Peritoneal Dialysis Adequacy Prescription Management Peritoneal Dialysis Background
Peritoneal Dialysis Adequacy & Prescription Management
Peritoneal Dialysis Background • Target small solute clearances have been based upon assumptions that peritoneal and renal clearances are added together • Renal small solute clearances are directly correlated with patient survival • There have been no randomized, controlled interventional trials examining the role of increases in peritoneal small solute clearances on patient survival
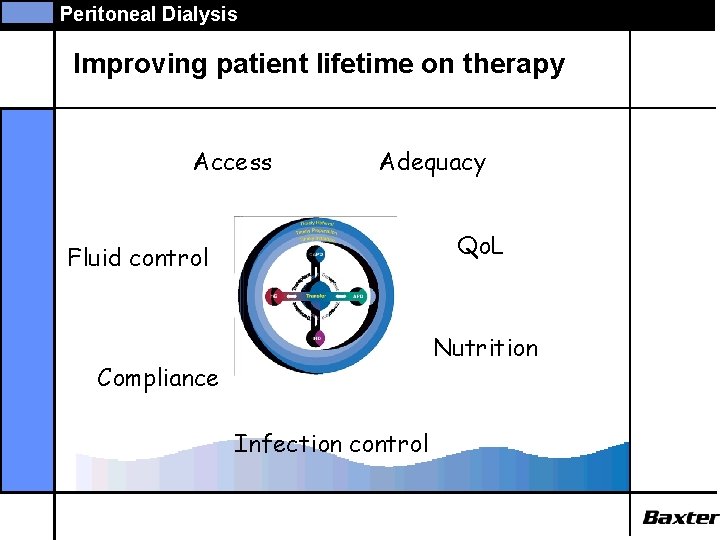
Peritoneal Dialysis Improving patient lifetime on therapy Access Adequacy Qo. L Fluid control Nutrition Compliance Infection control
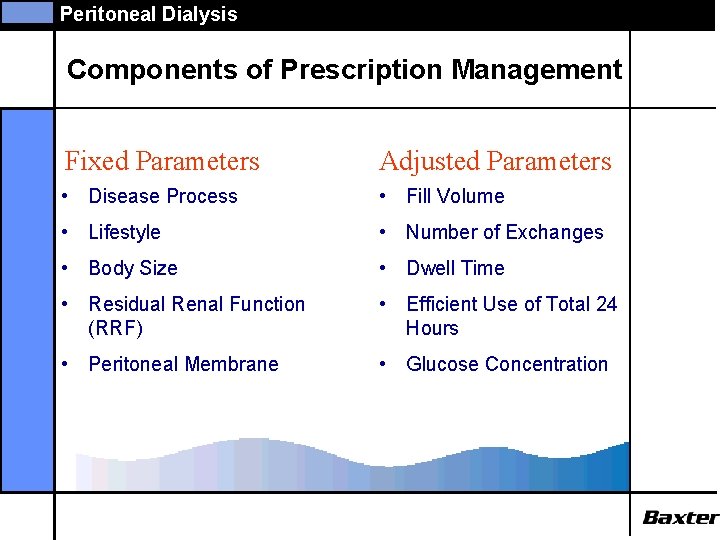
Peritoneal Dialysis Components of Prescription Management Fixed Parameters Adjusted Parameters • Disease Process • Fill Volume • Lifestyle • Number of Exchanges • Body Size • Dwell Time • Residual Renal Function (RRF) • Efficient Use of Total 24 Hours • Peritoneal Membrane • Glucose Concentration
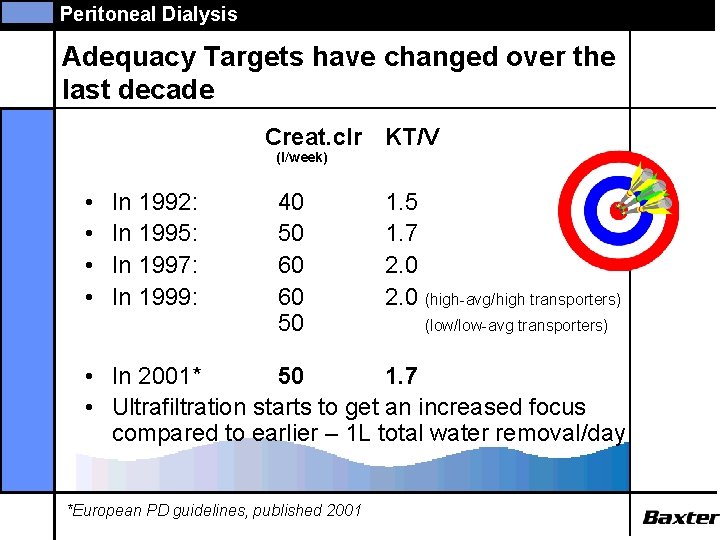
Peritoneal Dialysis Adequacy Targets have changed over the last decade Creat. clr KT/V (l/week) • • In 1992: In 1995: In 1997: In 1999: 40 50 60 60 50 1. 5 1. 7 2. 0 (high-avg/high transporters) (low/low-avg transporters) • In 2001* 50 1. 7 • Ultrafiltration starts to get an increased focus compared to earlier – 1 L total water removal/day *European PD guidelines, published 2001
Peritoneal Dialysis What is Clearance? • Clearance is the total amount of body fluid completely cleared of a solute during a certain time • ml/min • L/week • Ex: Creatinine clearance = 50 l/week means: 50 L of body fluid is totally cleared for creatinine during a week
