Pharmacology of general anesthetics Dr Ashraf Arafat MD





















- Slides: 87
Pharmacology of general anesthetics Dr. Ashraf Arafat, MD Assistant Professor Department of Anesthesia, King Saud University 1
General anesthesia Loss of consciousness Amnesia Analgesia Muscle relaxation 2
Intravenous Anesthetics 3
Benzodiazepines (BZ) Midazolam, lorazepam, and diazepam. Primary uses: sedation, amnesia, anxiolysis for Primary uses: premedication or as adjuncts to general anesthesia. Mechanism. Enhance inhibitory neurotransmission by Mechanism increasing the affinity of GABAA receptors for GABA. – Pharmacokinetics Effects are terminated by redistribution. All are metabolized in the liver. Diazepam clearance is reduced in the elderly. 4

Pharmacodynamics CNS – Amnestic, anticonvulsant, anxiolytic, musclerelaxant, and sedative-hypnotic (dosedependent manner). – No analgesia. Cardiovascular system – Mild systemic vasodilation and ↓ in cardiac output. HR is usually unchanged. Respiratory system – Mild dose-dependent ↓ in RR and TV. – Respiratory depression may be more if administered with an opioid 5
Adverse effects Pregnancy and labor – Risk of cleft lip and palate in the first trimester. – CNS depression in the neonate. Superficial thrombophlebitis and injection pain by diazepam and lorazepam. 6
Flumazenil – A competitive antagonist at the benzodiazepine binding site of GABAA receptors in the CNS. Reversal of sedative effects occurs within 2 minutes; peak effects at 10 minutes. Half-life is shorter than the benzodiazepine 7
Barbiturates q Such as thiopental and methohexital (highly alkaline). q Mechanism. Ø Facilitate inhibitory neurotransmission by enhancing GABAA receptor function. q Primary Use: Induction of anesthesia Advantages: Rapid onset (30 - 45 sec) Rapid onset ( Short duration (5 – 8 min) initial dose; redistributed from brain to muscle; Pharmacokinetics Hepatic metabolism & elimination. 8
Pharmacodynamics q. CNS – Dose-dependent CNS depression – ↓ in (CMRO 2) cause ↓ in ICP and (CBF). – Potent anticonvulsant properties q. Cardiovascular system – Depress myocardial contractility, leading to dose-dependent ↓ in BP and cardiac output, – Baroreceptor reflexes remain largely intact; 9
–Respiratory system – Dose-dependent decreases in RR and TV. – Apnea may result for 30 to 90 seconds after an induction dose. – Laryngeal reflexes are suppressed to a lesser degree compared with propofol; …. . high incidence of cough and laryngospasm. 10

Adverse effects Allergy. Absolutely contraindicated in Porphyria Venous irritation and tissue damage – Thiopental can cause severe pain and tissue necrosis if injected extravascularly or intra-arterially. If intra-arterial administration occurs, heparin, vasodilators, and regional sympathetic blockade may be helpful in treatment. Myoclonus and hiccups. Less suitable for day case surgery OR maintenance of anaesthesia Multiple doses or prolonged infusions may produce prolonged sedation or unconsciousness 11
Ketamine A sedative-hypnotic agent with potent analgesic properties ‘Dissociative anaesthesia’ with loss of consciousness and profound analgesia. Primary uses: Induction of GA. Sedation and analgesia. Mechanism: NMDA receptor antagonist 12
Pharmacokinetics Unconsciousness in 30 to 60 s after an IV. Terminated by redistribution in 15 to 20 minutes. Metabolized rapidly in the liver ; Elimination half-life is 2 to 3 hours. Repeated bolus doses or prolonged infusions result in accumulation. 13
Pharmacodynamics: CNS – Produces a “dissociative” state accompanied by amnesia and profound analgesia. – ↑ (CBF), ↑ (CMR), and ↑(ICP) pressure. ↑ Cardiovascular system – ↑ HR, and BP whilst COP is maintained. – Direct myocardial stimulation & a central sympathetic effect – Used in hemodynamically compromised patients. Respiratory system – Minimal respiratory depression – Potent bronchodilator. – laryngeal/pharyngeal reflexes are preserved 14
Adverse effects Oral secretions (increased salivation) . Emotional disturbance. agitation & hallucinations ↑ Muscle tone: increased uterine tone ↑ ICP : contraindicated in patients with ↑ ICP : head trauma or intracranial hypertension. Ocular effects. mydriasis, nystagmus, Ocular effects. diplopia, and ↑ intraocular pressure. PONV 15
Propofol (Diprivan) 1%(10 mg/m. L) isotonic oil-in-water emulsion, which contains egg (10 mg/m. L) lecithin, glycerol, and soybean oil. Highly lipid soluble Primary uses: A sedative/hypnotic (ICU) Induction or maintenance of anesthesia Mechanism: Facilitates inhibitory neurotransmission by enhancing the function (GABAA) receptors in CNS. Pharmacokinetics: Hepatic and extrahepatic metabolism to inactive metabolites which are renally excreted. 16
Pharmacodynamics: – CNS Induction : rapid onset of unconsciousness (30 to 45 seconds), followed by a rapid termination of effect by redistribution Emergence is rapid (short distribution half-life (1 – 2 min). Weak analgesic effects. ↓ (CBF) ↓ (ICP), ↓ (CMRO 2). and ↓ (CPP) due to markedly ↓ (MAP). 17

