PFAPA SYNDROME Cormac J OConnor MD LT MC




- Slides: 22
PFAPA SYNDROME Cormac J. O’Connor MD, LT, MC, USN Naval Hospital Camp Pendleton, CA
Introduction • Fever is the presenting complaint in 30 -50% of pediatric acute visits • Most “recurrent fevers” are actually superimposed viral infections
Introduction • In periodic fever cases in the U. S. , PFAPA is the most common cause
PFAPA • • • Periodic Fever Aphthous ulcers Pharyngitis Adenopathy
Key Points • PFAPA – Fevers are brief (<5 d), unheralded periodic fevers with “APA” symptoms and no other focus of disease – Wellness between fevers with normal growth, development and activity
Key Points • Patients with PFAPA are completely well • Have fewer viral URI’s than their siblings
Case Presentation • 2 ½-year-old boy in ER for 2 days of fever to 101 F and neck tenderness, without URI symptoms • Exam, CBC and UA were normal, d/c home with “febrile illness” • Symptoms resolved fully in 3 -4 days
Case Presentation • Symptoms recurred every 4 weeks for the next 18 months • Review of medical, family, social, travel, and exposure histories was unremarkable • Multiple ER visits resulted in febrile illness or URI diagnoses
Case Presentation • Most impressive was the speed of clinical change • Oral ulcers noted with fever • Referred to NMCSD pediatric infectious disease department
Case Presentation • Febrile episodes recurred every four weeks from 2 ½ - 4 years old • He is nearly 6 years old and in full health without sequelae

Discussion • Medline and Google searches using the keywords Recurrent, Pediatric and Fever identified in the literature similarities between this case and the PFAPA syndrome

Discussion • Identified in 1987 by Marshall, et al – aka Marshall’s syndrome, then later PFAPA syndrome • Etiology – Infectious vs. Autoimmune unclear • Incidence – Far greater than other recurrent fevers (Cyclic neutropenia, FMF, HIDS, etc. )
Discussion • Onset typically 2 -5 yo • Usually resolves by 8 yo • Male > female • No known ethnic predilection
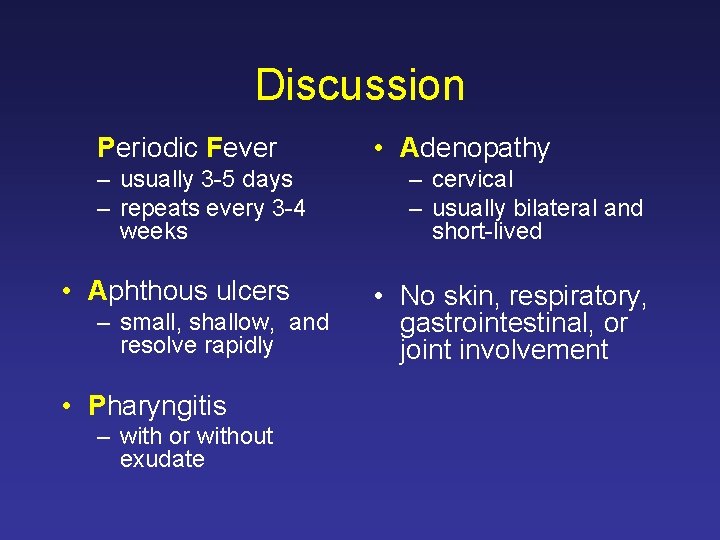
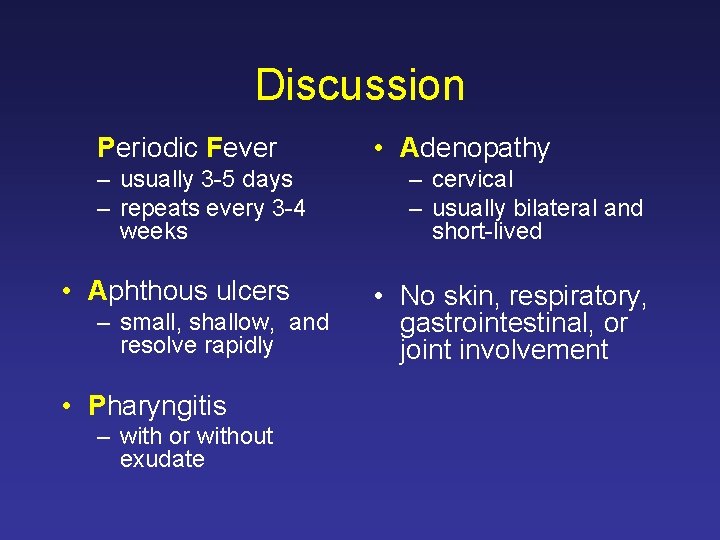
Discussion Periodic Fever – usually 3 -5 days – repeats every 3 -4 weeks • Aphthous ulcers – small, shallow, and resolve rapidly • Pharyngitis – with or without exudate • Adenopathy – cervical – usually bilateral and short-lived • No skin, respiratory, gastrointestinal, or joint involvement

