Periodic Fetal Heart Rate Changes The periodic fetal


- Slides: 42
Periodic Fetal Heart Rate Changes
� The periodic fetal heart rate refers to deviations from baseline that are temporally related to uterine contractions. � Acceleration refers to an increase in fetal heart rate above baseline and deceleration to a decrease below the baseline rate. � The nomenclature most commonly used in the United States is based on the timing of the deceleration in relation to contractions— thus, early, late, or variable in onset related to the corresponding uterine contraction.
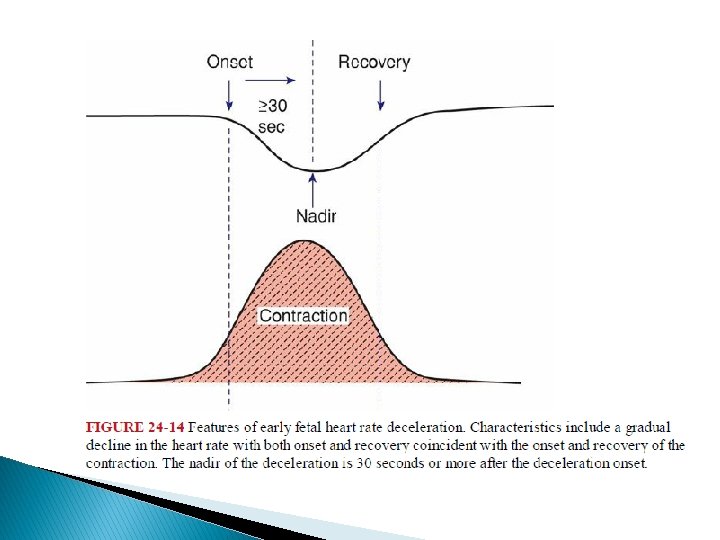
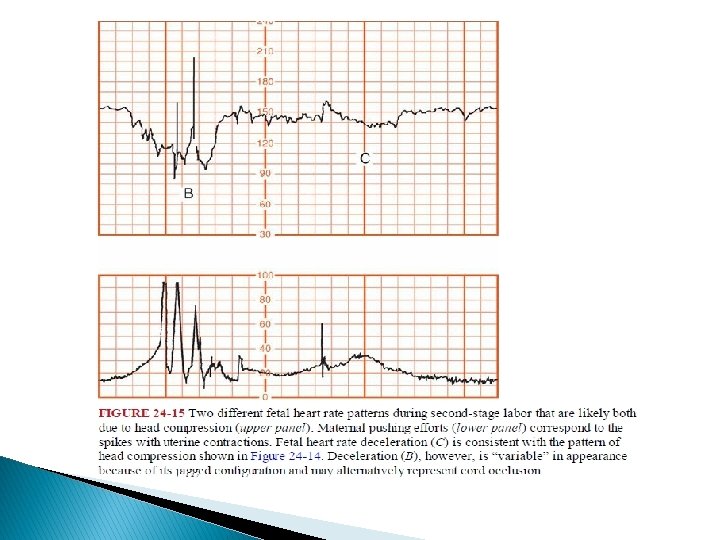
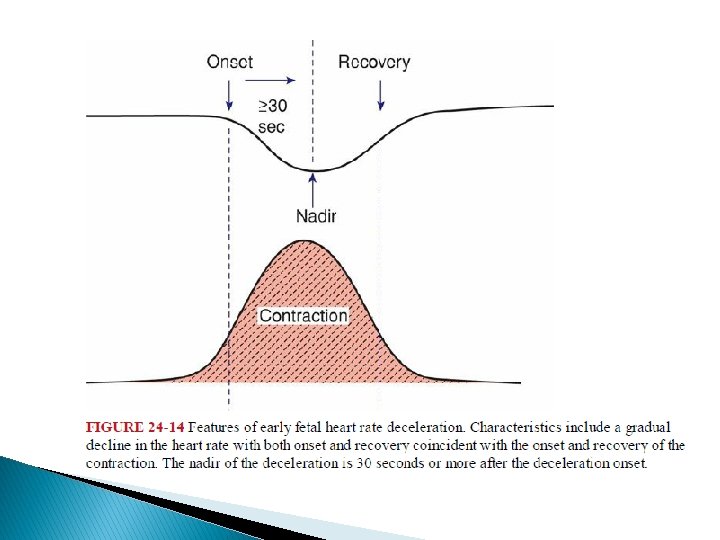
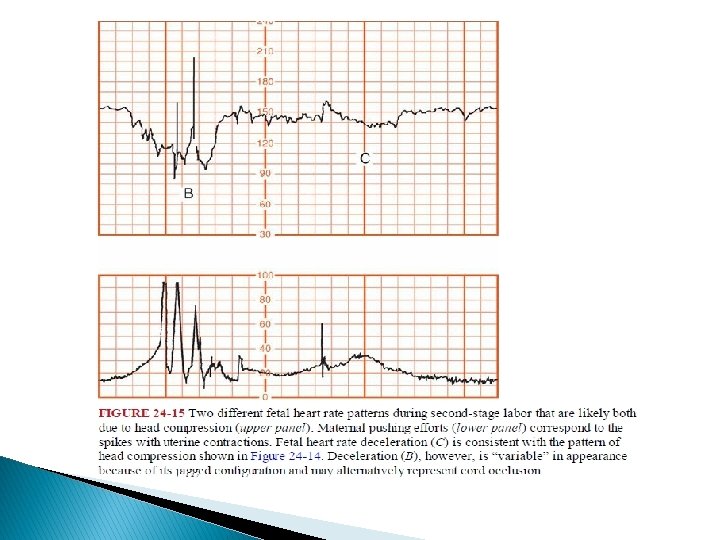
� The waveform of these decelerations is also significant for pattern recognition. � In early and late decelerations, the slope of fetal heart rate change is gradual, resulting in a curvilinear and uniform or symmetrical waveform. � With variable decelerations, the slope of fetal heart rate change is abrupt and erratic, giving the waveform a jagged appearance.
� The 1997 workshop proposed that decelerations be defined as recurrent if they occur with 50 percent or more of contractions in any 20 -minute period.
� Another system now used less often to describe decelerations is based on the pathophysiological events considered most likely to cause the pattern. � In this system, early decelerations are termed head compression, late decelerations are termed uteroplacental insufficiency, and variable decelerations become cord compression patterns.
� These Accelerations are visually apparent abrupt increases— defined as onset of acceleration to a peak in less than 30 seconds—in the fetal heart rate baseline. � At 32 weeks’ gestation and beyond, the acceleration has a peak of 15 bpm with a duration of 15 seconds or more but less than 2 minutes. � Before 32 weeks, a peak of 10 bpm for 15 seconds to 2 minutes is considered normal. � Prolonged acceleration was defined as 2 minutes or more but less than 10 minutes.
mechanisms for intrapartum accelerations � Fetal movement � Stimulation by uterine contractions � Umbilical cord occlusion � Fetal stimulation during pelvic examination � Fetal scalp blood sampling � Acoustic stimulation
� Finally, accelerations can occur during labor without any apparent stimulus. � Indeed, they are common in labor and are nearly always associated with fetal movement. � These accelerations are virtually always reassuring and almost always confirm that the fetus is not acidemic at that time.

