Peritonsillar Abscess Celina Martinez MSIII April 25 2006
Peritonsillar Abscess Celina Martinez, MSIII April 25, 2006
Clinical Presentation of A. E. • 47 y. o. AAF c/o “sore throat” and difficulty swallowing for 4 days • PMH – None • Meds – None • SH – Current cigarette use with 20 pack-year history – Moderate Et. OH use, current heroin use • ROS – + fever, throat pain, cough, wheezing, dysphagia – Throat pain is 7/10
Physical Exam VS: 137/86 HR 103 T 100. 8 98 -100% RA HEENT: – + lymphadenopathy bilaterally – Unable to visualize oropharynx, patient cannot fully open mouth Repeat exam of oropharynx – L tonsil swollen, with exudate – Uvula midline
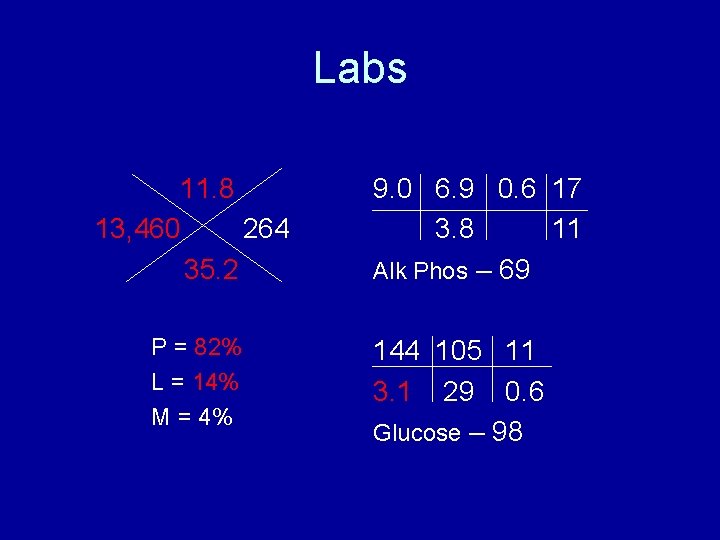
Labs 11. 8 13, 460 264 35. 2 P = 82% L = 14% M = 4% 9. 0 6. 9 0. 6 17 3. 8 11 Alk Phos – 69 144 105 11 3. 1 29 0. 6 Glucose – 98
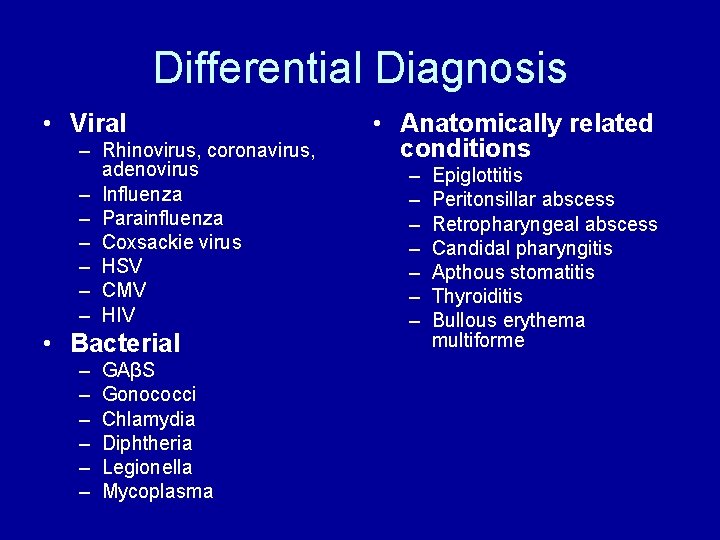
Differential Diagnosis • Viral – Rhinovirus, coronavirus, adenovirus – Influenza – Parainfluenza – Coxsackie virus – HSV – CMV – HIV • Bacterial – – – GAβS Gonococci Chlamydia Diphtheria Legionella Mycoplasma • Anatomically related conditions – – – – Epiglottitis Peritonsillar abscess Retropharyngeal abscess Candidal pharyngitis Apthous stomatitis Thyroiditis Bullous erythema multiforme

Imaging • Neck CT with Contrast – L tonsillar enlargement with 2 rim-enhancing peritonsillar hypodensities – Oropharyngeal narrowing at level of tonsillar enlargement – Swelling of adjacent soft palate with hypodensity compatible with fluid that crosses the midline • Impression – Enlargement of the left palatine tonsil with cystic/necrotic change and marked swelling of adjacent structures
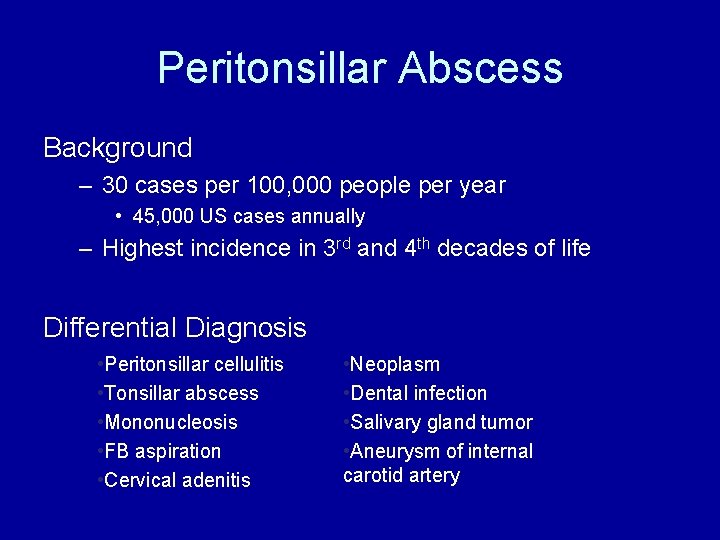
