Phacoantigenic Response to Ruptured Lens Capsule Clinicopathologic Case
- Slides: 20
Phacoantigenic Response to Ruptured Lens Capsule: Clinicopathologic Case Emily Deschler, MD Charleen Chu, MD, Ph. D March 2011
Brief History and Course • 58 year-old woman • Blind left eye since teens – unknown etiology • No history of trauma • Referred to glaucoma service when left eye became painful
Initial Physical Exam • Vision: – Right eye: 20/20 – Left eye: NLP • IOP: – Right eye: 11 – Left eye: 16 • Pupil: – Right eye: 4 -3 – Left eye: Irregular • Anterior segment – Right eye: Shallow anterior chamber with patent PI – Left eye: injected conjunctiva, cornea with PEE, shallow anterior chamber with patent PI x 2, iris with florid rubeosis, posterior synechiae, mature cataract • Fundus: – Right eye: Normal, c/d 0. 6 with healthy neuroretinal rim – Left eye: no view
Brief History and Course • Symptoms initially attributed to ocular surface disease and treated with artificial tears, topical steroids • 1 year later, pain continued and patient elected to proceed with enucleation (PHS 10 -35123)
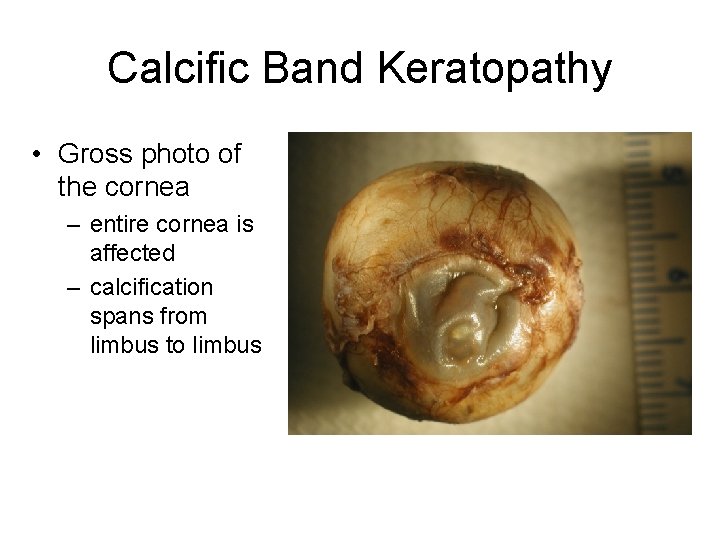
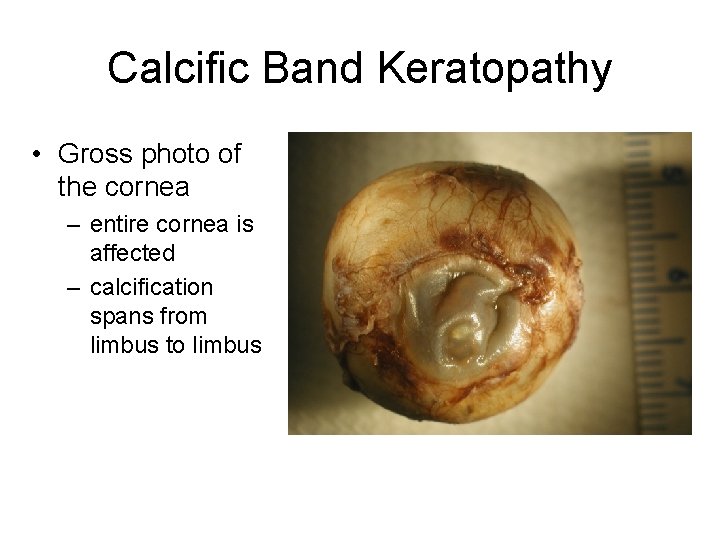
Calcific Band Keratopathy • Gross photo of the cornea – entire cornea is affected – calcification spans from limbus to limbus
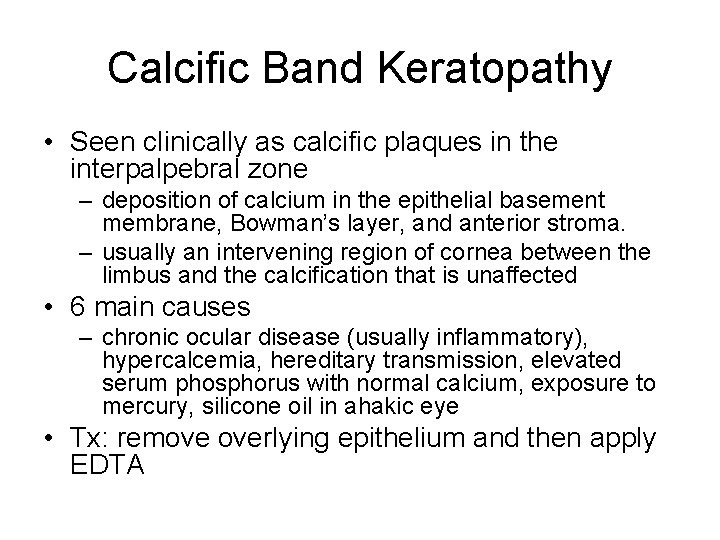
Calcific Band Keratopathy • Seen clinically as calcific plaques in the interpalpebral zone – deposition of calcium in the epithelial basement membrane, Bowman’s layer, and anterior stroma. – usually an intervening region of cornea between the limbus and the calcification that is unaffected • 6 main causes – chronic ocular disease (usually inflammatory), hypercalcemia, hereditary transmission, elevated serum