Diagnostic Criteria • Periodic fevers onset < 5 yo • Absence of URI sx including >1 of: – apthous stomatitis – cervical lymphadenitis – pharyngitis • Exclude cyclic neutropenia • Normal, asymptomatic intervals
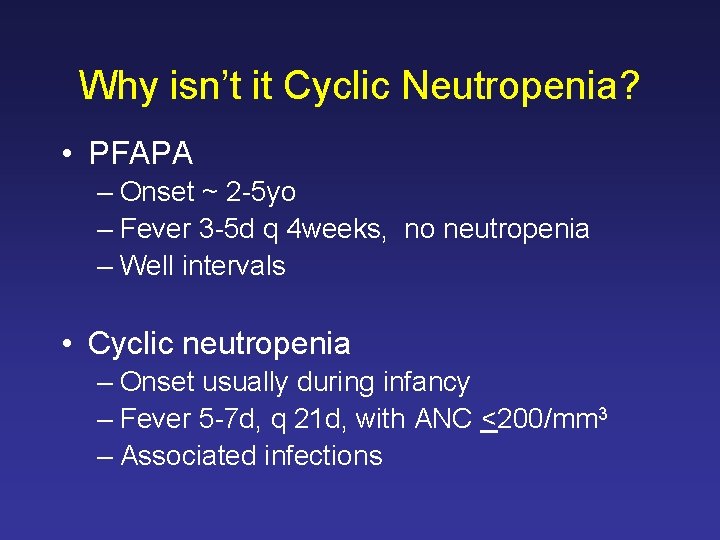
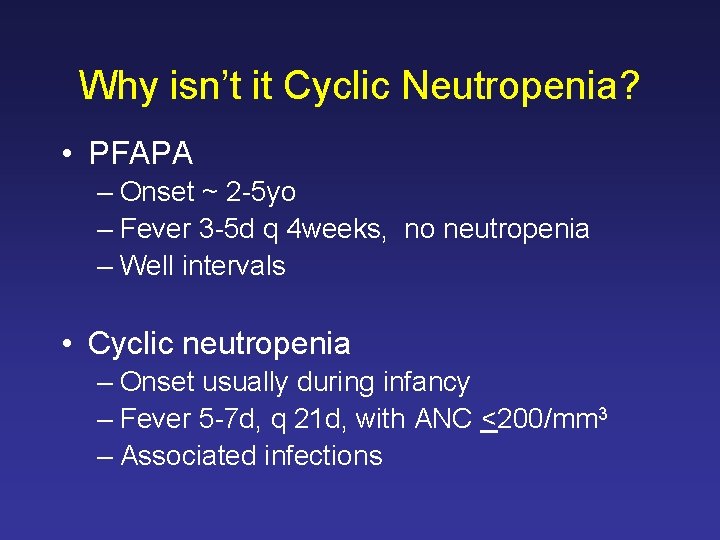
Why isn’t it Cyclic Neutropenia? • PFAPA – Onset ~ 2 -5 yo – Fever 3 -5 d q 4 weeks, no neutropenia – Well intervals • Cyclic neutropenia – Onset usually during infancy – Fever 5 -7 d, q 21 d, with ANC <200/mm 3 – Associated infections
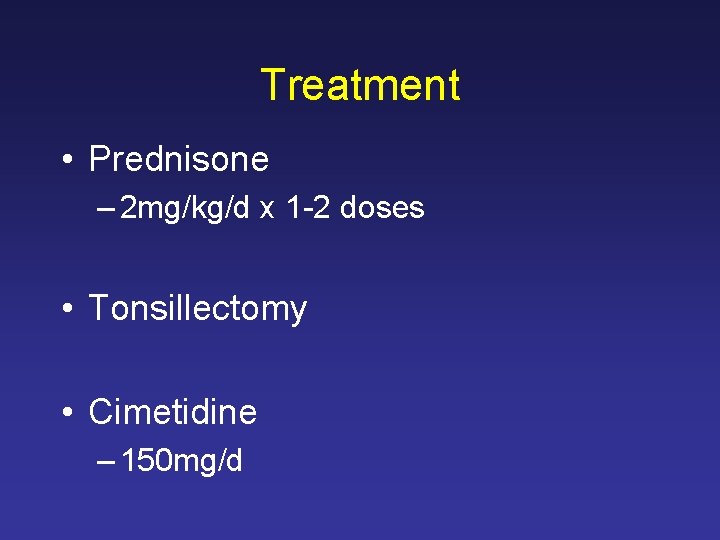
Treatment • Prednisone – 2 mg/kg/d x 1 -2 doses • Tonsillectomy • Cimetidine – 150 mg/d