Anticonvulsant. Less (PONV) occurs. – Cardiovascular system Direct myocardial depression with ↓ SVR Dose-dependent ↓ in preload, afterload, and contractility lead to ↓ in (BP) and COP. Hypotension may be marked in hypovolemic, elderly, or hemodynamically compromised patients. Heart rate (HR) is minimally affected, and baroreceptor reflex is blunted. 18

– Respiratory system Dose-dependent decreases in (RR) and (TV). ↓Ventilatory responses to hypoxia and hypercarbia. Apnoea is common. Laryngeal and pharyngeal muscle relaxation 19
Advantages Safe in porphyria; Antiemetic properties Use in day case surgery. Total intravenous anaesthesia (TIVA) Situations where volatile anaesthetics cannot be used (e. g. Ø Malignant hyperthermia (MH) patients, Ø Transfer of sedated patients, Ø Airway surgery when periods of apnoeic oxygenation are employed). 20

Adverse effects Venous irritation. Bacterial growth Lipid disorders. used cautiously in disorders of lipid metabolism (e. g. , hyperlipidemia and pancreatitis). Myoclonus and hiccups Propofol infusion syndrome : a rare fatal disorder that occurs in critically ill patients (usually children) subjected to prolonged, high-dose propofol infusions. (Rhabdomyolysis, metabolic acidosis, cardiac failure, and renal failure). 21
Etomidate Primary use: Induction in patients w/ cardiovascular problems Mechanism: Mechanism Facilitates inhibitory neurotransmission by enhancing GABAA receptor function. –Pharmacokinetics Effects of a single bolus dose are terminated by redistribution. Very high clearance in the liver and by circulating esterases to inactive metabolites. 22
Pharmacodynamics CNS – No analgesic properties. – ↓ (CBF), cerebral metabolic rate, (CMR), and (ICP), . Cardiovascular system – Minimal changes in HR, BP, and COP. Respiratory system – Dose-dependent ↓ in ( RR) & (TV). – Transient apnea may occur. N. B Useful in elderly and shocked patients 23
Adverse effects Myoclonus Excitatory phenomena (e. g. involuntary limb twitches); PONV; Venous irritation and superficial thrombophlebitis may be caused by the propylene glycol vehicle. Minimized by administration into a freeflowing IV carrier infusion. Adrenal suppression: Inhibits 11β-hydroxylase; suppression: - A single induction dose suppresses adrenal steroid synthesis for up to 24 hours. - Repeated doses or infusions is associated with increased 24 mortality in ICU patients.
Opioids q Opioids produce moderate sedation and profound analgesia. q They exert their effects by binding with opioid receptors in CNS ( 3 major opioid receptors μ (mu), κ (kappa), and δ (delta). Meperidine, Morphine, Alfentanil, Fentanyl, Sufentanil, Remifentanil Advantages: Minimal cardiac effects No myocardial depression 25

Fentanyl A potent synthetic opioid agonist with between 100 times the analgesic potency of morphine. Used in Ø Induction Ø Maintenance of GA Ø Supplement regional and spinal anesthesia. Ø Ability to maintain cardiac stability. Sufentanil citrate (Sufenta) ü 10 times as potent as fentanyl ü Rapid elimination , ü Relatively more rapid recovery as compared with fentanyl. 2 6
Alfentanil ü Shorter duration of action compared to fentanyl and sufentanil, Remifentanil (Ultiva) ü Ultra short acting and rapidly cleared ü widespread extrahepatic metabolism by blood and tissue nonspecific esterases, Morphine ü May produce hypotension and bronchoconstriction as a consequence of its histamine-releasing action. ü Morphine may be a poor choice for a patient with renal failure. 27
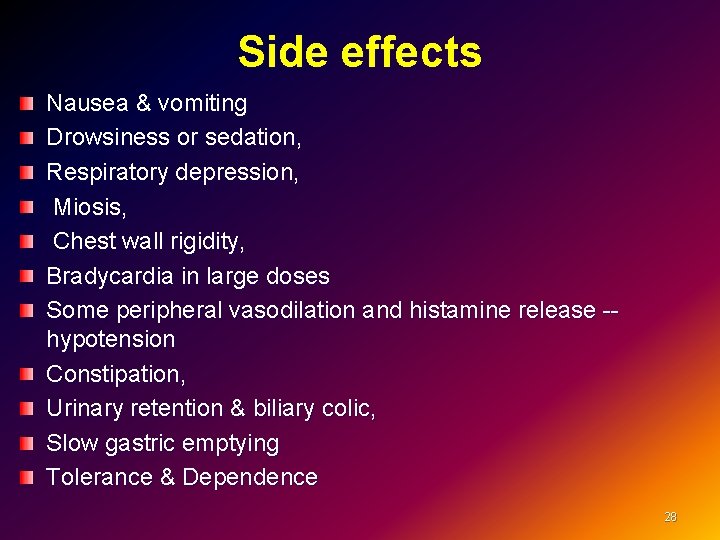
Side effects Nausea & vomiting Drowsiness or sedation, Respiratory depression, Miosis, Chest wall rigidity, Bradycardia in large doses Some peripheral vasodilation and histamine release -- hypotension Constipation, Urinary retention & biliary colic, Slow gastric emptying Tolerance & Dependence 28

