Percutaneous Mitral Valve Repair Coronary Sinus Approach Maurice


















- Slides: 48

Percutaneous Mitral Valve Repair Coronary Sinus Approach Maurice Buchbinder, MD Foundation for Cardiovascular Medicine La Jolla, CA Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
Disclosure. Stents? Why Degradable Speaker’s name: Maurice Buchbinder, MD �I have the following potential conflicts of interest to report: �Consulting �Employment in industry �Stockholder of a healthcare company �Owner of a healthcare company I do not have any potential conflict of interest Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

Edge-to-edge • e. Valve • Edwards Mobius Coronary sinus annuloplasty • Edwards Monarc • Cardiac Dimensions Carillon • Viacor PTMA Indirect annuloplasty • Ample PS 3 • Myocor i-Coapsys • St. Jude AAR Direct annuloplasty • Mitralign • Guided Delivery Systems • Quantum. Cor, Cordis DPA • Mi. Cardia, Mitral Solutions Mitral valve replacement • Cardi. AQ • Endovalve Maurice Buchbinder, MD • M- Valve Foundation for Cardiovascular Medicine Device Landscape: Percutaneous MV Repair
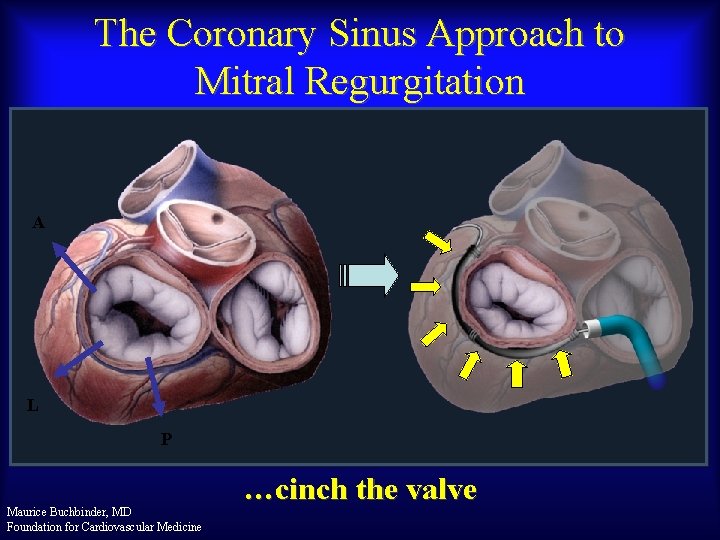
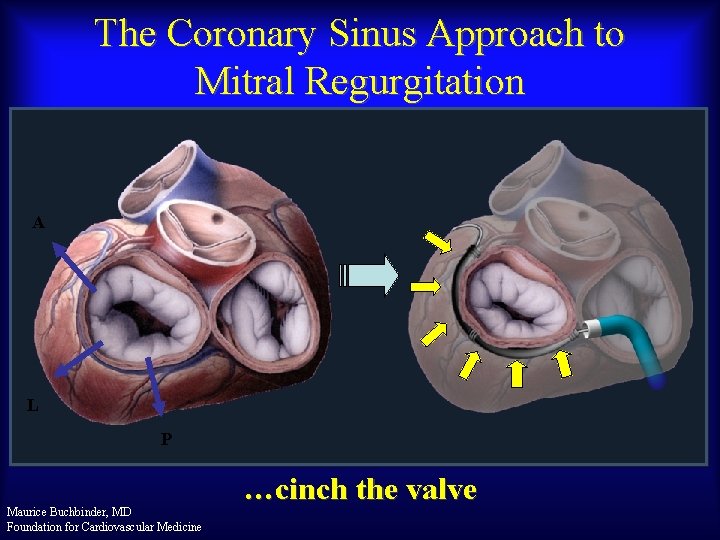
The Coronary Sinus Approach to Mitral Regurgitation A L P Maurice Buchbinder, MD Foundation for Cardiovascular Medicine …cinch the valve
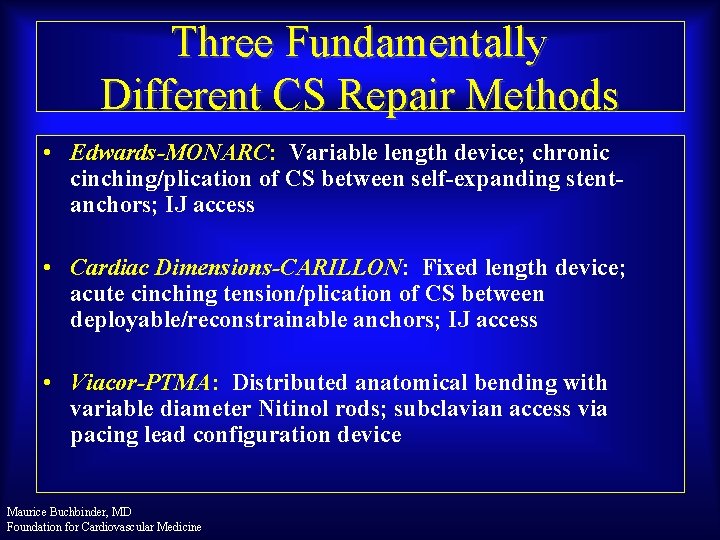
Three Fundamentally Different CS Repair Methods • Edwards-MONARC: Variable length device; chronic cinching/plication of CS between self-expanding stentanchors; IJ access • Cardiac Dimensions-CARILLON: Fixed length device; acute cinching tension/plication of CS between deployable/reconstrainable anchors; IJ access • Viacor-PTMA: Distributed anatomical bending with variable diameter Nitinol rods; subclavian access via pacing lead configuration device Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

The Edwards MONARC System Sliding Knob Location of Implant (Internal) Handle 12 F guiding catheter 9 F delivery system • Three components: – Self expanding distal anchor – Self expanding proximal anchor – Bridge connecting the anchors Maurice Buchbinder, MD Foundation for Cardiovascular Medicine Bridge Proximal Anchor Elongated bridge at implant Distal Anchor Foreshortened state at ~6 weeks
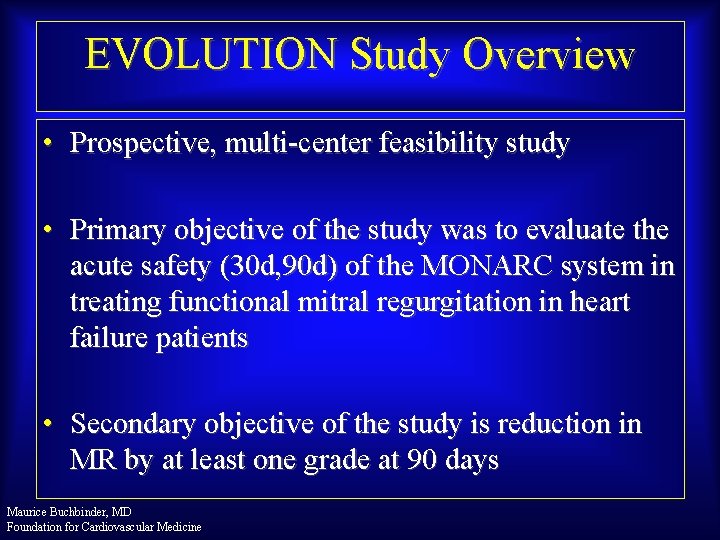
EVOLUTION Study Overview • Prospective, multi-center feasibility study • Primary objective of the study was to evaluate the acute safety (30 d, 90 d) of the MONARC system in treating functional mitral regurgitation in heart failure patients • Secondary objective of the study is reduction in MR by at least one grade at 90 days Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
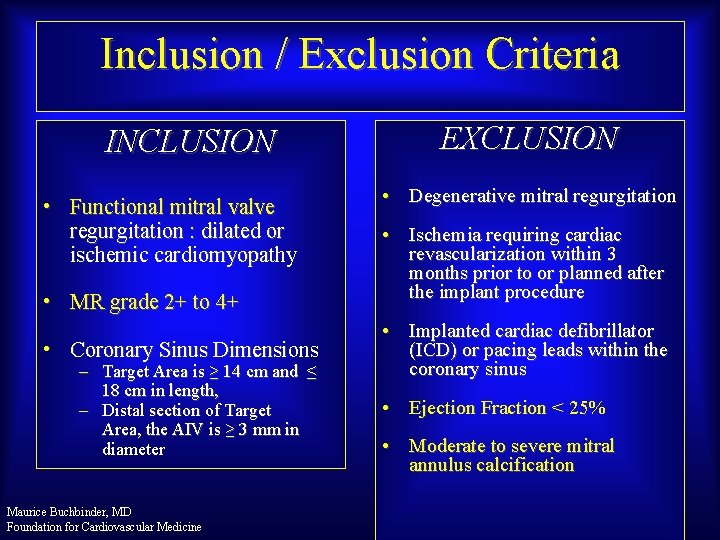
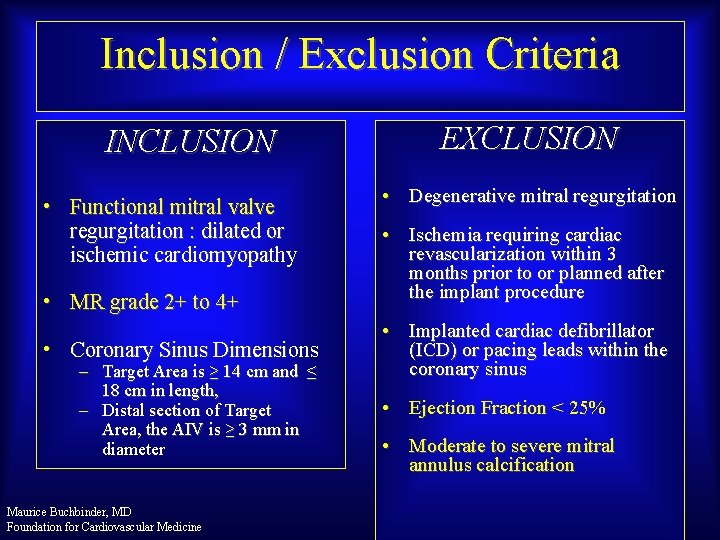
Inclusion / Exclusion Criteria INCLUSION • Functional mitral valve regurgitation : dilated or ischemic cardiomyopathy • MR grade 2+ to 4+ • Coronary Sinus Dimensions – Target Area is ≥ 14 cm and ≤ 18 cm in length, – Distal section of Target Area, the AIV is ≥ 3 mm in diameter Maurice Buchbinder, MD Foundation for Cardiovascular Medicine EXCLUSION • Degenerative mitral regurgitation • Ischemia requiring cardiac revascularization within 3 months prior to or planned after the implant procedure • Implanted cardiac defibrillator (ICD) or pacing leads within the coronary sinus • Ejection Fraction < 25% • Moderate to severe mitral annulus calcification
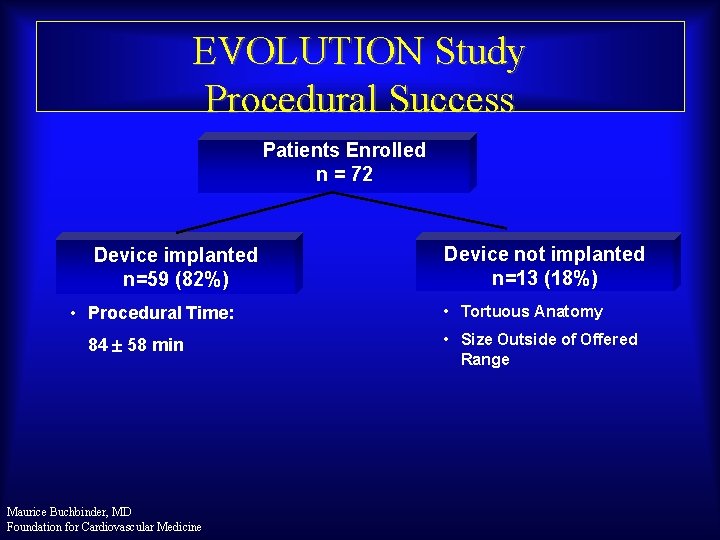
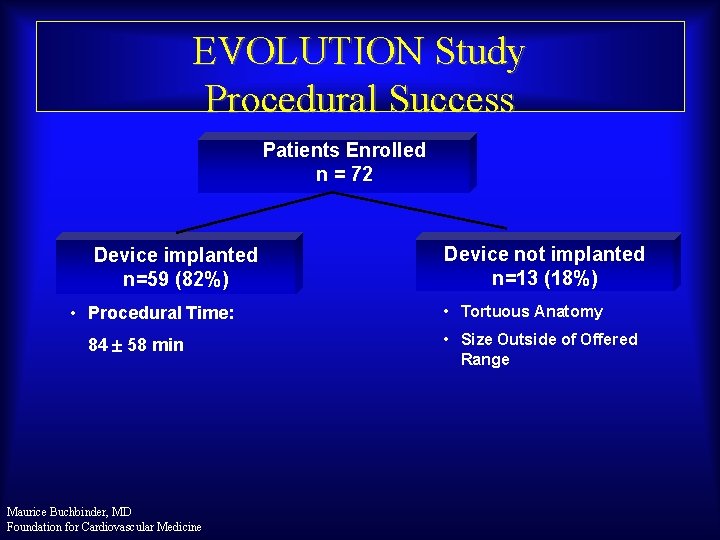
EVOLUTION Study Procedural Success Patients Enrolled n = 72 Device implanted n=59 (82%) • Procedural Time: 84 58 min Maurice Buchbinder, MD Foundation for Cardiovascular Medicine Device not implanted n=13 (18%) • Tortuous Anatomy • Size Outside of Offered Range

