Perometer 400 T measurement of lower limb volume
Perometer (400 T) measurement of lower limb volume: development of a standardised protocol Fiona Coutts, Andrew Grainger, Dr Cathy Bulley Queen Margaret University, Edinburgh, UK

Background • Various musculoskeletal, oncological or vascular conditions result in increased limb volume • Limb volume – outcome measures àFluid displacement àGeometric calculations from limb circumferences using tape measure àPerometer – optoelectronic imaging device; limb shape and volume (Pero-System Gmb. H, Wuppertal, Germany)

Purpose • True repeatable measurement important in monitoring treatment efficacy. • Perometer (400 T) optoelectronic imaging device used to assess limb volume. No protocol has been published to standardise its use.

Study Design Rest Period (A) Phase 1 Diurnal Variation (A) Foot position on base plate (B) Leg position (Rotation) (B) Phase 2 Speed of frame Movement (C) Standardised protocol End point of limb measurement (C) Use of software (D) Phase 3

Phase 1 A: Diurnal Variation • Issue: Does limb volume change through a day? • Results: Volumes averaged and % differences to initial volume were calculated. <2% volume change for each participant. • Design: n=2, healthy participants. 3 volume measurements @ 3 times per day, between 09. 00 and 18. 00. Tester Morning – Afternoon Morning – Evening 1 2 1. 1% 1. 6% 1. 8% 1. 2%

Phase 1 B: Foot position • Issue: Does the position of the limb on the base plate alter measurement data? • Results: Four centre squares (A, B, C, D) demonstrated the highest repeatability of measurement. Corner squares (1, 2, 3, 4) lowest repeatability. • Design: Cylinder placed in each of the 16 squares marked on the base plate, measured 3 times. 1 4 2 A B D C 3

Phase 1 C: End point of limb measurement • Issue: Standardised landmarks for measurement of volume? • Design: n=4, frame advanced to comfortable maximum vertical height, leg marked. Calculated as % of length Position 1 to 2 (see below) • Results: % leg length= 67. 6, 69, 79. 1, 81. 7; 65% of leg length was max. height for vertical frame advancement Grt Trochanter (1) 65% Femur Lat Femoral Epicondyle (2) Lateral Malleolus
Standardised Protocol 1 • Diurnal variation: keep standardised times for repeat visits • Foot position: maintain foot in the centre of the base plate at all times • End point of measurement: 65% of distance from lateral femoral Epicondyle to Greater Trochanter

Repeatability after phase 1 • n= 30 (22 F: 8 M) (25. 9± 3. 48 yrs, 171. 02± 6. 77 cm, 67. 32± 7. 68 Kg) Dominant leg – tested 9 times by a rater on 2 consecutive occasions ICC (p<0. 001) 95% CI 0. 996 -0. 999 Upper LOA 185. 18 ml Lower LOA -193. 81 ml Range % variation 378. 99 ml 4. 07% LOA= Limits of Agreement (Bland & Altman, 1986)

