PERISTOMAL HERNIA THE CASE FOR EXTRAPERITONEAL COLOSTOMY Garnet



- Slides: 25
PERISTOMAL HERNIA: THE CASE FOR EXTRAPERITONEAL COLOSTOMY Garnet Blatchford, M. D.

I have no disclosures to report
EXTRAPERITONEAL COLOSTOMY OLD CONCEPT, BUT FORGOTTEN? Principles and Practice of Surgery for the Colon, Rectum and Anus, Gordon/Nivatvongs – role of extraperitoneal colostomy uncertain Complications of Colon & Rectal Surgery, Hicks/Beck – no mention Colon and Rectal Surgery - Corman – no mention for colostomy, only ileostomy ASCRS textbook-extraperitoneal “extreme” lateral mesenteric closure
FACTORS IN PARACOLOSTOMY HERNIA Poor technique Lateral to rectus Trephine size Fascial fixation Closure of lateral space High intra-abdominal pressure Obesity Constipation Chronic cough Prostate enlargement

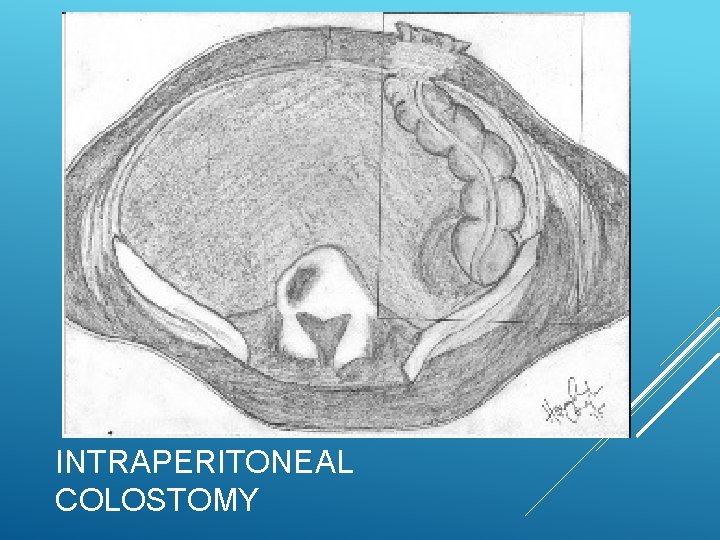
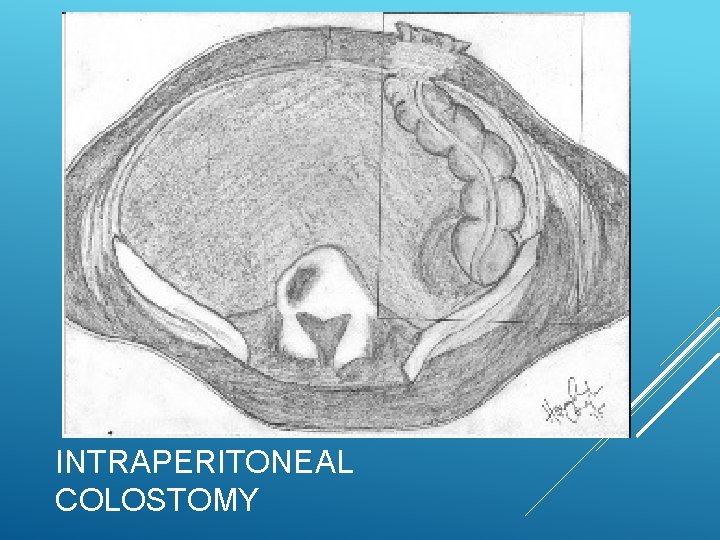
INTRAPERITONEAL COLOSTOMY
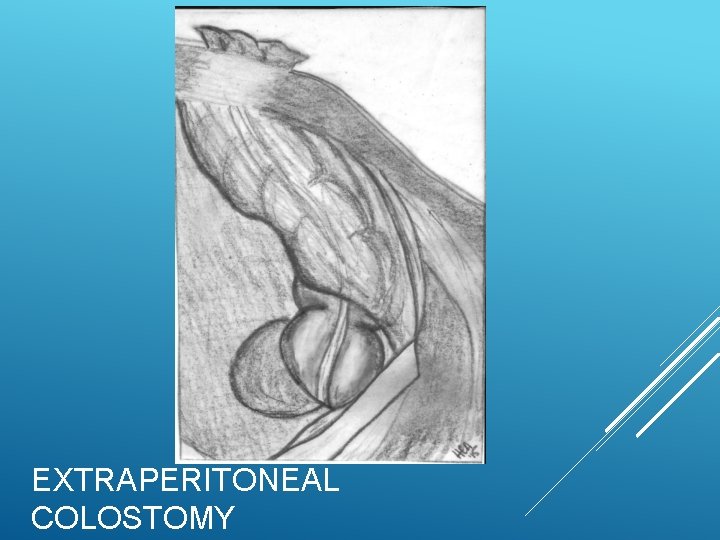
EXTRAPERITONEAL COLOSTOMY
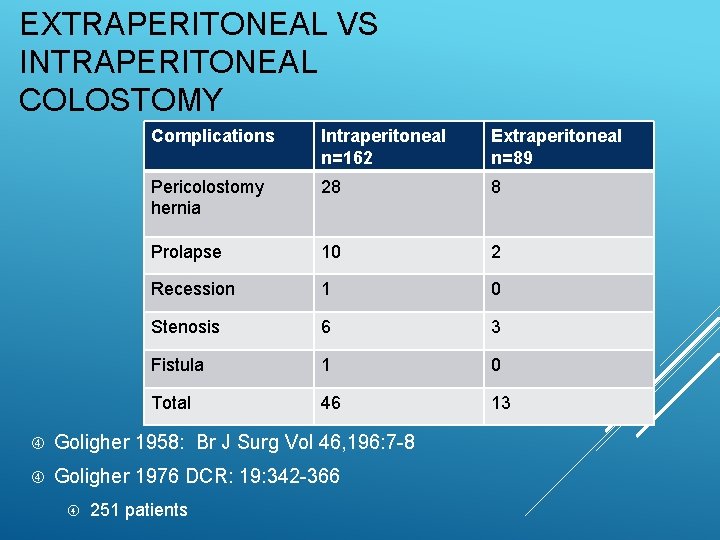
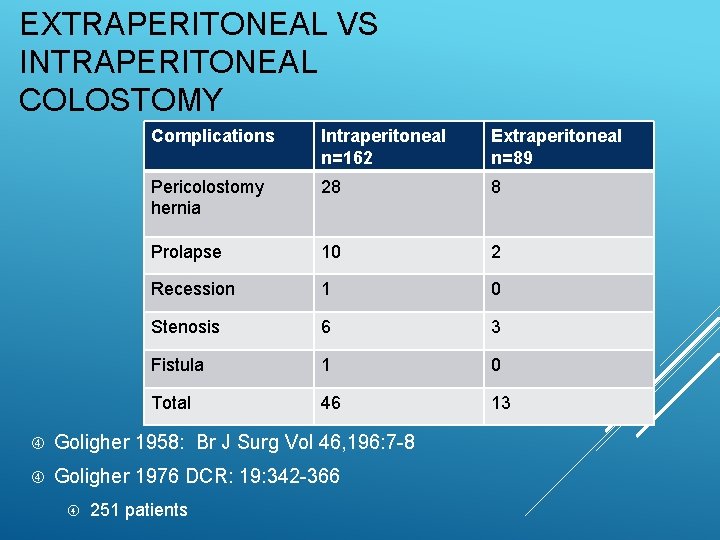
EXTRAPERITONEAL VS INTRAPERITONEAL COLOSTOMY Complications Intraperitoneal n=162 Extraperitoneal n=89 Pericolostomy hernia 28 8 Prolapse 10 2 Recession 1 0 Stenosis 6 3 Fistula 1 0 Total 46 13 Goligher 1958: Br J Surg Vol 46, 196: 7 -8 Goligher 1976 DCR: 19: 342 -366 251 patients
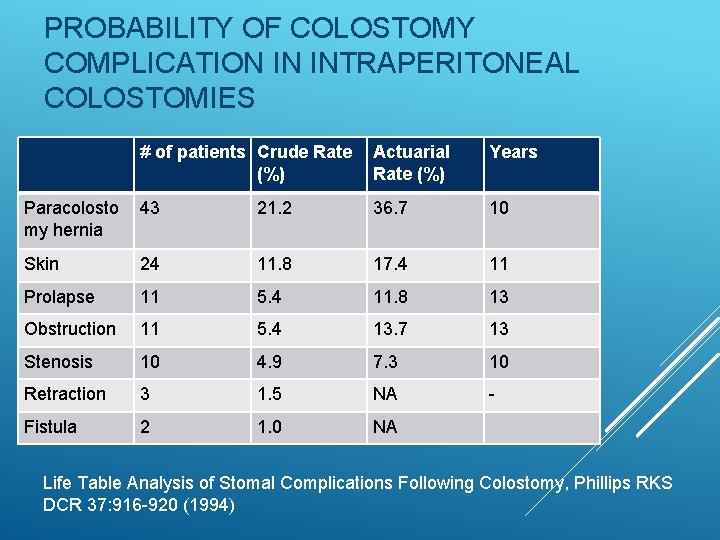
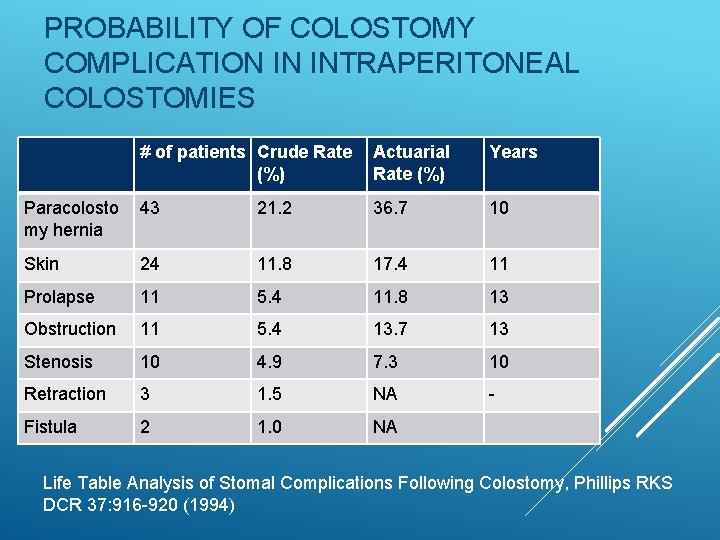
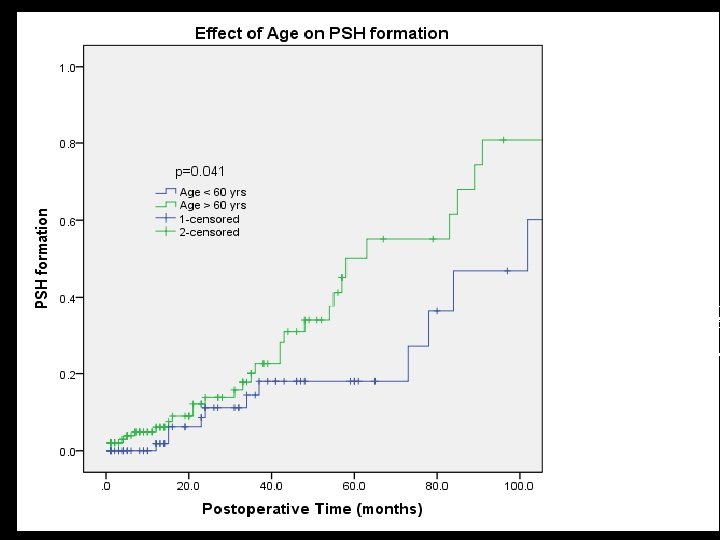
PROBABILITY OF COLOSTOMY COMPLICATION IN INTRAPERITONEAL COLOSTOMIES # of patients Crude Rate (%) Actuarial Rate (%) Years Paracolosto my hernia 43 21. 