� Fetal heart accelerations during the first or last 30 minutes during labor, or both, was a favorable sign for fetal well-being. � The absence of such accelerations during labor, however, is not necessarily an unfavorable sign unless coincidental with other nonreassuring changes.
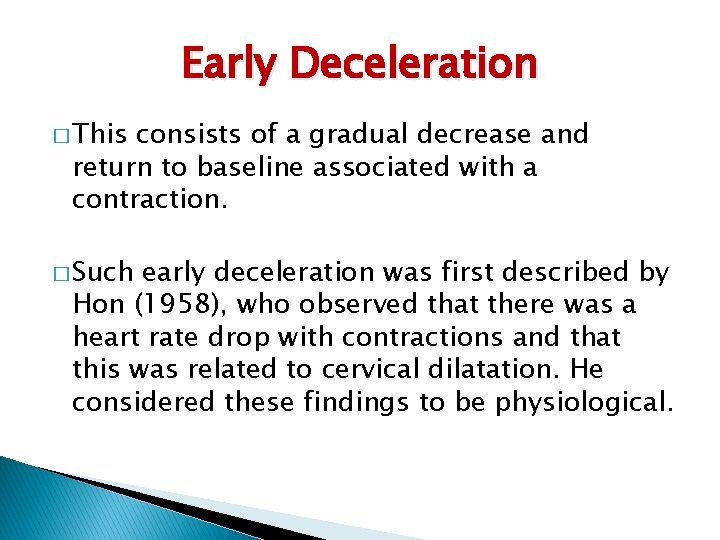
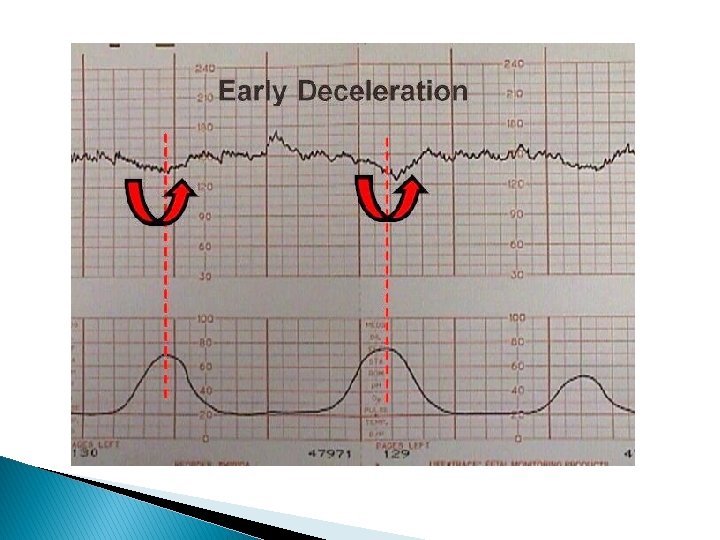
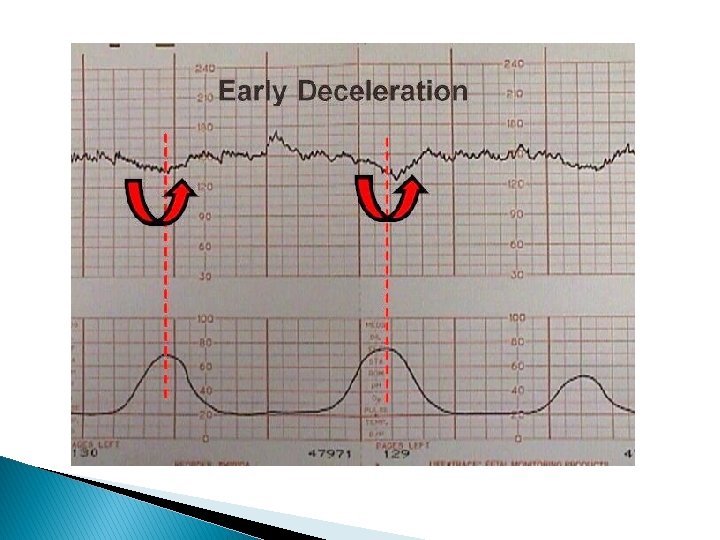
Early Deceleration � This consists of a gradual decrease and return to baseline associated with a contraction. � Such early deceleration was first described by Hon (1958), who observed that there was a heart rate drop with contractions and that this was related to cervical dilatation. He considered these findings to be physiological.
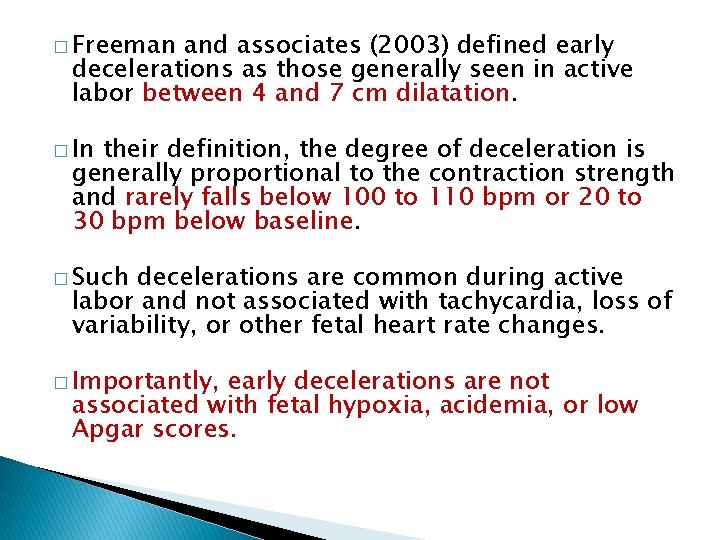
� Freeman and associates (2003) defined early decelerations as those generally seen in active labor between 4 and 7 cm dilatation. � In their definition, the degree of deceleration is generally proportional to the contraction strength and rarely falls below 100 to 110 bpm or 20 to 30 bpm below baseline. � Such decelerations are common during active labor and not associated with tachycardia, loss of variability, or other fetal heart rate changes. � Importantly, early decelerations are not associated with fetal hypoxia, acidemia, or low Apgar scores.
