Periodontal regeneration a reality Using conventional treatment methods
- Slides: 41
Periodontal regeneration - a reality Using conventional treatment methods, the outcome of therapy depends on which type of cells first reach contact the root surface. The use of different types of bone grafts or bone substitutes to accomplish periodontal tissue regeneration must be considered to be founded on an incorrect biological basis, since bone does not possess the ability to regenerate lost connective tissue attachment. KHU Perio HYS
Reattachment The reunion of connective tissue and root separated by incision or injury Kalkwarf et al. (1974) New attachment The reunion of connective tissue with a root surface that has been deprived of its periodontal ligament Isidor et al. (1985) This reunion occurs by the formation of new cementum with inserting fibers A. A. P. (1986) KHU Perio HYS
Periodontal regeneration It means healing after periodontal surgery that results in the restoration of attachment apparatus, namely, cementum, alveolar bone and periodontal ligament. Periodontal repair It implies healing after periodontal surgery that results in healing without restoration of the attachment apparatus. Repair of a periodontal defect can be mediated by formation of a long junctional epithelium, increased bone volume and density, as well as ankylosis, root resorption and fibrous adhesion. KHU Perio HYS
Mostly, regeneration of the attachment tissues take place partially. This can involve the formation of a cementum-mediated new fibrous attachment to a pathologically exposed root surface, without new bone formation. Conversely, new bone formation can obliterate angular bony defect, but the new bone may not be connected to the root surface because of an intervening long junctional epithelium. KHU Perio HYS
Complications of wound healing in the periodontal environment 1) 2) 3) 4) 5) Microbiota - diverse, pathogenic Multiple specialized cell types Multiple specialized junctional complexes Avascular tooth surface Stromal - cellular interactions KHU Perio HYS
