Pharmacology of general anesthetics 1 Intravenous Anesthetics 2


- Slides: 36
Pharmacology of general anesthetics 1

Intravenous Anesthetics 2
Benzodiazepines (BZ) The 3 main drugs used in this category are diazepam, lorazepam and midazolam. Primary uses: Anti-anxiety agent pre-op for premedication. Sedation They are inadequate for use in surgical anesthesia “on their own”, and must therefore be used with another anesthetic agent (i. e. an inhalation anesthetic). 3
Advantages: Relatively rapid onset Cause amnesia Relatively little cardiovascular effect Anti-convulsant Disadvantages: Not analgesic Cause respiratory depression Long-acting (diazepam or repeated inj. of midazolam) 4
a. diazepam (Valium) It is water-insoluble, so IV use requires a non-aqueous vehicle which can cause local irritation/pain b. midazolam (Dormicum) - water soluble, so drug of choice for IV administration - It has a more rapid onset and more rapid elimination than the other BZ’s. - The most potent amnestic c. lorazepam (Ativan) water-insoluble, less potent amnestic than midazolam, but a more potent amnestic than diazepam. 5
Barbiturates q The 3 main drugs used in this category are thiopental, thiamylal, and methohexital. q Primary Use: Induction of anesthesia Advantages: Rapid onset (10 - 30 sec) Short duration (5 – 8 min) initial dose; redistributed from brain to muscle; prolonged on repeated injection 6
Disadvantages: Not analgesic Decrease blood pressure Decrease respiratory rate and tidal volume or apnea. Coughing, laryngospasm, bronchospasm. 7
Opioids produce moderate sedation and profound analgesia. They exert their effects by binding with opioid receptors in CNS ( 3 major opioid receptors μ (mu), κ (kappa), and δ (delta). The opioids most commonly used are fentanyl sufentanil citrate (Sufenta) alfentanil (Alfenta) remifentanil (Ultiva) 8