2 36. 7 10 Skin 24 11. 8 17. 4 11 Prolapse 11 5. 4 11. 8 13 Obstruction 11 5. 4 13. 7 13 Stenosis 10 4. 9 7. 3 10 Retraction 3 1. 5 NA - Fistula 2 1. 0 NA Life Table Analysis of Stomal Complications Following Colostomy, Phillips RKS DCR 37: 916 -920 (1994)
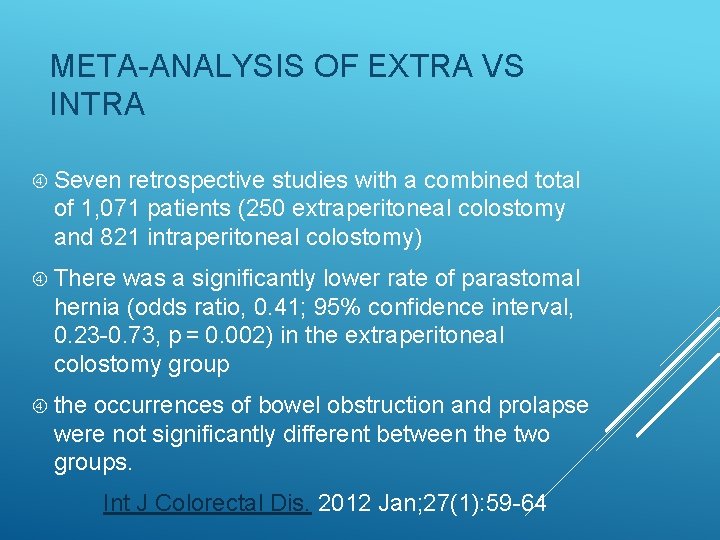
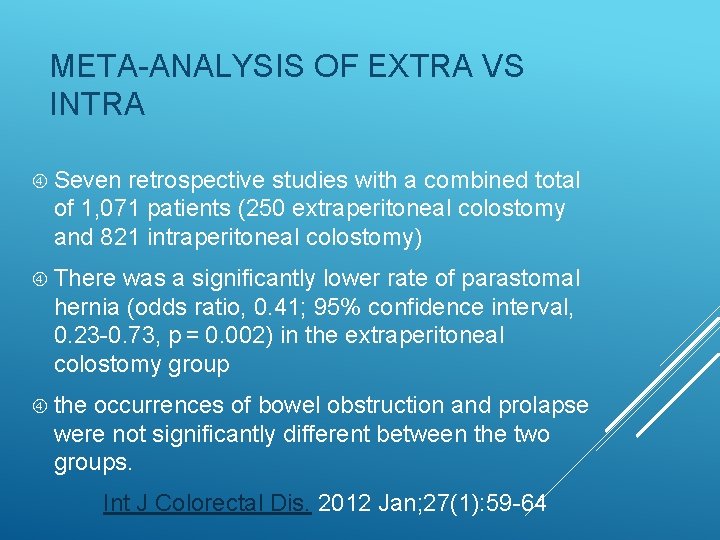
META-ANALYSIS OF EXTRA VS INTRA Seven retrospective studies with a combined total of 1, 071 patients (250 extraperitoneal colostomy and 821 intraperitoneal colostomy) There was a significantly lower rate of parastomal hernia (odds ratio, 0. 41; 95% confidence interval, 0. 23 -0. 73, p = 0. 002) in the extraperitoneal colostomy group the occurrences of bowel obstruction and prolapse were not significantly different between the two groups. Int J Colorectal Dis. 2012 Jan; 27(1): 59 -64