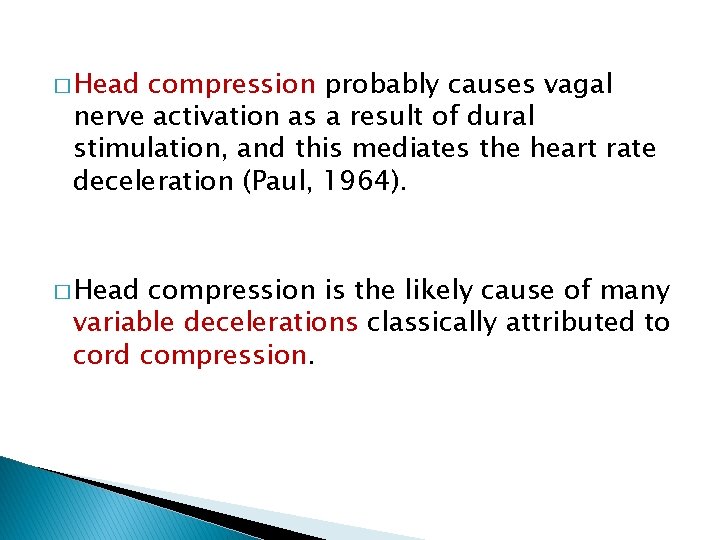
� Head compression probably causes vagal nerve activation as a result of dural stimulation, and this mediates the heart rate deceleration (Paul, 1964). � Head compression is the likely cause of many variable decelerations classically attributed to cord compression.
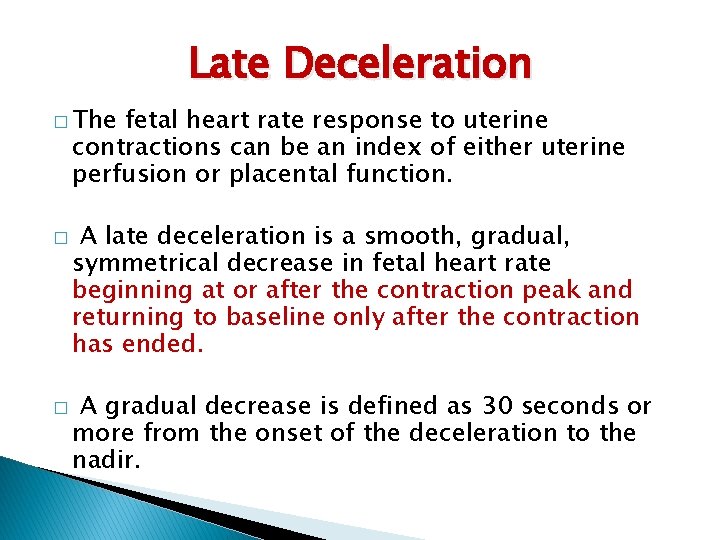
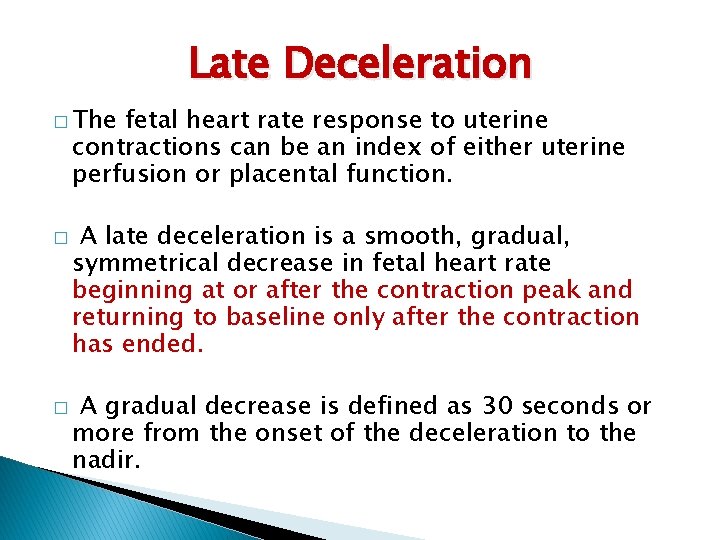
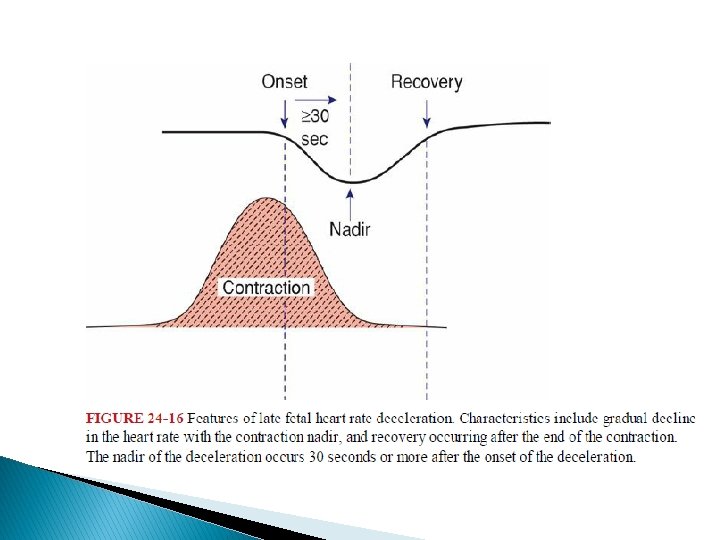
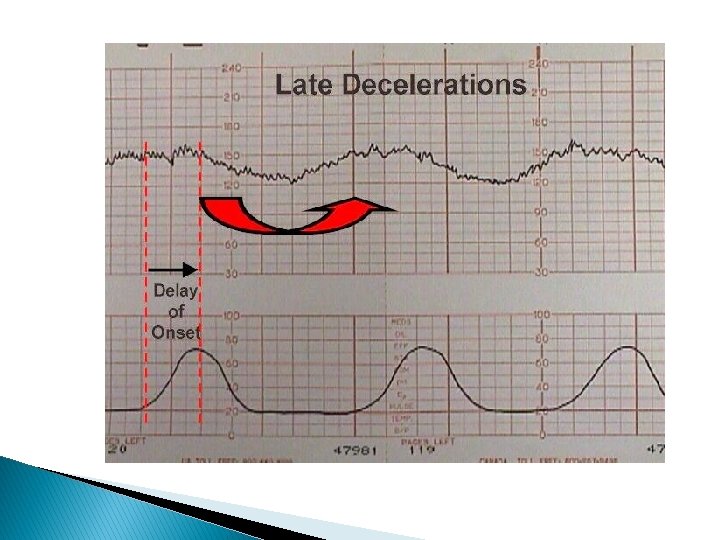
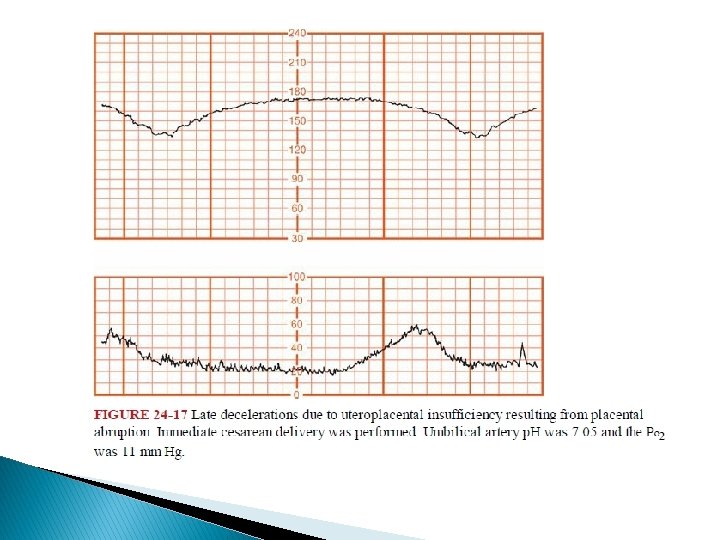
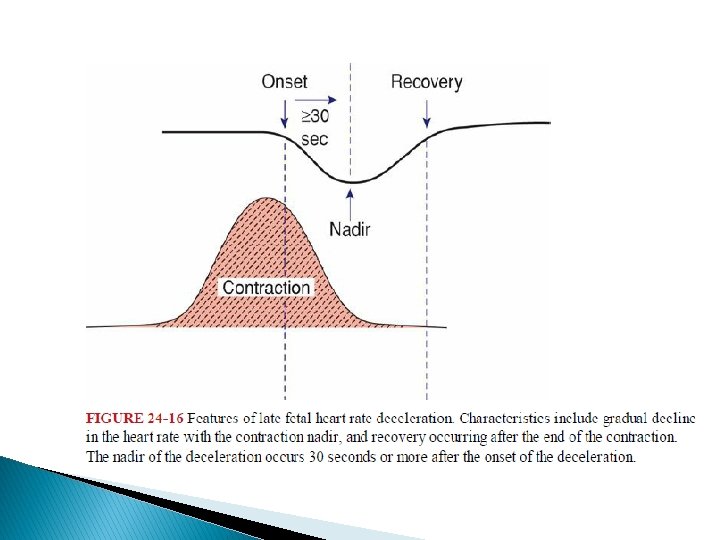
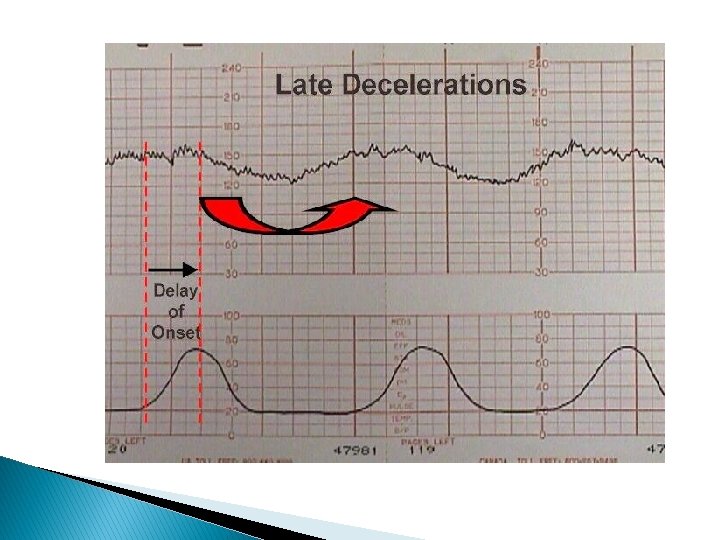
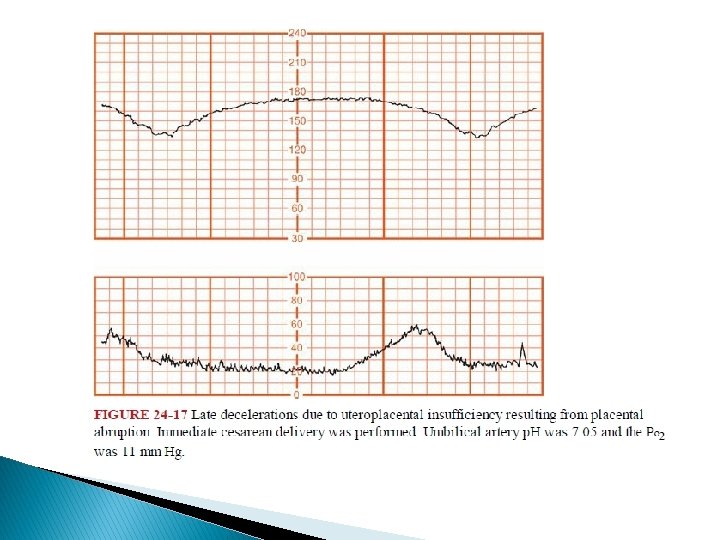
