PERFORMANCE BASED PRIVILEGING Presented by Lynn L Buchanan
PERFORMANCE BASED PRIVILEGING Presented by Lynn L. Buchanan, CPMSM, CPCS President, Buchanan & Assoc. Consulting for Alaska Assn. Medical Staff Services June 2010 ©Edge-U-Cate LLC, 2010. Do not reproduce without written consent.
Privileges – A Definition �A specific scope and content of patient care services ◦ Authorization granted by a healthcare organization ◦ Based on pre-determined criteria and consistently applied ◦ Based on evaluation of the individual’s credentials and performance/competence ◦ Organization-specific ◦ Specifically delineated
Healthcare experts agree that an organization’s privilege delineation system is the foundation of quality patient care
WHO must have privileges? � Licensed Independent Practitioners (LIPs) – all individuals who are permitted ◦ All individuals permitted by law and by hospital to provide patient care services independently in the hospital � PAs and APRNs (TJC – HR. 01. 02. 05, EP 10 -15) NOTE: Do not have to be medical staff members in order to have delineated clinical privileges
WHICH organizations generally grant privileges? � Acute care hospitals, critical access hospitals � Behavioral Healthcare hospitals � Ambulatory Care Centers (Surgi. Center, GI Lab, etc. ) � Some Acute Long Term Care facilities (as may be required by regulations and standards 0 Privileges are not granted by Managed Care Organizations
WHO is responsible? � The Medical Staff is responsible for planning and implementing a privileging process: ◦ Developing and approving procedure list / criteria ◦ Processing the application (defined procedure) ◦ Evaluating applicant-specific information (objective, evidence-based process) ◦ Submitting applicant-specific privileging recommendations to governing body ◦ Notification of privileging decision ◦ Monitoring the use of privileges and quality of care ◦ (ref. The Joint Commission – Intro to MS – HAS)