Peritonsillar Abscess Background – 30 cases per 100, 000 people per year • 45, 000 US cases annually – Highest incidence in 3 rd and 4 th decades of life Differential Diagnosis • Peritonsillar cellulitis • Tonsillar abscess • Mononucleosis • FB aspiration • Cervical adenitis • Neoplasm • Dental infection • Salivary gland tumor • Aneurysm of internal carotid artery

Peritonsillar Abscess Pathophysiology - Progression of tonsillitis Tonsillitis Peritonsilar Inflammation Abscess • Inflammation of supratonsillar soft palate and surrounding muscle • Pus collects between fibrous capsule and superior constrictor muscle of the pharynx – Common infectious agents • Common aerobes – Streptococcus pyogenes in 30% – H. influenzae, S. aureus, neisseria species • Common anaerobes – Fusobacterium, peptostreptococcus, prevotella, bacteroides
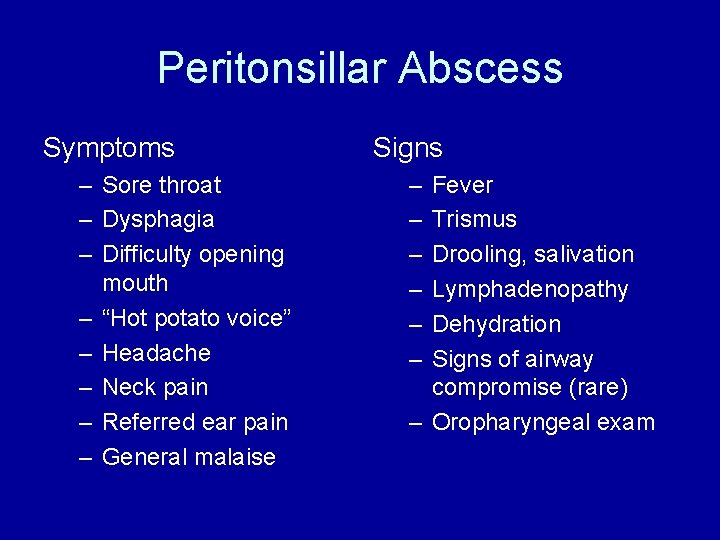
Peritonsillar Abscess Symptoms – Sore throat – Dysphagia – Difficulty opening mouth – “Hot potato voice” – Headache – Neck pain – Referred ear pain – General malaise Signs – – – Fever Trismus Drooling, salivation Lymphadenopathy Dehydration Signs of airway compromise (rare) – Oropharyngeal exam
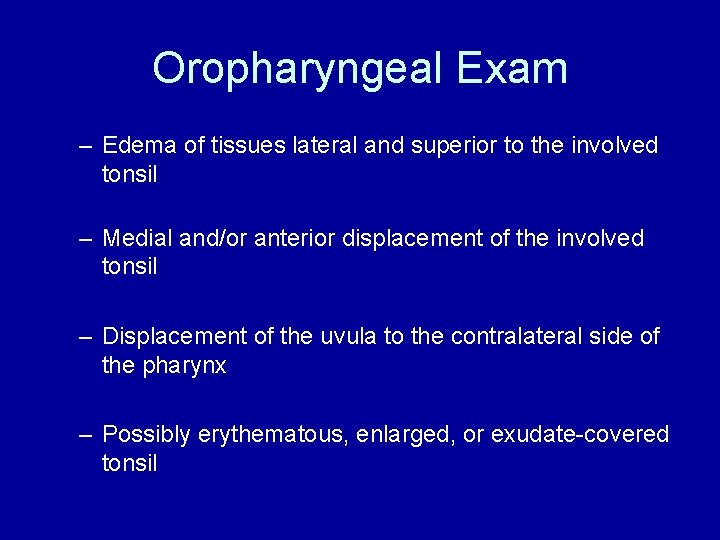
Oropharyngeal Exam – Edema of tissues lateral and superior to the involved tonsil – Medial and/or anterior displacement of the involved tonsil – Displacement of the uvula to the contralateral side of the pharynx – Possibly erythematous, enlarged, or exudate-covered tonsil
Peritonsillar Abscess Diagnosis is usually clinical! Other Tests – Intraoral ultrasound • Rule out retropharyngeal abscess and peritonsillar cellulitis – CT scan • Trismus, suspicion of invasion into deep neck tissue
