Performance Physical Therapy for the Tactical Athlete Case
- Slides: 9
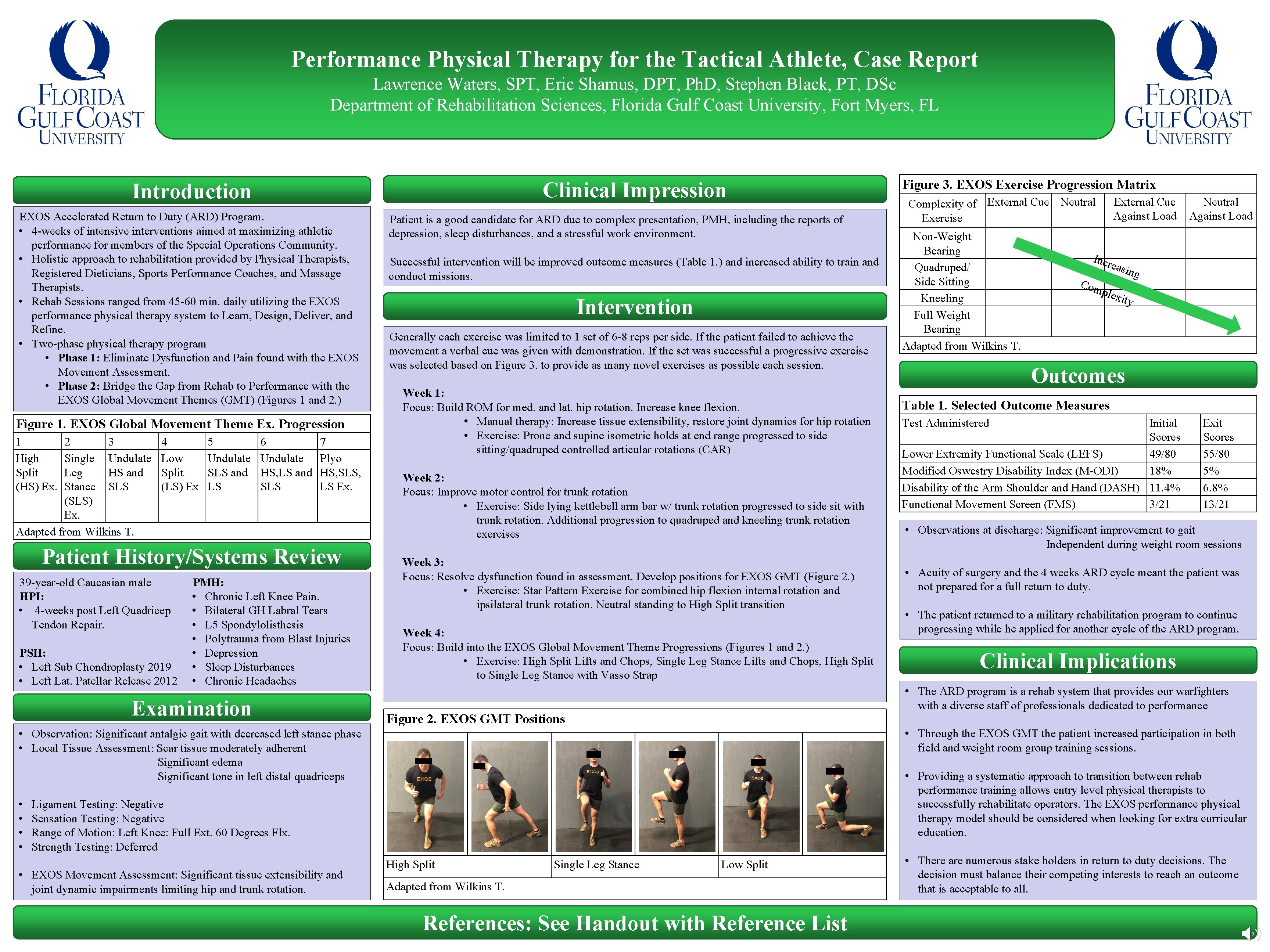
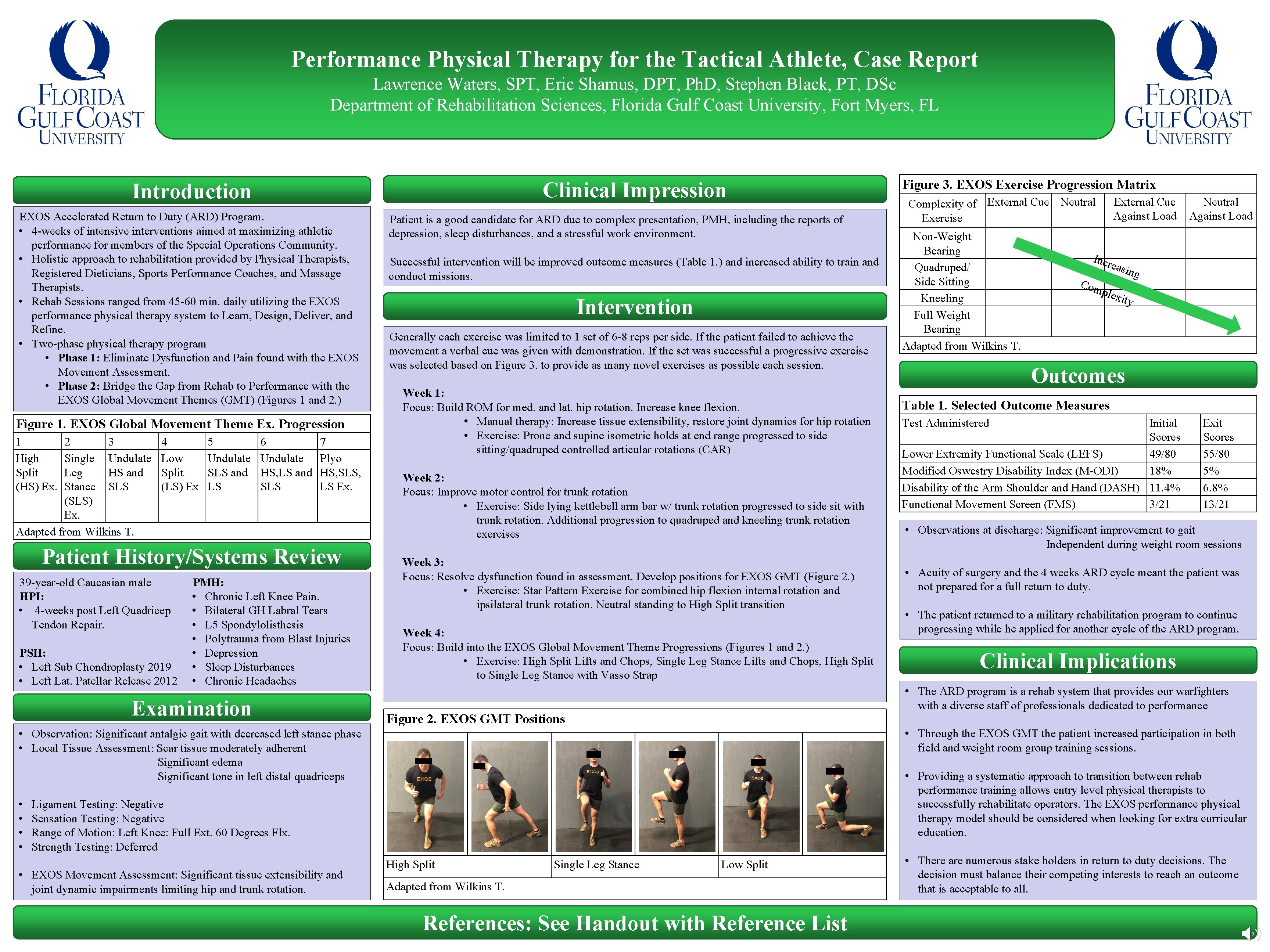
Performance Physical Therapy for the Tactical Athlete, Case Report Lawrence Waters, SPT, Eric Shamus, DPT, Ph. D, Stephen Black, PT, DSc Department of Rehabilitation Sciences, Florida Gulf Coast University, Fort Myers, FL Clinical Impression Introduction EXOS Accelerated Return to Duty (ARD) Program. • 4 -weeks of intensive interventions aimed at maximizing athletic performance for members of the Special Operations Community. • Holistic approach to rehabilitation provided by Physical Therapists, Registered Dieticians, Sports Performance Coaches, and Massage Therapists. • Rehab Sessions ranged from 45 -60 min. daily utilizing the EXOS performance physical therapy system to Learn, Design, Deliver, and Refine. • Two-phase physical therapy program • Phase 1: Eliminate Dysfunction and Pain found with the EXOS Movement Assessment. • Phase 2: Bridge the Gap from Rehab to Performance with the EXOS Global Movement Themes (GMT) (Figures 1 and 2. ) Figure 1. EXOS Global Movement Theme Ex. Progression 1 High Split (HS) Ex. 2 3 Single Undulate Leg HS and Stance SLS (SLS) Ex. Adapted from Wilkins T. 4 Low Split (LS) Ex 5 Undulate SLS and LS 6 Undulate HS, LS and SLS 7 Plyo HS, SLS, LS Ex. Patient History/Systems Review 39 -year-old Caucasian male HPI: • 4 -weeks post Left Quadricep Tendon Repair. PSH: • Left Sub Chondroplasty 2019 • Left Lat. Patellar Release 2012 PMH: • Chronic Left Knee Pain. • Bilateral GH Labral Tears • L 5 Spondylolisthesis • Polytrauma from Blast Injuries • Depression • Sleep Disturbances • Chronic Headaches Examination Patient is a good candidate for ARD due to complex presentation, PMH, including the reports of depression, sleep disturbances, and a stressful work environment. Successful intervention will be improved outcome measures (Table 1. ) and increased ability to train and conduct missions. Intervention Generally each exercise was limited to 1 set of 6 -8 reps per side. If the patient failed to achieve the movement a verbal cue was given with demonstration. If the set was successful a progressive exercise was selected based on Figure 3. to provide as many novel exercises as possible each session. Week 1: Focus: Build ROM for med. and lat. hip rotation. Increase knee flexion. • Manual therapy: Increase tissue extensibility, restore joint dynamics for hip rotation • Exercise: Prone and supine isometric holds at end range progressed to side sitting/quadruped controlled articular rotations (CAR) Week 2: Focus: Improve motor control for trunk rotation • Exercise: Side lying kettlebell arm bar w/ trunk rotation progressed to side sit with