Periarthritis Of Shoulder Joint DR M ABBASI RHEUMATOLOGIST
Periarthritis Of Shoulder Joint DR. M. ABBASI RHEUMATOLOGIST QUMS
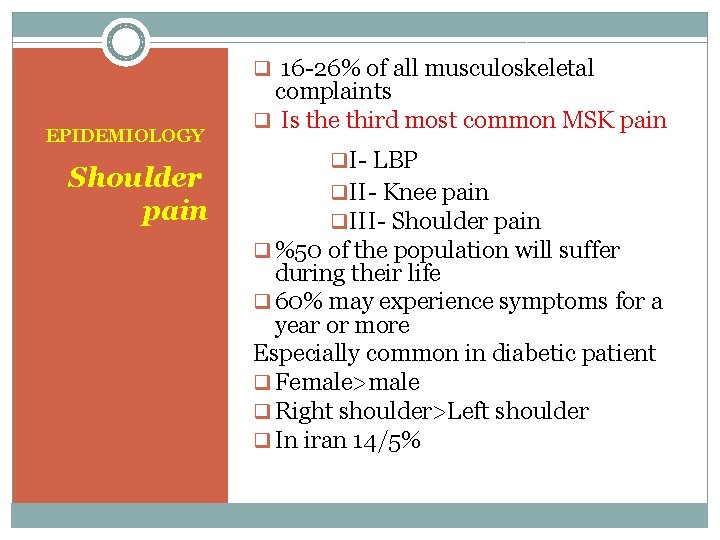
q 16 -26% of all musculoskeletal EPIDEMIOLOGY Shoulder pain complaints q Is the third most common MSK pain q. I- LBP q. II- Knee pain q. III- Shoulder pain q %50 of the population will suffer during their life q 60% may experience symptoms for a year or more Especially common in diabetic patient q Female>male q Right shoulder>Left shoulder q In iran 14/5%
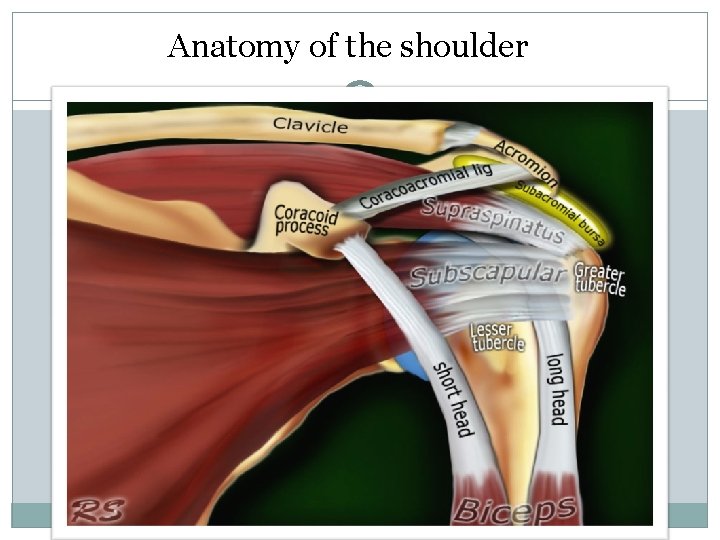
Anatomy of the shoulder

Anatomy of the shoulder
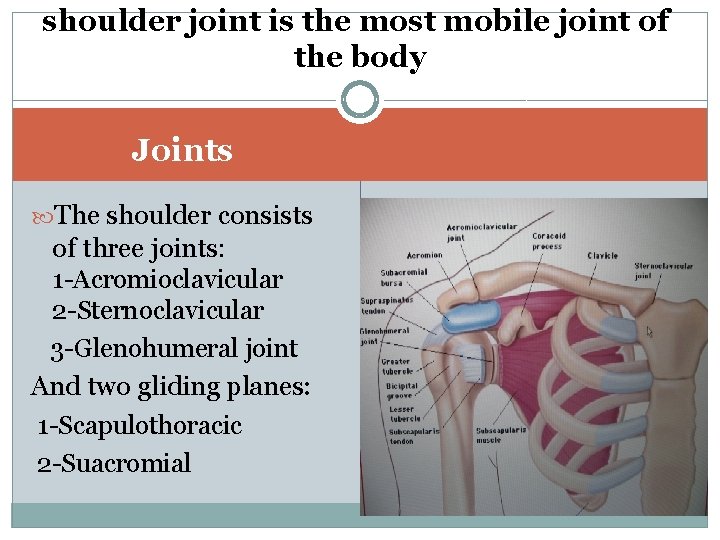
shoulder joint is the most mobile joint of the body Joints The shoulder consists of three joints: 1 -Acromioclavicular 2 -Sternoclavicular 3 -Glenohumeral joint And two gliding planes: 1 -Scapulothoracic 2 -Suacromial

Range of motion

Etiology of shoulder pain Periarticular disorders >80% Referral pain <15% Arthritis & OA 5%
Rotator cuff (R. C. ) tendinitis or common causes of periarticular disorders of shoulder impingement syndrome Rotator cuff tear Calcific tendinitis Bicipital tendinitis Frozen shoulder