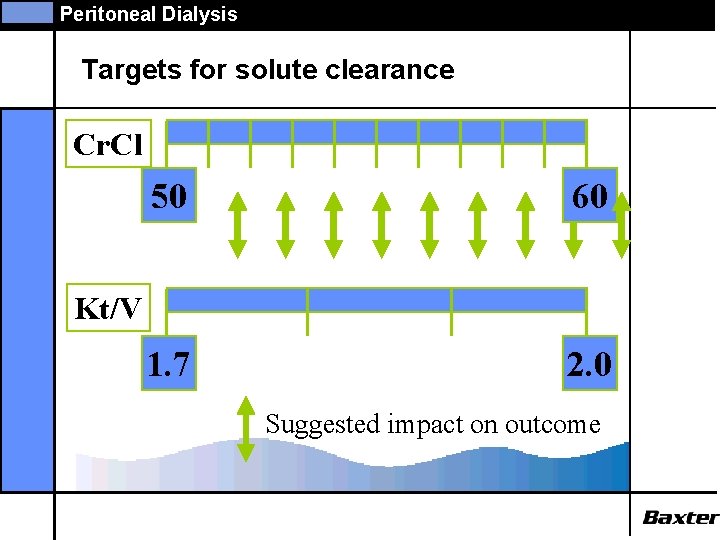
Peritoneal Dialysis Targets for solute clearance Cr. Cl 50 60 1. 7 2. 0 Kt/V Suggested impact on outcome
Peritoneal Dialysis The peritoneal equilibration test (PET) • Semiquantitative assessment of peritoneal membrane transport function • Assess rates of solute equilibration between peritoneal capillary blood and dialysate • Uses the ratio of solute concentrations in dialysate and plasma (D/P) at specific times to signify the extent of equilibration • Performed using a standardized method, using standard solutions (2. 27% glucose) Twardowski ZJ, Nolph KD, Khanna R et al Perit Dial Bull 1987; 7: 138.
Peritoneal Dialysis Clinical applications of the PET • • peritoneal membrane transport classification predict dialysis dose choose peritoneal dialysis regime monitor peritoneal membrane function diagnose acute membrane injury diagnose causes of inadequate ultrafiltration diagnose causes of inadequate solute clearance estimate D/P ratio of a solute at a particular time

Peritoneal Dialysis The peritoneal equilibration test (PET) • • • following a standard overnight exchange drain to dryness instill 2. 27% 2000 ml glucose bag roll patient to ensure mixing sample PD fluid at time 0, 2, 4 hours blood test (assume blood concentrations constant) • drain out at 4 hours and measure drain volume
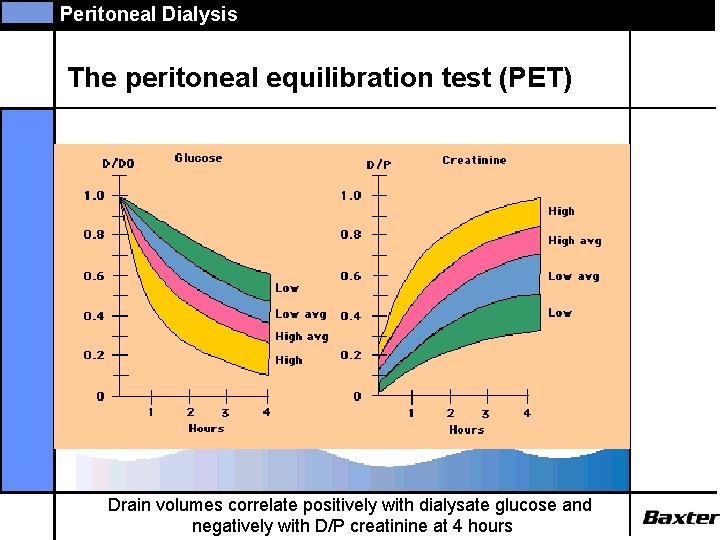
Peritoneal Dialysis The peritoneal equilibration test (PET) Drain volumes correlate positively with dialysate glucose and negatively with D/P creatinine at 4 hours
Peritoneal Dialysis Membrane transport type.