trunk rotation. Additional progression to quadruped and kneeling trunk rotation exercises Week 3: Focus: Resolve dysfunction found in assessment. Develop positions for EXOS GMT (Figure 2. ) • Exercise: Star Pattern Exercise for combined hip flexion internal rotation and ipsilateral trunk rotation. Neutral standing to High Split transition Week 4: Focus: Build into the EXOS Global Movement Theme Progressions (Figures 1 and 2. ) • Exercise: High Split Lifts and Chops, Single Leg Stance Lifts and Chops, High Split to Single Leg Stance with Vasso Strap Figure 2. EXOS GMT Positions Non-Weight Bearing Quadruped/ Side Sitting Kneeling Full Weight Bearing Adapted from Wilkins T. External Cue Against Load Incr Neutral Against Load easi ng Com plex ity Outcomes Table 1. Selected Outcome Measures Test Administered Initial Scores Lower Extremity Functional Scale (LEFS) 49/80 Modified Oswestry Disability Index (M-ODI) 18% Disability of the Arm Shoulder and Hand (DASH) 11. 4% Functional Movement Screen (FMS) 3/21 Exit Scores 55/80 5% 6. 8% 13/21 • Observations at discharge: Significant improvement to gait Independent during weight room sessions • Acuity of surgery and the 4 weeks ARD cycle meant the patient was not prepared for a full return to duty. • The patient returned to a military rehabilitation program to continue progressing while he applied for another cycle of the ARD program. Clinical Implications • Through the EXOS GMT the patient increased participation in both field and weight room group training sessions. • Providing a systematic approach to transition between rehab performance training allows entry level physical therapists to successfully rehabilitate operators. The EXOS performance physical therapy model should be considered when looking for extra curricular education. Ligament Testing: Negative Sensation Testing: Negative Range of Motion: Left Knee: Full Ext. 60 Degrees Flx. Strength Testing: Deferred • EXOS Movement Assessment: Significant tissue extensibility and joint dynamic impairments limiting hip and trunk rotation. Complexity of External Cue Neutral Exercise • The ARD program is a rehab system that provides our warfighters with a diverse staff of professionals dedicated to performance • Observation: Significant antalgic gait with decreased left stance phase • Local Tissue Assessment: Scar tissue moderately adherent Significant edema Significant tone in left distal quadriceps • • Figure 3. EXOS Exercise Progression Matrix High Split Single Leg Stance Low Split Adapted from Wilkins T. References: See Handout with Reference List • There are numerous stake holders in return to duty decisions. The decision must balance their competing interests to reach an outcome that is acceptable to all.
