PERIPHERAL NERVE INJURY PRINCIPLES OF REPAIR WALEED HADDAD




- Slides: 50
PERIPHERAL NERVE INJURY & PRINCIPLES OF REPAIR WALEED HADDAD CONSULTANT ORTHOPAEDICS HAND & UPPER LIMB SURGEON
Objectives • Know the anatomy of peripheral nerves • Understand types of nerve injuries • Know the pathological changes • Know and understand principles of repair • Know the limitation for direct nerve repair • Know the alternatives
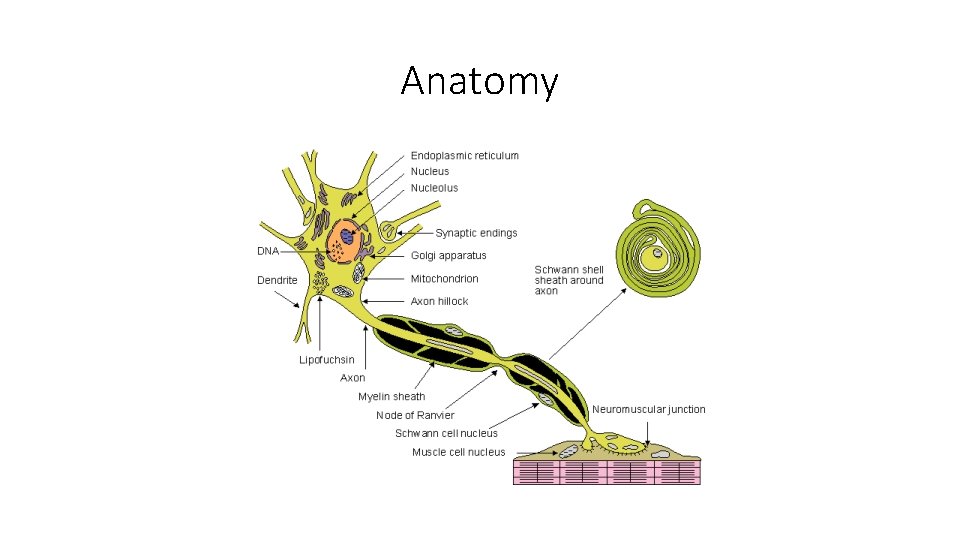
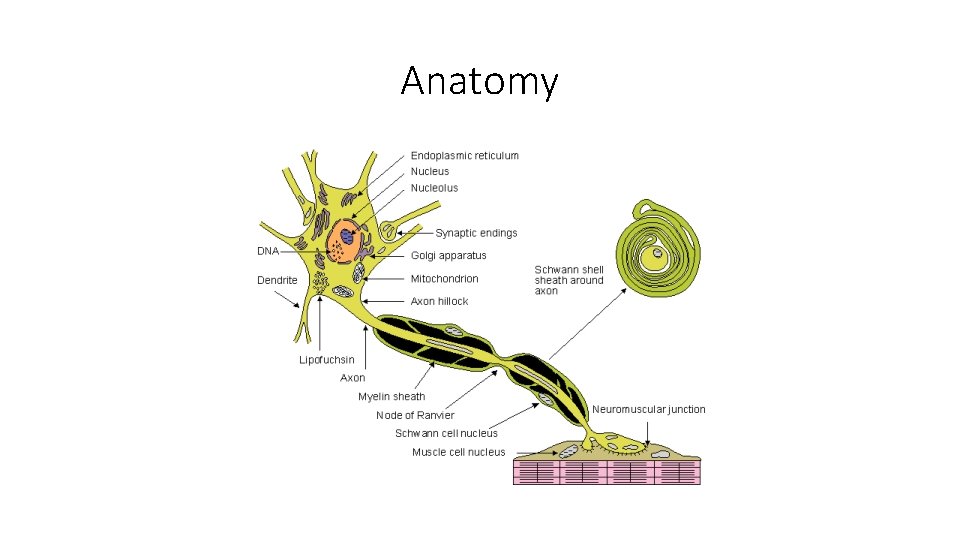
Anatomy
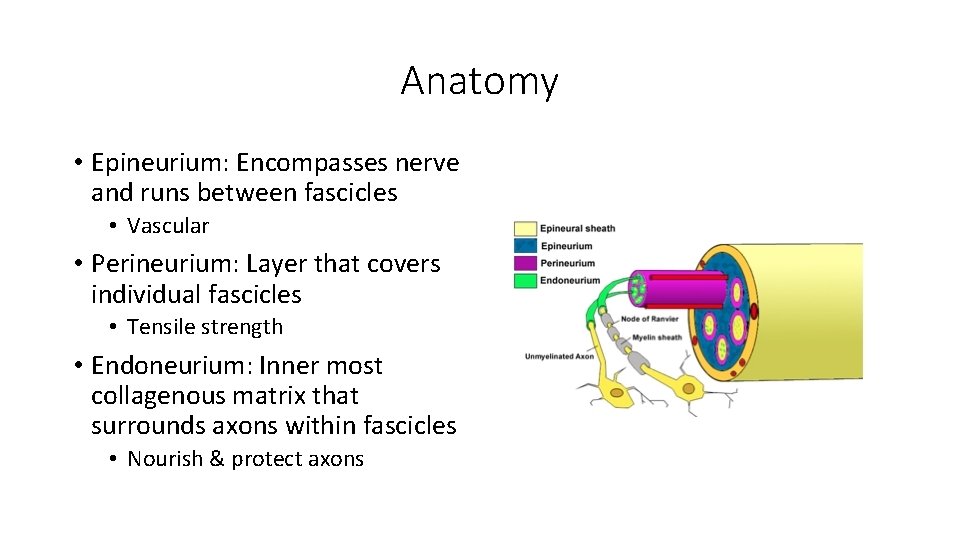
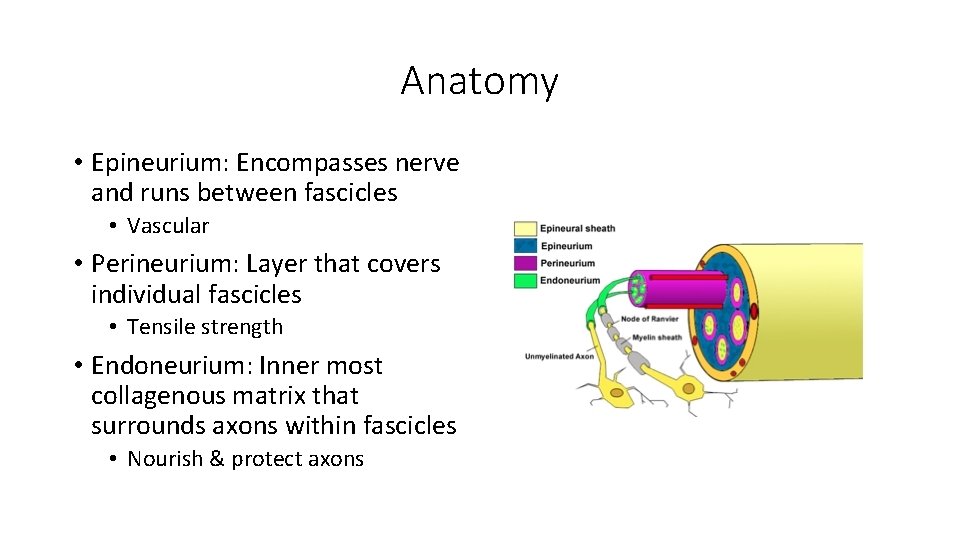
Anatomy • Epineurium: Encompasses nerve and runs between fascicles • Vascular • Perineurium: Layer that covers individual fascicles • Tensile strength • Endoneurium: Inner most collagenous matrix that surrounds axons within fascicles • Nourish & protect axons
Anatomy • Motor • Sensory • mixed
Causes of Peripheral Neuropathy • Trauma • Compression (entrapment) • Irritation • Metabolic disorders • Inflammatory (neuritis) • Virus • Age related changes
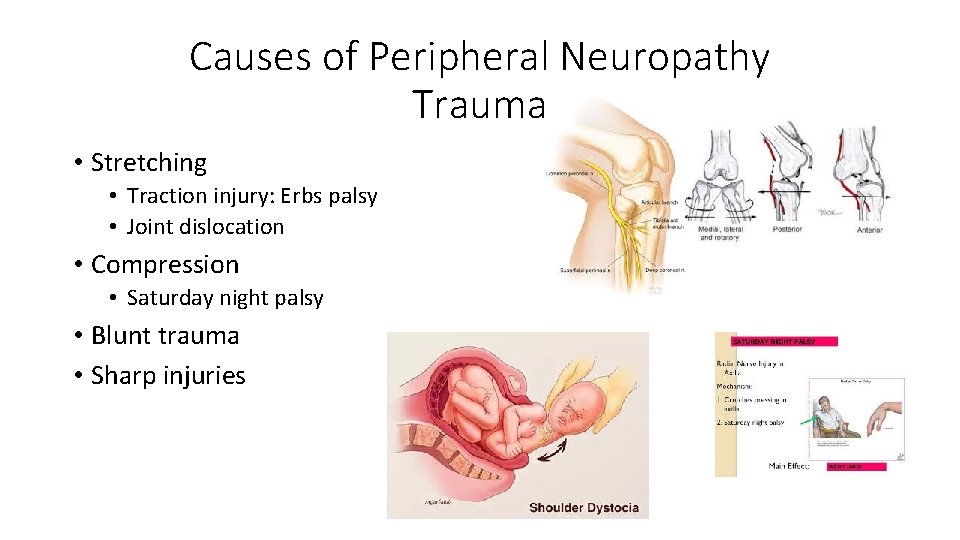
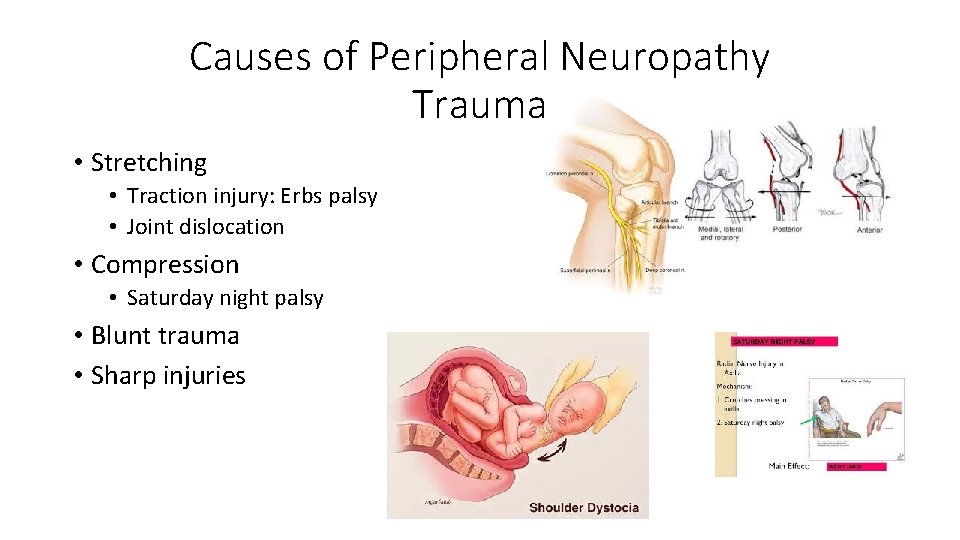
Causes of Peripheral Neuropathy Trauma • Stretching • Traction injury: Erbs palsy • Joint dislocation • Compression • Saturday night palsy • Blunt trauma • Sharp injuries
