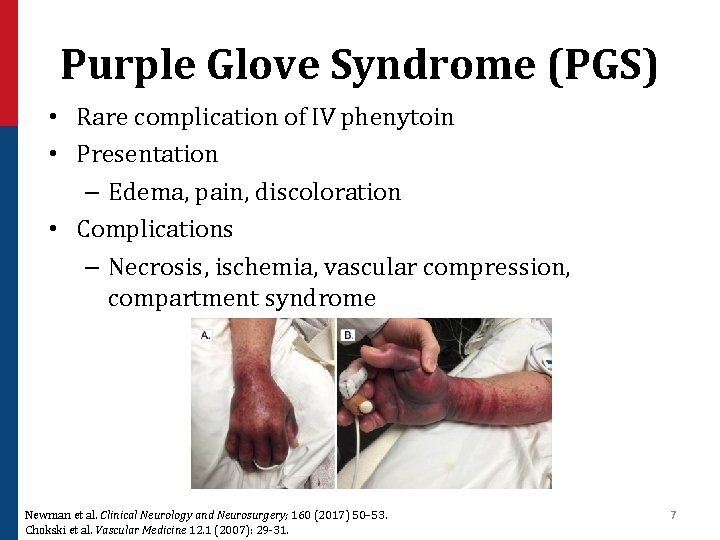
Purple Glove Syndrome (PGS) • Rare complication of IV phenytoin • Presentation – Edema, pain, discoloration • Complications – Necrosis, ischemia, vascular compression, compartment syndrome Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. Chokski et al. Vascular Medicine 12. 1 (2007): 29 -31. 7
Proposed Mechanisms of PGS • Small vascular tears allow for leakage of alkaline phenytoin solution • Drug solution induces vasoconstriction and irritation of soft tissue • Drug-induced vasculitis Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. Garbovsky et al. Journal of Medical Toxicology 11. 4 (2015): 445 -459. 8
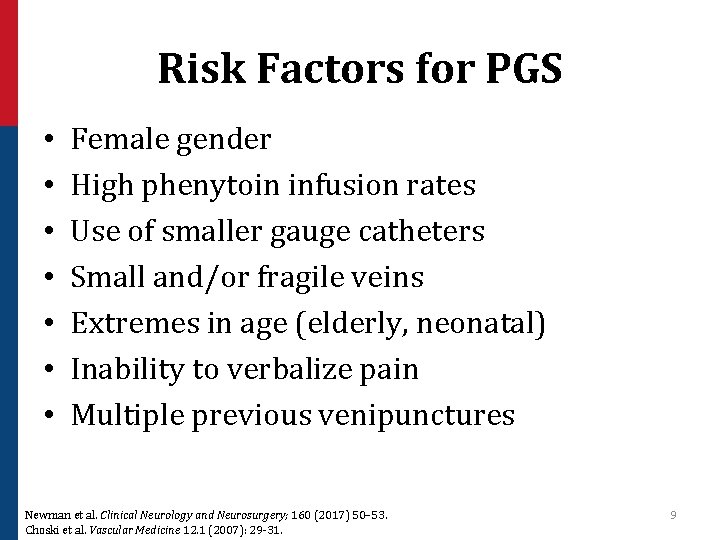
Risk Factors for PGS • • Female gender High phenytoin infusion rates Use of smaller gauge catheters Small and/or fragile veins Extremes in age (elderly, neonatal) Inability to verbalize pain Multiple previous venipunctures Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. Choski et al. Vascular Medicine 12. 1 (2007): 29 -31. 9
PATIENT CASE AT RWJUH SOMERSET 10
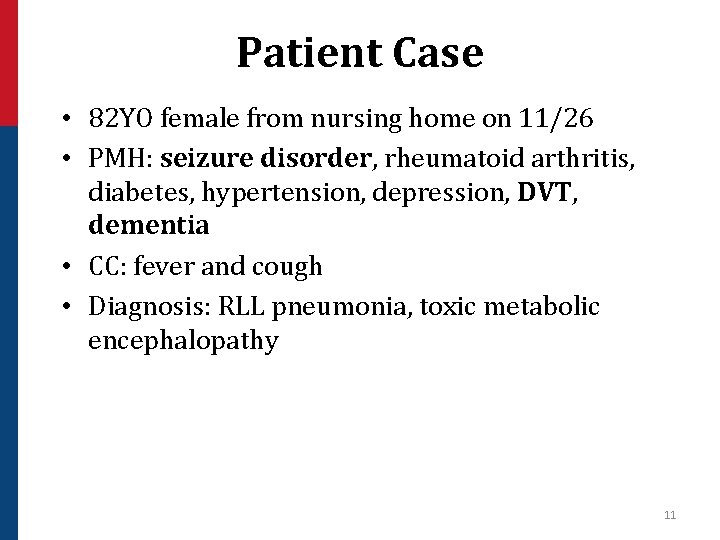
Patient Case • 82 YO female from nursing home on 11/26 • PMH: seizure disorder, rheumatoid arthritis, diabetes, hypertension, depression, DVT, dementia • CC: fever and cough • Diagnosis: RLL pneumonia, toxic metabolic encephalopathy 11
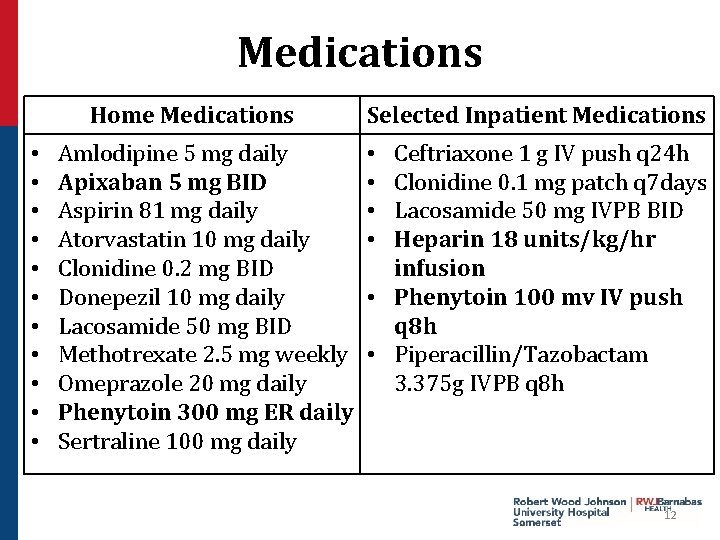
Medications Home Medications • • • Amlodipine 5 mg daily Apixaban 5 mg BID Aspirin 81 mg daily Atorvastatin 10 mg daily Clonidine 0. 2 mg BID Donepezil 10 mg daily Lacosamide 50 mg BID Methotrexate 2. 5 mg weekly Omeprazole 20 mg daily Phenytoin 300 mg ER daily Sertraline 100 mg daily Selected Inpatient Medications Ceftriaxone 1 g IV push q 24 h Clonidine 0. 1 mg patch q 7 days Lacosamide 50 mg IVPB BID Heparin 18 units/kg/hr infusion • Phenytoin 100 mv IV push q 8 h • Piperacillin/Tazobactam 3. 375 g IVPB q 8 h • • 12
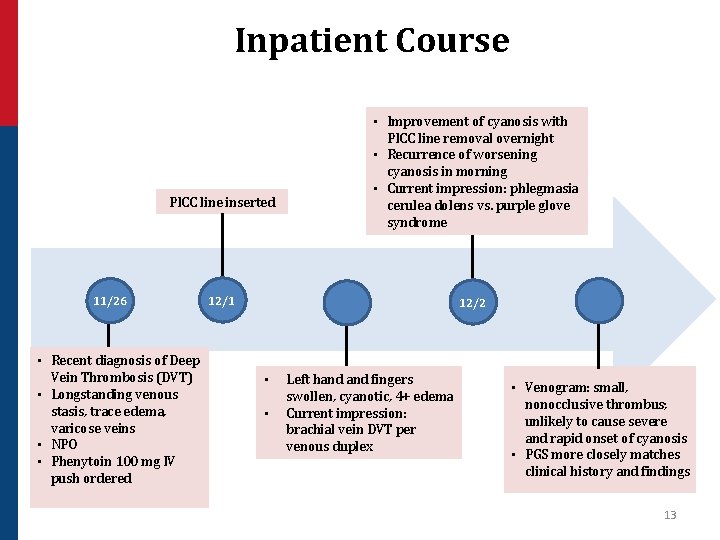
Inpatient Course PICC line inserted 11/26 • Recent diagnosis of Deep Vein Thrombosis (DVT) • Longstanding venous stasis, trace edema, varicose veins • NPO • Phenytoin 100 mg IV push ordered • Improvement of cyanosis with PICC line removal overnight • Recurrence of worsening cyanosis in morning • Current impression: phlegmasia cerulea dolens vs. purple glove syndrome 12/1 12/2 • • Left hand fingers swollen, cyanotic, 4+ edema Current impression: brachial vein DVT per venous duplex • Venogram: small, nonocclusive thrombus; unlikely to cause severe and rapid onset of cyanosis • PGS more closely matches clinical history and findings 13
IDENTIFICATION, MANAGEMENT, AND PREVENTION OF PGS 14
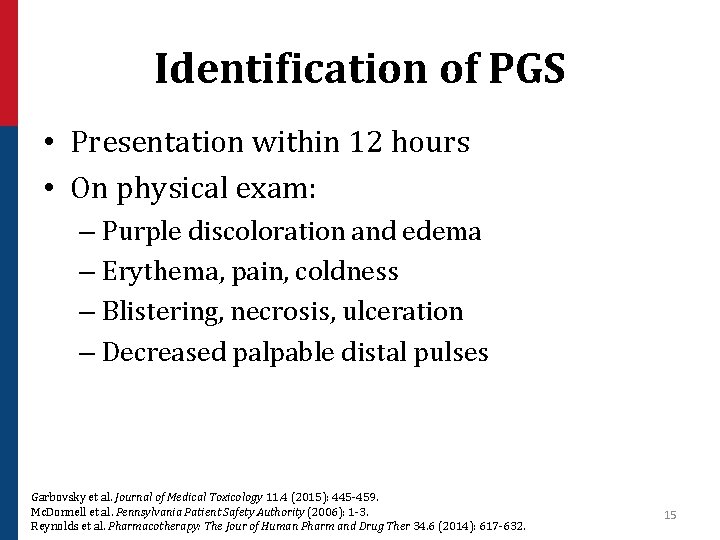
Identification of PGS • Presentation within 12 hours • On physical exam: – Purple discoloration and edema – Erythema, pain, coldness – Blistering, necrosis, ulceration – Decreased palpable distal pulses Garbovsky et al. Journal of Medical Toxicology 11. 4 (2015): 445 -459. Mc. Donnell et al. Pennsylvania Patient Safety Authority (2006): 1 -3. Reynolds et al. Pharmacotherapy: The Jour of Human Pharm and Drug Ther 34. 6 (2014): 617 -632. 15