Naloxone A specific opiate receptor antagonist, binding the receptor The effective dose is 1 to 4 μg/kg IV, and the duration of action is 30 to 45 minutes. Dose may need to be repeated or an infusion Side effects - Reversal of analgesia, nausea, vomiting, - Increased sympathetic nervous system activity, ( tachycardia, hypertension, pulmonary edema, and cardiac dysrhythmias). 29
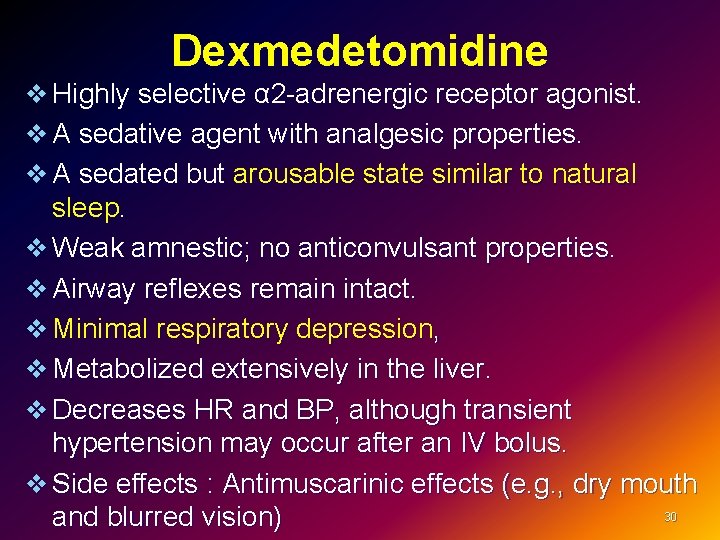
Dexmedetomidine v Highly selective α 2 -adrenergic receptor agonist. v A sedative agent with analgesic properties. v A sedated but arousable state similar to natural sleep. v Weak amnestic; no anticonvulsant properties. v Airway reflexes remain intact. v Minimal respiratory depression, v Metabolized extensively in the liver. v Decreases HR and BP, although transient hypertension may occur after an IV bolus. v Side effects : Antimuscarinic effects (e. g. , dry mouth 30 and blurred vision)

Inhalational Anesthetics 31

History of Anesthesia Ø Joseph Priestly – discovers N 2 O in 1773 Ø William Morton, dentist – first demonstration of successful surgical anesthesia with ether 1846 Ø Dr. John Snow administers chloroform to Queen Victoria (1853)– popularizes anesthesia for childbirth in UK He becomes the first anesthesia specialist. 32