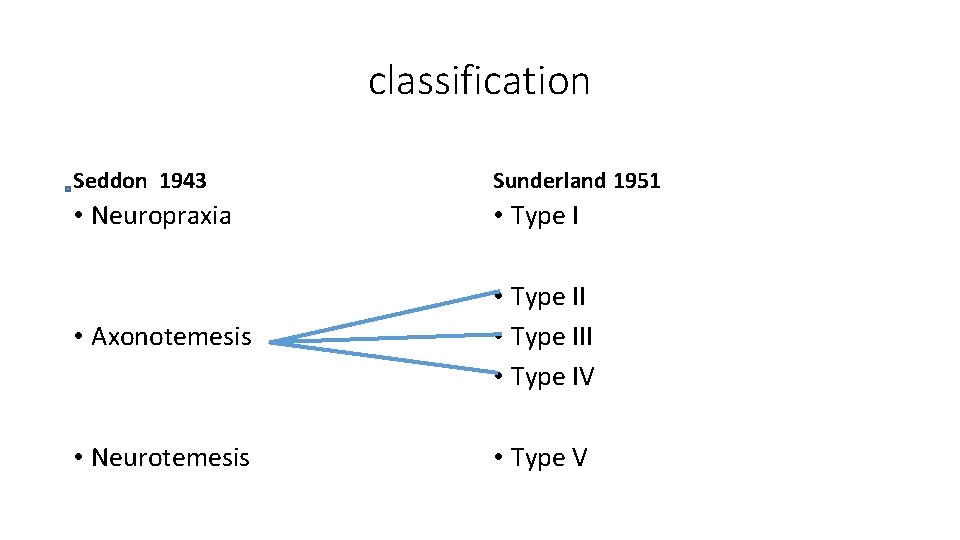
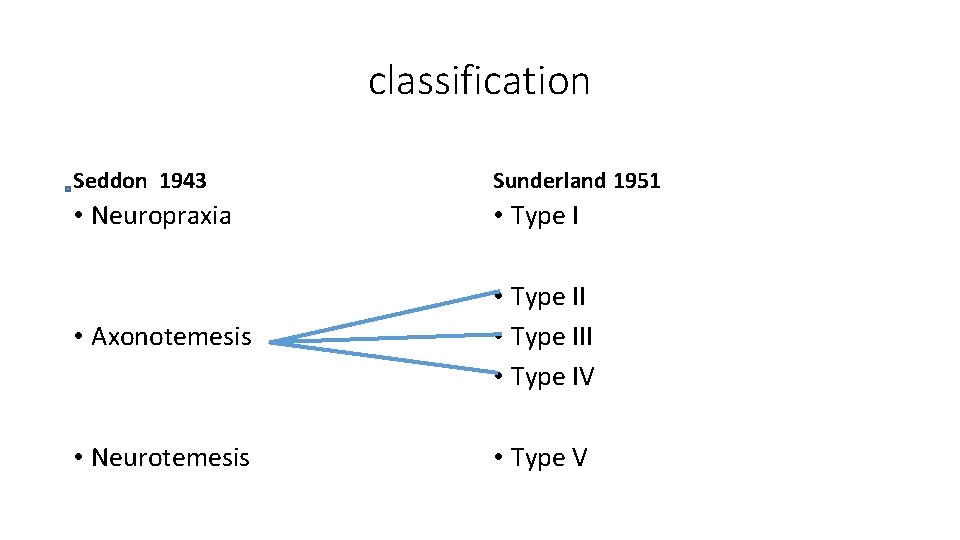
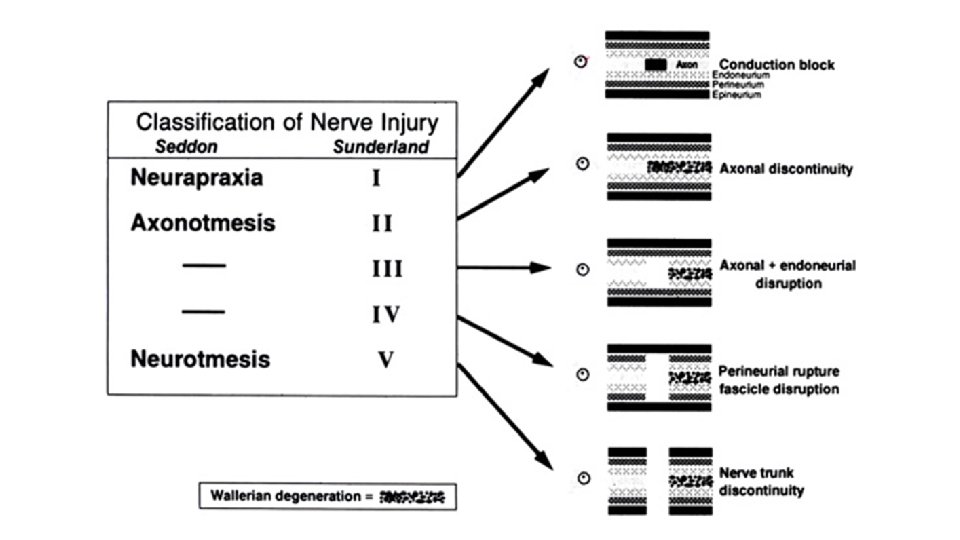
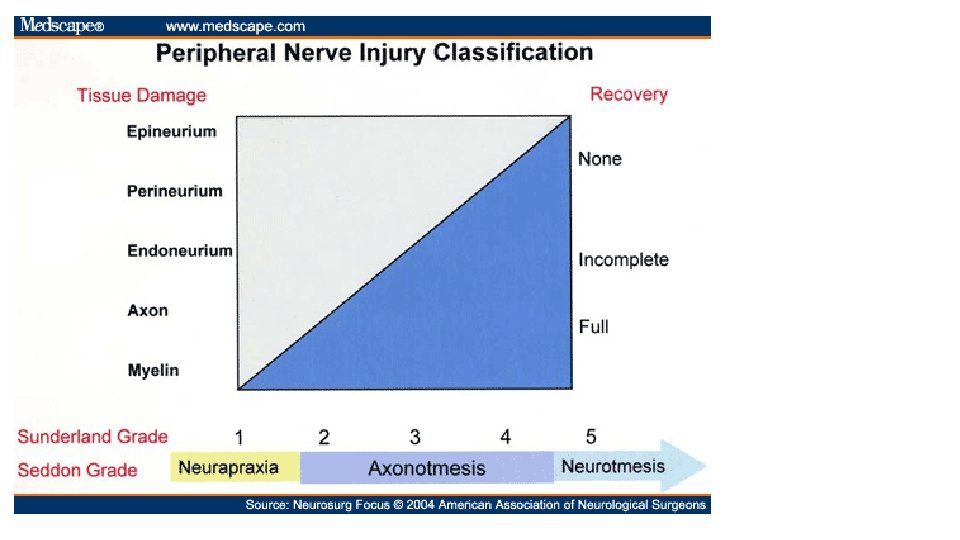
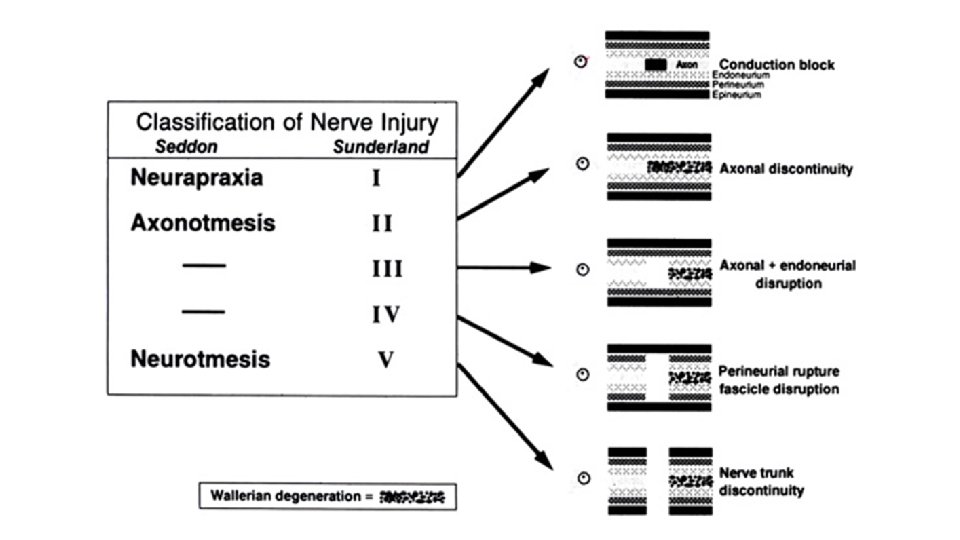
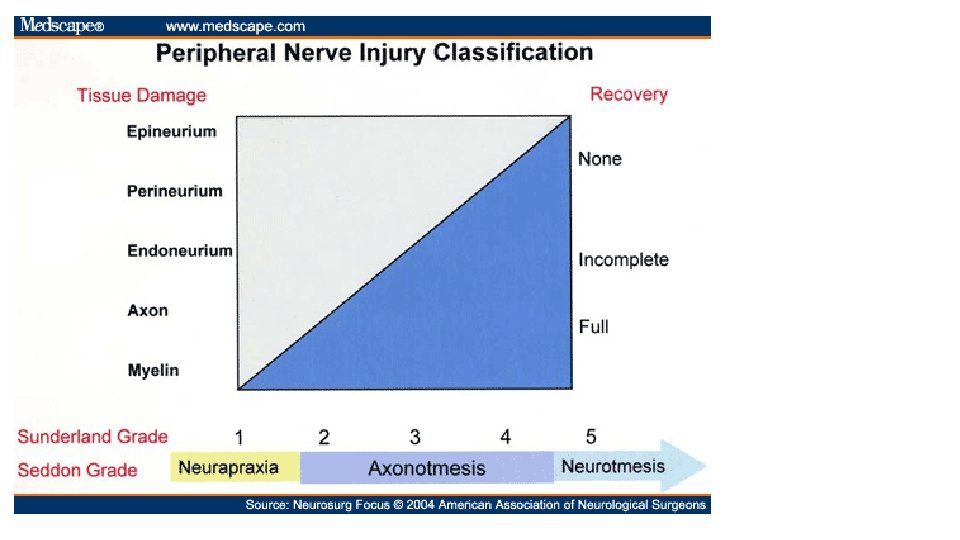
classification Seddon 1943 Sunderland 1951 • Neuropraxia • Type I • Axonotemesis • Type III • Type IV • Neurotemesis • Type V
Classification Seddon (neuropraxia) === Sunderland (type I) • Interruption of conduction at site of injury • Axon preserved • No wallerian degeneration • Motor fibers more susceptible to injury than sensory fibers
Classification Seddon (neuropraxia) === Sunderland (type I) • Large myelinated fibers more susceptible than fine or nonmyelinated fibers • Electrophysiologic Studies • NCV slowing or complete conduction block
Classification Seddon (neuropraxia) === Sunderland (type I) • Complete functional recovery after 1 st degree injuries because axonal continuity preserved and changes responsible for the conduction loss are fully reversible • Full restoration of function may take as long as 3 to 4 months after the injury
Classification Seddon (axonotemesis) === Sunderland (type II) • Axon and myelin sheath disruption … leads to conduction block with Wallerian degeneration • Endoneurium, perineurium and epineurium intact • Axon regenerates along intact endoneurial tube
