Pharmacology Pharmacokinetics Absorption Distribution Biotransformation metabolism Excretion Pharmacodynamics
Pharmacology • Pharmacokinetics – Absorption – Distribution – Biotransformation (metabolism) – Excretion • Pharmacodynamics – Receptor binding – Signal transduction – Physiologic effect 1
59 -291 Section 1, Lecture 3 Drug distribution The transport of a drug in the body by the bloodstream to its site of action • • • fat Protein-binding Water soluble vs. fat soluble Blood-brain barrier Areas of rapid distribution: heart, liver, kidneys, brain Areas of slow distribution: muscle, skin, 2
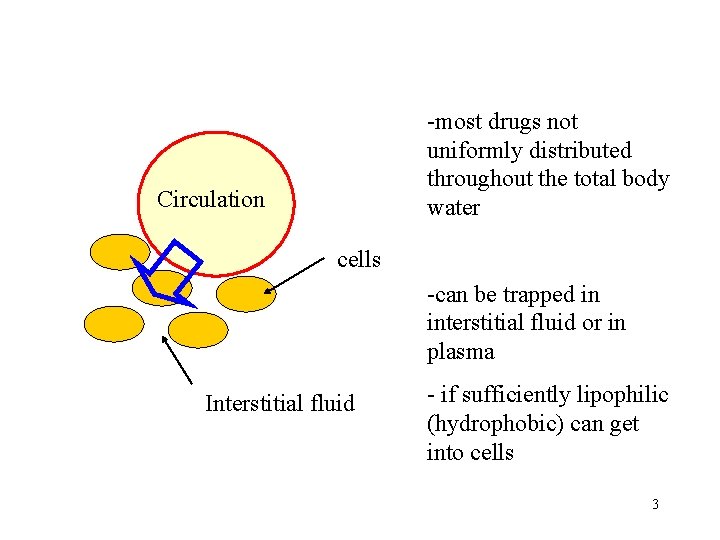
-most drugs not uniformly distributed throughout the total body water Circulation cells -can be trapped in interstitial fluid or in plasma Interstitial fluid - if sufficiently lipophilic (hydrophobic) can get into cells 3
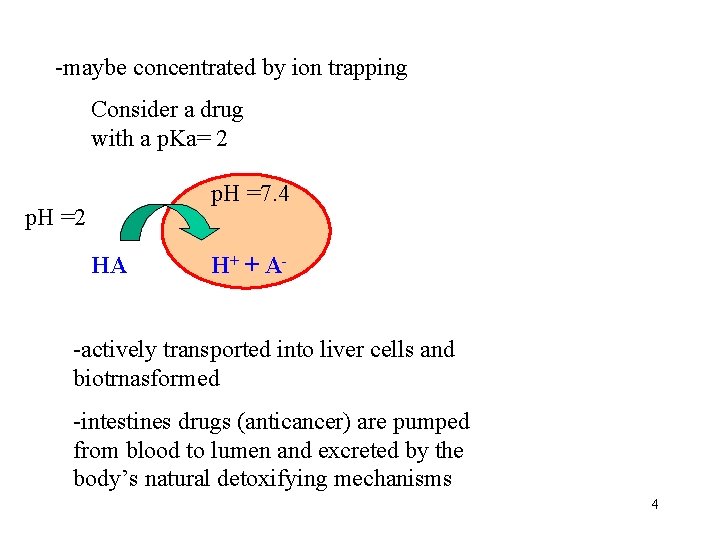
-maybe concentrated by ion trapping Consider a drug with a p. Ka= 2 p. H =7. 4 p. H =2 HA H+ + A- -actively transported into liver cells and biotrnasformed -intestines drugs (anticancer) are pumped from blood to lumen and excreted by the body’s natural detoxifying mechanisms 4
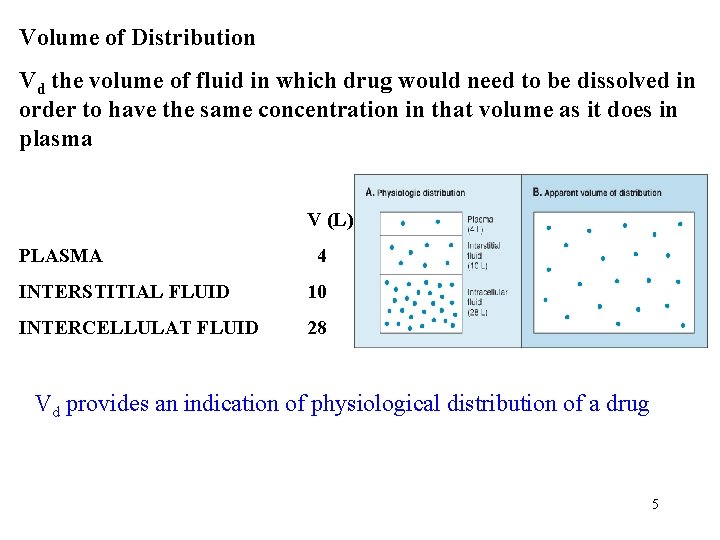
Volume of Distribution Vd the volume of fluid in which drug would need to be dissolved in order to have the same concentration in that volume as it does in plasma V (L) PLASMA 4 INTERSTITIAL FLUID 10 INTERCELLULAT FLUID 28 Vd provides an indication of physiological distribution of a drug 5