Echocardiography (Core Lab Data) LVEF, % Baseline MR Maurice Buchbinder, MD Foundation for Cardiovascular Medicine 38 ± 11 Range: 23 – 67 1+ 5 % 2+ 61 % 3+ 15 % 4+ 19 %
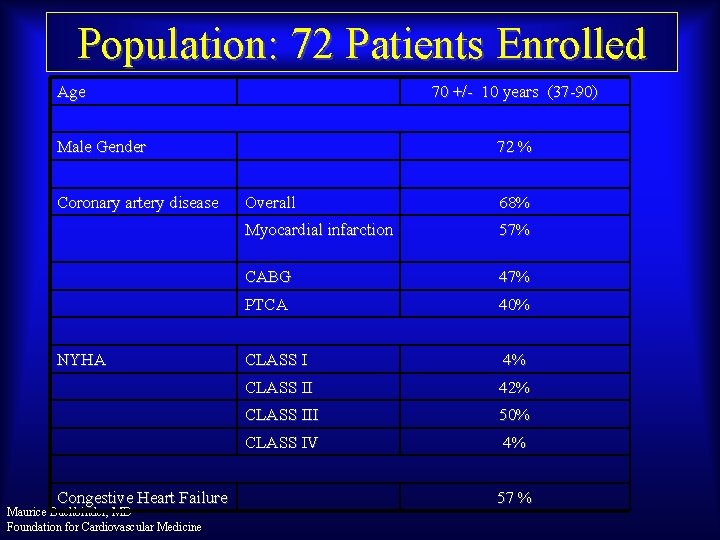
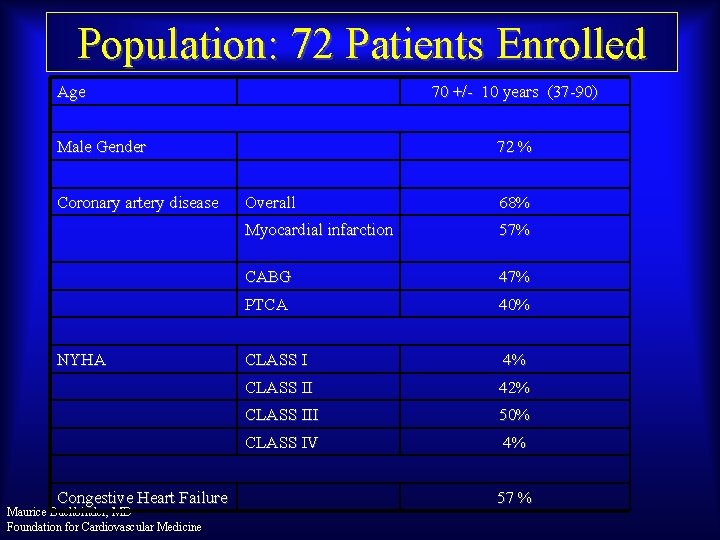
Population: 72 Patients Enrolled Age 70 +/- 10 years (37 -90) Male Gender Coronary artery disease NYHA Congestive Heart Failure Maurice Buchbinder, MD Foundation for Cardiovascular Medicine 72 % Overall 68% Myocardial infarction 57% CABG 47% PTCA 40% CLASS I 4% CLASS II 42% CLASS III 50% CLASS IV 4% 57 %
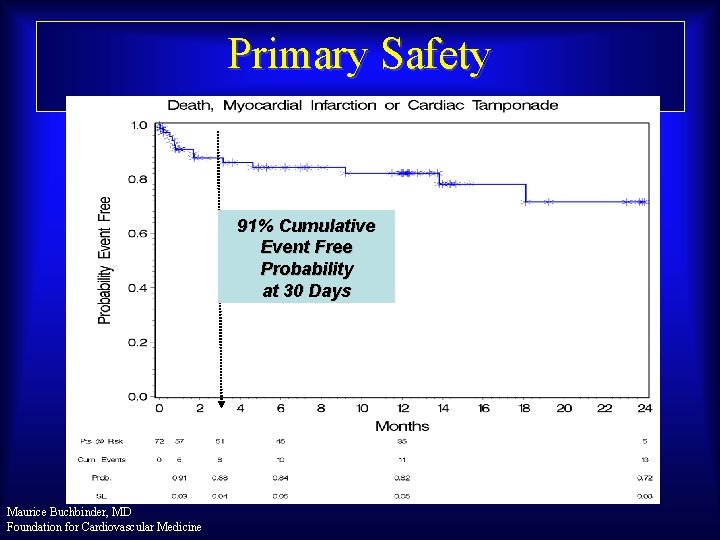
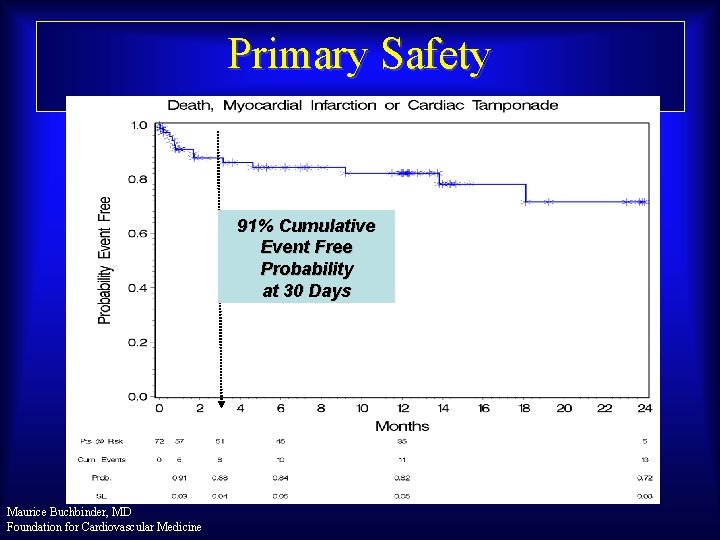
Primary Safety 91% Cumulative Event Free Probability at 30 Days Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
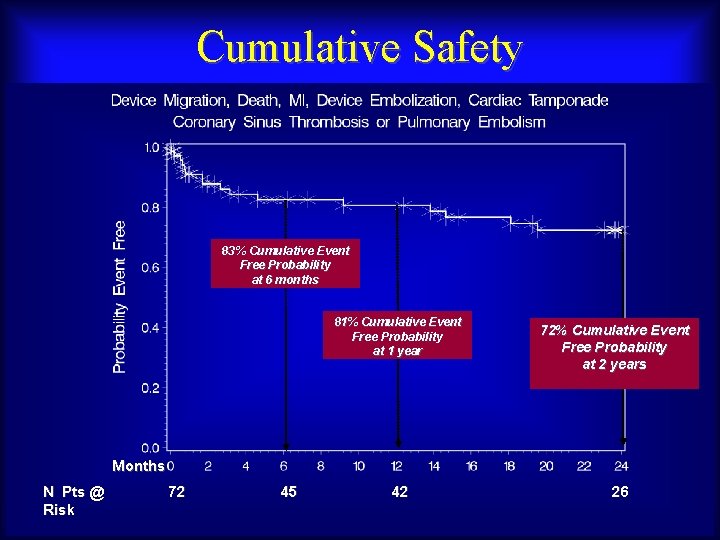
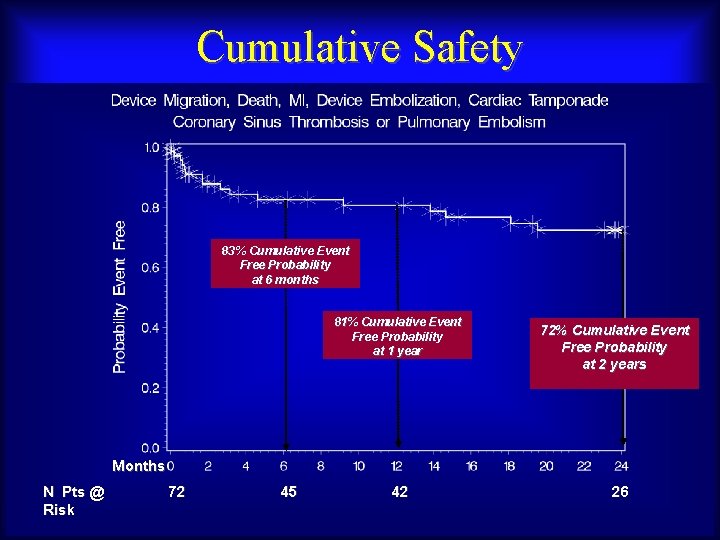
Cumulative Safety 83% Cumulative Event Free Probability at 6 months 81% Cumulative Event Free Probability at 1 year 72% Cumulative Event Free Probability at 2 years Months N Pts @ Risk Maurice Buchbinder, MD 72 Foundation for Cardiovascular Medicine 45 42 26
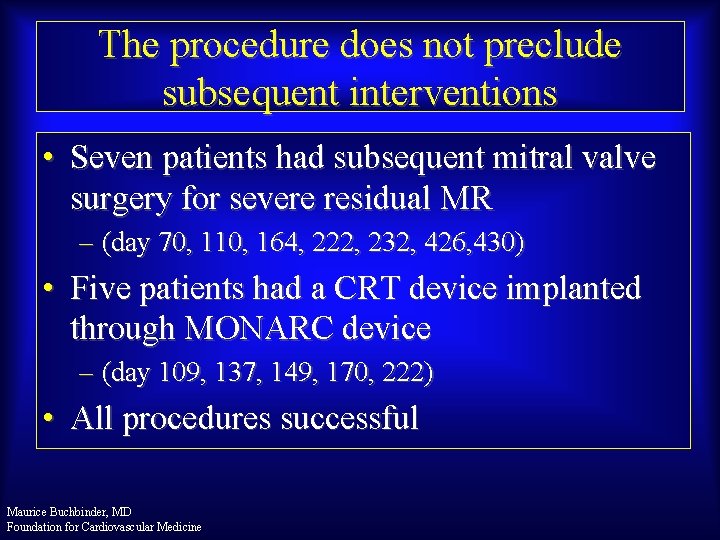
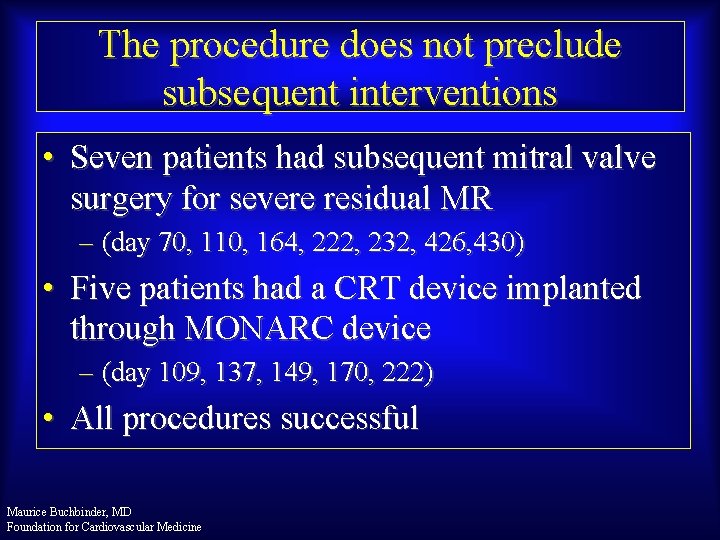
The procedure does not preclude subsequent interventions • Seven patients had subsequent mitral valve surgery for severe residual MR – (day 70, 110, 164, 222, 232, 426, 430) • Five patients had a CRT device implanted through MONARC device – (day 109, 137, 149, 170, 222) • All procedures successful Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