Classification Seddon (axonotemesis) === Sunderland (type II) • Complete loss of motor and sensory functions • Complete functional recovery expected • Time to recovery depends on severity and level of injury, as axons must regenerate distally • Usually months to recovery
Classification Seddon (axonotemesis) === Sunderland (type III) • Axons and endoneurial tube disrupted • Perineurium and epineurium intact • Complete loss of function • Onset of recovery delayed longer due to more severe retrograde injury to cell bodies, fibrosis • With longer delays in recovery, target organs may undergo changes that prevent full recovery
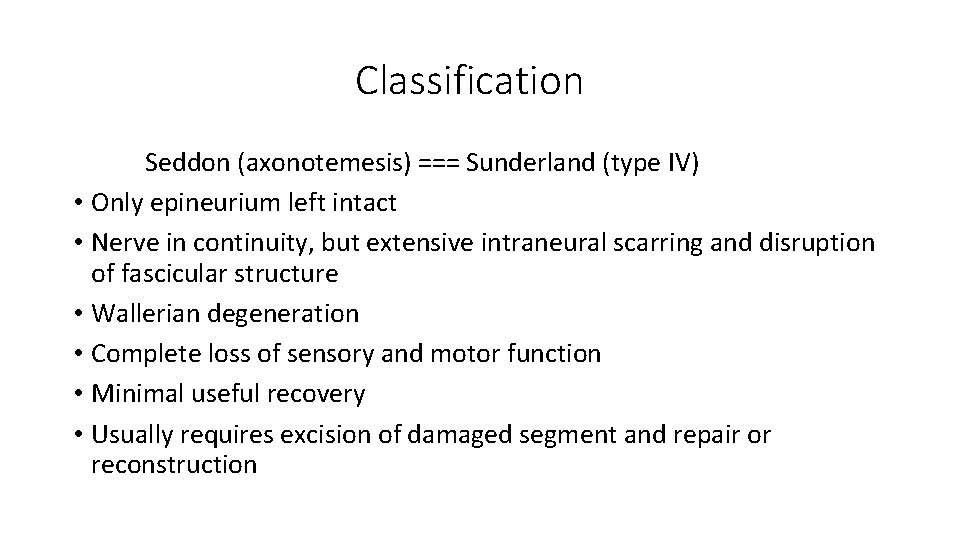
Classification Seddon (axonotemesis) === Sunderland (type IV) • Only epineurium left intact • Nerve in continuity, but extensive intraneural scarring and disruption of fascicular structure • Wallerian degeneration • Complete loss of sensory and motor function • Minimal useful recovery • Usually requires excision of damaged segment and repair or reconstruction
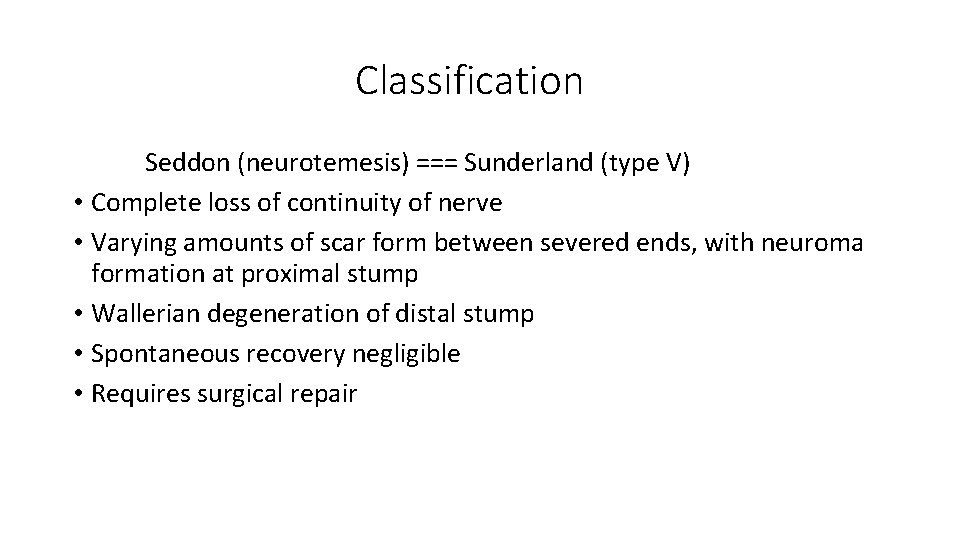
