Percutaneous cholecystotomy in acute cholecystitis 27 7 2013











- Slides: 32
Percutaneous cholecystotomy in acute cholecystitis 27 -7 -2013 JHGR
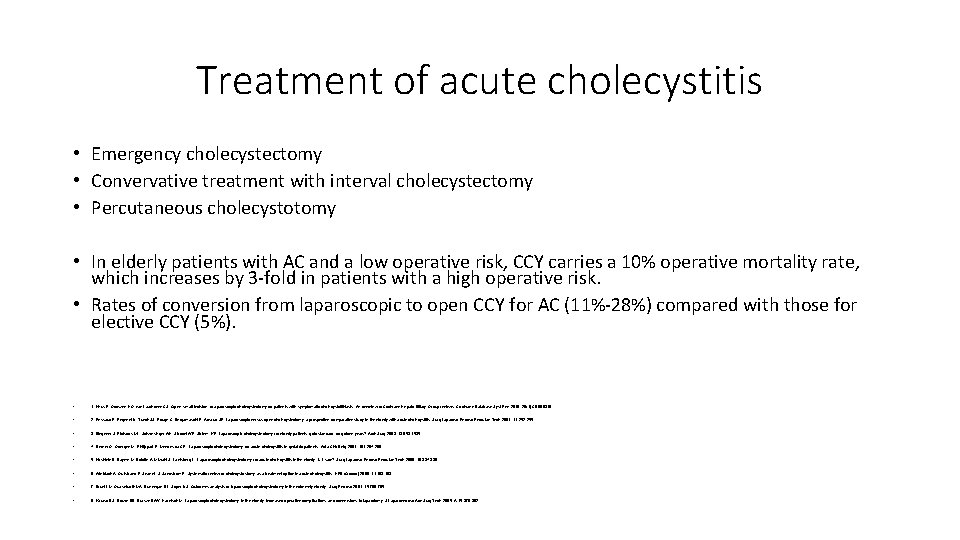
Treatment of acute cholecystitis • Emergency cholecystectomy • Convervative treatment with interval cholecystectomy • Percutaneous cholecystotomy • In elderly patients with AC and a low operative risk, CCY carries a 10% operative mortality rate, which increases by 3 -fold in patients with a high operative risk. • Rates of conversion from laparoscopic to open CCY for AC (11%-28%) compared with those for elective CCY (5%). • 1. Keus F, Gooszen HG, van Laarhoven CJ: Open, small-incision, or aparoscopic cholecystectomy for patients with symptomatic cholecystolithiasis. An overview of Cochrane Hepato-Biliary Group reviews. Cochrane Database Syst Rev 2010, 20(1): CD 008318. • 2. Pessaux P, Regenet N, Tuech JJ, Rouge C, Bergamaschi R, Arnaud JP: Laparoscopic versus open cholecystectomy: a prospective comparative study in the elderly with acute cholecystitis. Surg Laparosc Endosc Percutan Tech 2001, 11: 252 -255. • 3. Bingener J, Richards ML, Schwesinger WH, Strodel WE, Sirinek KR: Laparoscopic cholecystectomy for elderly patients: gold standard for golden years? Arch Surg 2003, 138: 531 -535. • 4. Decker G, Goergen M, Philippart P, Mendes da CP: Laparoscopic cholecystectomy for acute cholecystitis in geriatric patients. Acta Chir Belg 2001, 101: 294 -299. • 5. Kirshtein B, Bayme M, Bolotin A, Mizrahi S, Lantsberg L: Laparoscopic cholecystectomy for acute cholecystitis in the elderly: is it safe? Surg Laparosc Endosc Percutan Tech 2008, 18: 334 -339. • 6. Winbladh A, Gullstrand P, Svanvik J, Sandstrom P: Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford) 2009, 11: 183 -193. • 7. Brunt LM, Quasebarth MA, Dunnegan DL, Soper NJ: Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc 2001, 15: 700 -705. • 8. Kauvar DS, Brown BD, Braswell AW, Harnisch M: Laparoscopic cholecystectomy in the elderly: increased operative complications and conversions to laparotomy. J Laparoendosc Adv Surg Tech 2005, A 15: 379 -382.
Percutaneous cholecystotomy • first described by Radder in 1980 • immediate decompression of the acutely inflamed gallbladder • diagnostic tool in patients with unexplained sepsis. • Cholecystostomy drainage can even be performed at the bedside in the intensive care unit (ICU) in critically ill patients.