Device malfunctions seen on routine angiography at 90 -days • No coronary sinus thrombosis • 5 device malfunctions with no clinical complication – 1 Migration • Improper Sizing – 4 Proximal Anchor Device Separation • Device modification implemented Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

2 -Year Efficacy Quantitative Measurements of MR Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
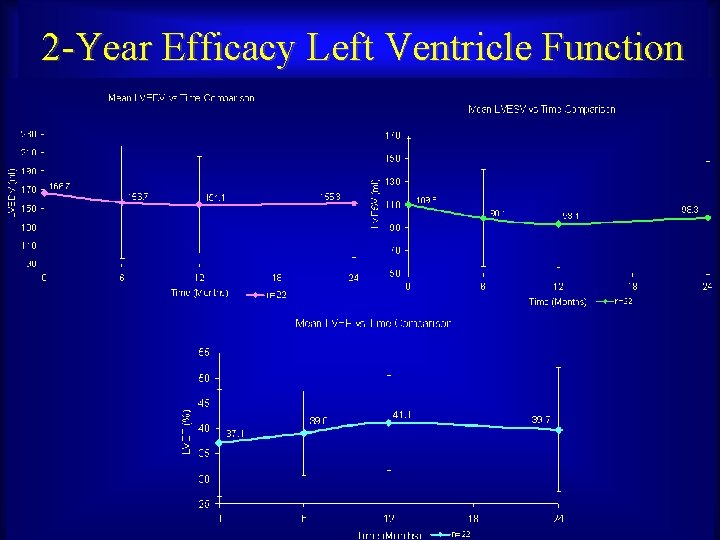
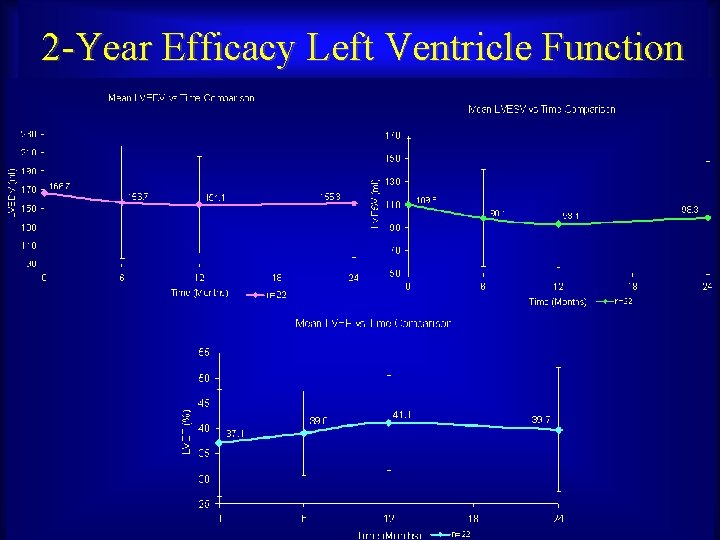
2 -Year Efficacy Left Ventricle Function Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

EVOLUTION Study 2 -Year Follow-up: NYHA Class Mean Median Maurice Buchbinder, MD Foundation for Cardiovascular Medicine Pre. Procedure 2 Year 2. 61 2. 04 3 2

Conclusions • EVOLUTION interim data with the MONARC system suggests: • Implantation in the coronary sinus is feasible • At 24 -months, 72% of patients are event-free as defined by the protocol • Encouraging 24 -months results in terms of MR reduction and physiological parameters. Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
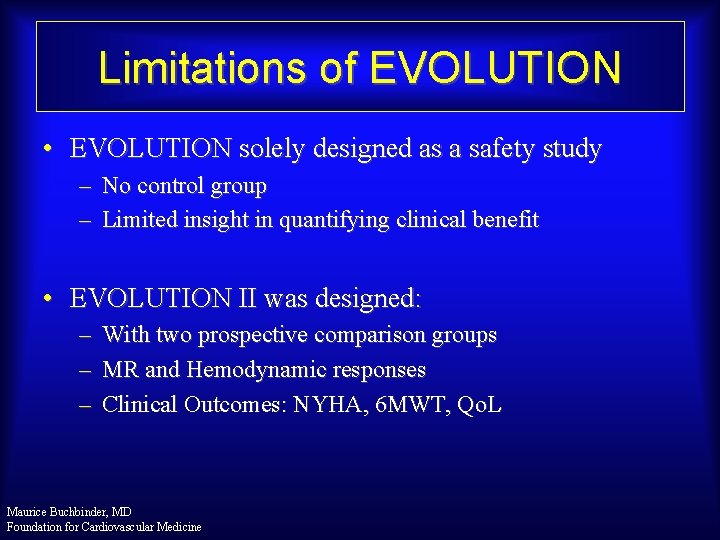
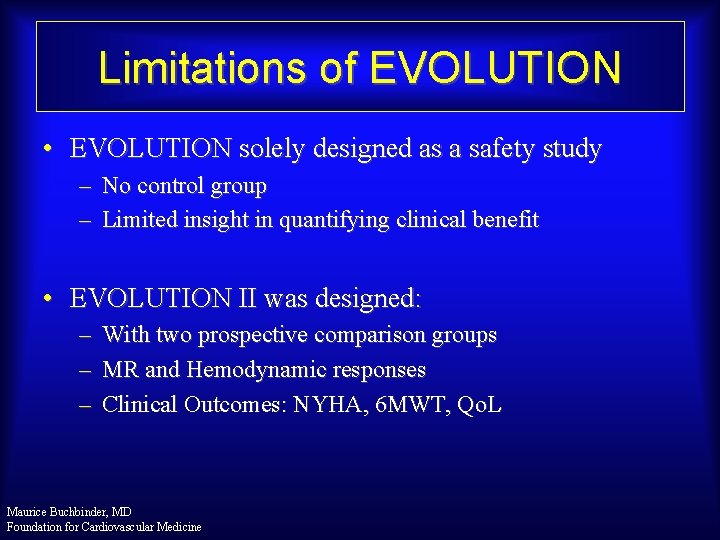
Limitations of EVOLUTION • EVOLUTION solely designed as a safety study – No control group – Limited insight in quantifying clinical benefit • EVOLUTION II was designed: – – – With two prospective comparison groups MR and Hemodynamic responses Clinical Outcomes: NYHA, 6 MWT, Qo. L Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

