Peripheral nerve Lower extremity Yohei Harada PGY 2

- Slides: 47
Peripheral nerve (Lower extremity) Yohei Harada, PGY 2 Neurology 09/12/2017
Objectives • To understand the anatomy of peripheral nerve in lower extremity • To understand the function of each peripheral nerve in lower extremity • To understand the exam/test of peripheral nerve disorder in lower extremity
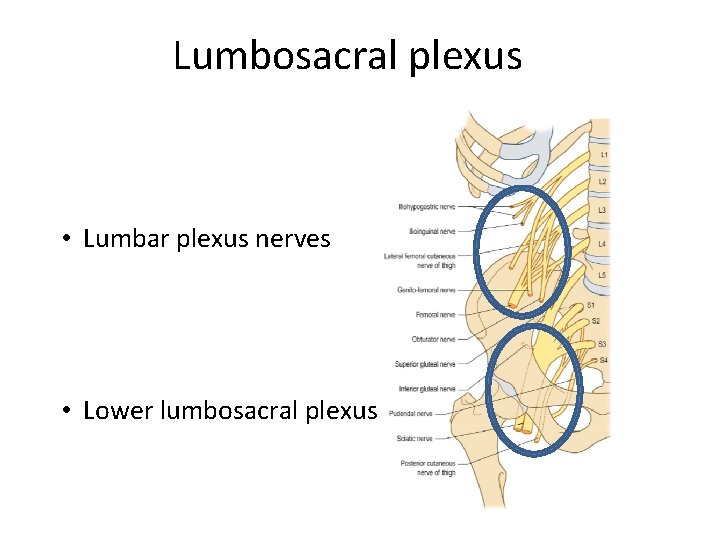
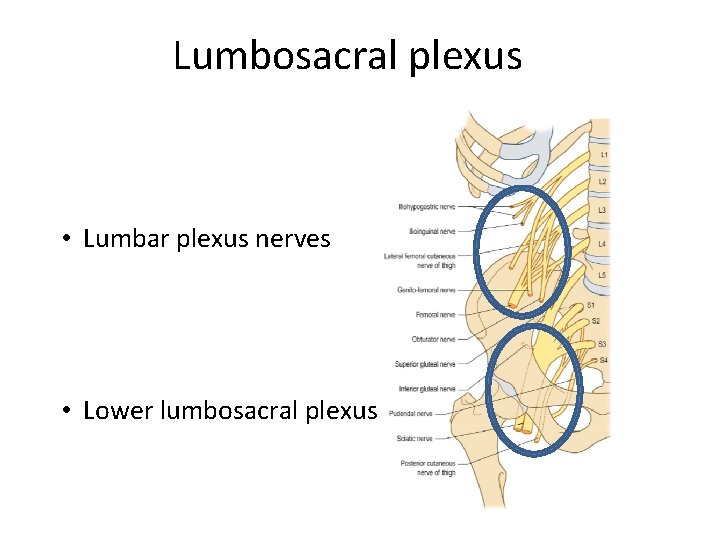
Lumbosacral plexus • Lumbar plexus nerves • Lower lumbosacral plexus
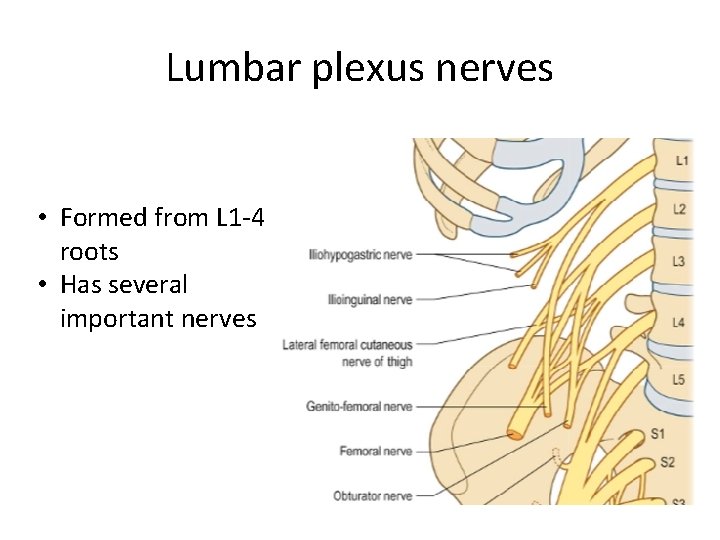
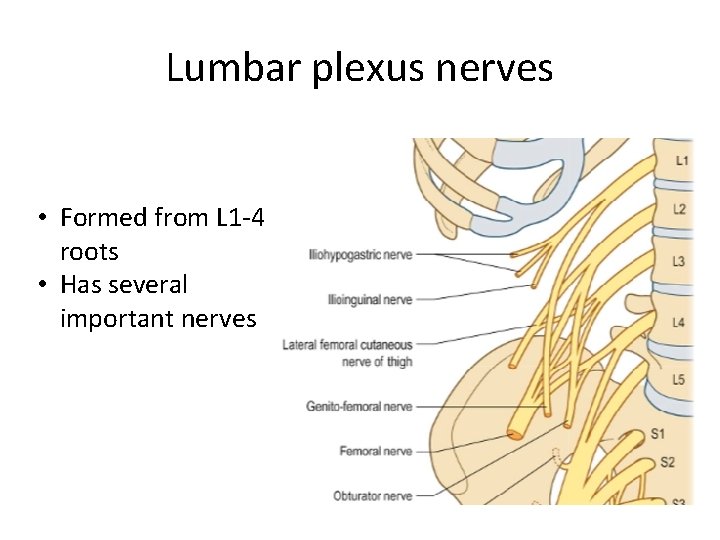
Lumbar plexus nerves • Formed from L 1 -4 roots • Has several important nerves
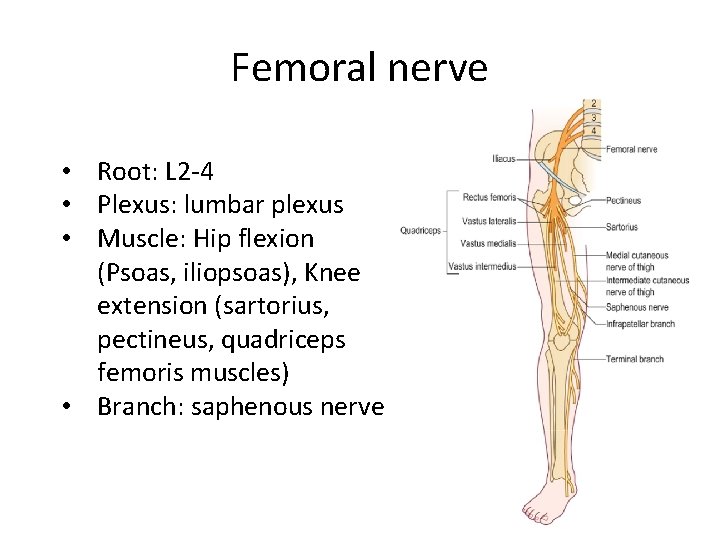
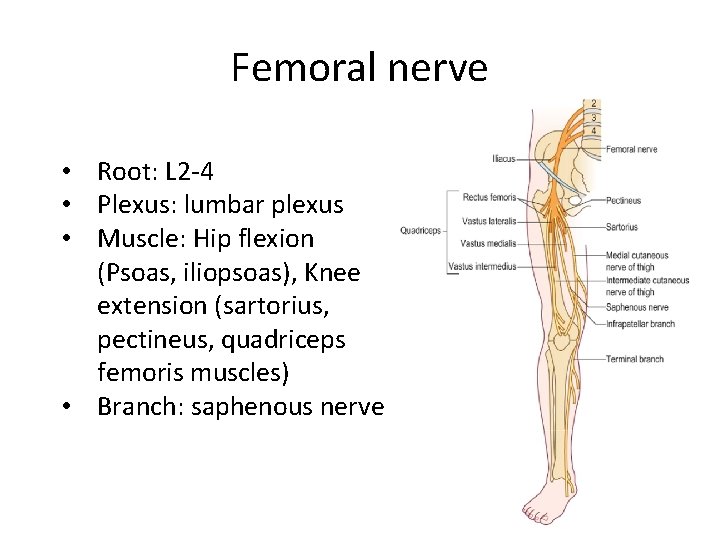
Femoral nerve • Root: L 2 -4 • Plexus: lumbar plexus • Muscle: Hip flexion (Psoas, iliopsoas), Knee extension (sartorius, pectineus, quadriceps femoris muscles) • Branch: saphenous nerve
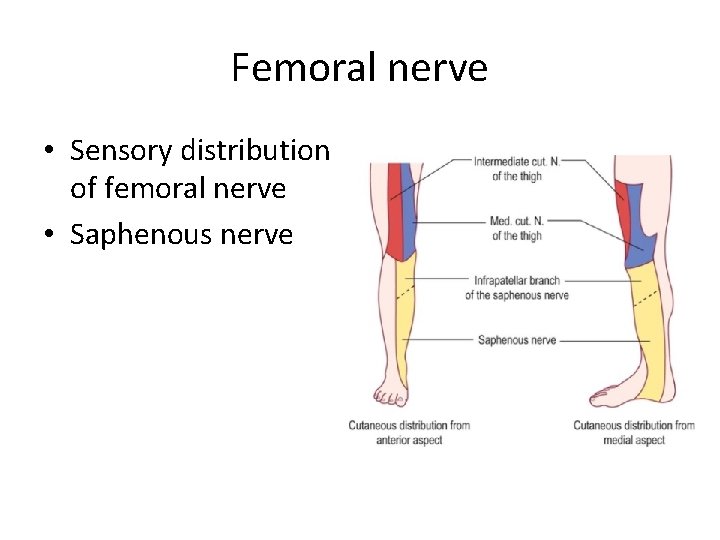
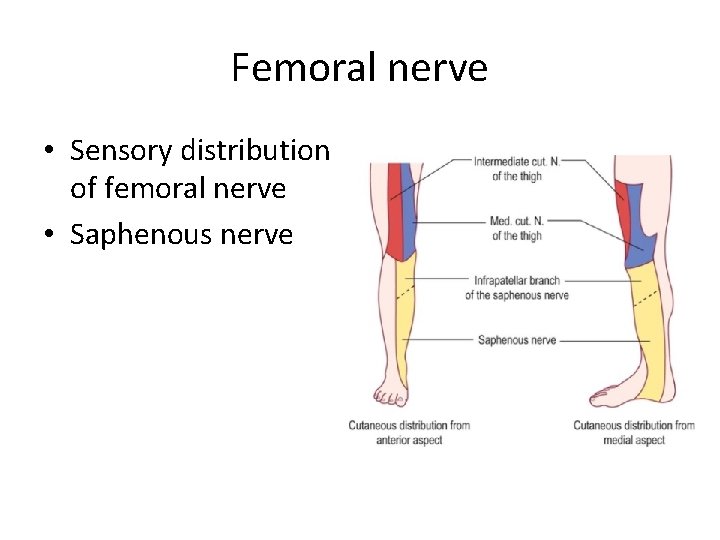
Femoral nerve • Sensory distribution of femoral nerve • Saphenous nerve
Clinical signs of femoral neuropathy • Buckling of the knee • Difficulty lifting up the thigh • Sensory disturbance may be seen over the medial and anterior thigh and the medial calf 1 Where in the thigh sensory is spared?
Clinical signs of femoral neuropathy • Buckling of the knee • Difficulty lifting up the thigh • Sensory disturbance may be seen over the medial and anterior thigh and the medial calf 1 Where in the thigh sensory is spared? • Lateral thigh (lateral femoral cutaneous nerve) • Proximal medial thigh (obturator nerve) • Posterior thigh (posterior cutaneous nerve of thigh)
Clinical signs of femoral neuropathy • Buckling of the knee • Difficulty lifting up the thigh • Sensory disturbance may be seen over the medial and anterior thigh and the medial calf 2 How about reflex?
Clinical signs of femoral neuropathy • Buckling of the knee • Difficulty lifting up the thigh • Sensory disturbance may be seen over the medial and anterior thigh and the medial calf 2 How about reflex? Reduced/Absent knee reflex
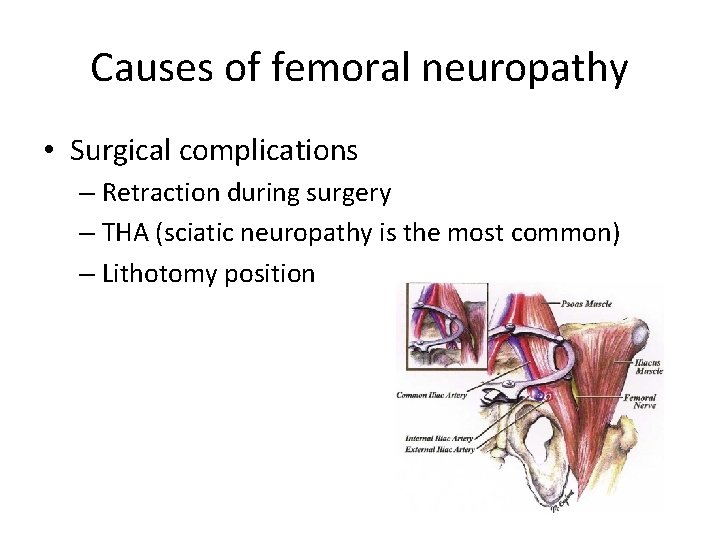
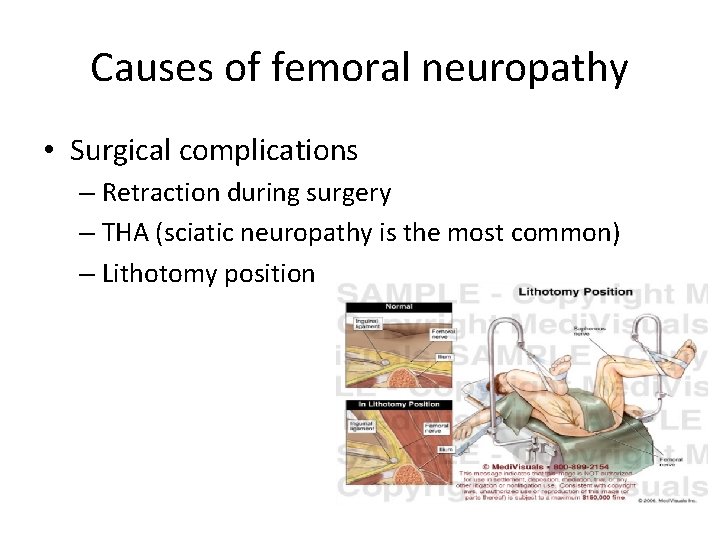
Causes of femoral neuropathy • Surgical complications – Retraction during surgery – THA (sciatic neuropathy is the most common) – Lithotomy position
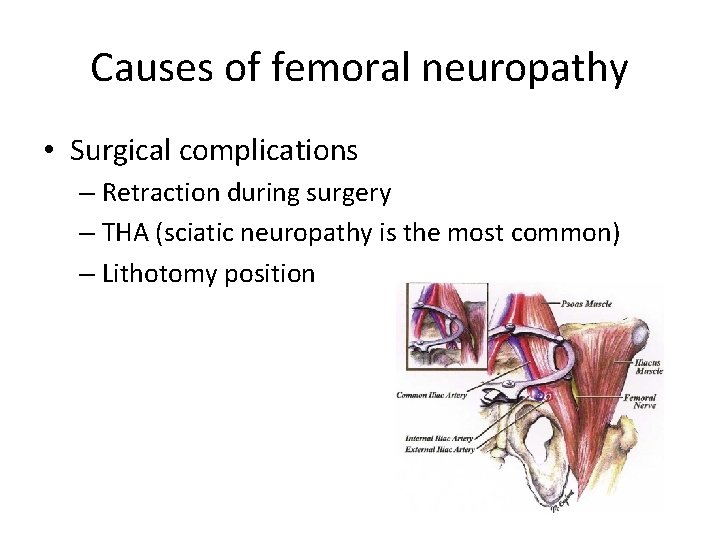
Causes of femoral neuropathy • Surgical complications – Retraction during surgery – THA (sciatic neuropathy is the most common) – Lithotomy position
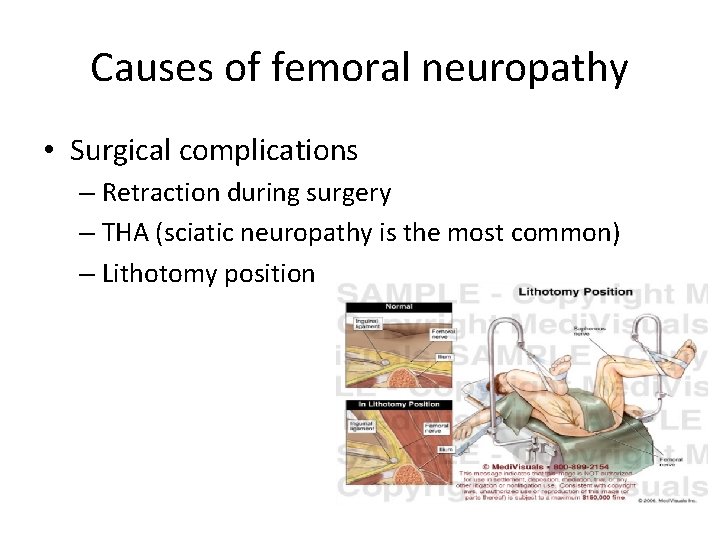
Causes of femoral neuropathy • Surgical complications – Retraction during surgery – THA (sciatic neuropathy is the most common) – Lithotomy position
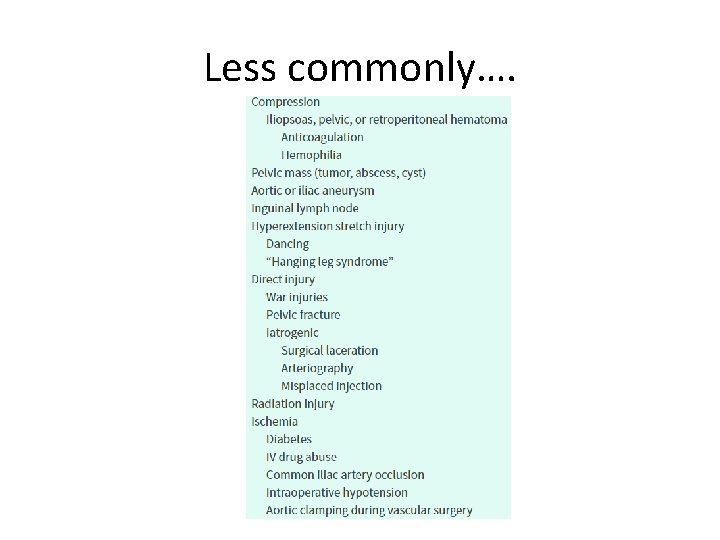
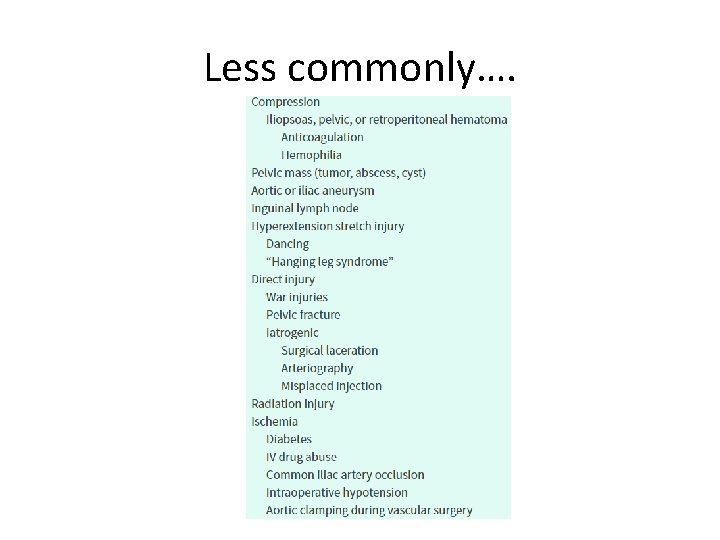
Less commonly….
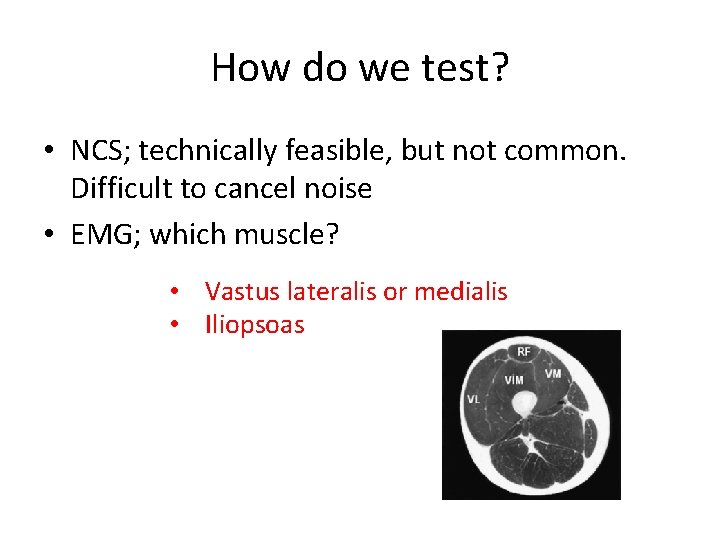
How do we test? • NCS; technically feasible, but not common. Difficult to cancel noise • EMG; which muscle?
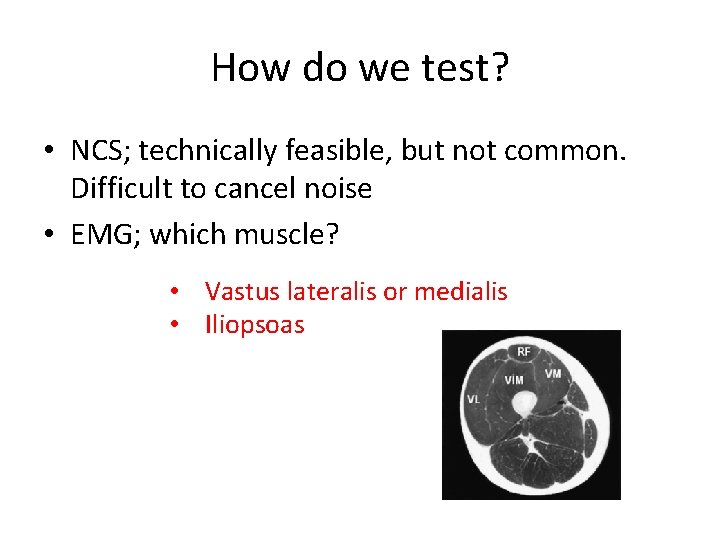
How do we test? • NCS; technically feasible, but not common. Difficult to cancel noise • EMG; which muscle? • Vastus lateralis or medialis • Iliopsoas
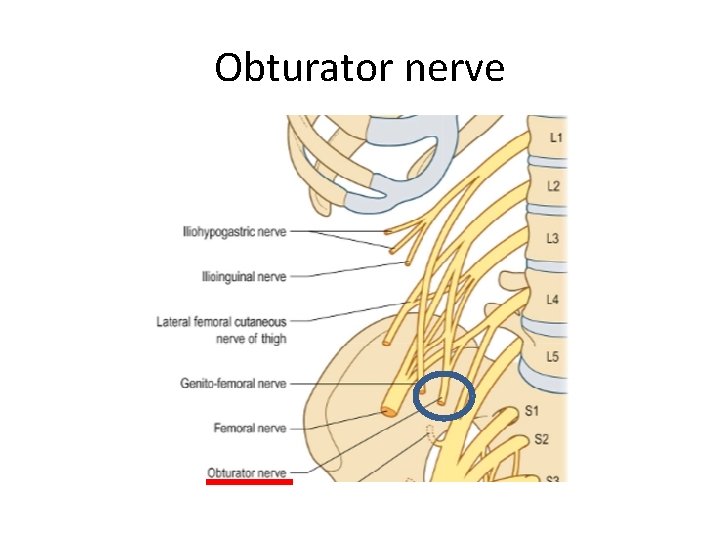
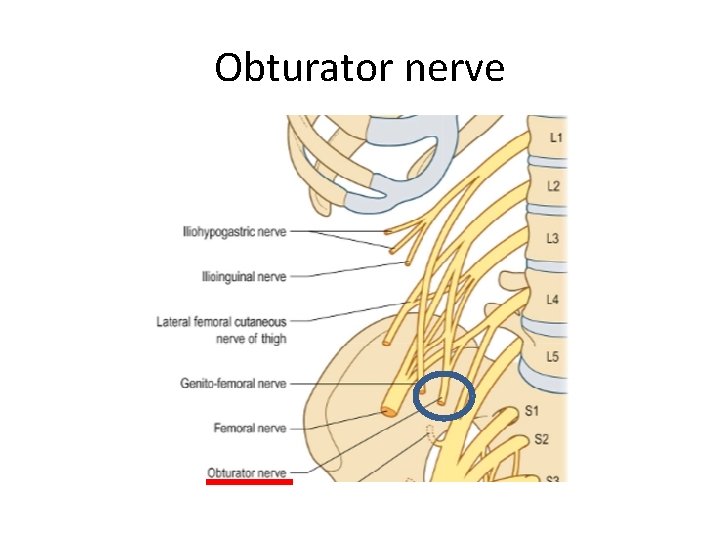
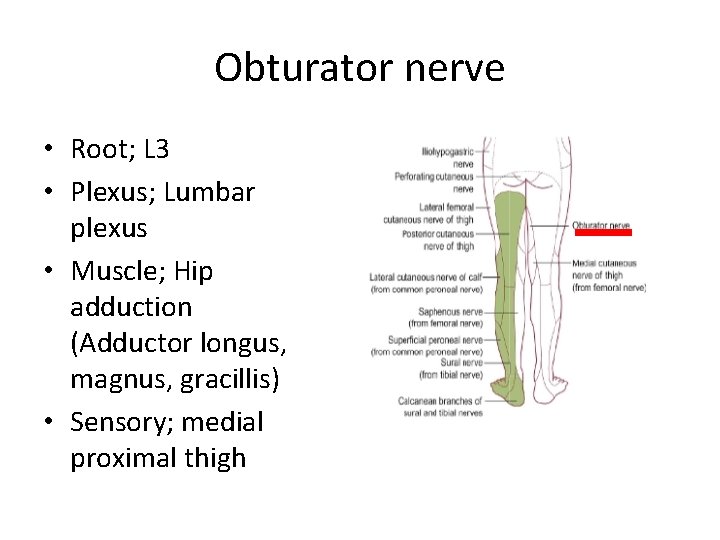
Obturator nerve
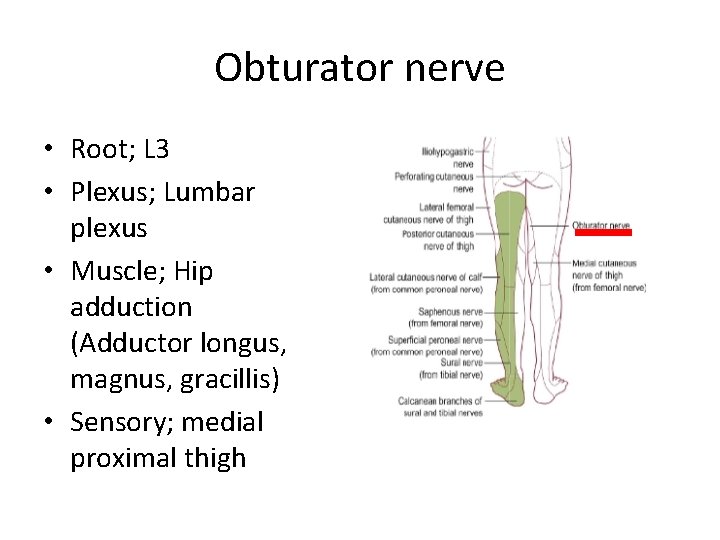
Obturator nerve • Root; L 3 • Plexus; Lumbar plexus • Muscle; Hip adduction (Adductor longus, magnus, gracillis) • Sensory; medial proximal thigh
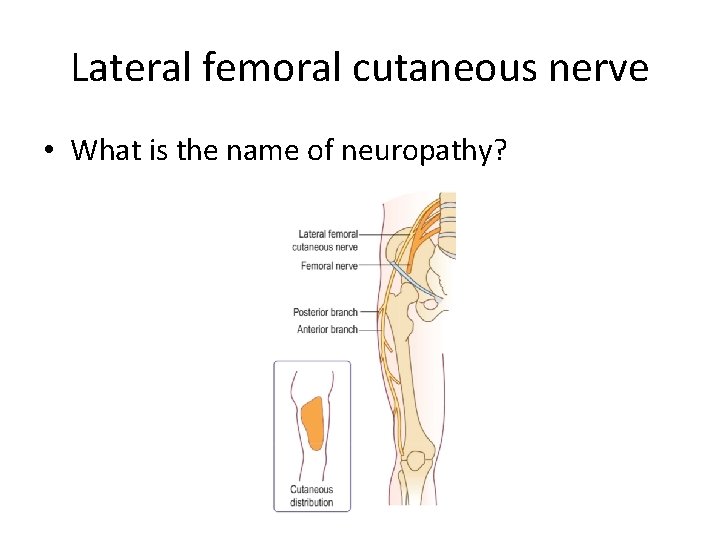
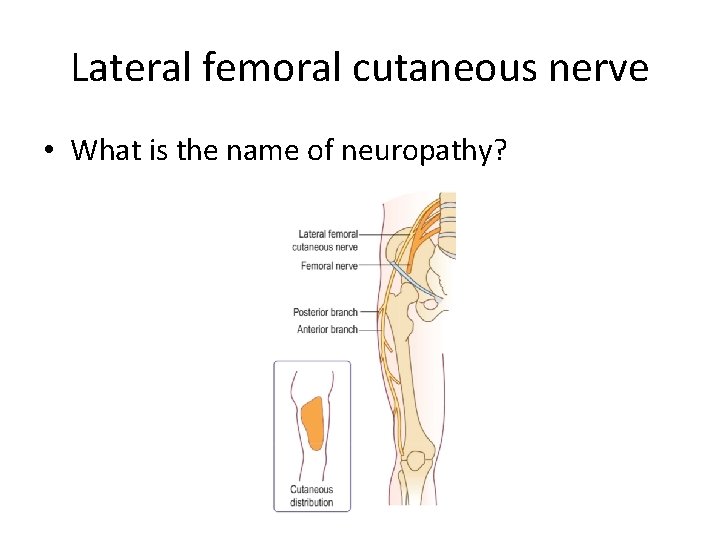
Lateral femoral cutaneous nerve • What is the name of neuropathy?