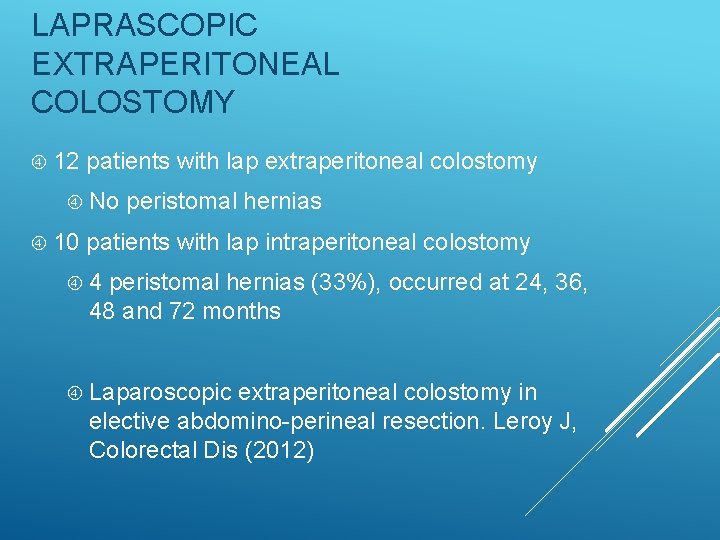
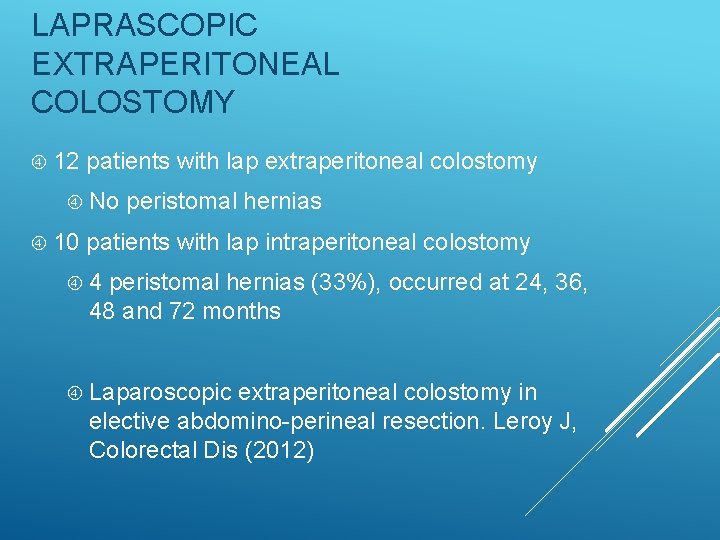
LAPRASCOPIC EXTRAPERITONEAL COLOSTOMY 12 patients with lap extraperitoneal colostomy No 10 peristomal hernias patients with lap intraperitoneal colostomy 4 peristomal hernias (33%), occurred at 24, 36, 48 and 72 months Laparoscopic extraperitoneal colostomy in elective abdomino-perineal resection. Leroy J, Colorectal Dis (2012)
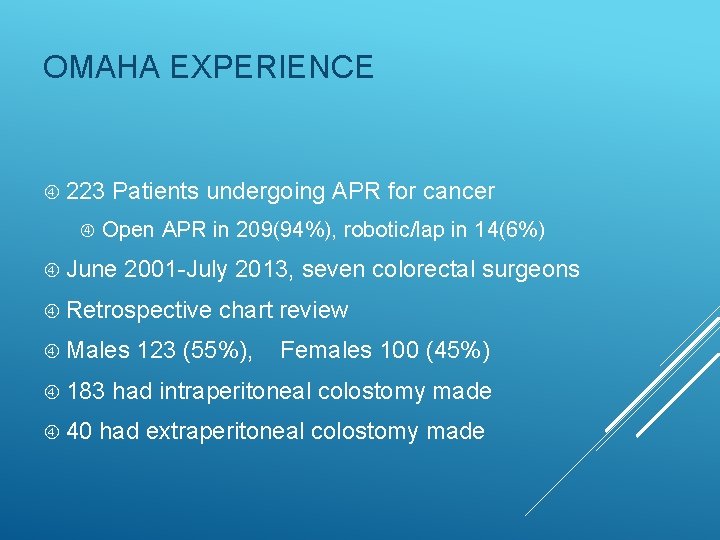
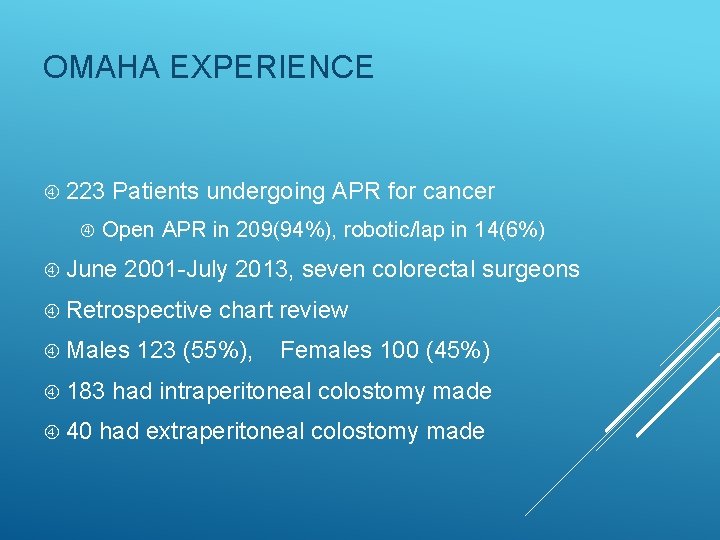
OMAHA EXPERIENCE 223 Patients undergoing APR for cancer Open APR in 209(94%), robotic/lap in 14(6%) June 2001 -July 2013, seven colorectal surgeons Retrospective Males 183 40 chart review 123 (55%), Females 100 (45%) had intraperitoneal colostomy made had extraperitoneal colostomy made