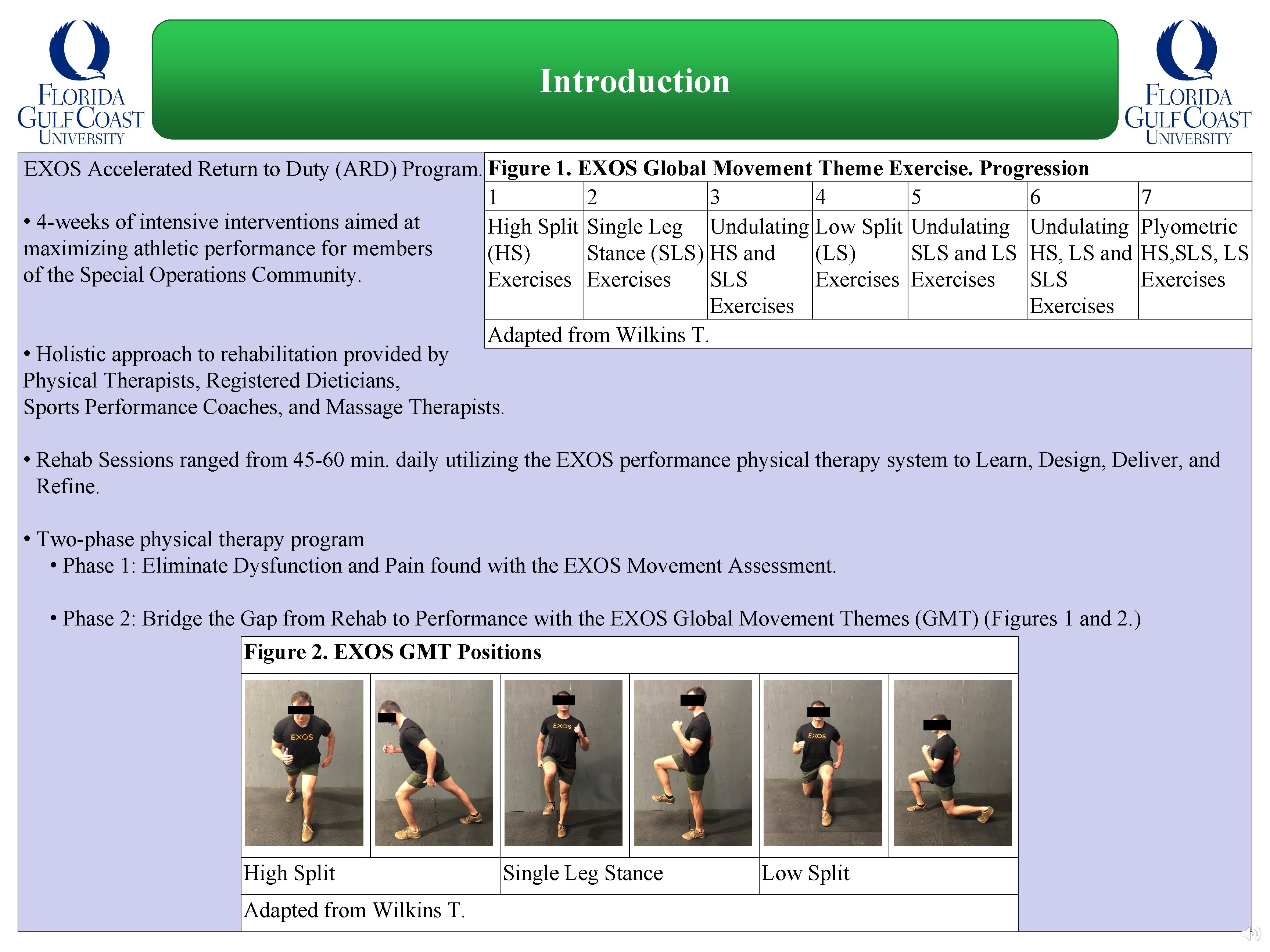
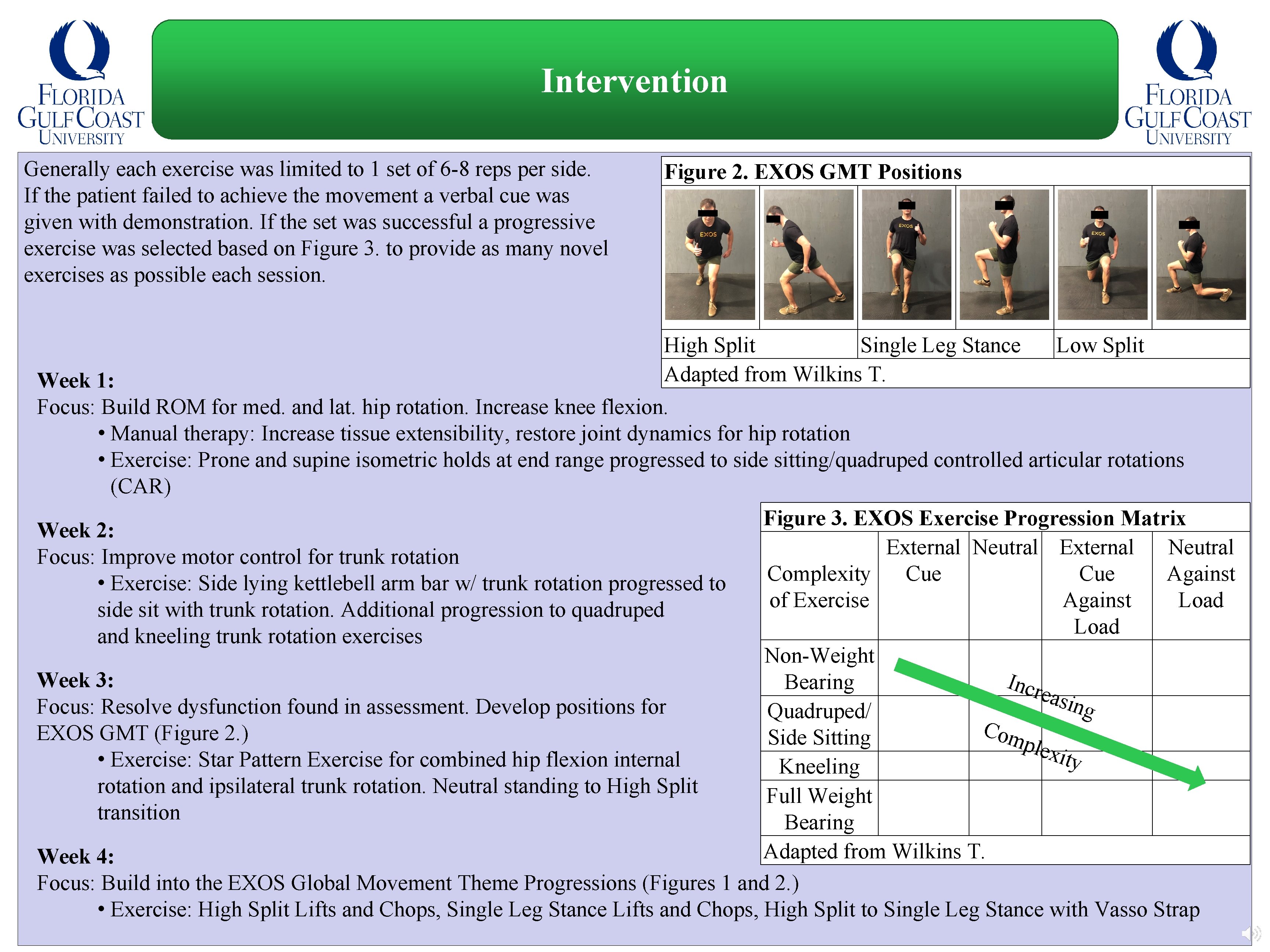
Introduction EXOS Accelerated Return to Duty (ARD) Program. Figure 1. EXOS Global Movement Theme Exercise. Progression 1 2 3 4 5 6 • 4 -weeks of intensive interventions aimed at High Split Single Leg Undulating Low Split Undulating maximizing athletic performance for members (HS) Stance (SLS) HS and (LS) SLS and LS HS, LS and of the Special Operations Community. Exercises SLS Exercises Adapted from Wilkins T. • Holistic approach to rehabilitation provided by Physical Therapists, Registered Dieticians, Sports Performance Coaches, and Massage Therapists. 7 Plyometric HS, SLS, LS Exercises • Rehab Sessions ranged from 45 -60 min. daily utilizing the EXOS performance physical therapy system to Learn, Design, Deliver, and Refine. • Two-phase physical therapy program • Phase 1: Eliminate Dysfunction and Pain found with the EXOS Movement Assessment. • Phase 2: Bridge the Gap from Rehab to Performance with the EXOS Global Movement Themes (GMT) (Figures 1 and 2. ) Figure 2. EXOS GMT Positions High Split Adapted from Wilkins T. Single Leg Stance Low Split
