Pharmacists as Medical Providers DON DOWNING CLINICAL PROFESSOR






- Slides: 20
Pharmacists as Medical Providers DON DOWNING CLINICAL PROFESSOR, UNIV. OF WA SCHOOL OF PHARMACY SEATTLE, WA DONDOWN@UW. EDU
Conflicts of Interest I have no commercial conflicts of interest and I am not being compensated for this webinar I am not a consultant or advisor for Wolters Kluwer Clinical Drug Information
Objectives Understanding the difference between pharmacist provider status & pharmacist medical provider status Creating provider leverage from existing state laws Establishing professional guidelines when both prescribing & selling prescription medications Unbundling pharmacy location licenses from pharmacist medical provider practice Establishing sustainable & responsible professional practices that improve patient outcomes

What is Provider Status?

Provider Status What is it that pharmacists are seeking? Is it… Professional, patient & legislative recognition of our clinical skills & services? A scope of practice expansion, incl. prescribing medications? Elimination of dependence on selling medications for income? A new revenue stream that compensates & sustains professional practice? “Full” membership on healthcare teams / medical boards? Getting out of the “drug benefit” wedge? A legislative acknowledgement that says pharmacists are providers? Ability to practice at the top of our license To be able to help patients in ways we struggle to provide right now
Pharmacist provider status State legislative recognition in name only No Federal recognition other than low-level MTM billings by pharmacies (but not pharmacists) Payment of some services through NDC#-based claims submissions Payment of some services through “incident-to” medical billings Facility fee payments for health system clinical care services But: mostly provision of valuable clinical services without sustainable compensation due to rejection of pharmacists as contracted, credentialed providers in health plan networks
Pharmacist medical provider status State and commercial health plans recognize pharmacists as contracted and credentialed medical providers (Feds soon…? ) Major medical CPT and ICD-10 codes used for provider claims Incident-to billing the exception rather than the rule Pharmacists making decisions not just taking orders Collaborative agreements are not direct supervision by physicians – they are coordination of care / expansion of care partnerships No PBM involvement Allows clinics, hospitals and community pharmacies to hire pharmacists as medical providers – not pharmacist providers

Getting there: Where is the Leverage?
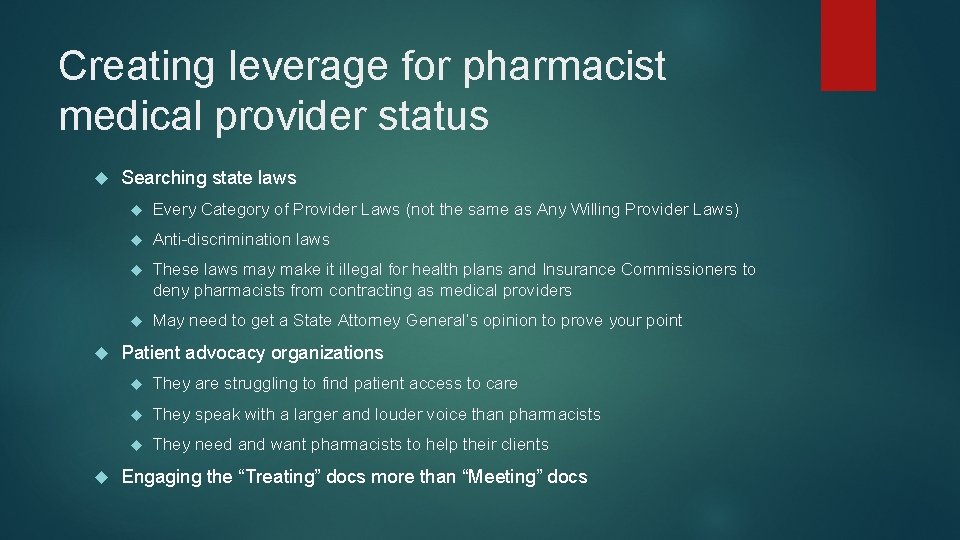
Creating leverage for pharmacist medical provider status Searching state laws Every Category of Provider Laws (not the same as Any Willing Provider Laws) Anti-discrimination laws These laws may make it illegal for health plans and Insurance Commissioners to deny pharmacists from contracting as medical providers May need to get a State Attorney General’s opinion to prove your point Patient advocacy organizations They are struggling to find patient access to care They speak with a larger and louder voice than pharmacists They need and want pharmacists to help their clients Engaging the “Treating” docs more than “Meeting” docs