Peritoneal Dialysis Calculation of Peritoneal Urea Clearance
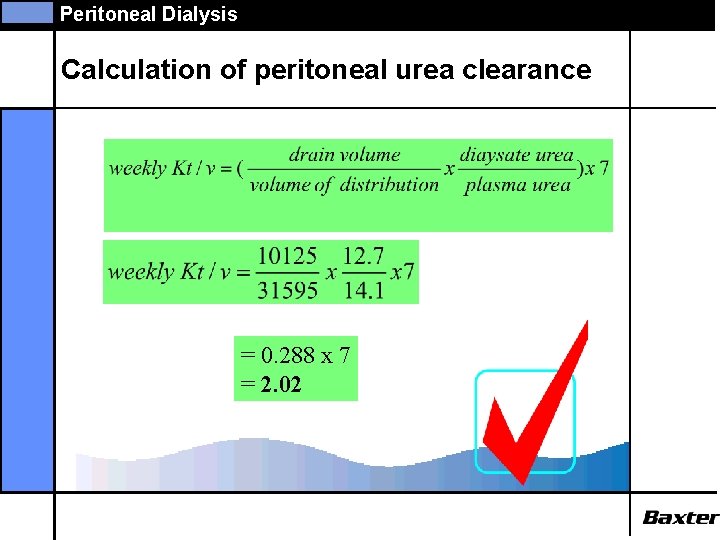
Peritoneal Dialysis Calculation of peritoneal urea clearance = 0. 288 x 7 = 2. 02
Peritoneal Dialysis Calculation of Peritoneal Creat. Clearance
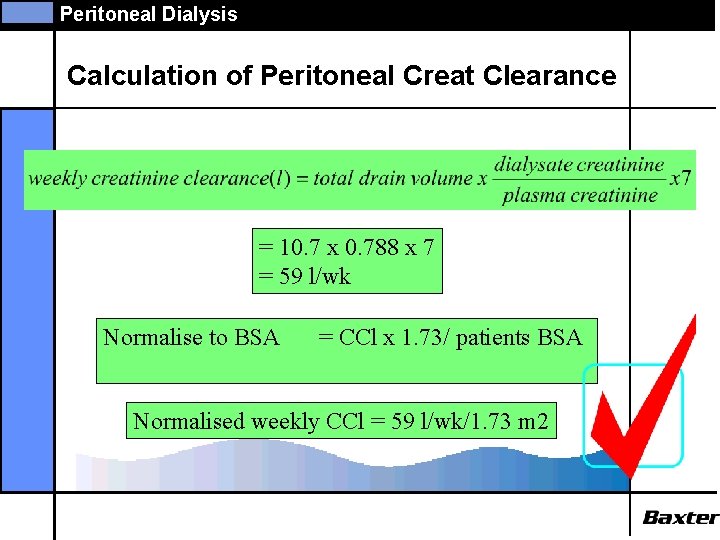
Peritoneal Dialysis Calculation of Peritoneal Creat Clearance = 10. 7 x 0. 788 x 7 = 59 l/wk Normalise to BSA = CCl x 1. 73/ patients BSA Normalised weekly CCl = 59 l/wk/1. 73 m 2
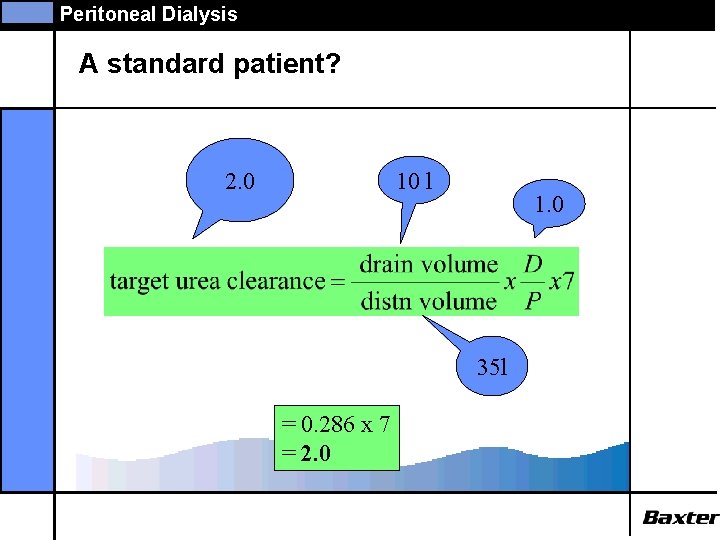
Peritoneal Dialysis A standard patient? 10 l 2. 0 1. 0 35 l = 0. 286 x 7 = 2. 0
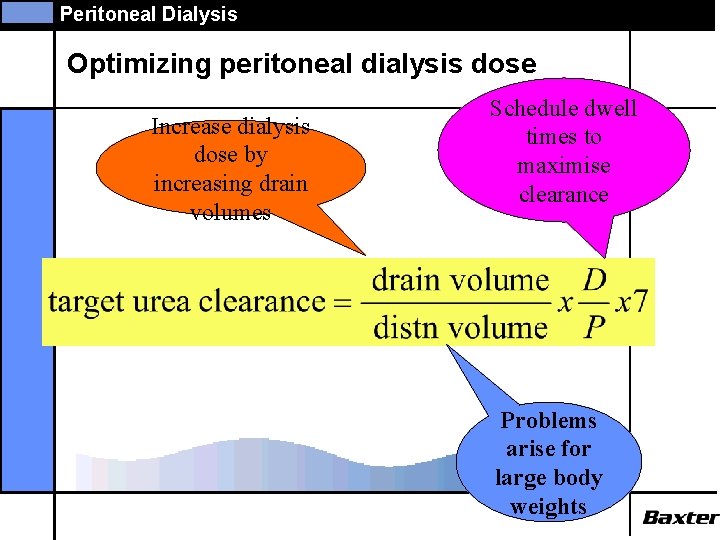
Peritoneal Dialysis Optimizing peritoneal dialysis dose Increase dialysis dose by increasing drain volumes Schedule dwell times to maximise clearance Problems arise for large body weights
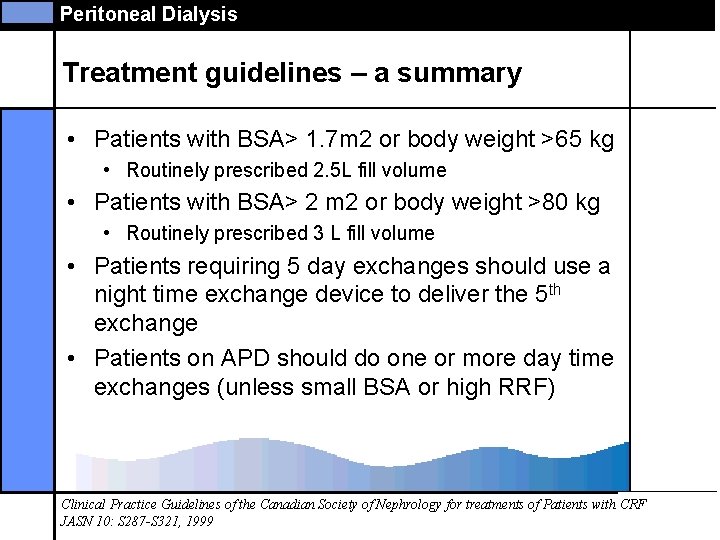
Peritoneal Dialysis Treatment guidelines – a summary • Patients with BSA> 1. 7 m 2 or body weight >65 kg • Routinely prescribed 2. 5 L fill volume • Patients with BSA> 2 m 2 or body weight >80 kg • Routinely prescribed 3 L fill volume • Patients requiring 5 day exchanges should use a night time exchange device to deliver the 5 th exchange • Patients on APD should do one or more day time exchanges (unless small BSA or high RRF) Clinical Practice Guidelines of the Canadian Society of Nephrology for treatments of Patients with CRF JASN 10: S 287 -S 321, 1999
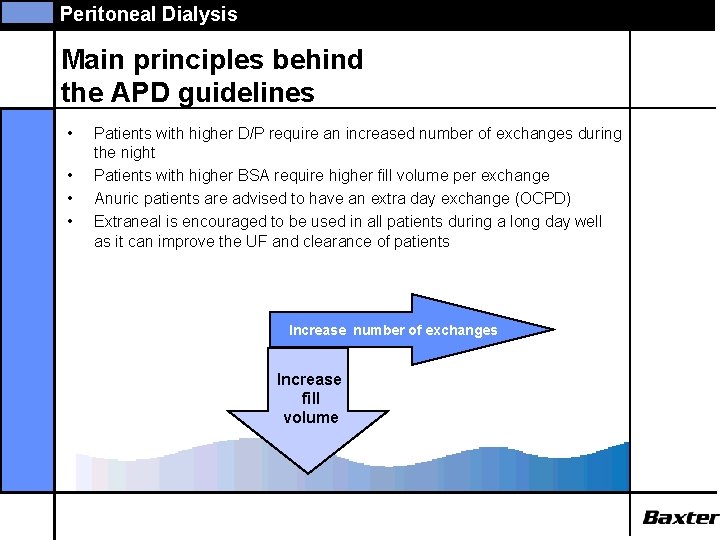