Absolute contraindications to PC • Interposed bowel preventing access to the gallbladder • severe bleeding diathesis
Relative contraindications for PC • decompressed gallbladder due to perforation • gallbladder completely packed with calculi • Gallbladder cancer

Currrent evidence • How to perform When to perform Who to perform
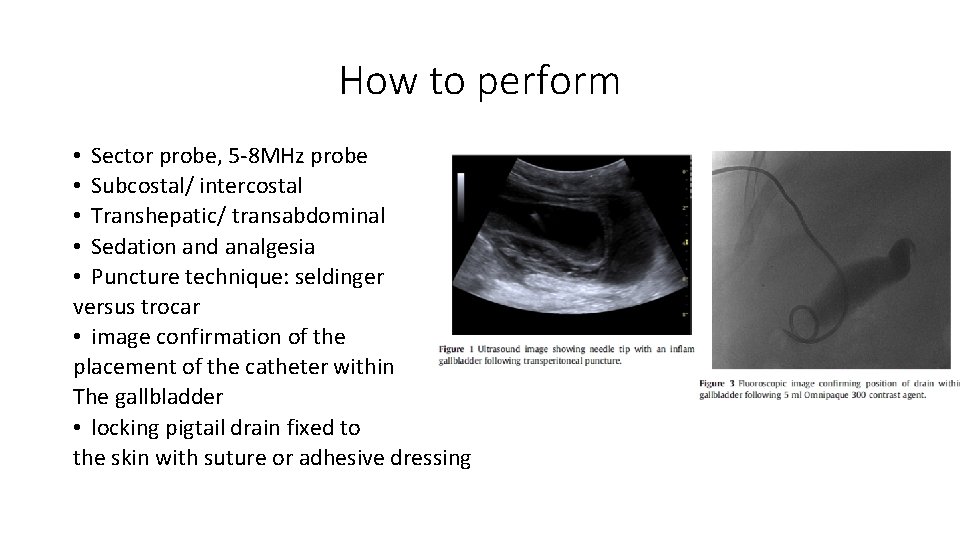
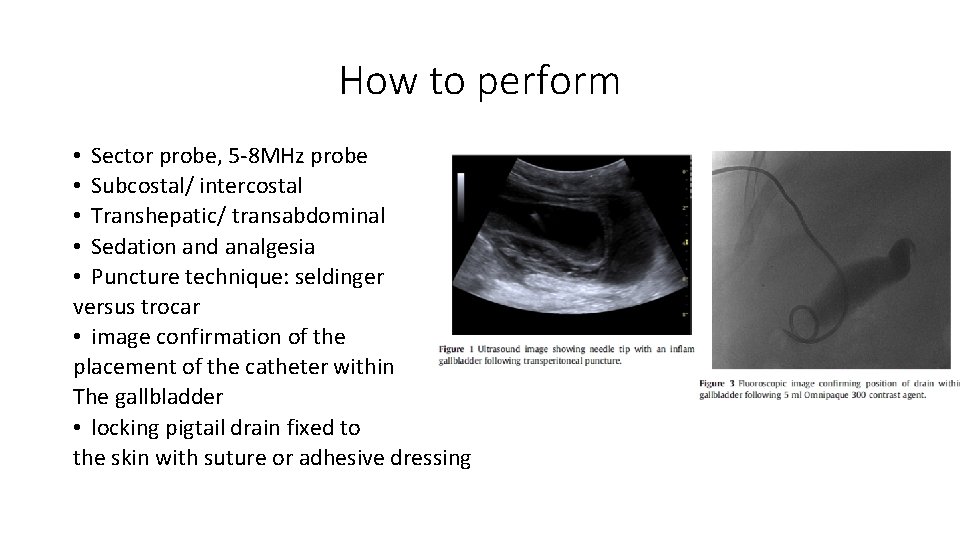
How to perform • Sector probe, 5 -8 MHz probe • Subcostal/ intercostal • Transhepatic/ transabdominal • Sedation and analgesia • Puncture technique: seldinger versus trocar • image confirmation of the placement of the catheter within The gallbladder • locking pigtail drain fixed to the skin with suture or adhesive dressing
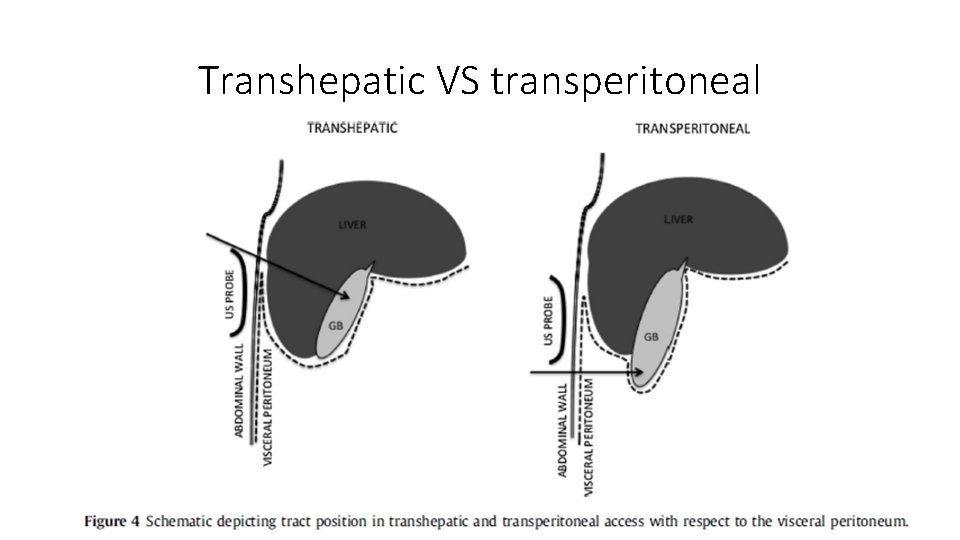
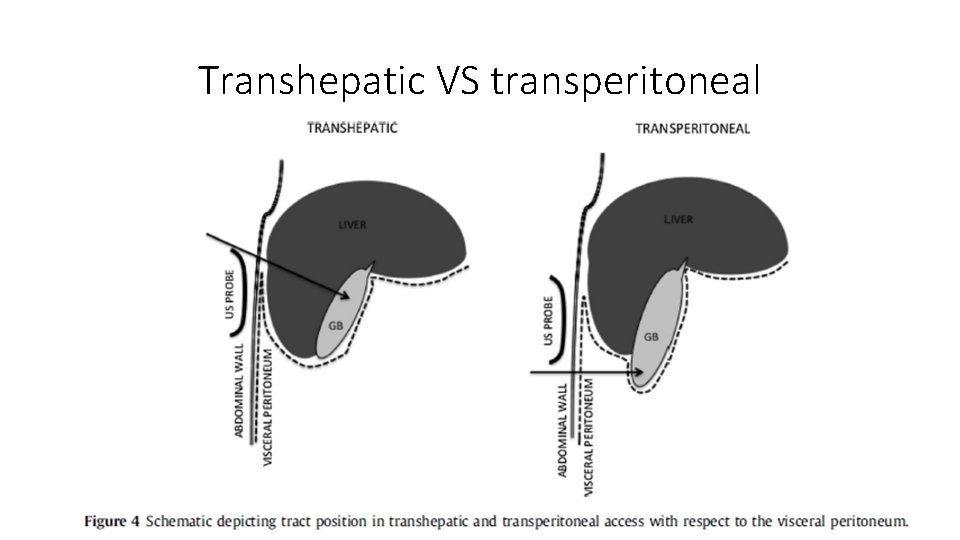
Transhepatic VS transperitoneal