Conflicts of Interest
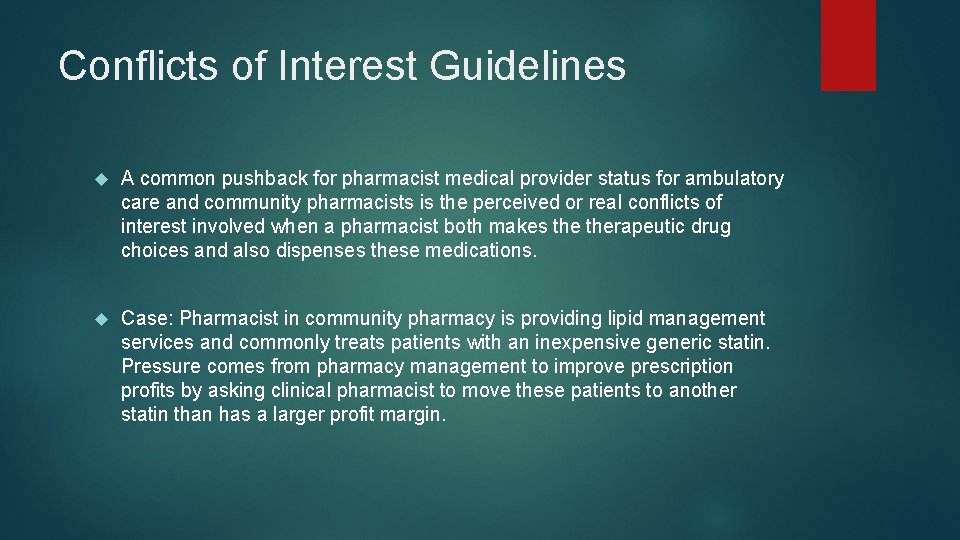
Conflicts of Interest Guidelines A common pushback for pharmacist medical provider status for ambulatory care and community pharmacists is the perceived or real conflicts of interest involved when a pharmacist both makes therapeutic drug choices and also dispenses these medications. Case: Pharmacist in community pharmacy is providing lipid management services and commonly treats patients with an inexpensive generic statin. Pressure comes from pharmacy management to improve prescription profits by asking clinical pharmacist to move these patients to another statin than has a larger profit margin.
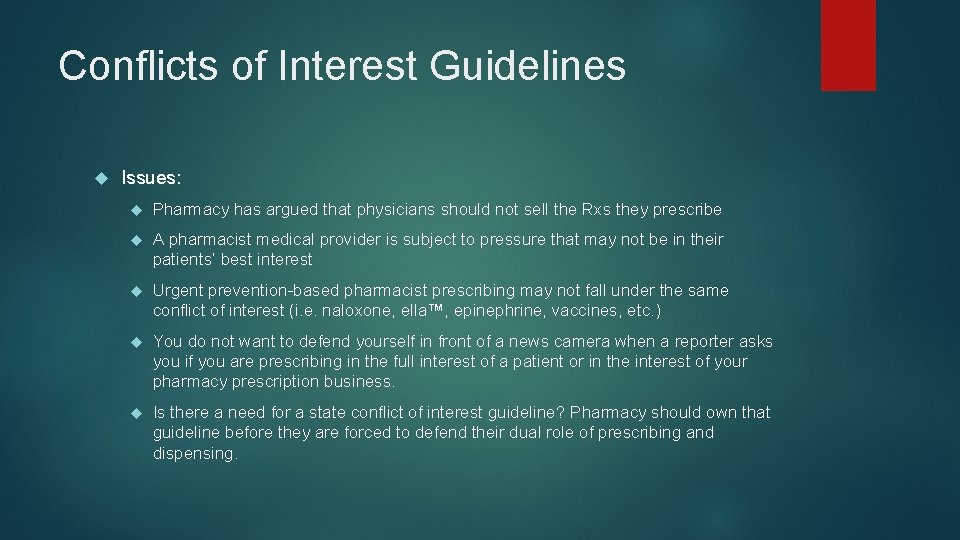
Conflicts of Interest Guidelines Issues: Pharmacy has argued that physicians should not sell the Rxs they prescribe A pharmacist medical provider is subject to pressure that may not be in their patients’ best interest Urgent prevention-based pharmacist prescribing may not fall under the same conflict of interest (i. e. naloxone, ella™, epinephrine, vaccines, etc. ) You do not want to defend yourself in front of a news camera when a reporter asks you if you are prescribing in the full interest of a patient or in the interest of your pharmacy prescription business. Is there a need for a state conflict of interest guideline? Pharmacy should own that guideline before they are forced to defend their dual role of prescribing and dispensing.
Pharmacy Location Licensure
Mandated Pharmacy Location licensure Most states have laws/rules that require pharmacists to practice in a licensed pharmacy Should a pharmacist medical provider who is not dispensing medications be required to get a pharmacy location license? If you are seeking pharmacist medical provider status, consider amending your state pharmacy regulations or get a legal opinion regarding the need for a location license as soon as possible.