Primary uses: Analgesia Advantages: Profound analgesia Relative cardiovascular stability High potency, short duration (15 -30 min. ; Remifentanil; 5 min) except morphine Reduces emergence phenomena Reversible by opioid receptor antagonists Disadvantages: Nausea Slow gastric emptying Respiratory depression at high doses (assisted 9
Fentanyl A potent synthetic opioid agonist with between 50100 times the analgesic potency of morphine. Used to aid induction and maintenance of general anesthesia and to supplement regional and spinal anesthesia. Ability to maintain cardiac stability. Sufentanil citrate (Sufenta) q Rapid induction of analgesia (similar to Fentanyl) q Compared to fentanyl and sufentanil, alfentanil has a shorter duration of action because its high protein binding and relatively low lipid solubility. 10
Remifentanil (Ultiva) Ultra short acting and rapidly cleared because it’s ester linkages are susceptible to hydrolysis by esterases in tissues and RBC’s. Morphine May produce hypotension and bronchoconstriction as a consequence of its histamine-releasing action. 11
Ketamine A complete i. v. anesthetic -causes “dissociative anesthesia” Primary uses: Induction or anesthesia in at risk patients w/ cardiovascular problems Sedation or general anesthesia in children Advantages: Cardiovascular stimulant Bronchodilator Profound analgesia and amnesia 12
Disadvantages: Emergence reactions (not in children <15; adults >65) Increases intracranial pressure Suppresses respiration (less severe than other anesthetics) 13
Propofol (Diprivan) Primary uses: A sedative/hypnotic Induction or maintenance of general anesthesia. Sedating intubated, mechanically ventilated patients. Advantages: Rapid induction and recovery times even after repeated injections Anti-emetic properties 14
Disadvantages: Pain on injection Involuntary muscular movement Respiratory depression , apnea bradycardia and hypotension. 15
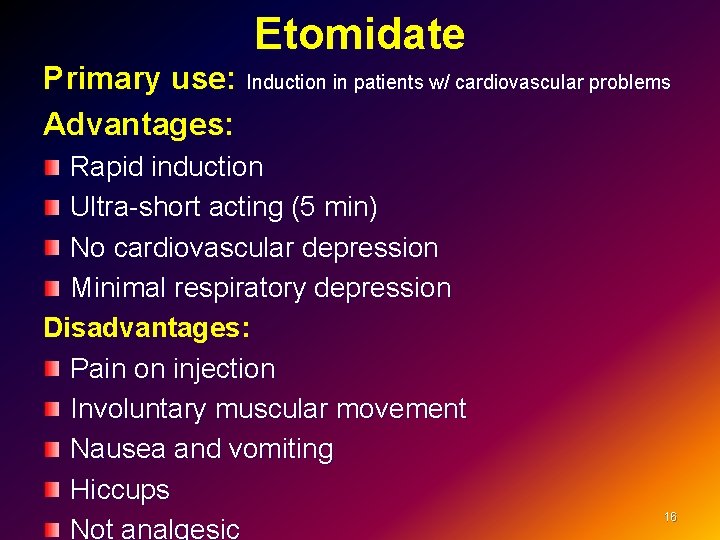