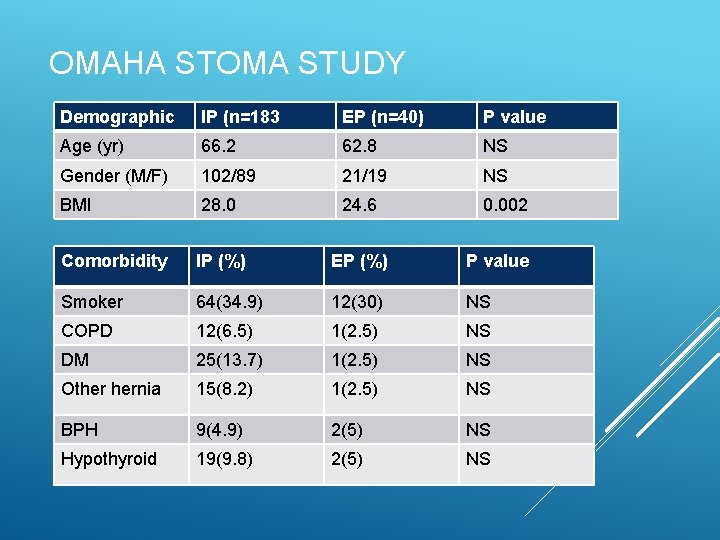
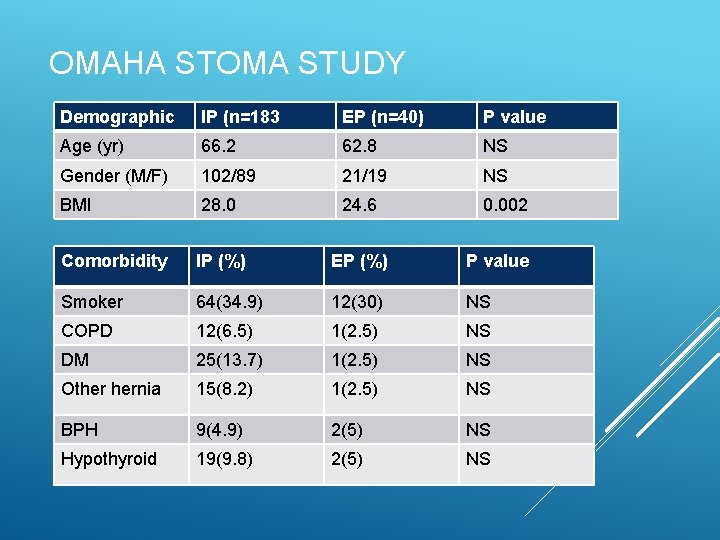
OMAHA STOMA STUDY Demographic IP (n=183 EP (n=40) P value Age (yr) 66. 2 62. 8 NS Gender (M/F) 102/89 21/19 NS BMI 28. 0 24. 6 0. 002 Comorbidity IP (%) EP (%) P value Smoker 64(34. 9) 12(30) NS COPD 12(6. 5) 1(2. 5) NS DM 25(13. 7) 1(2. 5) NS Other hernia 15(8. 2) 1(2. 5) NS BPH 9(4. 9) 2(5) NS Hypothyroid 19(9. 8) 2(5) NS
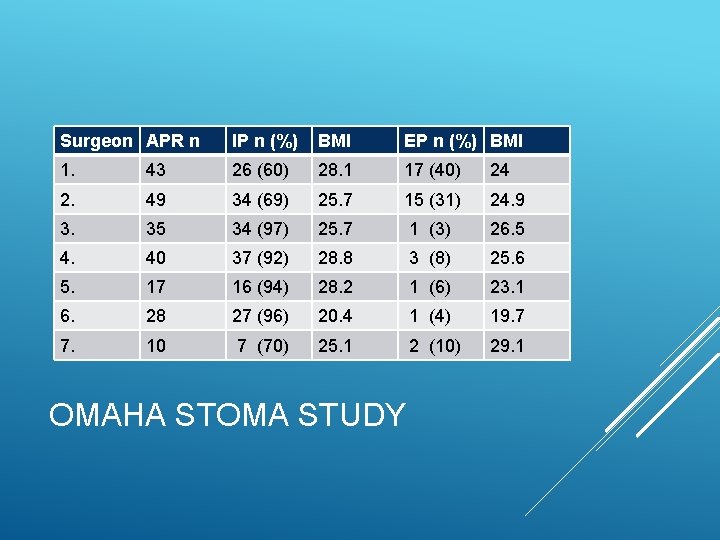
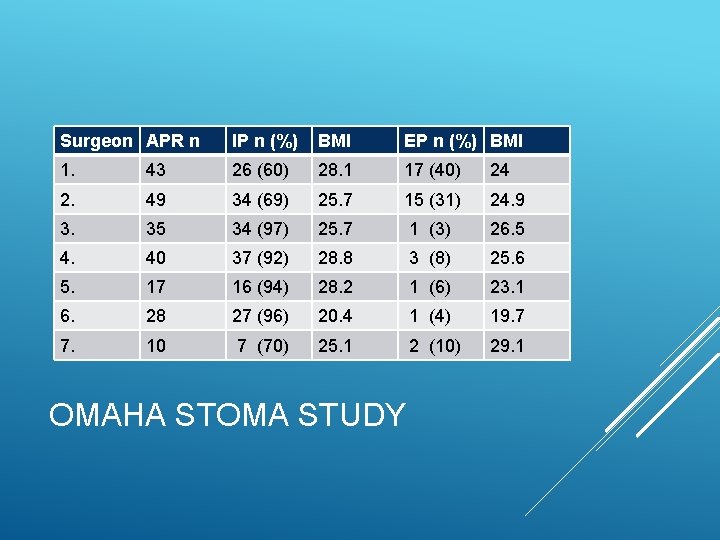
Surgeon APR n IP n (%) BMI EP n (%) BMI 1. 43 26 (60) 28. 1 17 (40) 24 2. 49 34 (69) 25. 7 15 (31) 24. 9 3. 35 34 (97) 25. 7 1 (3) 26. 5 4. 40 37 (92) 28. 8 3 (8) 25. 6 5. 17 16 (94) 28. 2 1 (6) 23. 1 6. 28 27 (96) 20. 4 1 (4) 19. 7 7. 10 7 (70) 25. 1 2 (10) 29. 1 OMAHA STOMA STUDY