A Brave New World

Pharmacist medical provider: Rules of the road Issues to ponder: Are you’re a specialist, a primary care provider or both in health plan networks? Does your compensation reasonably match the value you provide and your ability to provide sustainable clinical services? When do your clinical services need a prior referral or other similar mechanism in order to meet quality assurance requirements to: coordinate care, to not duplicate care, & to provide medically necessary services?
Rules of the Road Who will credential you with employers and health plans? Does your employer have a “delegated credentialing” contract with health plans? What is your scope of practice and how is that decided? What CPT/ICD-10 billing codes will you insist be appropriate for your services? Are you measuring outcomes?
Rules of the Road: Collaborative Agreements It’s time to look at your collaborative drug therapy management agreement (CDTA) regulations: Do CDTA regulations only allow pharmacists to implement, modify or discontinue drug therapy when the authorizing physician has a legitimate physician-patient relationship? What about patients who don’t have a physician provider? Shouldn’t you as a “medical provider” be their initial provider? Can only physicians sign CDTAs? Are CDTA relationships with physicians a direct supervisory relationship? Are pharmacists writing prescriptions or furnishing /dispensing prescriptions under protocol?
Pharmacist medical provider status Will your state pharmacist association, your state medical association, your state legislature, or your state’s health plans decide that pharmacist medical providers need to achieve a higher pharmacy practice status in order to provide and be compensated for pharmacist medical provider services? Is a pharmacy degree adequate? Do you need to complete a residency? Do you need Board Certification? Are these requirements barriers to patient access to care? Can schools of pharmacy graduate students who are prequalified to be pharmacist medical providers? States are answering these questions differently. Carefully consider the consequences.
Questions?
 Paul cornelison
Paul cornelison Promotion from assistant to associate professor
Promotion from assistant to associate professor Walt downing
Walt downing Shroud pfp
Shroud pfp John w reed inventor
John w reed inventor K-12 construction tacoma
K-12 construction tacoma Closed for the season mary downing hahn
Closed for the season mary downing hahn Elise downing
Elise downing Walt downing
Walt downing Introduction to medical terminology chapter 1 answer key
Introduction to medical terminology chapter 1 answer key Taking something that doesn't belong to you
Taking something that doesn't belong to you Forrester wave loyalty program service providers
Forrester wave loyalty program service providers Teta accredited providers list
Teta accredited providers list Teamsters local 237 retirees benefit fund
Teamsters local 237 retirees benefit fund Educational hub acca
Educational hub acca Adit exam
Adit exam United healthcare community plan
United healthcare community plan Ignition interlock device definition
Ignition interlock device definition Masshealth dental providers portal
Masshealth dental providers portal Gsa office of governmentwide policy
Gsa office of governmentwide policy The basic value proposition of community providers is:
The basic value proposition of community providers is: