periodontics Dental Stains LEC 9 Pigmented deposits on
- Slides: 6
periodontics Dental Stains LEC. 9 Pigmented deposits on the tooth surface are called dental stains. Stains are primarily an aesthetic problem and do not cause inflammation of the gingiva. The use of tobacco products, coffee, tea, certain mouthrinses and pigments in foods can contribute to stain formation. They should be carefully examined to determine their origin. Teeth are typically composed of a number of colors and a gradation of color occurs in an individual tooth from the gingival margin to the incisal edge of the tooth. The gingival margin often has a darker appearance because of the close approximation of the dentine below the enamel. In most people canine teeth are darker than central and lateral incisors and younger people characteristically have lighter teeth, particularly in the primary dentition. Teeth become darker as a physiological age change, this may be partly caused by the laying down of secondary dentine, incorporation of extrinsic stains and gradual wear of enamel allowing a greater influence on color of the underlying dentine. Also, and to be discussed further, tooth wear and gingival recession can directly or indirectly affect tooth color. Classification of tooth discoloration: The coronal portion of the tooth consists of enamel, dentine and pulp. Any change to these structures is likely to cause an alteration in the outward appearance of the tooth caused by its light transmitting and reflecting properties. Historically, tooth discoloration has been classified according to the location of the stain, which may be either intrinsic or extrinsic. 1. Extrinsic discoloration: Which arising from the accumulation of exogenous pigment, it is outside the tooth substance and lies on the tooth surface or in the acquired pellicle. The origin of the stain may be: A. Non-metallic B. Metallic 2. Intrinsic discoloration: Which occur secondary to endogenous factors that lead to discoloration of the underlying dentin, occurs following a change to the structural composition or thickness of the dental hard tissues. The normal color of teeth is determined by the blue, green and pink tints of the enamel and is reinforced by the yellow through to brown shades of dentine . ﺩ
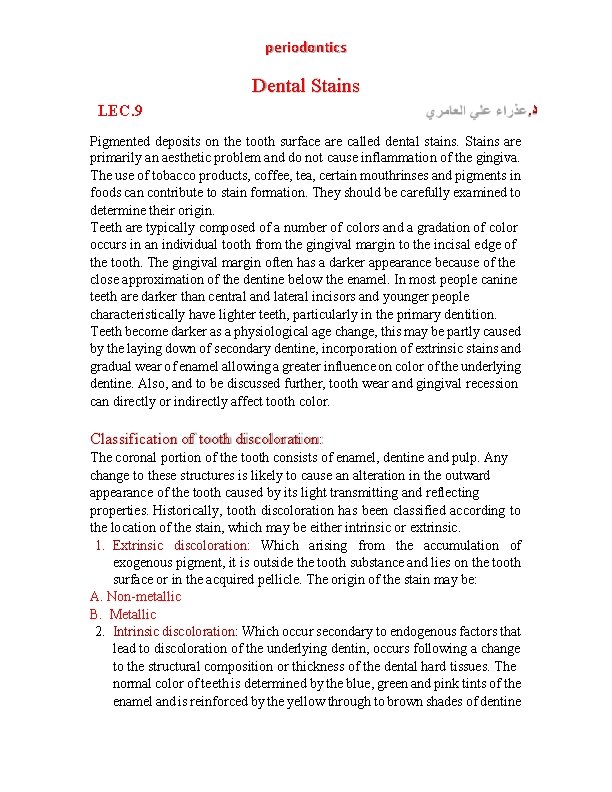
periodontics beneath. A number of metabolic diseases and systemic factors are known to affect the developing dentition and cause discoloration as a consequence. It classified to: A. Developmental defects B. Acquired defects 1. Extrinsic discoloration A. Non-metallic 1. Brown stains: are a very common type of stain that is bacteria free; these stains are usually due to a thin pigmented pellicle which is found most commonly on the buccal surface of maxillary molars and the lingual surfaces of lower anterior teeth. It is caused by the deposition of tannin (in chromatic beverages) and is generally associated with insufficient brushing. 2. Tobacco stains: It is dark brown/ black discoloration, mainly caused by deposition of the tar and mainly penetrate the pits and fissures of enamel. This stain does not entirely depend on the amount of tobacco consumed, but rather the amount of preexisting coating and roughened enamel that will eventually allow tobacco products to adhere which is found most commonly on the lingual surfaces of lower anterior teeth. 3. Black stain: is a thin black line, firmly attaches, tends to recur, common in woman, may occur in excellent hygiene. Near a gingival margin of facial and lingual surfaces. Diffuse patch on the proximal surface may be seen. It is caused by chromogenic bacteria e. g. G (+ve) rods Actinomyces species. 4. Green stains: frequently occur in children, affecting boys more than girls, and appears as a thick green or greenish yellow band on the facial surface of maxillary anterior teeth in the gingival third. Some believe it is a remnant of the primary enamel cuticle. Others suggest it could be due to fluorescent bacteria-Penicillium and fungi-Aspergillus. Photoactivation is essential for this type of bacteria which explains their presence on maxillary anterior teeth. 5. Orange stains: are the least common. They occur on the labial surface of the upper and lower anterior teeth, mainly caused by bacteria as Serratia marcescens, Flavobacterium lutescen and associated with poor oral hygiene.