Rotator cuff tendinitis Impingement may be defined as the encroachment of the acromion, coracoid process or AC joint on the rotator cuff as it passes beneath them during glenohumeral motion
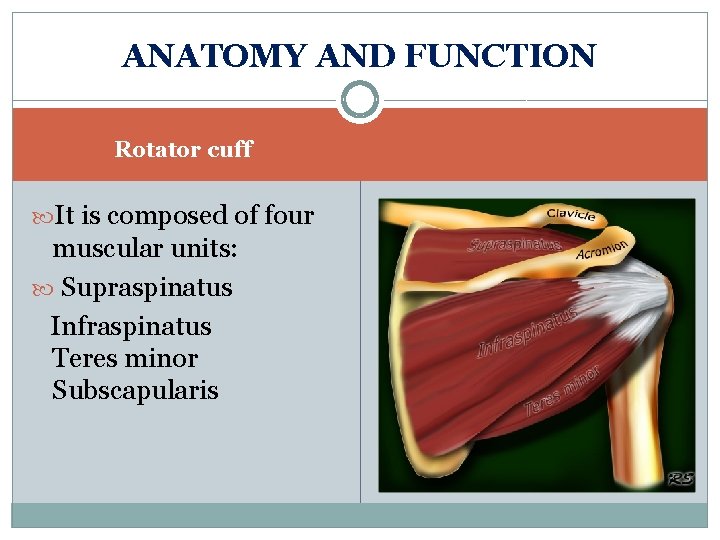
ANATOMY AND FUNCTION Rotator cuff It is composed of four muscular units: Supraspinatus Infraspinatus Teres minor Subscapularis
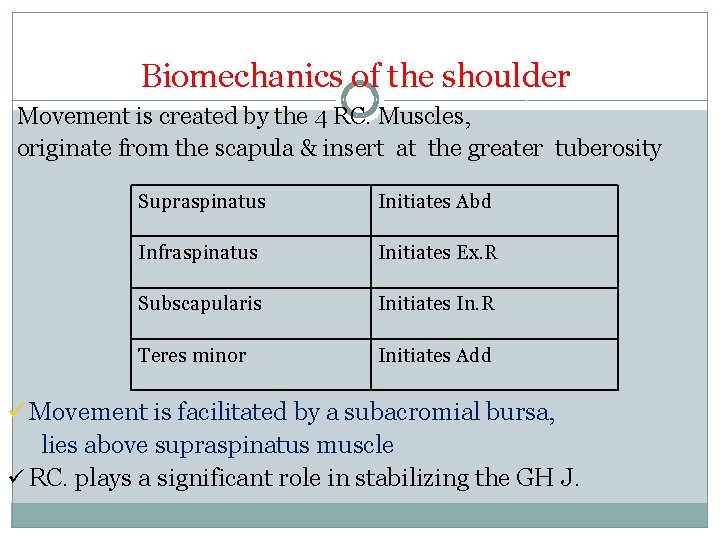
Biomechanics of the shoulder Movement is created by the 4 RC. Muscles, originate from the scapula & insert at the greater tuberosity Supraspinatus Initiates Abd Infraspinatus Initiates Ex. R Subscapularis Initiates In. R Teres minor Initiates Add ü Movement is facilitated by a subacromial bursa, lies above supraspinatus muscle ü RC. plays a significant role in stabilizing the GH J.
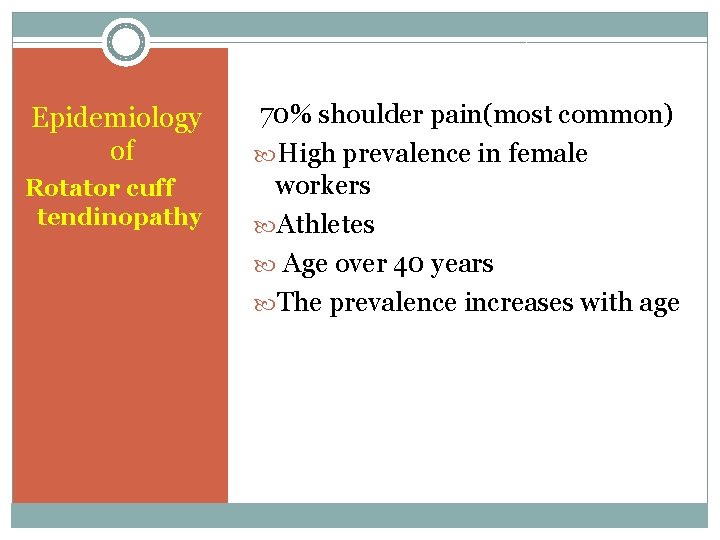
Epidemiology of Rotator cuff tendinopathy 70% shoulder pain(most common) High prevalence in female workers Athletes Age over 40 years The prevalence increases with age
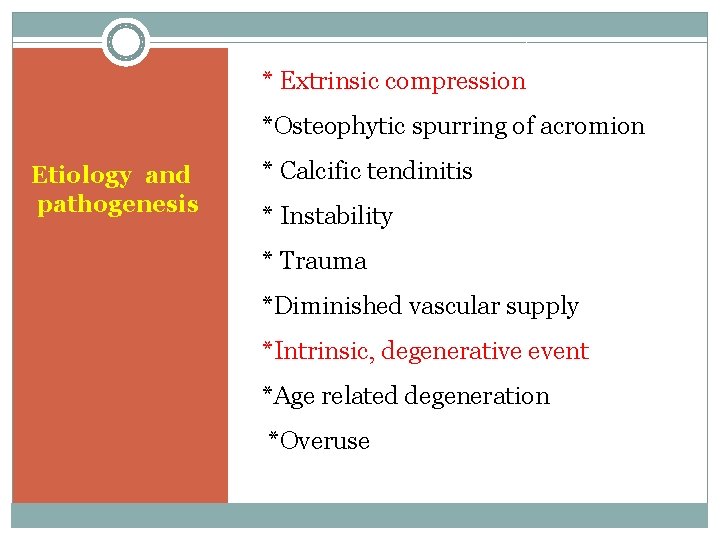
* Extrinsic compression *Osteophytic spurring of acromion Etiology and pathogenesis * Calcific tendinitis * Instability * Trauma *Diminished vascular supply *Intrinsic, degenerative event *Age related degeneration *Overuse
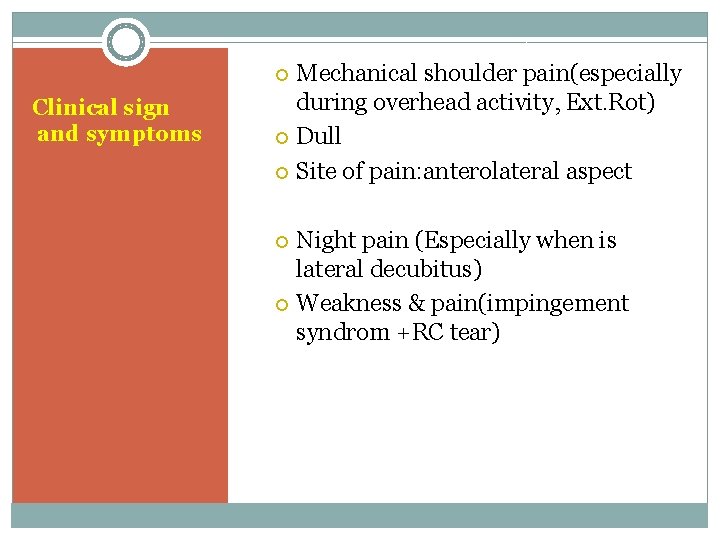
Mechanical shoulder pain(especially during overhead activity, Ext. Rot) Dull Site of pain: anterolateral aspect Clinical sign and symptoms Night pain (Especially when is lateral decubitus) Weakness & pain(impingement syndrom +RC tear)
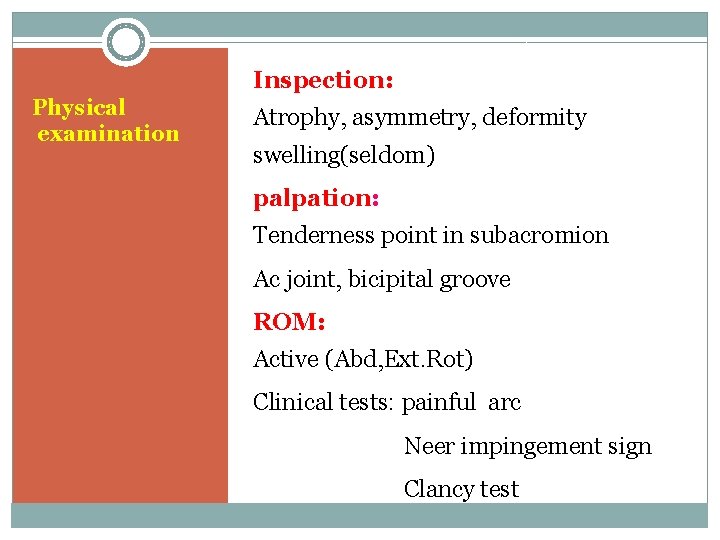
Inspection: Physical examination Atrophy, asymmetry, deformity swelling(seldom) palpation: Tenderness point in subacromion Ac joint, bicipital groove ROM: Active (Abd, Ext. Rot) Clinical tests: painful arc Neer impingement sign Clancy test