Peritoneal Dialysis Main principles behind the APD guidelines • • Patients with higher D/P require an increased number of exchanges during the night Patients with higher BSA require higher fill volume per exchange Anuric patients are advised to have an extra day exchange (OCPD) Extraneal is encouraged to be used in all patients during a long day well as it can improve the UF and clearance of patients Increase number of exchanges Increase fill volume
Peritoneal Dialysis Overview of guidelines RRF >2 ml/min All prescriptions include 9 hours overnight treatment. If targets are over achieved, reducing therapy time at night can be an option. Monitor with care Varied glucose concentrations and Extraneal® are advised to use in order to meet the required UF of min. 1 L
Peritoneal Dialysis Overview of guidelines RRF <2 ml/min All prescriptions include 9 hours overnight treatment if not otherwise noted Varied glucose concentrations and Extraneal® are advised to use in order to meet the required UF of min. 1 L APD* For these patient groups, APD therapy will probably not reach both KT/V and Creat clr. targets. Monitor with care. Two day time exchanges can be beneficial for motivated patients in order to meet targets.
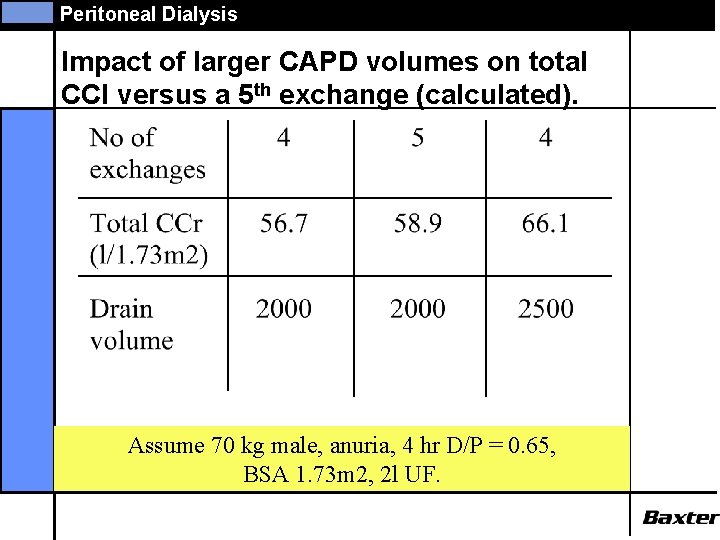
Peritoneal Dialysis Impact of larger CAPD volumes on total CCl versus a 5 th exchange (calculated). Assume 70 kg male, anuria, 4 hr D/P = 0. 65, BSA 1. 73 m 2, 2 l UF.