Traditional Regenerative Therapy Modified Widman Flap, Bone Graft Procedures, Root Planing & Soft Tissue Curettage Periodontal wound healing following traditional regenerative procedures result in the reformation of epithelial lining (long junctional epithelium) facing the instrumented root surfaces, with no new connective tissue attachment. Caton et al (1980) - monkey study KHU Perio HYS
Studies leading to the principle of guided tissue regeneration 1. Bone tissue does not form new connective tissue attachment. : ankylosis & root resorption Karring et al. (1980) 2. Gingival connective tissue does not form new connective tissue attachment. : root resorption Nyman et al. (1980) KHU Perio HYS
3. Periodontal ligament tissue has the capacity to form new connective tissue attachment. : true regeneration Karring et al. (1985) 4. Epithelial downgrowth prevents the formation of a new connective tissue attachment by preventing repopulation of the root surface by cells derived from the periodontal ligament. : the prevention of root resorption and ankylosis, which otherwise could be induced by gingival connective tissue and bone. Caton et al. (1980), Karring et al. (1984, 1985) KHU Perio HYS
Successful periodontal regeneration 1. Good flap design & flap management 2. Thorough root debridement 3. Appropriate regenerative materials 3. Suturing technique 4. Use of antimicrobial agents 5. Proper postoperative care KHU Perio HYS
Promoting the progenitor cell population 1. Coronally positioned or anchored flaps 2. Physical barriers ( e-PTFE & bioabsorbable materials) 3. Growth factors and attachment proteins 4. Bone augmentation devices or Space-maintaining devices KHU Perio HYS
The Methods for Evaluating Periodontal Regeneration 1. Clinical attachment level 2. Re-entry procedures 3. Pre- and post-treatment radiographs KHU Perio HYS
Clinical attachment level Large gains in clinical attachment can occur after therapy without regeneration of new periodontal ligament. These “ false” gains are due to resolution of inflammation, bone fill, reformation of the gingival collagen fibers and a long junctional epithelium. Probing methods are therefore not adequate to evaluating periodontal regenerative therapies. KHU Perio HYS