Physical examination

impingement sign Sensitivity 95% Specificity 95%

Clancy test Sensitivity: 95% Specificity : 95%
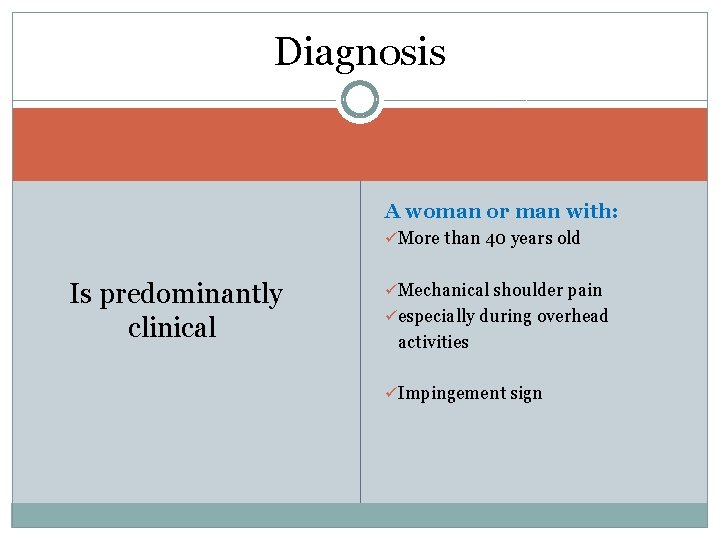
Diagnosis A woman or man with: üMore than 40 years old Is predominantly clinical üMechanical shoulder pain üespecially during overhead activities üImpingement sign
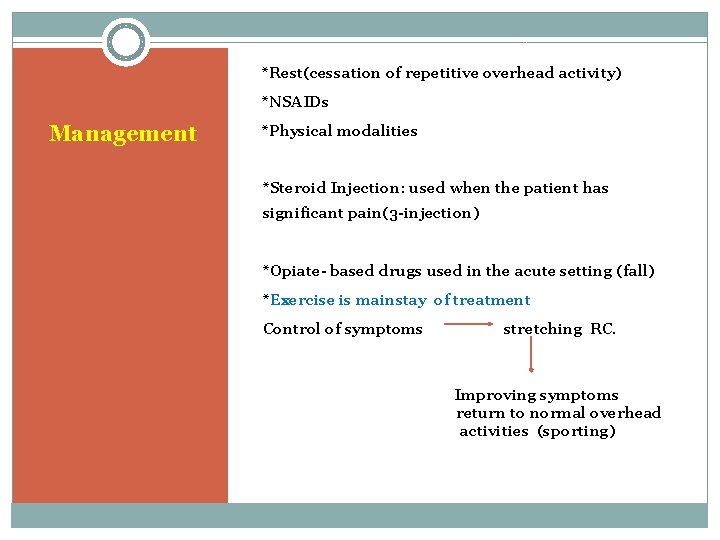
*Rest(cessation of repetitive overhead activity) *NSAIDs Management *Physical modalities *Steroid Injection: used when the patient has significant pain(3 -injection) *Opiate- based drugs used in the acute setting (fall) *Exercise is mainstay of treatment Control of symptoms stretching RC. Improving symptoms return to normal overhead activities (sporting)