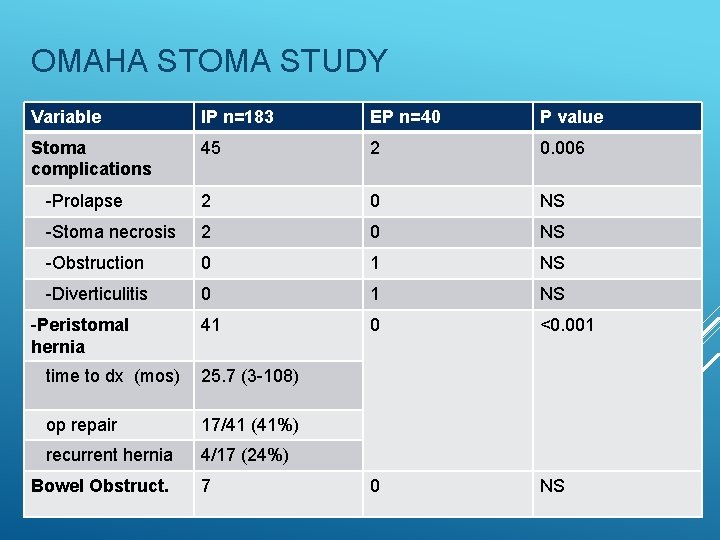
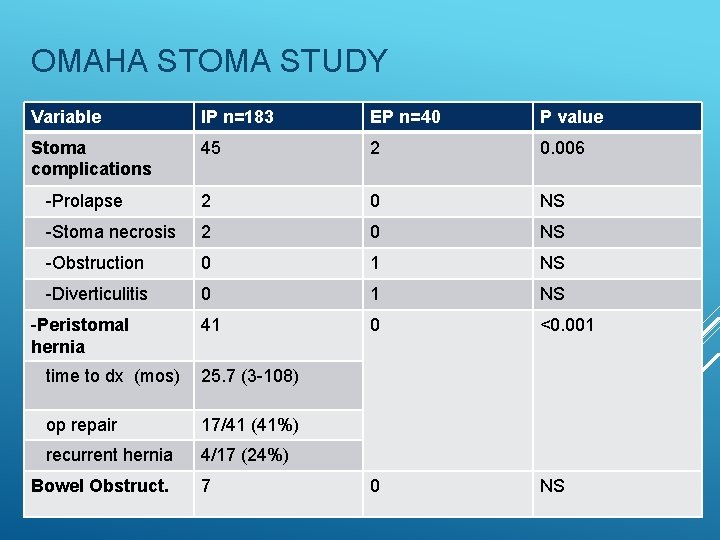
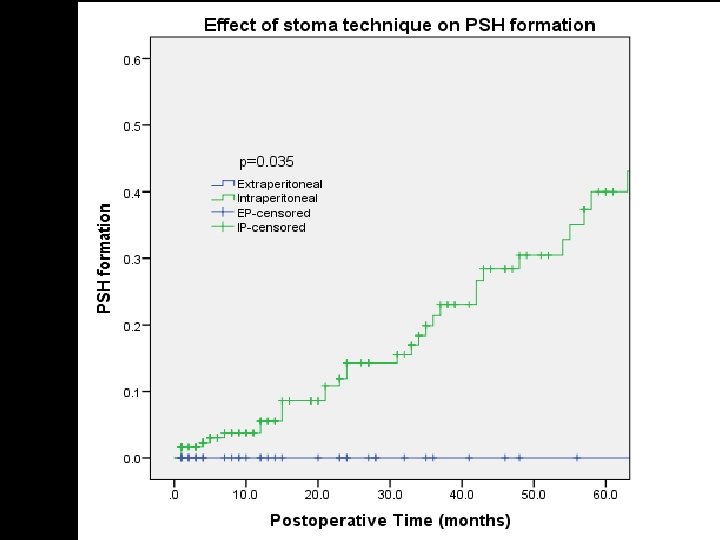
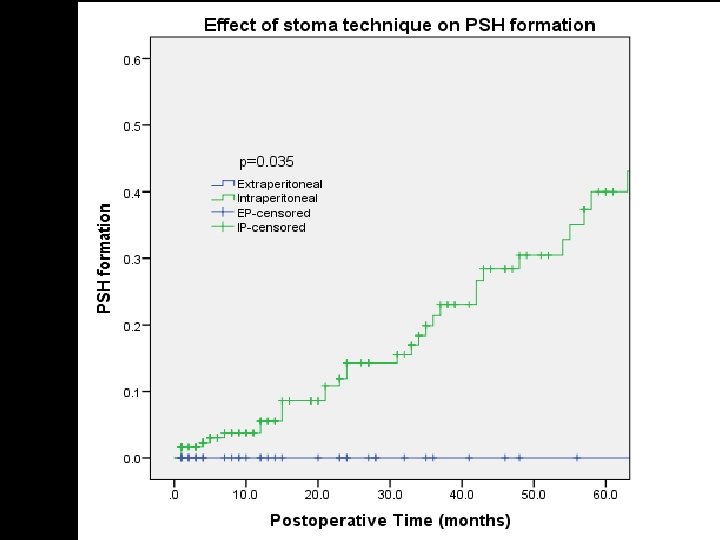
OMAHA STOMA STUDY Variable IP n=183 EP n=40 P value Stoma complications 45 2 0. 006 -Prolapse 2 0 NS -Stoma necrosis 2 0 NS -Obstruction 0 1 NS -Diverticulitis 0 1 NS 41 0 <0. 001 0 NS -Peristomal hernia time to dx (mos) 25. 7 (3 -108) op repair 17/41 (41%) recurrent hernia 4/17 (24%) Bowel Obstruct. 7
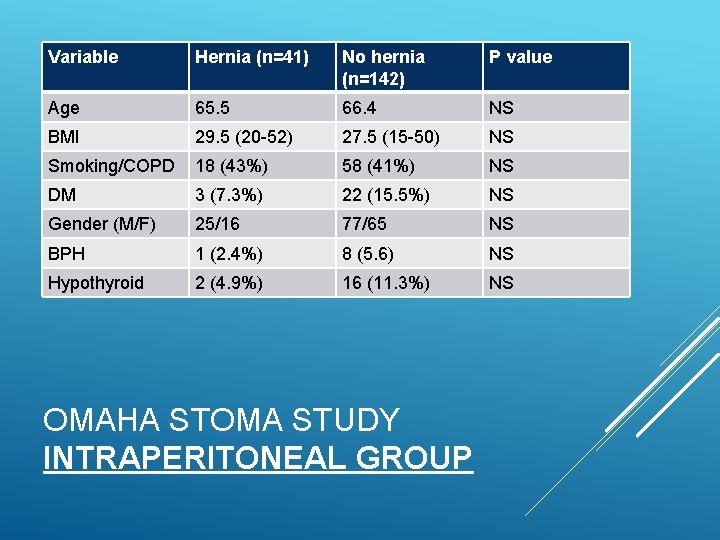
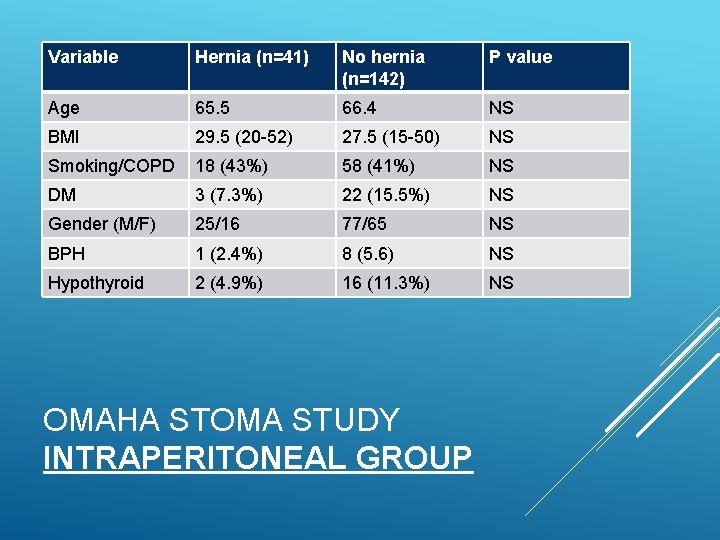
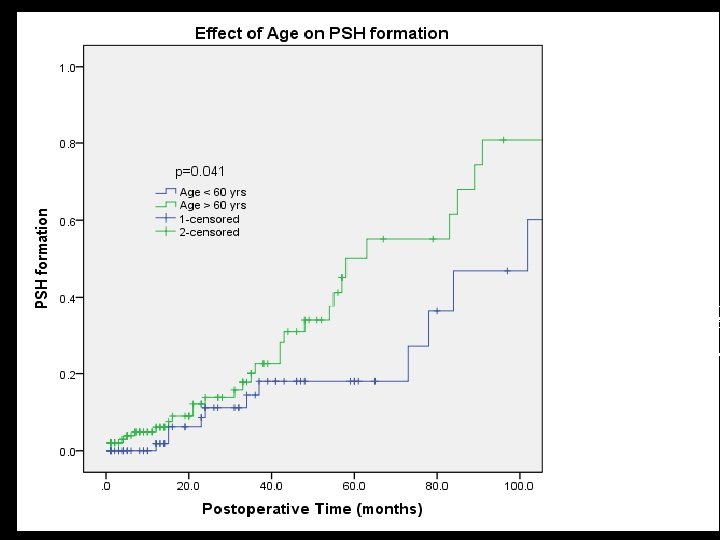
Variable Hernia (n=41) No hernia (n=142) P value Age 65. 5 66. 4 NS BMI 29. 5 (20 -52) 27. 5 (15 -50) NS Smoking/COPD 18 (43%) 58 (41%) NS DM 3 (7. 3%) 22 (15. 