Re-entry procedures Although this methods can measure the gross behavior of bone, bone measurements do not reflect connective tissue attachment levels and cannot distinguish bone that is attached to the root surface via a periodontal ligament. Re-entry procedures are therefore inappropriate for the evaluation of periodontal regenerative therapy. KHU Perio HYS
Pre- & post-treatment radiographs Changes in bone height, density and volume can be estimated by pre- and post-treatment radiographs but cannot distinguish whether the bone is connected to the tooth by new periodontal ligament and cementum (true regeneration) KHU Perio HYS
Barrier Membranes 1. Non-Resorbable Membrane expanded polytetrafluoroethylene (e-PTFE) 2. Bioresorbable Membrane Resolut, Guidor, Biomend, Bio. Gide, Atrisorb, Vicryl Periodontal Mesh, Biomesh KHU Perio HYS
Non-Resorbable Membrane The characteristics, structure & function of Gore-Tex membrane KHU Perio HYS
The classification according to purpose of usage GTPM GTAM • Periodontal regeneration • Collar & apron • Bone regeneration • Inner & outer portion KHU Perio HYS
Guided Tissue Periodontal Material For Periodontal Regeneration KHU Perio HYS
Open microstructure collar This portion permits connective tissue ingrowth and prevents apical migration of epithelium. Occlusive portion This portion stabilizes the wound area, permits selective cell repopulation for GTR, gives a strong enough structure to retain sutures snugged around the tooth, is easy to cut and shape with no sharp edges to perforate tissue, and in the event of complication, allows the membrane to be easily removed KHU Perio HYS
Guided Tissue Augmentation Material For Bone Regeneration KHU Perio HYS
Inner portion Stiffer to provide better spacemaking Outer portion Soft to contour to the bony defect margins and more porous to integrate with tissue, stabilize the wound and limit epithelial migration KHU Perio HYS
Bioresorbable Membrane The characteristics of commercially available bioresorbable membrane KHU Perio HYS
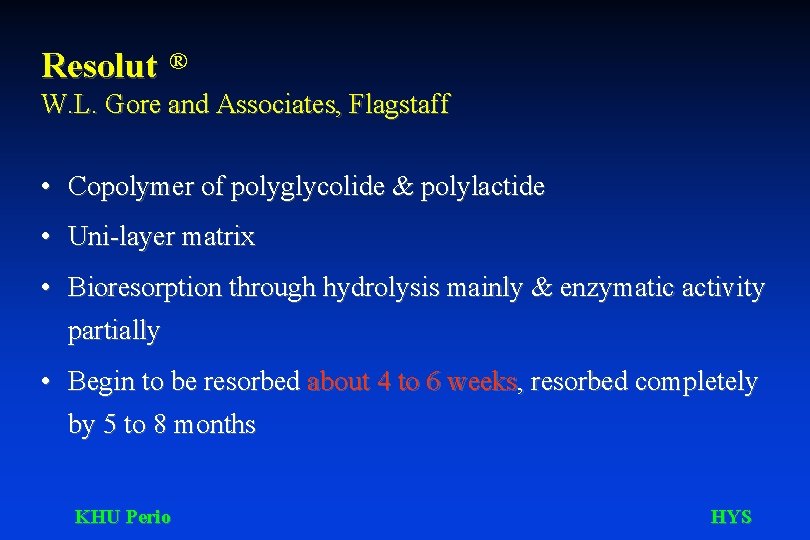
Resolut ® W. L. Gore and Associates, Flagstaff • Copolymer of polyglycolide & polylactide • Uni-layer matrix • Bioresorption through hydrolysis mainly & enzymatic activity partially • Begin to be resorbed about 4 to 6 weeks, resorbed completely by 5 to 8 months KHU Perio HYS