Rotator cuff tear

Anatomy of the shoulder
SIZE: Rotator cuff tearing Small: <1 cm Medium: 1 -3 cm Large: 3 -5 cm Massive: >5 cm ETIOLOGY: RA, SLE, renal osteodystrophy Glucocorticoids Stage III rotator cuff tendinitis
Can be acute or chronic , complete Etiology or incomplete Acute: predominantly in young patient (falling on an outstretcharm) Chronic : predominantly in old patient>50 Y History of trauma (50%) History of chronic impingement (95%) Decreased vascularity &cellularity
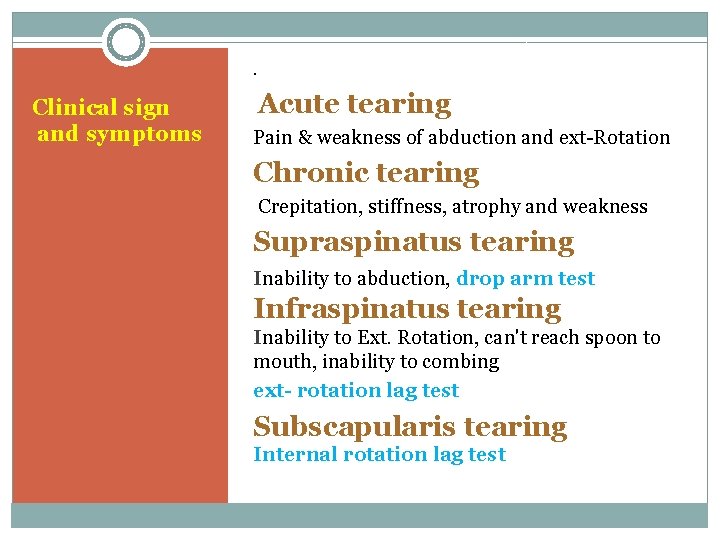
. Clinical sign and symptoms Acute tearing Pain & weakness of abduction and ext-Rotation Chronic tearing Crepitation, stiffness, atrophy and weakness Supraspinatus tearing Inability to abduction, drop arm test Infraspinatus tearing Inability to Ext. Rotation, can't reach spoon to mouth, inability to combing ext- rotation lag test Subscapularis tearing Internal rotation lag test
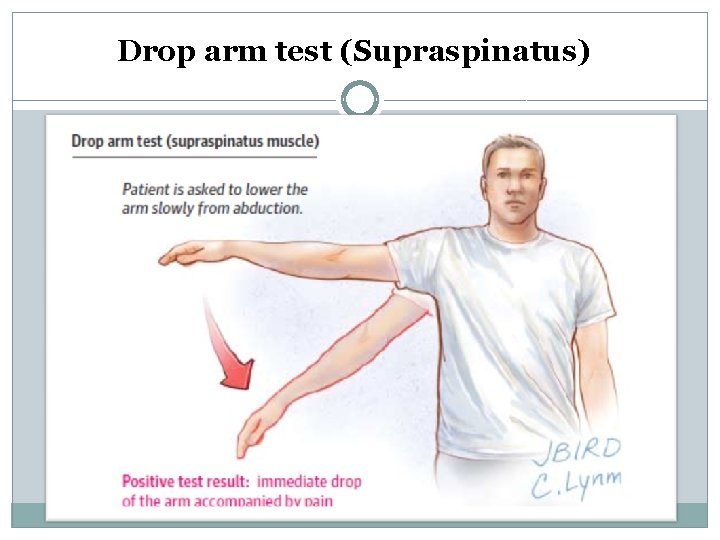
Drop arm test (Supraspinatus)
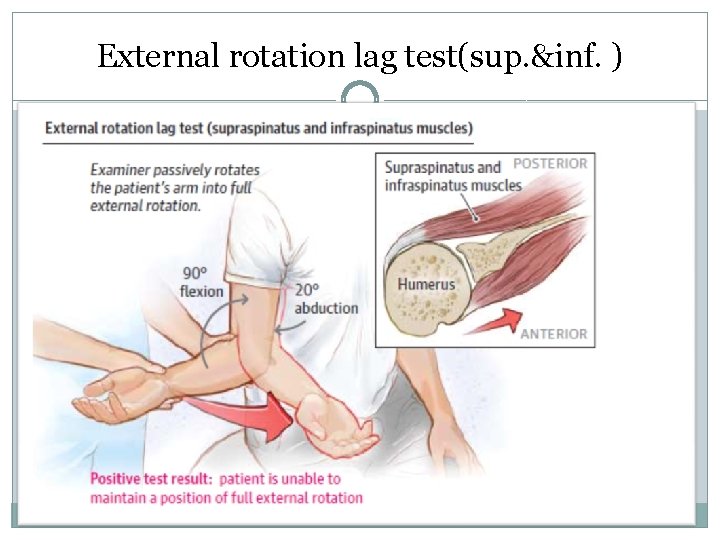
External rotation lag test(sup. &inf. )
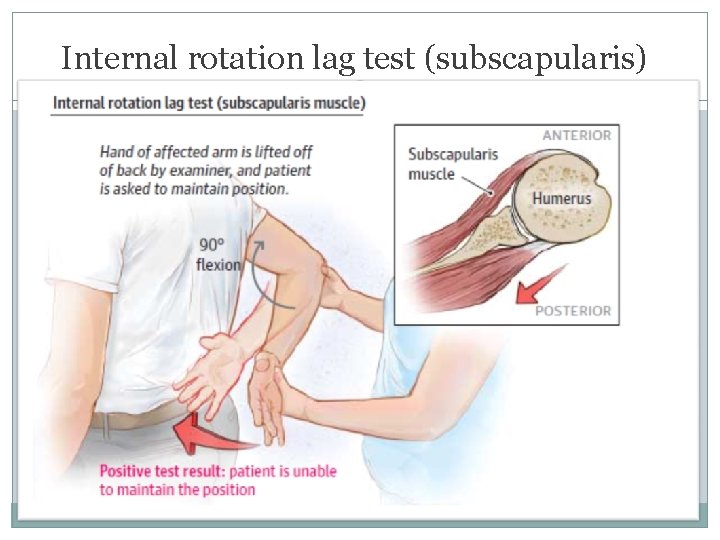
Internal rotation lag test (subscapularis)
Management ü Depend in the degree of tear ü Partial or full thickness - tears ü Age, functional status ü Degree of pain
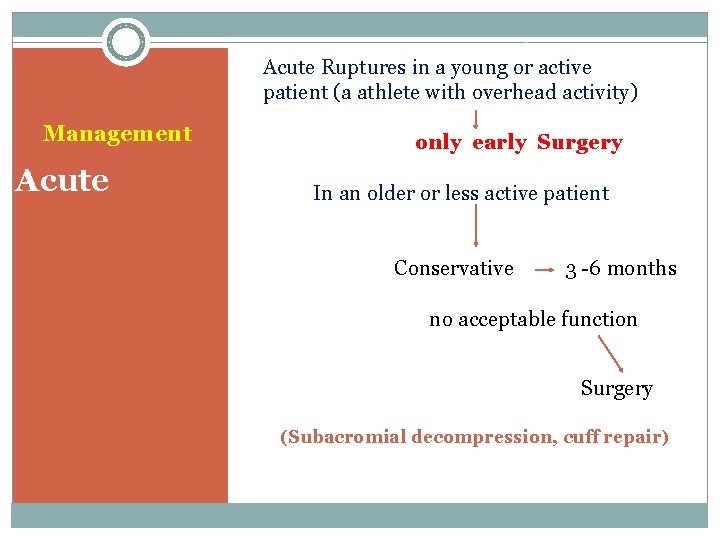
Acute Ruptures in a young or active patient (a athlete with overhead activity) Management Acute only early Surgery In an older or less active patient Conservative 3 -6 months no acceptable function Surgery (Subacromial decompression, cuff repair)
Treatment is conservative Treatment Surgery: Chronic 1. young patients with massive tearing and weakness 2. Old patients with sever pain that don’t control 3. RC tearing +biceps tendon tearing Response to conservative treatment (90% )