Characteristics of the ideal inhaled anesthetic agent Non-toxic. Non-allergenic. Not a malignant hyperthermia (MH) trigger. Stable in storage, non-flammable. No extra specialist equipment needed. Low solubility in blood and tissues, Analgesic Lack of injury to vital tissues. The lack of seizures, respiratory irritation, and circulatory stimulation; Resistance to physical and metabolic degradation No reaction with soda lime/breathing circuit 33
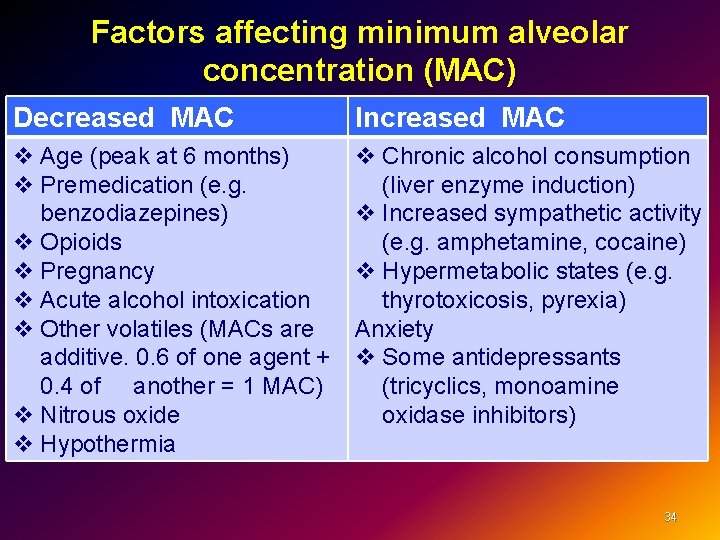
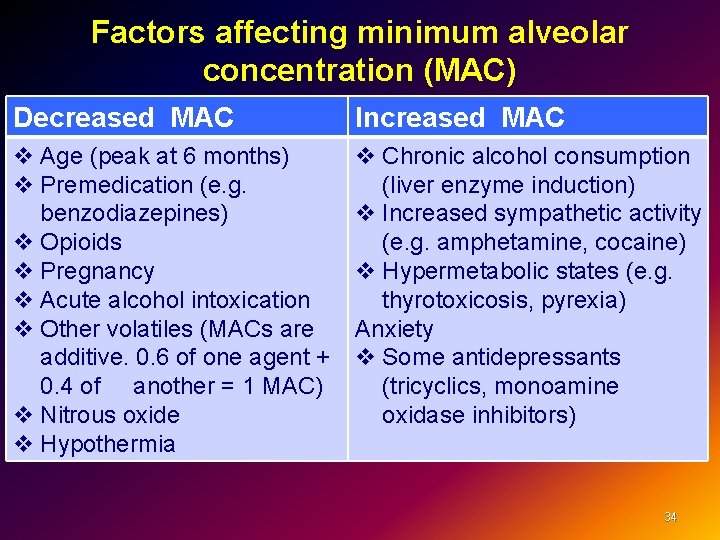
Factors affecting minimum alveolar concentration (MAC) Decreased MAC Increased MAC v Age (peak at 6 months) v Premedication (e. g. benzodiazepines) v Opioids v Pregnancy v Acute alcohol intoxication v Other volatiles (MACs are additive. 0. 6 of one agent + 0. 4 of another = 1 MAC) v Nitrous oxide v Hypothermia v Chronic alcohol consumption (liver enzyme induction) v Increased sympathetic activity (e. g. amphetamine, cocaine) v Hypermetabolic states (e. g. thyrotoxicosis, pyrexia) Anxiety v Some antidepressants (tricyclics, monoamine oxidase inhibitors) 34
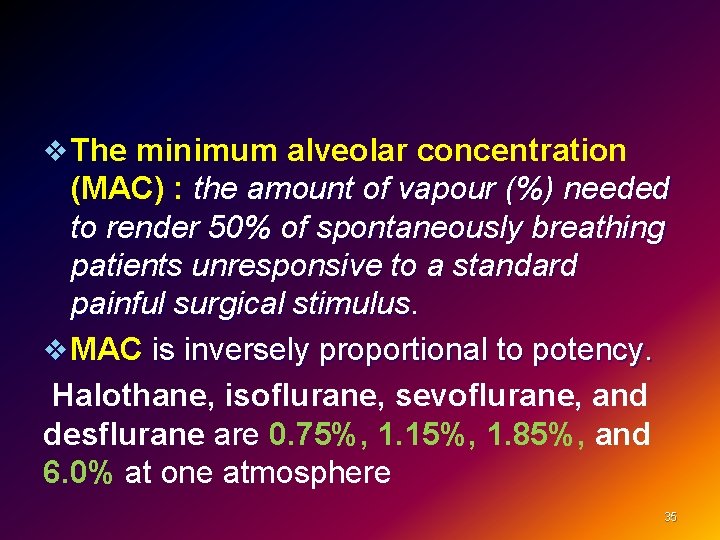
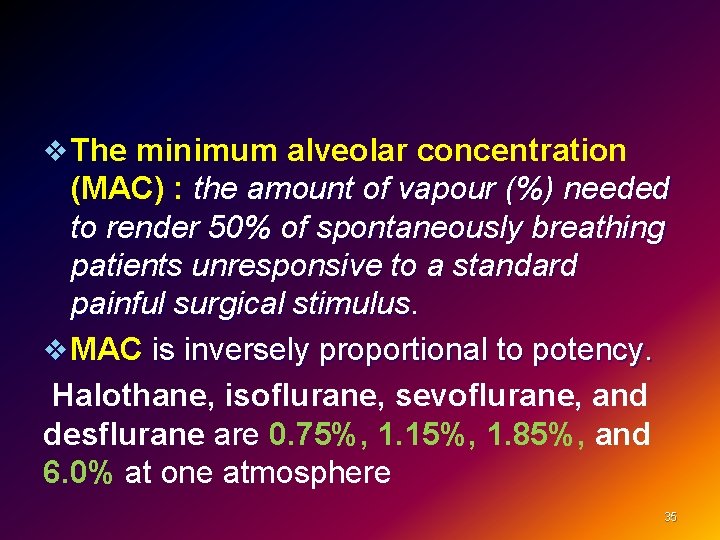
v The minimum alveolar concentration (MAC) : the amount of vapour (%) needed to render 50% of spontaneously breathing patients unresponsive to a standard painful surgical stimulus. v MAC is inversely proportional to potency. Halothane, isoflurane, sevoflurane, and desflurane are 0. 75%, 1. 15%, 1. 85%, and 6. 0% at one atmosphere 35
Volatile anesthetics – Present as liquids at room temperature and pressure – Vaporized into gases for administration 36
General pharmacokinetics The higher the vapor pressure, the more volatile the anesthetic. Blood solubility determines the speed of build-up / elimination from blood / brain Lower blood solubility means (faster induction/recovery) Inspired air → Alveolar air → Blood → Brain 37
Volatile anesthetics Mechanism: Various ion channels in the CNS involved in synaptic transmission (including GABAA, glycine, and glutamate receptors) may play a role. Metabolism: hepatic. Exhalation: This is the predominant route of elimination: CNS – Unconsciousness and amnesia. –↑ cerebral blood flow (CBF). – ↑ intracranial pressure BMR: reduced; a MAC of 2 reduces oxygen consumption by 30%. 38
Cardiovascular system – Myocardial depression and systemic vasodilation, reduce SVR – Hypotensive effect, – Change in HR, (desflurane) – Sensitize the myocardium to the arrhythmogenic effects of catecholamines. Neuromuscular system - Dose-dependent ↓ in skeletal muscle tone. -Potentiation of muscle relaxants. All volatile anaesthetics may precipitate malignant hyperthermia (MH). A dramatic increase in body temperature, acidosis, electrolyte imbalance and shock 39
Hepatic system: ↓ hepatic perfusion. Rarely, Hepatic system: (“halothane hepatitis”). Renal system. ↓ renal blood flow. system Respiratory system – Dose-dependent respiratory depression – ↓ TV↑RR – Airway irritation and, during light levels of anesthesia, may precipitate coughing, laryngospasm, or bronchospasm (sevoflurane makes it more suitable ) – Bronchodilator, (with the exception of desflurane). - Respiratory response to hypoxia and hypercarbia is reduced. 40