WHEN are privileges granted? � When a practitioner is providing direct patient care services within or on behalf of your organization � Time-limited (not to exceed 2 years)
WHY are privileges granted? � Ensure that patients are receiving quality patient care by practitioners qualified to treat a specific illness or perform a specific procedure. * • The Credentialing Handbook Aspen Publishing 1998
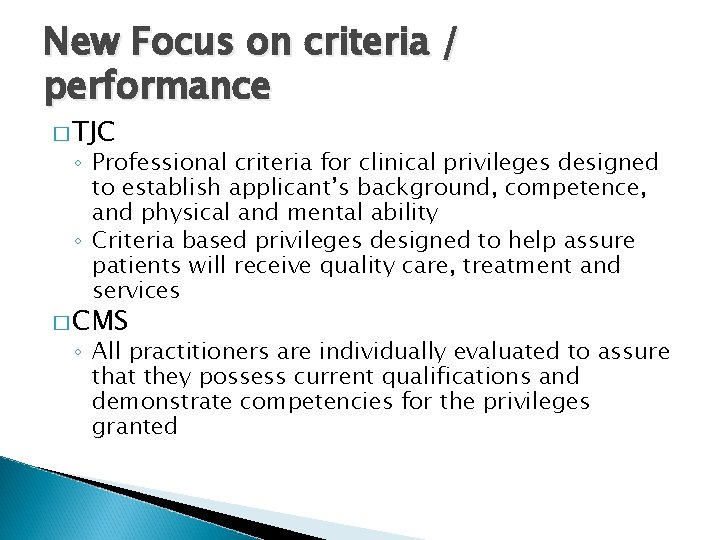
New Focus on criteria / performance � TJC ◦ Professional criteria for clinical privileges designed to establish applicant’s background, competence, and physical and mental ability ◦ Criteria based privileges designed to help assure patients will receive quality care, treatment and services � CMS ◦ All practitioners are individually evaluated to assure that they possess current qualifications and demonstrate competencies for the privileges granted
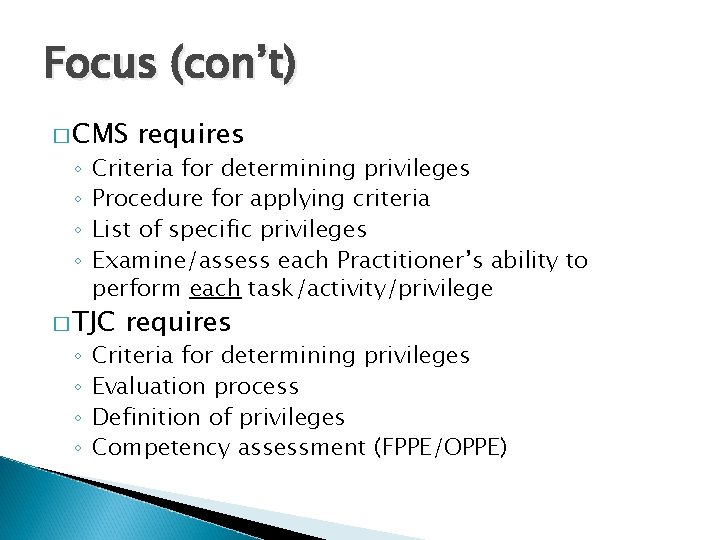
Focus (con’t) � CMS ◦ ◦ Criteria for determining privileges Procedure for applying criteria List of specific privileges Examine/assess each Practitioner’s ability to perform each task/activity/privilege � TJC ◦ ◦ requires Criteria for determining privileges Evaluation process Definition of privileges Competency assessment (FPPE/OPPE)
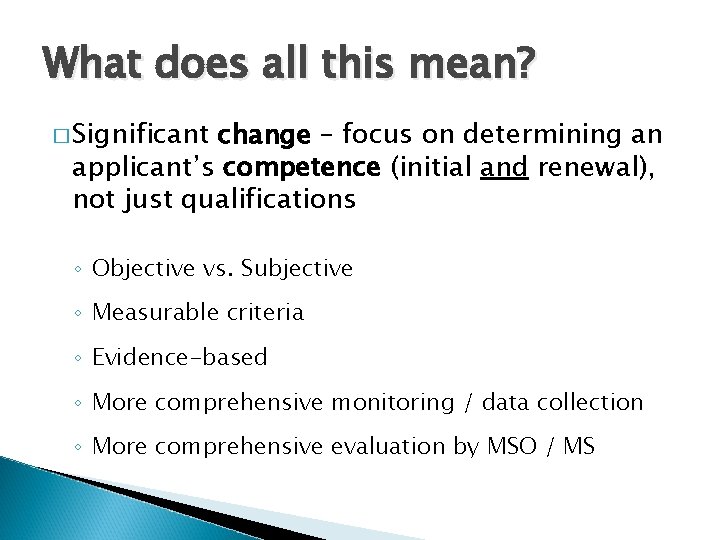
What does all this mean? � Significant change – focus on determining an applicant’s competence (initial and renewal), not just qualifications ◦ Objective vs. Subjective ◦ Measurable criteria ◦ Evidence-based ◦ More comprehensive monitoring / data collection ◦ More comprehensive evaluation by MSO / MS
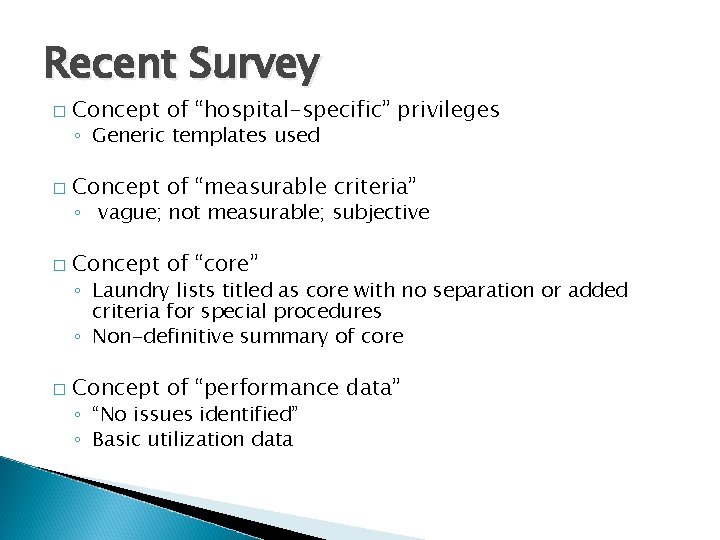
Recent Survey � Concept of “hospital-specific” privileges ◦ Generic templates used � Concept of “measurable criteria” ◦ vague; not measurable; subjective � Concept of “core” ◦ Laundry lists titled as core with no separation or added criteria for special procedures ◦ Non-definitive summary of core � Concept of “performance data” ◦ “No issues identified” ◦ Basic utilization data

CHANGE HAPPENS – whether we’re ready for it or not!!
