Pharmacy Speaks Making the case for PCN integration


- Slides: 26
#Pharmacy. Speaks Making the case for PCN integration – challenges and opportunities Michael Lennox

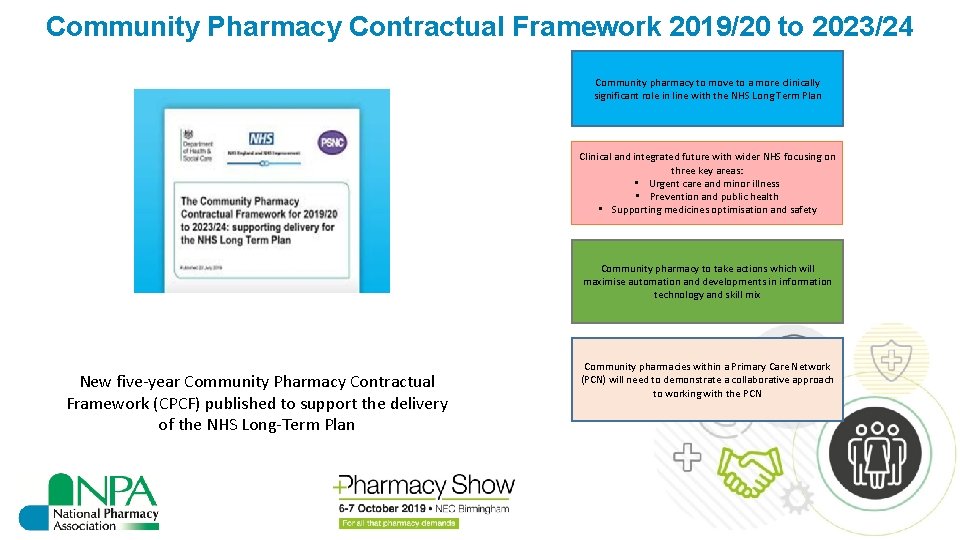
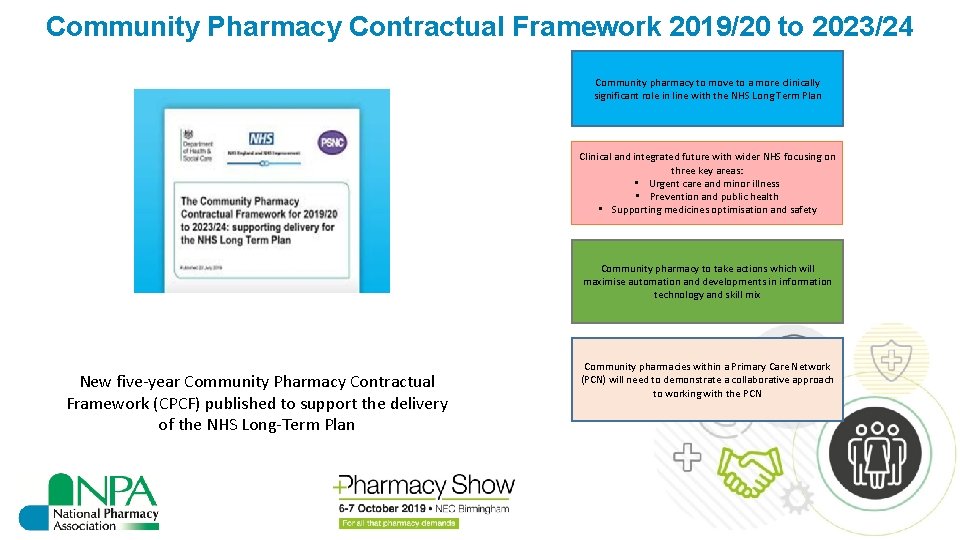
Community Pharmacy Contractual Framework 2019/20 to 2023/24 Community pharmacy to move to a more clinically significant role in line with the NHS Long Term Plan Clinical and integrated future with wider NHS focusing on three key areas: • Urgent care and minor illness • Prevention and public health • Supporting medicines optimisation and safety Community pharmacy to take actions which will maximise automation and developments in information technology and skill mix New five-year Community Pharmacy Contractual Framework (CPCF) published to support the delivery of the NHS Long-Term Plan Community pharmacies within a Primary Care Network (PCN) will need to demonstrate a collaborative approach to working with the PCN
The core funding for England’s pharmacies announced in July for the next five years is very unlikely to be enough to achieve the transformational improvements the NHS and pharmacists would like to see. For some pharmacies, it won’t even be enough to keep the doors open, unless other substantial sources of income can be found.
NPA position We need a sustainable business model which delivers a fair return for investment. The current situation is not only a disincentive to invest, but also it means that many of us are struggling to find the time to engage in new ventures whether that is local integration with Primary Care Networks, or gearing up for national services such as CPCS. There is risk of a widening gap from where contractors are now to where the NHS needs us to be.