phosphorus with normal calcium, exposure to mercury, silicone oil in ahakic eye • Tx: remove overlying epithelium and then apply EDTA
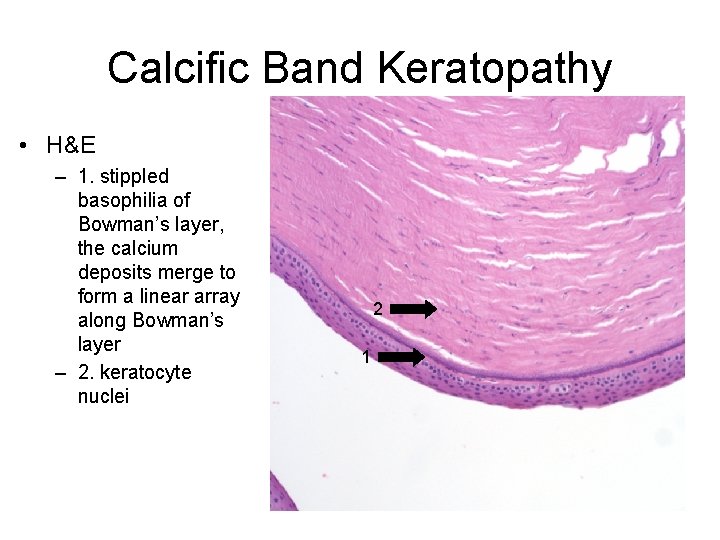
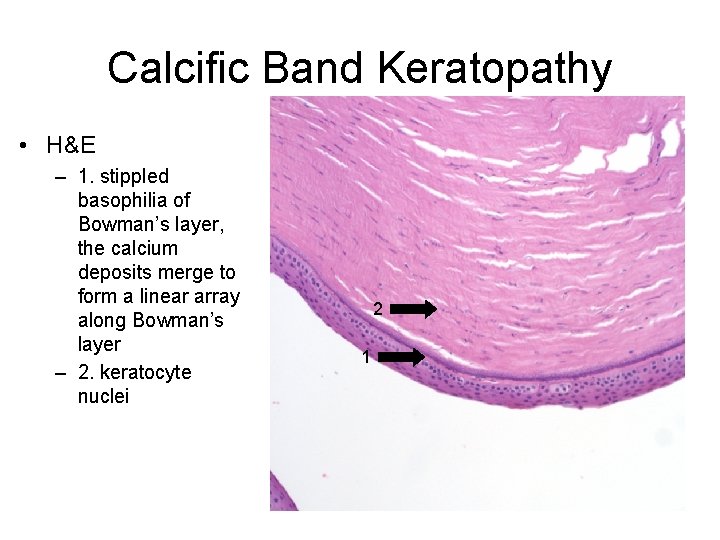
Calcific Band Keratopathy • H&E – 1. stippled basophilia of Bowman’s layer, the calcium deposits merge to form a linear array along Bowman’s layer – 2. keratocyte nuclei 2 1
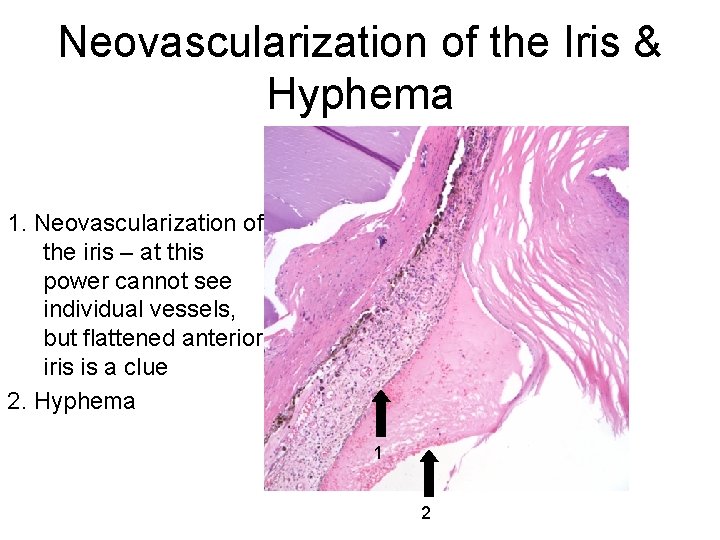
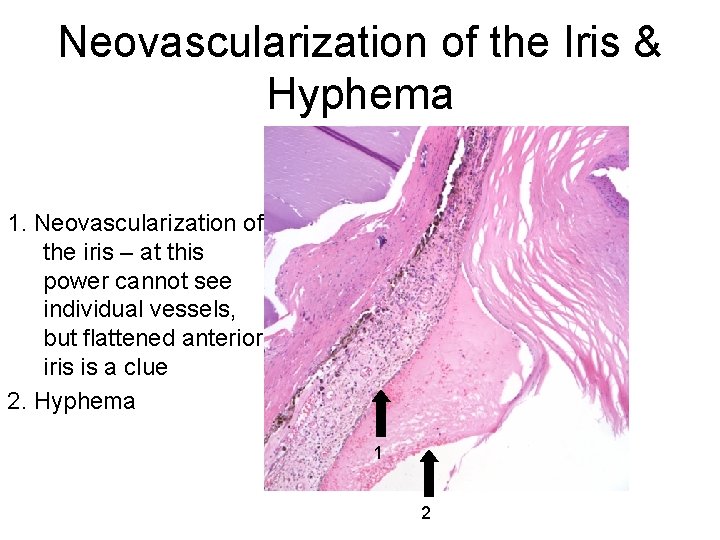
Neovascularization of the Iris & Hyphema 1. Neovascularization of the iris – at this power cannot see individual vessels, but flattened anterior iris is a clue 2. Hyphema 1 2
Disorders Predisposing to Neovascularization of Iris and Angle • Systemic vasular disease – Carotid disease – Giant cell arteritis • Ocular vascular disease – – – – Diabetes CRVO Coats Eales ROP Persistent fetal vasculature