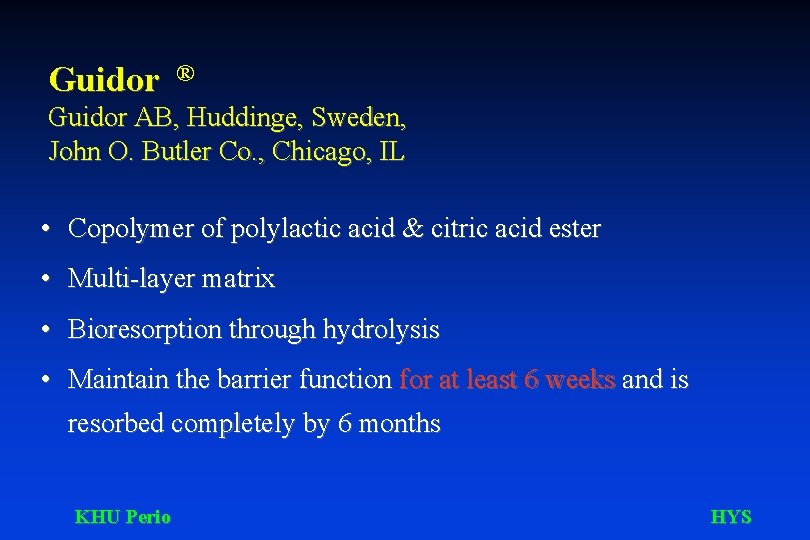
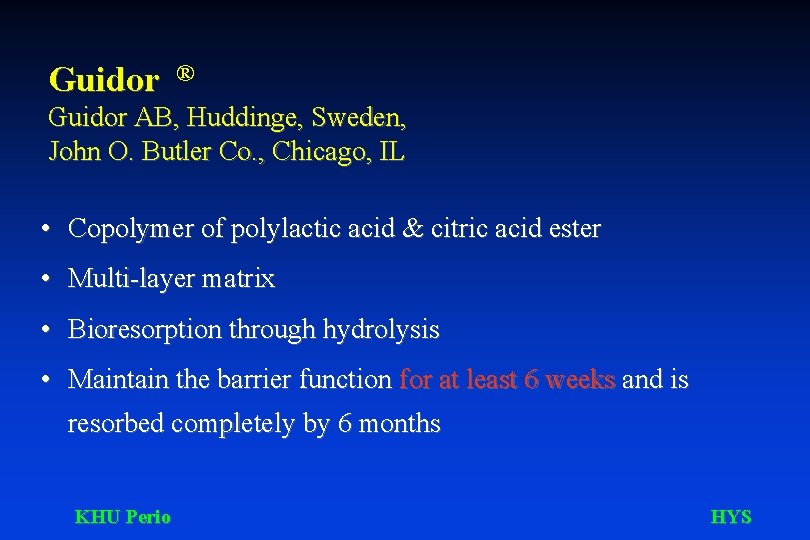
Guidor ® Guidor AB, Huddinge, Sweden, John O. Butler Co. , Chicago, IL • Copolymer of polylactic acid & citric acid ester • Multi-layer matrix • Bioresorption through hydrolysis • Maintain the barrier function for at least 6 weeks and is resorbed completely by 6 months KHU Perio HYS
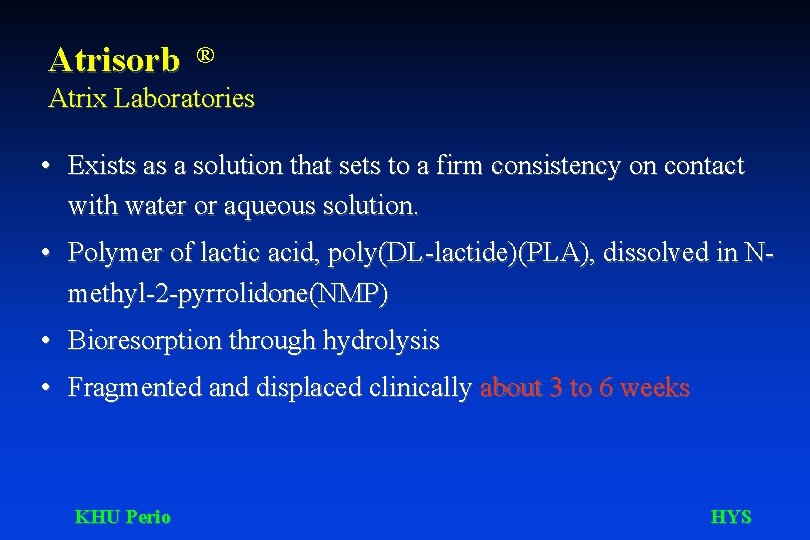
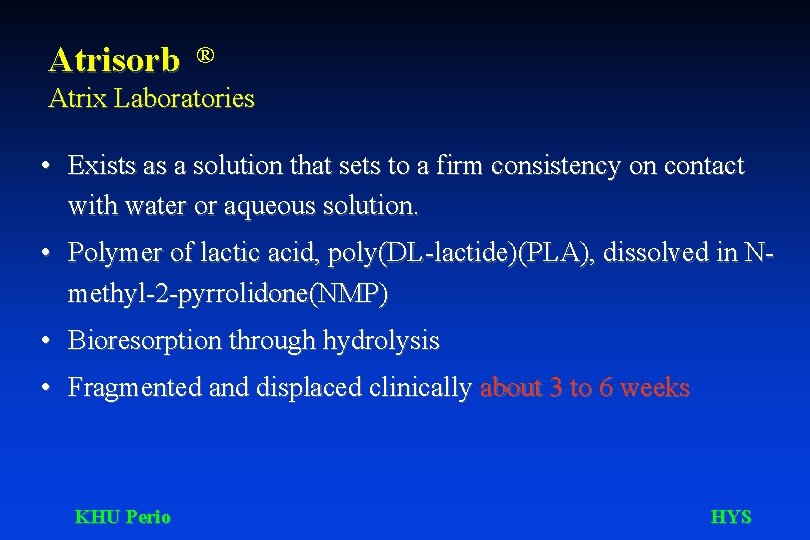
Atrisorb ® Atrix Laboratories • Exists as a solution that sets to a firm consistency on contact with water or aqueous solution. • Polymer of lactic acid, poly(DL-lactide)(PLA), dissolved in Nmethyl-2 -pyrrolidone(NMP) • Bioresorption through hydrolysis • Fragmented and displaced clinically about 3 to 6 weeks KHU Perio HYS
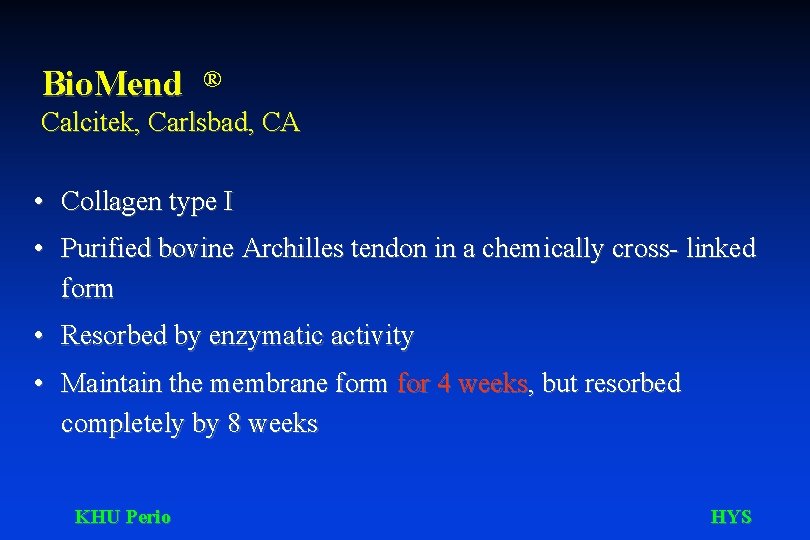
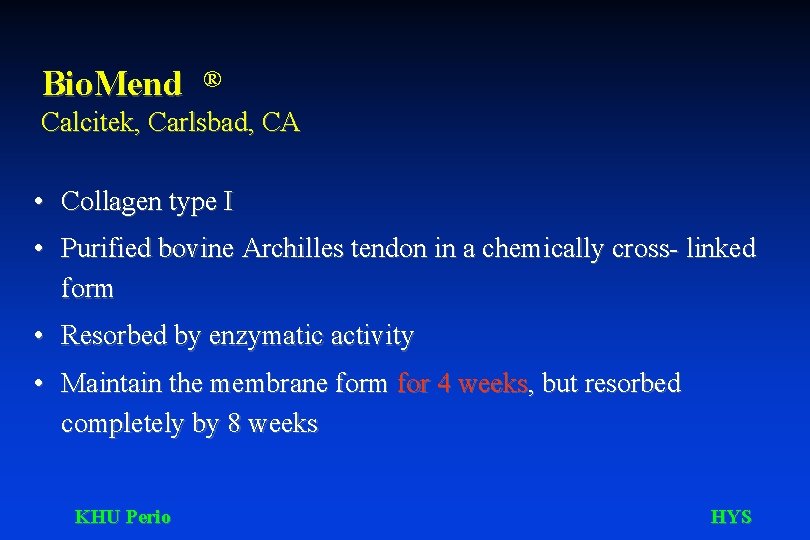
Bio. Mend ® Calcitek, Carlsbad, CA • Collagen type I • Purified bovine Archilles tendon in a chemically cross- linked form • Resorbed by enzymatic activity • Maintain the membrane form for 4 weeks, but resorbed completely by 8 weeks KHU Perio HYS
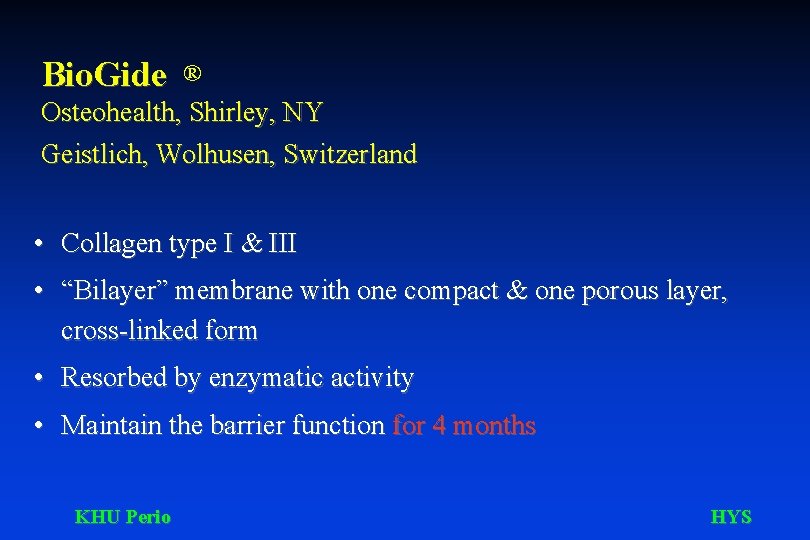
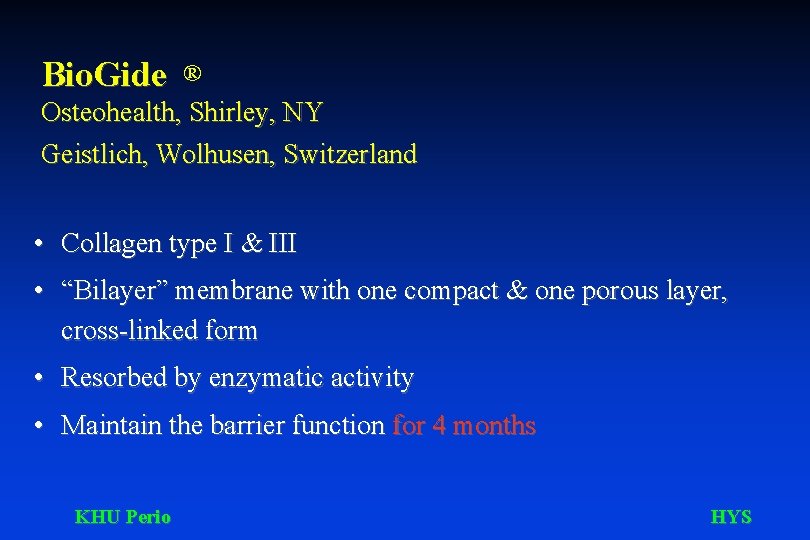
Bio. Gide ® Osteohealth, Shirley, NY Geistlich, Wolhusen, Switzerland • Collagen type I & III • “Bilayer” membrane with one compact & one porous layer, cross-linked form • Resorbed by enzymatic activity • Maintain the barrier function for 4 months KHU Perio HYS
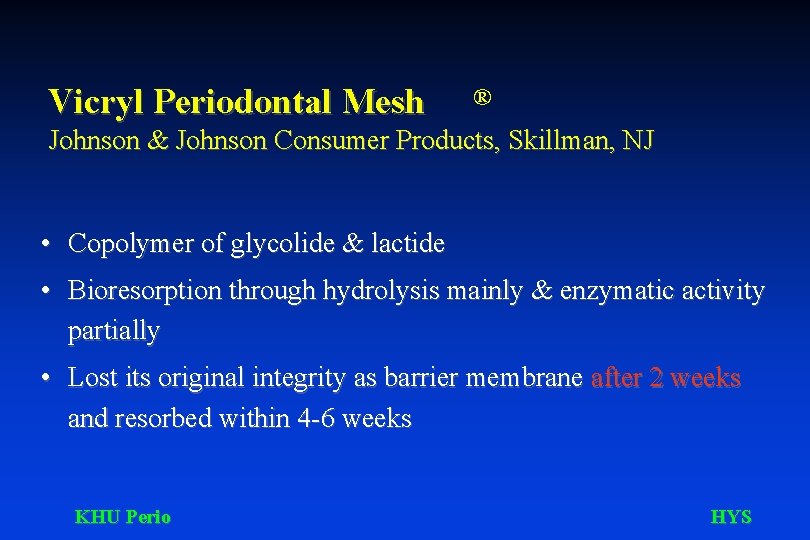
Vicryl Periodontal Mesh ® Johnson & Johnson Consumer Products, Skillman, NJ • Copolymer of glycolide & lactide • Bioresorption through hydrolysis mainly & enzymatic activity partially • Lost its original integrity as barrier membrane after 2 weeks and resorbed within 4 -6 weeks KHU Perio HYS
Lyodura ® Brown, Melsungen, Germany • Cadeveric pure dura mater • Pure collagen fibers strictly connected, with a high mechanical resistance to shear strength • Processed with sodium hydroxide and hydrogen peroxide to bacteria and enzymes, with glycerine to increase elasticity and shear strength • Maintain its integrity after 6 months (Fontana et al. 1994) • Creutzfeld Jakob disease KHU Perio HYS