Enrollment Distribution Feb ’ 09 – Jun ’ 10 Enrolled (n= 52) Intend to Treat (n = 34), 65% Observational Population Subjects that are excluded from a MONARC implant procedure solely due to coronary artery anatomy but fulfill all other inclusion/exclusion criteria Continue care with standard medical management Observational (n = 18), 35% Implant Population Subjects are implanted with a MONARC device Non-Implanted Population Implant (n = 30), 88% of ITT Non-Implant (n = 4), 12% of ITT Procedure Time = 73± 34 min Procedure Time = 103± 38 min Maurice Buchbinder, MD Foundation for Cardiovascular Medicine Subjects undergo an implant procedure but do not receive a MONARC device Continue care with standard medical management
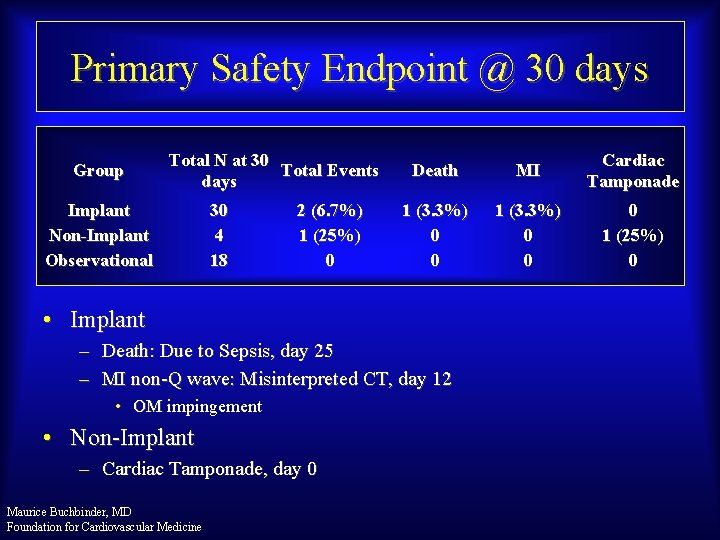
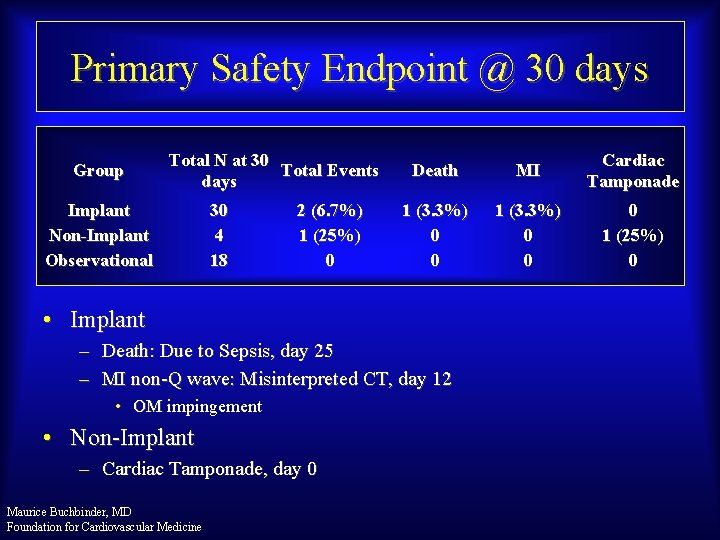
Primary Safety Endpoint @ 30 days Group Total N at 30 Total Events days Implant Non-Implant Observational 30 4 18 2 (6. 7%) 1 (25%) 0 Death MI Cardiac Tamponade 1 (3. 3%) 0 0 0 1 (25%) 0 • Implant – Death: Due to Sepsis, day 25 – MI non-Q wave: Misinterpreted CT, day 12 • OM impingement • Non-Implant – Cardiac Tamponade, day 0 Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
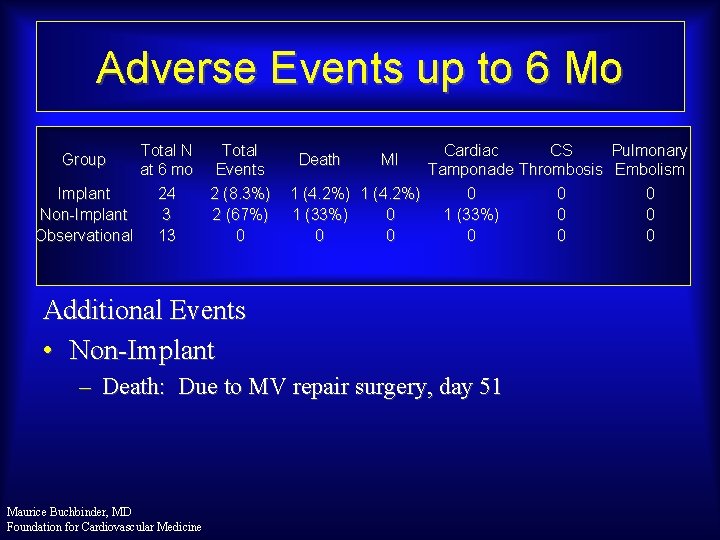
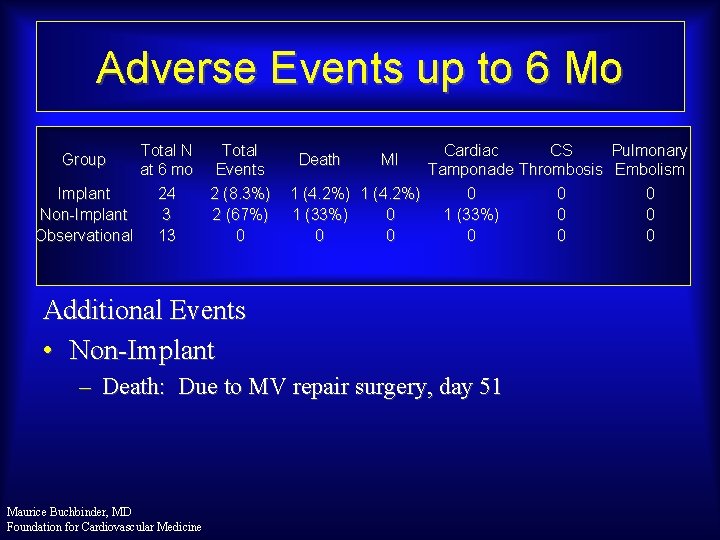
Adverse Events up to 6 Mo Total N at 6 mo Implant 24 Non-Implant 3 Observational 13 Group Total Events 2 (8. 3%) 2 (67%) 0 Cardiac CS Pulmonary Tamponade Thrombosis Embolism 1 (4. 2%) 0 0 0 1 (33%) 0 0 0 0 Death MI Additional Events • Non-Implant – Death: Due to MV repair surgery, day 51 Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
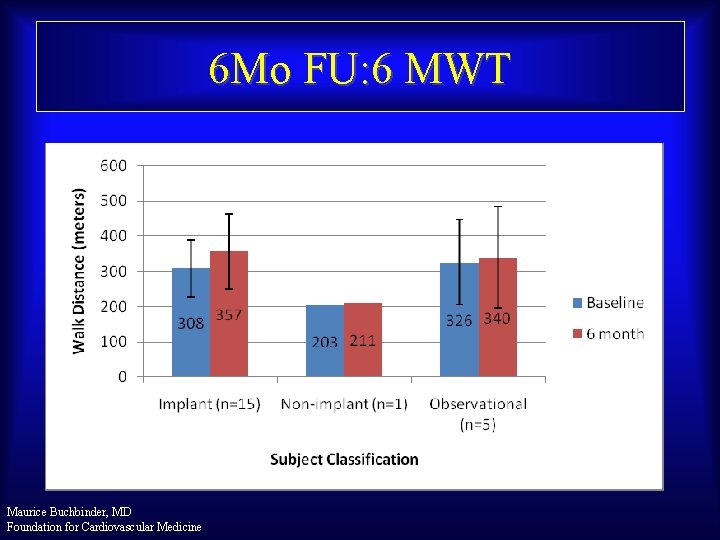
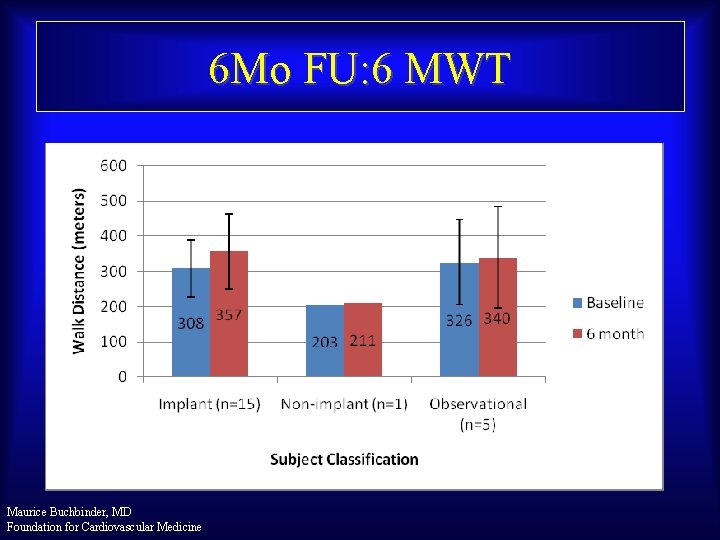
6 Mo FU: 6 MWT Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
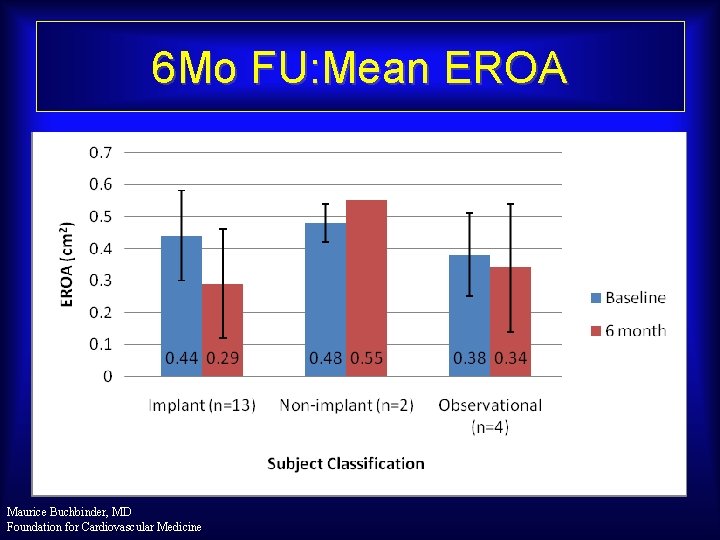
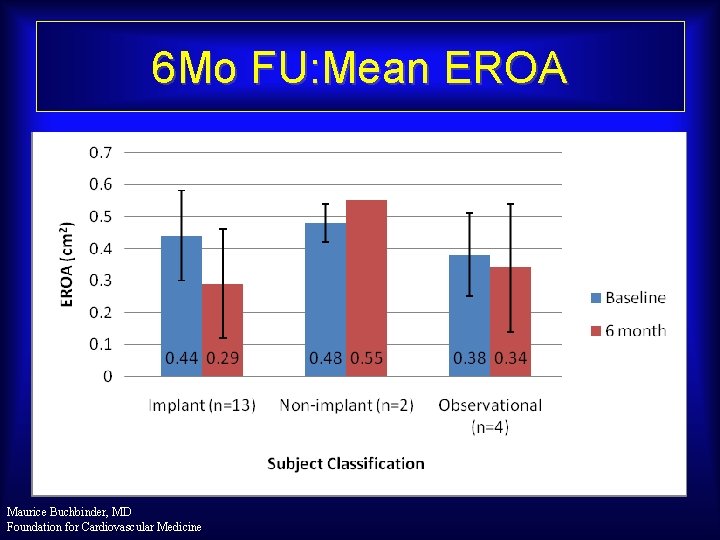
6 Mo FU: Mean EROA Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
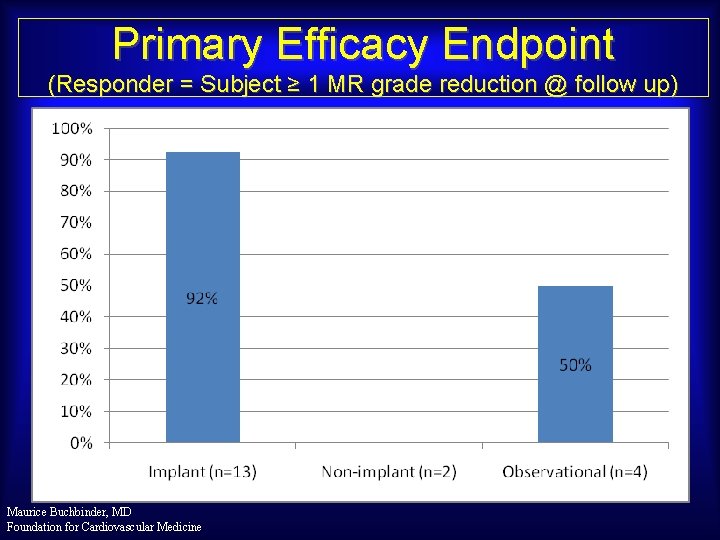
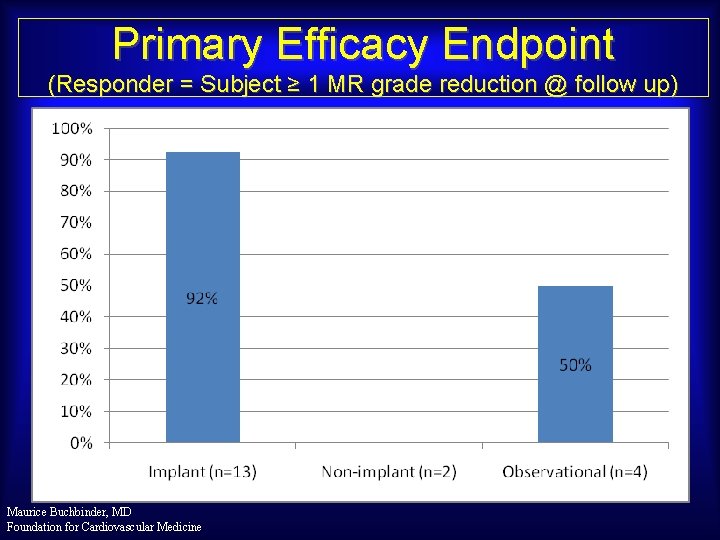
Primary Efficacy Endpoint (Responder = Subject ≥ 1 MR grade reduction @ follow up) Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