Post procedural care • Antibiotics • Daily flush with 10 ml NS • Cholecystogram: patency, position, gall stone • Tract maturation: ~2/52 • Removal: 1 mth after trial of spigot/ clamp drain • Recurrence rates of calculus cholecystitis are as high as 46% at 3 years
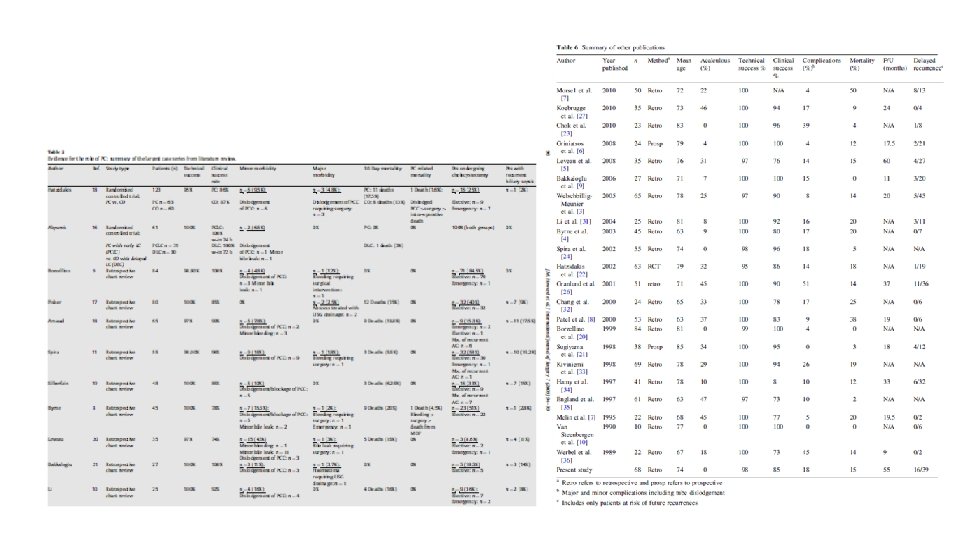
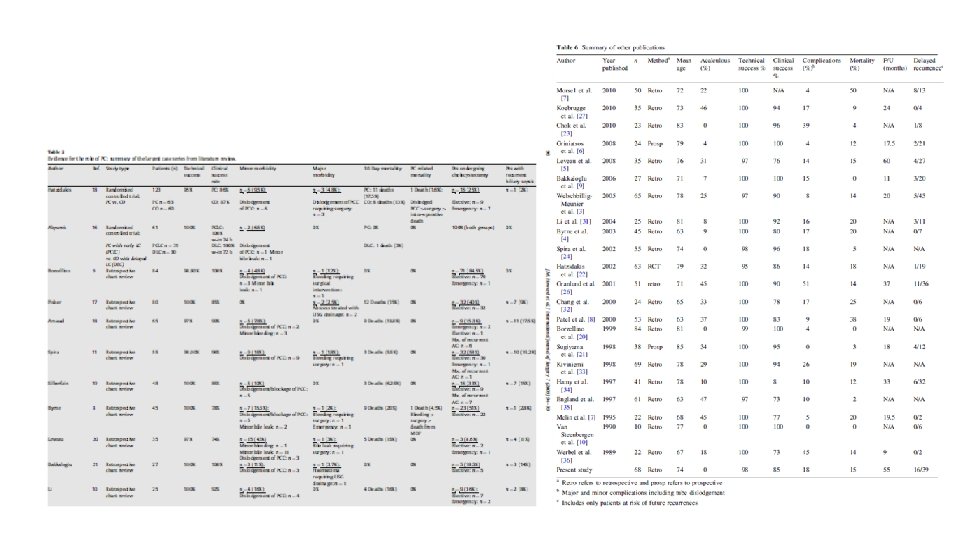
Outcome • • Successful rate >90% Successful clinical response: 85. 6% (1498/1751) Median time to clinical improvement: 3 days Acute complications: haemorrhage, sepsis (either exacerbation or de-novo), vasovagal reactions, bile leak, bowel perforation, and pneumothorax. (3%) Catheter migration is the most common complication, in 8. 6% (98/1144) of patients Mortality resulting from biliary infection is 3. 6% (64/1768), and directly resulting from PC as 0. 4% (7/1861 patients). 30 days mortality rates from PC : 1 -25%, compares to a mortality rate of 0. 96% (5/523) for patients undergoing elective surgical cholecystectomy, and 13% (7/54) patients post-emergency surgery. Lack of prospective, randomized, controlled trials limits the ability to define its specific role Winbladh A, Gullstrand P, Svanvik J, et al. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB ( Oxford) 2009; 11: 183 e 93 Chang L, Moonka R, Stelzner M. Percutaneous cholecystostomy for acute cholecystitis in veteran patients. Am J Surg 2000; 180: 198 e 202. 56. Avrahami R, Badani E, Watemberg S, et al. The role of percutaneous transhepatic cholecystostomy in the management of acute cholecystitis in high-risk patients. Int Surg 1995; 80: 111 e 4
When to perform • 2009 Cochrane review : no level A or level B evidence to support the use of PC over CCY in AC. • 53 studies, 1918 patients • significantly higher 30 -day mortality rate after PC (15. 4%) compared with CCY (4. 5%) (P<. 001). • ? PC patients being at higher risk than CCY patients • inconsistencies in the reporting of periprocedural outcomes • inconsistent reporting of disease severity and comorbidities • unclear inclusion criteria with regard to the ascertainment of AC diagnoses.