5%) NS Gender (M/F) 25/16 77/65 NS BPH 1 (2. 4%) 8 (5. 6) NS Hypothyroid 2 (4. 9%) 16 (11. 3%) NS OMAHA STOMA STUDY INTRAPERITONEAL GROUP
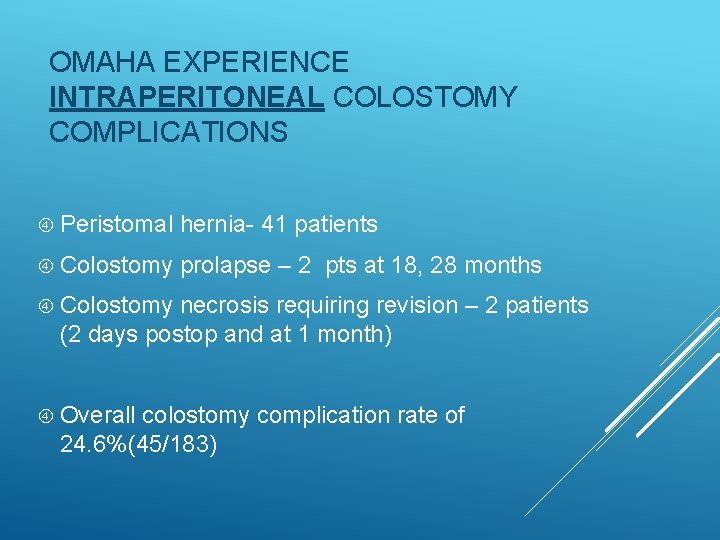
OMAHA EXPERIENCE INTRAPERITONEAL COLOSTOMY COMPLICATIONS Peristomal hernia- 41 patients Colostomy prolapse – 2 pts at 18, 28 months Colostomy necrosis requiring revision – 2 patients (2 days postop and at 1 month) Overall colostomy complication rate of 24. 6%(45/183)
OMAHA EXPERIENCE EXTRAPERITONEAL COLOSTOMY Complications in 2 (5%) p<0. 001 compared to intraperitoneal group Bowel obstruction at 2 months related to small bowel entering extraperitoneal space Diverticulitis of extraperitoneal segment required revision at 64 months No stomal prolapse/necrosis