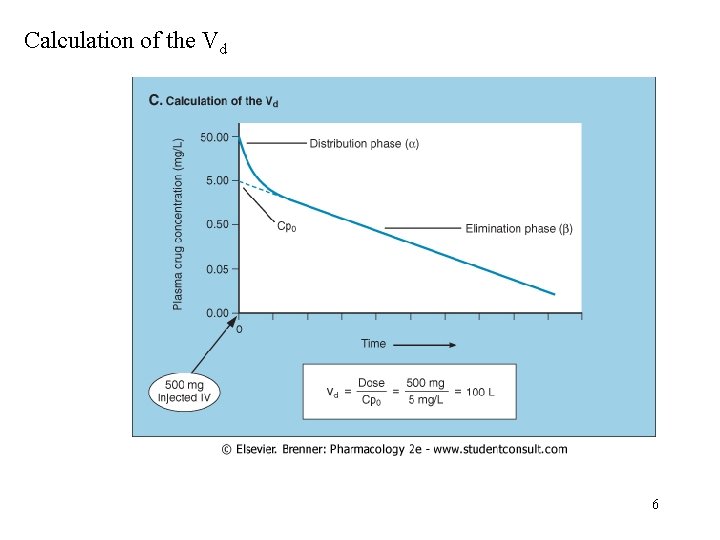
Calculation of the Vd 6
If Vd = plasma volume or extracellular (interstitial) volume drug remains outside of cells (Plasma or interstitial fluid) If Vd = total body water drug is evenly distributed (ie ethanol) 500 mg/ 11. 9 mg/L= 42 L If Vd = >> total body water indicates drugs are concentrated in cells by ion trapping (500 mg /2 mg/L= 250 L) Many weak bases have a large Vd due to intracellular ion trapping in the cells. Intracellular p. H is less than Plasma p. H >> weak bases are more in ionized from inside the cells 7
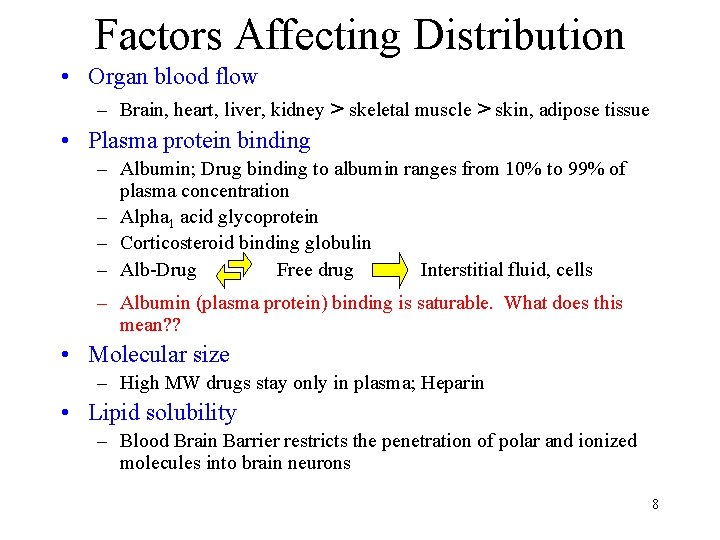
Factors Affecting Distribution • Organ blood flow – Brain, heart, liver, kidney > skeletal muscle > skin, adipose tissue • Plasma protein binding – Albumin; Drug binding to albumin ranges from 10% to 99% of plasma concentration – Alpha 1 acid glycoprotein – Corticosteroid binding globulin – Alb-Drug Free drug Interstitial fluid, cells – Albumin (plasma protein) binding is saturable. What does this mean? ? • Molecular size – High MW drugs stay only in plasma; Heparin • Lipid solubility – Blood Brain Barrier restricts the penetration of polar and ionized molecules into brain neurons 8