Late Deceleration � The fetal heart rate response to uterine contractions can be an index of either uterine perfusion or placental function. � � A late deceleration is a smooth, gradual, symmetrical decrease in fetal heart rate beginning at or after the contraction peak and returning to baseline only after the contraction has ended. A gradual decrease is defined as 30 seconds or more from the onset of the deceleration to the nadir.
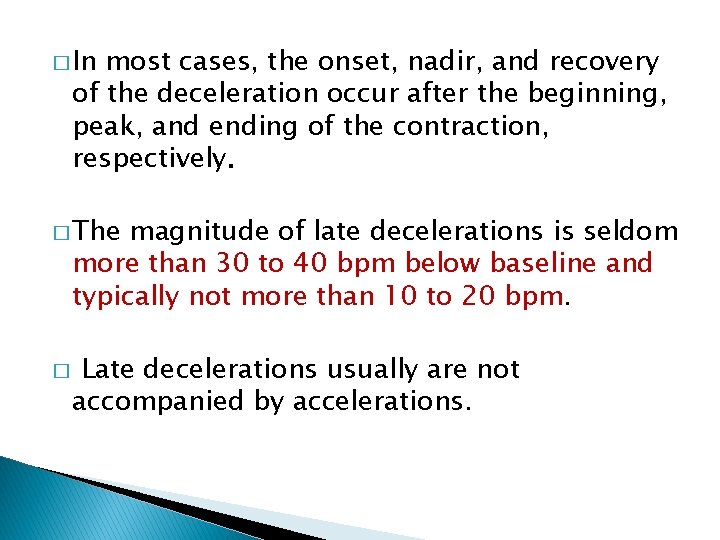
� In most cases, the onset, nadir, and recovery of the deceleration occur after the beginning, peak, and ending of the contraction, respectively. � The magnitude of late decelerations is seldom more than 30 to 40 bpm below baseline and typically not more than 10 to 20 bpm. � Late decelerations usually are not accompanied by accelerations.