Concerns after phase 1 • Rest period prior to commencement of measurement • Axial rotation of the limb in the frame • Speed of Perometer frame movement = Phase 2
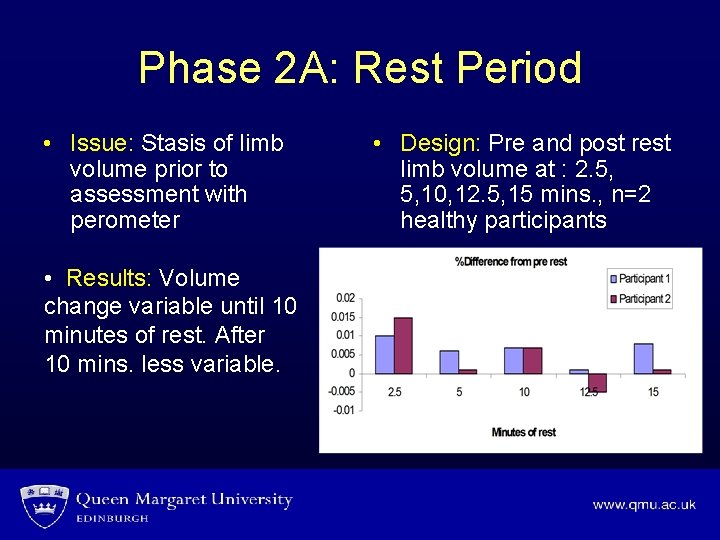
Phase 2 A: Rest Period • Issue: Stasis of limb volume prior to assessment with perometer • Results: Volume change variable until 10 minutes of rest. After 10 mins. less variable. • Design: Pre and post rest limb volume at : 2. 5, 5, 10, 12. 5, 15 mins. , n=2 healthy participants
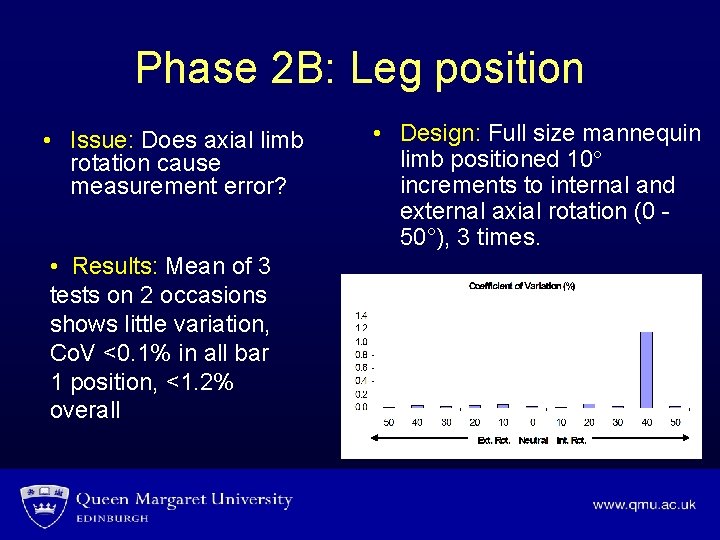
Phase 2 B: Leg position • Issue: Does axial limb rotation cause measurement error? • Results: Mean of 3 tests on 2 occasions shows little variation, Co. V <0. 1% in all bar 1 position, <1. 2% overall • Design: Full size mannequin limb positioned 10 increments to internal and external axial rotation (0 50°), 3 times.
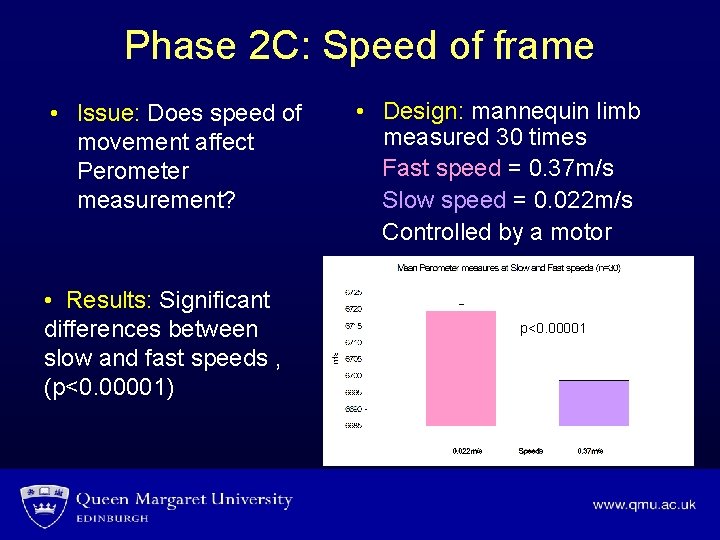
Phase 2 C: Speed of frame • Issue: Does speed of movement affect Perometer measurement? • Design: mannequin limb measured 30 times Fast speed = 0. 37 m/s Slow speed = 0. 022 m/s Controlled by a motor • Results: Significant differences between slow and fast speeds , (p<0. 00001) p<0. 00001 Motor
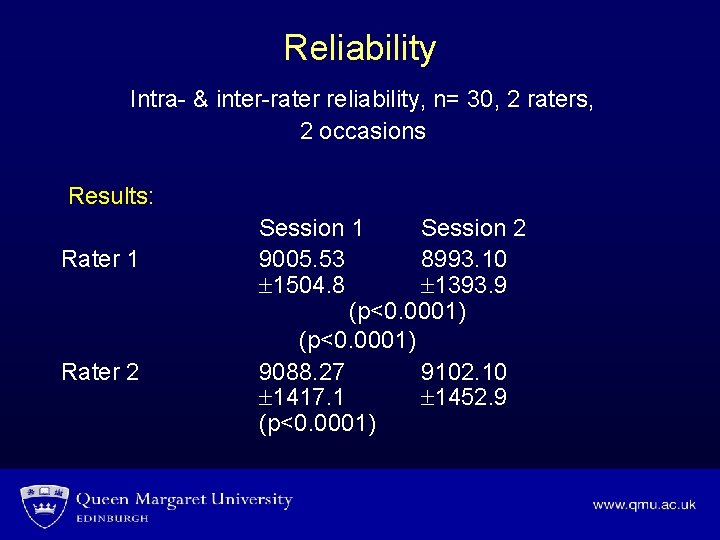
Reliability Intra- & inter-rater reliability, n= 30, 2 raters, 2 occasions Results: Rater 1 Rater 2 Session 1 Session 2 9005. 53 8993. 10 1504. 8 1393. 9 (p<0. 0001) 9088. 27 9102. 10 1417. 1 1452. 9 (p<0. 0001)

Phase 3: Use of software • Design: A) reliability study using independent measurement of length B) use of single limb length measures on 2 occasions • Issue: Software allows limb measurement length to change in two screens • Results: Variability A): n=30 B): n=10 Rater 1 = 20% Rater 2 = 16. 3% Rater 1= 3. 8%, Rater 2 = 5. 3%
Conclusions Protocol reliable if: 1. 10 min rest period before testing with elevated leg 2. Neutral axial rotation of limb 3. Foot placed in centre of base plate 4. Constant slow speed is maintained 5. Only 1 limb length measurement is taken and used on repeat visits
Clinical implications • Use of a standardised protocol will allow reliable data to be collected on repeated basis, • Monitor efficacy of management of patients with changing limb volume.

Queen Margaret University Thank You
Acknowledgements • MSc pre registration Physiotherapy students: 2007 Francis Burgin Áine O’Connor 2006 Nicola Dinsmore Georgina Enderson Mary. Anne Geraghty
- Slides: 19