Etomidate Primary use: Induction in patients w/ cardiovascular problems Advantages: Rapid induction Ultra-short acting (5 min) No cardiovascular depression Minimal respiratory depression Disadvantages: Pain on injection Involuntary muscular movement Nausea and vomiting Hiccups Not analgesic 16
Inhalational Anesthetics 17
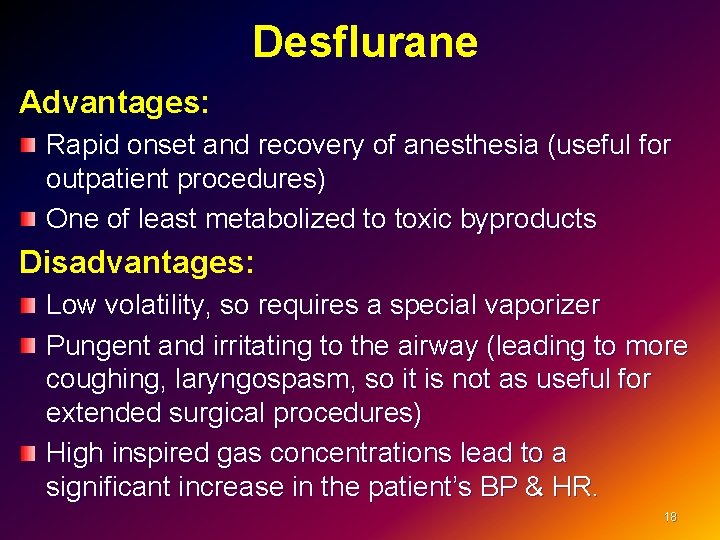
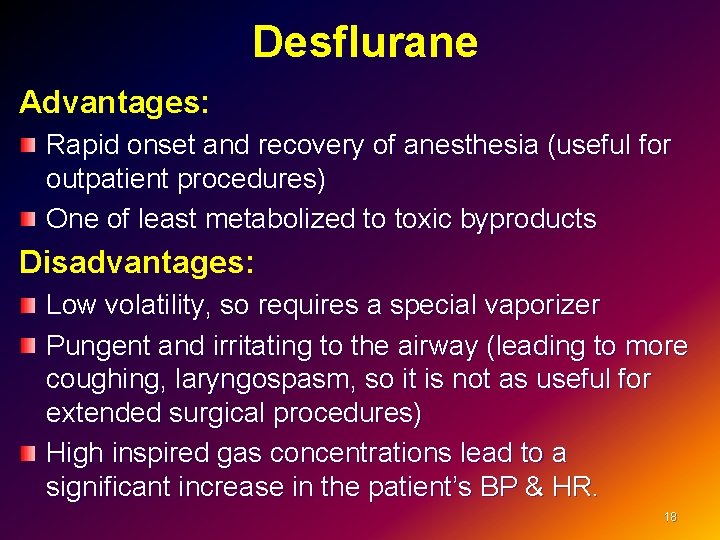
Desflurane Advantages: Rapid onset and recovery of anesthesia (useful for outpatient procedures) One of least metabolized to toxic byproducts Disadvantages: Low volatility, so requires a special vaporizer Pungent and irritating to the airway (leading to more coughing, laryngospasm, so it is not as useful for extended surgical procedures) High inspired gas concentrations lead to a significant increase in the patient’s BP & HR. 18
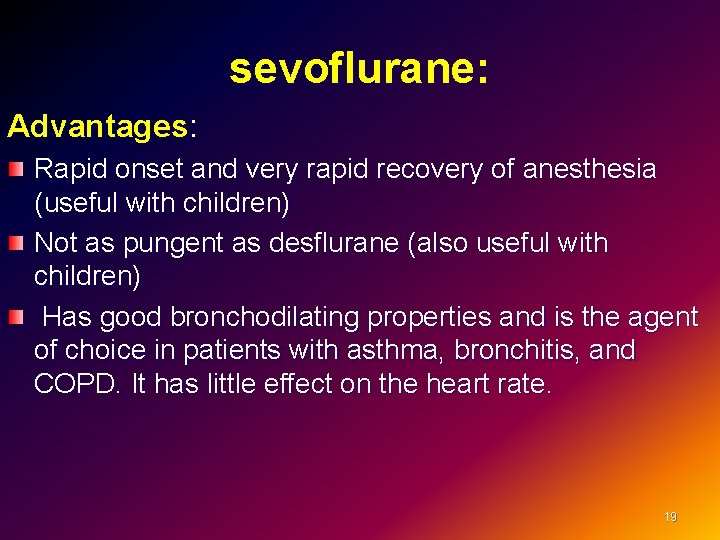
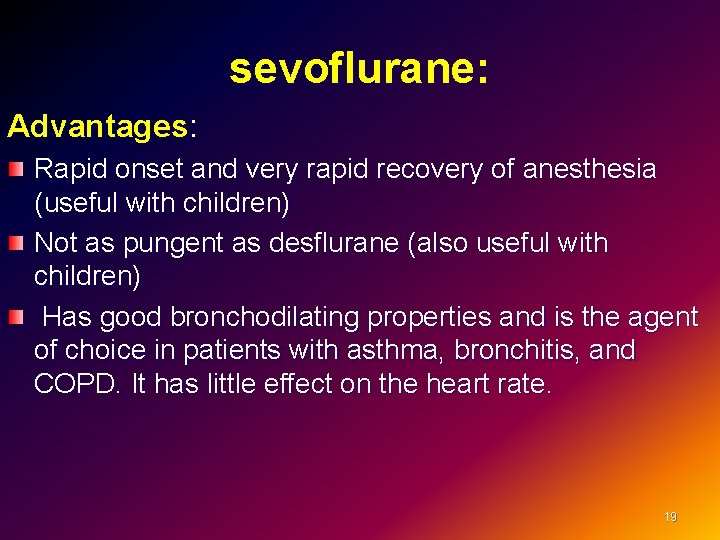
sevoflurane: Advantages: Rapid onset and very rapid recovery of anesthesia (useful with children) Not as pungent as desflurane (also useful with children) Has good bronchodilating properties and is the agent of choice in patients with asthma, bronchitis, and COPD. It has little effect on the heart rate. 19
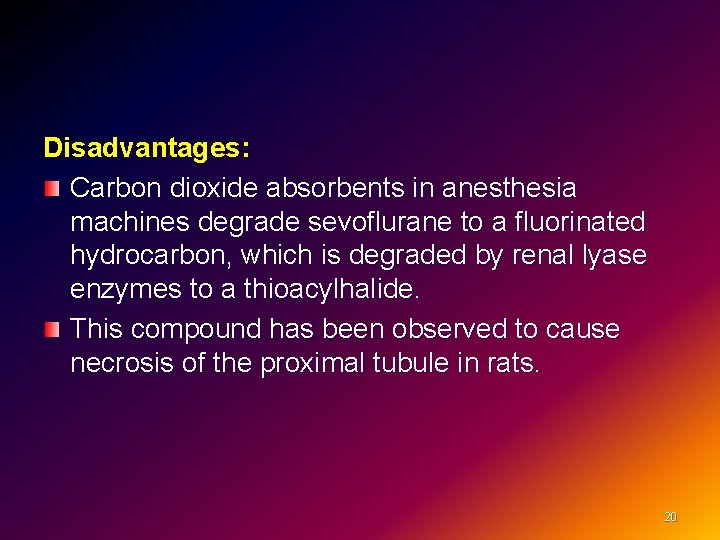
Disadvantages: Carbon dioxide absorbents in anesthesia machines degrade sevoflurane to a fluorinated hydrocarbon, which is degraded by renal lyase enzymes to a thioacylhalide. This compound has been observed to cause necrosis of the proximal tubule in rats. 20
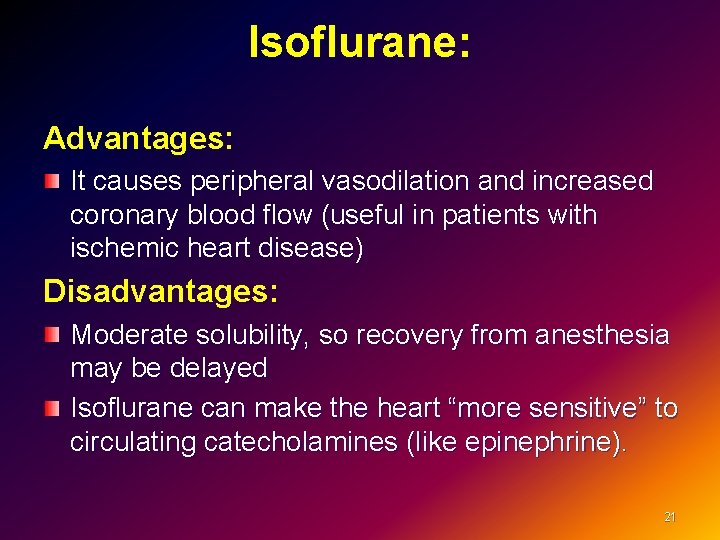
Isoflurane: Advantages: It causes peripheral vasodilation and increased coronary blood flow (useful in patients with ischemic heart disease) Disadvantages: Moderate solubility, so recovery from anesthesia may be delayed Isoflurane can make the heart “more sensitive” to circulating catecholamines (like epinephrine). 21
Halothane Used for induction in children (sweet pleasant odor); Toxicity – cardiac arrhythmias, “halothane hepatitis” (rare). 22