Biceps tendon FLEXION AND SUPINATION OF THE FOREARM FORWARD ELEVATION OF THE SHOULDER
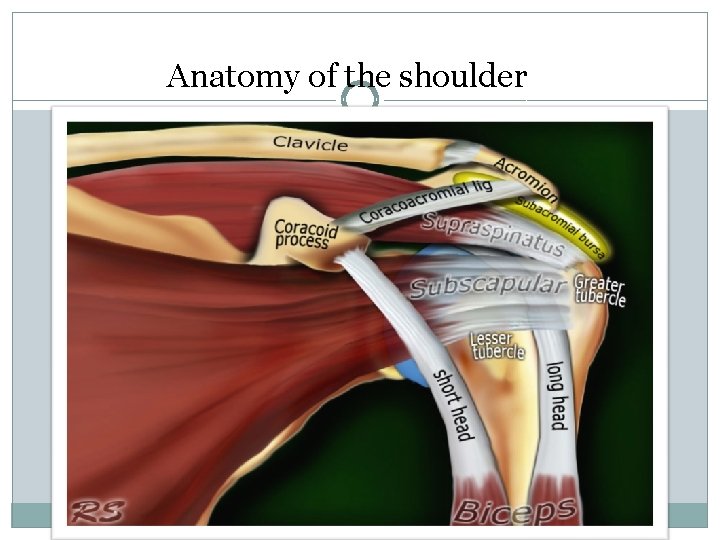
Anatomy of the shoulder
Men (halter) pidemiology of Bicipital tendinitis Women (gymnastic, repetitive carrying of small children)
Clinical sign and symptom *Pain over ant- aspect of the shoulder radiates to bicipital groove *Pain is exacerbated with overhead activities, shoulder extention & elbow flexion
Diagnostic maneuvers The most common finding Point tenderness by palpation of the bicipital groove Yergason's test Speed's test
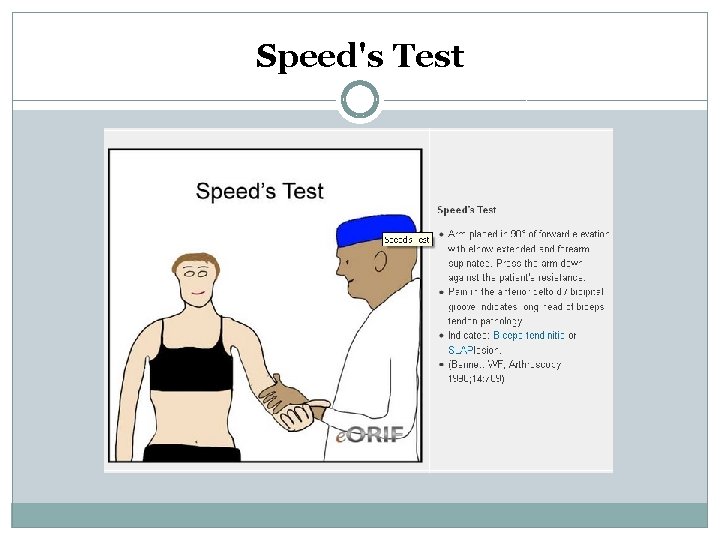
Speed's Test
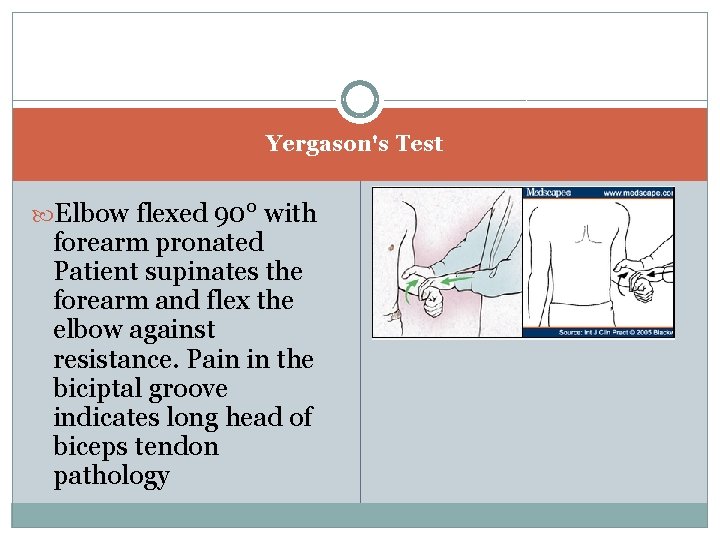
a Yergason's Test Elbow flexed 90° with forearm pronated Patient supinates the forearm and flex the elbow against resistance. Pain in the biciptal groove indicates long head of biceps tendon pathology