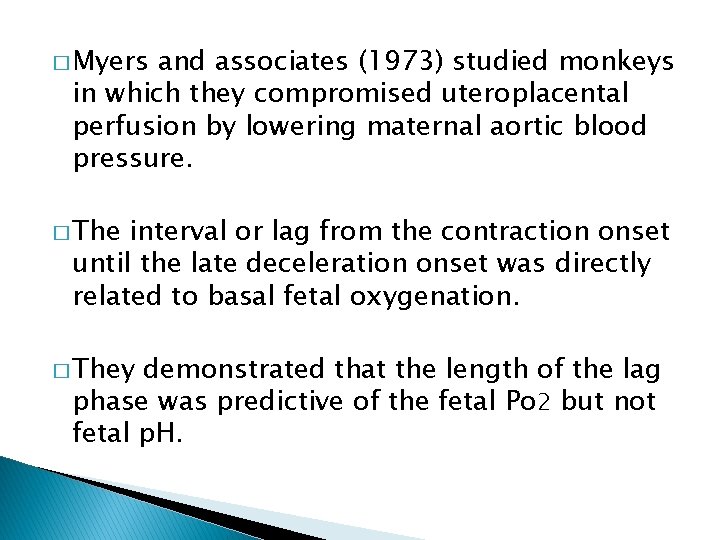
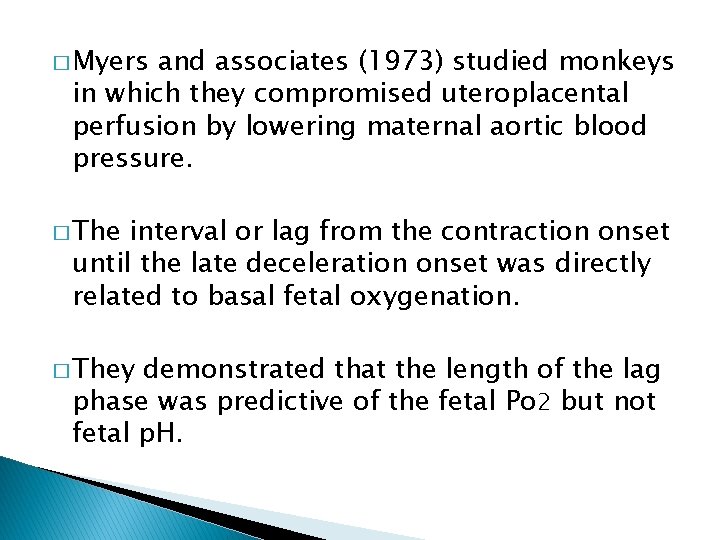
� Myers and associates (1973) studied monkeys in which they compromised uteroplacental perfusion by lowering maternal aortic blood pressure. � The interval or lag from the contraction onset until the late deceleration onset was directly related to basal fetal oxygenation. � They demonstrated that the length of the lag phase was predictive of the fetal Po 2 but not fetal p. H.
Mechanisms for intrapartum late decelerations � Any process that causes maternal hypotension � Epidural analgesia � Uterine hyperactivity caused by oxytocin stimulation � Placental dysfunction � Maternal diseases such as hypertension, diabetes, collagen-vascular disorders. � Placental abruption cause acute late decelerations.
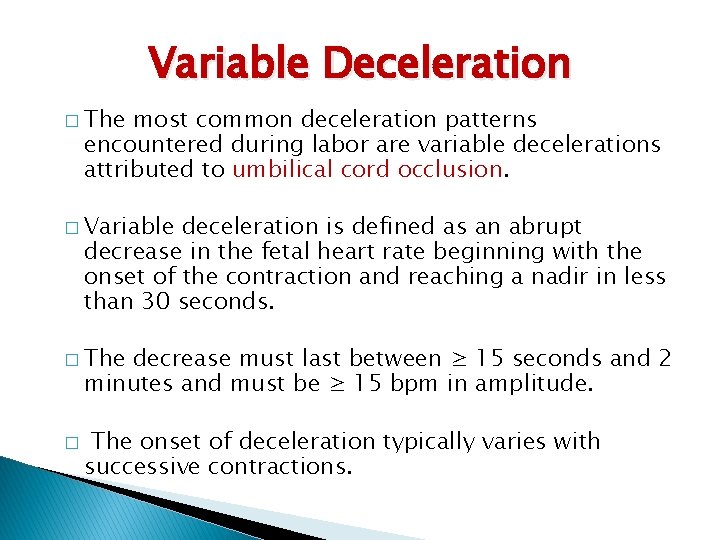
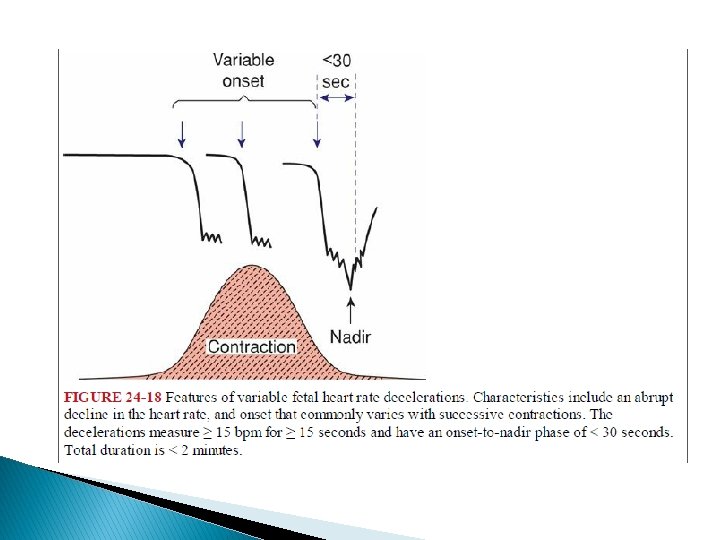
Variable Deceleration � The most common deceleration patterns encountered during labor are variable decelerations attributed to umbilical cord occlusion. � Variable deceleration is defined as an abrupt decrease in the fetal heart rate beginning with the onset of the contraction and reaching a nadir in less than 30 seconds. � The decrease must last between ≥ 15 seconds and 2 minutes and must be ≥ 15 bpm in amplitude. � The onset of deceleration typically varies with successive contractions.