Nitrous Oxide Not used alone (except where full anesthesia not necessary; e. g. dental procedures); Causes more nausea/vomiting; q Contraindicated in patients with air filled cavities (e. g. air embolus, pneumothorax, etc) or vitamin B 12 deficiency. 23
Neuromuscular blocking drugs 24
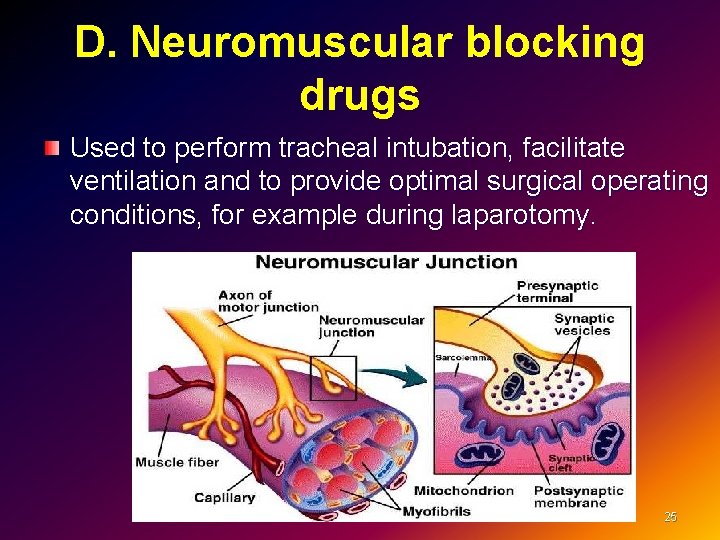
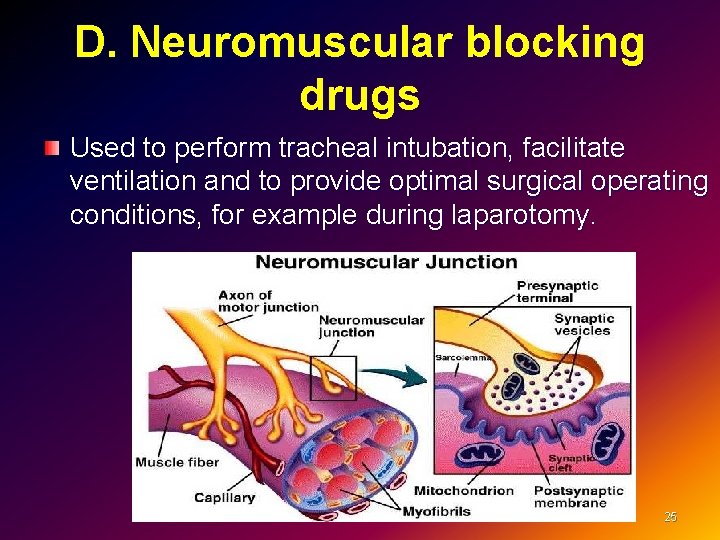
D. Neuromuscular blocking drugs Used to perform tracheal intubation, facilitate ventilation and to provide optimal surgical operating conditions, for example during laparotomy. 25
Depolarizing(Succinycholine) Structurally similar to acetylcholine and function as competitive inhibitors. Very short duration of action Metabolized very quickly by an enzyme called plasma cholinesterase. A useful drug in situations where muscle relaxation is needed for only a short time such as to facilitate intubation. 26
Side effects : Fasciculations. Muscle pain Bradycardia. Increases in ocular and gastric pressure, Hyperkalemia. Anaphylaxis. Malignant hyperthermia: a dramatic increase in body temperature, acidosis, electrolyte imbalance and shock 27
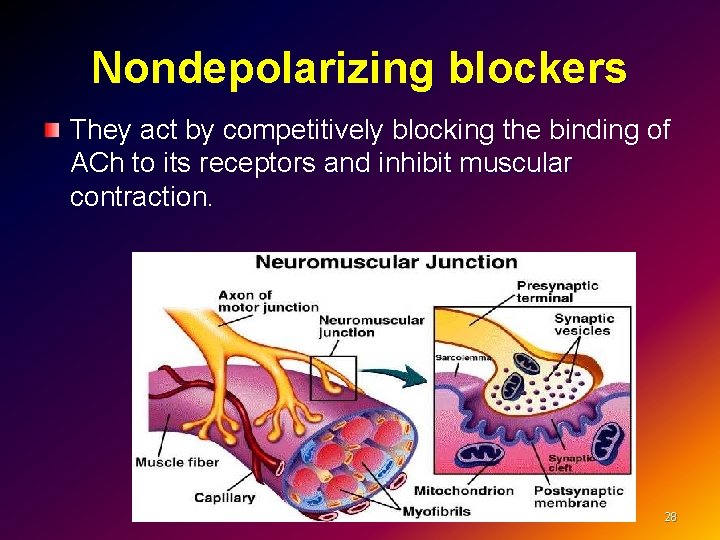
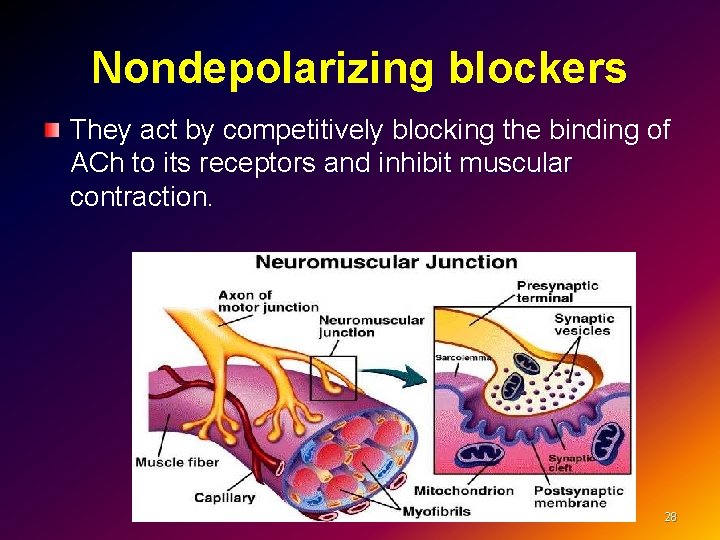
Nondepolarizing blockers They act by competitively blocking the binding of ACh to its receptors and inhibit muscular contraction. 28
Pancuronium bromide (Pavulon) The first steroid NMBD in clinical use has a slow onset and long duration of action. It does not cause histamine release Weak sympathomimetic properties and causes tachycardia. It is partly de-acylated in the liver to a metabolite with neuromuscular blocking properties, and partly excreted unchanged in the urine. Its action is prolonged in renal and hepatic impairment. 29
Atracurium besylate (Tracrium) Widely used and have an intermediate onset and duration of action. It causes release of histamine but has no direct cardiovascular effects. Metabolism is by Hofmann degradation and ester hydrolysis in the plasma, hence its duration of action is independent of renal and hepatic function. A breakdown product of atracurium, laudanosine may accumulate due to very slow hepatic metabolism and upon crossing into the brain may cause seizures 30