Patient History and Systems Review 39 -year-old Caucasian male HPI: • 4 -weeks post Left Quadricep Tendon Repair. PSH: • Left Knee Sub Chondroplasty 2019 • Left Lat. Patellar Release 2012 PMH: • Chronic Left Knee Pain. • Bilateral GH Labral Tears • L 5 Spondylolisthesis • Polytrauma from Blast Injuries • Depression • Sleep Disturbances • Chronic Headaches
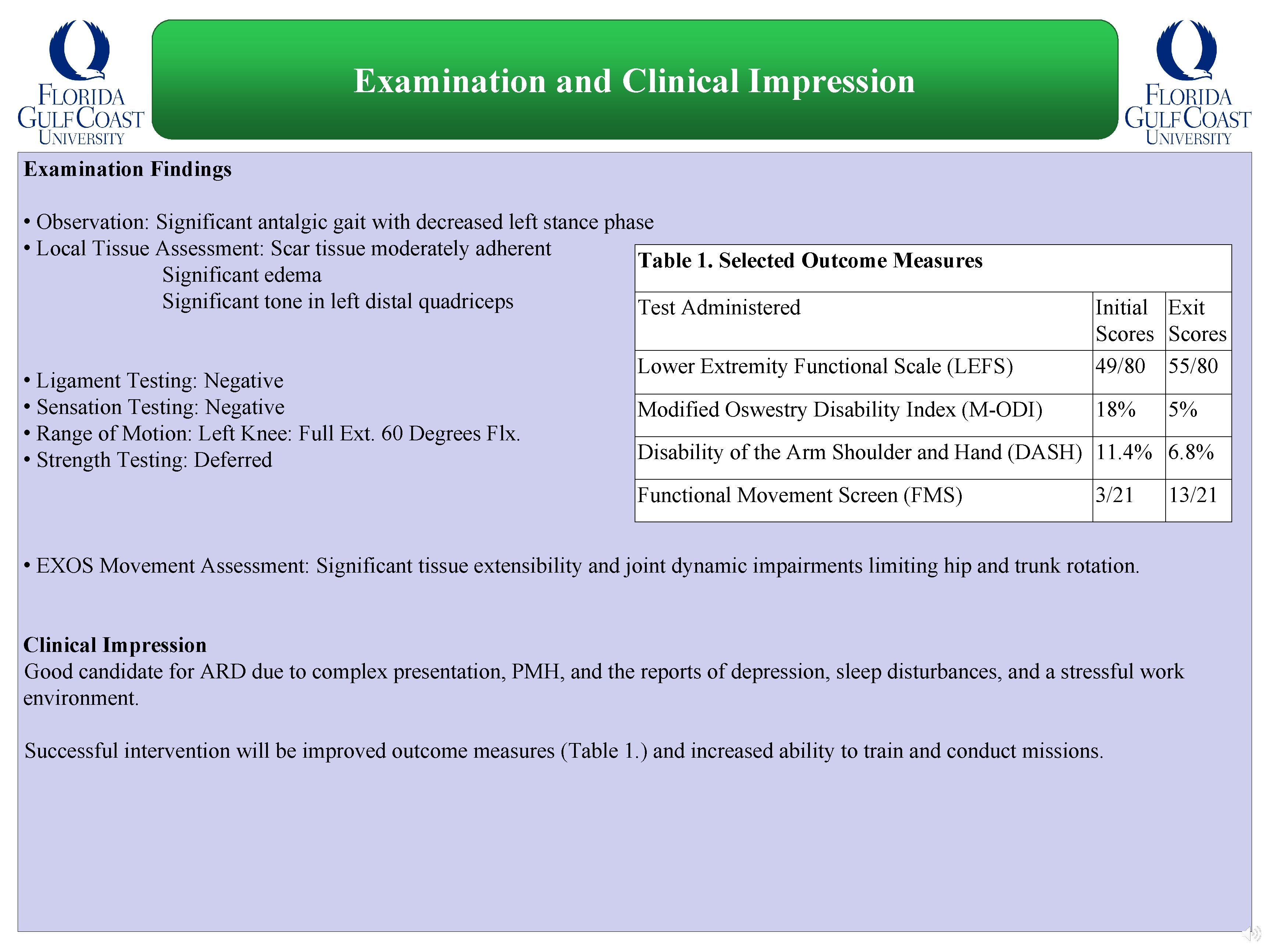
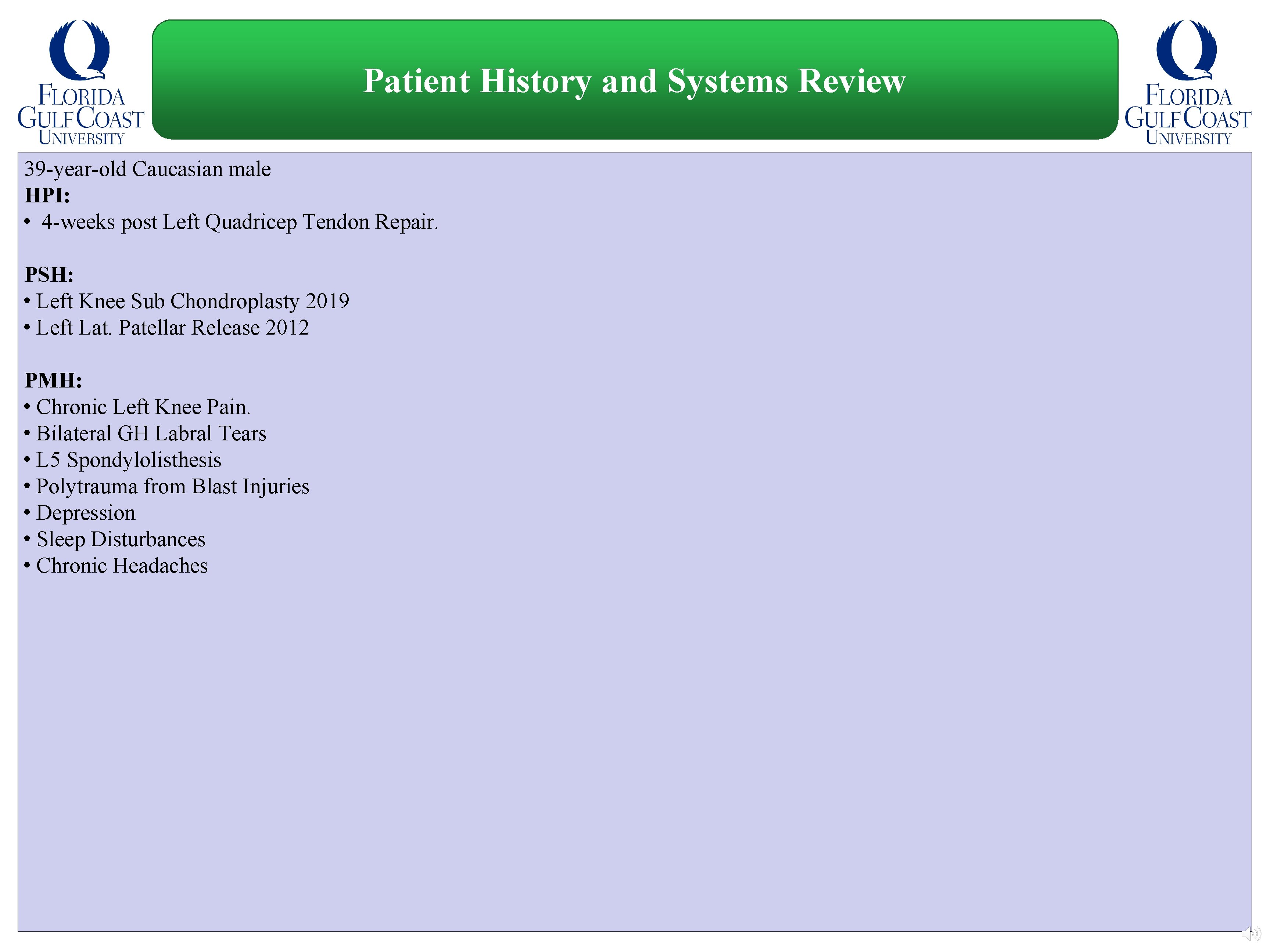
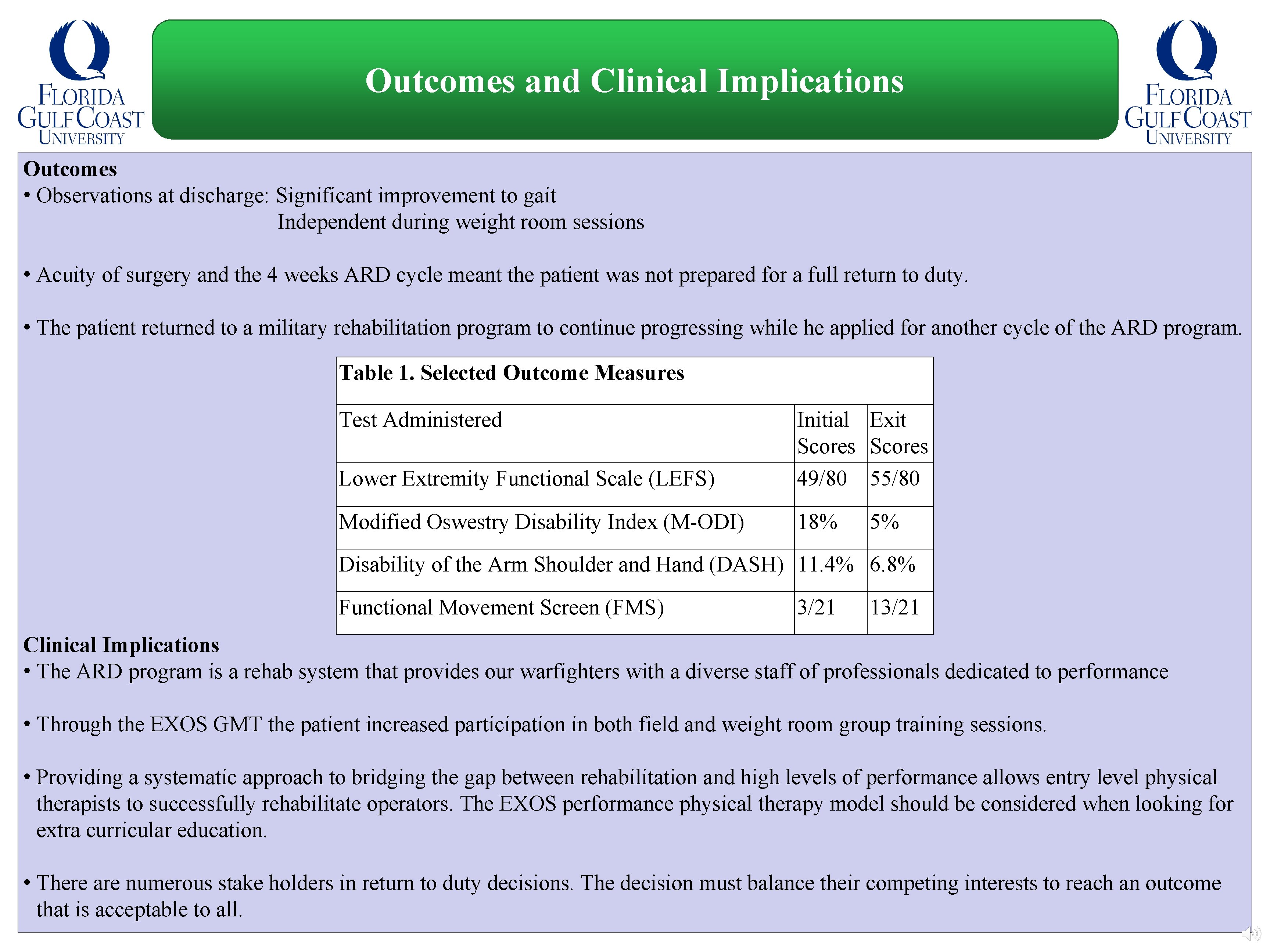
Examination and Clinical Impression Examination Findings • Observation: Significant antalgic gait with decreased left stance phase • Local Tissue Assessment: Scar tissue moderately adherent Table 1. Selected Outcome Measures Significant edema Significant tone in left distal quadriceps Test Administered • Ligament Testing: Negative • Sensation Testing: Negative • Range of Motion: Left Knee: Full Ext. 60 Degrees Flx. • Strength Testing: Deferred Lower Extremity Functional Scale (LEFS) Initial Exit Scores 49/80 55/80 Modified Oswestry Disability Index (M-ODI) 18% 5% Disability of the Arm Shoulder and Hand (DASH) 11. 4% 6. 