PC VS Surgery Revisiting Percutaneous Cholecystostomy for Acute Cholecystitis Based on a 10 -Year Experience Youmna Abi-Haidar, MD; Vivian Sanchez, MD; Sandra A. Williams, MS; Kamal M. F. Itani, MD Arch Surg. 2012; 147(5): 416 -422 • Design: Retrospective cohort study. • Patients: All consecutive patients with AC per the Tokyo criteria who underwent PC or CCY from January 1, 2001, through December 31, 2010. • Main Outcome Measures: Differences in baseline characteristics and outcomes between PC and CCY patients, odds of PC vs CCY use, and odds of death after PC or CCY.



Conclusion • PC should be reserved for patients with prohibitive risks for surgery, irrespective of the severity of AC or the risk of conversion from laparoscopic to open CCY. • Targeted investigations into operative risk stratification models for AC patients are warranted.
PC VS conservative treatment Hatzidakis AA, Prassopoulos P, Petinarakis I, Sanidas E, Chrysos E, Chalkiadakis G, et al. Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol 2002; 12(7): 1778 e 84. • 60 patients (42 with calculous and 18 with acalculous cholecystitis): conservative treatment, • 63 patients (44 with calculous and 19 with acalculous cholecystitis) : PC. • APACHE II score of >=12 • Tubes were successfully placed in 60 of the 63 patients (95%) in the PC group, 54 patients (86%) had clinical resolution of cholecystitis • 7 had surgery due to tube dislodgement (3 patients), persisting symptoms (3 patients), or after unsuccessful PC (1 patient). • 30 -day mortality in the PC group: 18%.
PC VS conservative treatment Hatzidakis AA, Prassopoulos P, Petinarakis I, Sanidas E, Chrysos E, Chalkiadakis G, et al. Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol 2002; 12(7): 1778 e 84. • conservative group: successful resolution of symptoms in 52 of 60 patients (87%) • 30 -day mortality rate: 13% (8 patients). • no significant difference in mortality between the two groups • Conclusion: 1. PC did not reduce mortality compared to conservative treatment of cholecystitis. 2. PC should be reserved for those who fail to improve with conservative treatment initially ~3 days
Haemodialysis patients • an independent risk factor for developing acute cholecystitis • incidence of acute cholecystitis being 5. 8 per 1000 patient-years in the ESRD patients, compared with 0. 92 per 1000 patient-years in the control group • Mortality rates of up to 70% following emergency abdominal surgery in haemodialysis patients • retrospective study showed 100% technical success, and 79% clinical success in 11 out of 14 chronic HD patients with ASA grade IV, treated with PC for acute cholecystitis, with a mean follow-up time of 13. 3 (4 -21) months • Chen Y-T, Ou S-M, Chao P-W, et al. Acute cholecystitis in end-stage renal disease patients: a nation-wide longitudinal study. Dig Liver Dis 2012. 8. • Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373 e 83.

ICU patients, acalculous cholecystitis • acalculous cholecystitis, which accounts for 2 -14% of all cases of acute cholecystitis. • case series of 57 patients with acute acalculous cholecystitis, PC was technically successful in all patients, with symptomatic resolution within 4 days in 93%. • Of the 28 patients managed with PC as the definitive treatment, cholecystostomy tubes were removed within a median period of 51 days. • Recurrent acute cholecystitis occurred in 7% (2/28) over a median follow-up of 32 months • Hamp T, Fridrich P, Mauritz W, et al. Cholecystitis after trauma. J Trauma 2009; 66: 400 e 6. • Pelinka LE, Schmidhammer R, Hamid L, et al. Acute acalculous cholecystitis after trauma: a prospective study. J Trauma 2003; 55: 323 e 9. • Theodorou P, Maurer CA, Spanholtz TA, et al. Acalculous cholecystitis in severely burned patients: incidence and predisposing factors. Burns 2009; 35: 405 e 11.