The format has changed � From � To Laundry List of privileges only Core / Select – with criteria � Can be defined by: �Practitioner Specialty �Level of training/experience �Patient risk categories �Procedures / treatments
Core Privileging Format � Core (General) Privileges: Listing of those privileges that are commonly performed by residency-trained practitioners in a specific specialty and fall within general criteria ◦ Must include listing of privileges included in core ◦ Must include opportunity to “de-select” � Non-Core (Selected) Privileges: Defined privileges that require additional training/expertise and/or certain volume to obtain and maintain competence (defined by MS)
Criteria has changed � Separate criteria for membership from criteria for privileges ◦ ◦ Admitting Board Certification Availability Other? ? � Review your Bylaws, Policies & Procedures
Developing Criteria measurable criteria (“must have adequate training” is not measurable!!) � Need � Must be uniformly applied throughout facility (regardless of who’s doing it and where) ◦ e. g. , multiple specialties doing same procedure which may require defined “equivalent” criteria” � Must be defensible – if there is an adverse or perceived adverse outcome, can you stand behind your privileging P&Ps, the defined criteria, and the process used to privilege?
Developing Criteria (con’t) � Avoid “exceptions” to criteria whenever possible – consider defining “alternatives” instead � If applicant fails to meet established criteria, it is not reportable to NPDB as a “denial of privilege” – he/she simply isn’t eligible to apply for the privilege. � If applicant fails to meet eligibility requirements, does not invoke right to fair hearing.
Developing Criteria (con’t) � Criteria should be developed for � Criteria may also include ◦ Obtaining privilege ◦ Maintaining privilege ◦ Age groups (Example: “At ABC Hospital, Internal Medicine privileges are generally limited to patients 16 years or older”
Developing Criteria (con’t) Basic Criteria (applicable to the core/general privileges in a specialty) � Education / training / board cert (be specific) � Licensure and/or certification � Experience (yrs in practice, volume, etc) � Other requirements: evidence of physical ability to perform requested privilege, peer recommendations, data from professional practice review, other