8% Functional Movement Screen (FMS) 3/21 13/21 • EXOS Movement Assessment: Significant tissue extensibility and joint dynamic impairments limiting hip and trunk rotation. Clinical Impression Good candidate for ARD due to complex presentation, PMH, and the reports of depression, sleep disturbances, and a stressful work environment. Successful intervention will be improved outcome measures (Table 1. ) and increased ability to train and conduct missions.
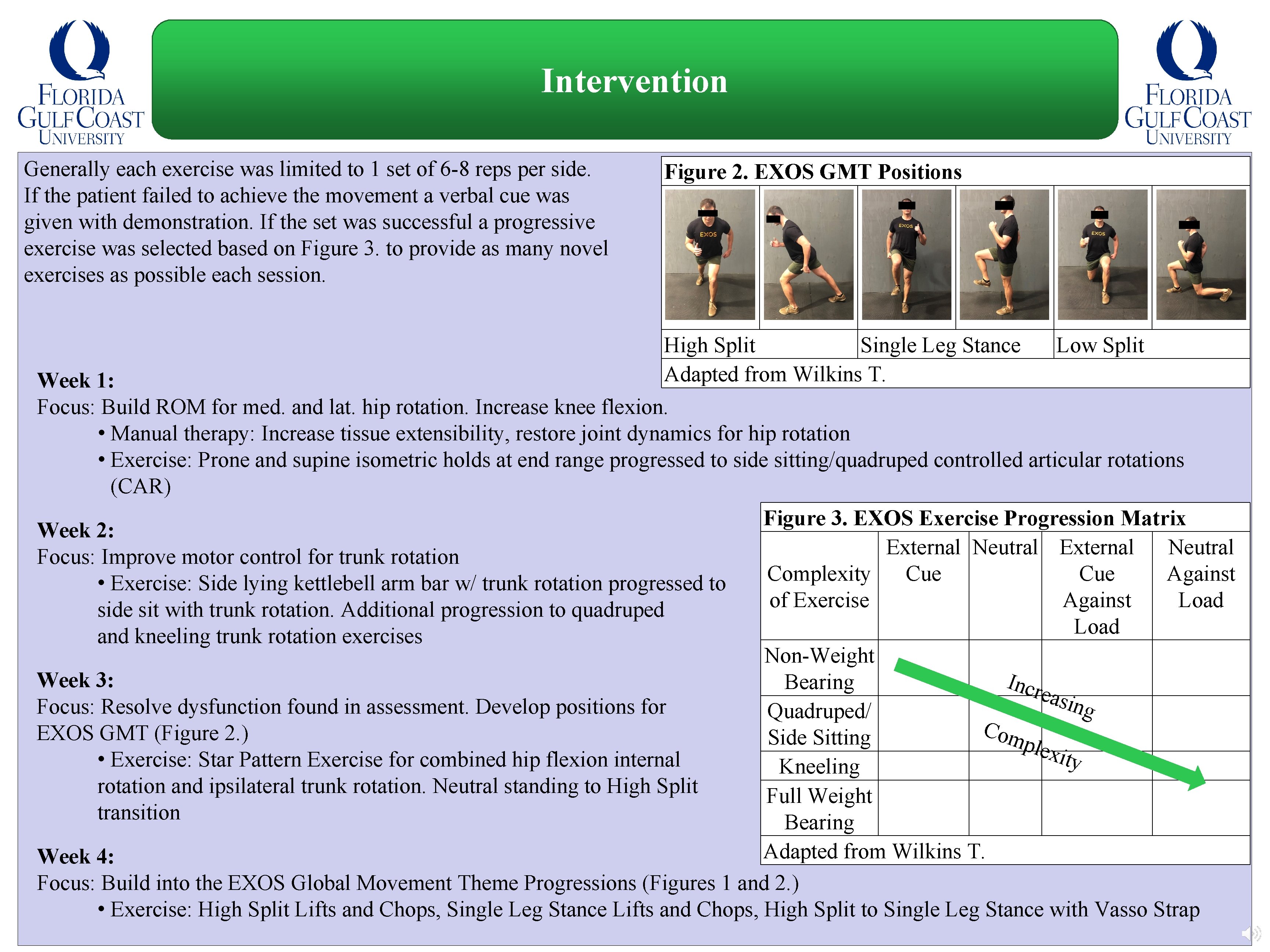
Intervention Generally each exercise was limited to 1 set of 6 -8 reps per side. If the patient failed to achieve the movement a verbal cue was given with demonstration. If the set was successful a progressive exercise was selected based on Figure 3. to provide as many novel exercises as possible each session. Figure 2. EXOS GMT Positions High Split Single Leg Stance Low Split Adapted from Wilkins T. Week 1: Focus: Build ROM for med. and lat. hip rotation. Increase knee flexion. • Manual therapy: Increase tissue extensibility, restore joint dynamics for hip rotation • Exercise: Prone and supine isometric holds at end range progressed to side sitting/quadruped controlled articular rotations (CAR) Figure 3. EXOS Exercise Progression Matrix