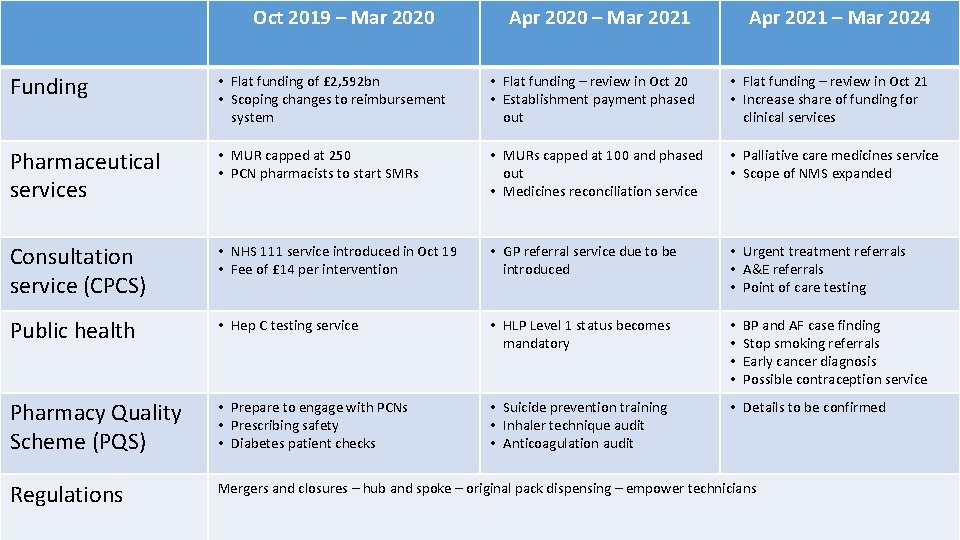
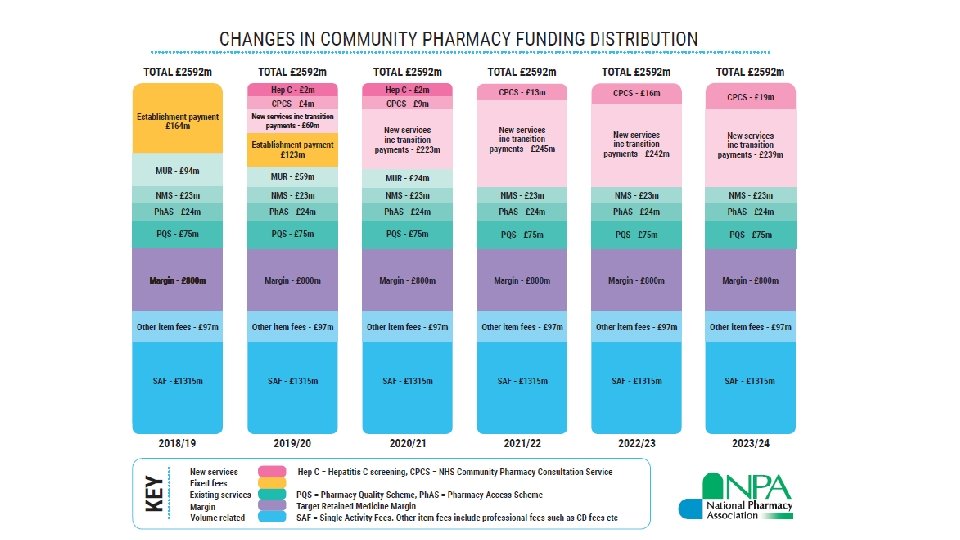
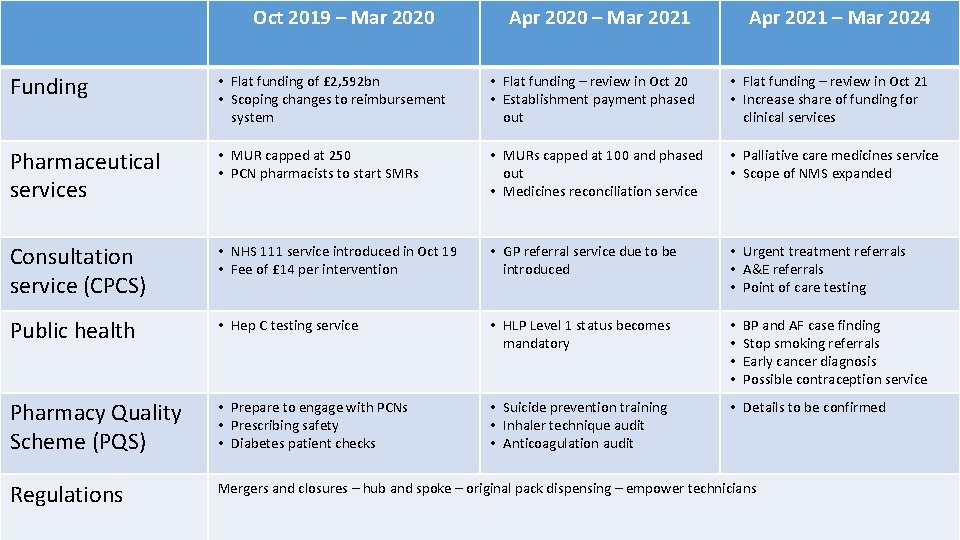
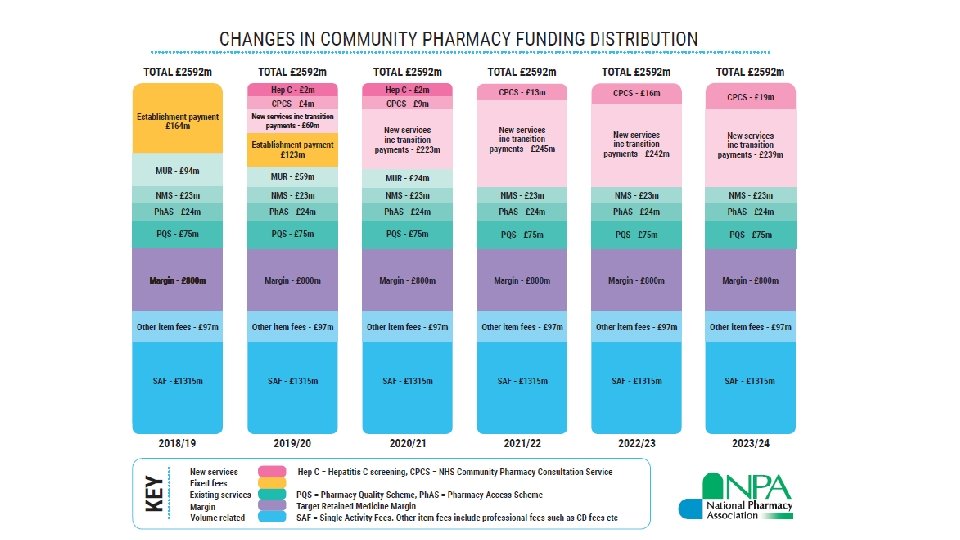
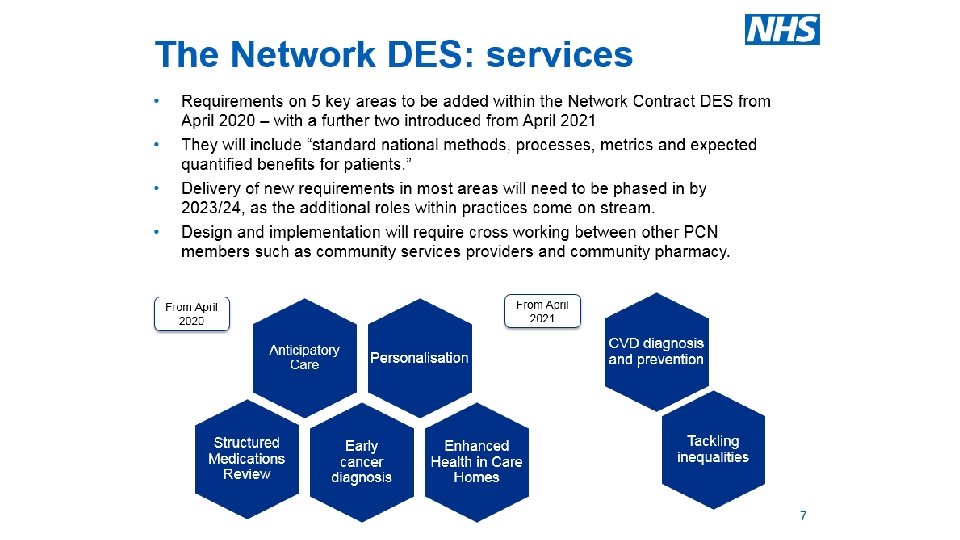
Oct 2019 – Mar 2020 Apr 2020 – Mar 2021 Apr 2021 – Mar 2024 Funding • Flat funding of £ 2, 592 bn • Scoping changes to reimbursement system • Flat funding – review in Oct 20 • Establishment payment phased out • Flat funding – review in Oct 21 • Increase share of funding for clinical services Pharmaceutical services • MUR capped at 250 • PCN pharmacists to start SMRs • MURs capped at 100 and phased out • Medicines reconciliation service • Palliative care medicines service • Scope of NMS expanded Consultation service (CPCS) • NHS 111 service introduced in Oct 19 • Fee of £ 14 per intervention • GP referral service due to be introduced • Urgent treatment referrals • A&E referrals • Point of care testing Public health • Hep C testing service • HLP Level 1 status becomes mandatory • • Pharmacy Quality Scheme (PQS) • Prepare to engage with PCNs • Prescribing safety • Diabetes patient checks • Suicide prevention training • Inhaler technique audit • Anticoagulation audit • Details to be confirmed Regulations Mergers and closures – hub and spoke – original pack dispensing – empower technicians BP and AF case finding Stop smoking referrals Early cancer diagnosis Possible contraception service
Fundamentally, the shift to services implied in the new contractual framework for pharmacies in England presents an opportunity for those who can build on the strength of their relationships, with patients and others locally, to deliver high quality, compassionate care and reap the rewards professionally and commercially.