Bicipital rupture *ACUTE RUPTURE RESULT FROM OVERUSE IN YOUNG PATIENT(WEIGHT-LIFTING) SUDDEN PAIN (MOST COMMON) *IN OLDER PATIENT THINNING & EVENTUAL RUPTURE OCCUR SPONTANEOUSLY
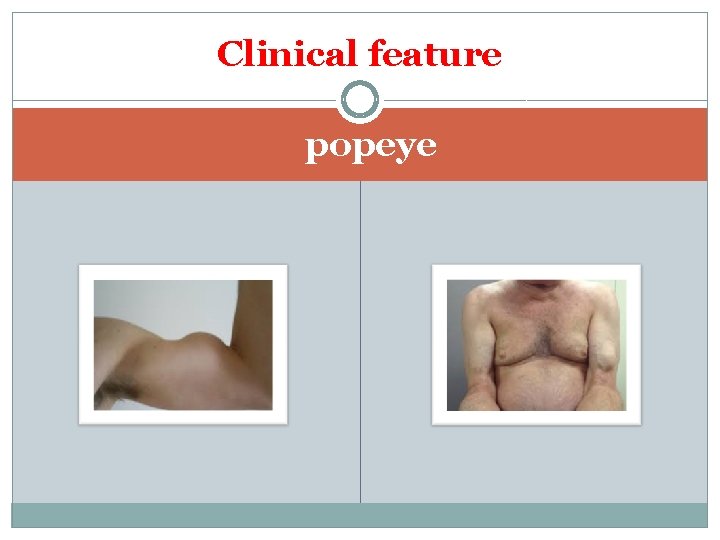
Clinical feature popeye
§ Plain radiography Paraclinic Degenerative changes in superior border of glenoid or bicipital groove
q. Ultrasonography (US) Imaging For detection of: q Subluxation q. Diagnosis of tears & tendinitis
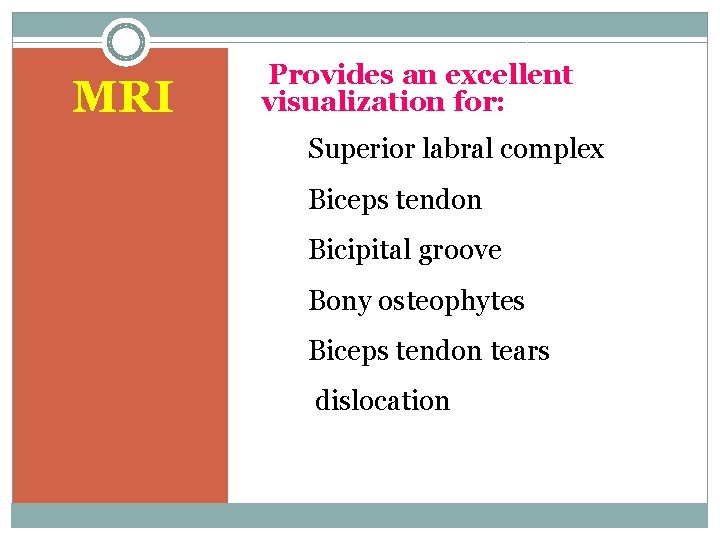
MRI Provides an excellent visualization for: Superior labral complex Biceps tendon Bicipital groove Bony osteophytes Biceps tendon tears dislocation
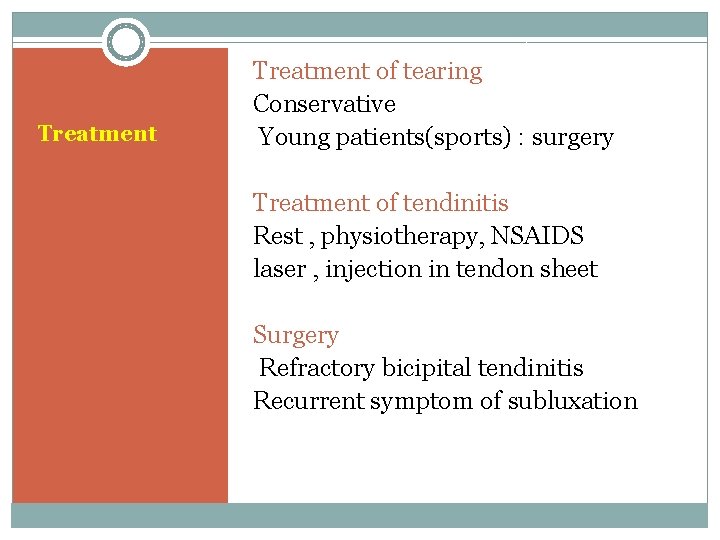
Treatment of tearing Conservative Young patients(sports) : surgery Treatment of tendinitis Rest , physiotherapy, NSAIDS laser , injection in tendon sheet Surgery Refractory bicipital tendinitis Recurrent symptom of subluxation