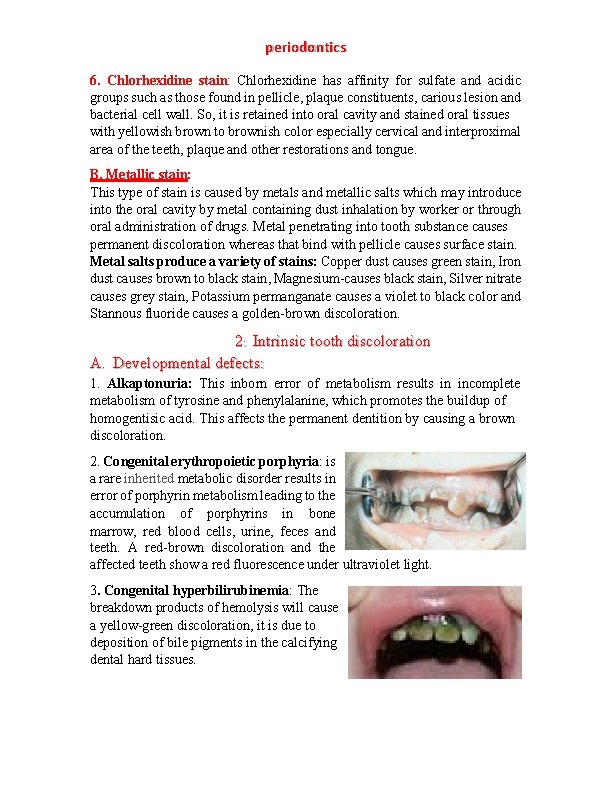
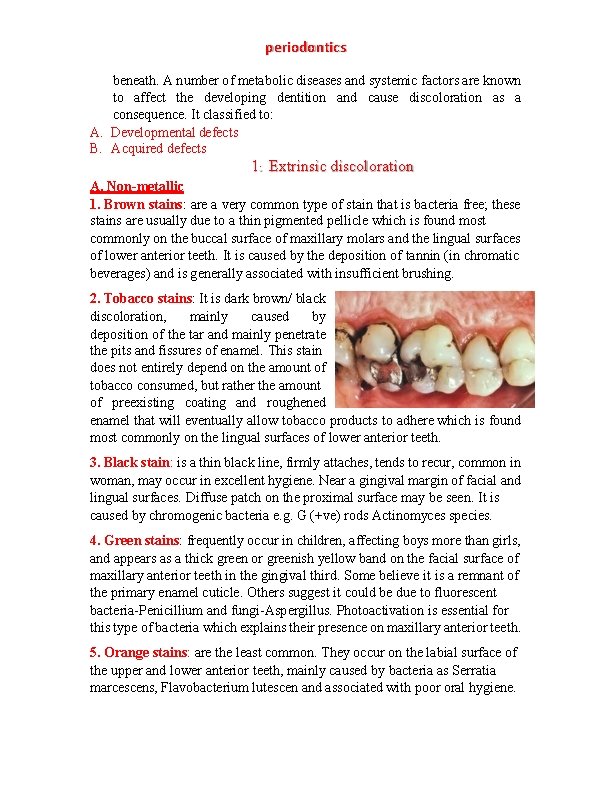
periodontics 6. Chlorhexidine stain: Chlorhexidine has affinity for sulfate and acidic groups such as those found in pellicle, plaque constituents, carious lesion and bacterial cell wall. So, it is retained into oral cavity and stained oral tissues with yellowish brown to brownish color especially cervical and interproximal area of the teeth, plaque and other restorations and tongue. B. Metallic stain: This type of stain is caused by metals and metallic salts which may introduce into the oral cavity by metal containing dust inhalation by worker or through oral administration of drugs. Metal penetrating into tooth substance causes permanent discoloration whereas that bind with pellicle causes surface stain. Metal salts produce a variety of stains: Copper dust causes green stain, Iron dust causes brown to black stain, Magnesium-causes black stain, Silver nitrate causes grey stain, Potassium permanganate causes a violet to black color and Stannous fluoride causes a golden-brown discoloration. 2. Intrinsic tooth discoloration A. Developmental defects: 1. Alkaptonuria: This inborn error of metabolism results in incomplete metabolism of tyrosine and phenylalanine, which promotes the buildup of homogentisic acid. This affects the permanent dentition by causing a brown discoloration. 