Mean MR Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
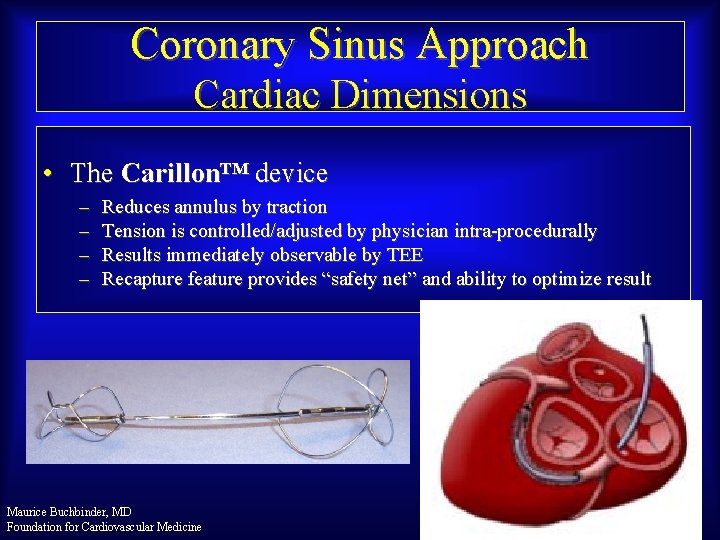
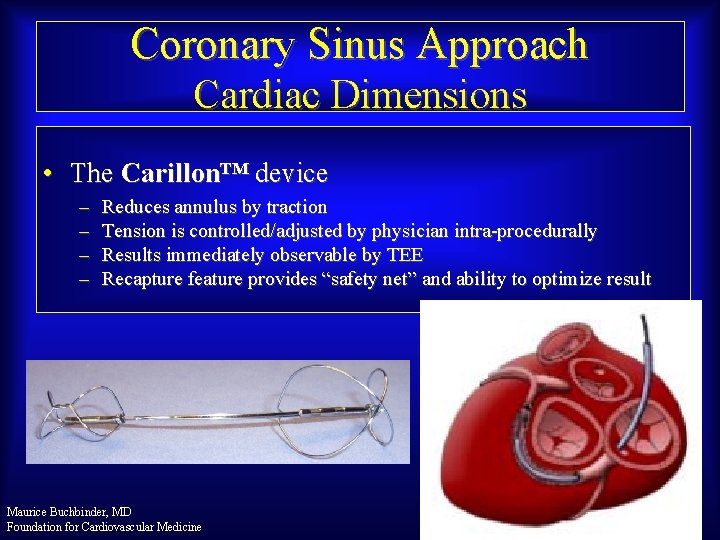
Coronary Sinus Approach Cardiac Dimensions • The Carillon™ device – – Reduces annulus by traction Tension is controlled/adjusted by physician intra-procedurally Results immediately observable by TEE Recapture feature provides “safety net” and ability to optimize result Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
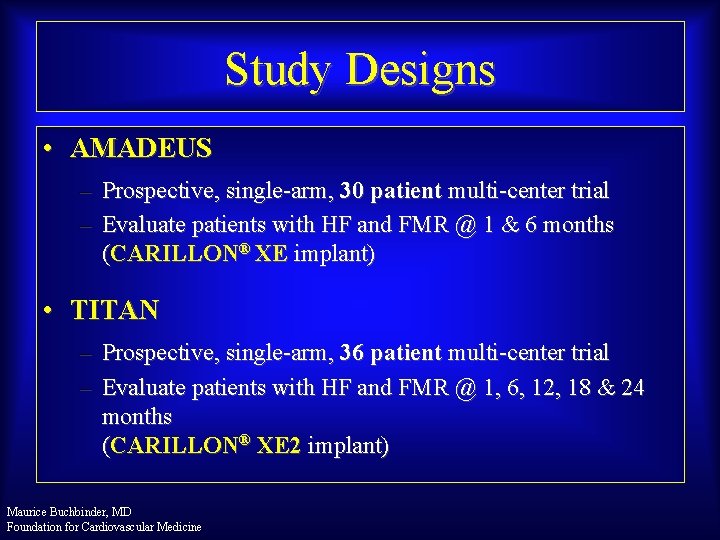
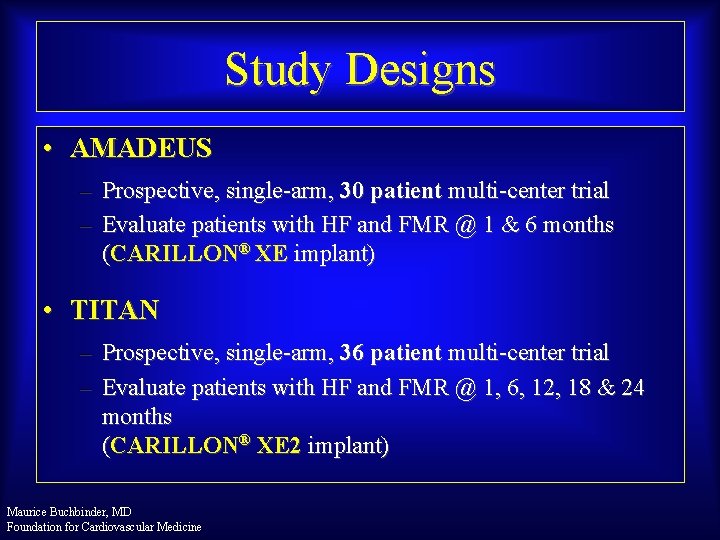
Study Designs • AMADEUS – Prospective, single-arm, 30 patient multi-center trial – Evaluate patients with HF and FMR @ 1 & 6 months (CARILLON® XE implant) • TITAN – Prospective, single-arm, 36 patient multi-center trial – Evaluate patients with HF and FMR @ 1, 6, 12, 18 & 24 months (CARILLON® XE 2 implant) Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