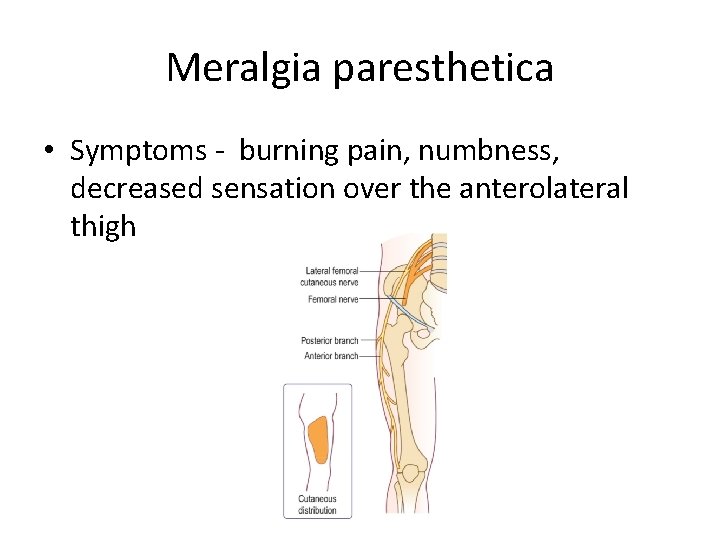
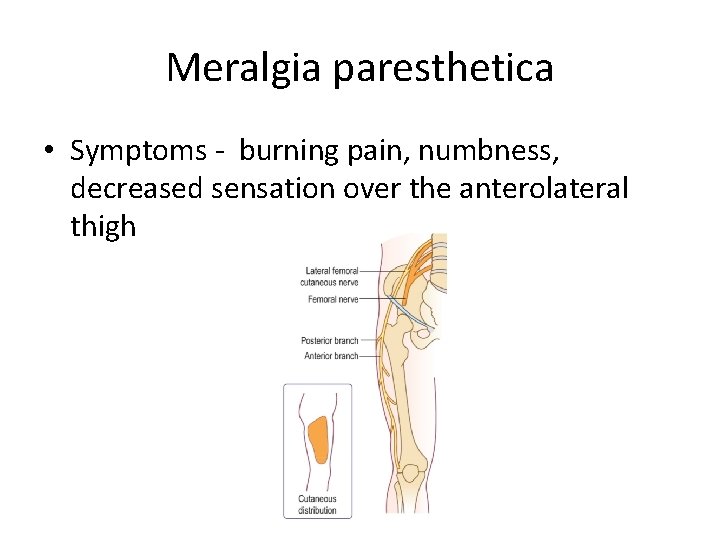
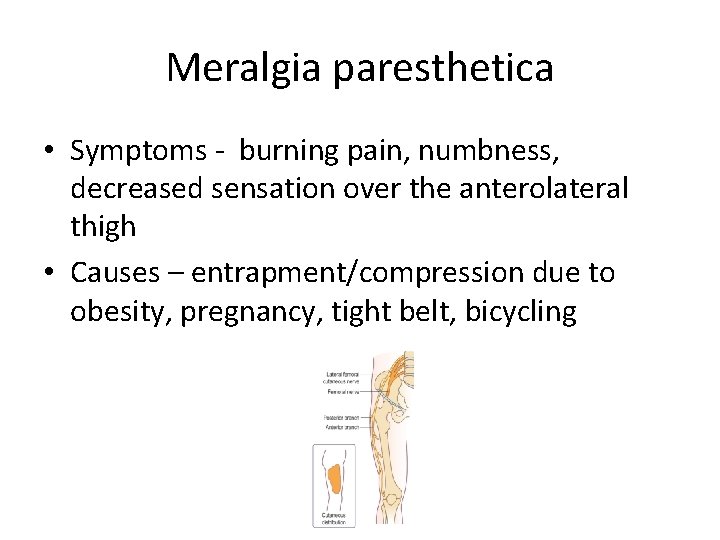
Meralgia paresthetica • Symptoms - burning pain, numbness, decreased sensation over the anterolateral thigh
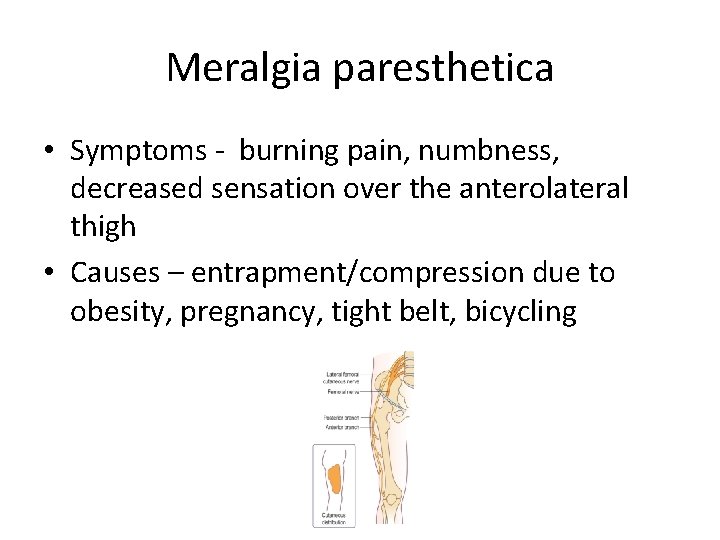
Meralgia paresthetica • Symptoms - burning pain, numbness, decreased sensation over the anterolateral thigh • Causes – entrapment/compression due to obesity, pregnancy, tight belt, bicycling
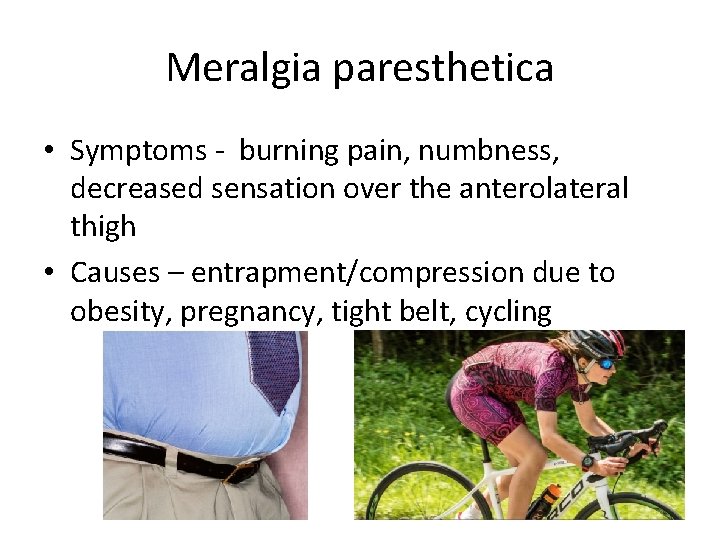
Meralgia paresthetica • Symptoms - burning pain, numbness, decreased sensation over the anterolateral thigh • Causes – entrapment/compression due to obesity, pregnancy, tight belt, cycling
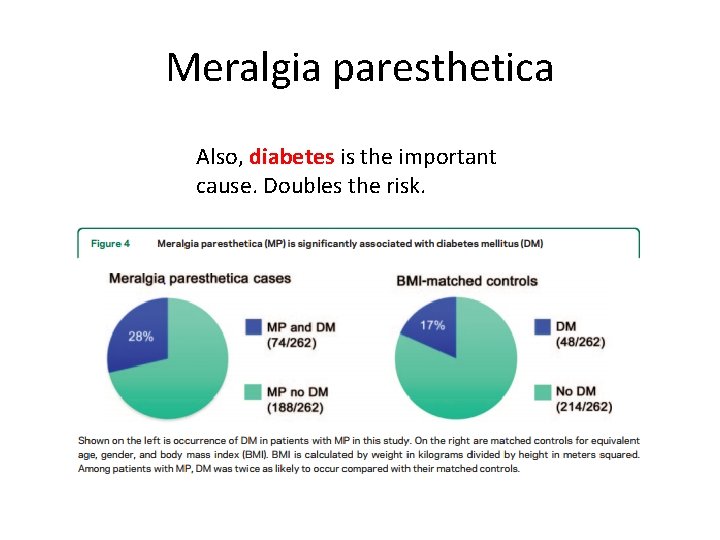
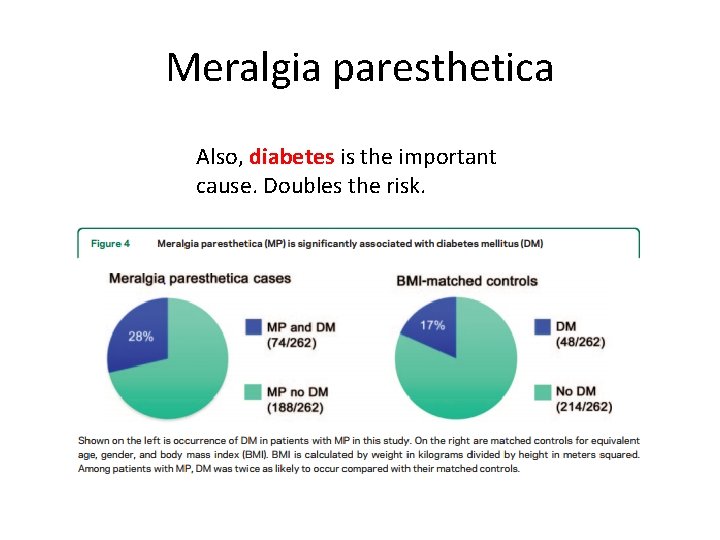
Meralgia paresthetica Also, diabetes is the important cause. Doubles the risk.