® Bio. Mesh Samyang Co. Korea • Composed of polylactic acid, lactide/glycolide copolymer, reinforced in its mechanical strength by polyglycolic acid fiber • Porous surface & interconnective porous structure • Bioresorption through hydrolysis into lactic and glycolic acid • Maintain its physical integrity for 4 weeks and separates tissue for 6 to 8 weeks ( in vivo ) KHU Perio HYS
The meaning of the words bioabsorbable, biodegradable, and bioresorbable Vert (1989) and Vert et al. (1992) KHU Perio HYS
Biodegradable Solid polymeric materials and devices that break down as a result of macromolecular degradation with dispersion in vivo, but there is no proof of elimination from the body. Biodegradable polymeric systems or devices can be attacked by biological elements so that the integrity of the system and, in some cases but not necessarily the macromolecules themselves, is affected and gives fragments or other degradation by-products. KHU Perio HYS
Bioresorbable Solid polymeric materials and devices that can degrade and further resorb in vivo, ie, that are eliminated through natural pathways either because of simple filtration of degradation byproducts or after metabolization. Bioresorption is a concept that reflects total elimination of the initial foreign material and of degradation by-products (lowmolecular weight compounds) with no residual side effects. KHU Perio HYS
Bioabsorbable Solid polymeric materials and devices that can dissolve in body fluids without any polymer chain cleavage or molecular mass decrease. Slow dissolution of water-soluble implants in body fluids is an example. A bioabsorbable polymer can be bioresorbable if the dispersed macromolecular are excreted. KHU Perio HYS
The effects of micromovement Micromovement of graft and/or membrane during the early phases of wound healing directly influences cellular differentiation. Micromovement of as little as 20 um during early fracture healing has been shown to alter the differentiation of mesenchymal cells from osteoblasts to fibroblasts. Wikesjö & Nilvéus (1990) KHU Perio HYS
