peptic ulcer disease Definition Disruption of mucosal and




















- Slides: 80
peptic ulcer disease
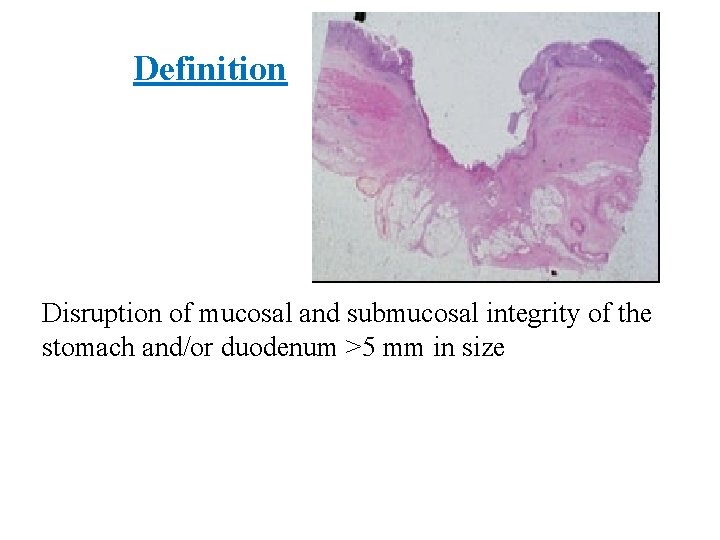
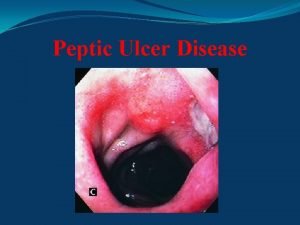
Definition Disruption of mucosal and submucosal integrity of the stomach and/or duodenum >5 mm in size
Epidemiology Peptic ulcer disease Prevalence: 12% of men and 10% of women in U. S. q. Duodenal ulcers § 6– 15% of the Western population q. Gastric ulcers § Less common than DU § occur later in life than DU; peak in 6 decade § More than half occur in males
Epidemiology Helicobacter pylori infection q. Prevalence : Ø 30% in U. S. Ø 10% of Americans < 30 years Ø 80% in developing parts of the world
Risk Factors q. Genetic predisposition Ø First-degree relatives of patients with DU or GU are at 3 -fold increased risk for ulcer Ø Patients with blood group O may be at increased risk; the antigen may be a target of H. pylori.
Risk Factors q. Psychological stress ØEvidence for causal effect is mainly anecdotal. ØIncreased numbers of stressful events do not distinguish patients with DU from those without DU.
Risk factors for H. pylori § § § § Birth or residence in a developing country Domestic crowding Unsanitary living conditions Unclean food or water Exposure to gastric contents Poor socioeconomic status Less education
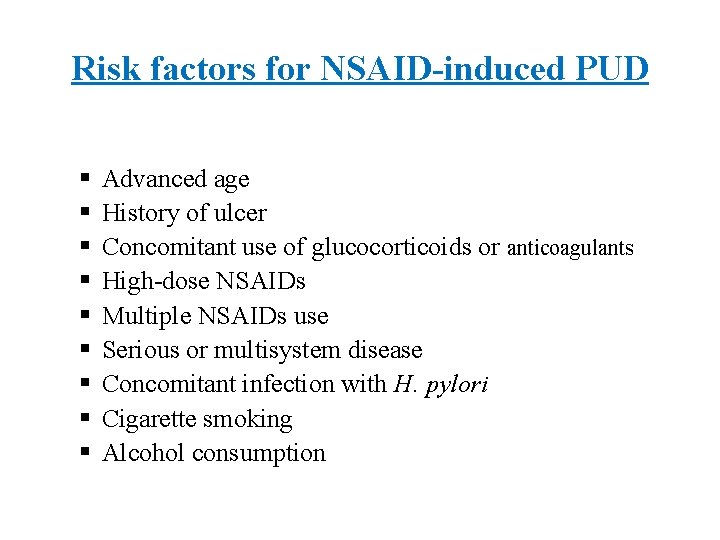
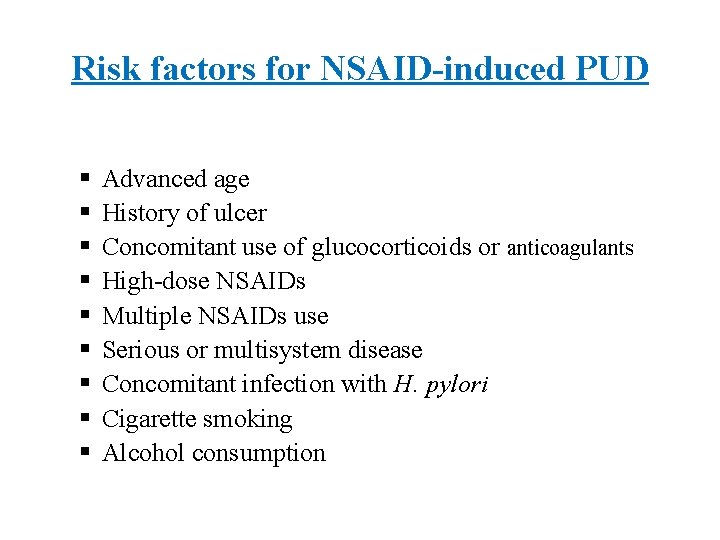