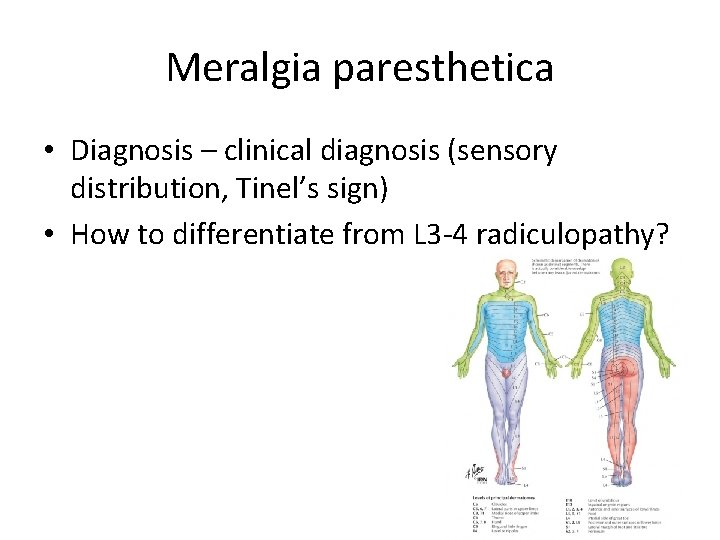
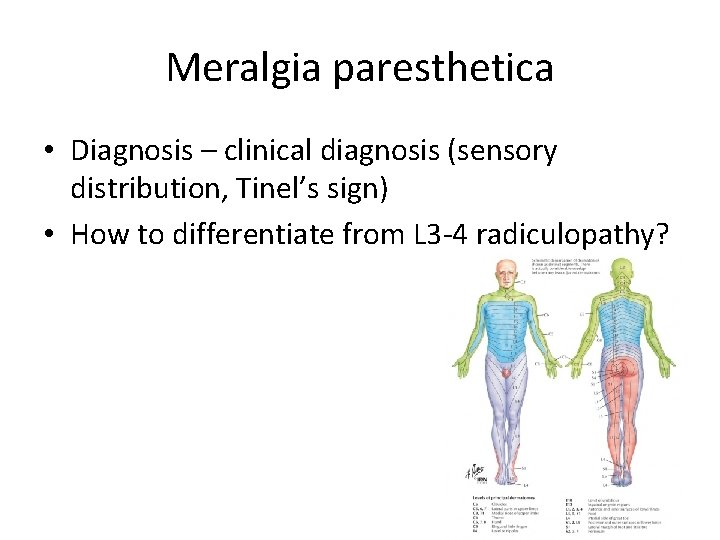
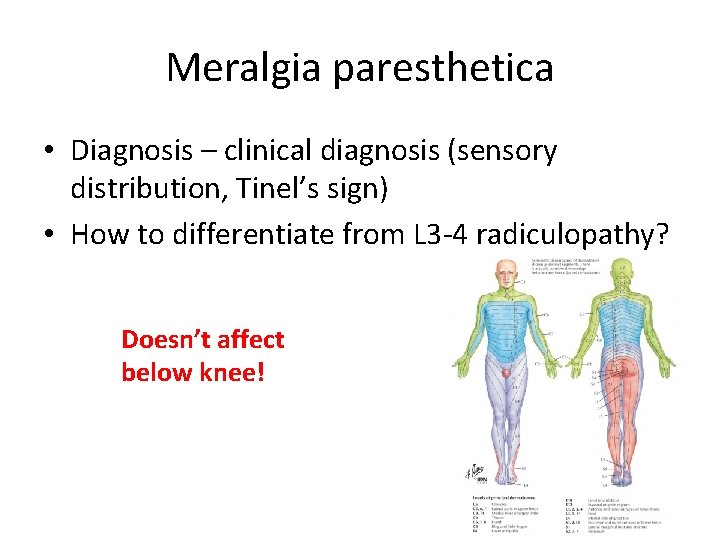
Meralgia paresthetica • Diagnosis – clinical diagnosis (sensory distribution, Tinel’s sign) • How to differentiate from L 3 -4 radiculopathy?
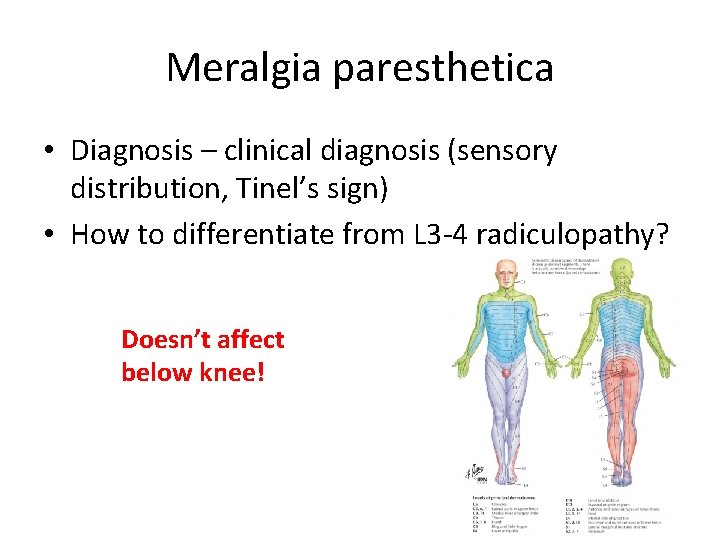
Meralgia paresthetica • Diagnosis – clinical diagnosis (sensory distribution, Tinel’s sign) • How to differentiate from L 3 -4 radiculopathy? Doesn’t affect below knee!

Meralgia paresthetica • Diagnosis – NCS
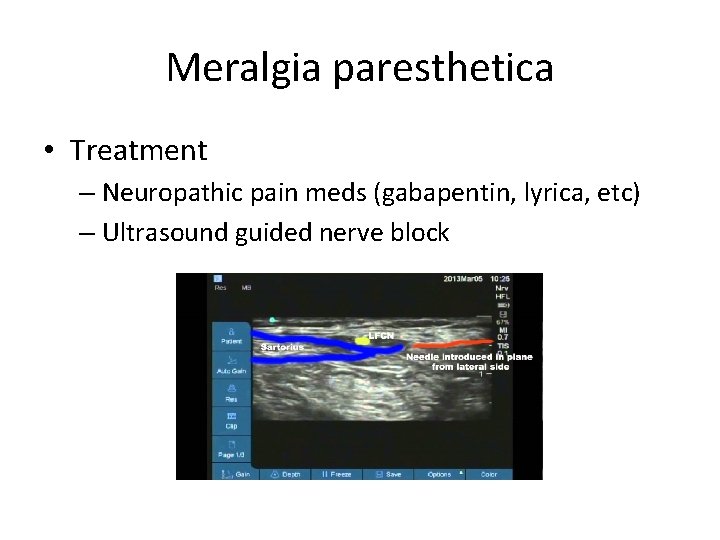
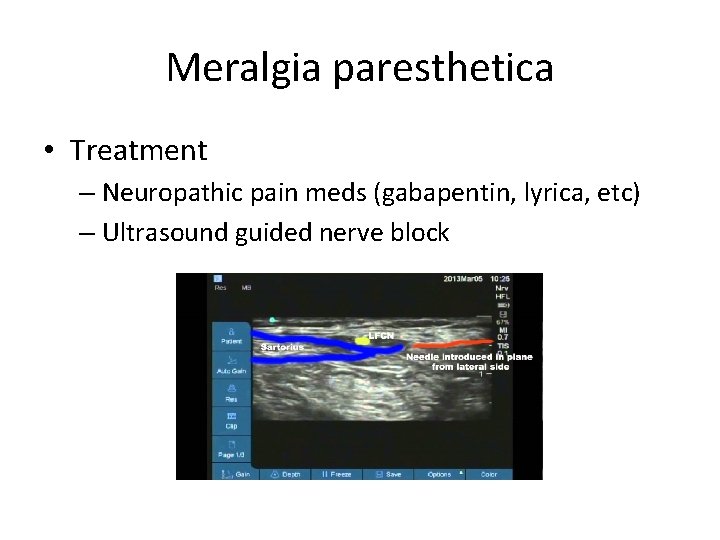
Meralgia paresthetica • Treatment – Neuropathic pain meds (gabapentin, lyrica, etc) – Ultrasound guided nerve block
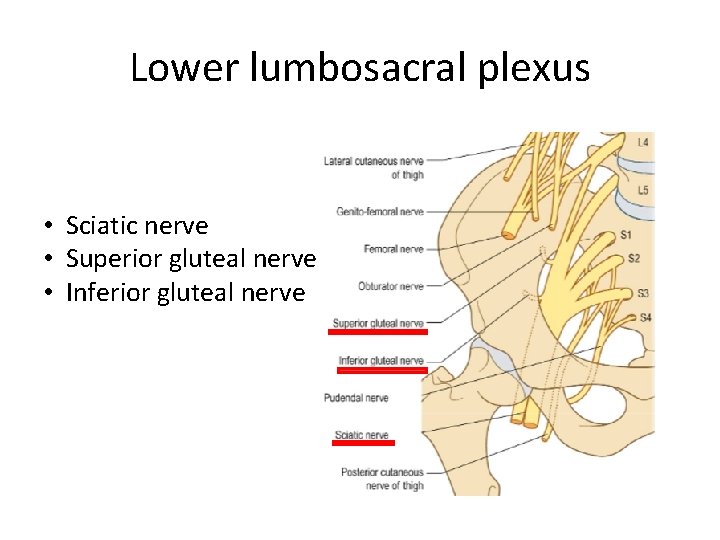
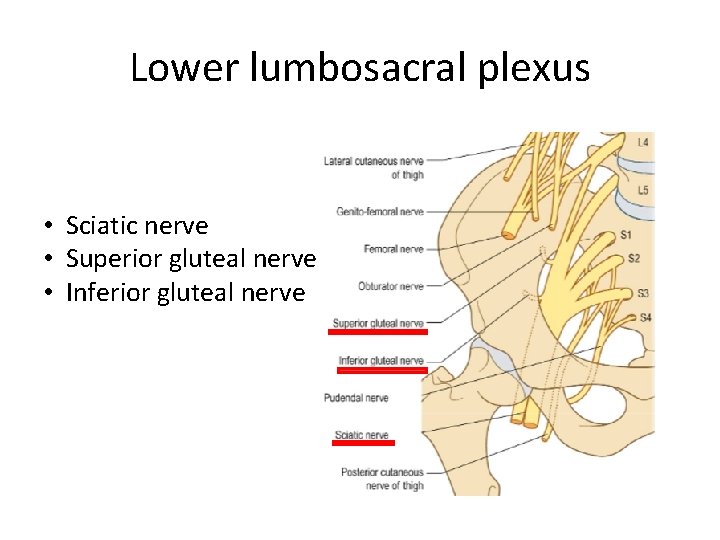
Lower lumbosacral plexus • Sciatic nerve • Superior gluteal nerve • Inferior gluteal nerve
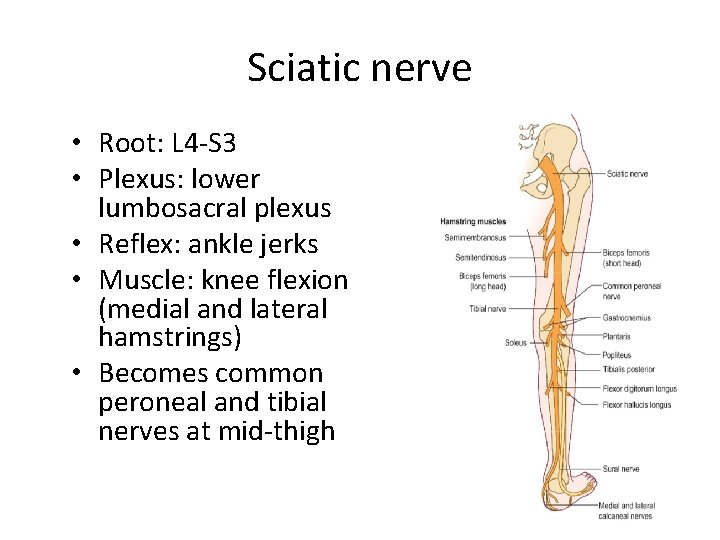
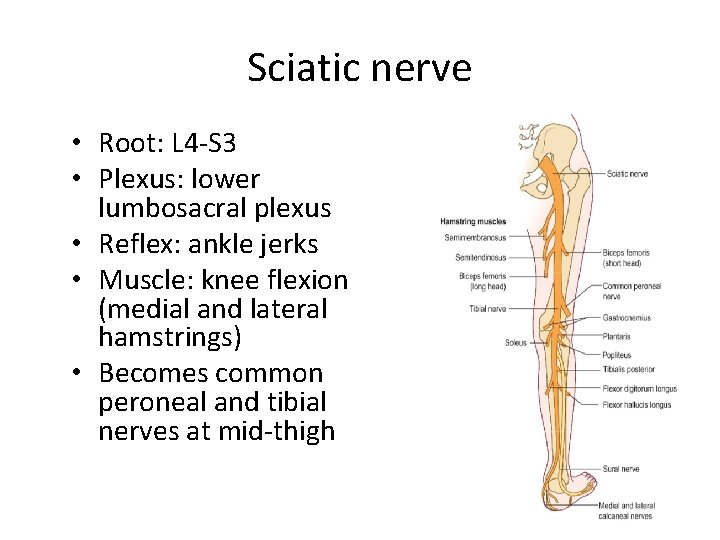
Sciatic nerve • Root: L 4 -S 3 • Plexus: lower lumbosacral plexus • Reflex: ankle jerks • Muscle: knee flexion (medial and lateral hamstrings) • Becomes common peroneal and tibial nerves at mid-thigh
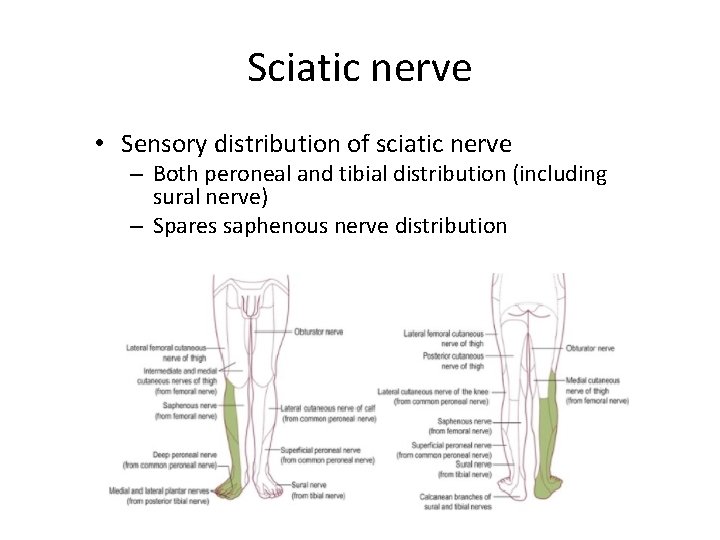
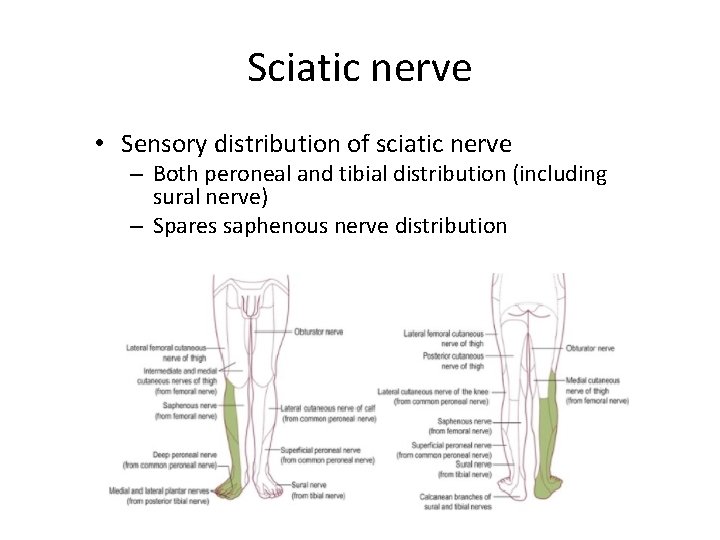
Sciatic nerve • Sensory distribution of sciatic nerve – Both peroneal and tibial distribution (including sural nerve) – Spares saphenous nerve distribution