Classification Seddon (neurotemesis) === Sunderland (type V) • Complete loss of continuity of nerve • Varying amounts of scar form between severed ends, with neuroma formation at proximal stump • Wallerian degeneration of distal stump • Spontaneous recovery negligible • Requires surgical repair
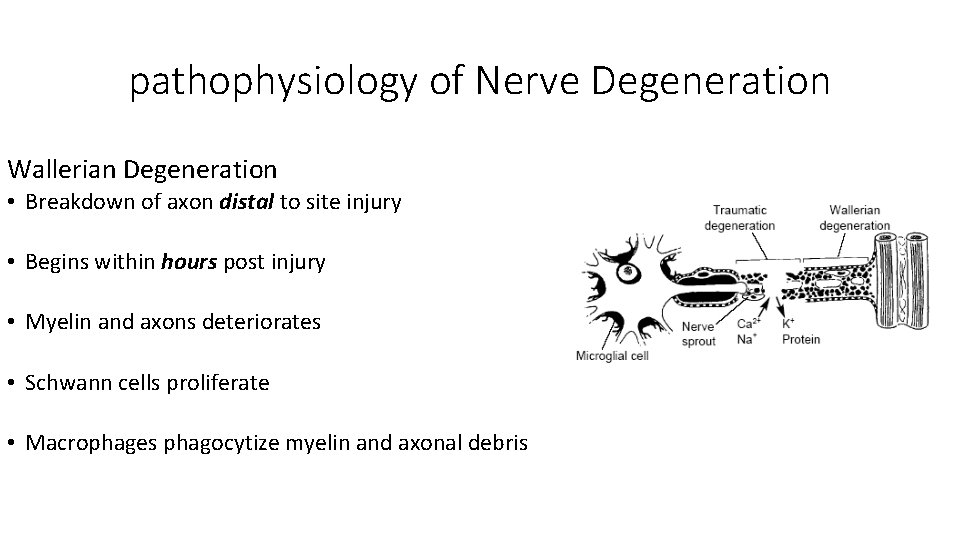
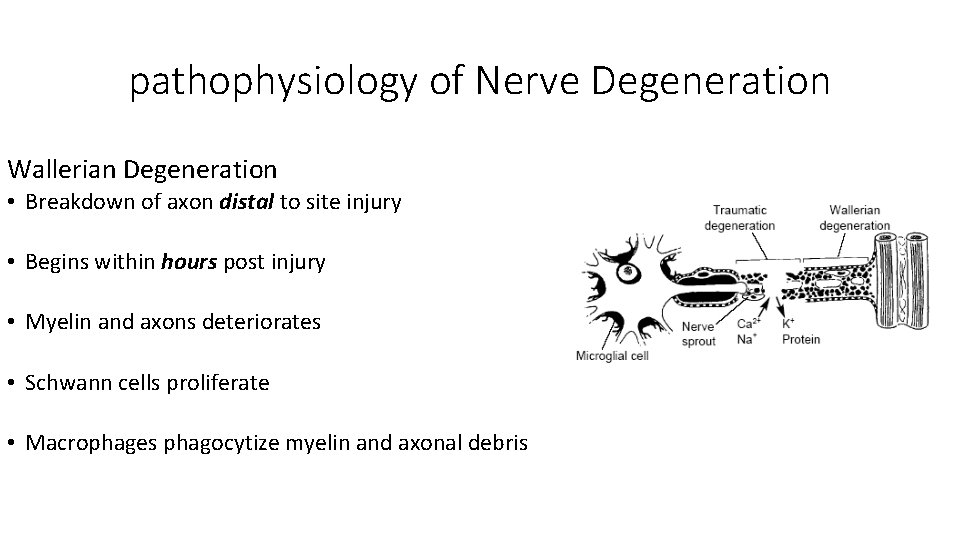
pathophysiology of Nerve Degeneration Wallerian Degeneration • Breakdown of axon distal to site injury • Begins within hours post injury • Myelin and axons deteriorates • Schwann cells proliferate • Macrophages phagocytize myelin and axonal debris
Pathophysiology of Entrapment Neuropathy • Most accepted theories of nerve pathophysiology from compression involve ischemia and altered axonal transport. • damage to the blood–nerve barrier • followed by endoneurial edema and perineural thickening, which alter the microcirculation. • With continued compression, demyelination occurs and axons begin to degenerate,
Pathophysiology of Nerve Regeneration • Rate of regeneration varies depending on the type & location • In humans, an average outgrowth of 1 -2 mm/day is generally quoted • Proximal budding occurs after 1 month delay
Functional Recovery after Nerve Injury Clinical outcomes variable and related to: 1. AGE – single most important factor 2. Level of injury - distance regenerating axons must go to reach target organs, distal > prox 3. Length of injury zone 4. Type of injury – sharp transection > crush 5. Timing of nerve repair 6. Status of end organ at time of re-innervation 7. Technical expertise of surgeon