2. Congenital erythropoietic porphyria: is a rare inherited metabolic disorder results in error of porphyrin metabolism leading to the accumulation of porphyrins in bone marrow, red blood cells, urine, feces and teeth. A red-brown discoloration and the affected teeth show a red fluorescence under ultraviolet light. 3. Congenital hyperbilirubinemia: The breakdown products of hemolysis will cause a yellow-green discoloration, it is due to deposition of bile pigments in the calcifying dental hard tissues.
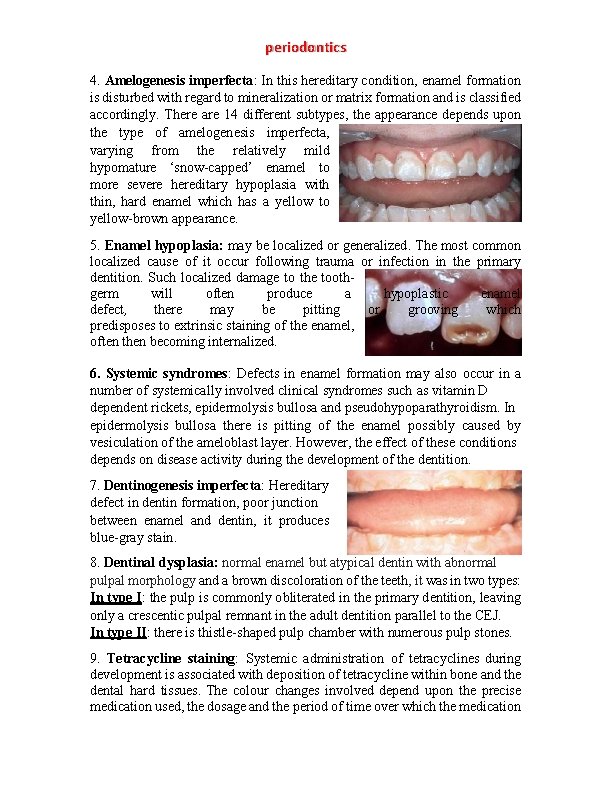
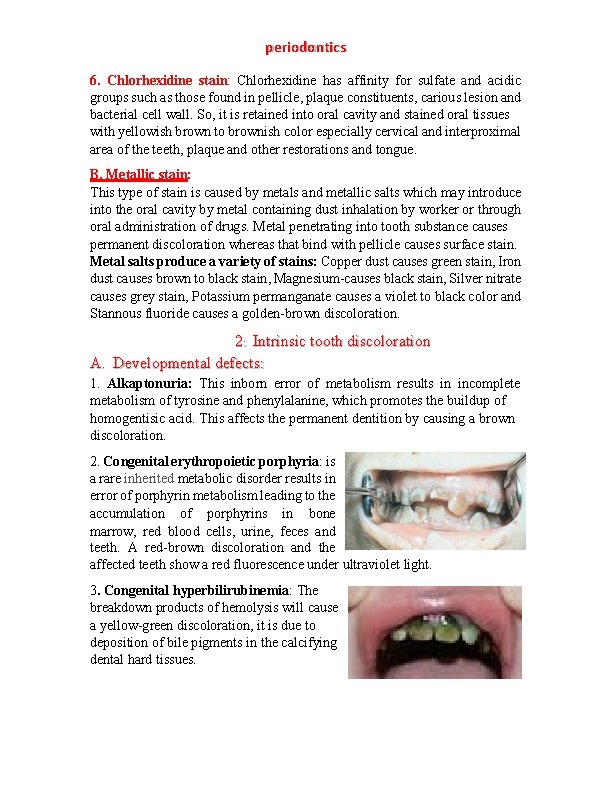
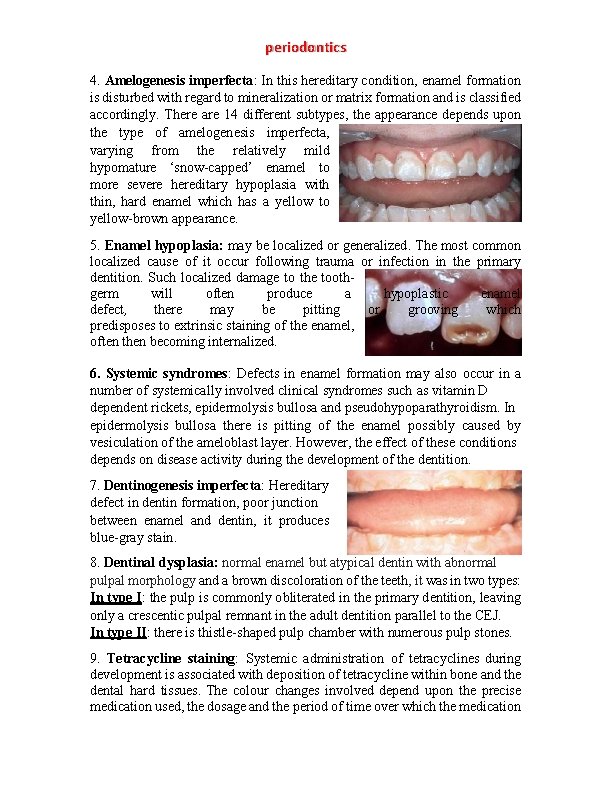
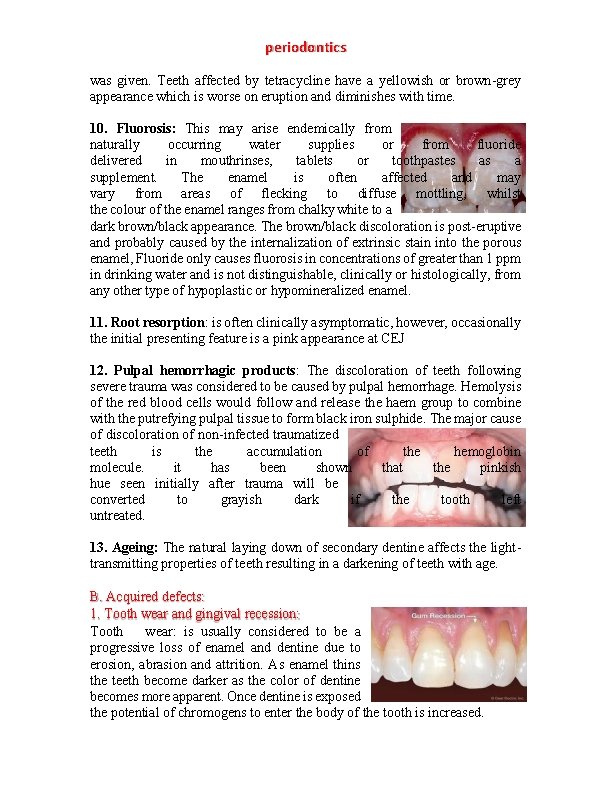
periodontics 4. Amelogenesis imperfecta: In this hereditary condition, enamel formation is disturbed with regard to mineralization or matrix formation and is classified accordingly. There are 14 different subtypes, the appearance depends upon the type of amelogenesis imperfecta, varying from the relatively mild hypomature ‘snow-capped’ enamel to more severe hereditary hypoplasia with thin, hard enamel which has a yellow to yellow-brown appearance. 5. Enamel hypoplasia: may be localized or generalized. The most common localized cause of it occur following trauma or infection in the primary dentition. Such localized damage to the toothgerm will often produce a hypoplastic enamel defect, there may be pitting or grooving which predisposes to extrinsic staining of the enamel, often then becoming internalized. 