Sciatic nerve • Which nerve is affected by sciatic neuropathy? 1. Peroneal nerve 2. Tibial nerve 3. Both
Sciatic nerve • Which nerve is affected by sciatic neuropathy? 1. Peroneal nerve 2. Tibial nerve 3. Both 3. However… Initially, peroneal nerves are preferentially affected in sciatic nerve lesion.
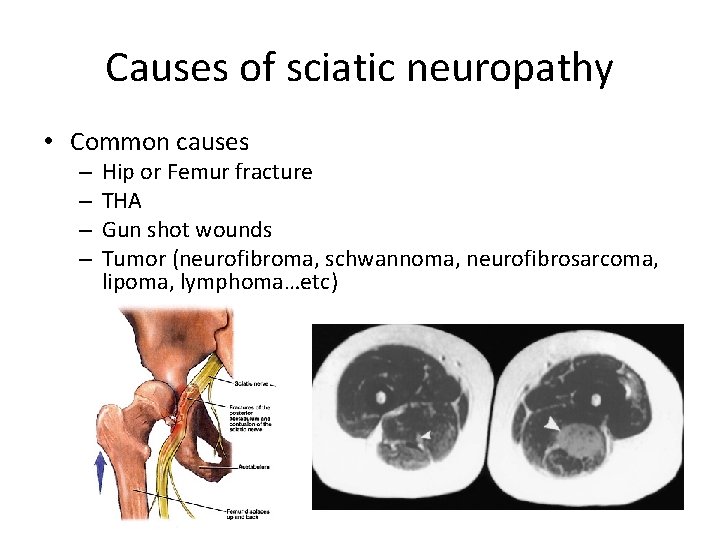
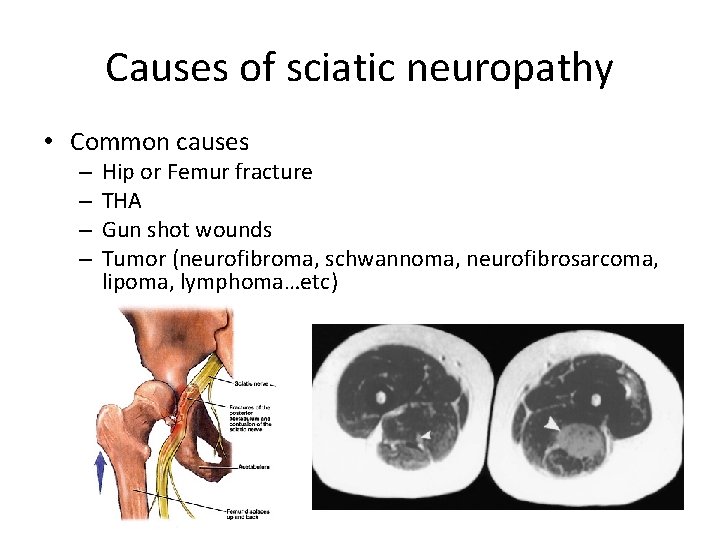
Causes of sciatic neuropathy • Common causes – – Hip or Femur fracture THA Gun shot wounds Tumor (neurofibroma, schwannoma, neurofibrosarcoma, lipoma, lymphoma…etc)
Let’s create a case • This is a sciatic neuropathy case. A 52 yo woman was referred for evaluation of 6 months history of left foot drop. She initially felt numbness over ( where? ). This was shortly followed by left foot dropping. Most recently, she noted a sensation of tightness and pain from ( where? ) to ( where? ).
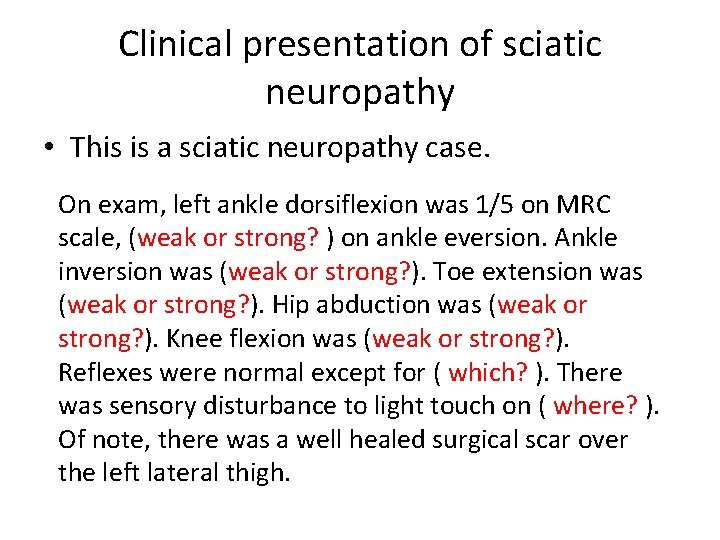
Clinical presentation of sciatic neuropathy • This is a sciatic neuropathy case. On exam, left ankle dorsiflexion was 1/5 on MRC scale, (weak or strong? ) on ankle eversion. Ankle inversion was (weak or strong? ). Toe extension was (weak or strong? ). Hip abduction was (weak or strong? ). Knee flexion was (weak or strong? ). Reflexes were normal except for ( which? ). There was sensory disturbance to light touch on ( where? ). Of note, there was a well healed surgical scar over the left lateral thigh.
• Might be a bit too complicated until understanding peroneal and tibial.