When to Suspect and What to Do? • In typical presentations – No concern for other dx • After 3 -4 febrile episodes • One expert recommends only CBC, throat Cx, ESR, & ASO titer
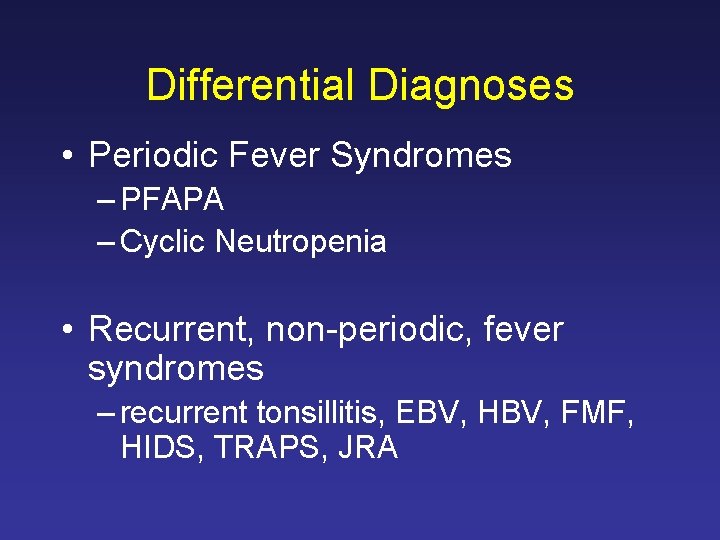
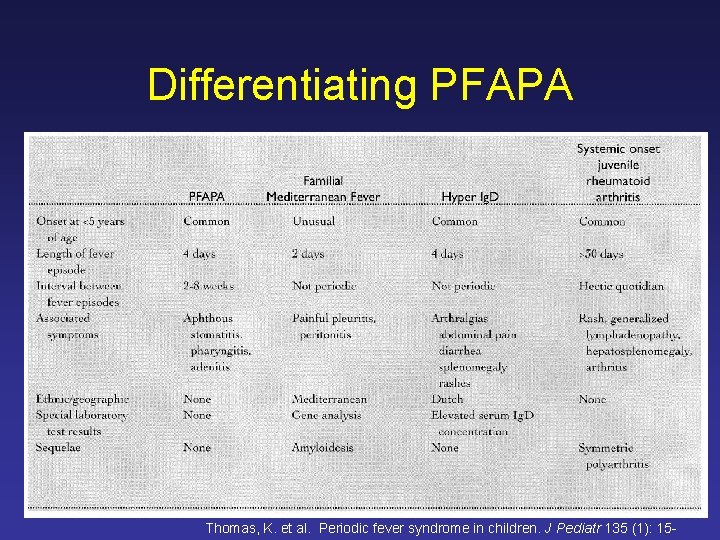
Differential Diagnoses • Periodic Fever Syndromes – PFAPA – Cyclic Neutropenia • Recurrent, non-periodic, fever syndromes – recurrent tonsillitis, EBV, HBV, FMF, HIDS, TRAPS, JRA
Conclusion • PFAPA is the #1 cause of periodic fever in the U. S. A. • Punctual periodic fevers, with aphthous ulcers, pharyngitis, and cervical adenopathy • Completely well intervals
Questions?
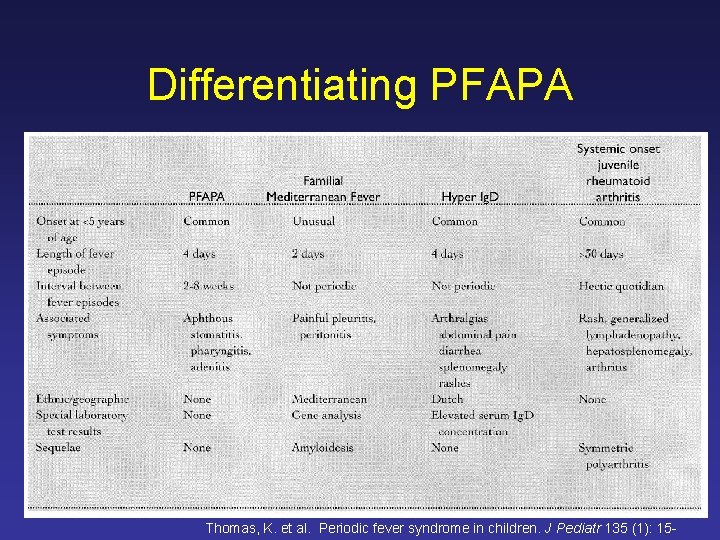
Differentiating PFAPA Thomas, K. et al. Periodic fever syndrome in children. J Pediatr 135 (1): 15 -
 Ekaih
Ekaih Pfapa criteria
Pfapa criteria Chris oconnor
Chris oconnor Maggie o connor age
Maggie o connor age Nancy oconnor
Nancy oconnor Cormac conroy
Cormac conroy Cormac flanagan
Cormac flanagan Cormac reynolds
Cormac reynolds Cormac toher
Cormac toher Cormac engineering
Cormac engineering Cormac toher
Cormac toher Cormac odea
Cormac odea Michael cormac roth
Michael cormac roth Syndrome méningé
Syndrome méningé Where does negative selection occur
Where does negative selection occur Androgen insensitivity syndrome
Androgen insensitivity syndrome Scheie stripe
Scheie stripe Dystopia canthorum
Dystopia canthorum Cri du chat karyotype
Cri du chat karyotype Nephrotic syndrome differential diagnosis
Nephrotic syndrome differential diagnosis Hellp syndrome symptoms
Hellp syndrome symptoms Occupational asthma
Occupational asthma Deiodinase
Deiodinase