Level of Injury • In cases of laceration the site or the level of injury is easy • The problem comes with • Closed injuries • Entrapment neuropthies
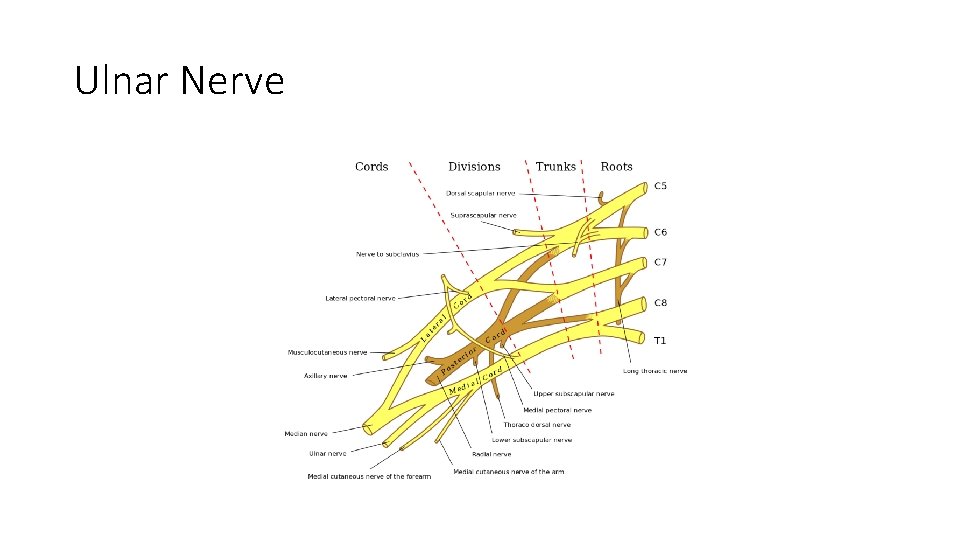
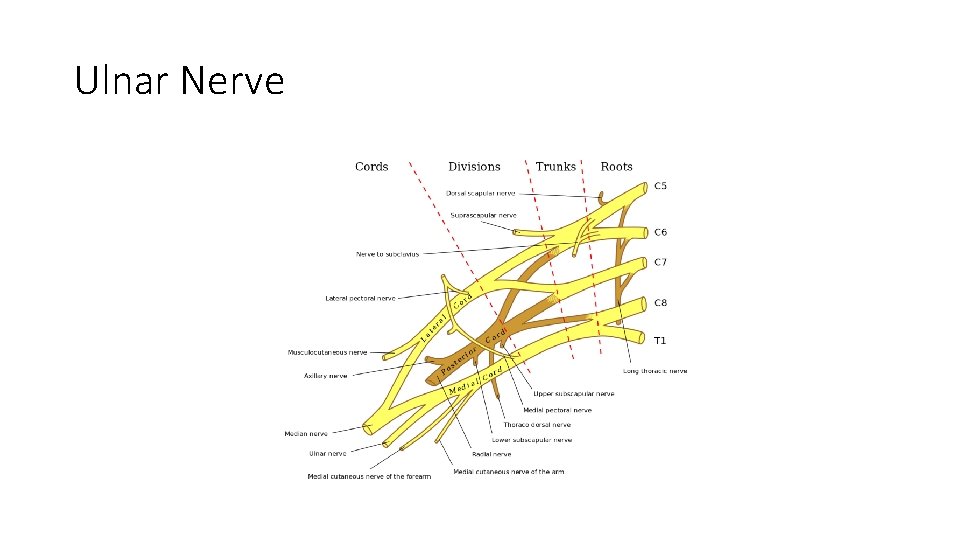
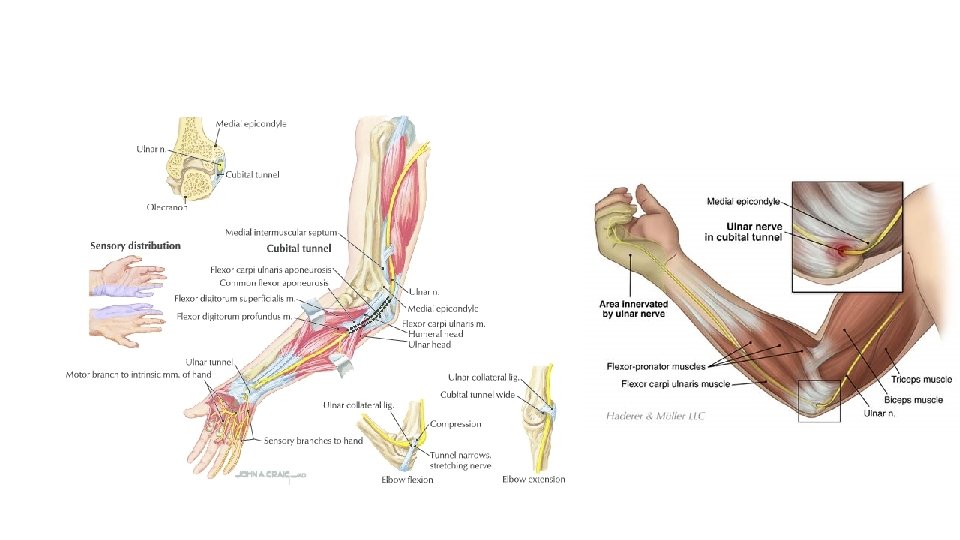
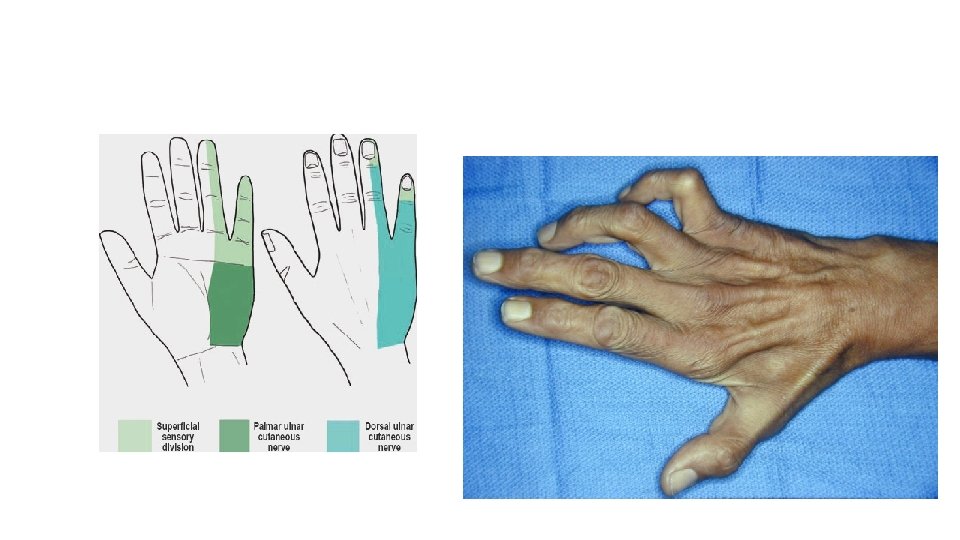
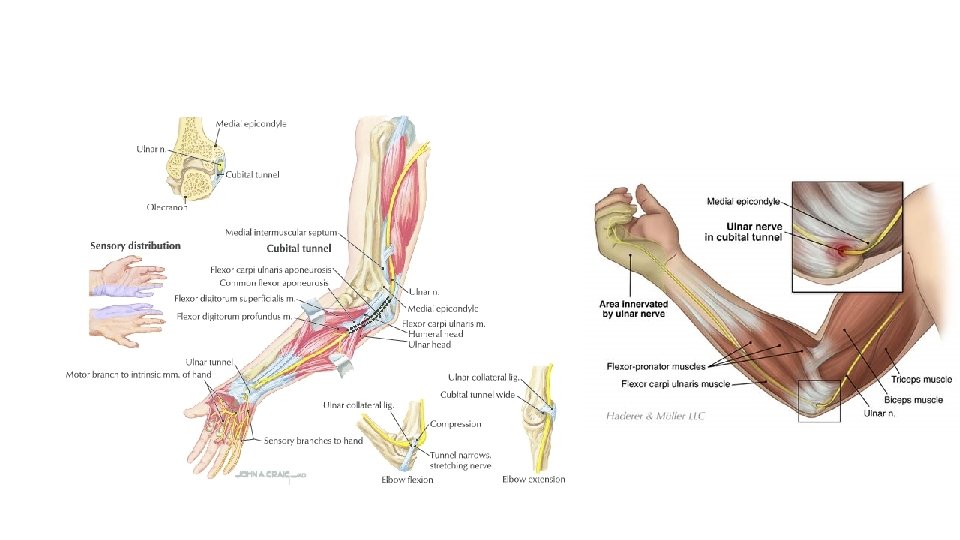
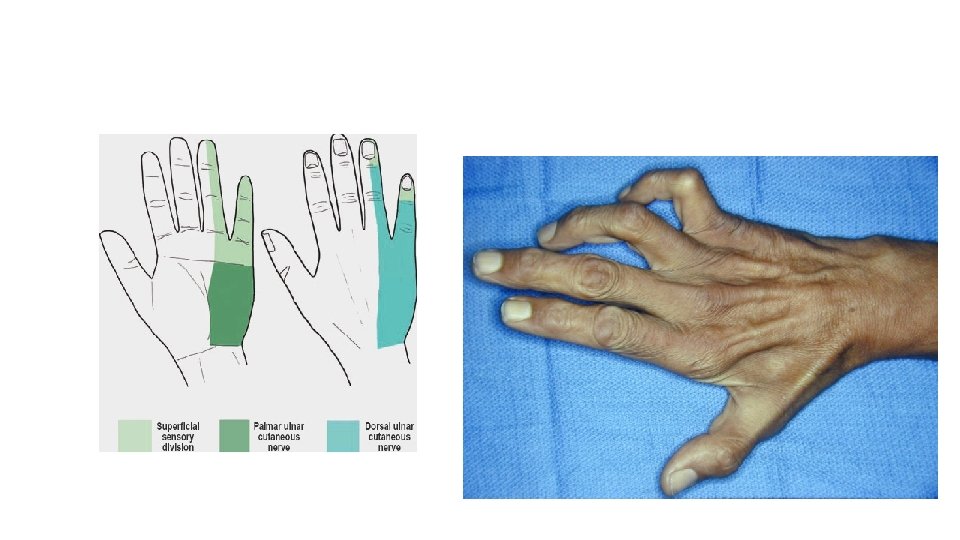
Ulnar Nerve
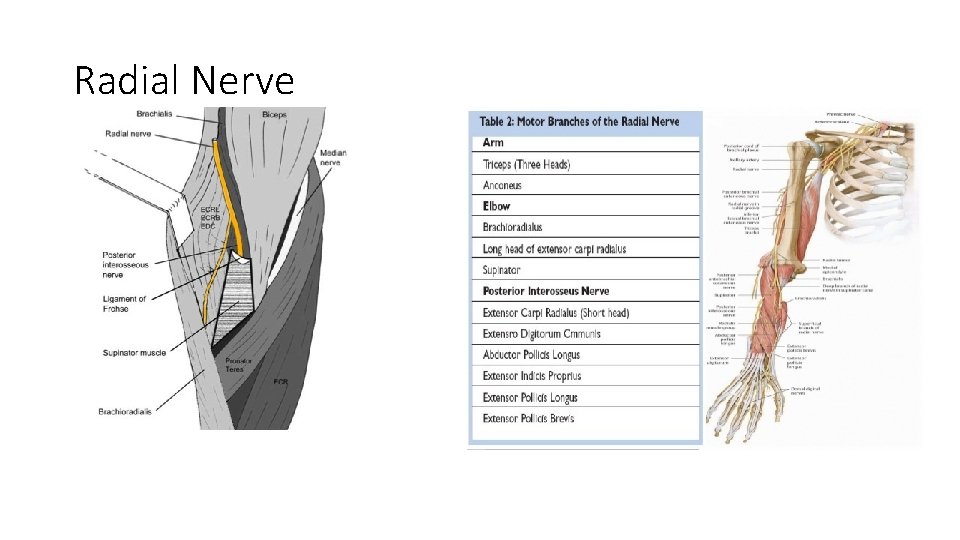
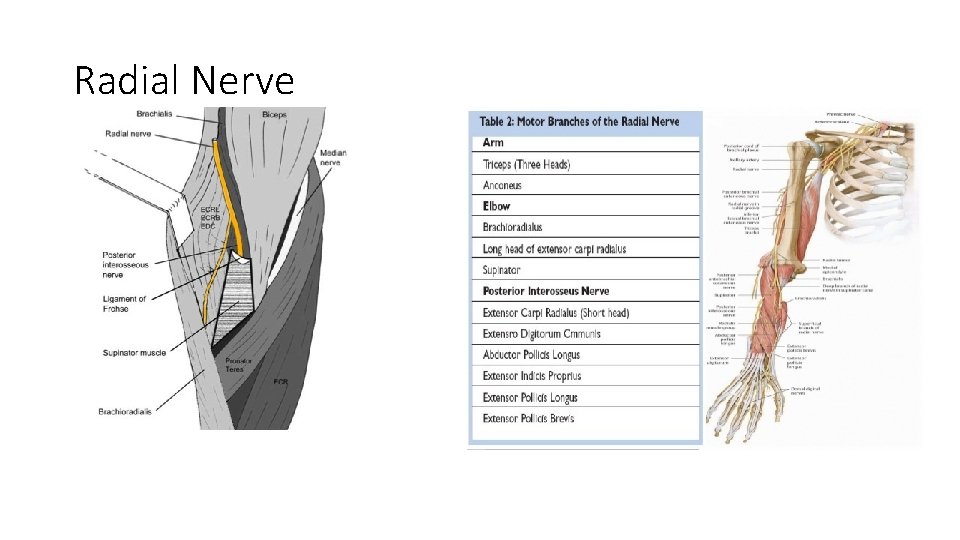
Radial Nerve
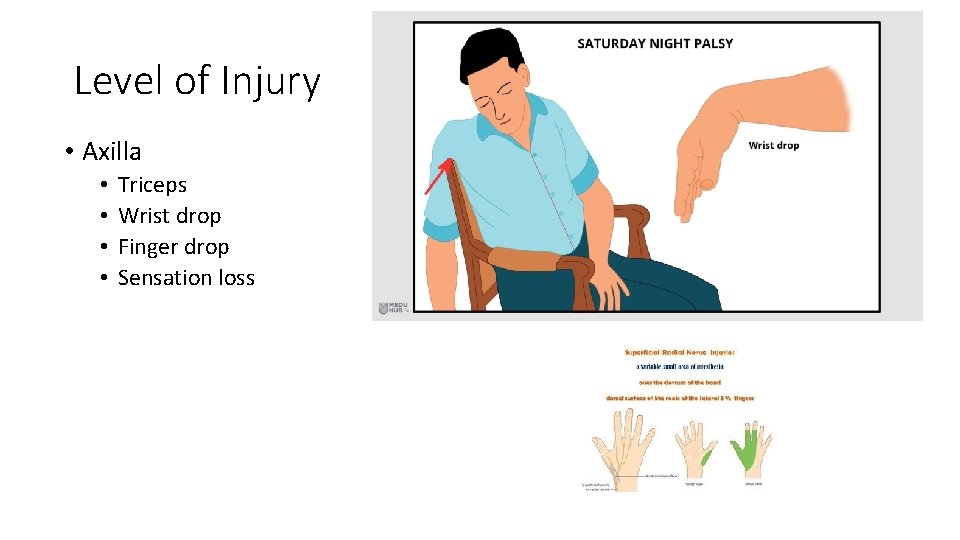
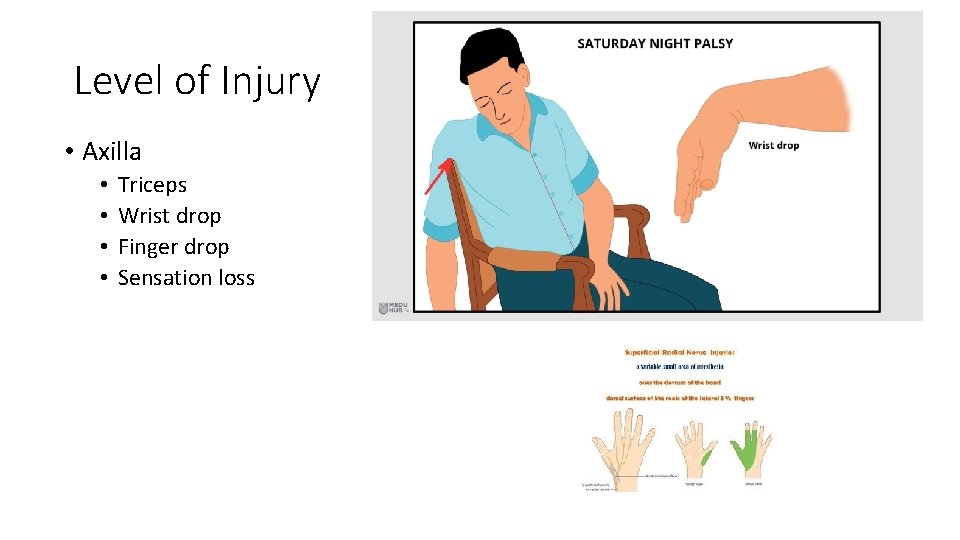
Level of Injury • Axilla • • Triceps Wrist drop Finger drop Sensation loss
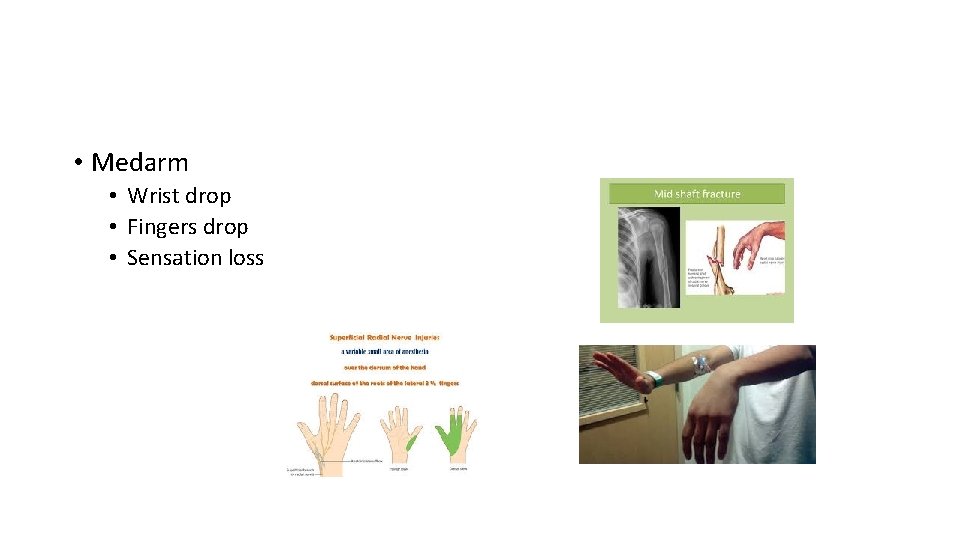
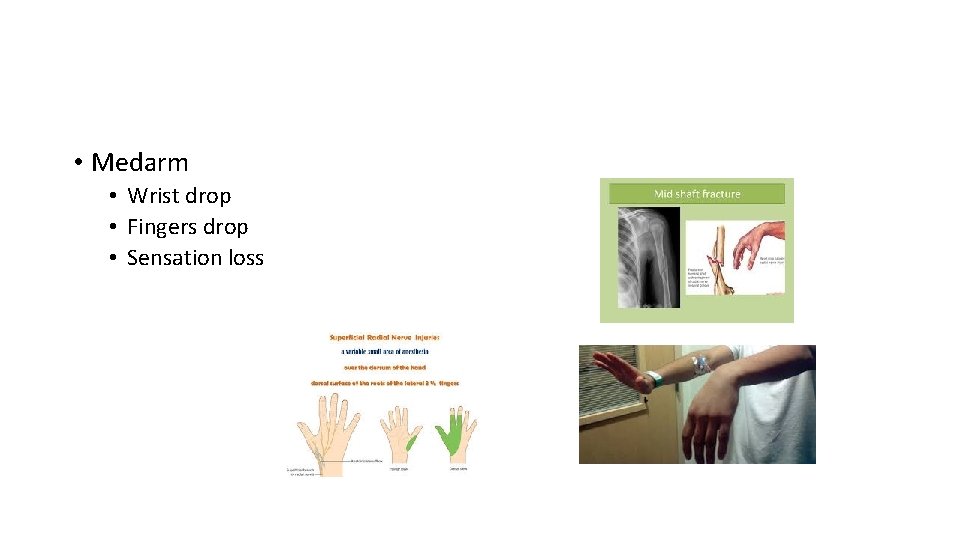
• Medarm • Wrist drop • Fingers drop • Sensation loss
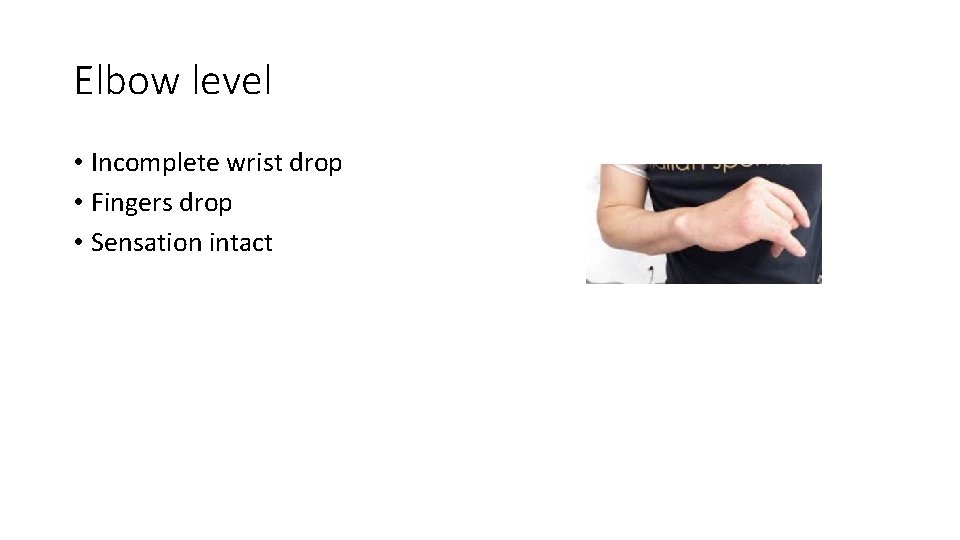
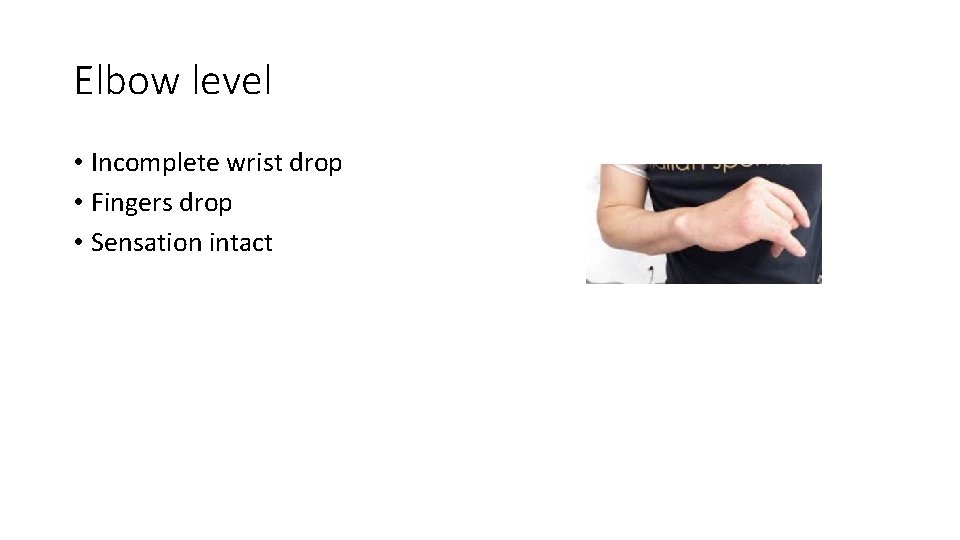
Elbow level • Incomplete wrist drop • Fingers drop • Sensation intact
Indication for Surgery • Failure of recovery within 3 months • Cases with definit nerve injury • • • Laceration Gunshot Crush injury Iatrogenic Post reduction • Chronic nerve injury with painful neuroma