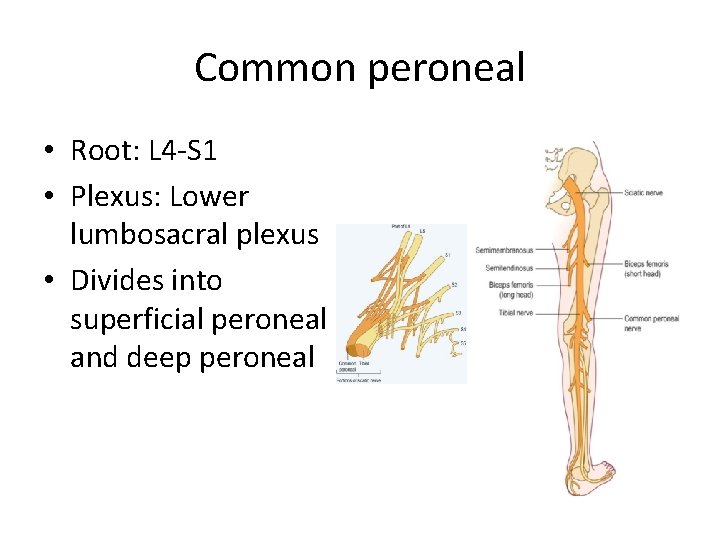
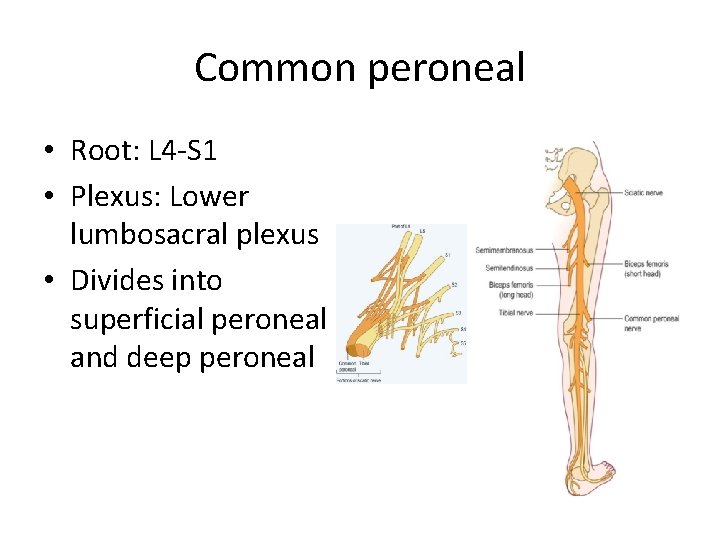
Common peroneal • Root: L 4 -S 1 • Plexus: Lower lumbosacral plexus • Divides into superficial peroneal and deep peroneal
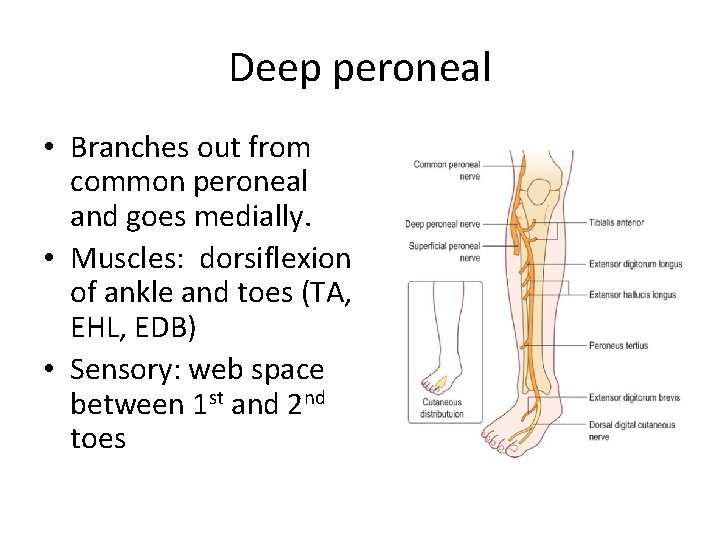
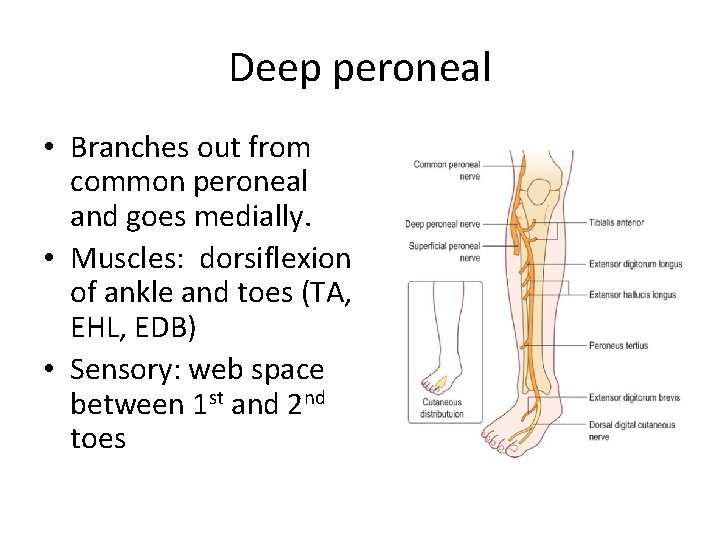
Deep peroneal • Branches out from common peroneal and goes medially. • Muscles: dorsiflexion of ankle and toes (TA, EHL, EDB) • Sensory: web space between 1 st and 2 nd toes
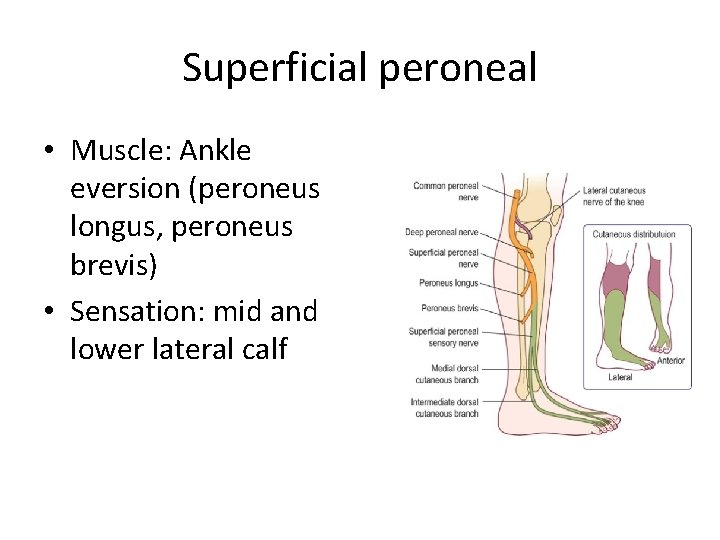
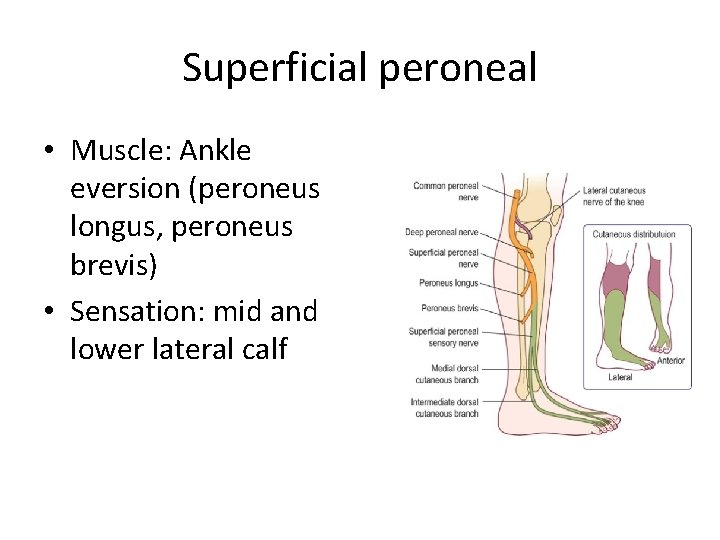
Superficial peroneal • Muscle: Ankle eversion (peroneus longus, peroneus brevis) • Sensation: mid and lower lateral calf
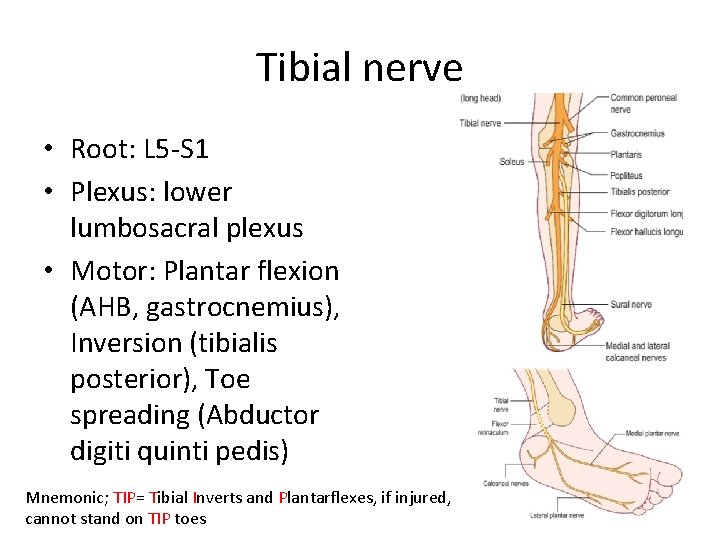
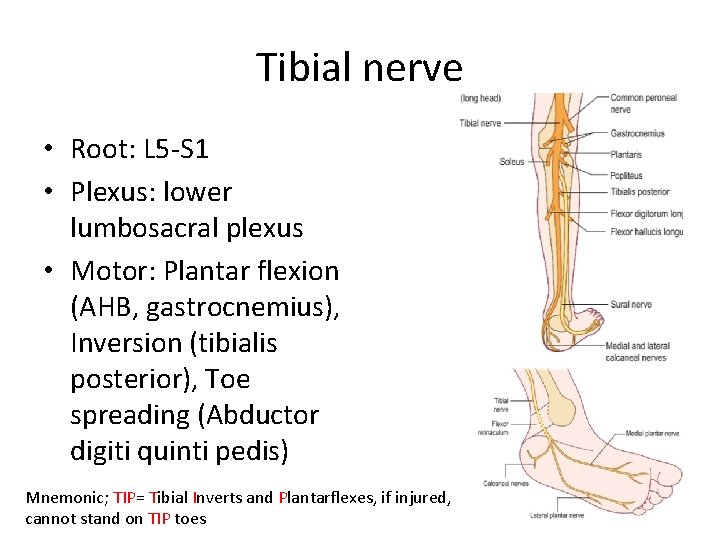
Tibial nerve • Root: L 5 -S 1 • Plexus: lower lumbosacral plexus • Motor: Plantar flexion (AHB, gastrocnemius), Inversion (tibialis posterior), Toe spreading (Abductor digiti quinti pedis) Mnemonic; TIP= Tibial Inverts and Plantarflexes, if injured, cannot stand on TIP toes
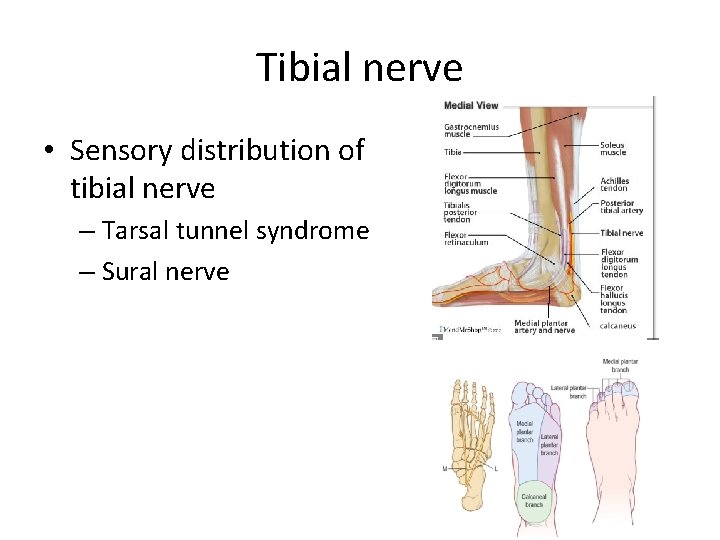
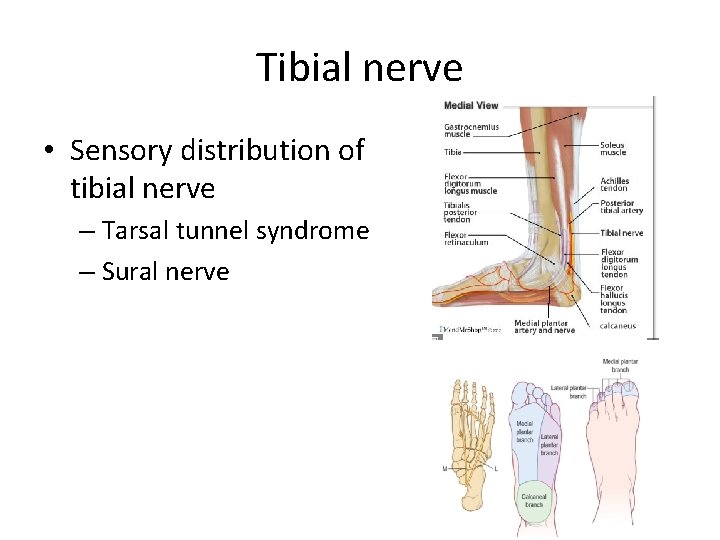
Tibial nerve • Sensory distribution of tibial nerve – Tarsal tunnel syndrome – Sural nerve
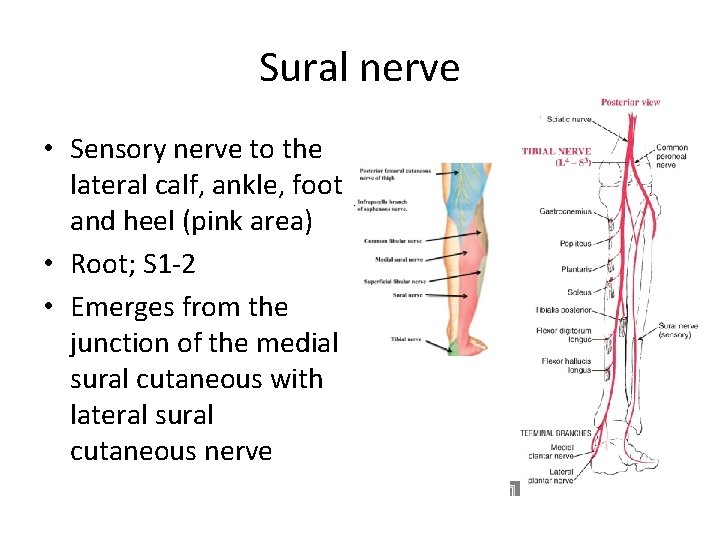
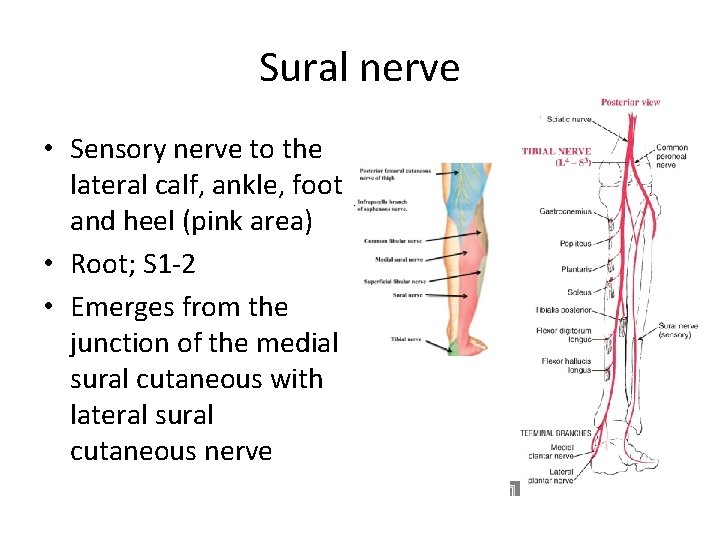