Risk factors for NSAID-induced PUD § § § § § Advanced age History of ulcer Concomitant use of glucocorticoids or anticoagulants High-dose NSAIDs Multiple NSAIDs use Serious or multisystem disease Concomitant infection with H. pylori Cigarette smoking Alcohol consumption
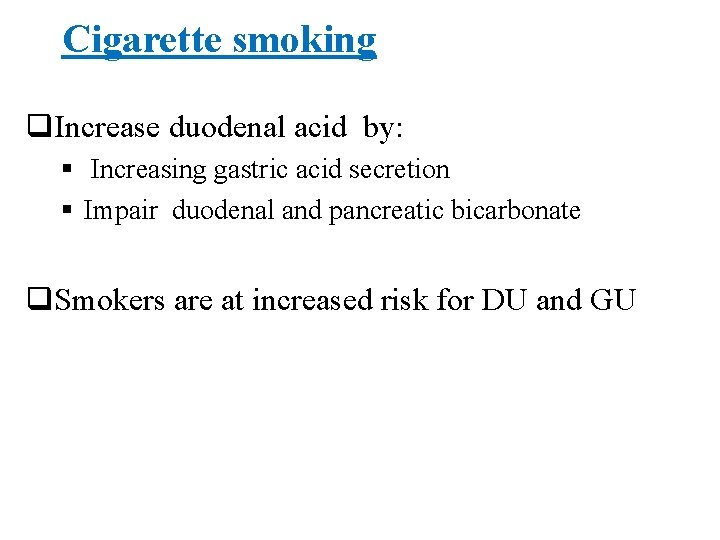
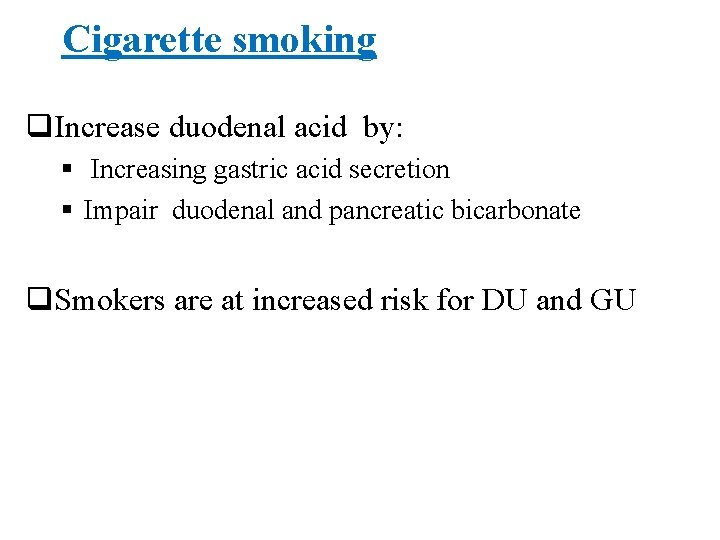
Cigarette smoking q. Increase duodenal acid by: § Increasing gastric acid secretion § Impair duodenal and pancreatic bicarbonate q. Smokers are at increased risk for DU and GU
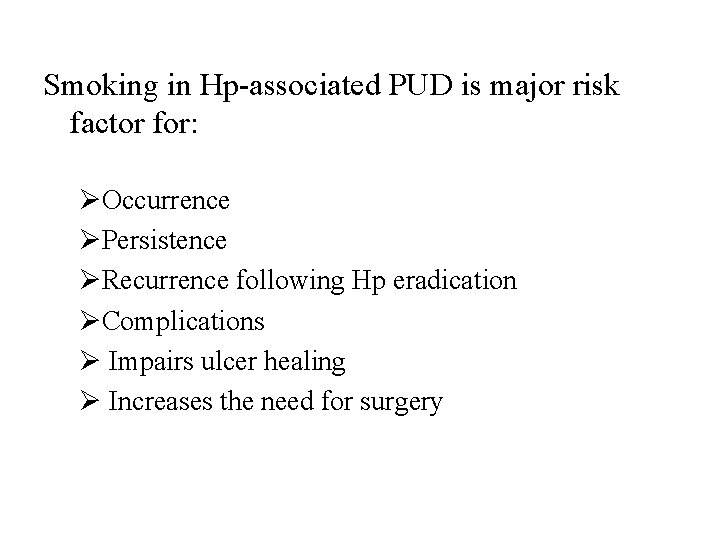
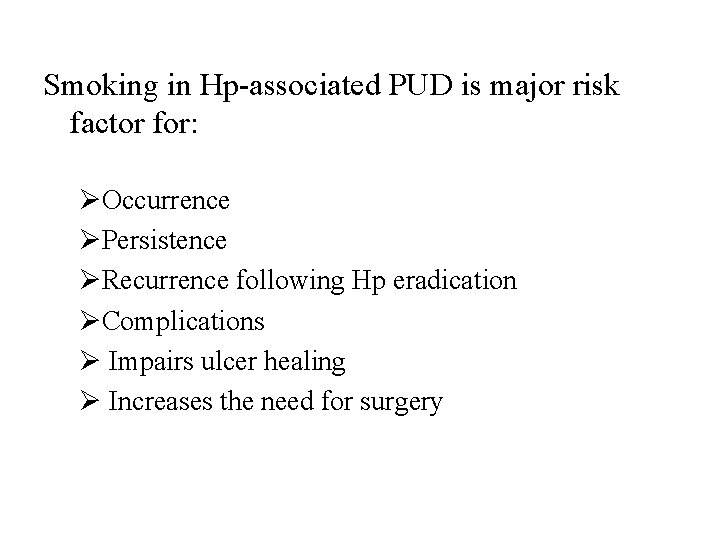
Smoking in Hp-associated PUD is major risk factor for: ØOccurrence ØPersistence ØRecurrence following Hp eradication ØComplications Ø Impairs ulcer healing Ø Increases the need for surgery
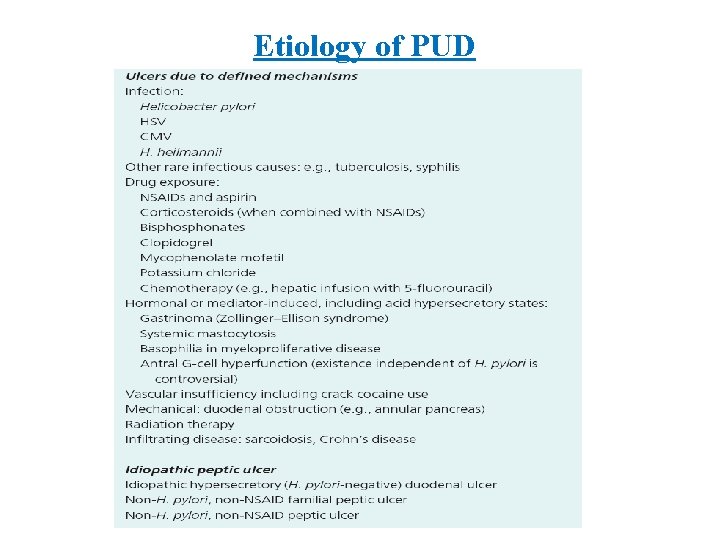
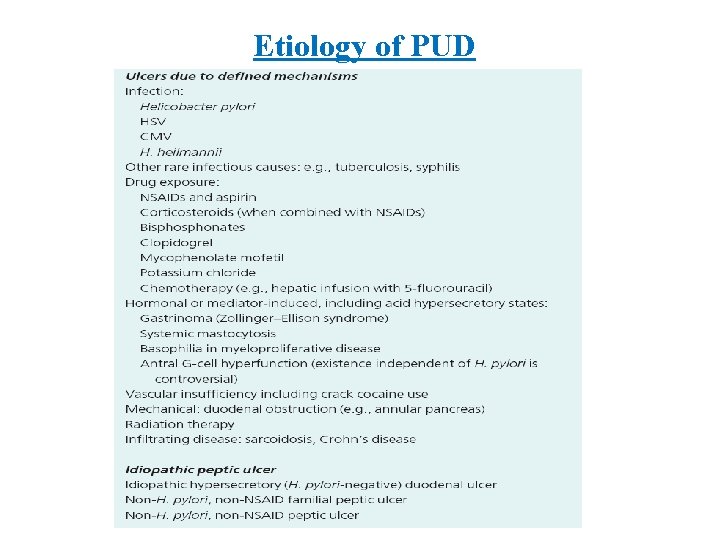
Etiology of PUD

Disease Associated with PUD Ø COPD Ø CRF Ø Cirrhosis Ø Organ transplant Ø Nephrolithiasis Ø α 1 antitrypsin deficiency Ø Hyperparathyroidism Ø Systemic mastocytosis Ø Coronary artery disease Ø Polycythemia vera Ø Chronic pancreatitis
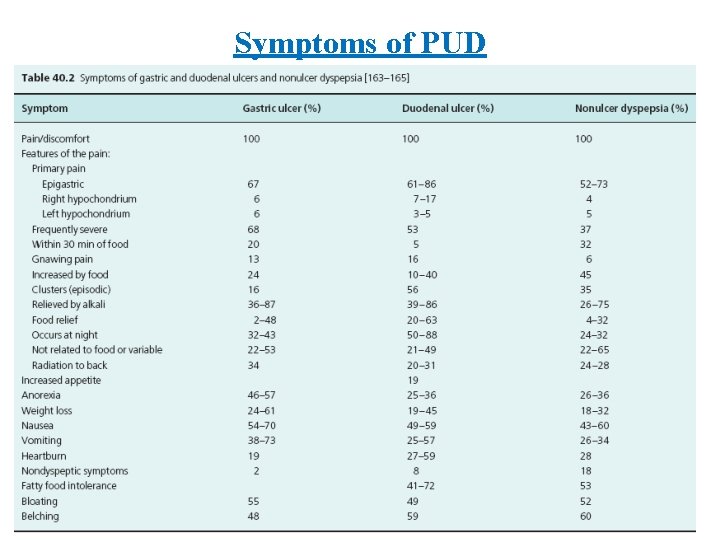
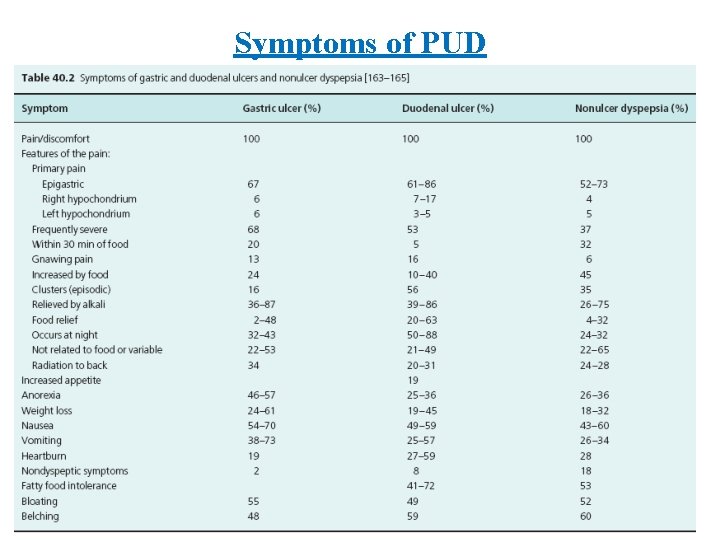
Symptoms of PUD
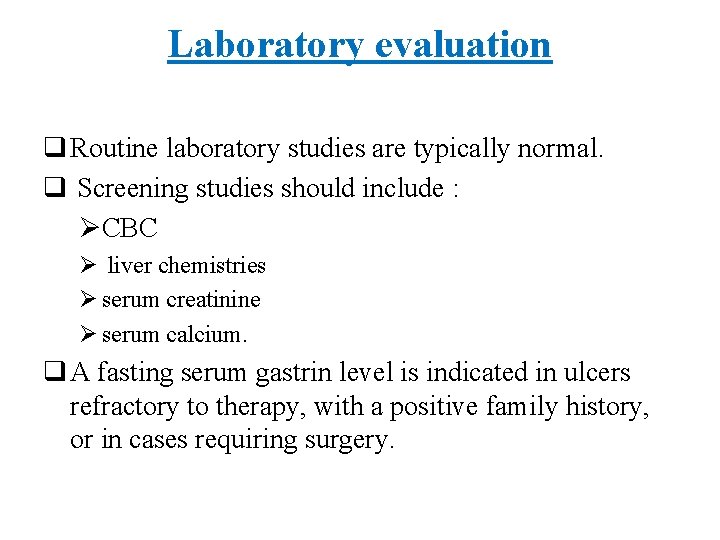
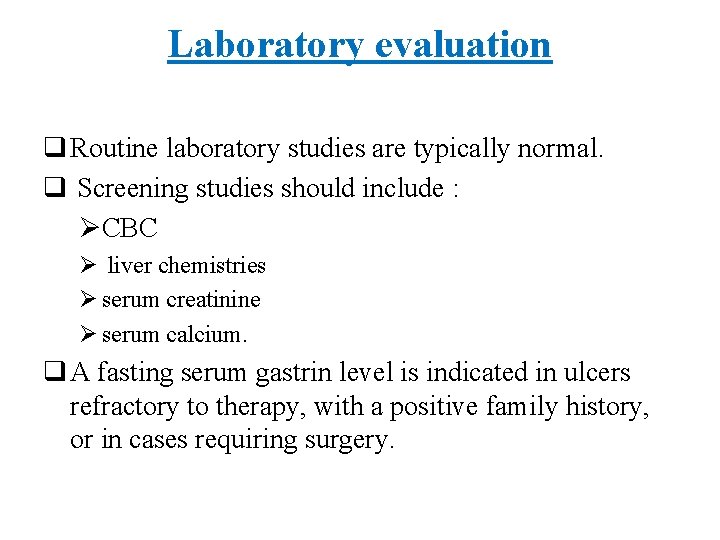
Laboratory evaluation q Routine laboratory studies are typically normal. q Screening studies should include : ØCBC Ø liver chemistries Ø serum creatinine Ø serum calcium. q A fasting serum gastrin level is indicated in ulcers refractory to therapy, with a positive family history, or in cases requiring surgery.