Phillips “When surgeons who devote a substantial amount of their time to colorectal surgery and who have extensive personal experience of stomal surgery are also found to have a high rate of stoma related complications (cumulative risk of 58. 1% at 13 years) it is time to question some of the tenets that are currently accepted as a sene qua non of good stomal surgery” CONCLUSIONS
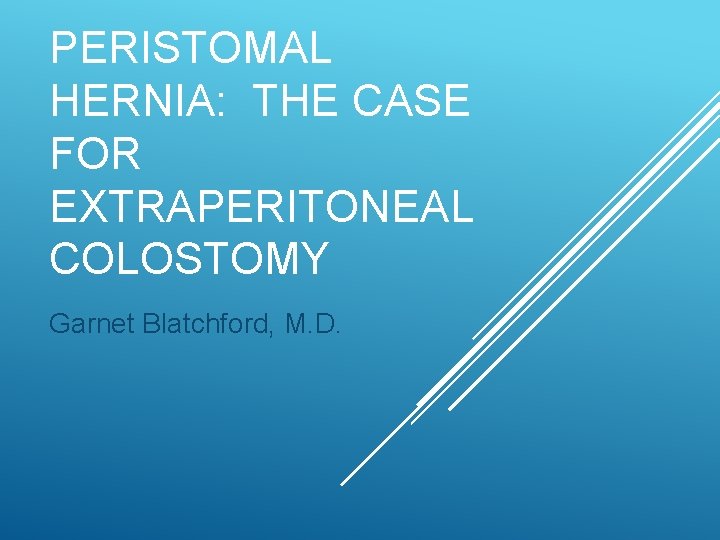
Extraperitoneal colostomy should be the preferred technique for permanent stoma We need to be teaching this technique to our residents when making permanent stomas CONCLUSION OMAHA EXPERIENCE
FOR DISCUSSION: ? If the colon is not amenable to extraperitoneal approach should we do a sugerbaker technique at the original surgery with biologics? Should this technique be done for permanent ileostomies? CONCLUSIONS CONT.