Timing of Surgery • Role of 3 • Primary repair: within 3 days • Delayed primary repair: within 3 weeks • Delayed repair: 3 months Time limit for repair is 18 months +/-

Primary Repair • Clean wound • Sharp cut • No other complicated injuries
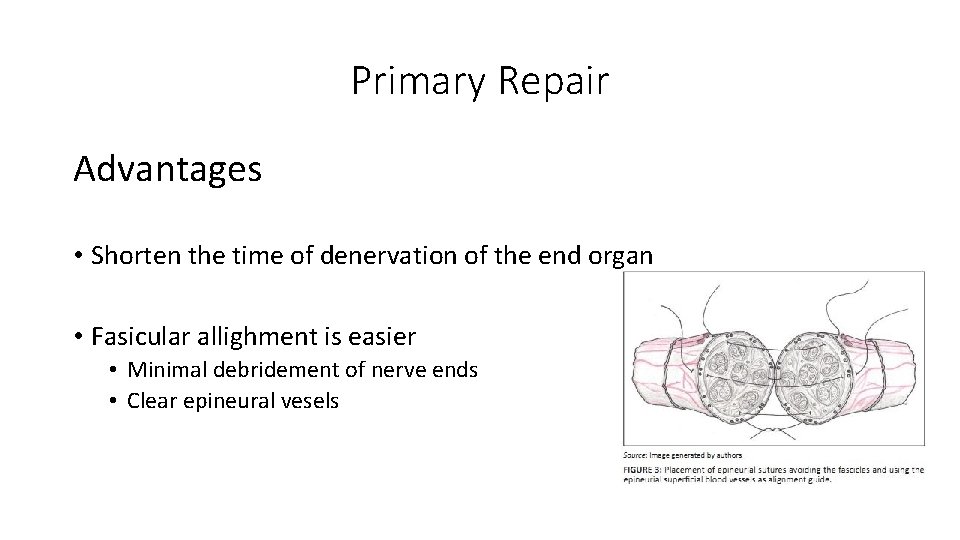
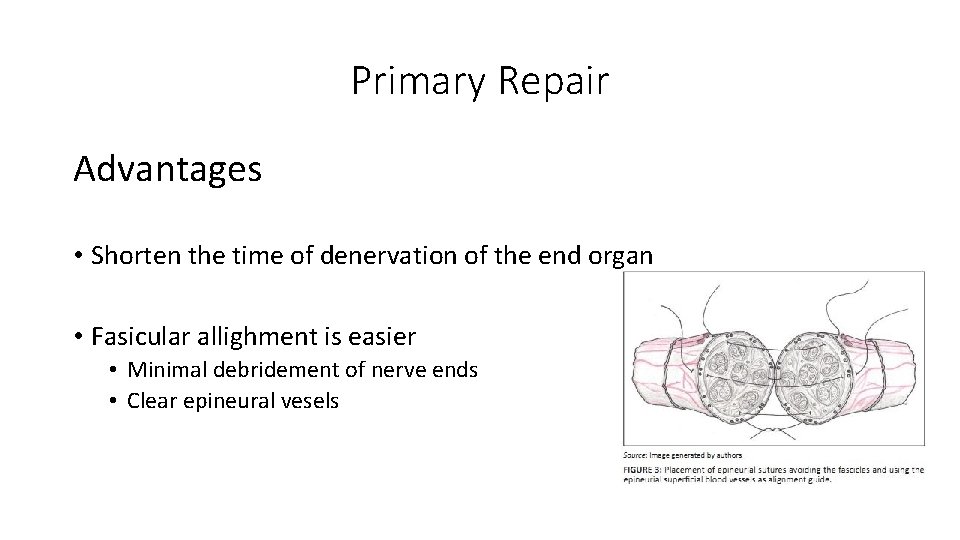
Primary Repair Advantages • Shorten the time of denervation of the end organ • Fasicular allighment is easier • Minimal debridement of nerve ends • Clear epineural vesels

Delayed Primary Repair 3 weeks • Untidy wounds: uncertain how much is the damage • Crush injury • gunshot • Debride, debride … nerve repair • May need a graft
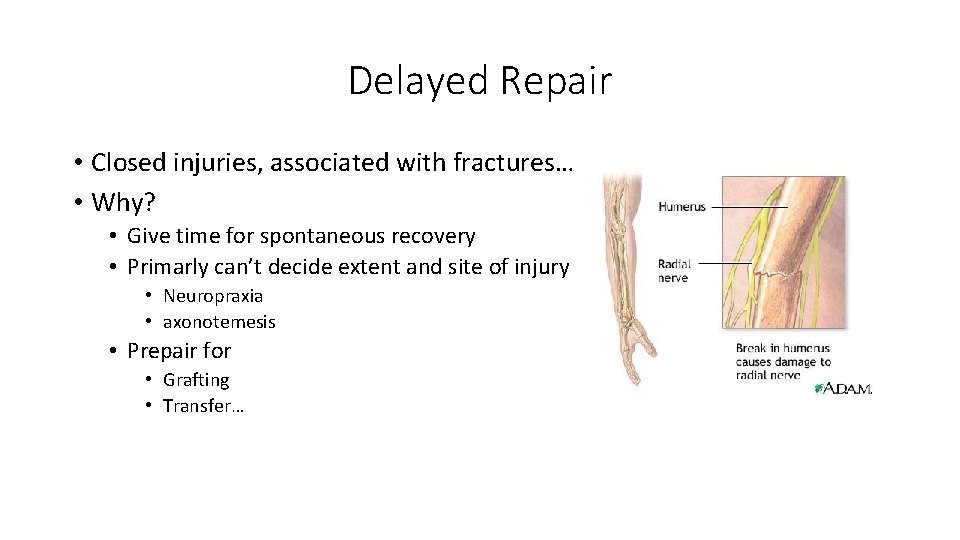
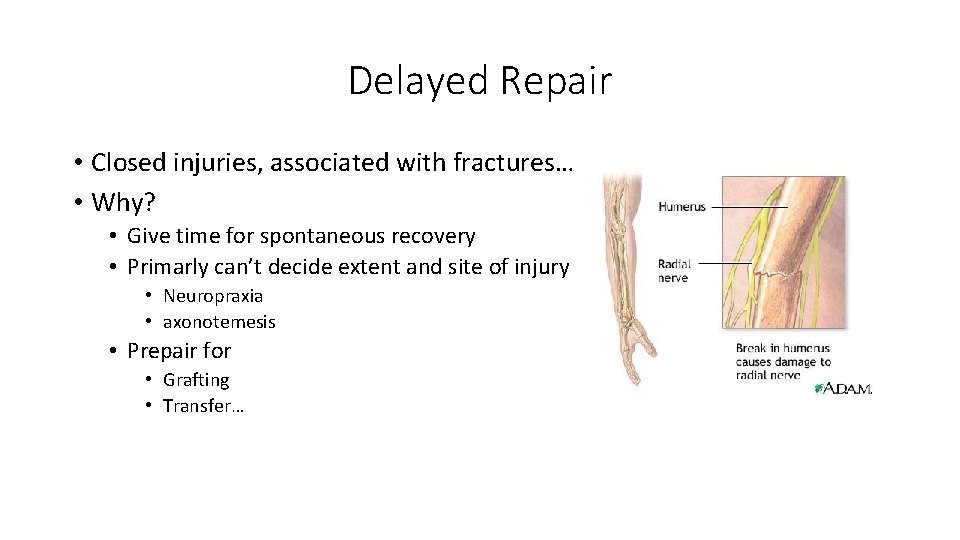
Delayed Repair • Closed injuries, associated with fractures… • Why? • Give time for spontaneous recovery • Primarly can’t decide extent and site of injury • Neuropraxia • axonotemesis • Prepair for • Grafting • Transfer…
Types of Nerve Repair • Neurorraphy • Epineurial repair • Perineurial repair • Epiperineurial repair • Fasiculr repair
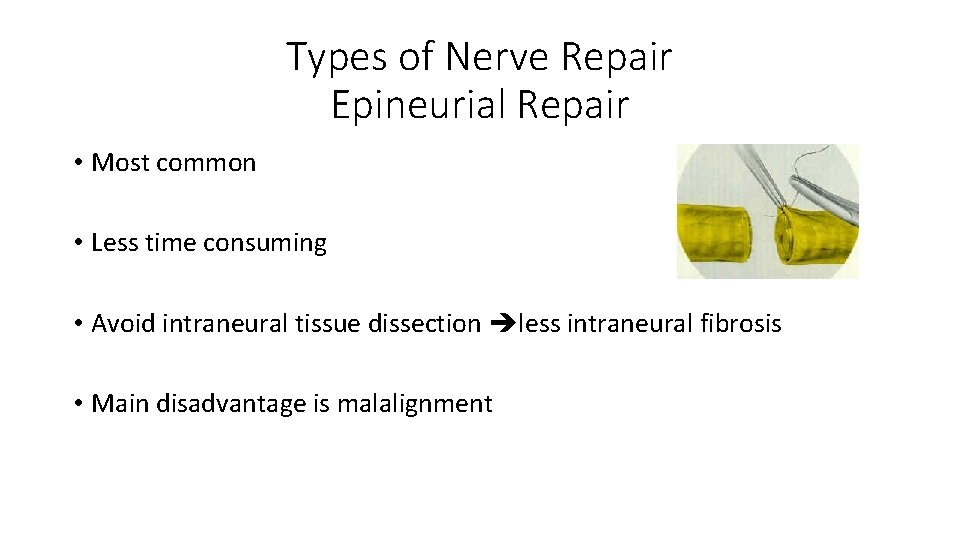
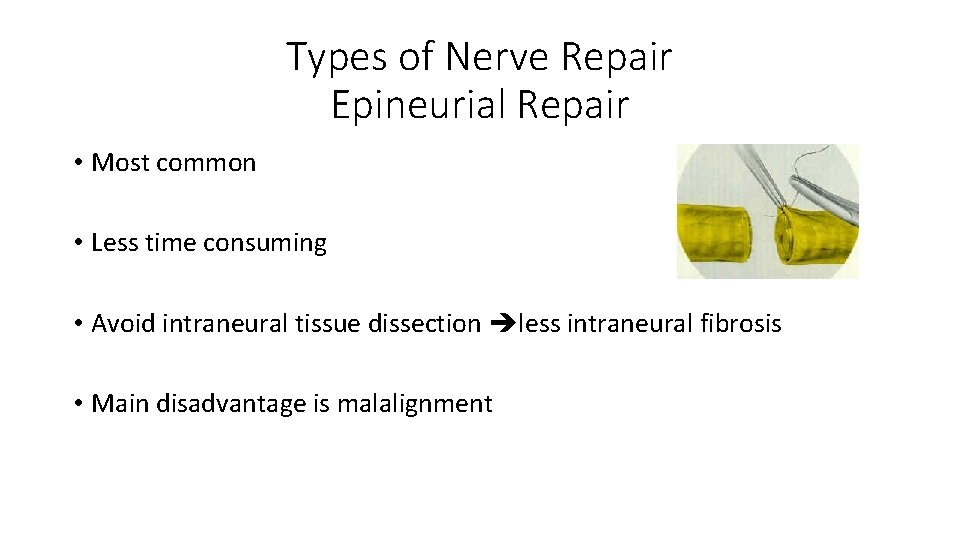