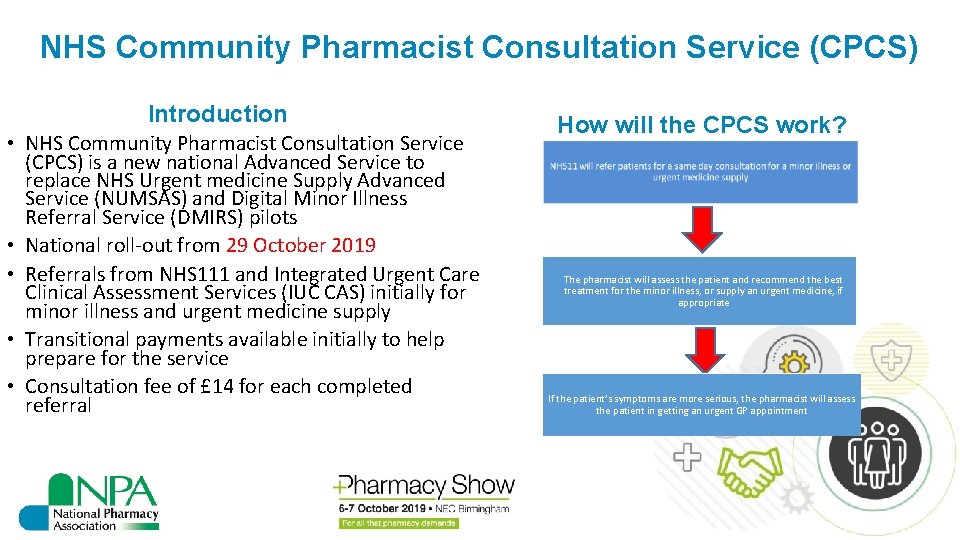
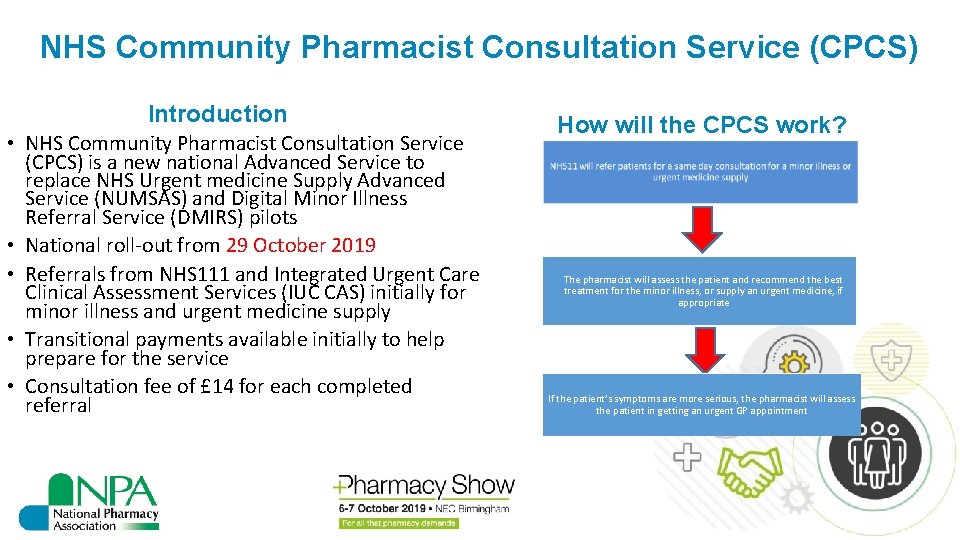
NHS Community Pharmacist Consultation Service (CPCS) Introduction • NHS Community Pharmacist Consultation Service (CPCS) is a new national Advanced Service to replace NHS Urgent medicine Supply Advanced Service (NUMSAS) and Digital Minor Illness Referral Service (DMIRS) pilots • National roll-out from 29 October 2019 • Referrals from NHS 111 and Integrated Urgent Care Clinical Assessment Services (IUC CAS) initially for minor illness and urgent medicine supply • Transitional payments available initially to help prepare for the service • Consultation fee of £ 14 for each completed referral How will the CPCS work? The pharmacist will assess the patient and recommend the best treatment for the minor illness, or supply an urgent medicine, if appropriate If the patient’s symptoms are more serious, the pharmacist will assess the patient in getting an urgent GP appointment
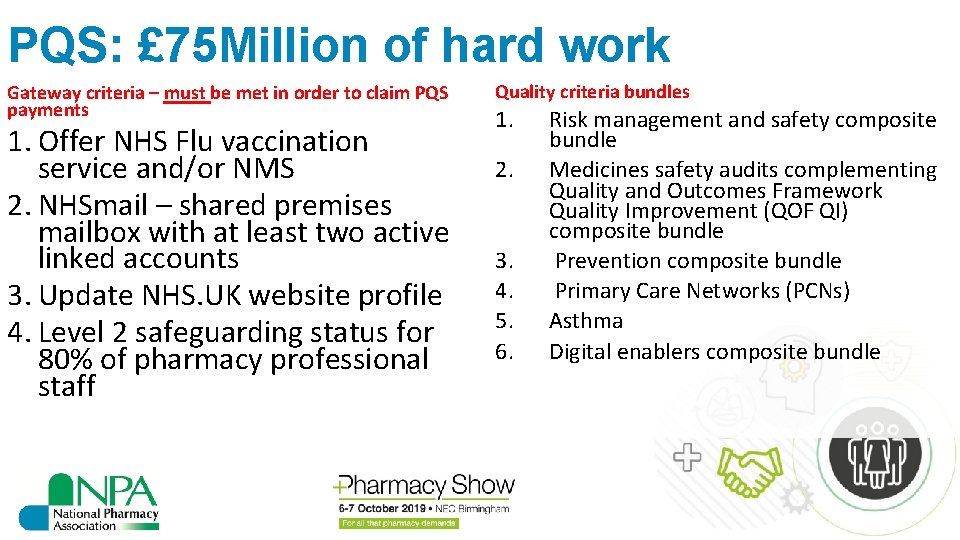
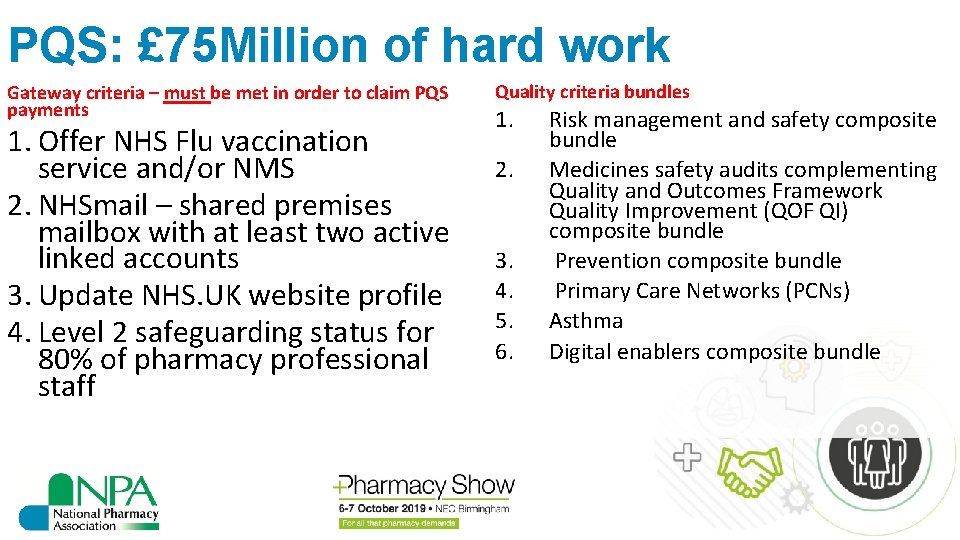