AMADEUS™ & TITAN™ Patient Enrollment • CAD requiring intervention • Inadequate Vein Size • Dissection / Perforation on Access • Insufficient MR Reduction • Coronary Compromise • 1 st Gen Device Anchor Slip Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
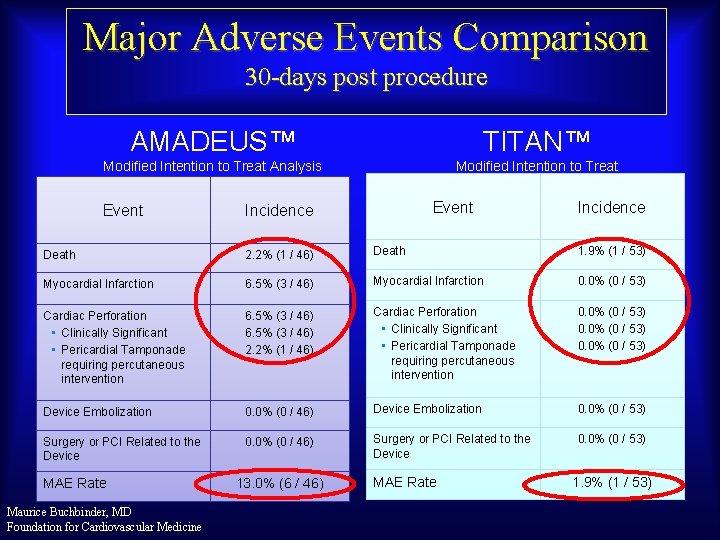
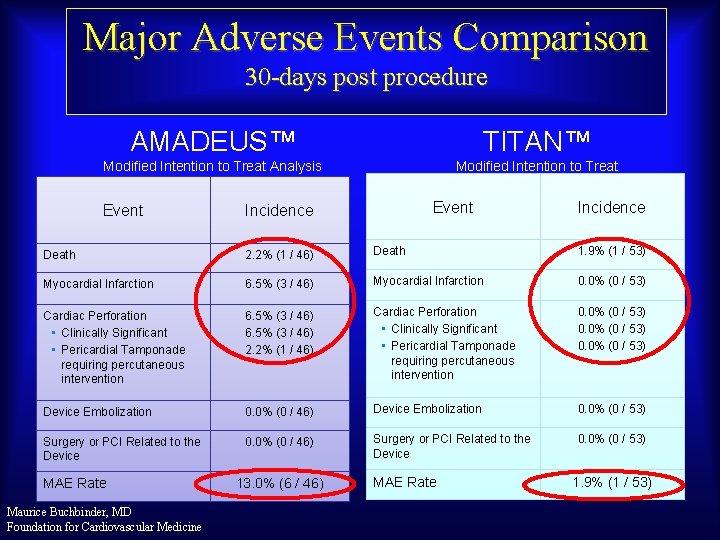
Major Adverse Events Comparison 30 -days post procedure AMADEUS™ TITAN™ Modified Intention to Treat Analysis Event Incidence Death 2. 2% (1 / 46) Death 1. 9% (1 / 53) Myocardial Infarction 6. 5% (3 / 46) Myocardial Infarction 0. 0% (0 / 53) Cardiac Perforation • Clinically Significant • Pericardial Tamponade requiring percutaneous intervention 6. 5% (3 / 46) 2. 2% (1 / 46) Cardiac Perforation • Clinically Significant • Pericardial Tamponade requiring percutaneous intervention 0. 0% (0 / 53) Device Embolization 0. 0% (0 / 46) Device Embolization 0. 0% (0 / 53) Surgery or PCI Related to the Device 0. 0% (0 / 46) Surgery or PCI Related to the Device 0. 0% (0 / 53) MAE Rate Maurice Buchbinder, MD Foundation for Cardiovascular Medicine 13. 0% (6 / 46) MAE Rate 1. 9% (1 / 53)
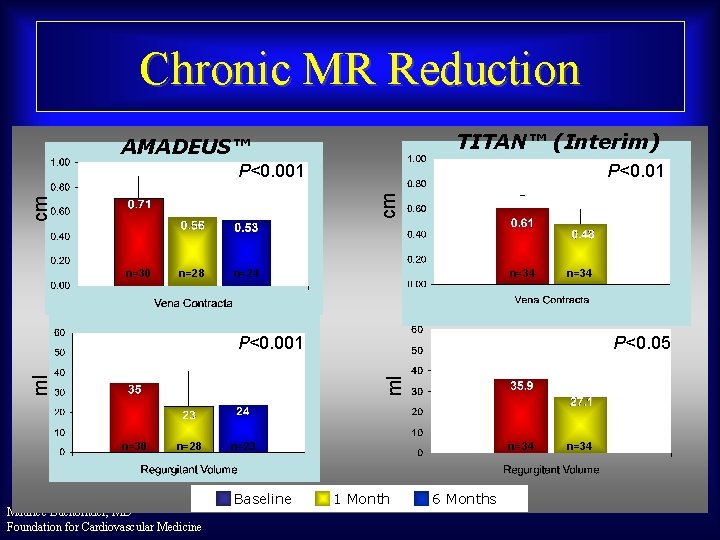
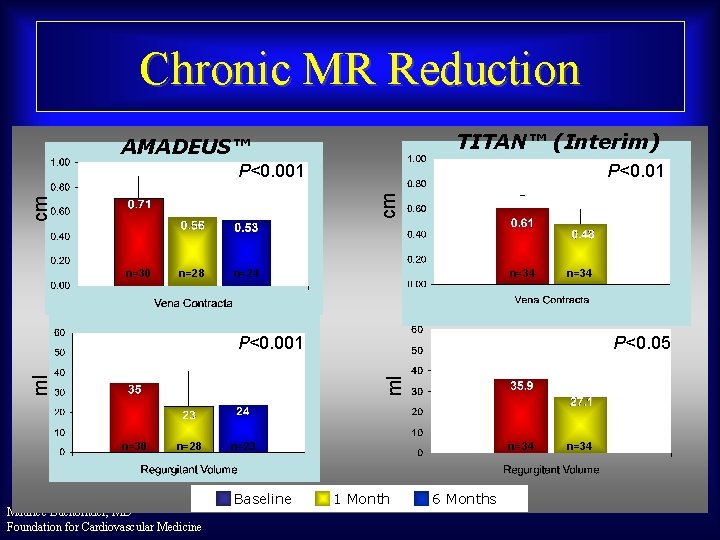
Chronic MR Reduction TITAN™ (Interim) AMADEUS™ P<0. 01 cm cm P<0. 001 n=30 n=28 n=24 n=34 P<0. 05 ml ml P<0. 001 n=30 n=28 Maurice Buchbinder, MD Foundation for Cardiovascular Medicine n=23 Baseline n=34 1 Month 6 Months n=34
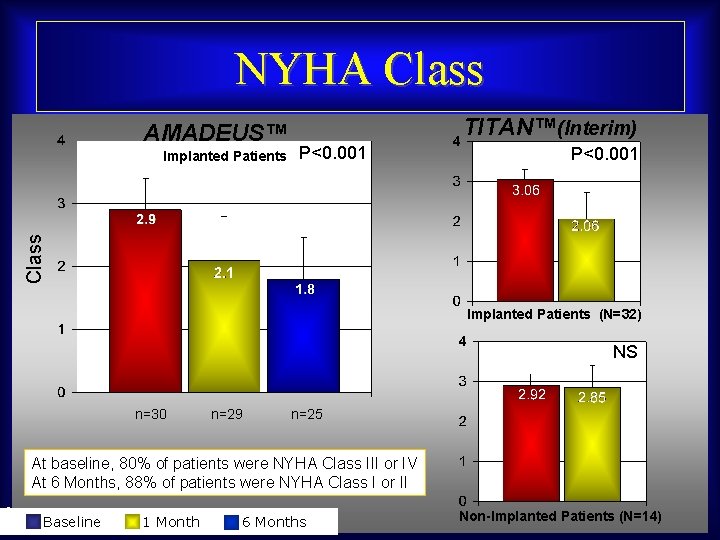
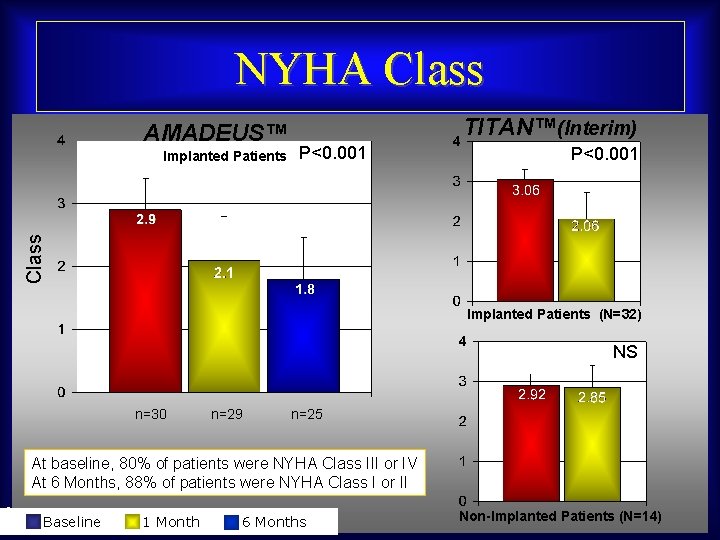
NYHA Class AMADEUS™ P<0. 001 Class Implanted Patients TITAN™(Interim) Implanted Patients (N=32) NS n=30 n=29 n=25 At baseline, 80% of patients were NYHA Class III or IV At 6 Months, 88% of patients were NYHA Class I or II Maurice Buchbinder, MD Baseline 1 Month Foundation for Cardiovascular Medicine 6 Months Non-Implanted Patients (N=14)

Six Minute Walk Test AMADEUS™ TITAN™(Interim) P<0. 001 Meters P<0. 001 Implanted Patients (N=32) NS n=30 n=28 n=23 Implanted Patients Maurice Buchbinder, MD Baseline 1 Month Foundation for Cardiovascular Medicine 6 Months Non-Implanted Patients (N=14)