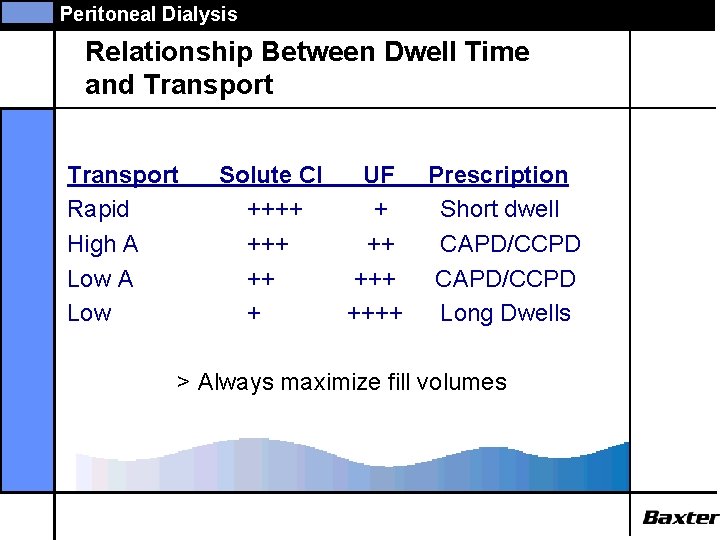
Peritoneal Dialysis Relationship Between Dwell Time and Transport Rapid High A Low Solute Cl UF ++++ + ++++ Prescription Short dwell CAPD/CCPD Long Dwells > Always maximize fill volumes
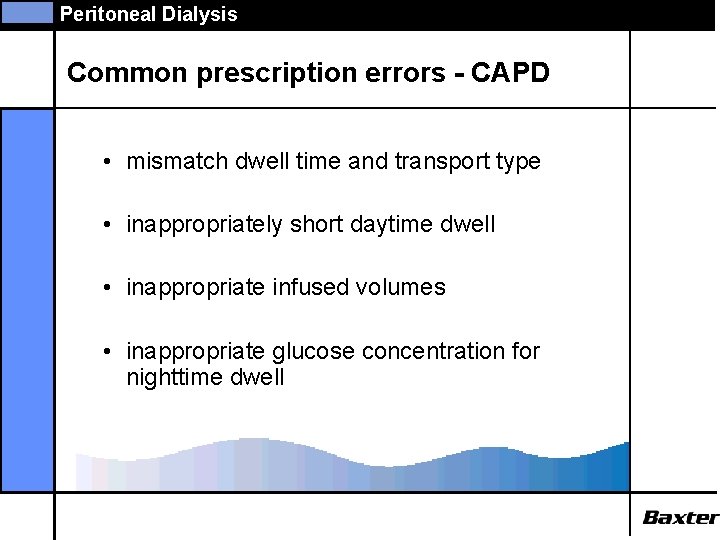
Peritoneal Dialysis Common prescription errors - CAPD • mismatch dwell time and transport type • inappropriately short daytime dwell • inappropriate infused volumes • inappropriate glucose concentration for nighttime dwell
Peritoneal Dialysis Common prescription errors - APD • inappropriate use of a dry day • inappropriately long drain times • failure to increase target dose to account for intermittent therapy • failure to consider a CAPD exchange during the day to increase clearance
Peritoneal Dialysis ADEMEX • ADEMEX (ADEquacy of PD in MEXico) is a randomized, active controlled, prospective trial • Hypothesis tested: increases in peritoneal clearance of small solutes improves the PD patients’ survival • The primary outcome was mortality.
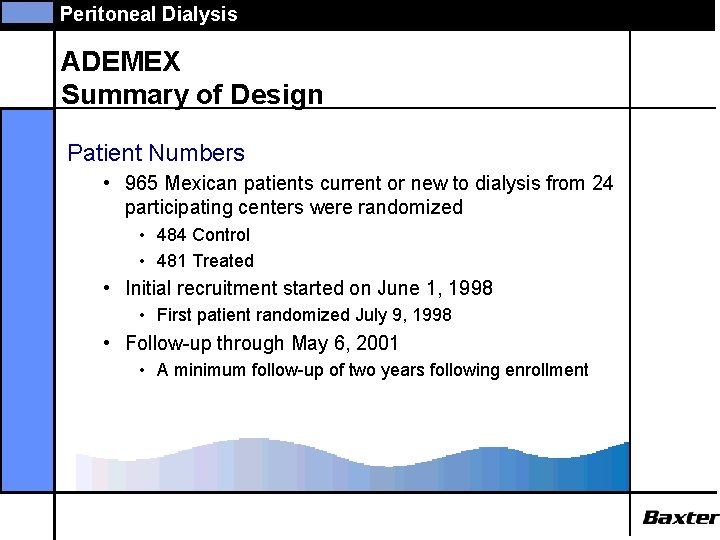
Peritoneal Dialysis ADEMEX Summary of Design Patient Numbers • 965 Mexican patients current or new to dialysis from 24 participating centers were randomized • 484 Control • 481 Treated • Initial recruitment started on June 1, 1998 • First patient randomized July 9, 1998 • Follow-up through May 6, 2001 • A minimum follow-up of two years following enrollment
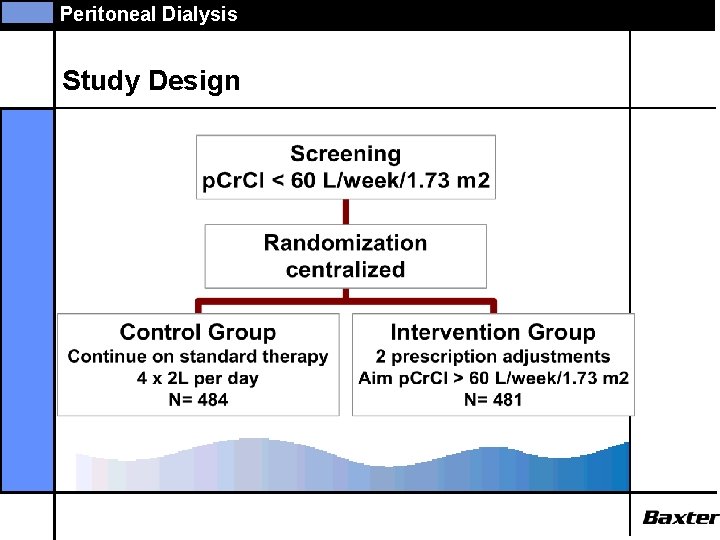
Peritoneal Dialysis Study Design
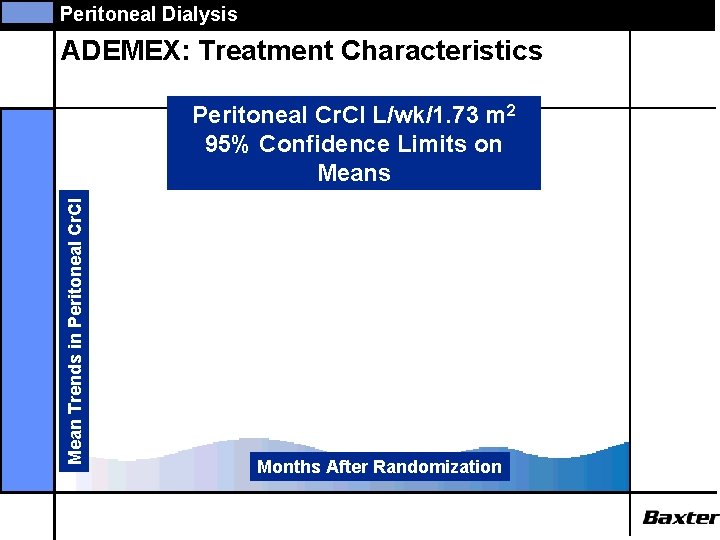