Isoflurane: Advantages: It causes peripheral vasodilation A drop in blood pressure, systemic vascular resistance (SVR) Tachycardia (sympathetic stimulation) Increased coronary blood flow. Disadvantages: Moderate solubility, so recovery from anesthesia may be delayed Isoflurane can make the heart “more sensitive” to circulating catecholamines (like epinephrine). 41
sevoflurane Advantages: Low solubility in blood-- produces rapid induction and emergence Non-irritant with Pleasant smelling (suitable for children) Has good bronchodilating properties Agent of choice in asthma, bronchitis, and COPD. It causes bradycardia, blood pressure and SVR Mild respiratory and cardiac suppression (cardiac output is maintained) Disadvantages: Carbon dioxide absorbents in anesthesia machines degrade sevoflurane to Compound A 42
Desflurane Advantages: Rapid onset and recovery of anesthesia due to a low blood/gas solubility coefficient (0. 42). (outpatient procedures) One of least metabolized to toxic byproducts Disadvantages: Requires a special vaporizer Pungent and irritating to the airway (leading to more coughing, laryngospasm) cannot be used for induction It increases salivary and respiratory secretions High inspired gas concentrations lead to a significant ↑ in the patient’s BP & HR. 43
Halothane Used for induction in children (sweet pleasant odor); Side effects: Sensitize the myocardium to the arrhythmogenic effects of catecholamines, of Myocardial depression, “Halothane hepatitis” (rare) related to repeated exposure, Blood pressure usually falls, . Very soluble in blood and adipose Prolonged emergence 44
Nitrous Oxide MAC is 104% at one atmosphere CNS Mechanism: antagonism of NMDA receptors in CNS. - Weak anesthetic, produce analgesia - Usually combined with other anesthetics. - Used alone e. g. dental procedures); q Cardiovascular system - Mild myocardial depressant & a mild sympathetic stimulant. - HR and BP are usually unchanged. - ↑ pulmonary vascular resistance. Respiratory system. 45 Respiratory system. Little effect on respiration 45

Nausea/vomiting; Risk of bone marrow depression Inhibits vitamin B-12 metabolism Second Gas Effect: Increased uptake of volatile agent when given together with N 2 O q Expansion of closed gas spaces. nitrous oxide is 35 times more soluble in blood than nitrogen, Contraindicated in (e. g. air embolus, pneumothorax, Middle Ear Surgery etc) Diffuse into the cuff of ETT. Diffusion hypoxia. After discontinuation, its rapid elimination from the blood into the lung may lead to a low partial pressure of oxygen in the alveoli. 46

Xenon A gas and exhibits many properties of an ideal anaesthetic agent : Colourless, Odourless, Non-flammable, Stable in storage, Low oil/gas and blood/gas coefficients, Cardiovascularly stable, Excreted unmetabolized, Non-toxic, MH safe Disadvantage : very expensive. 47
Neuromuscular blocking drugs 48

D. Neuromuscular blocking drugs Used to Perform tracheal intubation, Facilitate ventilation, Provide optimal surgical operating conditions. 49

Neuromuscular blockers 50
Depolarizing(Succinycholine) Structurally similar to acetylcholine … activate the acetylcholine receptors (Ach) depolarization of postjunctional membrane. Fastest onset (60 s) Very short duration of action A short time intubation (Rapid sequence induction) Metabolized very quickly by plasma cholinesterase. Characterized by Transient muscle fasciculations followed by relaxation. Acetylcholine esterase (ACh. E) inhibitors potentiate rather than reverse the block.
Side effects of Succinycholine: Myalgia : abdomen, back, and neck Cardiac dysrhythmias. sinus bradycardia, junctional rhythm, and even asystole after the first dose in children and following repeated dose within a short time interval in adults Hyperkalemia -Major burns, renal failure -Massive tissue injuries, muscular dystrophies Extensive denervation of skeletal muscle, upper motor neuron diseases. A transient increase in intraocular pressure 52
Increased intragastric pressure Increase in intracranial pressure. Succinycholine apnea ( apnea Prolonged blockade) : -Low levels of plasma cholinesterase as in severe liver or kidney disease, - A drug-induced inhibition of its activity, - A genetically atypical enzyme. Anaphylaxis. over 50% of anaphylactic reactions . to NMBDs. Malignant hyperthermia (MH). 53
Nondepolarizing blockers They act by competitively blocking the binding of ACh to its receptors and inhibit muscular contraction. – It is characterized by : Absence of fasciculations. a slower onset than suxamethonium Highly ionized, poorly lipid soluble and protein bound at physiological p. H Potentiation by other nondepolarizing NMBDs and volatile anesthetic agents. Reversal by ACh. E inhibitors. 54
2 types Benzylisoquinoliniums, e. g. atracurium, cisatracurium, mivacurium Aminosteroids, e. g. pancuronium, vecuronium, rocuronium 55
Mivacurium Short-acting. Rapidly hydrolyzed by plasma cholinesterase. Used with caution in patients with known atypical plasma cholinesterase activity or using cholinesterase inhibitors. Histamine release causing a transient hypotension and tachycardia. 56
Atracurium besylate (Tracrium) Widely used and have an intermediate onset and duration of action. Histamine release , No direct cardiovascular effects. Metabolism is spontaneously by Hofmann by degradation and ester hydrolysis in the plasma, Its duration of action is independent of renal and hepatic function. A breakdown product of atracurium, (laudanosine ) A breakdown product of atracurium, may accumulate and cause seizures 57
Cisatracurium(Nimbex) Isomer of atracurium Relatively slow onset of action. Less laudanosine. Not release histamine. Hofmann degradation and does not accumulate in renal failure. 58

Pancuronium bromide (Pavulon) The first steroid NMBD in clinical use has a slow onset and long duration of action. onset and It does not cause histamine release Weak sympathomimetic properties and causes tachycardia. It is partly metabolised in the liver. Its action is prolonged in renal and hepatic impairment. 59
Vecuronium bromide(Norcuron) Vecuronium is structurally similar to pancuronium but has a slightly faster onset and shorter (intermediate) duration of action. Not release histamine No cardiovascular effects. Metabolism in the liver into active metabolites in the before being excreted in the bile and urine. Prolonged clinical effect in elderly patients and those with liver or renal disease. 60
Rocuronium. An analog of vecuronium The most rapid onset of the clinically available nondepolarizing NMBDs. Intubating conditions can be achieved in 60 -90 seconds after Intubating conditions can be achieved in an induction dose of 0. 6 mg/Kg. Increasing the dose to 1. 2 mg/kg shortens the time. Used when a rapid sequence induction. An intermediate duration of action. Not release histamine No cardiovascular effects. Higher incidence of anaphylactic reactions Metabolised in the liver and excreted in the bile and renal. In renal failure ------in a longer duration of action 61
Clinical Choice of NMBD Urgency for tracheal intubation, Duration of the procedure, Coexisting medical conditions that may affect the NMJ, Side effects Metabolism Cost-effectiveness Ø SCh makes it a good choice for rapid intubation. Ø Rocuronium will decrease the risk of hyperkalemia in patients with burns. Ø Pancuronium can produce a tachycardia that is undesirable in patients with severe IHD, but its vagolytic effects may be appropriate in pediatrics. 62
Anticholinesterases (Neostigmine) (acetylcholinesterase inhibitors) are agents that inhibit the action of the acetylcholinesterase enzyme at the neuromuscular junction. (Increases concentration of Ach at NMJ) q Clinical tests of adequate resolution of neuromuscular block include the ability to lift the head from the bed for 5 seconds, q No role for anticholinesterases in reversing the effects of suxamethonium. 63
Neostigmine Side effects Bradycardia, miosis, GI upset, Nausea, bronchospasm, increased bronchial secretions, sweating and salivation. For this reason an antimuscarinic such as glycopyrronium 0. 01 mg/kg or atropine 0. 02 glycopyrronium mg/kg must be administered along with the anticholinesterase. Intravenous injection at a dose of 0. 05 mg/kg Intravenous injection at a dose (maximum 5 mg). 64

Sugammadex (a cyclodextrin) Binds irreversibly to rocuronium and vecuronium, rendering them inactive. It has a role in failed intubation/ ventilation scenarios by reversing muscle relaxation when rapid resumption of airway reflexes and respiratory function is required. 65

Peripheral nerve stimulator Check the depth of neuromuscular blockade Determine that neuromuscular blockade is reversed at least 3 twitches on a train of four should be detected before attempting reversal. 66
Local anesthetics (LAs) 67
Local anesthetics Weak bases Mechanism : reversibly blocking sodium channels to prevent depolarization Lipid solubility: potency, plasma protein binding determines, duration of action of local anesthetics. Addition of vasoconstrictor: ü Prolongation of anesthetic action ü Decreased risk of toxicity ü Decrease in bleeding from surgical manipulation. 68
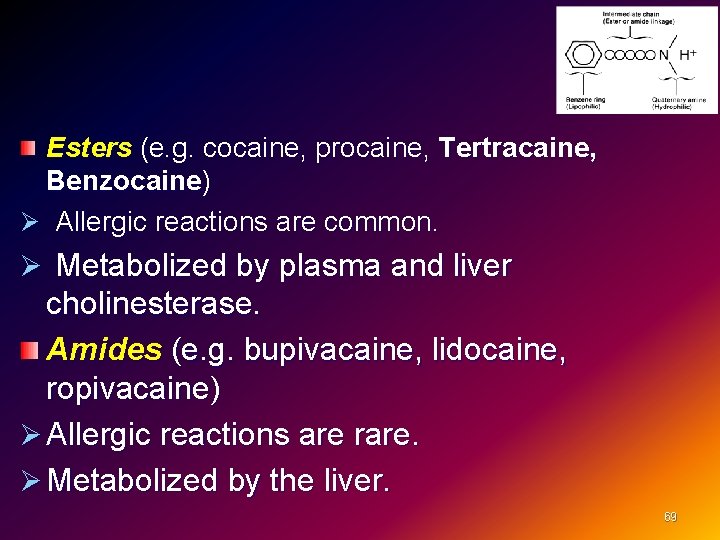
Esters (e. g. cocaine, procaine, Tertracaine, Benzocaine) Ø Allergic reactions are common. Ø Metabolized by plasma and liver cholinesterase. Amides (e. g. bupivacaine, lidocaine, ropivacaine) Ø Allergic reactions are rare. Ø Metabolized by the liver. 69
Applications of local anesthesia: Minor nerve blockade, e. g. radial nerve; Major nerve trunk blockade, e. g. brachial plexus block; Intravenous regional anaesthesia. Topical application: to skin for analgesia (e. g. , benzocaine) or mucous membranes (for diagnostic procedures) Spinal & epidural anesthesia: Local infiltration, e. g. laceration suturing, postoperatively to surgical wounds; i. v. infusion: for control of cardiac arrhythmias (e. g. , lidocaine for ventricular arrhythmias) With propofol injection, e. g. by adding 10 mg lidocaine. 70