Types of Nerve Repair Epineurial Repair • Most common • Less time consuming • Avoid intraneural tissue dissection less intraneural fibrosis • Main disadvantage is malalignment
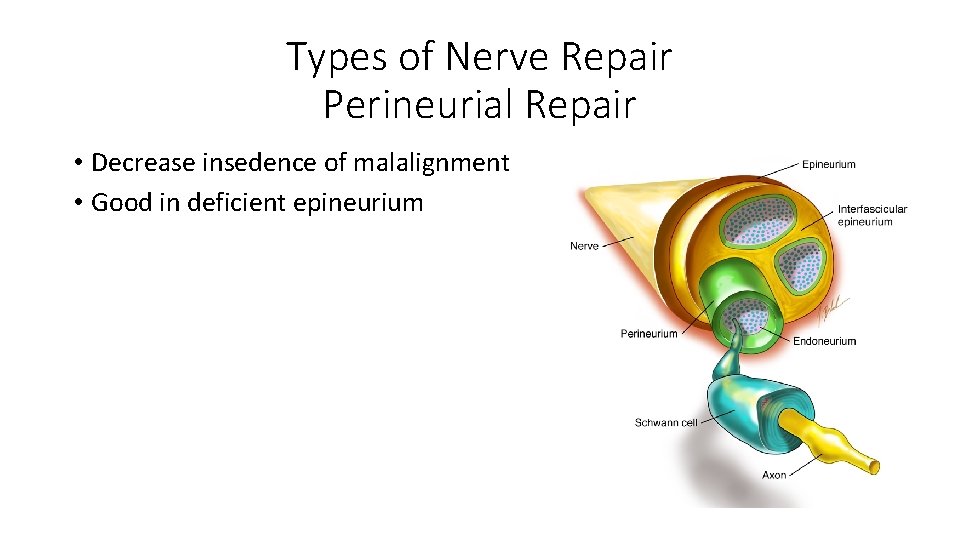
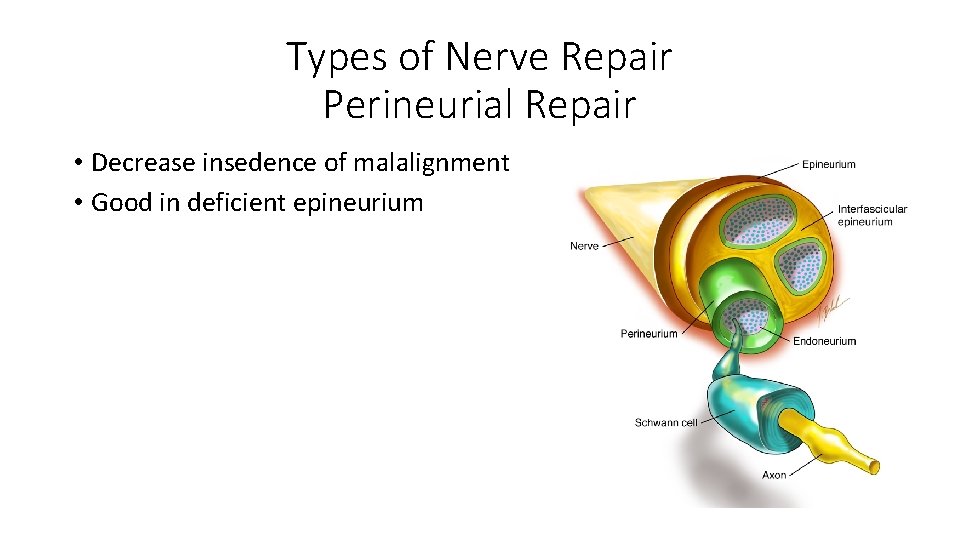
Types of Nerve Repair Perineurial Repair • Decrease insedence of malalignment • Good in deficient epineurium
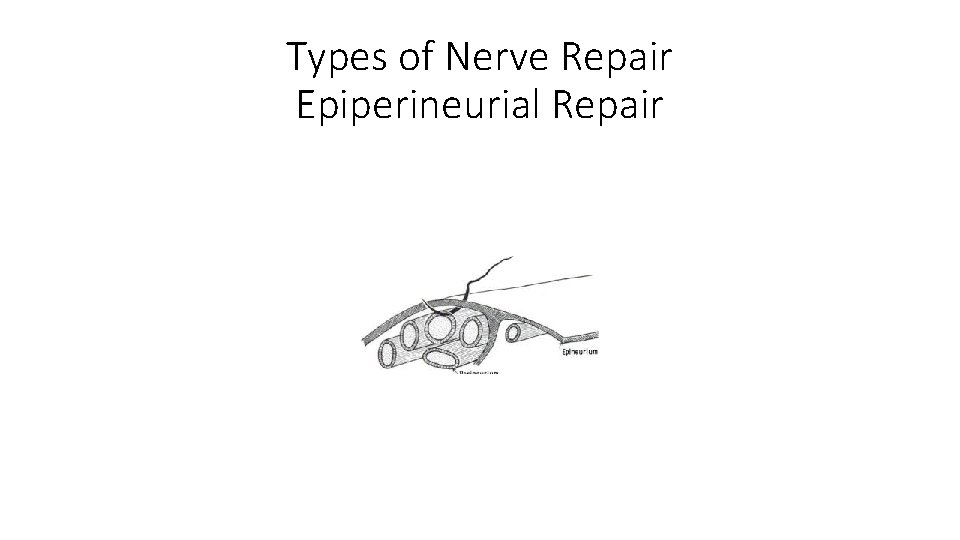
Types of Nerve Repair Epiperineurial Repair
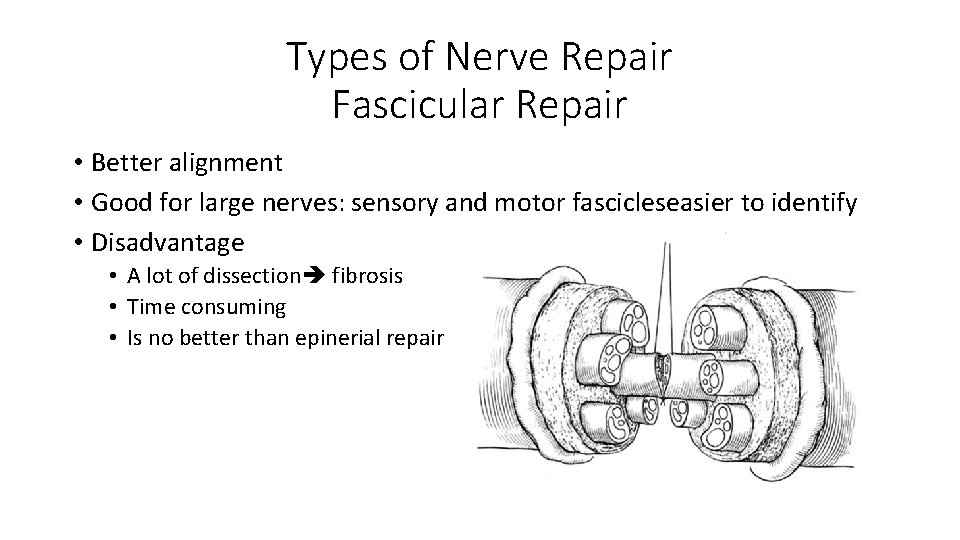
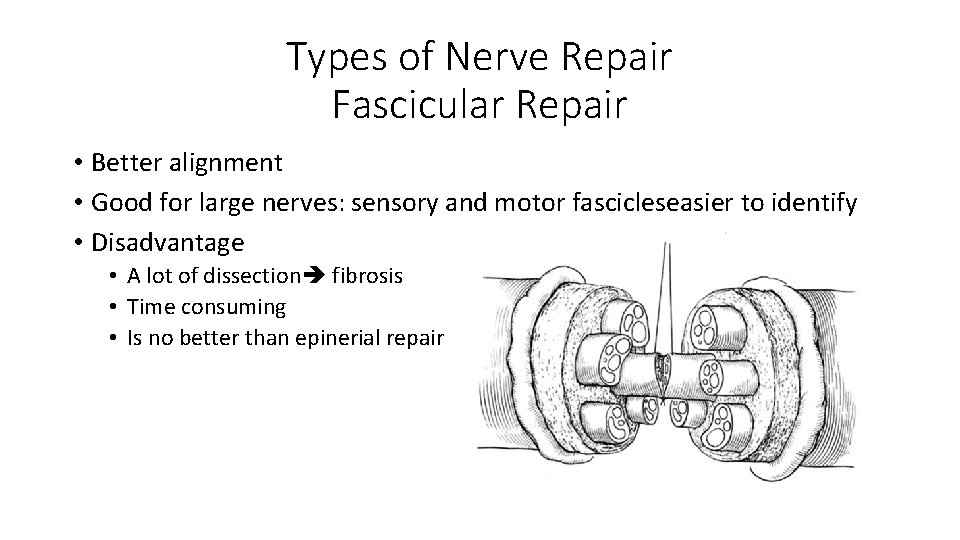
Types of Nerve Repair Fascicular Repair • Better alignment • Good for large nerves: sensory and motor fascicleseasier to identify • Disadvantage • A lot of dissection fibrosis • Time consuming • Is no better than epinerial repair
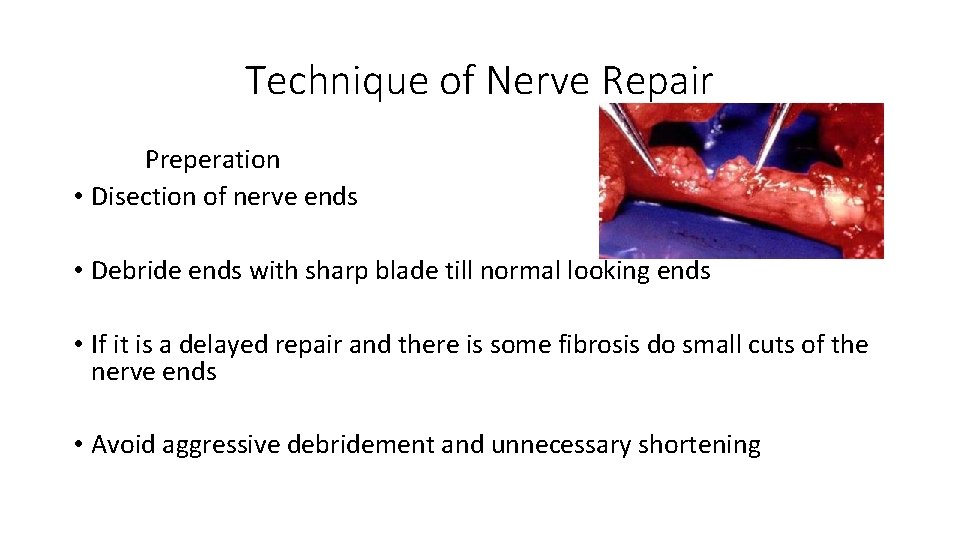
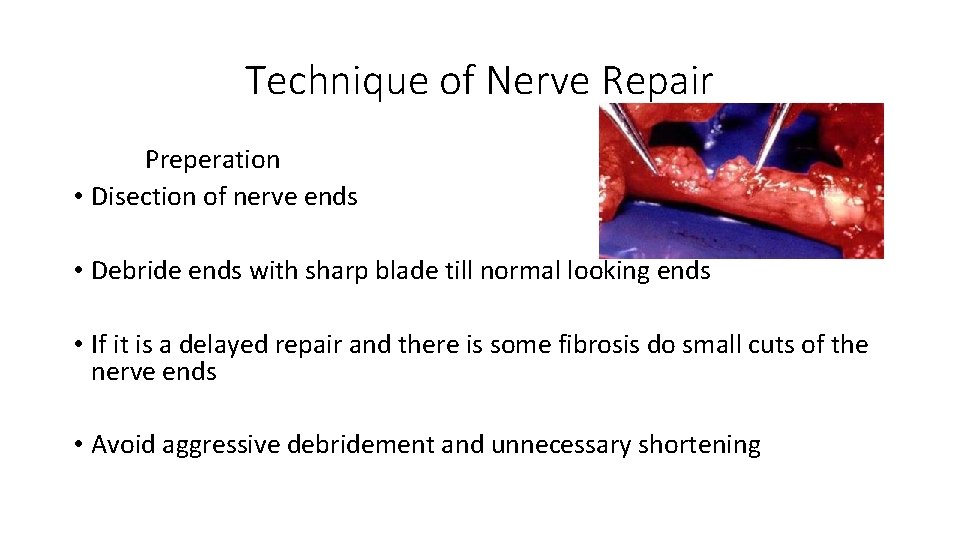
Technique of Nerve Repair Preperation • Disection of nerve ends • Debride ends with sharp blade till normal looking ends • If it is a delayed repair and there is some fibrosis do small cuts of the nerve ends • Avoid aggressive debridement and unnecessary shortening
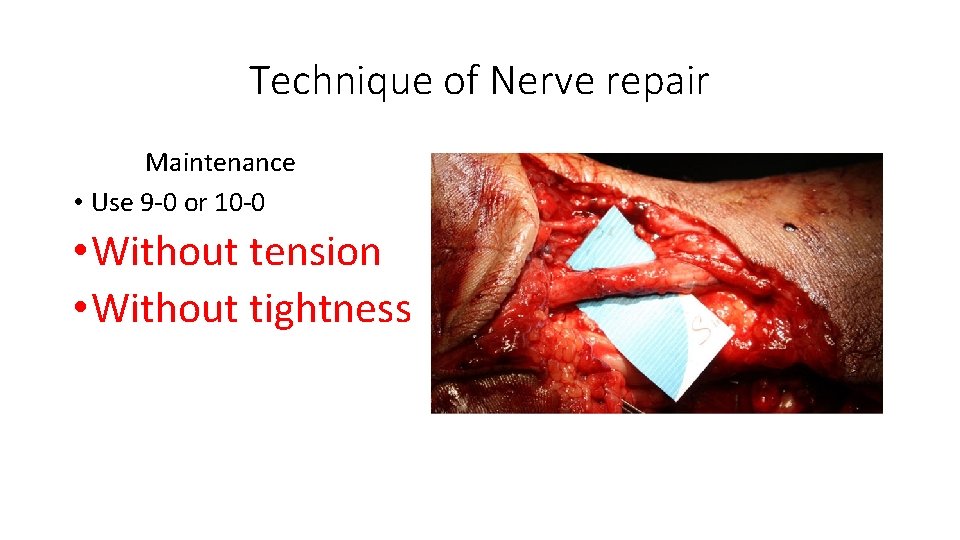
Technique of Nerve repair Approximation • Disection of nerve ending leaving a minimal gap • During approximation avoid extensive intrafasicular dissection Alignment • Blood vesels should be aligned