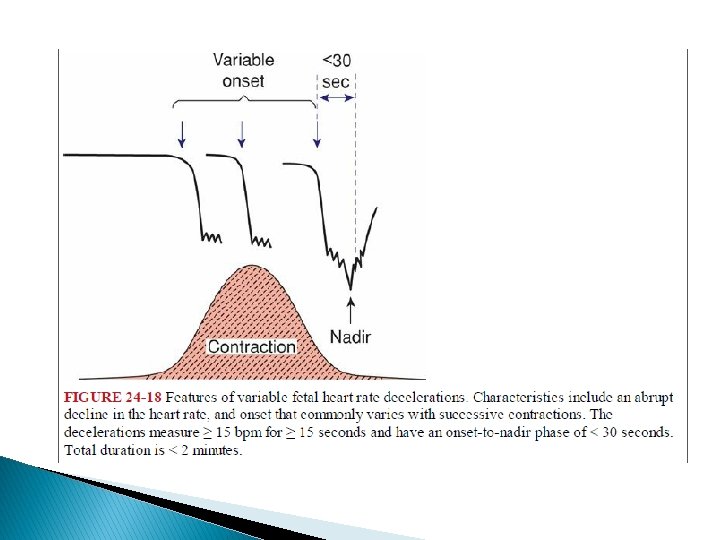
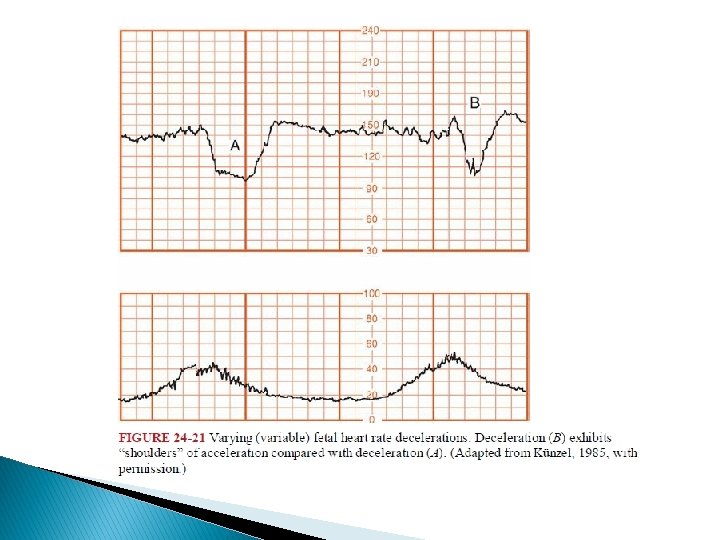
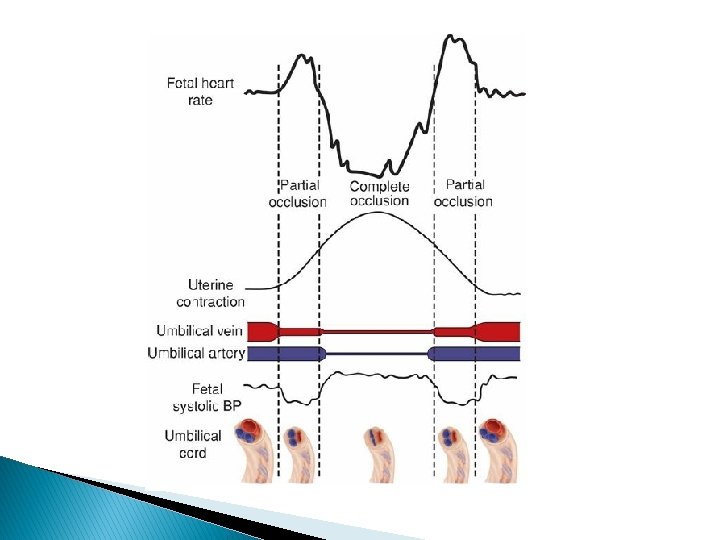
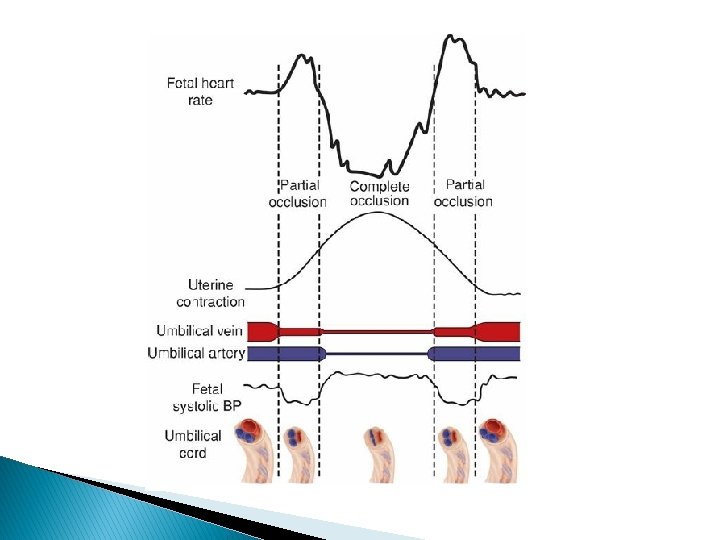
� Two types of variable decelerations are shown � The deceleration denoted by “A” is very much like that seen with complete umbilical cord occlusion in experimental animals. � Deceleration “B, ” however, has a different configuration because of the “shoulders” of acceleration before and after the deceleration component.
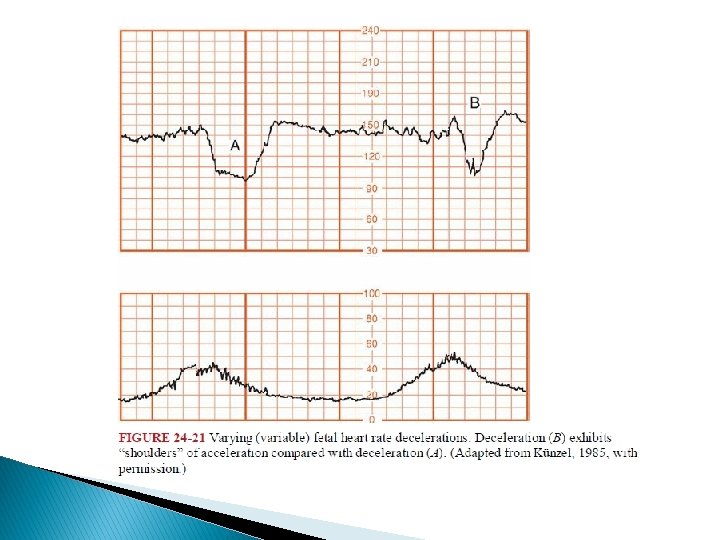
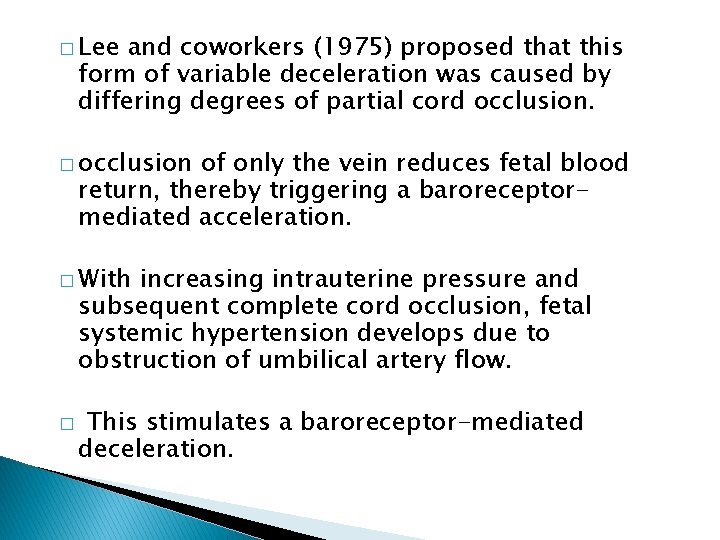
� Lee and coworkers (1975) proposed that this form of variable deceleration was caused by differing degrees of partial cord occlusion. � occlusion of only the vein reduces fetal blood return, thereby triggering a baroreceptormediated acceleration. � With increasing intrauterine pressure and subsequent complete cord occlusion, fetal systemic hypertension develops due to obstruction of umbilical artery flow. � This stimulates a baroreceptor-mediated deceleration.