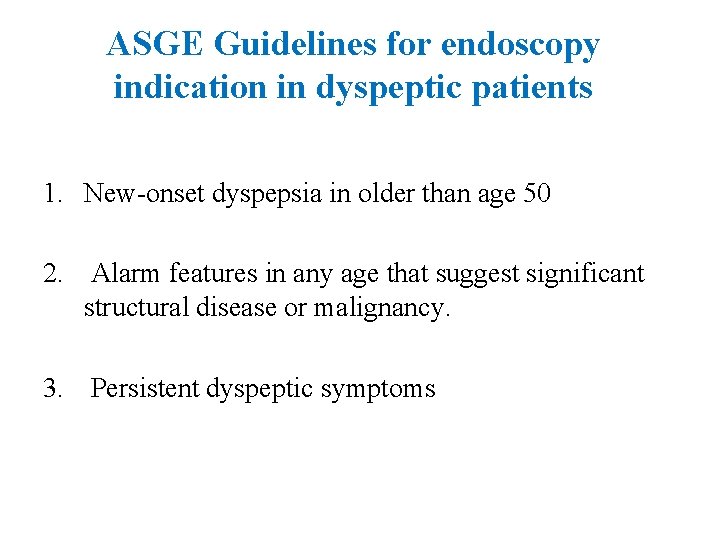
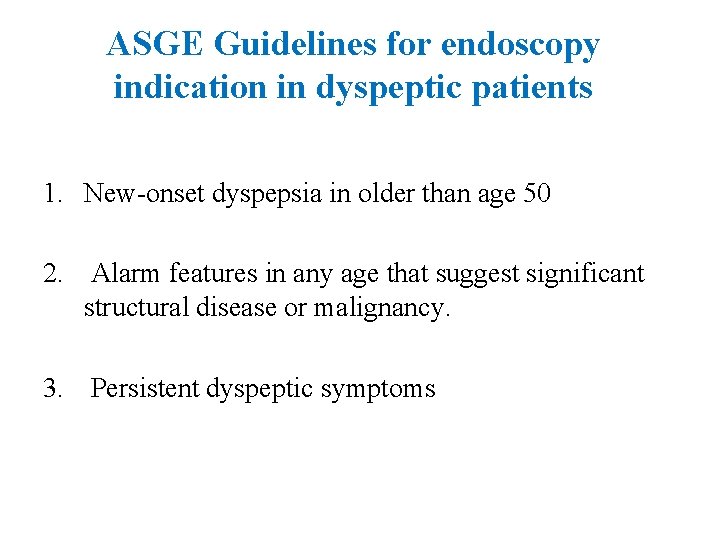
ASGE Guidelines for endoscopy indication in dyspeptic patients 1. New-onset dyspepsia in older than age 50 2. Alarm features in any age that suggest significant structural disease or malignancy. 3. Persistent dyspeptic symptoms
Alarm features q Family history of upper GI malignancy q Weight loss q Overt GI bleeding, iron deficiency anemia q Progressive dysphagia or odynophagia q Persistent vomiting q Palpable mass q Lymphadenopathy.
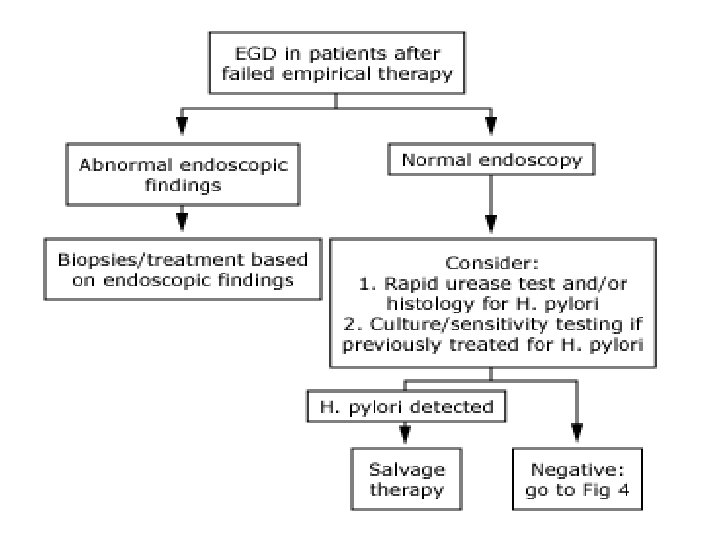
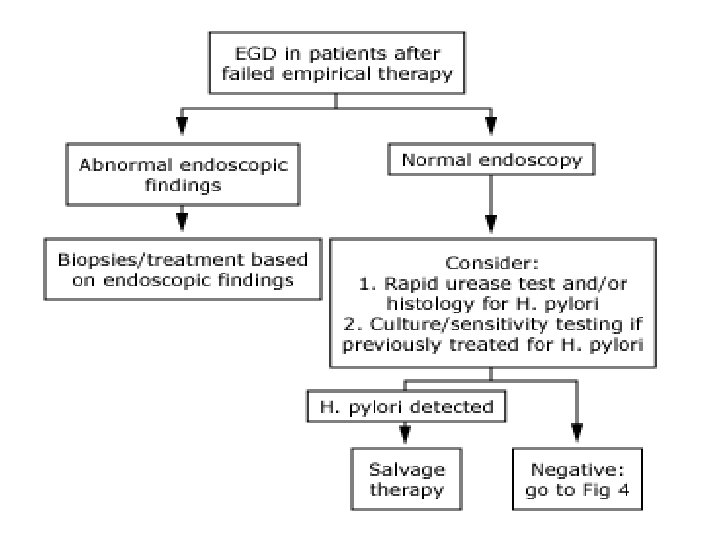
Dyspeptic patients younger than 50 without alarm features q Should be test for H. pylori Ø If positive : H. pylori eradication Ø If negative : Øshort trial (4 -8 weeks) PPI or Ø EGD q NSAID stopped, if possible.