Week 2: External Neutral Focus: Improve motor control for trunk rotation Complexity Cue Against • Exercise: Side lying kettlebell arm bar w/ trunk rotation progressed to of Exercise Against Load side sit with trunk rotation. Additional progression to quadruped Load and kneeling trunk rotation exercises Non-Weight Week 3: Incr Bearing easi n Focus: Resolve dysfunction found in assessment. Develop positions for g Quadruped/ C omp EXOS GMT (Figure 2. ) Side Sitting lexi t • Exercise: Star Pattern Exercise for combined hip flexion internal y Kneeling rotation and ipsilateral trunk rotation. Neutral standing to High Split Full Weight transition Bearing Adapted from Wilkins T. Week 4: Focus: Build into the EXOS Global Movement Theme Progressions (Figures 1 and 2. ) • Exercise: High Split Lifts and Chops, Single Leg Stance Lifts and Chops, High Split to Single Leg Stance with Vasso Strap
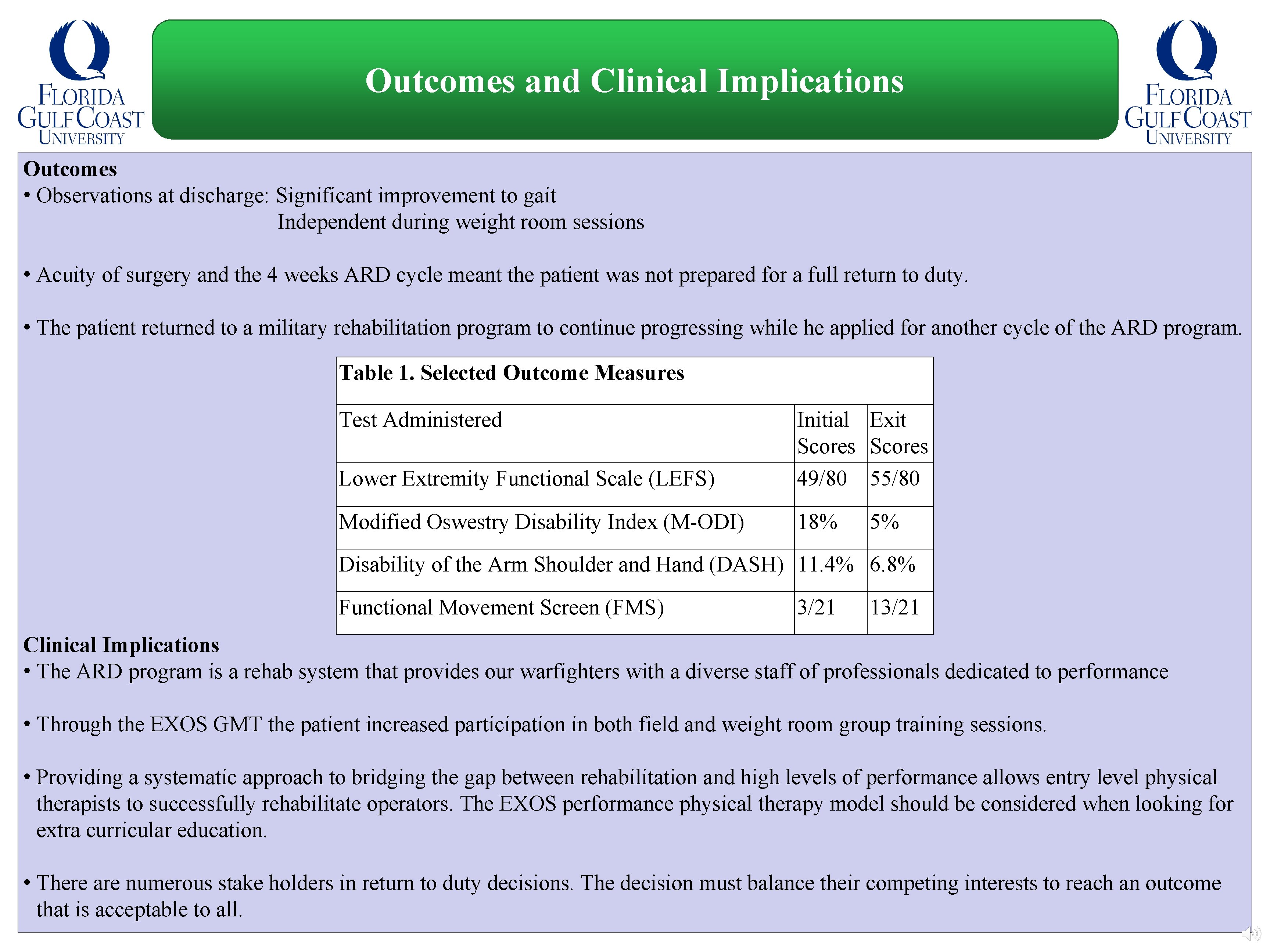
Outcomes and Clinical Implications Outcomes • Observations at discharge: Significant improvement to gait Independent during weight room sessions • Acuity of surgery and the 4 weeks ARD cycle meant the patient was not prepared for a full return to duty. • The patient returned to a military rehabilitation program to continue progressing while he applied for another cycle of the ARD program. Table 1. Selected Outcome Measures Test Administered Lower Extremity Functional Scale (LEFS) Initial Exit Scores 49/80 55/80 Modified Oswestry Disability Index (M-ODI) 18% 5% Disability of the Arm Shoulder and Hand (DASH) 11. 4% 6. 8% Functional Movement Screen (FMS) 3/21 13/21 Clinical Implications • The ARD program is a rehab system that provides our warfighters with a diverse staff of professionals dedicated to performance • Through the EXOS GMT the patient increased participation in both field and weight room group training sessions. • Providing a systematic approach to bridging the gap between rehabilitation and high levels of performance allows entry level physical therapists to successfully rehabilitate operators. The EXOS performance physical therapy model should be considered when looking for extra curricular education. • There are numerous stake holders in return to duty decisions. The decision must balance their competing interests to reach an outcome that is acceptable to all.