6. Systemic syndromes: Defects in enamel formation may also occur in a number of systemically involved clinical syndromes such as vitamin D dependent rickets, epidermolysis bullosa and pseudohypoparathyroidism. In epidermolysis bullosa there is pitting of the enamel possibly caused by vesiculation of the ameloblast layer. However, the effect of these conditions depends on disease activity during the development of the dentition. 7. Dentinogenesis imperfecta: Hereditary defect in dentin formation, poor junction between enamel and dentin, it produces blue-gray stain. 8. Dentinal dysplasia: normal enamel but atypical dentin with abnormal pulpal morphology and a brown discoloration of the teeth, it was in two types: In type I: the pulp is commonly obliterated in the primary dentition, leaving only a crescentic pulpal remnant in the adult dentition parallel to the CEJ. In type II: there is thistle-shaped pulp chamber with numerous pulp stones. 9. Tetracycline staining: Systemic administration of tetracyclines during development is associated with deposition of tetracycline within bone and the dental hard tissues. The colour changes involved depend upon the precise medication used, the dosage and the period of time over which the medication
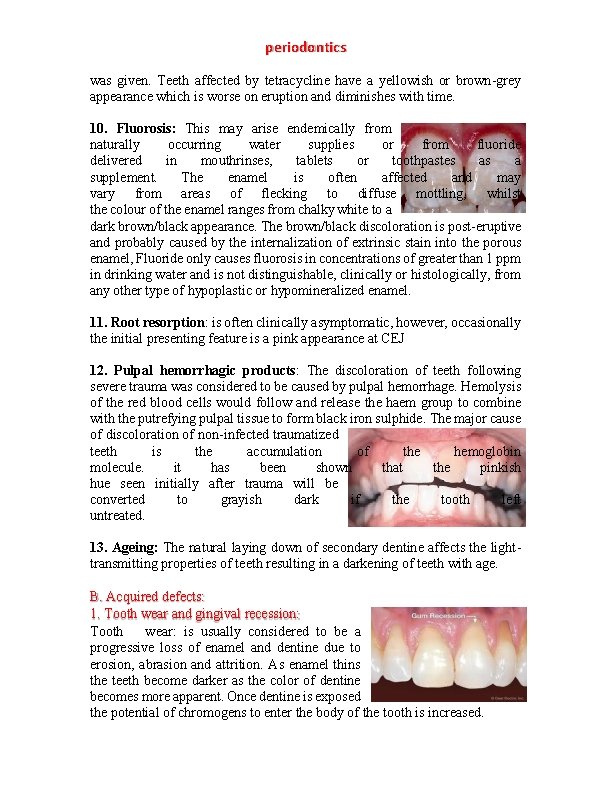
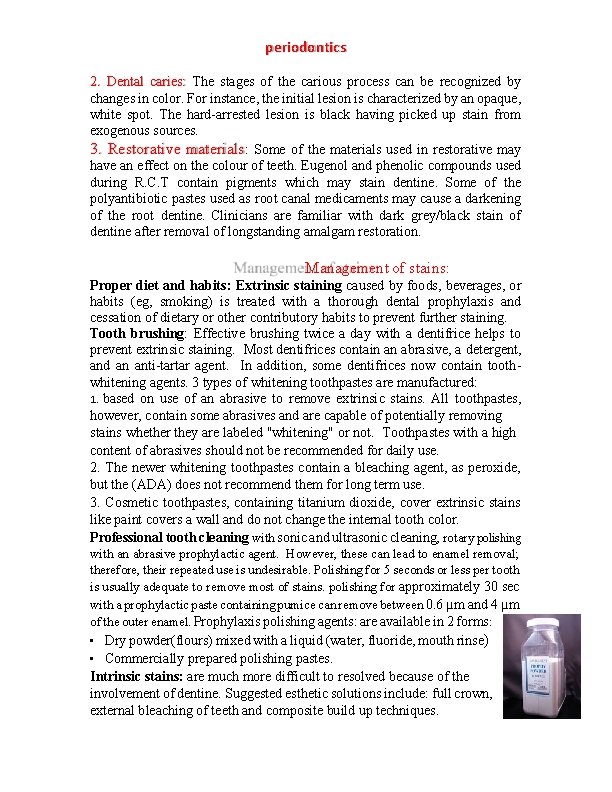
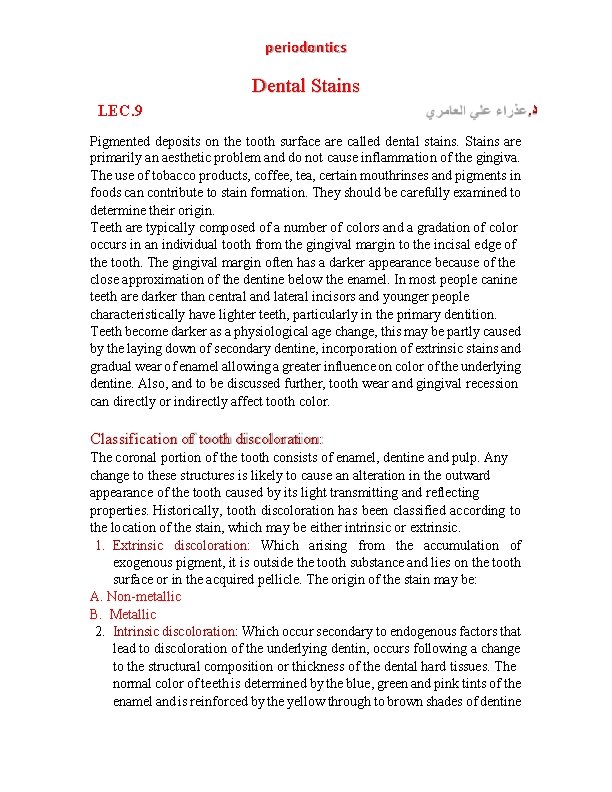
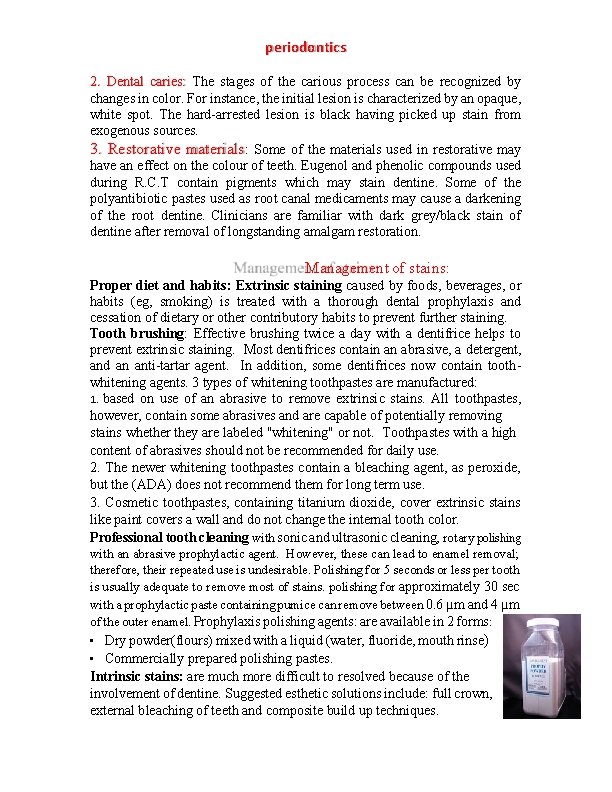