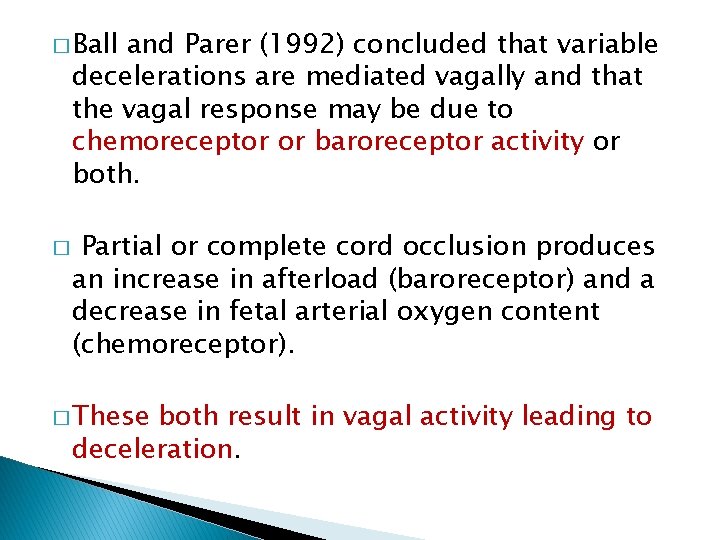
� Ball and Parer (1992) concluded that variable decelerations are mediated vagally and that the vagal response may be due to chemoreceptor or baroreceptor activity or both. � Partial or complete cord occlusion produces an increase in afterload (baroreceptor) and a decrease in fetal arterial oxygen content (chemoreceptor). � These both result in vagal activity leading to deceleration.
� According to the American College of Obstetricians and Gynecologists (2013 a), recurrent variable decelerations with minimal to moderate variability are indeterminate, whereas those with absent variability are abnormal.
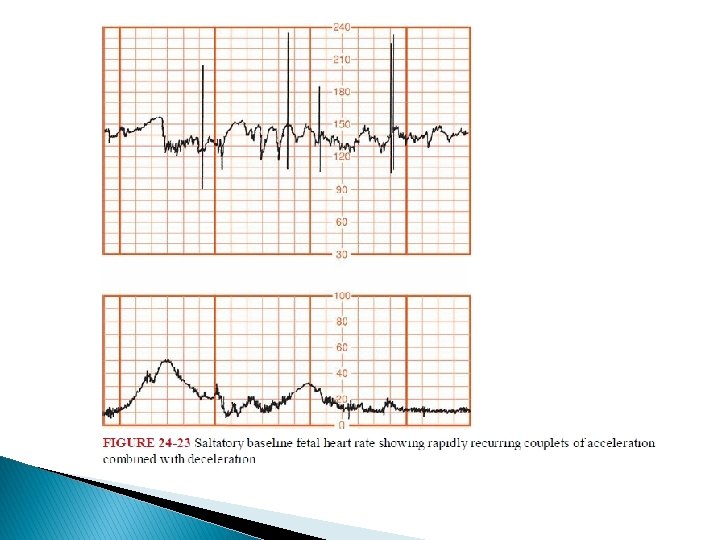
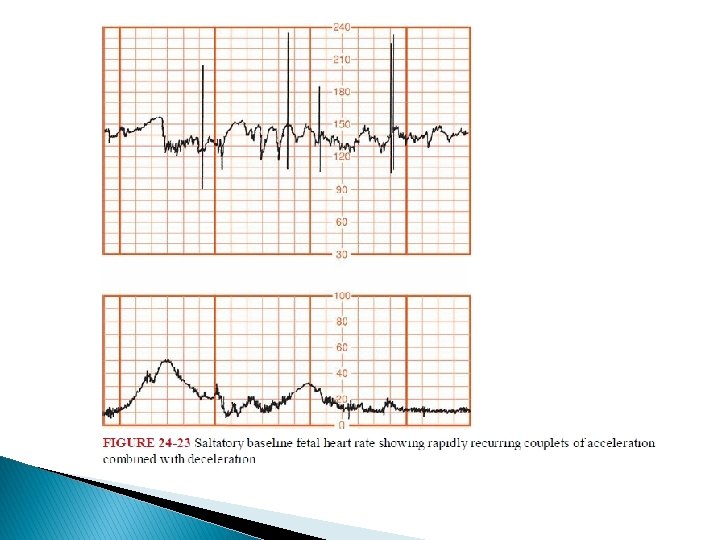
� Other fetal heart rate patterns have been associated with umbilical cord compression. � Saltatory baseline heart rate was first described by Hammacher and colleagues (1968) and linked to umbilical cord complications during labor. � � The pattern consists of rapidly recurring couplets of acceleration and deceleration causing relatively large oscillations of the baseline fetal heart rate. We also observed a relationship between cord occlusion and the saltatory pattern.
� Lambda is a pattern involving an acceleration followed by a variable deceleration with no acceleration at the end of the deceleration. � � This pattern typically is seen in early labor and is not ominous. This lambda pattern may result from mild cord compression or stretch.