QOL / KCCQ TITAN™(Interim) AMADEUS™ P<0. 0001 Score P<0. 001 Implanted Patients (N=32) NS n=30 n=26 n=25 Implanted Patients Maurice Buchbinder, MD Baseline 1 Month Foundation for Cardiovascular Medicine 6 Months Non-Implanted Patients (N=14)
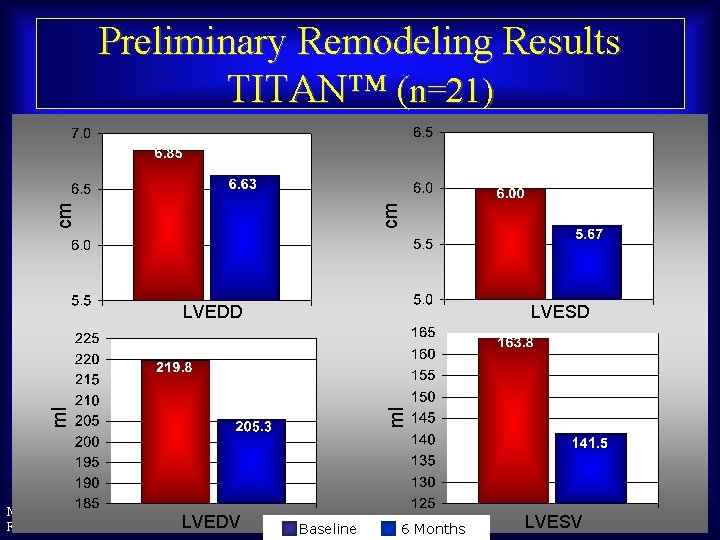
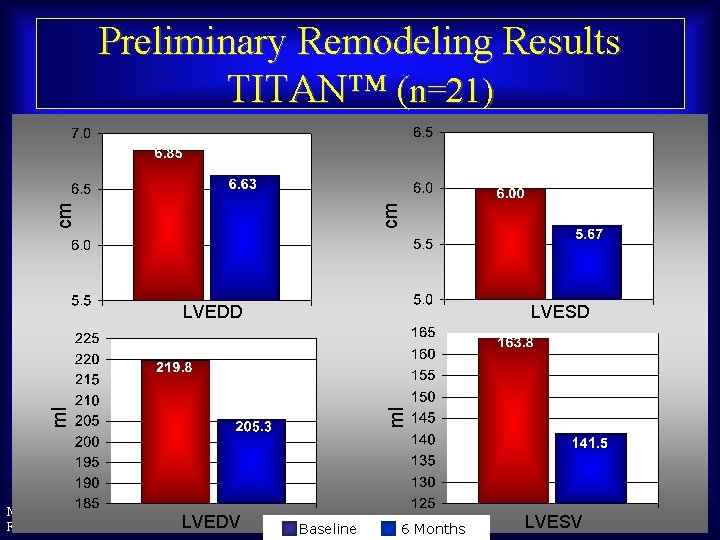
cm cm Preliminary Remodeling Results TITAN™ (n=21) LVESD ml ml LVEDD Maurice Buchbinder, MD LVEDV Foundation for Cardiovascular Medicine Baseline 6 Months LVESV
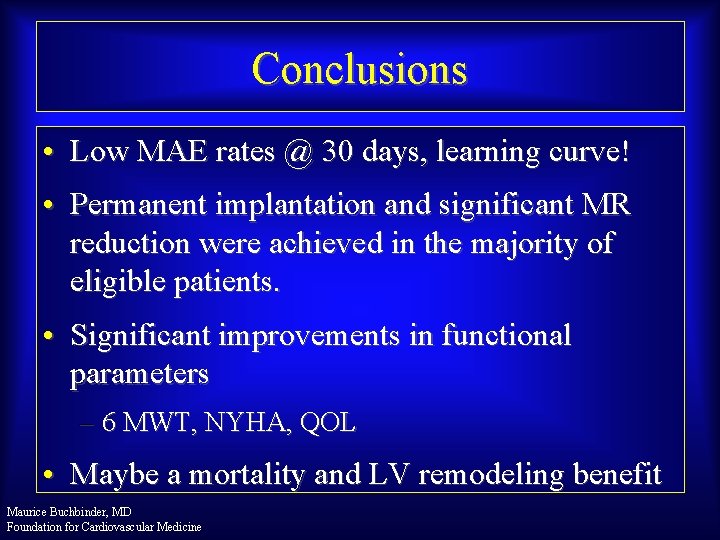
Conclusions • Low MAE rates @ 30 days, learning curve! • Permanent implantation and significant MR reduction were achieved in the majority of eligible patients. • Significant improvements in functional parameters – 6 MWT, NYHA, QOL • Maybe a mortality and LV remodeling benefit Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

Coronary Sinus Mitral Repair Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
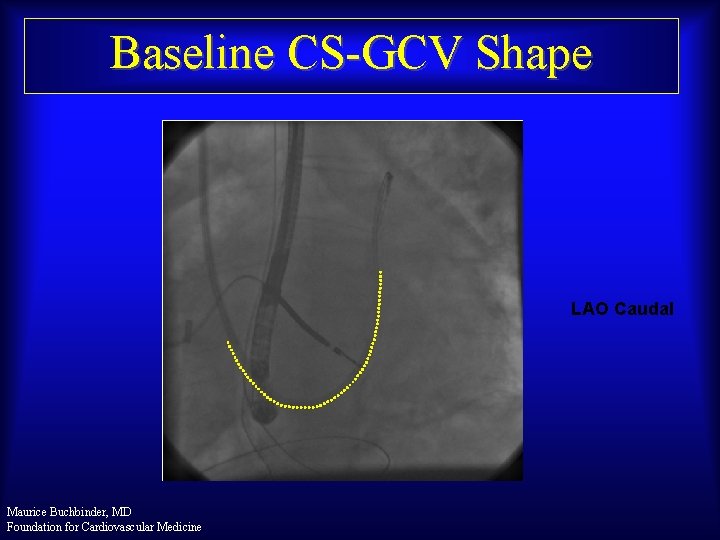
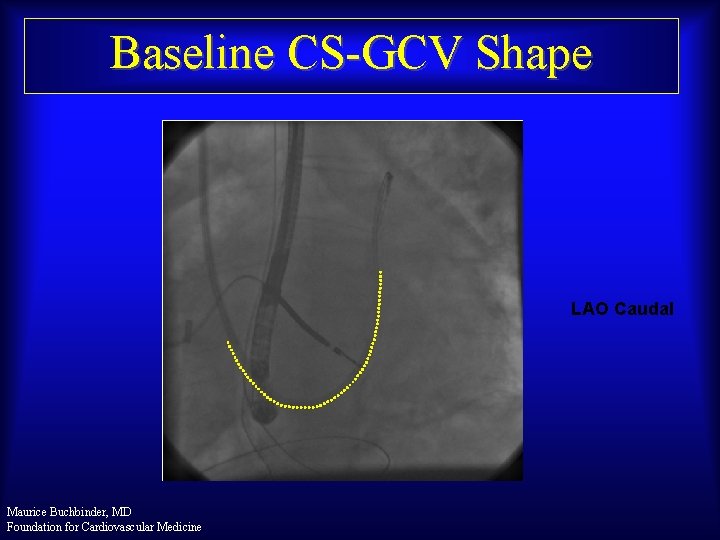
Baseline CS-GCV Shape LAO Caudal Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

PTMA Implant Proximal Adjustment Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
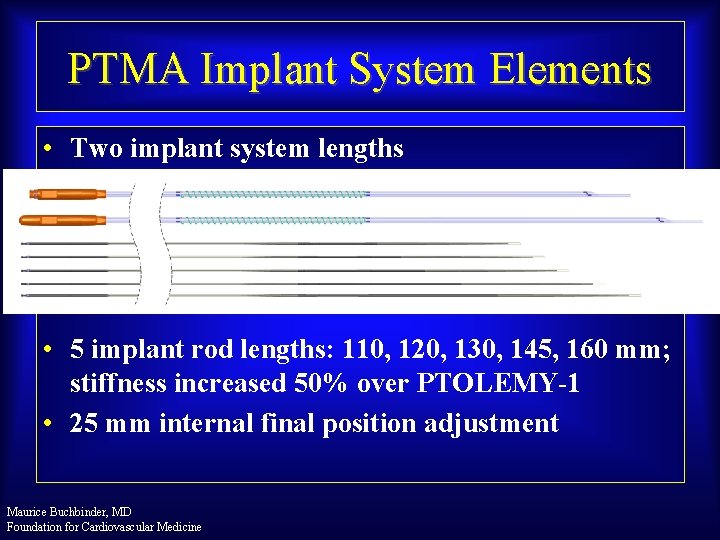
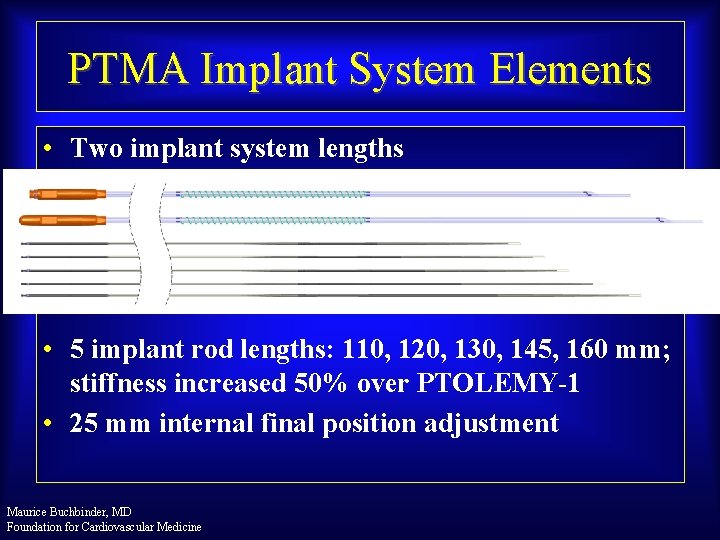
PTMA Implant System Elements • Two implant system lengths • 5 implant rod lengths: 110, 120, 130, 145, 160 mm; stiffness increased 50% over PTOLEMY-1 • 25 mm internal final position adjustment Maurice Buchbinder, MD Foundation for Cardiovascular Medicine

PTOLEMY-1 Patient Study Flow • Start: May 2006 • Close April 2008 Maurice Buchbinder, MD Foundation for Cardiovascular Medicine
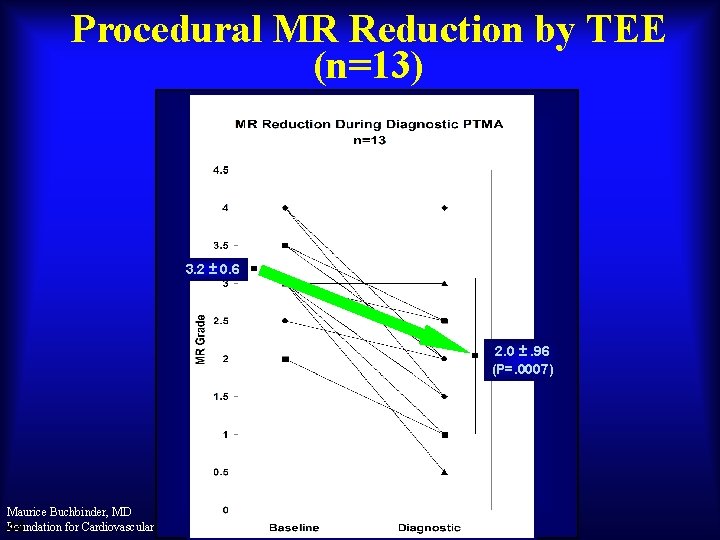
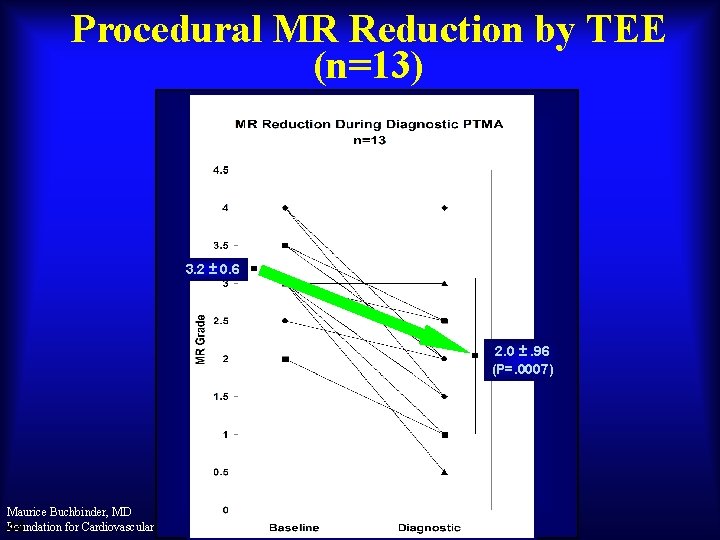
Procedural MR Reduction by TEE (n=13) 3. 2 ± 0. 6 2. 0 ±. 96 (P=. 0007) Maurice Buchbinder, MD Foundation for Cardiovascular Medicine 44