Anterior segment ischemia • Ocular disease – – – Cronic uveitis Chronic retinal detachment Endophthalmitis Stickler syndrome Retinoschisis • Intraocular tumors – Uveal melanoma – Metastatic disease – Retinoblastoma • Ocular therapy – Radition therapy
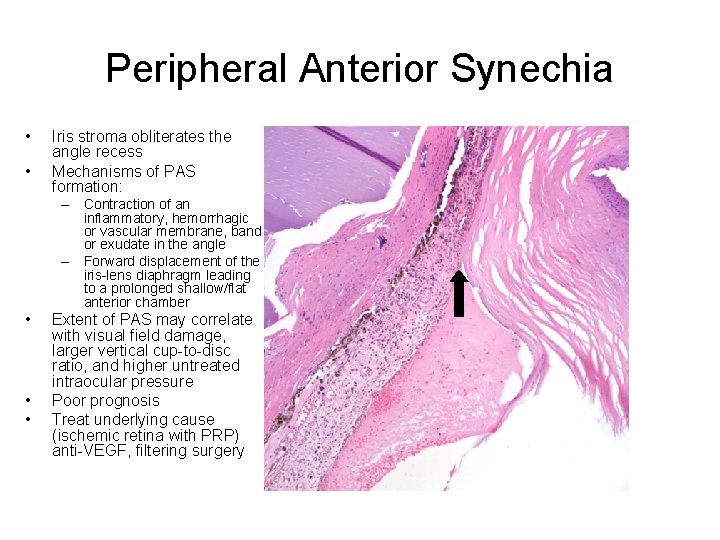
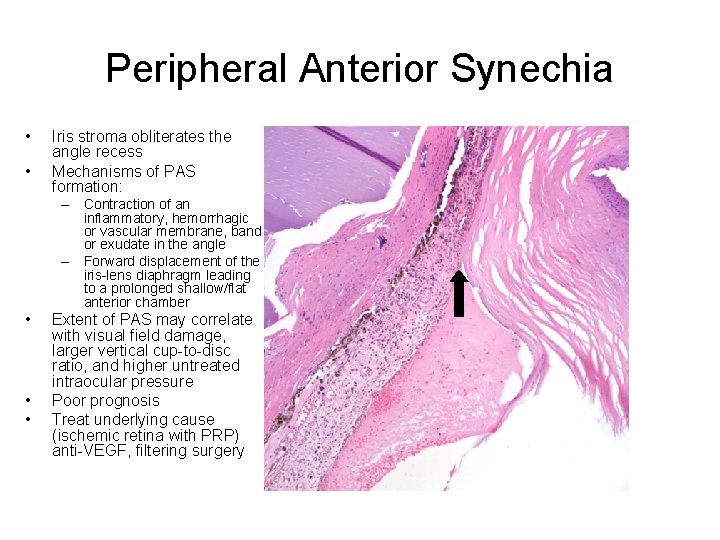
Peripheral Anterior Synechia • • Iris stroma obliterates the angle recess Mechanisms of PAS formation: – Contraction of an inflammatory, hemorrhagic or vascular membrane, band or exudate in the angle – Forward displacement of the iris-lens diaphragm leading to a prolonged shallow/flat anterior chamber • • • Extent of PAS may correlate with visual field damage, larger vertical cup-to-disc ratio, and higher untreated intraocular pressure Poor prognosis Treat underlying cause (ischemic retina with PRP) anti-VEGF, filtering surgery