Speed of onset of action: Ø p. Ka (p. H at which 50% of the drug is in the ionized form); eg. lidocaine (p. Ka 7. 9) has a quicker speed of onset than bupivacaine (p. Ka 8. 1) Ø Additives effect : bicarbonate The rate of systemic absorption depends on the site of administration: Ø mucous membranes >intercostals >major nerve block >infiltration 71
Duration of action Ø Protein-bound LAs have a longer duration of action Ø Ester LAs may have a prolonged duration of action (pregnancy, liver disease or when the enzyme is atypical or absent (e. g. pseudocholinesterase deficiency) Ø Addition of vasoconstrictors Hyperbaric solutions of LA (e. g. by the addition of dextrose) effect the spread of LA when injected into the CSF 72
Lidocaine Amide type anesthetic Lidocaine was introduced in 1948 The most commonly used local anesthetic Rapid onset and a duration of 60 -75 minutes Extended with epinephrine for up to 2 hours Metabolized in the liver and excreted by the kidneys. Contraindicated in patients with a known sensitivity to amide type anesthetics Has also antiarrhythmic action. 73
Bupivacaine Amide-type local anesthetic Introduced in 1963 Onset of action is slower than lidocaine and anesthesia is long acting Provides 2 -4 hours of anesthesia Extended with epinephrine for up to 7 hours More cardio-toxic than lidocaine, difficult to treat. More cardio-toxic Metabolized in the liver and excreted by the kidneys Contraindication: known hypersensitivity 74
Levobupivacaine v less serious CNS and CVS toxicity Ropivacaine v A less toxic, long-lasting LA v Undergoes extensive hepatic metabolism, 75
EMLA Ø Prilocaine and lidocaine. Ø Surface anaesthesia when applied to skin and left for (>45 min). Ø Paediatrics and dressing changes. Amethocaine gel Ø A quicker onset than EMLA. Other forms of LA are poorly absorbed through intact skin. 76
Intravenous regional anaesthesia (IVRA) A BP cuff is applied to the upper arm with a cannula in the hand. After exsanguination of the limb, the BP cuff is inflated to 100 mm. Hg above systolic BP. Prilocaine is the preferred drug and is injected i. v. Good analgesia for distal limb procedures (e. g. fracture manipulation or carpel tunnel decompression). The cuff is let down after at least 20 min to allow the LA to spread into the adjacent tissues in order to prevent toxic plasma levels of LA following systemic absorption. A second cannula must always be sited in the other arm for emergency use. 77
Local Anesthetic Toxicity Central nervous system – initially-- lightheadedness, circumoral numbness, dizziness, tinnitus, visual change – later-- drowsiness, disorientation, slurred speech, loss of consciousness, convulsions – finally-- respiratory depression Cardiovascular – Myocardial depression and vasodilation-- hypotension and circulatory collapse – Cardiac arrest Allergic reactions-- rare (less than 1%) – preservatives or metabolites of esters – rash, bronchospasm 78
Treatment Supportive, airway /tracheal intubation , IV fluids Vasopressors (e. g. epinephrine), Control of seizures with, for example, benzodiazepines, thiopental. CPR. IV lipid emulsion Intralipid 20% 1. 5 m. L/kg for LA toxicity/cardiovascular collapse. 79
Other side effects Allergy : o Common with the esters, especially with procaine (para-aminobenzoic acid). o Related to additives such as vasoconstrictors or preservatives. Prilocaine metabolism : o Excess prilocine cause methaemoglobinaemia. o Treated with methylene blue. 80

81
Case 9 -Muscle Relaxants (Neuromuscular Junction Blockers) A 4 - years old male patient booked for squint surgery right eye Ø How you will assess this patient preoperatively Ø Discuss fasting time and premedication 82
q The patient seen in preoperative anesthesia clinic and cleared for squint surgery under general anesthesia , Bwt: 16 kg Ø What are the physiological difference between adult and pediatric patient Ø Discuss anesthesia consideration and special concern for such this surgery Ø Discuss anesthesia plan , induction, medications methods for securing the airway , maintenance of anesthesia and intravenous fluid requirement 83