periodontics was given. Teeth affected by tetracycline have a yellowish or brown-grey appearance which is worse on eruption and diminishes with time. 10. Fluorosis: This may arise endemically from naturally occurring water supplies or from fluoride delivered in mouthrinses, tablets or toothpastes as a supplement. The enamel is often affected and may vary from areas of flecking to diffuse mottling, whilst the colour of the enamel ranges from chalky white to a dark brown/black appearance. The brown/black discoloration is post-eruptive and probably caused by the internalization of extrinsic stain into the porous enamel, Fluoride only causes fluorosis in concentrations of greater than 1 ppm in drinking water and is not distinguishable, clinically or histologically, from any other type of hypoplastic or hypomineralized enamel. 11. Root resorption: is often clinically asymptomatic, however, occasionally the initial presenting feature is a pink appearance at CEJ 12. Pulpal hemorrhagic products: The discoloration of teeth following severe trauma was considered to be caused by pulpal hemorrhage. Hemolysis of the red blood cells would follow and release the haem group to combine with the putrefying pulpal tissue to form black iron sulphide. The major cause of discoloration of non-infected traumatized teeth is the accumulation of the hemoglobin molecule. it has been shown that the pinkish hue seen initially after trauma will be converted to grayish dark if the tooth left untreated. 13. Ageing: The natural laying down of secondary dentine affects the lighttransmitting properties of teeth resulting in a darkening of teeth with age. B. Acquired defects: 1. Tooth wear and gingival recession: Tooth wear: is usually considered to be a progressive loss of enamel and dentine due to erosion, abrasion and attrition. As enamel thins the teeth become darker as the color of dentine becomes more apparent. Once dentine is exposed the potential of chromogens to enter the body of the tooth is increased.
periodontics 2. Dental caries: The stages of the carious process can be recognized by changes in color. For instance, the initial lesion is characterized by an opaque, white spot. The hard-arrested lesion is black having picked up stain from exogenous sources. 3. Restorative materials: Some of the materials used in restorative may have an effect on the colour of teeth. Eugenol and phenolic compounds used during R. C. T contain pigments which may stain dentine. Some of the polyantibiotic pastes used as root canal medicaments may cause a darkening of the root dentine. Clinicians are familiar with dark grey/black stain of dentine after removal of longstanding amalgam restoration. Management of stains: Proper diet and habits: Extrinsic staining caused by foods, beverages, or habits (eg, smoking) is treated with a thorough dental prophylaxis and cessation of dietary or other contributory habits to prevent further staining. Tooth brushing: Effective brushing twice a day with a dentifrice helps to prevent extrinsic staining. Most dentifrices contain an abrasive, a detergent, and an anti-tartar agent. In addition, some dentifrices now contain toothwhitening agents. 3 types of whitening toothpastes are manufactured: 1. based on use of an abrasive to remove extrinsic stains. All toothpastes, however, contain some abrasives and are capable of potentially removing stains whether they are labeled "whitening" or not. Toothpastes with a high content of abrasives should not be recommended for daily use. 2. The newer whitening toothpastes contain a bleaching agent, as peroxide, but the (ADA) does not recommend them for long term use. 3. Cosmetic toothpastes, containing titanium dioxide, cover extrinsic stains like paint covers a wall and do not change the internal tooth color. Professional tooth cleaning with sonic and ultrasonic cleaning, rotary polishing with an abrasive prophylactic agent. However, these can lead to enamel removal; therefore, their repeated use is undesirable. Polishing for 5 seconds or less per tooth is usually adequate to remove most of stains. polishing for approximately 30 sec with a prophylactic paste containing pumice can remove between 0. 6 µm and 4 µm of the outer enamel. Prophylaxis polishing agents: are available in 2 forms: • Dry powder(flours) mixed with a liquid (water, fluoride, mouth rinse) • Commercially prepared polishing pastes. Intrinsic stains: are much more difficult to resolved because of the involvement of dentine. Suggested esthetic solutions include: full crown, external bleaching of teeth and composite build up techniques.