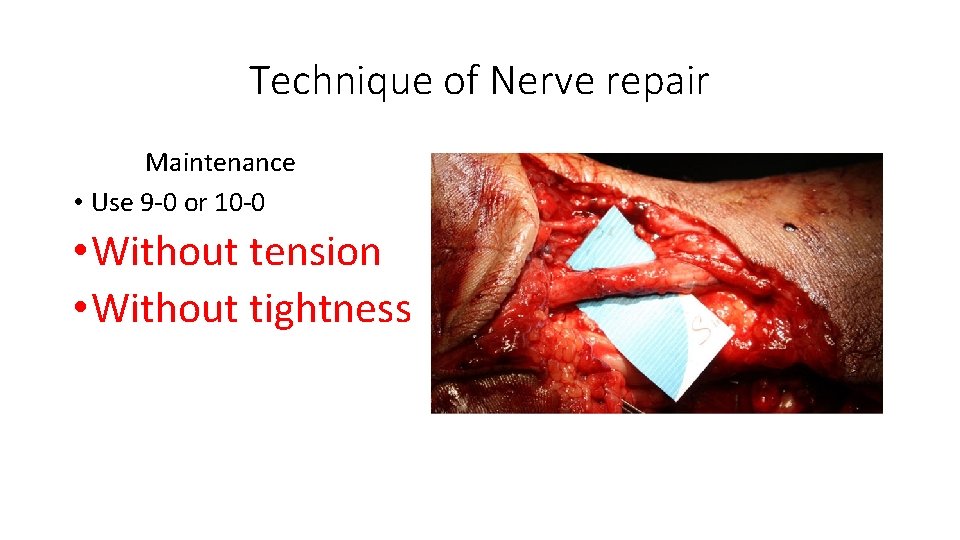
Technique of Nerve repair Maintenance • Use 9 -0 or 10 -0 • Without tension • Without tightness
Technique of Nerve Repair Tension • Encourages gapping and scar formation • Reduces blood flow: 8% elongation = 46% decrease in perfusion • Grafting better than repair in tension (autografts)
Technique of Nerve Repair Avoiding tension • Disection of the nerve • Nerve transposition • Joint flexion • Bone shortening
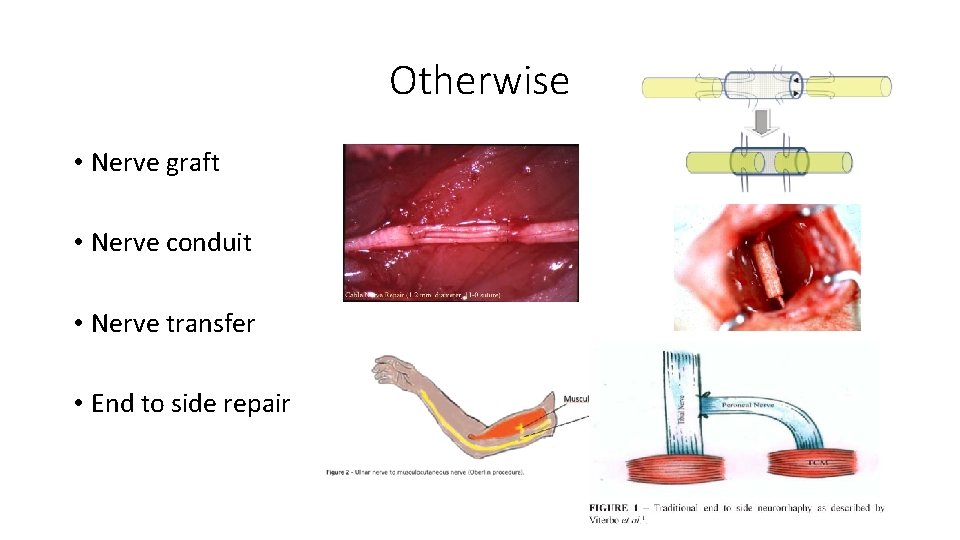
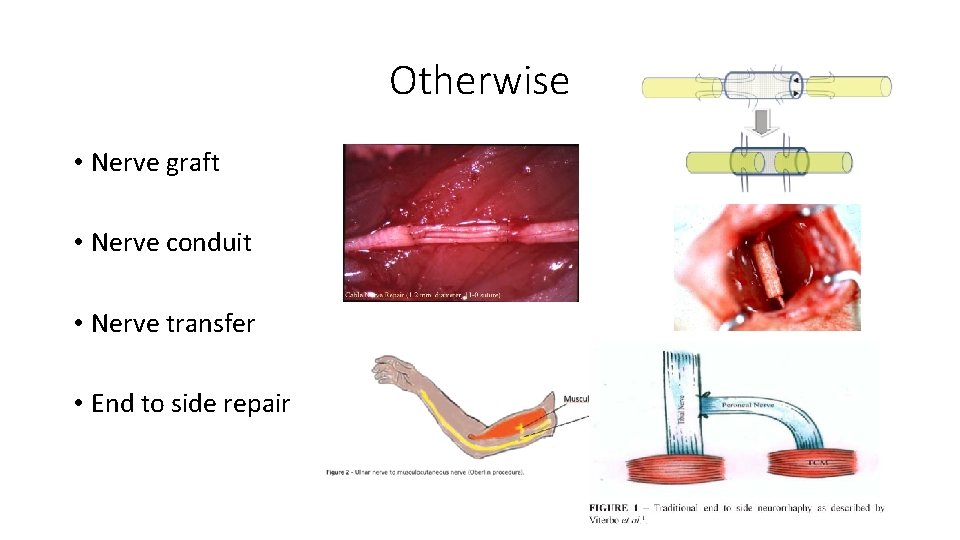
Otherwise • Nerve graft • Nerve conduit • Nerve transfer • End to side repair
Functional Recovery after Nerve Injury Clinical outcomes variable and related to: • • AGE – single most important factor Level of injury - distance regenerating axons must go to reach target organs, distal > prox Length of injury zone Type of injury – sharp transection > crush Timing of nerve repair Status of end organ at time of re-innervation Technical expertise of surgeon
Why Is Regeneration Incomplete After Repair? • Recovery and regeneration takes months axon-motor/sensory atrophy and never recover completely • Regeneration should cross anastomosis ? ? ? Scaring • malalignment especialy in mixed nerves • Long time of muscle denervation atrophy

QUESTIONS