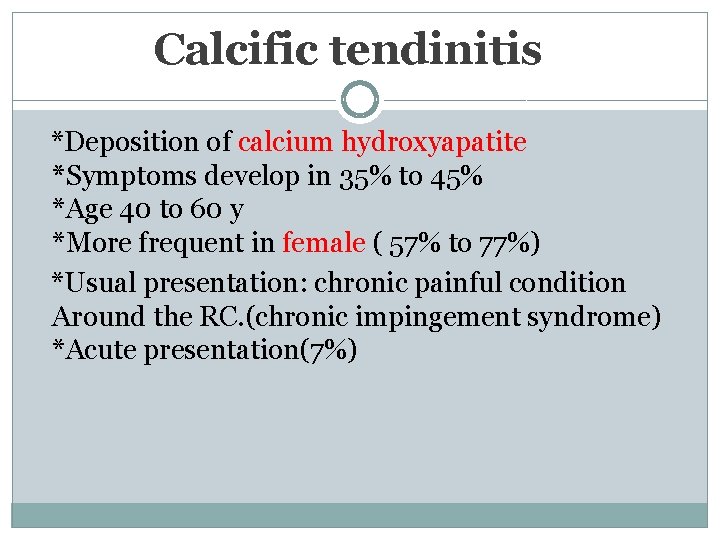
Calcific tendinitis *Deposition of calcium hydroxyapatite *Symptoms develop in 35% to 45% *Age 40 to 60 y *More frequent in female ( 57% to 77%) *Usual presentation: chronic painful condition Around the RC. (chronic impingement syndrome) *Acute presentation(7%)
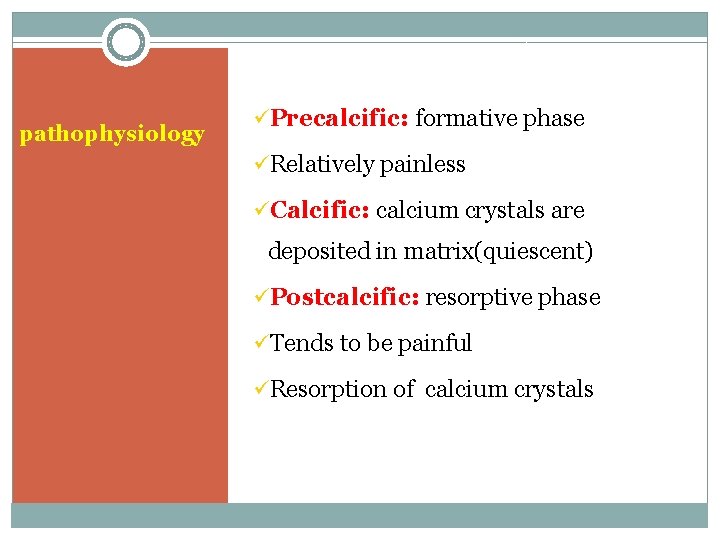
pathophysiology üPrecalcific: formative phase üRelatively painless üCalcific: calcium crystals are deposited in matrix(quiescent) üPostcalcific: resorptive phase üTends to be painful üResorption of calcium crystals
Acute shoulder pain (Resorptive phase) üAcute subacromial & subdeltoid bursitis üMigration of hydroxyapatite microcrystals to bursa: induce acute inflammation üAge: 50 -60 y, female
Acute severe pain Clinical history limiting active & passive movement Occasionally erythema Sometimes swelling No history of injury or overuse
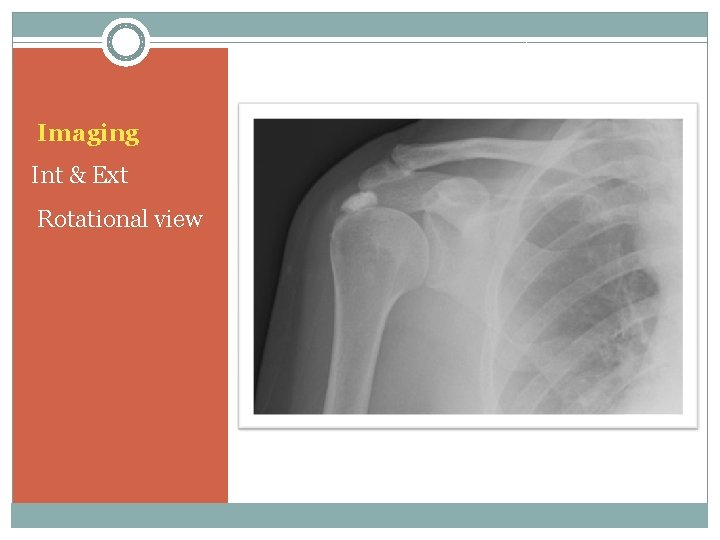
Imaging Int & Ext Rotational view
Chronic symptoms conservative treatment management Subacromial arthroscopy(stable phase) Acute stage Resting, the arm in sling NSAIDs Steroid injection (subacromial) Prednisolone: 15 -20 mg/day - Rapidly taper Recovery in few days or weeks