Developing Criteria (con’t) Privilege-Specific (Selected) Privileges � Assumes � For basic criteria has been met, PLUS: each selected privilege: ◦ Training criteria, regardless of specialty (can be “equivalent”) �Formal program, subspecialty board, CME, proctored ◦ Experience (optional) – example: volume requirements to maintain proficiency in procedure)
Developing Criteria (con’t) � Good criteria – where do you find it? ? ? ◦ Specialty boards ◦ Commercial products ◦ ◦ �White Papers (HC Pro) �E Privileges (Morrisey, Cactus, Med. Kinetics) Networking with colleagues Consultants Internet!!!! (you’d be amazed!) Your medical staff
Developing Criteria (con’t) Dealing with that “new” privilege a practitioner may want to begin doing in your organization � Cannot apply for privilege you don’t offer! � Have a Policy & Procedure ◦ Medical Staff & Administration must determine if new privilege is feasible (based on patient population, community need, capital expenditure, support staff, space, etc) ◦ If it is determined that new privilege would be in best interest, must first develop criteria and have it approved � Only then can practitioner apply for privilege
Process has changed �OLD 1. 2. 3. 4. WAY: (usually a laundry list) Make sure applicant fills out request Check for signature At reappointment, compare for changes Have Department Chair review, check off and sign
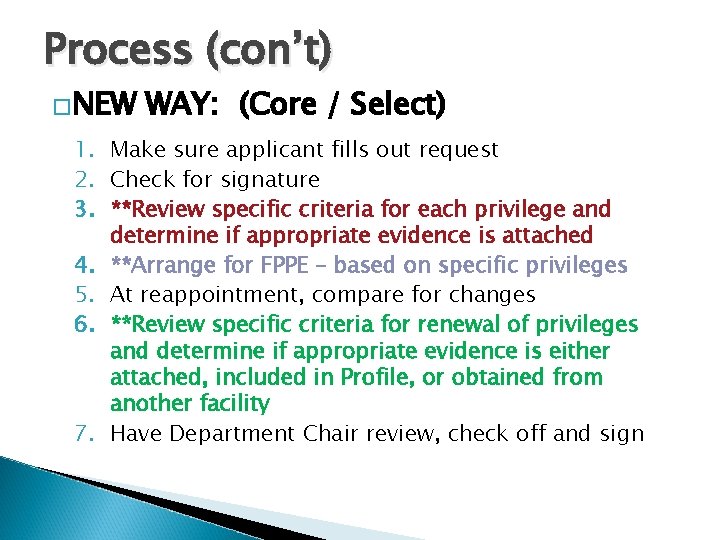
Process (con’t) �NEW WAY: (Core / Select) 1. Make sure applicant fills out request 2. Check for signature 3. **Review specific criteria for each privilege and determine if appropriate evidence is attached 4. **Arrange for FPPE – based on specific privileges 5. At reappointment, compare for changes 6. **Review specific criteria for renewal of privileges and determine if appropriate evidence is either attached, included in Profile, or obtained from another facility 7. Have Department Chair review, check off and sign
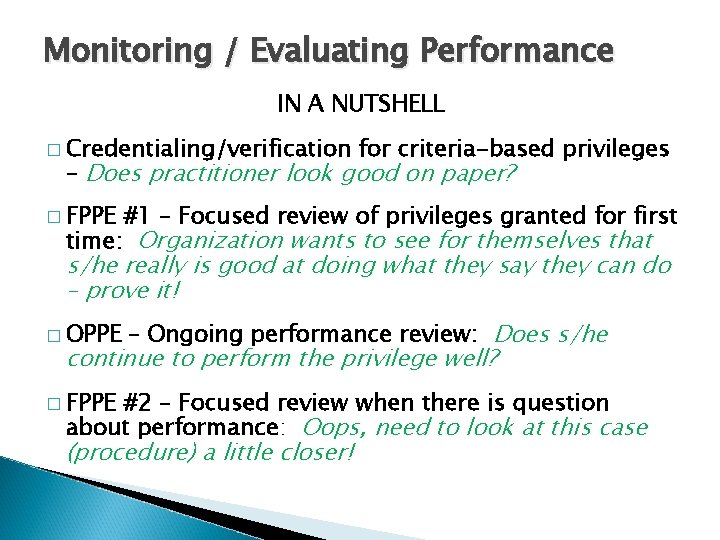
Monitoring / Evaluating Performance IN A NUTSHELL � Credentialing/verification for criteria-based privileges – Does practitioner look good on paper? � FPPE #1 – Focused review of privileges granted for first time: Organization wants to see for themselves that s/he really is good at doing what they say they can do – prove it! � OPPE – Ongoing performance review: Does s/he continue to perform the privilege well? � FPPE #2 – Focused review when there is question about performance: Oops, need to look at this case (procedure) a little closer!