EXERCISE: A patient suffering from hyperalbumineuria requires 5 times the normal dose of an analgesic. Why? What kind of a Vd would you expect this patient to have for this analgesic? 9
Drug Biotransformation (Drug metabolism) • Enzyme-catalyzed conversion of drugs to their inactive metabolites, more soluble forms, or a more potent metabolite • Main purpose: To detoxify and inactive drugs and other foreign substances • Liver (main site), Kidneys, lungs, plasma, intestinal mucosa • Metabolites are usually more water soluble and excreted by kidneys • Prodrugs are biotransfomed to active drugs – Prodrug is absorbed better than biotransformed • First-pass biotransformation 10
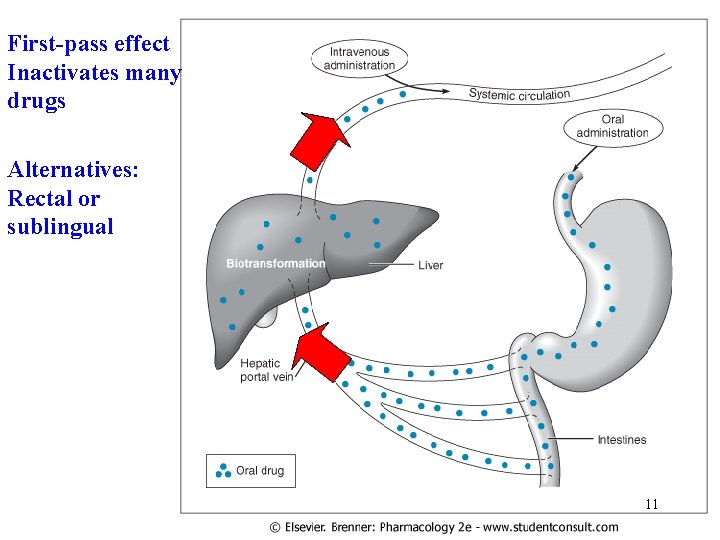
First-pass effect Inactivates many drugs Alternatives: Rectal or sublingual 11
Phases of Drug transformation Phase I- create a chemical functional group on the drug that can be recognized by Phase-II enzymes. Product of phase I enzymes still have biological activity Phase II- no biological activity 12
Phase I Biotransformation • Oxidative reactions – Catalyzed by enzymes of microsomal fraction (ER) of liver • Microsomal cytochrome P 450 monooxygenase • Hydrolytic reactions • Reductive reactions 13
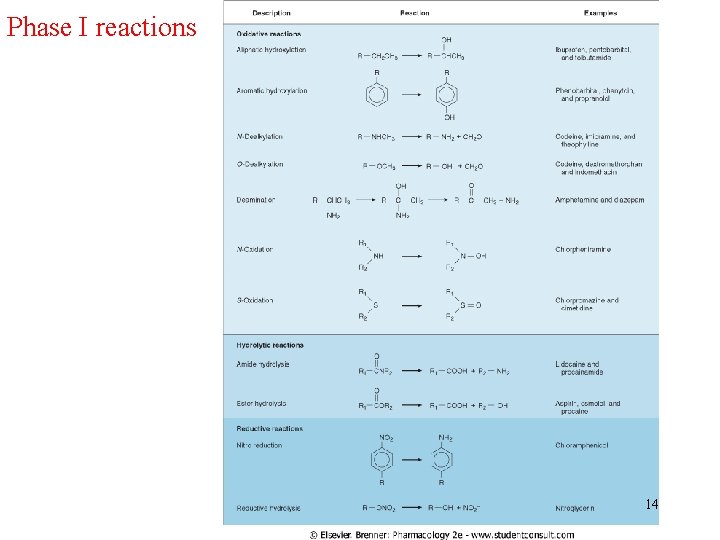
Phase I reactions 14
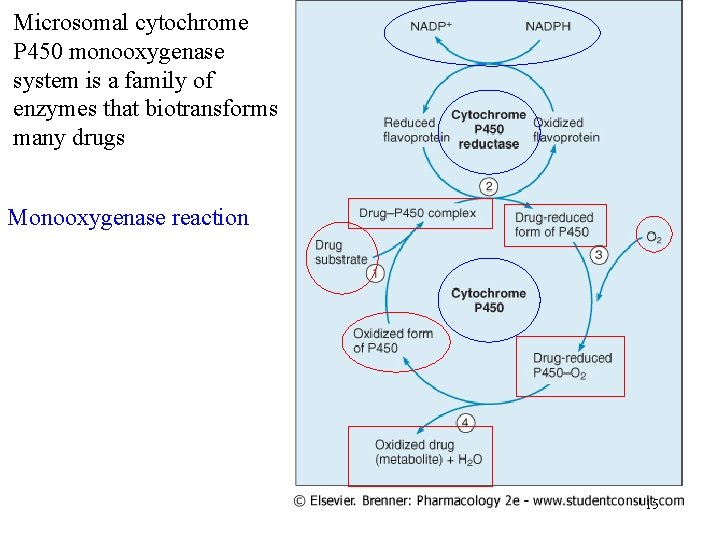
Microsomal cytochrome P 450 monooxygenase system is a family of enzymes that biotransforms many drugs Monooxygenase reaction 15
- Slides: 15