Cisatracurium(Nimbex) Isomer of atracurium Less laudanosine formed. Unlike atracurium it does not release histamine. It is metabolised by Hofmann degradation and does not accumulate in renal failure. 31
Vecuronium bromide(Norcuron) Vecuronium is structurally similar to pancuronium but has a slightly faster onset and shorter (intermediate) duration of action. It does not release histamine or have any cardiovascular effects. Metabolism in the liver occurs active metabolites before being excreted in the bile and urine. Lack of dependence on good kidney function for elimination provide advantages over other neuromuscular blocking agents. 32
Rocuronium. The most rapid onset of the clinically available non -depolarizing NMBDs. Intubating conditions can be achieved in 60 -90 seconds after an induction dose of 0. 6 mg/Kg. An intermediate duration of action. Metabolised in the liver and excreted in the bile. Minimal cardiovascular effects. Does not release histamine, Higher incidence of anaphylactic reactions 33
Anticholinesterases (Neostigmine) (acetylcholinesterase inhibitors) are agents that inhibit the action of the acetylcholinesterase enzyme at the neuromuscular junction. q Clinical tests of adequate resolution of neuromuscular block include the ability to lift the head from the bed for 5 seconds, q No role for anticholinesterases in reversing the effects of suxamethonium. 34
Side effects Bradycardia, miosis, GI upset, Nausea, bronchospasm, increased bronchial secretions, sweating and salivation. For this reason an antimuscarinic such as glycopyrronium or atropine must be administered along with the anticholinesterase to minimise these effects. 35

36
 What is my three word location
What is my three word location Care of iv cannula site ppt