Critical Size Defect The smallest size intraosseous wound in a particular bone and species of animal that will not heal spontaneously during the lifetime of the animal. Schmitz and Hollinger (1985) Attempted repair of a CSD results in the formation of fibrous connective tissue rather than bone. Frame (1980), Takagi and Urist (1982) KHU Perio HYS
The pathogenesis of critical size defect dependent non-union 1. Periosteal sheath lacking support, may fold inwards towards the bony segments and form a fibroblastic barrier, preventing union and leading to eburnation of the bone ends. 2. The Hematoma occuring at the time of injury may not be able to organize and bridge the large gap. The trellis necessary for the migration of blood vessels and other osteogenic elements is thus absent, making complete repair unlikely. KHU Perio HYS
The role of periosteum in osteogenesis New bone formation was deposited subperiosteally in the osteoperiosteal portion of all the flaps, but that isolated deposits of new bone were never present in the periosteal parts of the flaps. Maintenance of the integrity of the cells of the cambium layer of the periosteum is essential if osteogenesis by periosteal cells is to occur Melcher and Accursi (1971) - Rat study KHU Perio HYS
Calvarial Defect Model Morphologically and embryologically, the calvaria develops from a membrane precursor and thus resembles the membranous bones of the face. Anatomically, the calvaria consists of two cortical plates with regions of intervening cancellous bone similar to the mandible. Physiologically, the cortical bone in the calvaria resembles as atrophic mandible. KHU Perio HYS
Objectives of Root Planing 1. Securing biologically acceptable root surfaces 2. Resolving inflammation 3. Reducing probing depths 4. Facilitating oral hygiene procedures 5. Improving or maintaining attachment levels 6. Preparing tissues for surgical procedures - controversial KHU Perio HYS
• Cytotoxicities of Periodontally-Involved Cementum • Root Surface Smoothness and Roughness • Removal of Cementum, Frequency of Stroke? • Removal of Calculus & Residual Calculus • Which Instrument to use for Root Surface Debridement? • Evaluation on thoroughness of Root Planing and Root Surface Debridement ? KHU Perio HYS