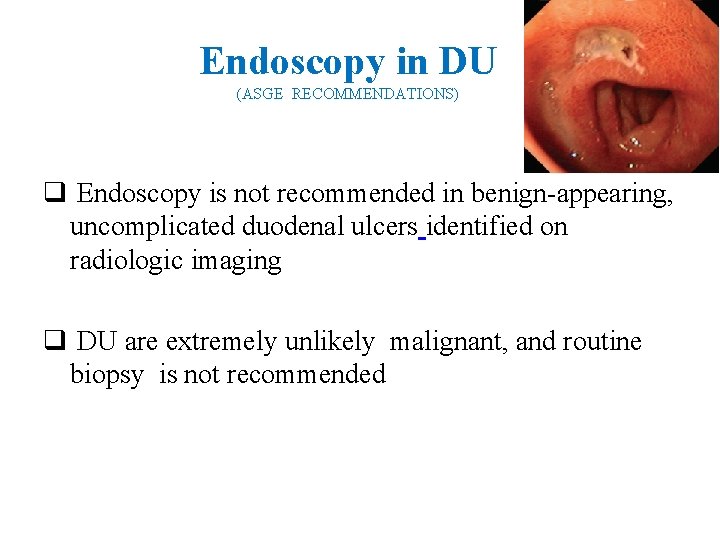
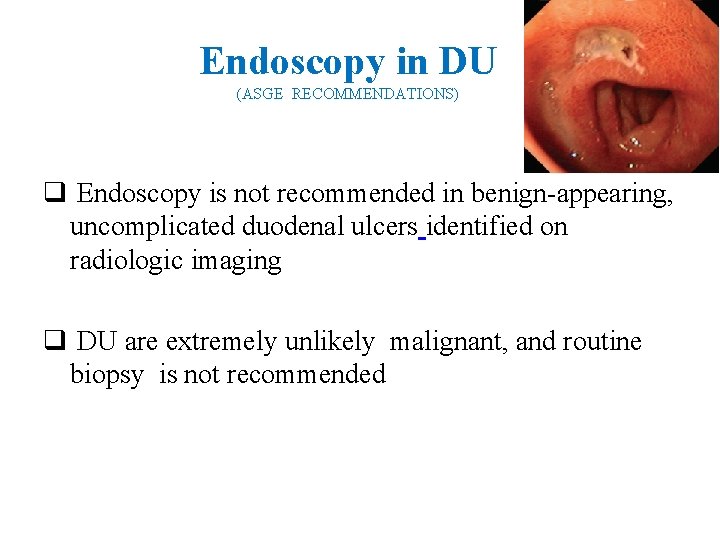
Endoscopy in DU (ASGE RECOMMENDATIONS) q Endoscopy is not recommended in benign-appearing, uncomplicated duodenal ulcers identified on radiologic imaging q DU are extremely unlikely malignant, and routine biopsy is not recommended

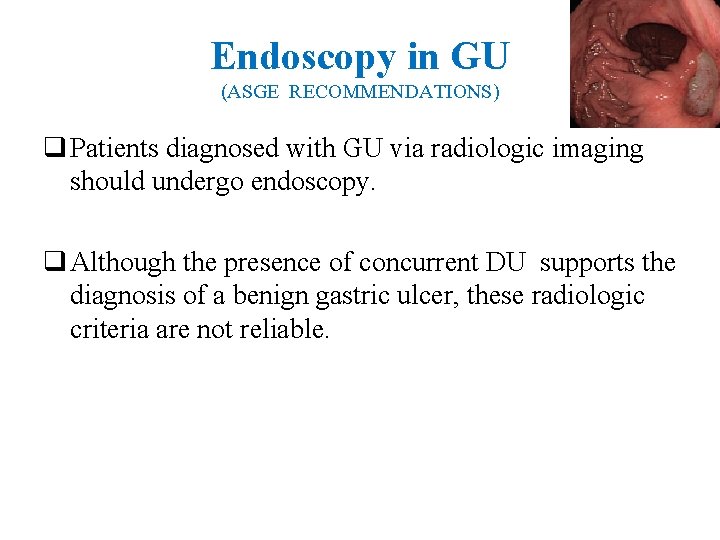
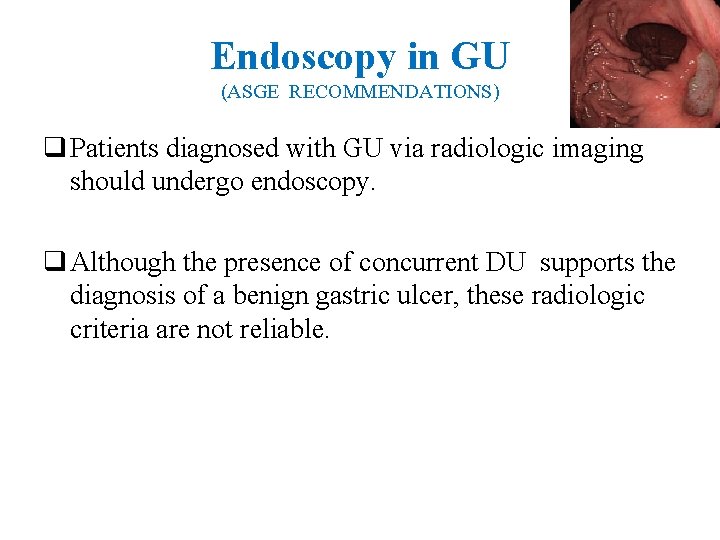
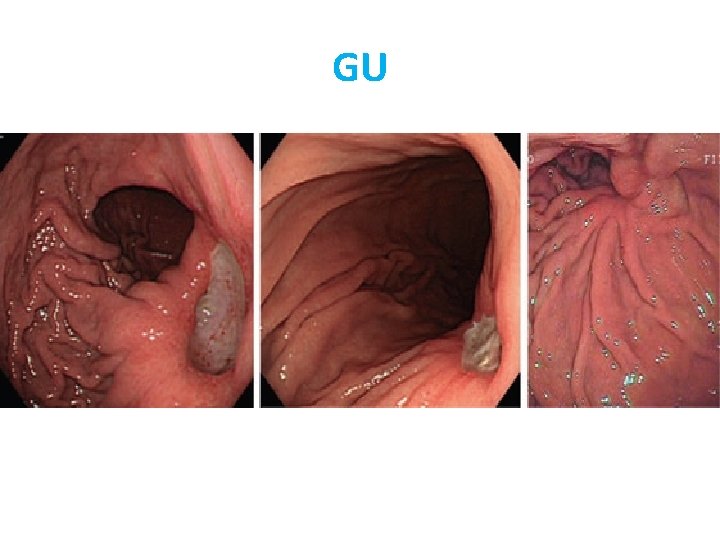
Endoscopy in GU (ASGE RECOMMENDATIONS) q Patients diagnosed with GU via radiologic imaging should undergo endoscopy. q Although the presence of concurrent DU supports the diagnosis of a benign gastric ulcer, these radiologic criteria are not reliable.

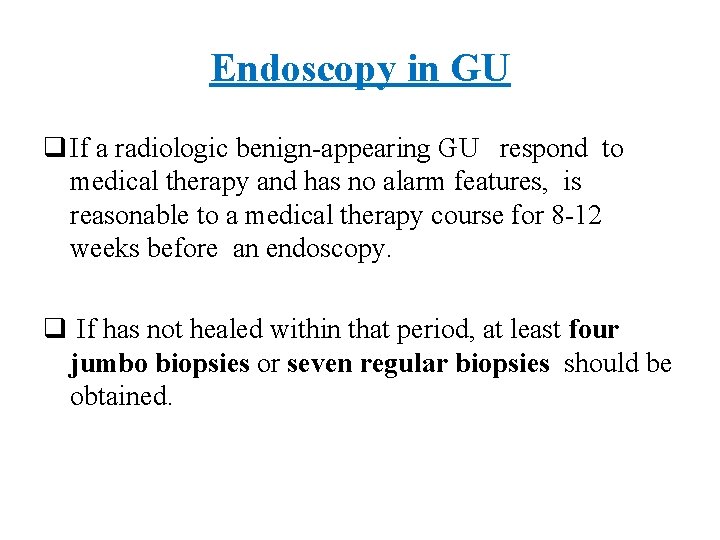
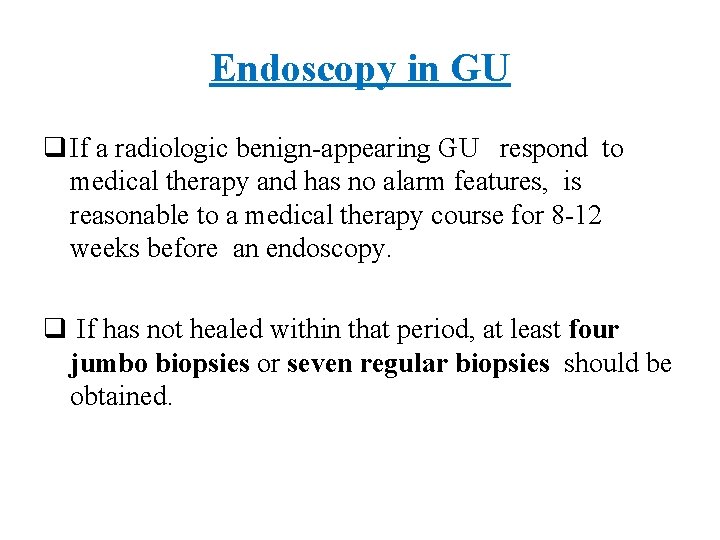
Endoscopy in GU q If a radiologic benign-appearing GU respond to medical therapy and has no alarm features, is reasonable to a medical therapy course for 8 -12 weeks before an endoscopy. q If has not healed within that period, at least four jumbo biopsies or seven regular biopsies should be obtained.