Pregnancy • gallstones: 1 -3% of patients • Acute cholecystitis in pregnancy traditionally managed conservatively, leading to prolonged treatment, anxiety, and multiple hospital admissions • as a temporizing measure until elective cholecystectomy post-partum • first or final trimester treated with less invasive procedures, i. e percutaneous techniques, enabling elective cholecystectomy • in the “safe” second trimester, or post-partum, cholecystectomy • Dietrich 3 rd CS, Hill CC, Hueman M. Surgical diseases presenting in pregnancy. Surg Clin North Am 2008; 88: 403 e 19. viieviii.
Who to perform • vascular surgeons with endovascular skills • clinical records of all high-risk patients who underwent PC placement by surgeons (group A; n 22) for acute cholecystitis were reviewed. Treatment outcomes were compared with patients who underwent PC by interventional radiologists (group B; n 26). Percutaneous cholecystostomy for acute cholecystitis in high-risk patients: experience of a surgeon-initiated interventional program Eric J. Silberfein, M. D. , Wei Zhou, M. D. , Panagiotis Kougias, M. D. , Hosam F. El Sayed, M. D. , Tam T. Huynh, M. D. , Daniel Albo, M. D. , Ph. D. , David H. Berger, M. D. , F. Charles Brunicardi, M. D. , Peter H. Lin, M. D. * Department of Surgery, Baylor College of Medicine, Michael E. De. Bakey VA Medical Center, Houston VAMC (112), 2002 Holcomb Blvd. ,

Who to perform • percutaneous image-guided procedure can be performed safely by surgeons with appropriate catheter-based skills. • institutional support • establishment of a relevant credentialing guideline • the creation of a collaborative surgeon-initiated interventional program has enabled surgeons to provide comprehensive care including percutaneous to surgical management strategies to patients with biliary disease.
• A Cochrane review published in 2009 concluded that here was no level A or level B evidence to support the use of PC over CCY in AC. • Healthy young patient: CCY, old critical ill patient: PC, ? subgroup in between • Current literature and fail to answer which therapy is the best option in ACC in high risk patients. • At present both treatment strategies are used in this patient category • The preference and expertise of the responsible surgeon or the general opinion within the hospital usually determines the choice of treatment.

RCT • Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy (CHOCOLATE trial) • Kirsten Kortram 1, Bert van Ramshorst 1, Thomas L Bollen 2, Marc GH Besselink 1, Dirk J Gouma 3, Tom Karsten 4, • Philip M Kruyt 5, Grard AP Nieuwenhuijzen 6, Johannes C Kelder 7, Ellen Tromp 7 and Djamila Boerma 1*