Peritoneal Dialysis ADEMEX: Treatment Characteristics Mean Trends in Peritoneal Cr. Cl L/wk/1. 73 m 2 95% Confidence Limits on Means p<. 001 Months After Randomization
Peritoneal Dialysis ADEMEX: Treatment Characteristics Mean Trends in p. Kt/V Peritoneal Kt/V 95% Confidence Limits on Means p<. 001 Months After Randomization
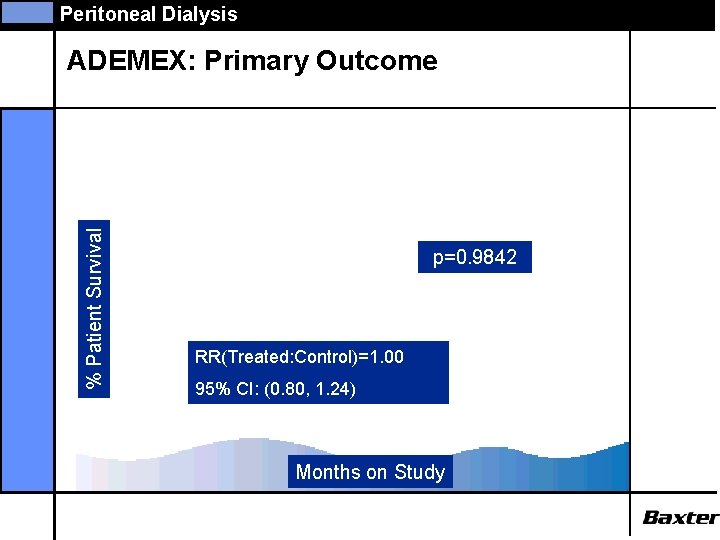
Peritoneal Dialysis % Patient Survival ADEMEX: Primary Outcome p=0. 9842 RR(Treated: Control)=1. 00 95% CI: (0. 80, 1. 24) Months on Study
Peritoneal Dialysis ADEMEX: Conclusions • There was no difference in patient survival with variations in peritoneal small solute clearance within ranges achievable in current clinical practice. • Survival remained similar between the two groups even after adjusting for factors known to be associated with mortality in patients on PD (age, diabetes, albumin, n. PNA, anuria)
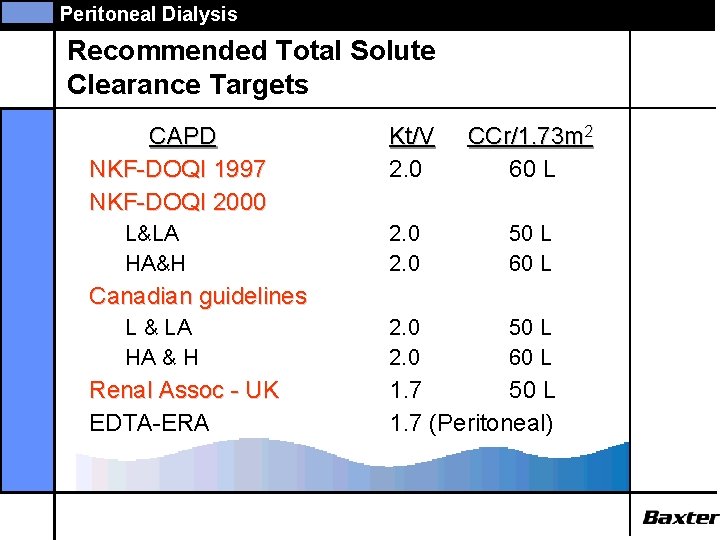
Peritoneal Dialysis Recommended Total Solute Clearance Targets CAPD NKF-DOQI 1997 NKF-DOQI 2000 L&LA HA&H Kt/V 2. 0 CCr/1. 73 m 2 60 L 2. 0 50 L 60 L Canadian guidelines L & LA HA & H Renal Assoc - UK EDTA-ERA 1. 7 50 L 1. 7 (Peritoneal)
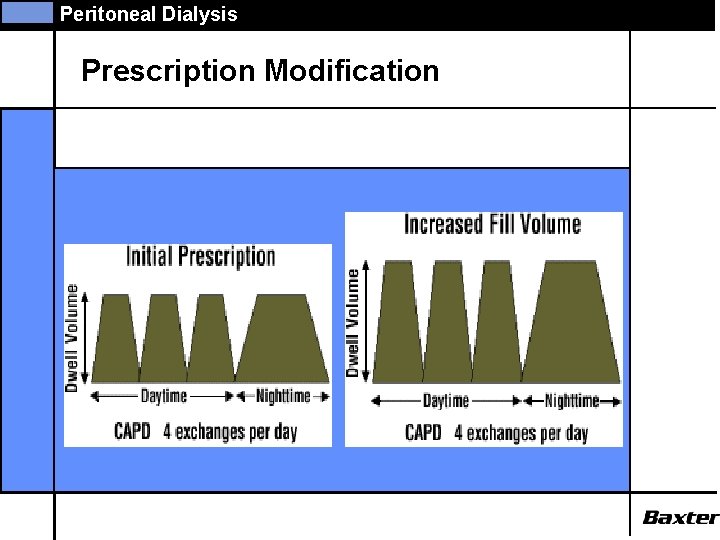
Peritoneal Dialysis Prescription Modification
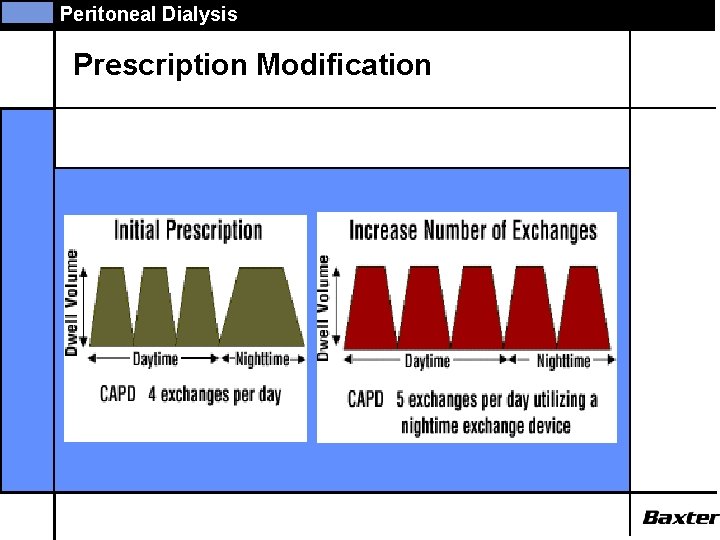
Peritoneal Dialysis Prescription Modification
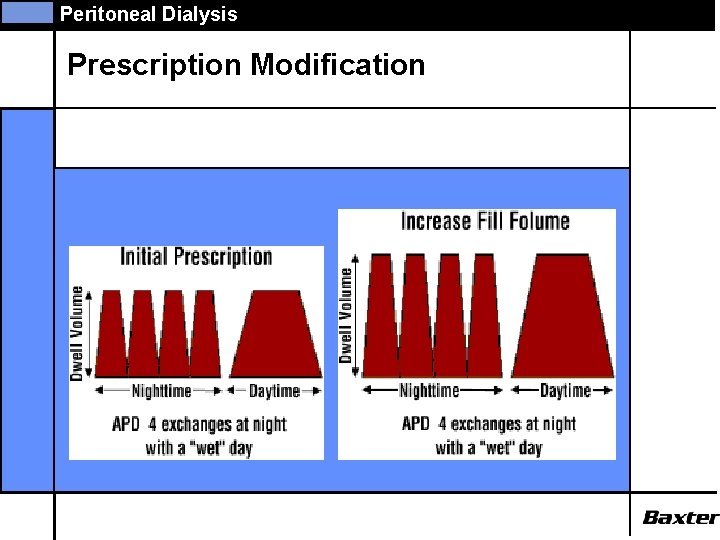
Peritoneal Dialysis Prescription Modification
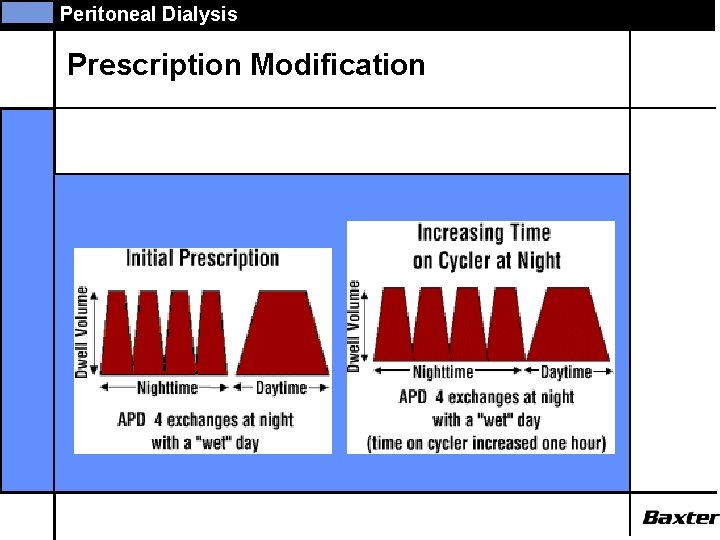
Peritoneal Dialysis Prescription Modification
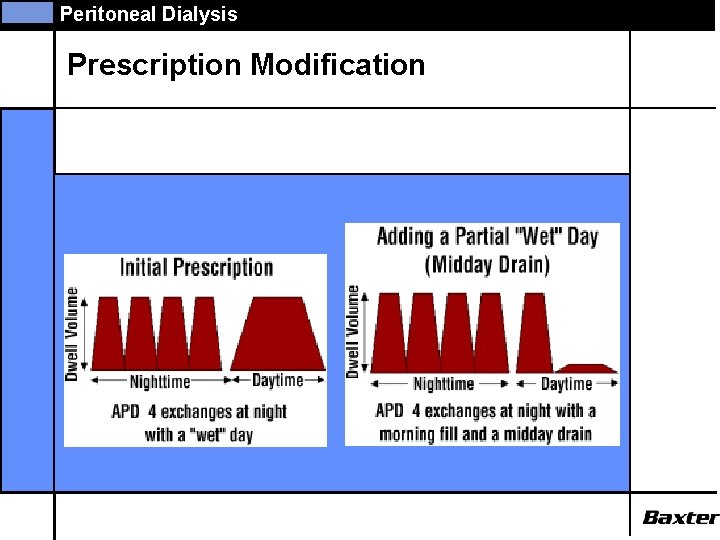
Peritoneal Dialysis Prescription Modification