PQS: £ 75 Million of hard work Gateway criteria – must be met in order to claim PQS payments 1. Offer NHS Flu vaccination service and/or NMS 2. NHSmail – shared premises mailbox with at least two active linked accounts 3. Update NHS. UK website profile 4. Level 2 safeguarding status for 80% of pharmacy professional staff Quality criteria bundles 1. 2. 3. 4. 5. 6. Risk management and safety composite bundle Medicines safety audits complementing Quality and Outcomes Framework Quality Improvement (QOF QI) composite bundle Prevention composite bundle Primary Care Networks (PCNs) Asthma Digital enablers composite bundle
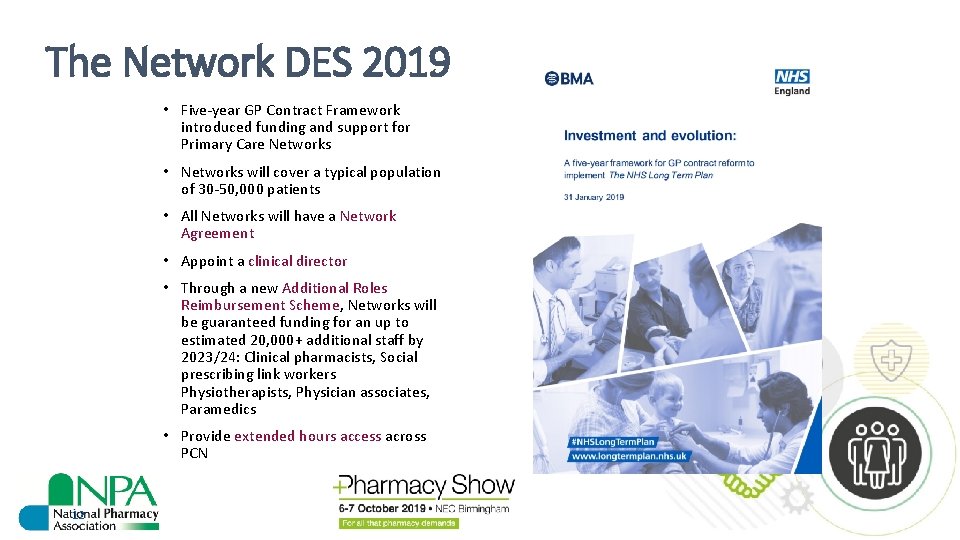
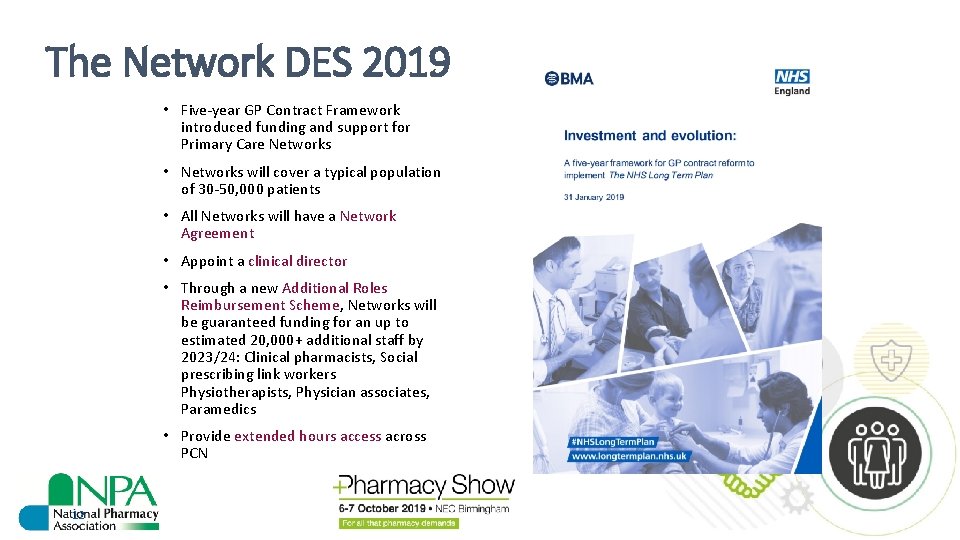
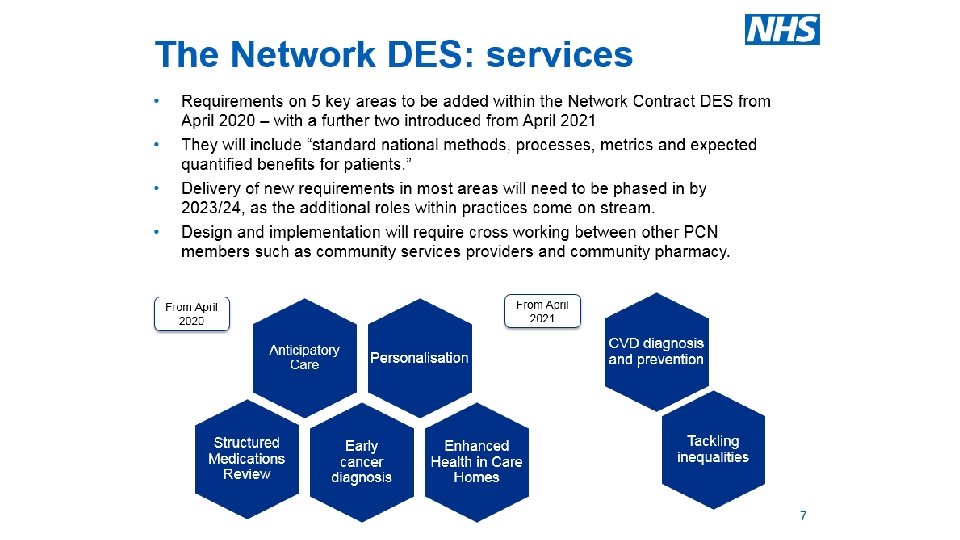
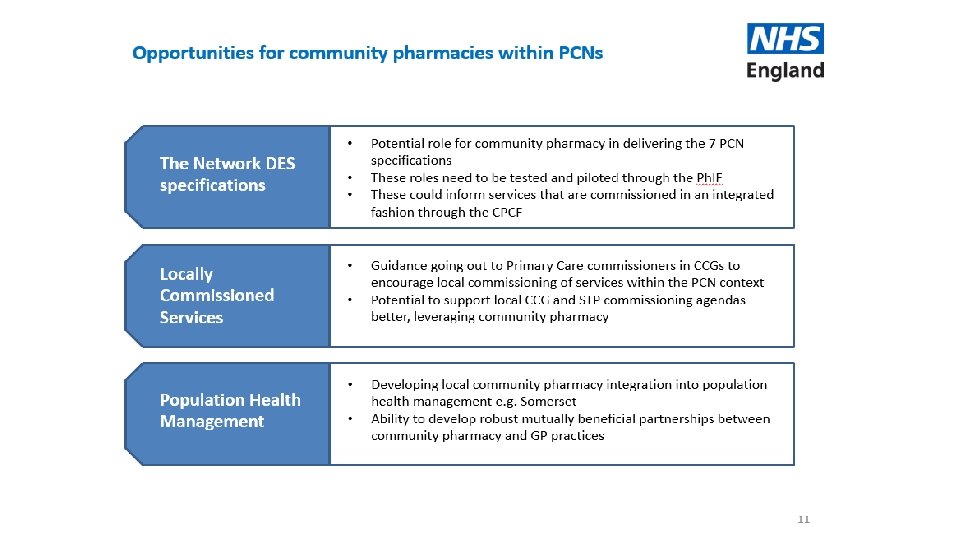
The Network DES 2019 • Five-year GP Contract Framework introduced funding and support for Primary Care Networks • Networks will cover a typical population of 30 -50, 000 patients • All Networks will have a Network Agreement • Appoint a clinical director • Through a new Additional Roles Reimbursement Scheme, Networks will be guaranteed funding for an up to estimated 20, 000+ additional staff by 2023/24: Clinical pharmacists, Social prescribing link workers Physiotherapists, Physician associates, Paramedics • Provide extended hours access across PCN 12