Methods/Design • randomised controlled, parallel-group, superiority multicenter trial. • APACHE-II score 7 -14, with acute calculous cholecystitis • 2 year period • 284 patients • 30 high volume teaching hospitals • primary endpoint: major complications within three months following randomization and need for re-intervention and mortality during the follow-up period of one year. • Secondary endpoints: all other complications, duration of hospital admission, difficulty of procedures and total costs.
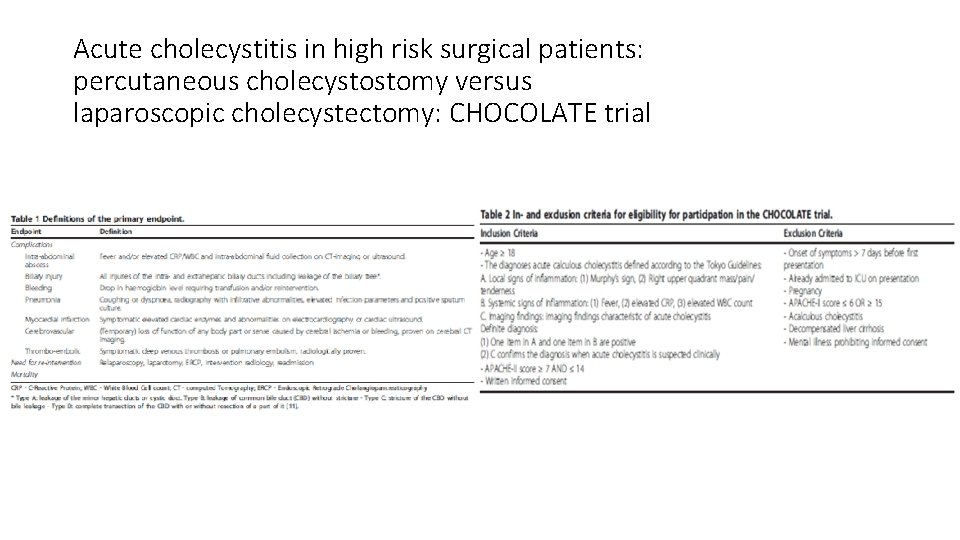
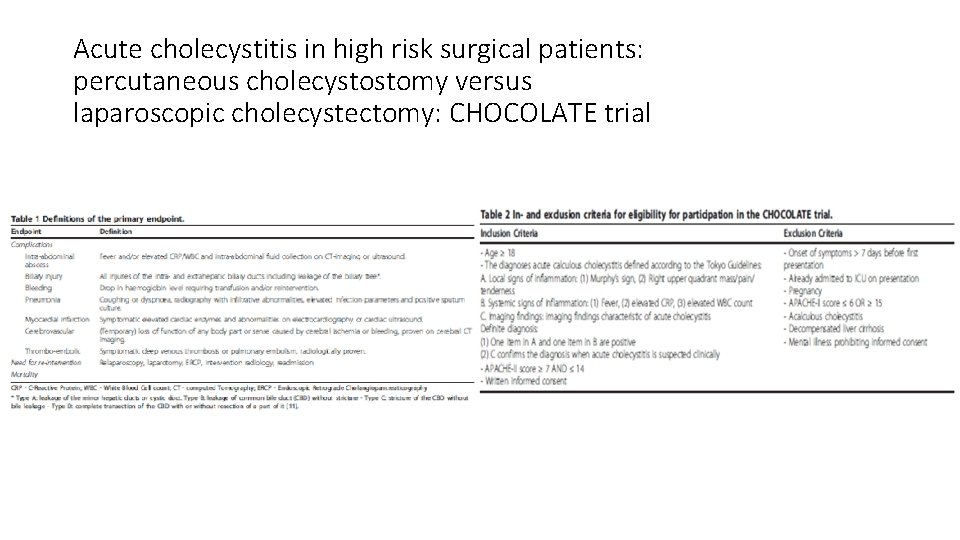
Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy: CHOCOLATE trial

Thank you!

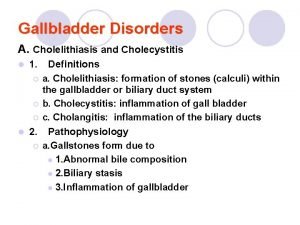
 Cholecystitis
Cholecystitis Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Chronic calculous cholecystitis
Chronic calculous cholecystitis Acute cholecystitis clinical features
Acute cholecystitis clinical features Biliary colic treatment
Biliary colic treatment Amnio vs cvs
Amnio vs cvs Percutaneous image-guided lumbar decompression (pild)
Percutaneous image-guided lumbar decompression (pild) Percutaneous transhepatic cholangiography and drainage
Percutaneous transhepatic cholangiography and drainage Terminal testicular cancer
Terminal testicular cancer Chest xray labelled
Chest xray labelled Intraoperative cholangiogram
Intraoperative cholangiogram Perbedaan cholelithiasis dan cholecystitis
Perbedaan cholelithiasis dan cholecystitis Behandeling cholecystitis
Behandeling cholecystitis Scarred gallbladder
Scarred gallbladder Hepatitis a incubation period
Hepatitis a incubation period Cholecystitis chr calculosa
Cholecystitis chr calculosa Cholecystitis pathogenesis
Cholecystitis pathogenesis Nursing diagnosis for cholecystitis
Nursing diagnosis for cholecystitis Acute glomerulonephritis causes
Acute glomerulonephritis causes Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Acute blood loss anemia
Acute blood loss anemia Bell clapper deformity pictures
Bell clapper deformity pictures Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation Acute intermittent porphyria
Acute intermittent porphyria Health hazards pictogram
Health hazards pictogram Pancreatitis grade ct
Pancreatitis grade ct Accs em
Accs em Worcestershire acute hospitals nhs trust
Worcestershire acute hospitals nhs trust Pancreatitis nursing diagnosis
Pancreatitis nursing diagnosis Parietal pain
Parietal pain Point real world example
Point real world example Gastritis x ray
Gastritis x ray Global registry of acute coronary events
Global registry of acute coronary events