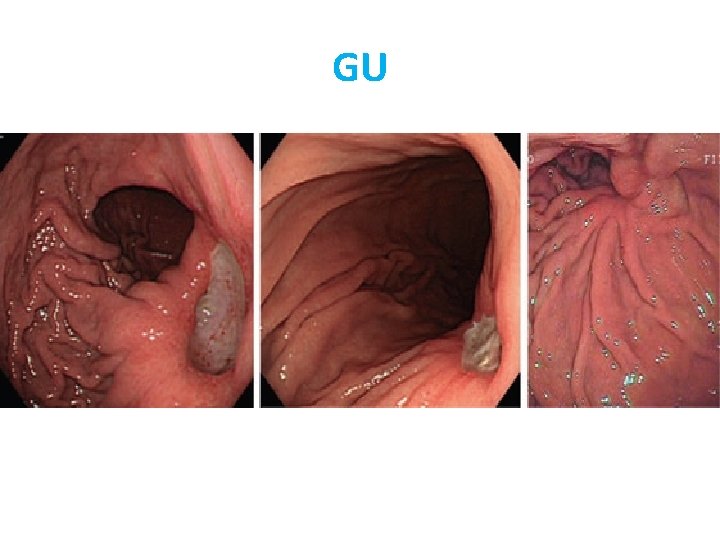
GU
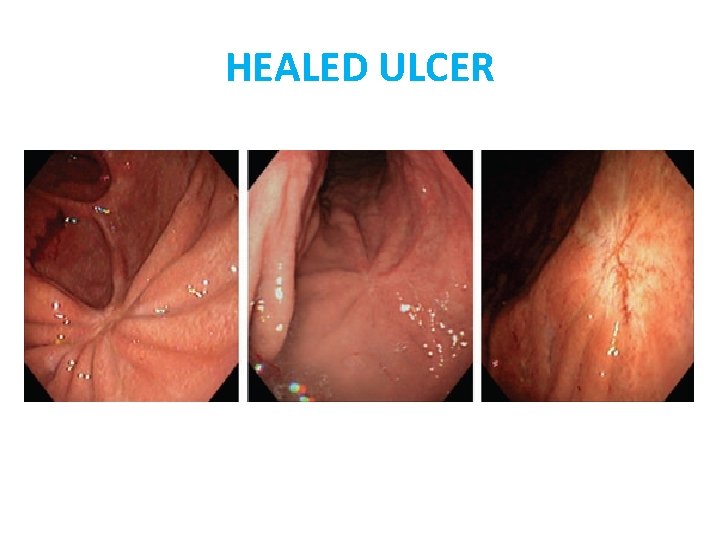
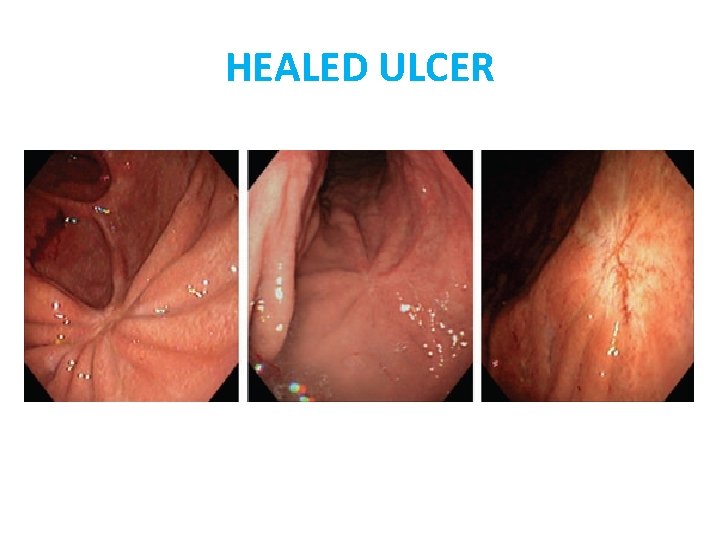
HEALED ULCER
Biopsy in GU q Biopsy of all gastric ulcers was recommended in the past because older data suggested that 5% to 11% of GU represented malignancy q There are no recent data to recommend the need for biopsy of all GU.
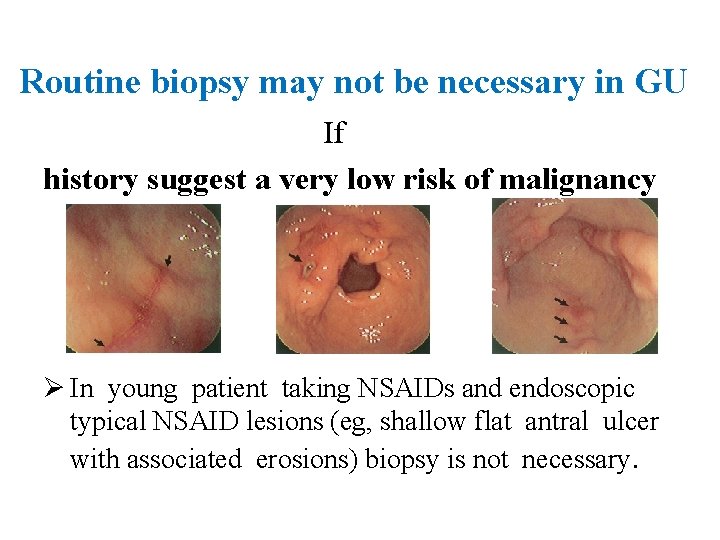
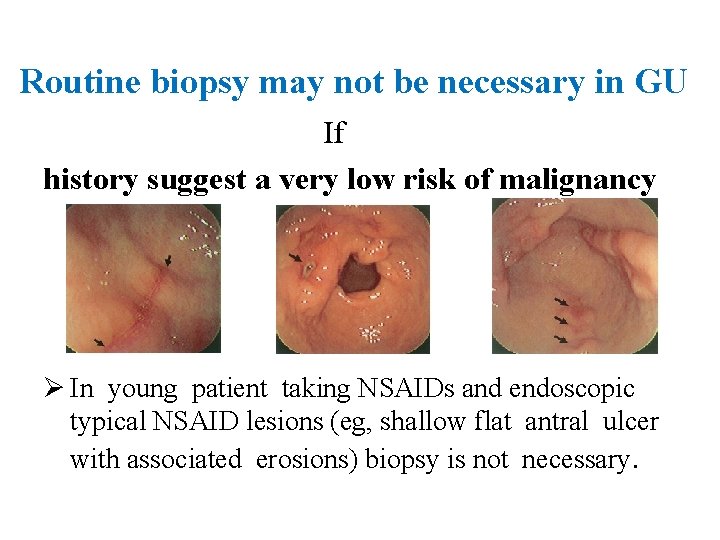
Routine biopsy may not be necessary in GU If history suggest a very low risk of malignancy Ø In young patient taking NSAIDs and endoscopic typical NSAID lesions (eg, shallow flat antral ulcer with associated erosions) biopsy is not necessary.
Role of endoscopic surveillance in DU q Is not recommended if symptoms resolve after a course of acid suppression with H Pylori eradication and discontinuation of NSAID. q Is recommended in persistent symptoms for ØRule out refractory peptic ulcers Ø Rule out ulcers with nonpeptic etiologies

surveillance endoscopy in GU May be unnecessary: ØWhen history suggest a low risk of cancer (eg, a young patient taking NSAIDs with endoscopic appearance of typical NSAID-associated lesions) Ø In benign GU on EGD and biopsy with a defined etiology (eg, NSAID or H Pylori ) that is asymptomatic after a course of therapy
Surveillance EGD indication in GU 1. Endoscopically suspicious for malignancy, even if biopsy samples are benign. 2. Symptomatic despite an appropriate therapy and previous benign biopsy(for detect refractory , benign nonpeptic etiologies and occult malignancy) 3. Those did not biopsied at index EGD for any reason ( active GIB, coagulopathy, patien instability) 4. Gastric ulcers without a clear etiology
ASGE Recommendations in PUD 1. H Pylori testing should be performed in all PUD because it is a common etiology. 2. DU is extremely unlikely to be malignant, and routine biopsy is not recommended. 3. EGD is not recommended in benign-appearing, uncomplicated DU identified on radiologic imaging.