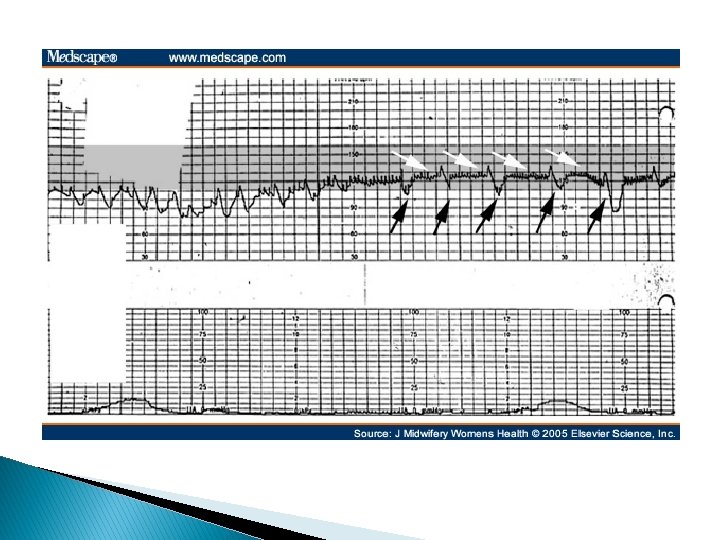
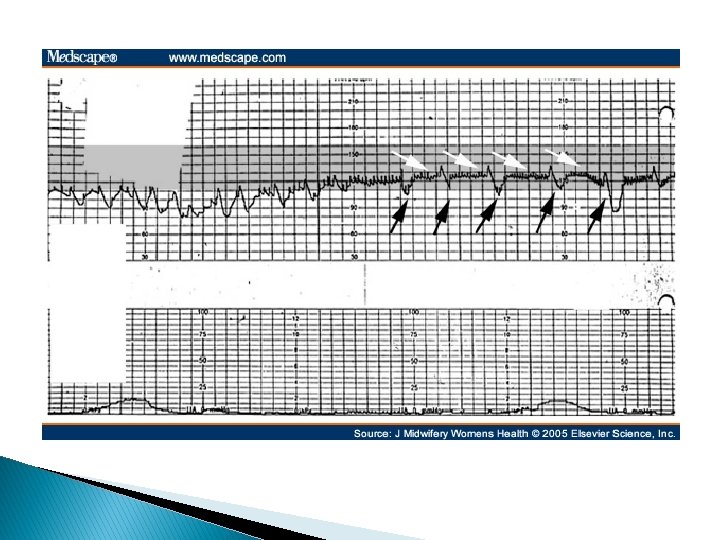
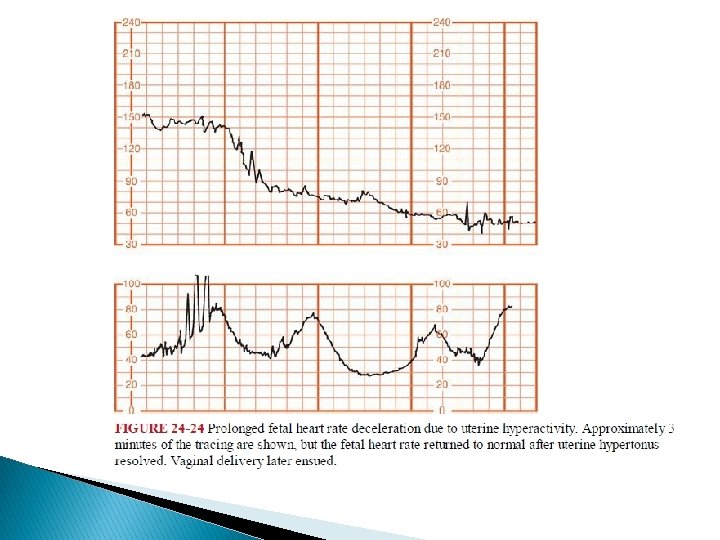
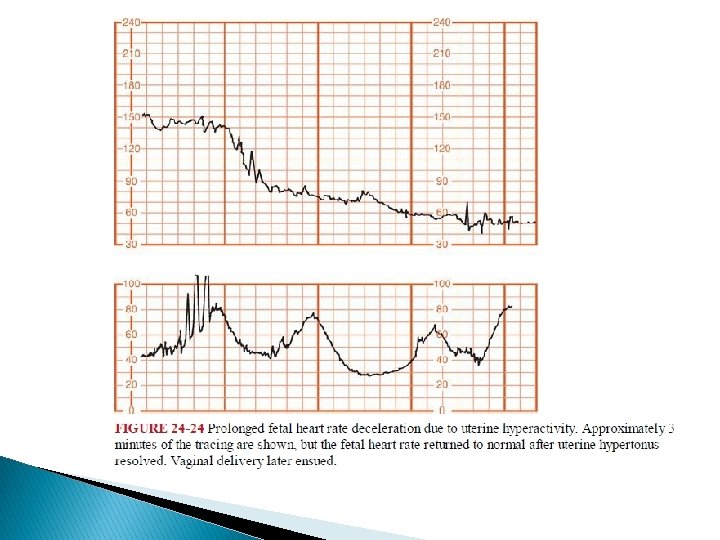
Prolonged Deceleration � This pattern, is defined as an isolated deceleration greater than 15 bpm lasting 2 minutes or longer but < 10 minutes from onset to return to baseline. � Prolonged decelerations are difficult to interpret because they are seen in many different clinical situations.
common causes of Prolonged Deceleration � cervical examination � uterine hyperactivity � cord entanglement � maternal supine hypotension � Epidural, spinal, or paracervical analgesia
� Eberle and coworkers (1998) reported that prolonged decelerations occurred in 4 percent of normal parturients given either epidural or intrathecal labor analgesia. � Hill and associates (2003) observed prolonged deceleration in 1 percent of women given epidural analgesia during labor at Parkland Hospital.
Other causes of prolonged deceleration � maternal hypoperfusion or hypoxia from any cause � placental abruption � umbilical cord knots or prolapse � maternal seizures including eclampsia and epilepsy � application of a fetal scalp electrode � impending birth � maternal Valsalva maneuver
� The placenta is very effective in resuscitating the fetus if the original insult does not recur immediately. � Occasionally, such self-limited prolonged decelerations are followed by loss of beat tobeat variability, baseline tachycardia, and even a period of late decelerations, all of which resolve as the fetus recovers.
� � Freeman and colleagues (2003) emphasize rightfully that the fetus may die during prolonged decelerations. Thus, management of prolonged decelerations can be extremely tenuous. Management of isolated prolonged decelerations is based on bedside clinical judgment, which inevitably will sometimes be imperfect given the unpredictability of these decelerations.

 Fetal heart rate deceleration
Fetal heart rate deceleration True sinusoidal pattern
True sinusoidal pattern Sinusoidal ctg
Sinusoidal ctg Veal chop mine
Veal chop mine Sinusoidal fetal heart rate
Sinusoidal fetal heart rate Fetal heart rate monitor
Fetal heart rate monitor Intrapartum meaning
Intrapartum meaning Elizabeth mulroney
Elizabeth mulroney What is physical changes
What is physical changes Fetal heart sound location
Fetal heart sound location Anterior pig
Anterior pig Nichd category
Nichd category Practoscope
Practoscope Find the average acceleration of a northbound subway
Find the average acceleration of a northbound subway The rate at which velocity changes.
The rate at which velocity changes. Heart dullness
Heart dullness How to dissect a sheep heart
How to dissect a sheep heart Stars plowhorses puzzles dogs
Stars plowhorses puzzles dogs Normal heart rate by age
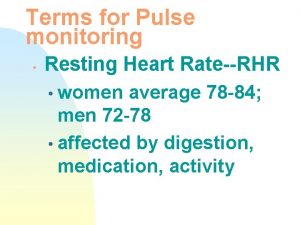
Normal heart rate by age Iht spirit heart rate monitors
Iht spirit heart rate monitors Resting heart rate women
Resting heart rate women Mhr=220-16
Mhr=220-16 Heart rate during exercise
Heart rate during exercise Heart rate of 80 bpm
Heart rate of 80 bpm Athletic heart rate
Athletic heart rate Apical pulse
Apical pulse Pediatric heart rate chart
Pediatric heart rate chart Pediatric heart rate chart
Pediatric heart rate chart Mhr zone
Mhr zone Is 80 bpm resting good
Is 80 bpm resting good Pulse
Pulse Heart rate during exercise
Heart rate during exercise How does music affect heart rate
How does music affect heart rate Athlete heart rate
Athlete heart rate Heat balance equation
Heat balance equation Heart rate during exercise
Heart rate during exercise Fast and easy ecg
Fast and easy ecg Respiration rate chart
Respiration rate chart Pseudoephedrine heart rate
Pseudoephedrine heart rate Target heart rate formula
Target heart rate formula Heart rate clicker
Heart rate clicker Membrane potential of cardiac muscle
Membrane potential of cardiac muscle American researcher who involved in getting heart rate
American researcher who involved in getting heart rate