References 1. Shaffer SW, Moore JH. U. S. Army physical therapist roles and contributions in operations Enduring Freedom and Iraqi Freedom. U Army Med Dept J. 2016 Apr-Sep; (2 -16): 52 -7. 2. Moore JH, Goffar SL, Teyhen DS, Pendergrass TL, Childs JD, Ficke JR. The role of U. S. military physical therapists during recent combat campaigns. Phys Ther. 2013; 93(9): 1268 -75. 3. Hospitalizations, active component, U. S. armed forces, 2016. Medical Surveillance Monthly Report. 2017; 24(4): 9. 4. Jones BH, Canham-Chervak M, Canada S, Mitchener TA, Moore S. Medical surveillance of injuries in the U. S. military descriptive epidemiology and recommendations for improvement. Am J Prev Med. 2010; 38(1 suppl): S 42 -60. 5. Gutierrez E. Soldier musculoskeletal injuries, risk factors, and recommendations. NSCA TSAC Report. 2019; (53): 28 -35. 6. Davis JD. A review of musculoskeletal injuries in the United States Army: demographics, risk factors, and the role of the physical therapist in prevention and return to duty. NSCA TSAC Report. 2017; (47): 6 -11. 7. Roy TC, Knapik JJ, Ritland BM, Murphy N, Sharp MA. Risk factors for musculoskeletal injuries for soldiers deployed to Afghanistan. Aviat Space Environ Med. 2012 Nov; 83(11): 1060 -6. 8. Roy TC, Ritland BM, Sharp MA. A description of injuries in men and women while serving in Afghanistan. Military Med. 2015 Feb; 180(2): 126 -31. 9. Abt JP, Sell TC, Lovalekar MT, et al. Injury epidemiology of U. S. Army special operations forces. Military Med. 2014 Oct; 179(10): 1106 -12. 10. Bucci S. The importance of special operations forces today and going forward. Index of U. S. Military Strength. 2015. https: //www. heritage. org/military-strength-topical-essays/2015 -essays/the-importance-special-operations-forces-todayand 11. Sell K, Deuster PA, NSCA-National Strength & Conditioning Association, National Strength & Conditioning Association (U. S. ) Staff. NSCA'S Essentials of Tactical Strength and Conditioning. Champaign, IL: Human Kinetics Publishers; 2017. ISBN: 9781492546184 12. Carlton SD, Orr RM. The impact of occupational load carriage on carrier mobility: A critical review of the literature. Int J Occup Saf Ergon. 2014; 20(1): 33 -41.
References 13. Smith L, Westrick R, Sauers S, Cooper A, Scofield D, et al. Underreporting of musculoskeletal injuries in the U. S. Army. Sports Health. 2016; 8(6): 507 -13. 14. Knapik JJ, Rieger W, Palkoska F, Van Camp S, Darakjy S. United States Army physical readiness training: Rationale and evaluation of the physical training doctrine. J Strength Cond Res. 2009; 23(4): 1353 -62. 15. Chalupa R, Aberle C, Johnson A. Observed rates of lower extremity stress fractures after implementation of the army physical readiness training program at JBSA Fort Sam Houston. U Army Med Dep J. 2016 Jan-Mar; (1 -16): 6 -9. 16. Kelly TK, Masi R, Walker B, Knapp S, Leuschner KJ. An assessment of the army's tactical human optimization, rapid rehabilitation and reconditioning program. Rand Health Q. 2013 Jun; 3(2): 8. 17. Grier T, Anderson MK, Depenbrock P, Eiserman R, Nindl BC, Jones BH. Evaluation of the US army special forces tactical human optimization, rapid rehabilitation, and reconditioning program. J Spec Oper Med. 2018; 18(2): 42 -8. 18. Robson S, Lytell MC, Sims CS, et al. Fit for duty? Evaluating the physical fitness requirements of battlefield airmen. Rand Health Q. 2018 Jan; 7(2): 8. 19. Abt J. USASOC injury prevention/performance optimization musculoskeletal screening initiative. 2012. https: //apps. dtic. mil/docs/citations/ADA 610969 20. Goss DL, Christopher GE, Faulk RT, Moore J. Functional training program bridges rehabilitation and return to duty. J Spec Oper Med. 2009; 9(2): 29 -48. 21. Gutschick JH, Lazicki RS. Returning a special operations candidate to duty following an airborne operation injury: A case report. Int J Sports Phys. 2020; 15(1): 1 -12. 22. Wilkins T. EXOS physical therapy framework. January 2020 Pensacola Fl. 23. Nicholas MK, Linton SJ, Watson PJ, Main CJ. The “Decade of the Flags” Working Group. Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: a reappraisal. Phys Ther. 2011; 91(5): 737 -53. 24. Gouin J, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: Methods and mechanisms. Crit Care Nurs Clin North Am. 2012; 24(2): 201 -13. 25. Kollock RO, Lyons M, Sanders G, Hale D. The effectiveness of the functional movement screen in determining injury risk in tactical occupations. Ind Health. 2019; 57(4): 406 -18.
References 26. Teyhen DS, Shaffer SW, Lorenson CL, et al. The functional movement screen: A reliability study. J Orthop Sports Phys Ther. 2012; 42(6): 530 -40. 27. Davis JD, Orr R, Knapik JJ, Harris D. Functional movement screen (FMS™) scores and demographics of U. S. Army pre-ranger candidates. Military Med. 2019. 28. Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA. Measurement properties of the lower extremity functional scale: A systematic review. J Orthop Sports Phys Ther. 2016; 46(3): 200 -16. 29. Roy TC, Fish KL, Lopez HP, Piva SR. Preliminary validation of the military low back pain questionnaire. Military Med. 2014; 179(2): 121 -5. 30. Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (Quick. DASH). J Orthop Sports Phys Ther. 2014; 44(1): 30 -9. 31. Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the first world congress in sports physical therapy, Bern. Br J Sports Med. 2016 Jul; 50(14): 853 -64.