How will PCNs improve primary care? • Strengthen and redesign health and social care, bring together a range of professionals to work together to provide enhanced personalised and preventative care for their local community • Provide structure and funding for services to be developed locally • Align clinical and financial aims and a unified, capitated budget – making joint decisions on how funding is spent • Share resources, employ a broader range of staff, extend services or offer new services
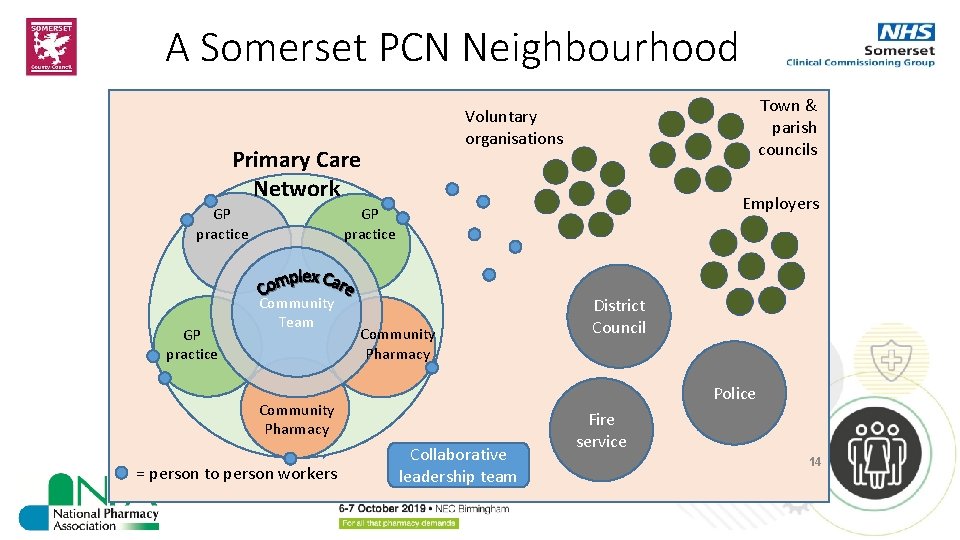
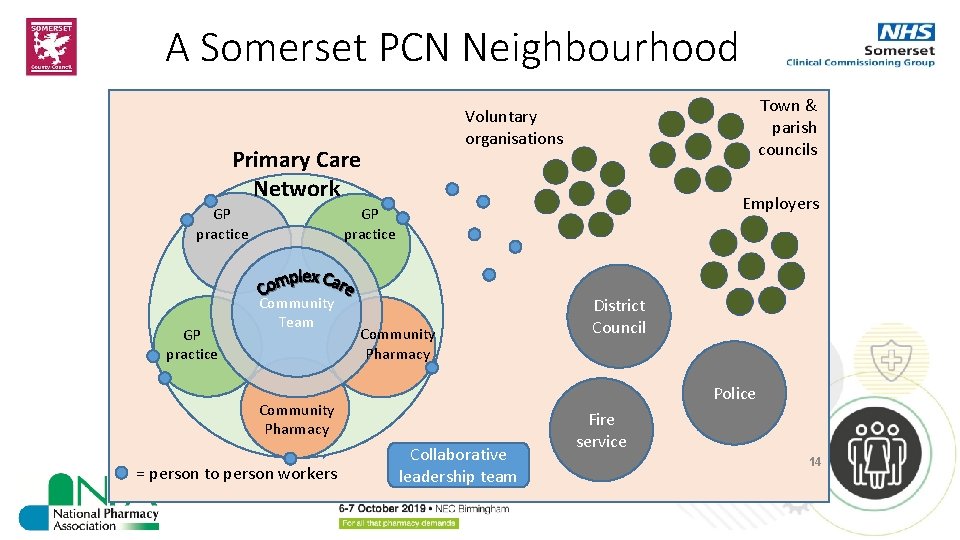
A Somerset PCN Neighbourhood Primary Care Network GP practice Town & parish councils Voluntary organisations Employers GP practice Community Team Community Pharmacy Police Community Pharmacy = person to person workers District Council Collaborative leadership team Fire service 14

Work together to Optimise Processes BAU WOW! 15
NPA position We support a future based on services, especially services that build on the frequent interaction local community pharmacies have with patients due to the access to medicines provided by pharmacies. We want a qualityfocused system that provides access to medicines and clinical services together.