Peritoneal Dialysis APD - Increasing Clearance • Increase fill volumes • Add a daytime exchange • Increase Time on Cycler • Increase Number of Nighttime Exchanges
Peritoneal Dialysis APD - Increasing Clearance • Increase fill volumes • • Effective means of improving clearance Minimum impact on patient lifestyle Adjust nighttime exchanges first Use 2. 0 L or greater whenever possible • Add a daytime exchange • Increase Time on Cycler • Increase Number of Nighttime Exchanges
Peritoneal Dialysis APD - Increasing Clearance • Increase fill volumes • Add a daytime exchange • This is a very effective means of improving clearance • Home. Choice can be programmed to deliver the midday exchange • Increase Time on Cycler • Increase Number of Nighttime Exchanges
Peritoneal Dialysis APD - Increasing Clearance • Increase fill volumes • Add a daytime exchange • Increase Time on Cycler • Cycler time can be extended to 10 hours • Increasing cycler time with a constant number of exchanges increases dwell time which increases clearance • Increase Number of Nighttime Exchanges
Peritoneal Dialysis APD - Increasing Clearance • • Increase fill volumes Add a daytime exchange Increase Time on Cycler Increase Number of Nighttime Exchanges • May increase clearance, but only if time on cycler is also increased
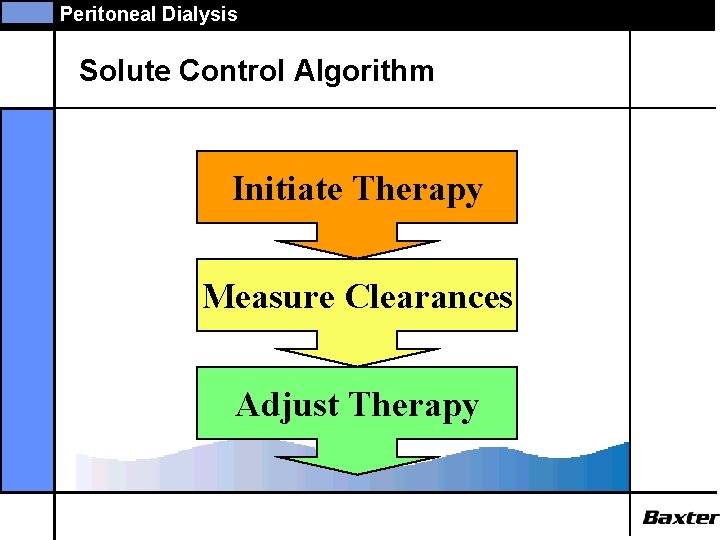
Peritoneal Dialysis Solute Control Algorithm Initiate Therapy Measure Clearances Adjust Therapy