FROZEN SHOULDER (RETRACTILE CAPSULITIS)
Prevalence: 2 -3% EPIDEMIOLOGY Etiology Women 40 -50 years Primary or idiopathic Secondary: Diabetes, parkinsonism, TB, thyroid disorder, MI, lung tumor, Cervical radiculopathy Major skeletal trauma and soft tissue injury Change from simple or acute tendinitis to capsulitis(mixed shoulder)
Stage I Diffuse inflammatory synovitis pathophysiology Stage II Adherence of the capsule Stage III Loss of ROMof normal joint thickening and narrowing of joint capsule
Signs and symptoms Acute or insidious onset, pain at the extreme of motion, background ache in the suprascapular and deltoid regions Adhesive phase : 4 -12 mo Pain gradually decrease tation of active & passive ROM Resolution phase : ROM gradually will be better, duration without treatment lasts 1 -3 y
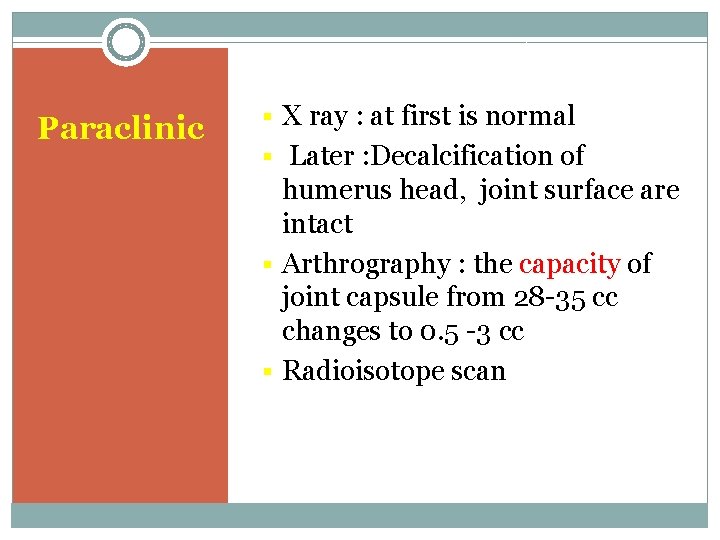
Paraclinic § X ray : at first is normal § Later : Decalcification of humerus head, joint surface are intact § Arthrography : the capacity of joint capsule from 28 -35 cc changes to 0. 5 -3 cc § Radioisotope scan
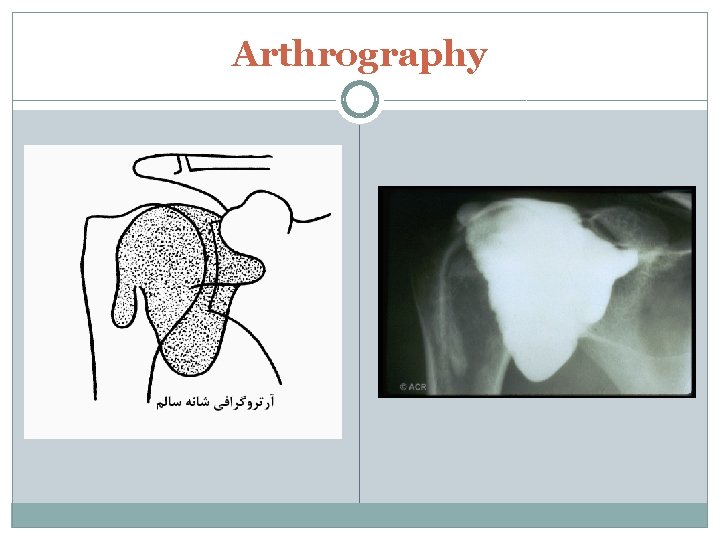
Arthrography

Arthrography
Exercise is the main treatment Gentle stretching Treatment Stage I § NSAID § Steroid injection § Oral steroid § Ice packs, ultrasound § Trans cutaneous electro neuron stimulation(TENS) Refractory conditions Close manipulation Hydraulic distention Surgery Arthroscopic capsulotomy

Thanks
- Slides: 66