During surgery the patient developed sever bradycardia Ø Discuss the cause and treatment The surgery lasted 2 hours and the patient extubated and shifted to recovery room Ø what is your post-operative analgesia plan 84
Case scenario A 47 -year-old patient is undergoing the clipping of an intracranial aneurysm of the anterior communicating artery under general anesthesia. The surgery is being even the smallest movement by the patient could have devastating consequences performed under a microscope, so 85
Ø How can the patient be protected and the surgery allowed to proceed? Ø What are the Clinical Pharmacology of the Neuromuscular Blockers? 86
Ø Maintenance of Blockade: How Much is Enough? Ø Reversal of the Neuromuscular Blockade and Emergence 87
 Arafat in uniforma
Arafat in uniforma Yasir arafat
Yasir arafat Yasir arafat
Yasir arafat Dua after fajr
Dua after fajr Jasser arafat
Jasser arafat Yasir arafat
Yasir arafat Barbiturates moa
Barbiturates moa Classification of local anesthetics
Classification of local anesthetics What is regional anesthesia
What is regional anesthesia Second gas effect
Second gas effect Minimum alveolar concentration
Minimum alveolar concentration Baricity of local anesthetics
Baricity of local anesthetics Mac isoflurane
Mac isoflurane Classification of local anesthetics
Classification of local anesthetics Spinal block location
Spinal block location Mohsen ashraf
Mohsen ashraf Ashraf marwan
Ashraf marwan Ashraf husain
Ashraf husain Peggy boylan-ashraf sjsu
Peggy boylan-ashraf sjsu Ashraf husain
Ashraf husain Dr tariq ashraf
Dr tariq ashraf Conistipation
Conistipation Dopamine synthesis
Dopamine synthesis Ansc 497
Ansc 497 What is ion trapping in pharmacology
What is ion trapping in pharmacology Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals First pass effect in pharmacology
First pass effect in pharmacology Potency vs efficacy
Potency vs efficacy First pass effect drugs
First pass effect drugs Define pharmacology
Define pharmacology Clinical pharmacology residency
Clinical pharmacology residency Pharmacology tutor anderson
Pharmacology tutor anderson Respiratory pharmacology quiz
Respiratory pharmacology quiz Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Clinical pharmacology seminar
Clinical pharmacology seminar What is pharmacology
What is pharmacology Maintenance dose definition
Maintenance dose definition What is ion trapping in pharmacology
What is ion trapping in pharmacology Bioavailability calculation example
Bioavailability calculation example Branches of pharmacology
Branches of pharmacology Toxicology and applied pharmacology
Toxicology and applied pharmacology Basic principles of pharmacology
Basic principles of pharmacology Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Mechanism of drug action
Mechanism of drug action Bioavailability definition
Bioavailability definition What is pharmacology
What is pharmacology Concept of essential drugs
Concept of essential drugs Venipuncture for radiologic technologists
Venipuncture for radiologic technologists Clinical pharmacology
Clinical pharmacology Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Pharmacology module
Pharmacology module Adrenal drugs pharmacology
Adrenal drugs pharmacology Slidetodoc.com
Slidetodoc.com Loading dose formula in pharmacology
Loading dose formula in pharmacology Estado estable
Estado estable Metabolism definition in pharmacology
Metabolism definition in pharmacology Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Pharmacology for veterinary technicians
Pharmacology for veterinary technicians Rationale meaning in pharmacology
Rationale meaning in pharmacology Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Computational pharmacology
Computational pharmacology First pass effect in pharmacology
First pass effect in pharmacology Fish pharmacology
Fish pharmacology Reverse pharmacology
Reverse pharmacology Potentiation example
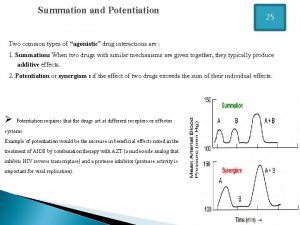
Potentiation example Basic & clinical pharmacology
Basic & clinical pharmacology Pharmacology pay
Pharmacology pay First pass metabolism definition pharmacology
First pass metabolism definition pharmacology Clinical pharmacology seminar
Clinical pharmacology seminar Therapeutic index
Therapeutic index Difference between tolerance and tachyphylaxis
Difference between tolerance and tachyphylaxis Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology First pass effect in pharmacology
First pass effect in pharmacology Parkinson's disease definition
Parkinson's disease definition Chronic gout
Chronic gout Pharmacology chapter 1
Pharmacology chapter 1 Pharmacology newcastle
Pharmacology newcastle Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Guaifenasin
Guaifenasin Alpha 1 vs alpha 2 receptors
Alpha 1 vs alpha 2 receptors Define pharmacology
Define pharmacology First order kinetics
First order kinetics Glomerular
Glomerular Planos en cinematografia
Planos en cinematografia Where did general lee surrender to general grant?
Where did general lee surrender to general grant? Inductive general to specific
Inductive general to specific General objectives of evs lesson plan
General objectives of evs lesson plan Most general to most specific classification
Most general to most specific classification