ASGE recommendation cont. 4. Surveillance EGD be considered in DU with persistent symptoms. 5. Most GU need biopsy because malignant GU may appear benign in EGD. • However, in young patients taking NSAIDs with multiple benign-appearing GU, malignancy is very low. Therefore, biopsy and surveillance endoscopy should be individualized.
ASGE recommendation cont. 6. Surveillance endoscopy indication in GU: Ø Symptomatic despite a medical therapy. Ø Ulcer without a clear etiology ØIf biopsy was not obtained at the index EGD. 7. In refractory PUD, surveillance endoscopy should be performed until the ulcer has healed or the etiology has been defined.

ASGE recommendation cont. 8. Endoscopy should be performed early in the course of hospitalization in bleeding PUD 9. In rebleeding after initial endoscopic hemostasis, repeat endoscopic therapy is recommended before considering surgical or radiologic intervention. 10. Endoscopy is not recommend in clinical evidence of acute perforation.
ASGE recommendation cont. 11. Endoscopy recommended for evaluation of gastric outlet obstruction. 12. Endoscopic balloon dilation be considered for the management of benign gastric outlet obstruction.
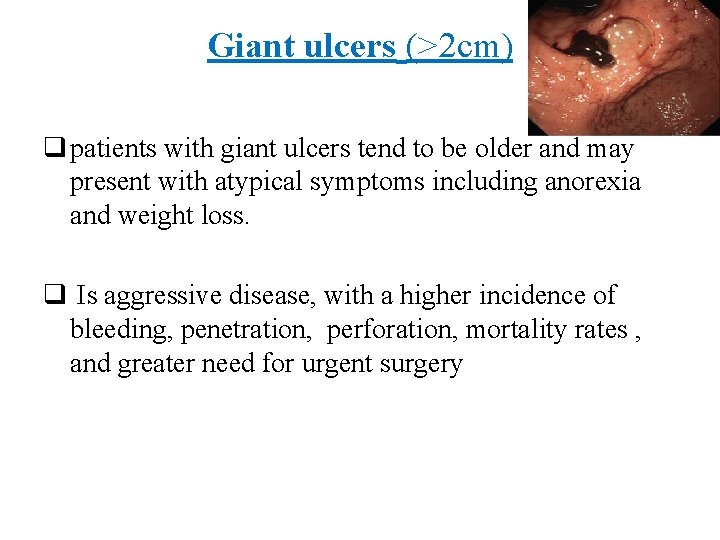
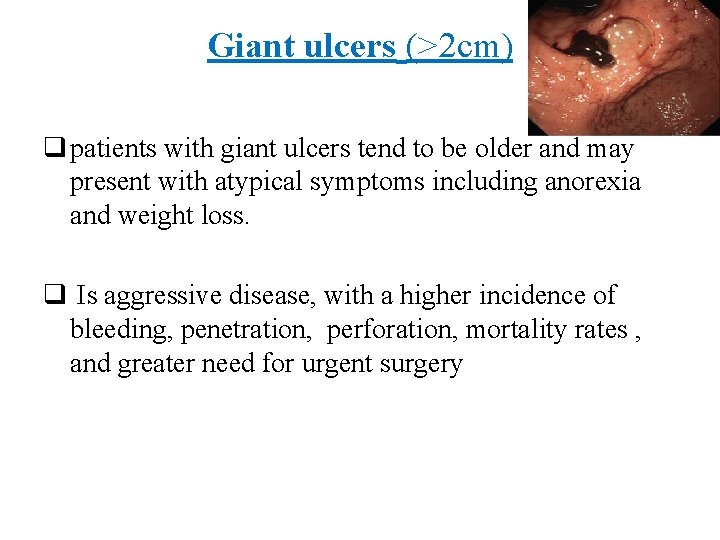
Giant ulcers (>2 cm) q patients with giant ulcers tend to be older and may present with atypical symptoms including anorexia and weight loss. q Is aggressive disease, with a higher incidence of bleeding, penetration, perforation, mortality rates , and greater need for urgent surgery

Rol of EGD in giant ulcer 1. EGD is important for the diagnosis of giant GU because barium studies may miss these ulcers due to their large, shallow craters 2. Ruling out malignancy , Crohn's , eosinophilic gastroenteritis 3. Surveillance and documentation of healing
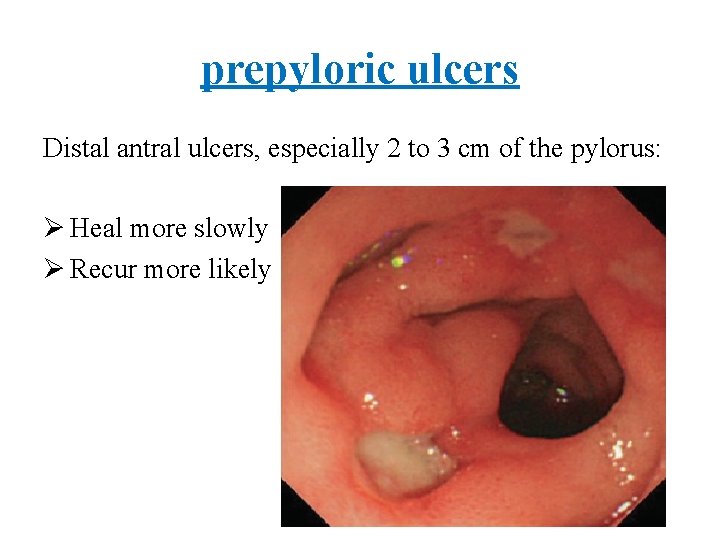
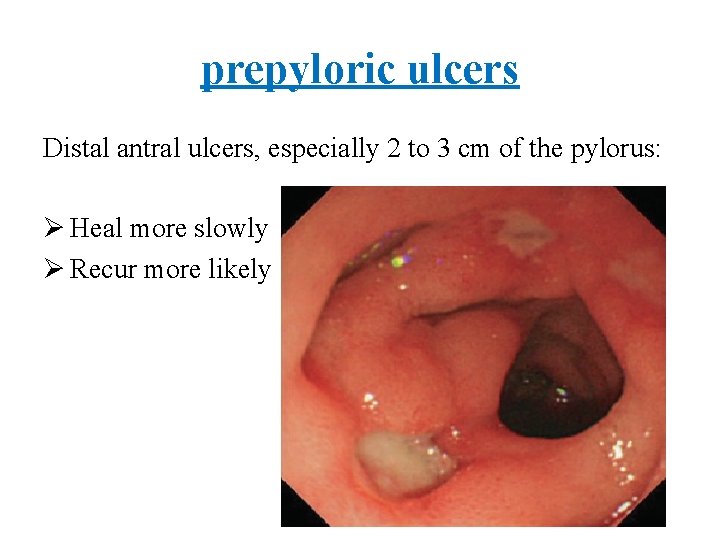
prepyloric ulcers Distal antral ulcers, especially 2 to 3 cm of the pylorus: Ø Heal more slowly Ø Recur more likely
Refractory ulcers q Fail to heal despite 8 to 12 weeks of PPI q Surveillance EGD should be considered until: ØHealing is documented or Ø Etiology is defined (eg, surreptitious NSAID use, high gastrin states, ischemia). q Surgical consultation may be considered for persistent nonhealing PUD.