Peritoneal Dialysis Monitoring frequency • KT/V and Creat. clr: • Within 6 -8 weeks after commencing dialysis • Every subsequent 6 month • If patients clinical status changes unexpectedly, or if prescription is altered, take supplemental clearance measurements • PET • Within 6 weeks of initiating PD • Repeat if unexpected changes in peritoneal UF occur Clinical Practice Guidelines of the Canadian Society of Nephrology for treatments of Patients with CRF JASN 10: S 287 -S 321, 1999
Peritoneal Dialysis Making monitoring of adequacy easier Using a software program makes monitoring easier: • Automated calculations of creat clearance, KT/V, n. PNA • Reporting function gives easy overview of one patient or whole patient population • Easy to identify problem patients where actions might be needed • Track and document improvements over time
Peritoneal Dialysis Auditing clinical outcomes in PD • Monitor patient and technique survival in all large programs • Monitor % of patients in all PD programs who fail to achieve targets • Record % of patients in all PD programs with inadequate n. PNA values and severe hypoalbuminemia • A good program will have 80 -85% of patients achieving adequacy targets • Review the proportions of patients exceeding targets every 3 -6 months Clinical Practice Guidelines of the Canadian Society of Nephrology for treatments of Patients with CRF JASN 10: S 287 -S 321, 1999
Peritoneal Dialysis Conclusion. • There is uncertainty about the target clearance in PD • Patient management in peritoneal dialysis involves much more than small solute clearance – of particular importance are for example residual renal function and ultrafiltration volume, as well as the other complex of factors central to holistic management of renal failure patients.
- Slides: 49