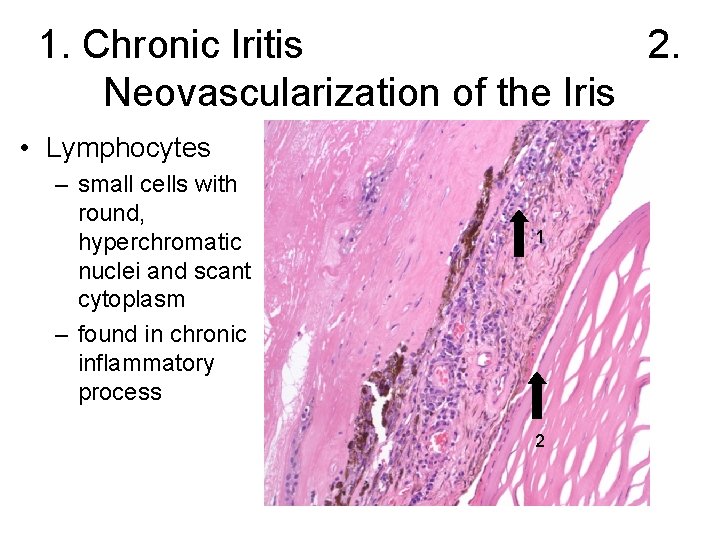
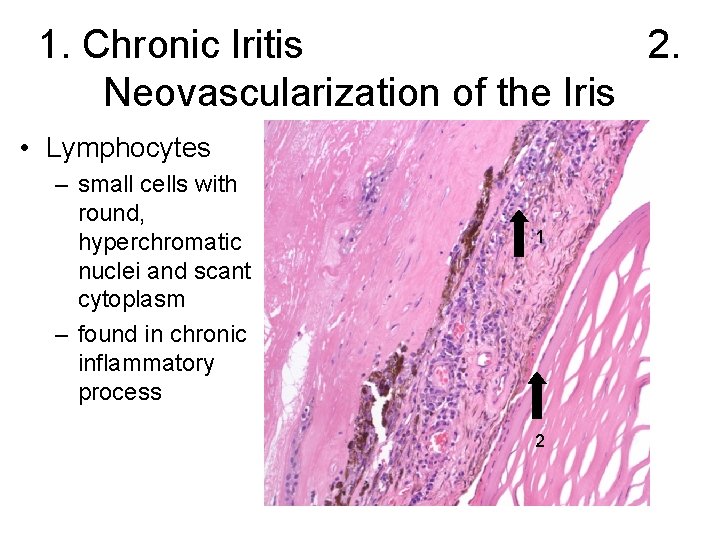
1. Chronic Iritis 2. Neovascularization of the Iris • Lymphocytes – small cells with round, hyperchromatic nuclei and scant cytoplasm – found in chronic inflammatory process 1 2
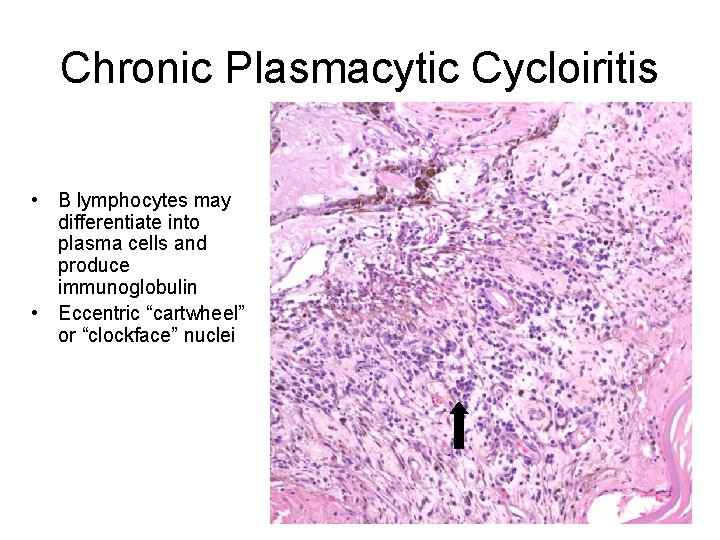
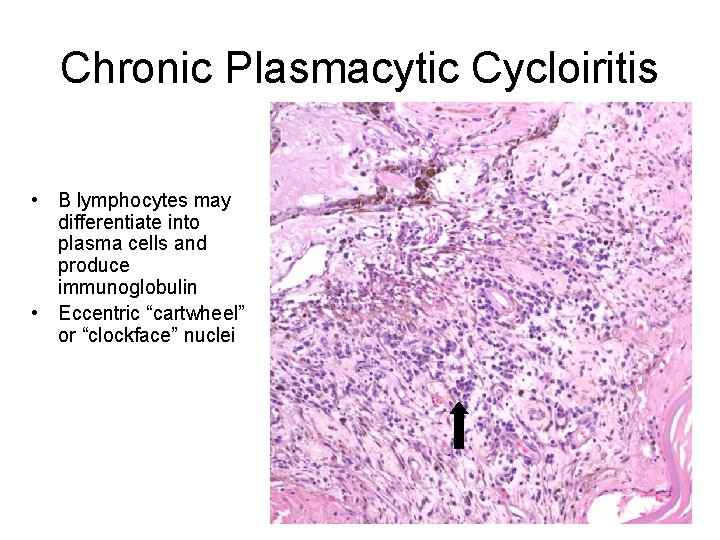
Chronic Plasmacytic Cycloiritis • B lymphocytes may differentiate into plasma cells and produce immunoglobulin • Eccentric “cartwheel” or “clockface” nuclei
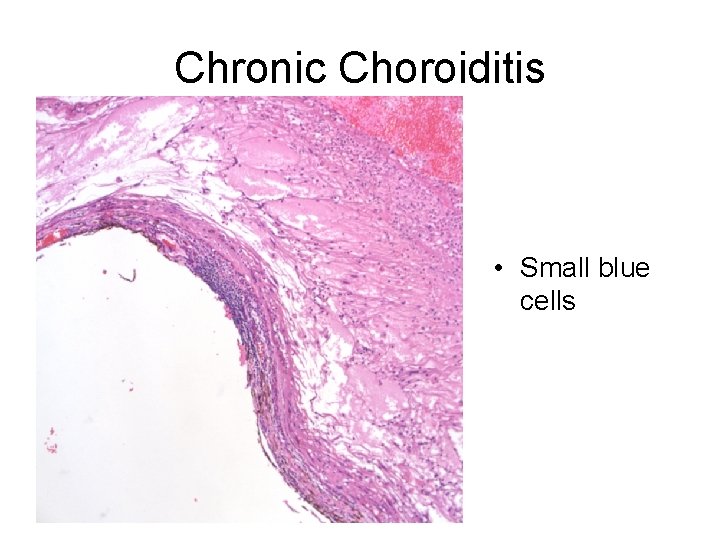
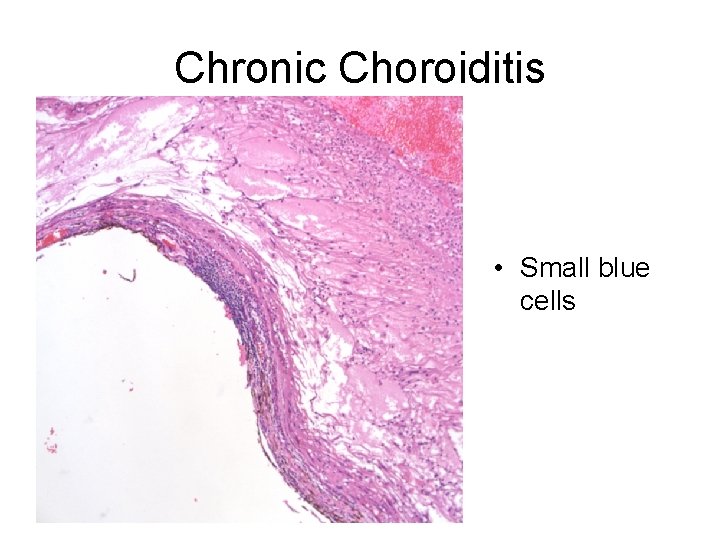
Chronic Choroiditis • Small blue cells
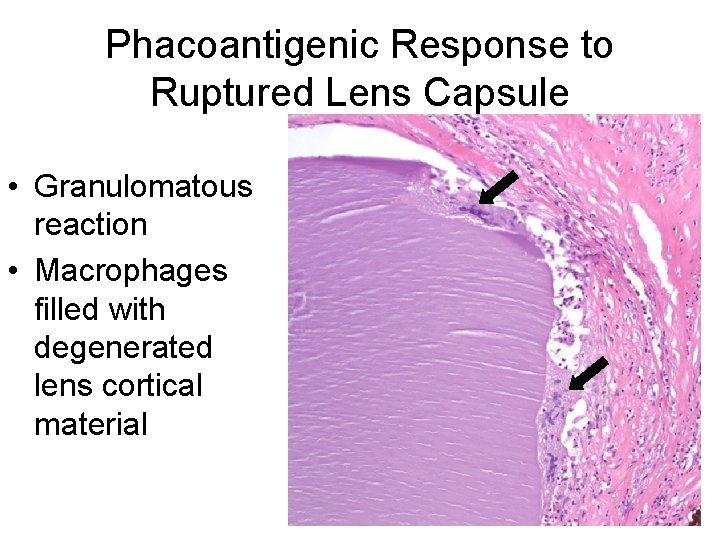
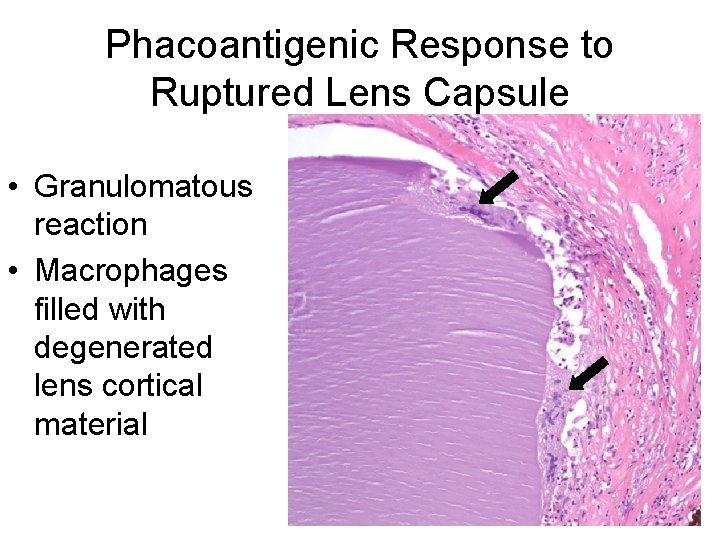
Phacoantigenic Response to Ruptured Lens Capsule • Granulomatous reaction • Macrophages filled with degenerated lens cortical material
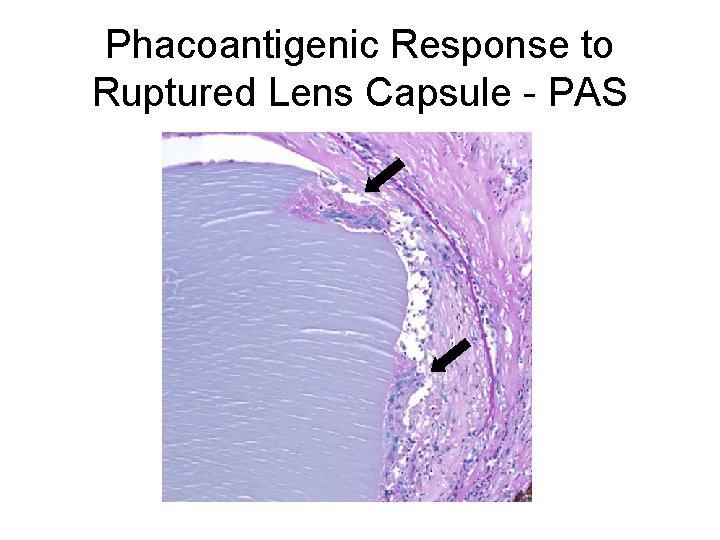