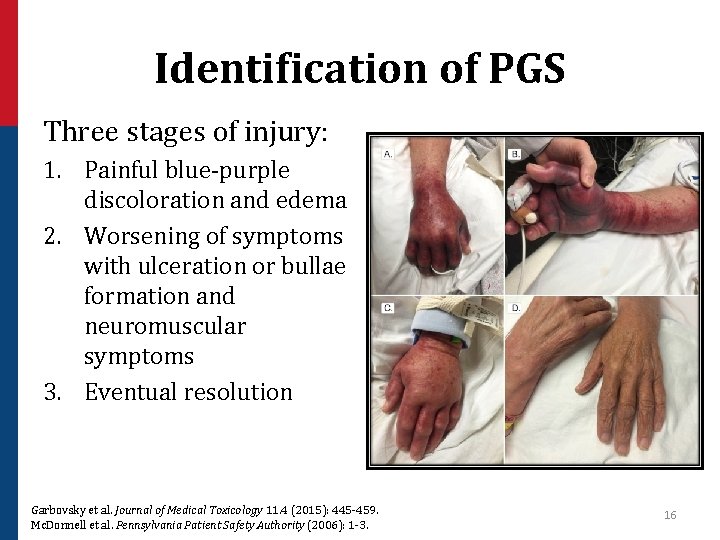
Identification of PGS Three stages of injury: 1. Painful blue-purple discoloration and edema 2. Worsening of symptoms with ulceration or bullae formation and neuromuscular symptoms 3. Eventual resolution Garbovsky et al. Journal of Medical Toxicology 11. 4 (2015): 445 -459. Mc. Donnell et al. Pennsylvania Patient Safety Authority (2006): 1 -3. 16
Differential for PGS • • • Deep vein thrombosis Cellulitis Intravenous infiltration Necrotizing fasciitis Compartment syndrome Raynaud’s phenomenon Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. 17
Management of PGS • Discontinue IV phenytoin • Supportive care – Limb elevation – Local dry heat application – Pain management • Pharmacological interventions – Intradermal hyaluronidase – Topical nitroglycerin Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. Reynolds et al. Pharmacotherapy: The Jour of Human Pharm and Drug Ther 34. 6 (2014): 617 -632. Sokol et al. Jour of Child Neuro 13. 5 (1998): 246 Edwards et al. Anesthesia & Analgesia 94. 3 (2002): 672 -673. 18
Prevention of PGS • Maximum rate of 50 mg/min • Avoid dextrose; dilute in normal saline only • Use of IV catheters larger than 20 gauge with 0. 22 micron in-line filter • Flush with normal saline before and following administration • Use of large-bore veins only Newman et al. Clinical Neurology and Neurosurgery; 160 (2017) 50– 53. Mc. Donnell et al. Pennsylvania Patient Safety Authority (2006): 1 -3. 19
BACK TO PATIENT CASE… 20
Patient Follow Up • Fasciotomy or amputation of hand • Patient deteriorating, family declined interventions • Transferred to hospice 21
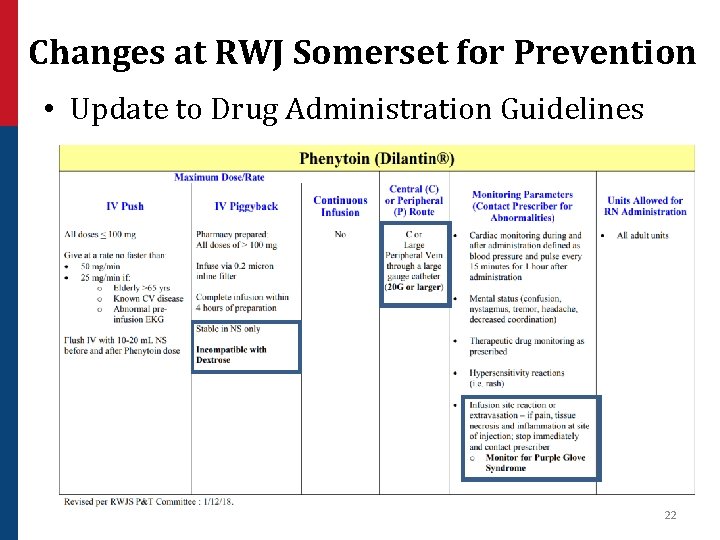
Changes at RWJ Somerset for Prevention • Update to Drug Administration Guidelines 22
Conclusions • Hallmark signs and symptoms - purple discoloration and edema • Management - supportive care with weak evidence for pharmacological agents • Prevention of phenytoin- induced PGS includes education to interdisciplinary team 23
Assessment Question 1 • Which of the following is a method to prevent PGS? a) b) c) d) Ensure only diluted in dextrose Use of IV catheters larger than 20 gauge Utilize a 0. 1 micron filter Use of small veins only 24
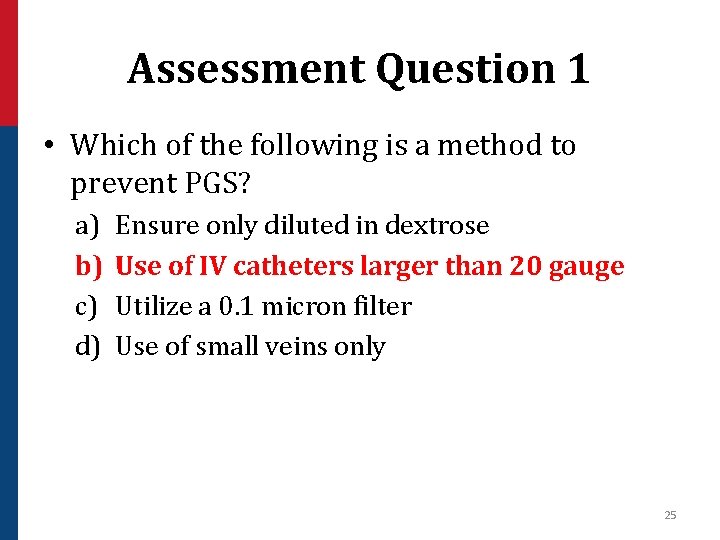
Assessment Question 1 • Which of the following is a method to prevent PGS? a) b) c) d) Ensure only diluted in dextrose Use of IV catheters larger than 20 gauge Utilize a 0. 1 micron filter Use of small veins only 25
Assessment Question 2 • Which of the following is an appropriate intervention for management of PGS? a) b) c) d) Limb elevation Cold compress Warm, moist compress Switch to fosphenytoin 26
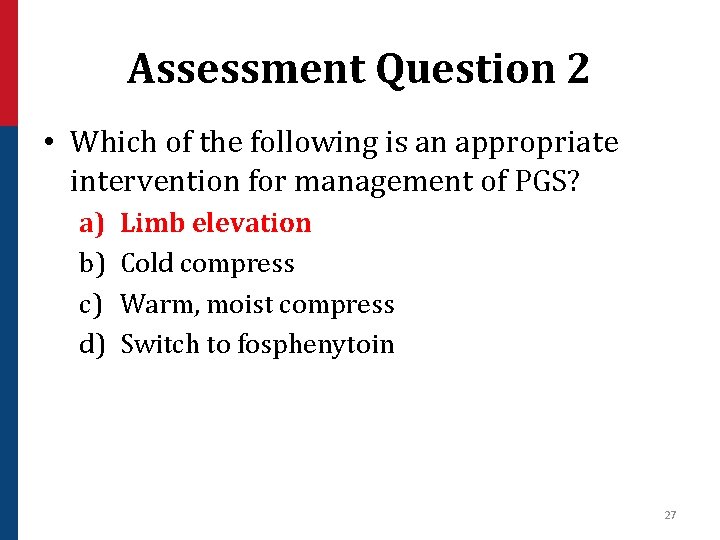
Assessment Question 2 • Which of the following is an appropriate intervention for management of PGS? a) b) c) d) Limb elevation Cold compress Warm, moist compress Switch to fosphenytoin 27
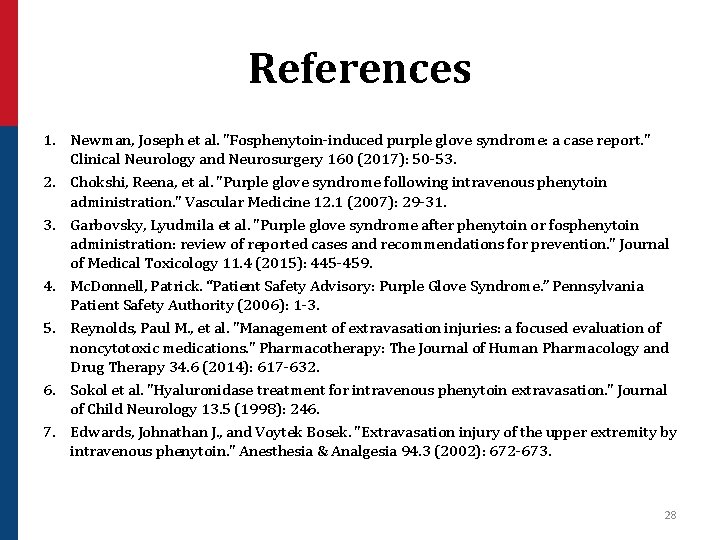
References 1. Newman, Joseph et al. "Fosphenytoin-induced purple glove syndrome: a case report. " Clinical Neurology and Neurosurgery 160 (2017): 50 -53. 2. Chokshi, Reena, et al. "Purple glove syndrome following intravenous phenytoin administration. " Vascular Medicine 12. 1 (2007): 29 -31. 3. Garbovsky, Lyudmila et al. "Purple glove syndrome after phenytoin or fosphenytoin administration: review of reported cases and recommendations for prevention. " Journal of Medical Toxicology 11. 4 (2015): 445 -459. 4. Mc. Donnell, Patrick. “Patient Safety Advisory: Purple Glove Syndrome. ” Pennsylvania Patient Safety Authority (2006): 1 -3. 5. Reynolds, Paul M. , et al. "Management of extravasation injuries: a focused evaluation of noncytotoxic medications. " Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy 34. 6 (2014): 617 -632. 6. Sokol et al. "Hyaluronidase treatment for intravenous phenytoin extravasation. " Journal of Child Neurology 13. 5 (1998): 246. 7. Edwards, Johnathan J. , and Voytek Bosek. "Extravasation injury of the upper extremity by intravenous phenytoin. " Anesthesia & Analgesia 94. 3 (2002): 672 -673. 28
Phenytoin-Induced Purple Glove Syndrome: A Case Report Rebecca Chow, Pharm. D PGY-1 Pharmacy Practice Resident 29
- Slides: 29