Care of iv cannula site ppt Iv cannula labelling
Iv cannula labelling Extravasation vs infiltration vs phlebitis
Extravasation vs infiltration vs phlebitis Line & catheter label - intravenous burette
Line & catheter label - intravenous burette Medication administration test answers
Medication administration test answers National standard for user applied labelling
National standard for user applied labelling Concepts of medication administration pretest
Concepts of medication administration pretest Site:slidetodoc.com
Site:slidetodoc.com Baricity of local anesthetics
Baricity of local anesthetics Vrg
Vrg Classification of local anesthetics
Classification of local anesthetics Spinal anesthesia structures pierced
Spinal anesthesia structures pierced Site:slidetodoc.com
Site:slidetodoc.com Mac anesthesia minimum alveolar concentration
Mac anesthesia minimum alveolar concentration What is regional anesthesia
What is regional anesthesia 2nd gas effect
2nd gas effect Sevoflurane mac value
Sevoflurane mac value Ansc 497
Ansc 497 Pharmacology chapter 1
Pharmacology chapter 1 Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Pharmacology newcastle
Pharmacology newcastle Basic principles of pharmacology
Basic principles of pharmacology Pharmacology definition
Pharmacology definition First pass effect
First pass effect Define pharmacology
Define pharmacology Glomerular filtration
Glomerular filtration Glomerular filtrate
Glomerular filtrate Basic & clinical pharmacology
Basic & clinical pharmacology Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Clinical pharmacology seminar
Clinical pharmacology seminar Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals What is ion trapping in pharmacology
What is ion trapping in pharmacology Efficacy definition pharmacology
Efficacy definition pharmacology First pass effect
First pass effect Clinical pharmacology residency
Clinical pharmacology residency Pharmacology tutor anderson
Pharmacology tutor anderson