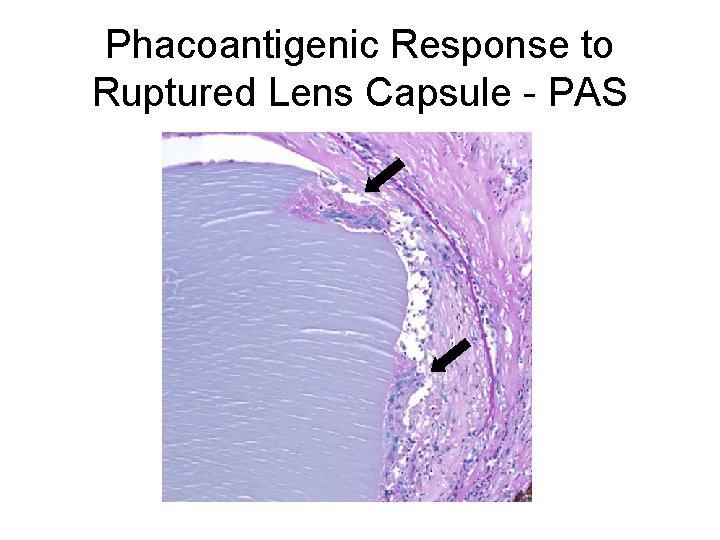
Phacoantigenic Response to Ruptured Lens Capsule - PAS
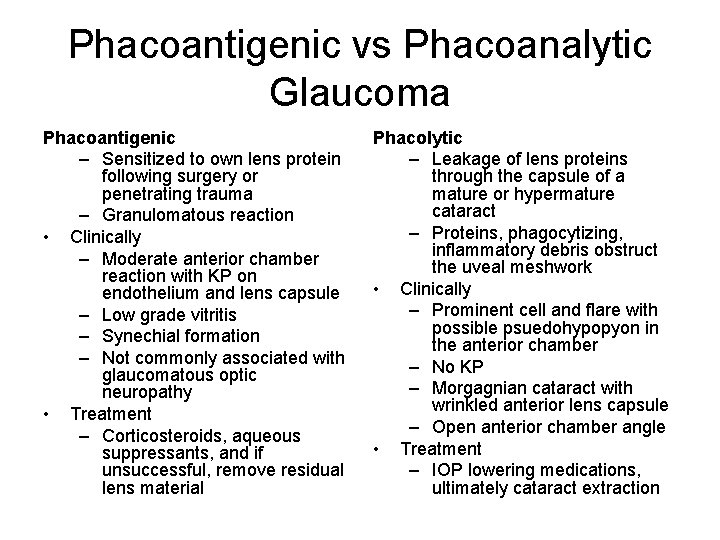
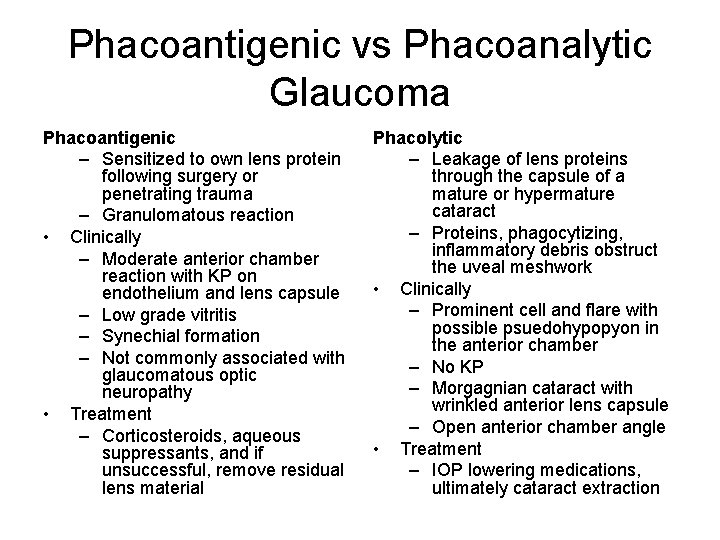
Phacoantigenic vs Phacoanalytic Glaucoma Phacoantigenic – Sensitized to own lens protein following surgery or penetrating trauma – Granulomatous reaction • Clinically – Moderate anterior chamber reaction with KP on endothelium and lens capsule – Low grade vitritis – Synechial formation – Not commonly associated with glaucomatous optic neuropathy • Treatment – Corticosteroids, aqueous suppressants, and if unsuccessful, remove residual lens material Phacolytic – Leakage of lens proteins through the capsule of a mature or hypermature cataract – Proteins, phagocytizing, inflammatory debris obstruct the uveal meshwork • Clinically – Prominent cell and flare with possible psuedohypopyon in the anterior