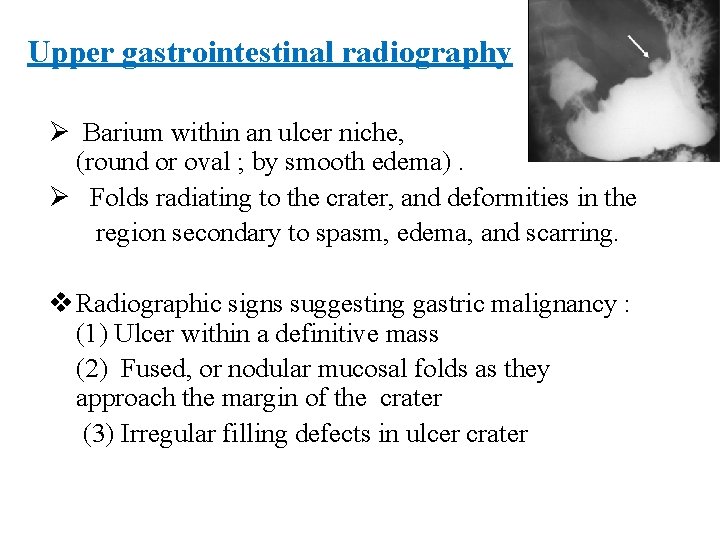
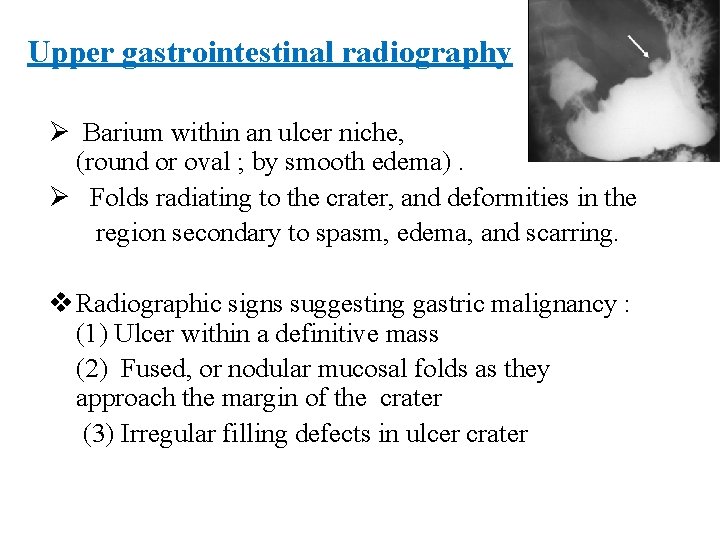
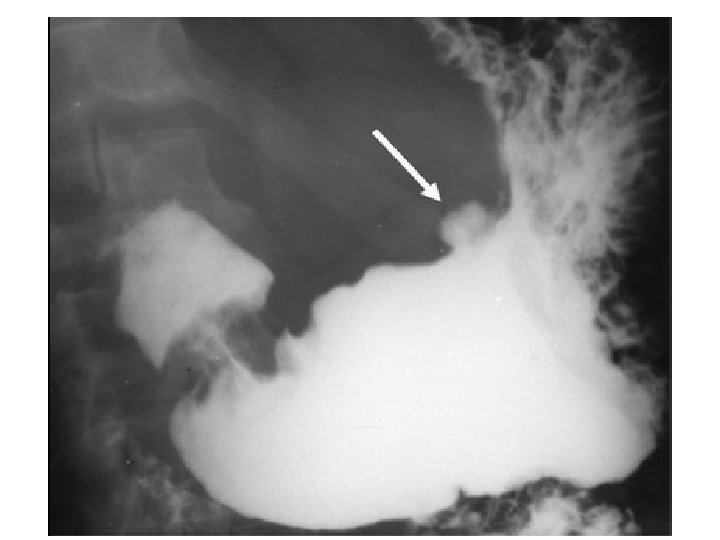
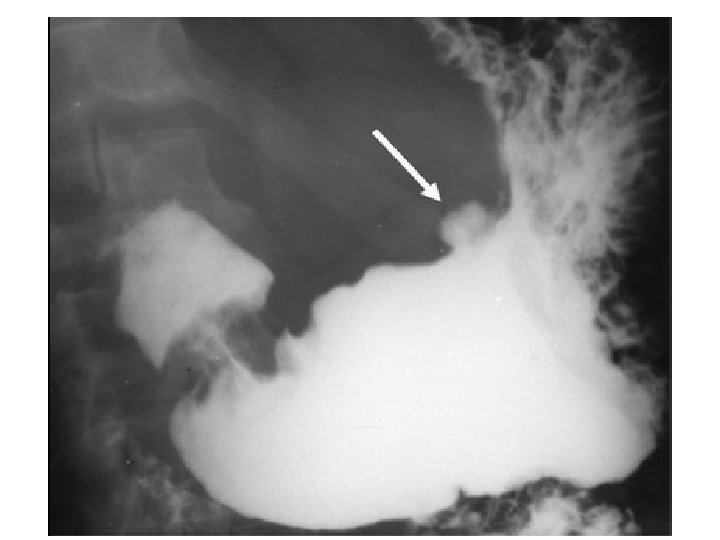
Upper gastrointestinal radiography Ø Barium within an ulcer niche, (round or oval ; by smooth edema). Ø Folds radiating to the crater, and deformities in the region secondary to spasm, edema, and scarring. v Radiographic signs suggesting gastric malignancy : (1) Ulcer within a definitive mass (2) Fused, or nodular mucosal folds as they approach the margin of the crater (3) Irregular filling defects in ulcer crater

CT Scan Spiral and multislice contrast CT is clearly the most valuable test for penetrating or perforated ulcer § § § Free air Fluid collections Inflammatory changes in surrounding soft tissues Extravasation or sinus tracks Localizing the site of perforation or penetration

AGA Guideline on the Management of H. pylori Infection q H. pylori Infection is one of the most common worldwide human infections q Is associated with a number of important upper GI conditions : Ø Chronic gastritis Ø Peptic ulcer disease Ø Gastric malignancy.
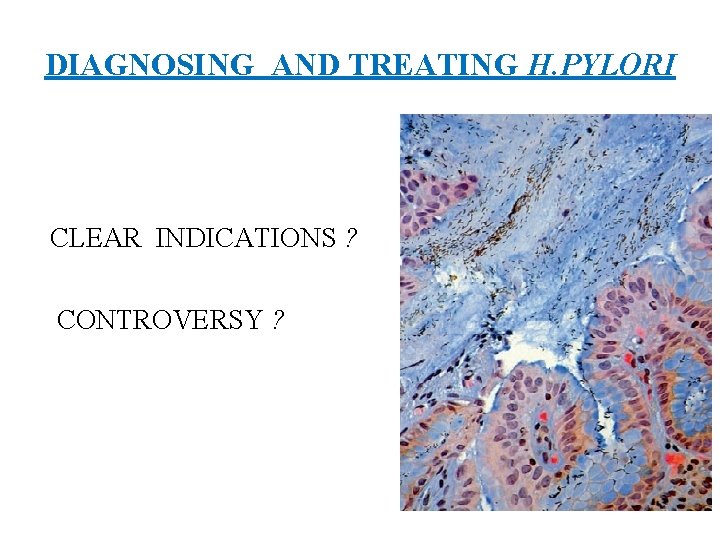
DIAGNOSING AND TREATING H. PYLORI CLEAR INDICATIONS ? CONTROVERSY ?
Clear indication for H. P test-and-treat 1. Active peptic ulcer disease 2. Past history of documented peptic ulcer 3. Gastric MALT lymphoma. 4. Uninvestigated dyspepsia in: § Under the age of 55 yr and no “alarm features”
Contraversy indication for H. P test-and-treat q. Functional dyspepsia § Small but significant clinical benefit from H. pylori eradication. q GERD § H. pylori eradication not worsens nor improves GERD symptoms. § Treatment of H. pylori should not be withheld related to concerns of creating or worsening of GERD

Contraversy indication for H. P test-andtreat q. NSAIDs § Regardless of NSAID, all patients with a PUD should be tested and treated for H. pylori. q. Iron deficiency § Data support an association but do not prove cause and effect.

Contraversy indication for H. P testand-treat q. Gastric adenocarcinoma § Curing H. pylori may prevent progression of metaplasia to gastric adenocarcinoma, there is no definitive population based data
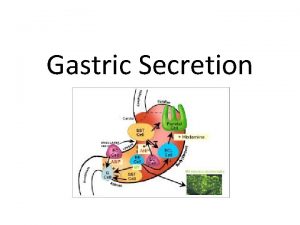
Diagnosting tests for H. pylori q. Endoscopic: 1. Rapid urease test 2. Histology 3. Culture q Non endoscopic: 1. Sreology 2. Urese breath test 3. Fecal antigen test
Rapid urease test (RUT) q Base: PH↑ due to H. pylori urease q Biopsy for RUT should be done from two site q Sensitivity>90% and specificity >95% q Acute ulcer bleeding at the time of testing may decrease the sensitivity
False negative RUT q Unfortunately, most patients referred for EGD are taking PPI or have recently received antibiotics or bismuth. § This cause 20% False negative RUT
What is your plan after a negative RUT? Ø histology of same RUT biopsies Or Ø UBT or FAT at a later date
Histology for H. pylori q Is imperfect gold standard because detection of H. pylori is related to site, number and size of gastric biopsies q Three biopsies must be obtained: 1. One from anglularis 2. One from greater curvature of corpus 3. One from greater curvature of antrum q Sensitivity and specificity >95%
Antibody Tests Ø Is present 21 days after infection and remain long after eradication Ø Only Ig. G is recomended Ø Poor PPV limits usefulness in clinical practice in low prevalence area.