Sural nerve • Sensory nerve to the lateral calf, ankle, foot and heel (pink area) • Root; S 1 -2 • Emerges from the junction of the medial sural cutaneous with lateral sural cutaneous nerve
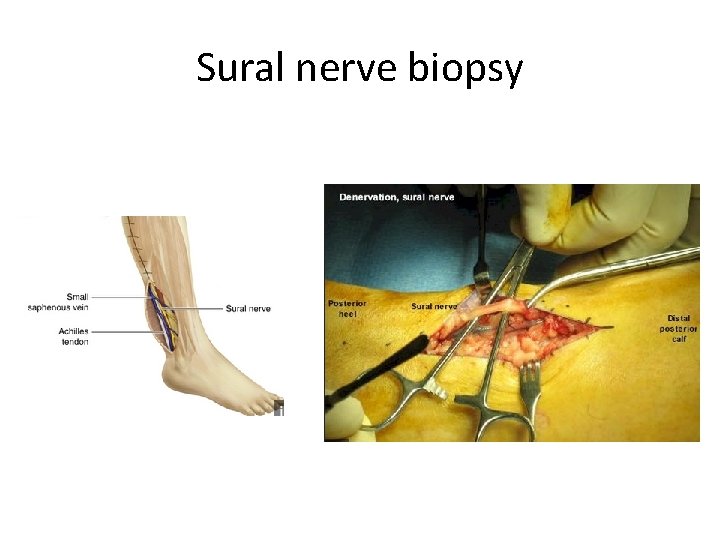
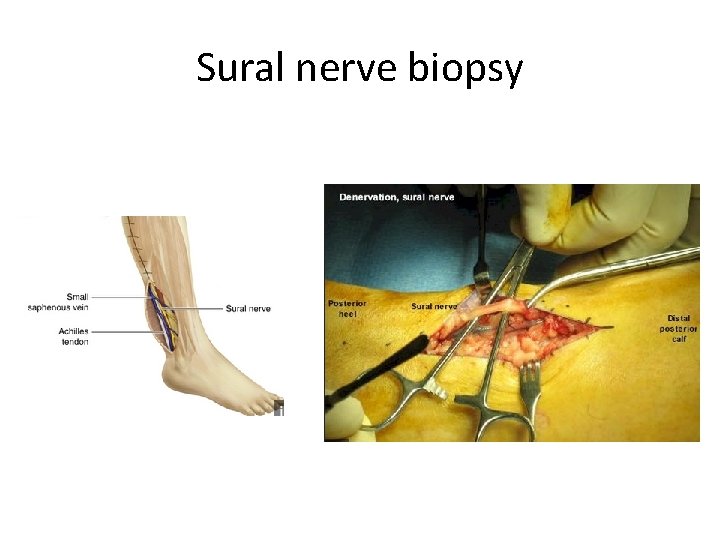
Sural nerve biopsy
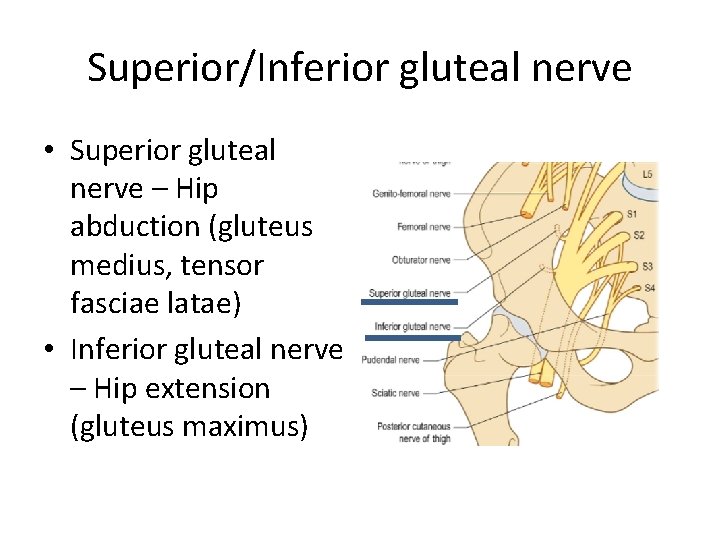
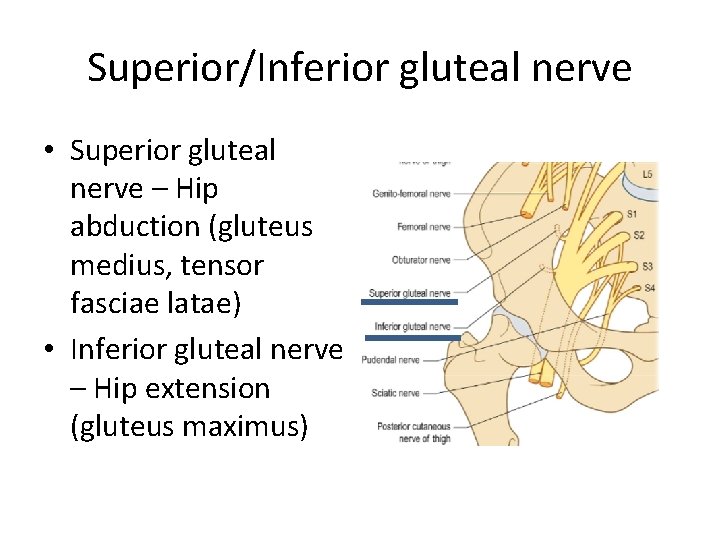
Superior/Inferior gluteal nerve • Superior gluteal nerve – Hip abduction (gluteus medius, tensor fasciae latae) • Inferior gluteal nerve – Hip extension (gluteus maximus)
Let’s create a case • This is a sciatic neuropathy case. A 52 yo woman was referred for evaluation of 6 months history of left foot drop. She initially felt numbness over ( where? ). This was shortly followed by left foot dropping. Most recently, she noted a sensation of tightness and pain from ( where? ) to ( where? ).
Clinical presentation of sciatic neuropathy • This is a sciatic neuropathy case. On exam, left ankle dorsiflexion was 1/5 on MRC scale, (weak or strong? ) on ankle eversion. Ankle inversion was (weak or strong? ). Toe extension was (weak or strong? ). Hip abduction was (weak or strong? ). Knee flexion was (weak or strong? ). Reflexes were normal except for ( which? ). There was sensory disturbance to light touch on ( where? ). Of note, there was a well healed surgical scar over the left lateral thigh.
thanks