chamber – No KP – Morgagnian cataract with wrinkled anterior lens capsule – Open anterior chamber angle • Treatment – IOP lowering medications, ultimately cataract extraction
Discussion: Phacoantigenic response to ruptured lens capsule • Occurs following surgery or penetrating trauma causing sensitization to one’s own lens protein – Granulomatous reaction – Variable clinical presentation: moderate AC reaction with KP on corneal endothelium and anterior lens surface (unlike phacolytic) with moderate AC reaction. Low grade vitritis, synechial formation, residual lens material may be in AC – Not commonly associated with glaucomatous optic neuropathy. • Treatment – Corticosteroids, aqueous suppressants, and if unsuccessful, remove residual lens material
Discussion: Phacolytic response to mature cataract • Proteins, phagocytizing macrophages, and other inflammatory debris obstruct the trabecular meshwork • Generally an elderly person with a history of poor vision presents with sudden onset pain, conjunctival injection, elevated IOP, corneal edema, prominent cell and flair without KP and open anterior chamber angle • Cellular debris may be present in the anterior chamber presenting as pseudohypopyon. The anterior capsule may appear wrinkled representing loss of lens material • Treatment: – IOP lowering medications, ultimately cataract extraction
• Diagnosis: – Phacoantigenic immune response to ruptured lens capsule • Additional diagnoses: – Idiopathic chronic panophthalmitis – Neovascularization of the iris – Peripheral anterior synechiae – Calcific band keratopathy
Sources • Basic Clinical Science Course Section 10: Glaucoma. American Academy of Ophthalmology 2009 -2010 • Yanoff, Myron and Fine, Ben. Ocular Pathology. Mosby. 2002