Peritonsillar Abscess Treatment – IV hydration – IV steroids – IV pain control – Antibiotics • Penicillin V 500 mg TID for 10 -14 days • Metronidazole 500 mg BID for 10 -14 days OR • Clindamycin 300 mg QID for 10 days
Peritonsillar Abscess Treatment – Needle aspiration • Anesthetic spray, 2 -4 cc of lidocaine w/epi • 19 -gauge needle; keep proximal half covered w/cap • Point needle medially, keep medial to molars to avoid vessels! • Needle can be inserted 1 -2 cm safely • Culture aspirate and gram stain aspirate
Peritonsillar Abscess • When to defer to otolaryngology – Marked trismus – Unsuccessful aspiration – Deep neck invasion
Current Literature • Losanoff JE, Missavage AE. Neglected peritonsillar abscess resulting in necrotizing soft tissue infection of the neck and chest wall. Int J Clin Pract. 2005 Dec; 59(12): 1476 -8. – NSTI from peritonsillar abscess is rapidly spreading and life threatening. – High index of suspicion, early diagnosis, broadspectrum antibiotics and aggressive surgical management are essential. • Fasano CJ, Chudnofsky C, Vanderbeek P. Bilateral peritonsillar abscesses: not your usual sore throat. Emerg Med. 2005 Jul; 29(1): 45 -7. – Bilateral tonsil swelling, midline uvula
References • • Johnson RF, Stewart MG. The contemporary approach to diagnosis and management of peritonsillar abscess. Curr Opin Otolaryngol Head Neck Surg. 2005 Jun; 13(3): 157 -60. Thomas GR, et al. Managing Common Otolaryngologic Emergencies. Emerg Med 37(5): 18 -47, 2005. Bisno AL. Acute Pharyngitis. N Engl J Med. 2001 Jan 18; 344(3): 205 -11 Steyer TE. Peritonsillar Abscess: Diagnosis and Treatment. Am Fam Physician. 2002 Jan 1; 65(1): 93 -6.
- Slides: 16