PTOLEMY 2 Trial Europe & Canada • • Indications: II + III NYHA Heart Failure quantitative echo criteria for moderate to severe MR • • • Number of Subjects: 50 enrolled, 30 implants – Europe 30 enrolled, 20 implants - Canada • • • Follow-up periods: Discharge, 1, 3, 6, & 12 mo 2 – 5 years implanted patients • • • Design: Non-randomized, parallel follow-up 8 Centers Europe 3 Centers Canada Enrollment rate = 1 pt /mo /ctr Maurice Buchbinder, MD Foundation for Cardiovascular Medicine • Endpoints: • • • • Safety – 30 days 1° Device / Procedure-Related Major Cardiac Adverse Events Efficacy – 6 months & 12 months 1° MR reduction – echo core lab 2° Quality of life: - Minnesota QOL - 6 minute walk distance Obs: EQ-5 D Obs: Left ventricular size Obs: Rehospitalization rate Obs: Mortality and morbidity

PTOLEMY-2 Interim Progress Patients Brought To Cath Lab (n=17) 15 PTMA Implant Attempted (n=15) Venography exclusion (1) L Subclavian access unsuccessful; planned repeat from R (1) Access site bleeding complication (1) No acute PTMA efficacy (1) OM 1 Impingement (1) 12 Patient Recovered With PTMA Implant (n=12) 9 80% Implant Procedure Success Rate Perc PTMA Removal @ 57 days, OM 1 Bridging (1) Perc PTMA Removal @ 133 days, Pocket Dehiscence (1) Patient death @ 9 days, VT (1) Implanted Patients With Ongoing Follow-up (n=9) Maurice Buchbinder, MD Foundation for Cardiovascular Medicine 47
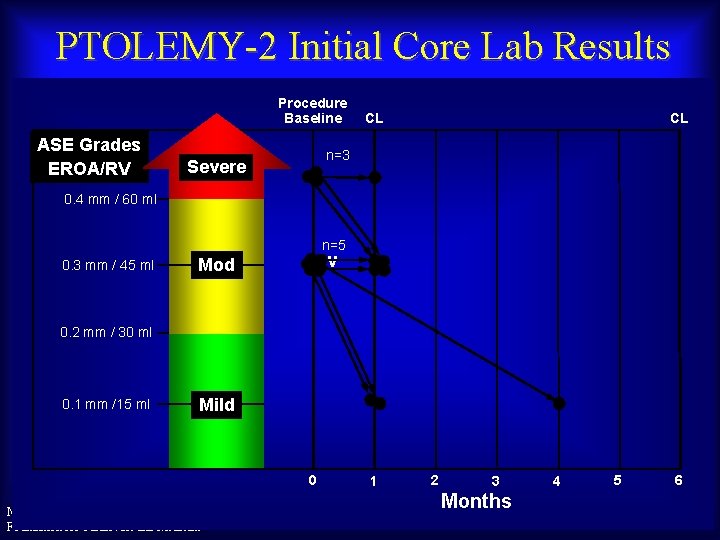
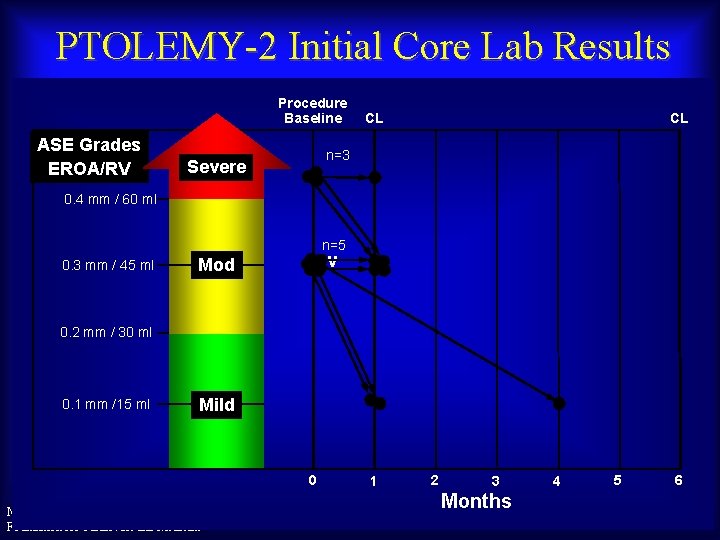
PTOLEMY-2 Initial Core Lab Results Procedure Baseline ASE Grades EROA/RV CL CL n=3 Severe 0. 4 mm / 60 ml n=5 0. 3 mm / 45 ml Mod – v 0. 2 mm / 30 ml 0. 1 mm /15 ml Mild 0 Maurice Buchbinder, MD Foundation for Cardiovascular Medicine 1 2 3 Months 4 5 6
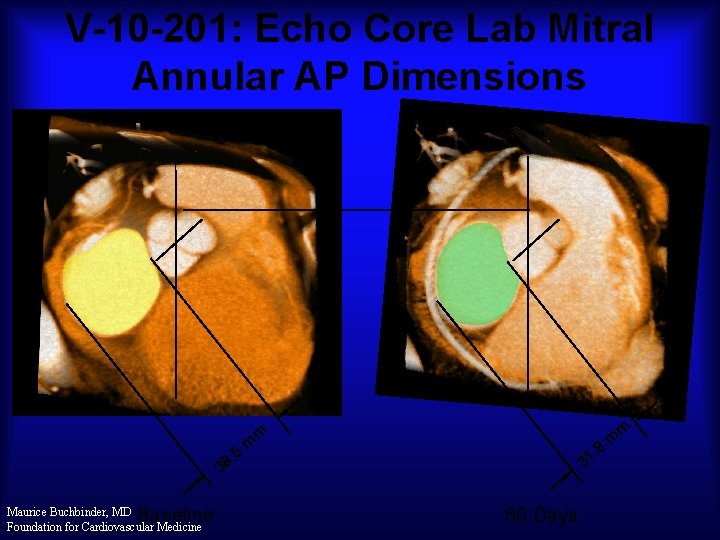
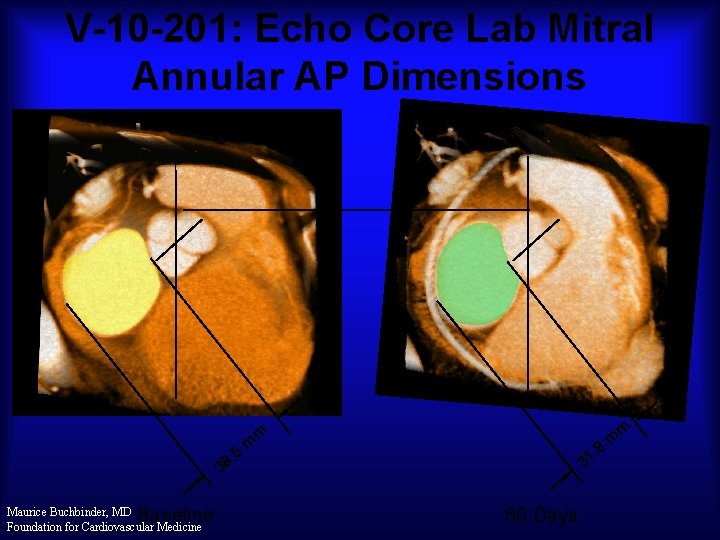
V-10 -201: Echo Core Lab Mitral Annular AP Dimensions m m . 5 8 3 Baseline Maurice Buchbinder, MD Foundation for Cardiovascular Medicine m 8 . 31 60 Days m
Edge-to-edge • e. Valve Coronary sinus annuloplasty • • ? Cardiac Dimensions Carillon • Indirect annuloplasty • • • Direct annuloplasty • Mitralign • Guided Delivery Systems • Quantum. Cor, Cordis DPA • Mi. Cardia, Mitral Solutions Mitral valve replacement • Cardi. AQ • Endovalve Maurice Buchbinder, MD • M-Valve Foundation for Cardiovascular Medicine Today’s Device Landscape: Percutaneous MV Repair
 Pht mitral valve
Pht mitral valve Pht mitral valve
Pht mitral valve Tendyne
Tendyne Apical pulse location
Apical pulse location Vein
Vein Auricle of heart
Auricle of heart Nucleotide excision repair
Nucleotide excision repair Base excision repair vs mismatch repair
Base excision repair vs mismatch repair Percutaneous image-guided lumbar decompression (pild)
Percutaneous image-guided lumbar decompression (pild) Common bile duct diameter
Common bile duct diameter Intrapericardial colon
Intrapericardial colon Ellis curve in pleural effusion
Ellis curve in pleural effusion Indication for cholecystectomy
Indication for cholecystectomy Amnio vs cvs
Amnio vs cvs Contoh soal perkalian sinus
Contoh soal perkalian sinus Sinus arrest vs sinus block
Sinus arrest vs sinus block Types of servo valve
Types of servo valve Ducto toraxico
Ducto toraxico Iam
Iam Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Define mitral stenosis
Define mitral stenosis Adlov
Adlov Wilkins score ms
Wilkins score ms Severe ms heart
Severe ms heart Valva mitral
Valva mitral Mitral klapan prolapsi
Mitral klapan prolapsi Rvh cxr
Rvh cxr Estenose mitral
Estenose mitral Aortal stenoz
Aortal stenoz Valvuloplastia mitral percutánea
Valvuloplastia mitral percutánea Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Aortic regurgitation murmur
Aortic regurgitation murmur Pinched and blue facies
Pinched and blue facies Rhuematic
Rhuematic Mitral facies
Mitral facies Frémissement cataire diastolique
Frémissement cataire diastolique Carvallo belirtisi
Carvallo belirtisi Valvula mitral en paracaidas
Valvula mitral en paracaidas Site:slidetodoc.com
Site:slidetodoc.com Pansystolic murmur causes
Pansystolic murmur causes Atheromatous thoracic aorta
Atheromatous thoracic aorta Professor richard schilling
Professor richard schilling Crux cordis
Crux cordis Shepherd crook rca
Shepherd crook rca Superadded changes in coronary atherosclerosis
Superadded changes in coronary atherosclerosis Global registry of acute coronary events
Global registry of acute coronary events Pulmonary semilunar valve
Pulmonary semilunar valve Cardiac plexus
Cardiac plexus Ductus cysticus
Ductus cysticus