NPA position Community pharmacies need to be recognised as the front door to health – an indispensable component of the urgent care pathway, vibrant health and wellbeing hubs and a mainstay of support for people with long-term medical conditions.
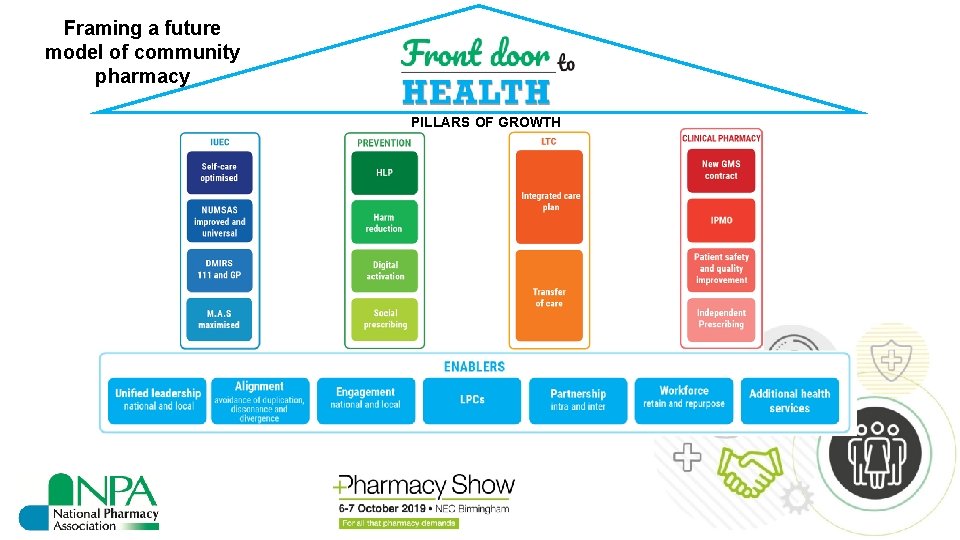
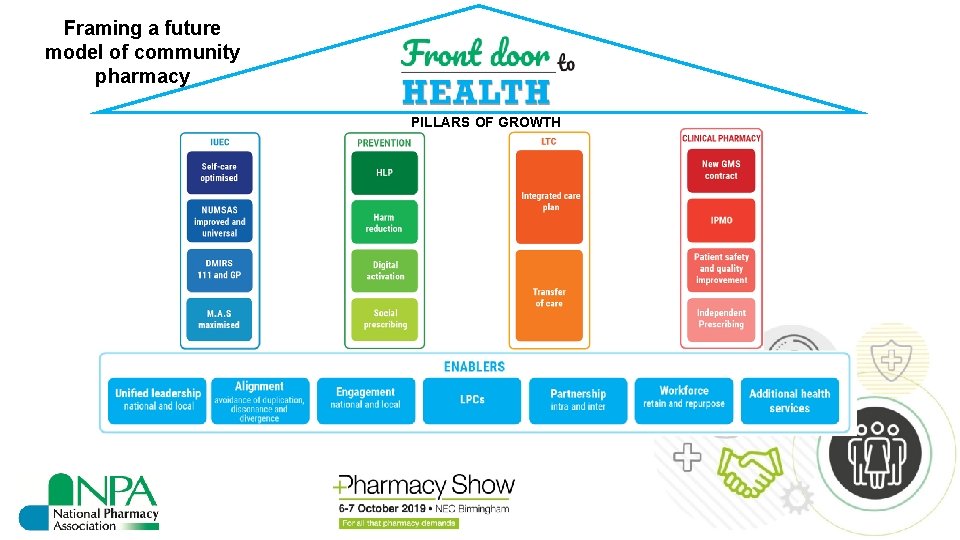
Framing a future model of community pharmacy PILLARS OF GROWTH
Priorities for community pharmacies in PCNs • NHS England sees the initial priorities for community pharmacy engagement in PCNs to be: • provision of integrated urgent care services e. g. CPCS (NUMSAS and DMIRS) • work on prevention, such as provision of public health interventions and services, building on the work of HLPs • These priorities are now reflected in changes to the community pharmacy contract in 2019/20 • Locally, other priorities may be agreed with PCN leaders, which may initially include optimising the provision of existing services, such as NMS and electronic repeat dispensing
Why should community pharmacies get involved? • The future development of local services will be influenced by PCNs • PCNs will be the local focus for primary care provision and potential future local sub-contracting • Provides the opportunity to work with other providers to plan and shape your role in local population health • There will be opportunities via PCNs, but only if you engage, collectively with other pharmacies • If you are not part of PCNs, then the system will likely bypass you and opportunities to better use your unique skillset will be lost
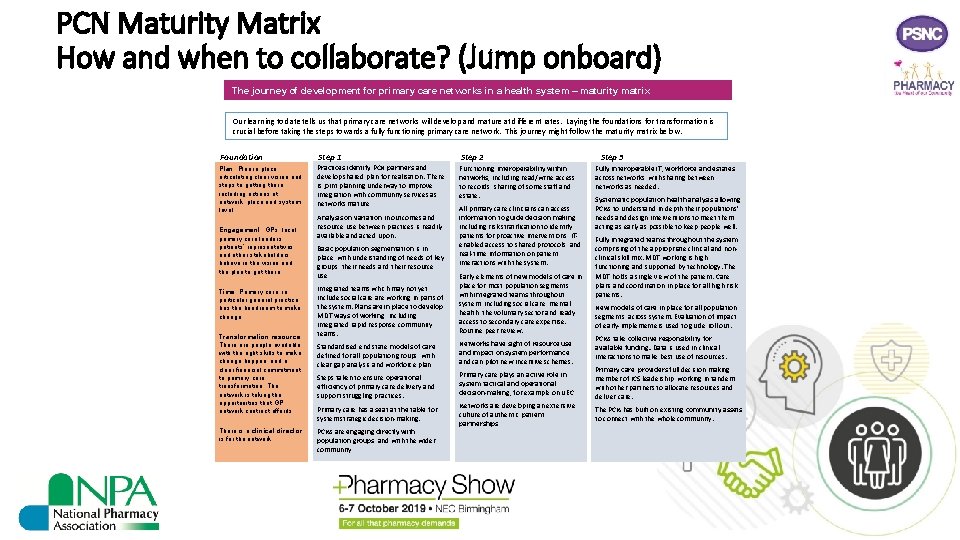
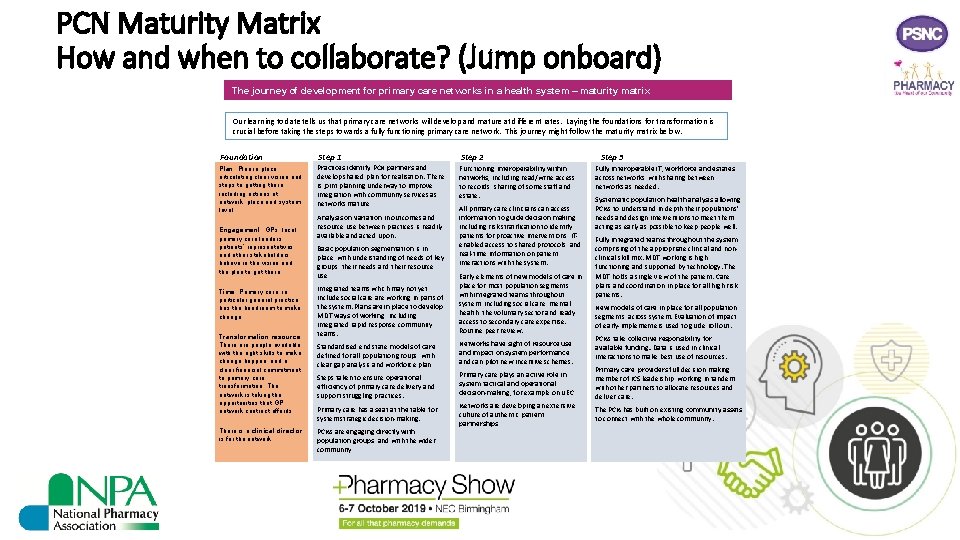
PCN Maturity Matrix How and when to collaborate? (Jump onboard) The journey of development for primary care networks in a health system – maturity matrix Our learning to date tells us that primary care networks will develop and mature at different rates. Laying the foundations for transformation is crucial before taking the steps towards a fully functioning primary care network. This journey might follow the maturity matrix below. Foundation Step 1 Step 2 Plan: Plan in place articulating clear vision and steps to getting there, including actions at network, place and system level. Practices identify PCN partners and develop shared plan for realisation. There is joint planning underway to improve integration with community services as networks mature Functioning interoperability within networks, including read/write access to records, sharing of some staff and estate. Engagement: GPs, local primary care leaders, patients’ representatives, and other stakeholders believe in the vision and the plan