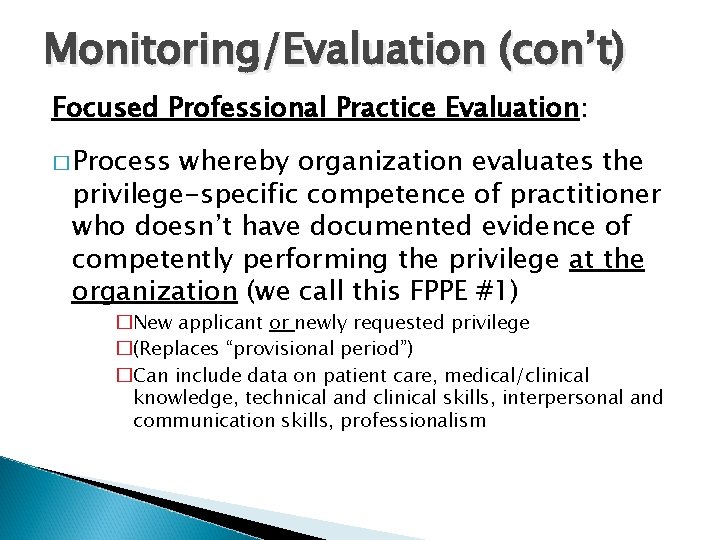
Monitoring/Evaluation (con’t) Focused Professional Practice Evaluation: � Process whereby organization evaluates the privilege-specific competence of practitioner who doesn’t have documented evidence of competently performing the privilege at the organization (we call this FPPE #1) �New applicant or newly requested privilege �(Replaces “provisional period”) �Can include data on patient care, medical/clinical knowledge, technical and clinical skills, interpersonal and communication skills, professionalism
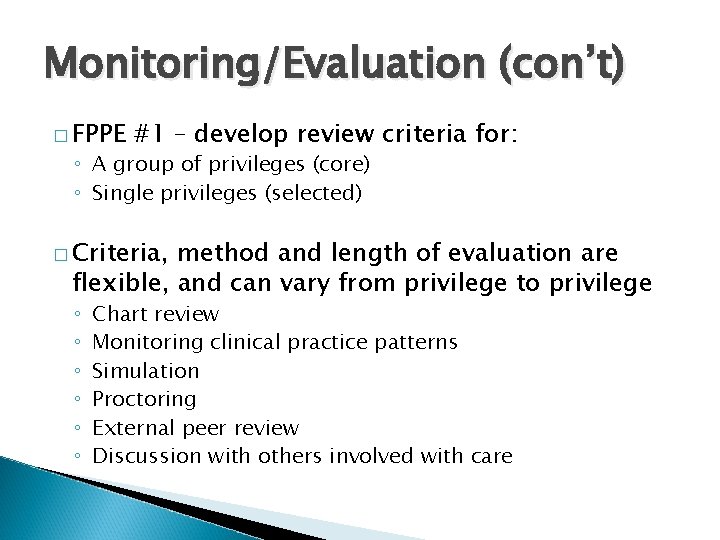
Monitoring/Evaluation (con’t) � FPPE #1 – develop review criteria for: ◦ A group of privileges (core) ◦ Single privileges (selected) � Criteria, method and length of evaluation are flexible, and can vary from privilege to privilege ◦ ◦ ◦ Chart review Monitoring clinical practice patterns Simulation Proctoring External peer review Discussion with others involved with care
Monitoring/Evaluation (con’t) � FPPE: Process also used when question arises re: currently privileged practitioner’s ability to provide safe, high quality patient care (we call this FPPE #2) ◦ Requires medical staff evaluation ◦ MS. 08. 01 Intro – Effective January 2008
Monitoring/Evaluation (con’t) Ongoing Professional Practice Evaluation (OPPE) � Process that allows the organization to identify professional practice trends impacting quality patient care and safety (in between reappointment periods). Examples: ◦ ◦ ◦ Review of operative procedures Blood and pharmacy use Test and procedure requests Morbidity and mortality data Use of consultants Other criteria determined by medical staff
Performance-based privileges - Evidence based privileging : Information from these evaluations must be part of the decisionmaking process � Joint Commission ◦ Decision to grant, deny, renew privilege(s) is objective and evidence based ◦ Ongoing professional practice evaluation information is factored into the privileging decision � CMS ◦ All practitioners are individually evaluated to assure that they possess current qualifications and demonstrated competencies for the privileges granted
Evidence based privileging �Joint Commission ◦ Decision to grant, deny, renew privilege(s) is objective and evidence based ◦ Ongoing professional practice evaluation information is factored into the privileging decision �CMS ◦ All practitioners are individually evaluated to assure that they possess current qualifications and demonstrated competencies for the privileges granted
QUESTIONS?
- Slides: 34