to get there. Time: Primary care, in particular general practice, has the headroom to make change. Transformation resource: There are people available with the right skills to make change happen, and a clear financial commitment to primary care transformation. The network is taking the opportunities that GP network contract affords There is a clinical director is for the network. Analysis on variation in outcomes and resource use between practices is readily available and acted upon. Basic population segmentation is in place, with understanding of needs of key groups, their needs and their resource use All primary care clinicians can access information to guide decision making, including risk stratification to identify patients for proactive interventions, ITenabled access to shared protocols, and real-time information on patient interactions with the system. Integrated teams which may not yet include social care working in parts of the system. Plans are in place to develop MDT ways of working, including integrated rapid response community teams. Early elements of new models of care in place for most population segments, with integrated teams throughout system, including social care, mental health, the voluntary sector and ready access to secondary care expertise. Routine peer review. Standardised end state models of care defined for all population groups, with clear gap analysis and workforce plan Networks have sight of resource use and impact on system performance, and can pilot new incentive schemes. Steps taken to ensure operational efficiency of primary care delivery and support struggling practices. Primary care plays an active role in system tactical and operational decision-making, for example on UEC Primary care has a seat at the table for system strategic decision-making. Networks are developing an extensive culture of authentic patient partnerships PCNs are engaging directly with population groups, and with the wider community Step 3 Fully interoperable IT, workforce and estates across networks, with sharing between networks as needed. Systematic population health analysis allowing PCNs to understand in depth their populations’ needs and design interventions to meet them, acting as early as possible to keep people well. Fully integrated teams throughout the system, comprising of the appropriate clinical and nonclinical skill mix. MDT working is high functioning and supported by technology. The MDT holds a single view of the patient. Care plans and coordination in place for all high risk patients. New models of care in place for all population segments, across system. Evaluation of impact of early-implementers used to guide roll out. PCNs take collective responsibility for available funding. Data is used in clinical interactions to make best use of resources. Primary care providers full decision making member of ICS leadership, working in tandem with other partners to allocate resources and deliver care. The PCN has built on existing community assets to connect with the whole community.
Collectiveyou responsibility Remember can not collaborate …………. . on your own
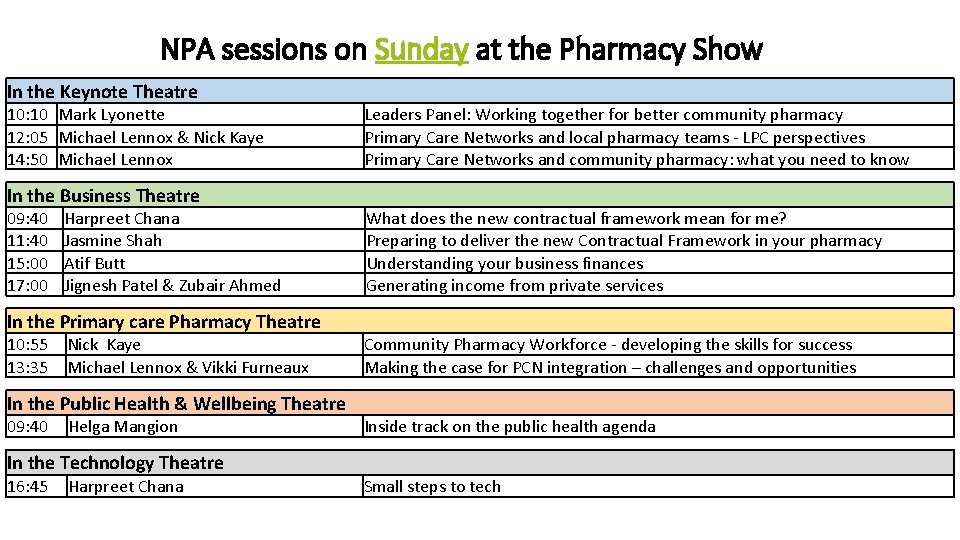
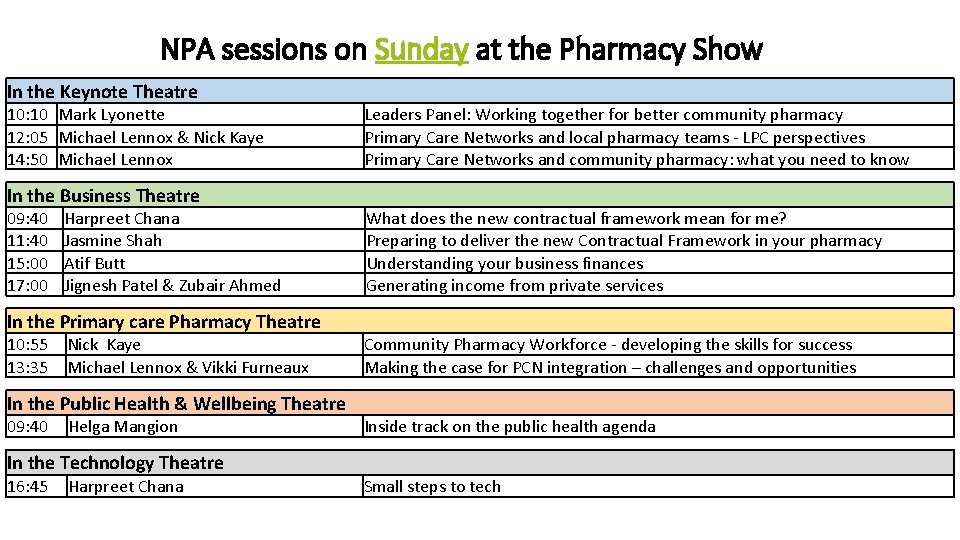
NPA sessions on Sunday at the Pharmacy Show In the Keynote Theatre 10: 10 Mark Lyonette 12: 05 Michael Lennox & Nick Kaye 14: 50 Michael Lennox Leaders Panel: Working together for better community pharmacy Primary Care Networks and local pharmacy teams - LPC perspectives Primary Care Networks and community pharmacy: what you need to know In the Business Theatre 09: 40 11: 40 15: 00 17: 00 Harpreet Chana Jasmine Shah Atif Butt Jignesh Patel & Zubair Ahmed What does the new contractual framework mean for me? Preparing to deliver the new Contractual Framework in your pharmacy Understanding your business finances Generating income from private services In the Primary care Pharmacy Theatre 10: 55 13: 35 Nick Kaye Michael Lennox & Vikki Furneaux Community Pharmacy Workforce - developing the skills for success Making the case for PCN integration – challenges and opportunities In the Public Health & Wellbeing Theatre 09: 40 Helga Mangion Inside track on the public health agenda In the Technology Theatre 16: 45 Harpreet Chana Small steps to tech
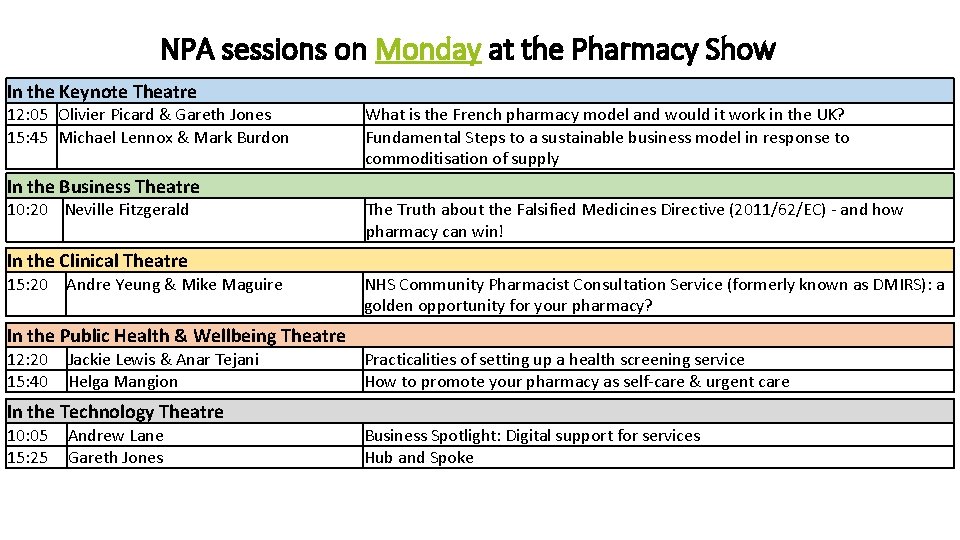
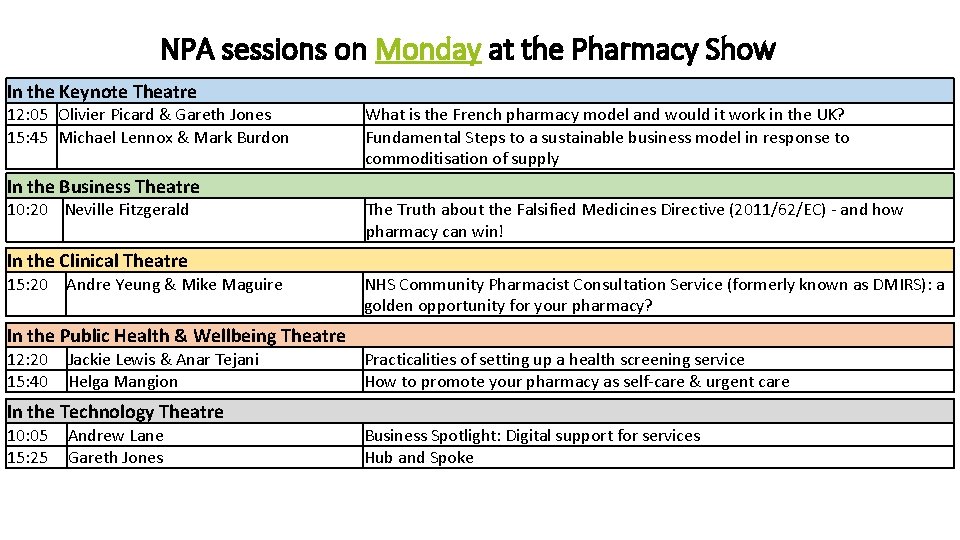
NPA sessions on Monday at the Pharmacy Show In the Keynote Theatre 12: 05 Olivier Picard & Gareth Jones 15: 45 Michael Lennox & Mark Burdon What is the French pharmacy model and would it work in the UK? Fundamental Steps to a sustainable business model in response to commoditisation of supply In the Business Theatre 10: 20 Neville Fitzgerald The Truth about the Falsified Medicines Directive (2011/62/EC) - and how pharmacy can win! In the Clinical Theatre 15: 20 Andre Yeung & Mike Maguire NHS Community Pharmacist Consultation Service (formerly known as DMIRS): a golden opportunity for your pharmacy? In the Public Health & Wellbeing Theatre 12: 20 15: 40 Jackie Lewis & Anar Tejani Helga Mangion Practicalities of setting up a health screening service How to promote your pharmacy as self-care & urgent care In the Technology Theatre 10: 05 15: 25 Andrew Lane Gareth Jones Business Spotlight: Digital support for services Hub and Spoke