Urea Breath Tests(UBT) q C 13/C 14 labeled urea labeled CO 2 q C 14 UBT is safe. but C 13 test is preferred in children and pregnancy q Sensitivity and specificity exceeding 95% q Accurate in post treatment eradication

Recommendation prior to the UBT 1. DC bismuth and antibiotics for 28 days 2. DC PPI for 7– 14 days 3. DC H 2 RA for 24– 48 hour before the UBT ü Antacids do not affect the accuracy of UBT
Fecal Antigen Test (FAT) q Is approved by the FDA for: Ø H. pylory infection screening Ø Establishing cure following therapy(more than 4 or perhaps 8– 12 wk after treatment) q Sensitivity is reduced by recent use of bismuth antibiotics, and PPI q Specificity is reduced in the setting of GIB
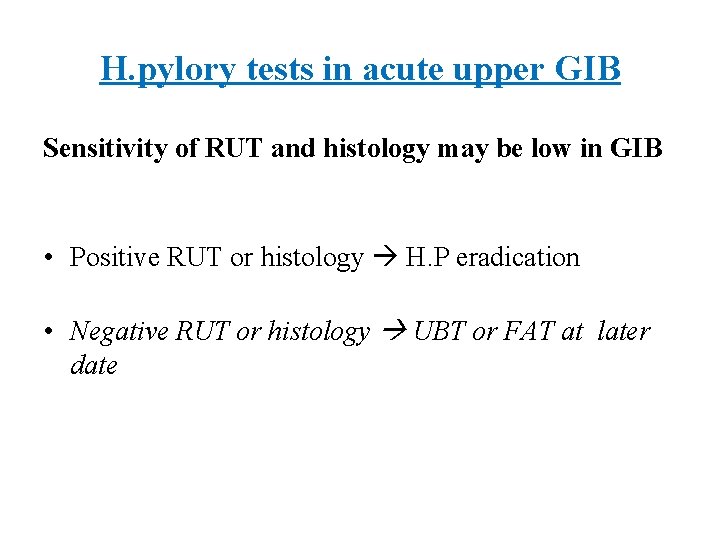
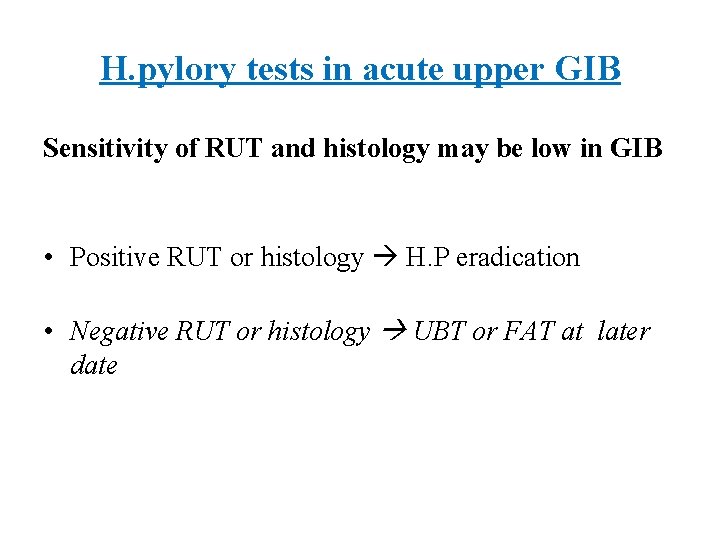
H. pylory tests in acute upper GIB Sensitivity of RUT and histology may be low in GIB • Positive RUT or histology H. P eradication • Negative RUT or histology UBT or FAT at later date
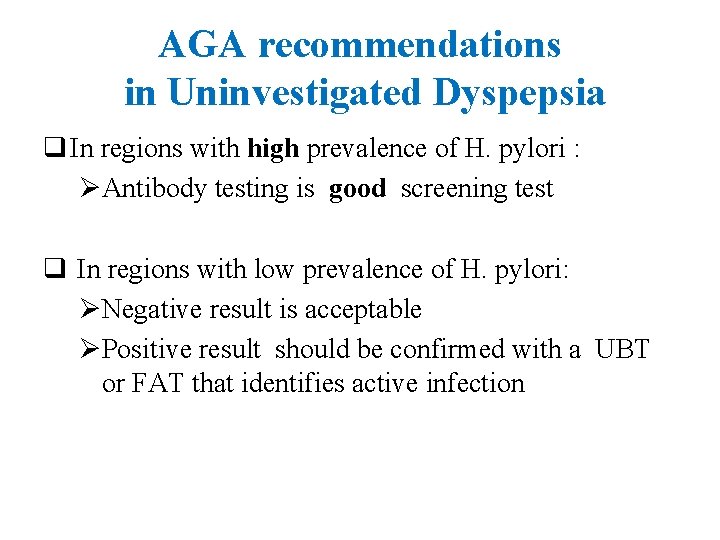
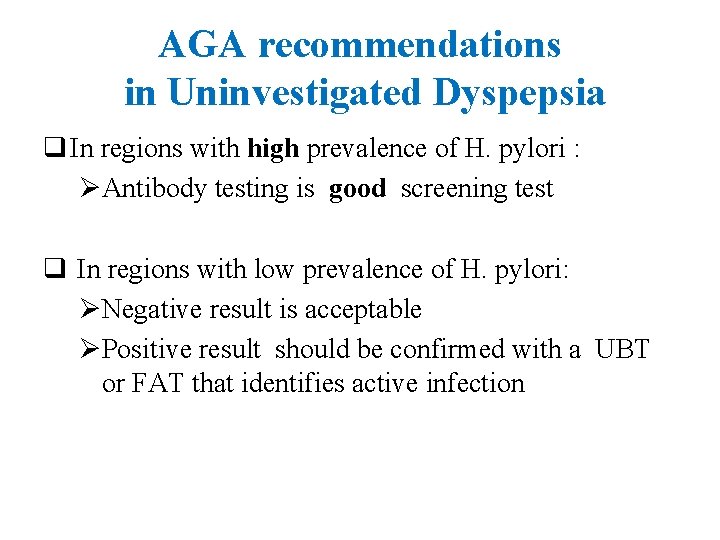
AGA recommendations in Uninvestigated Dyspepsia q In regions with high prevalence of H. pylori : ØAntibody testing is good screening test q In regions with low prevalence of H. pylori: ØNegative result is acceptable ØPositive result should be confirmed with a UBT or FAT that identifies active infection
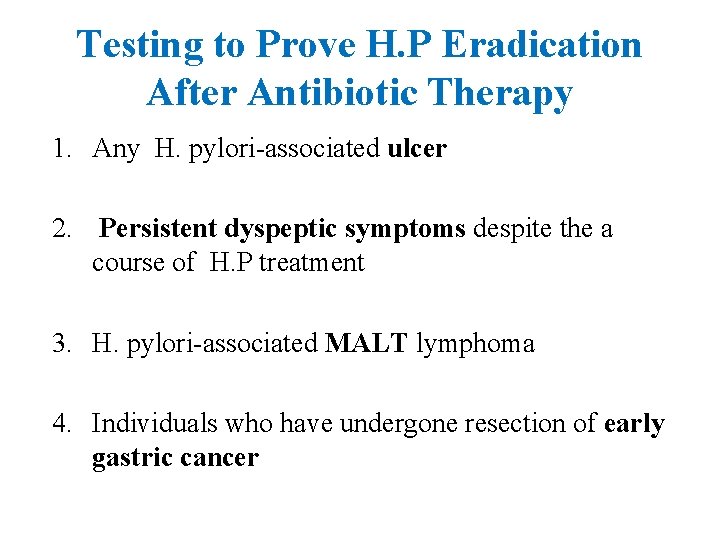
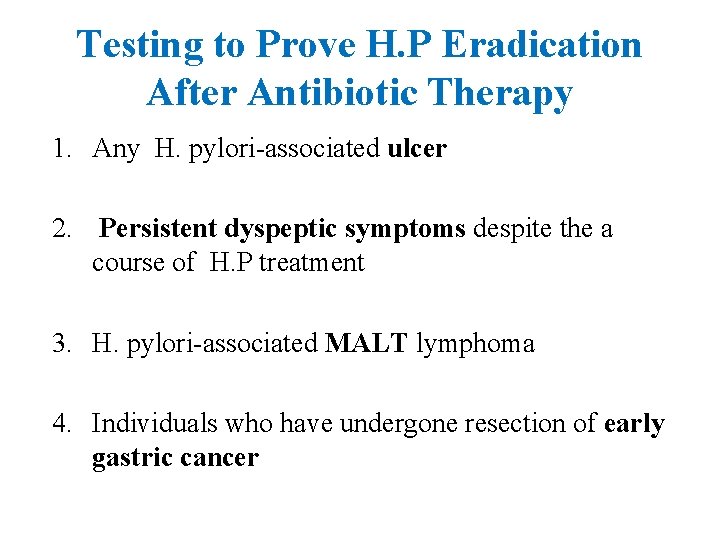
Testing to Prove H. P Eradication After Antibiotic Therapy 1. Any H. pylori-associated ulcer 2. Persistent dyspeptic symptoms despite the a course of H. P treatment 3. H. pylori-associated MALT lymphoma 4. Individuals who have undergone resection of early gastric cancer
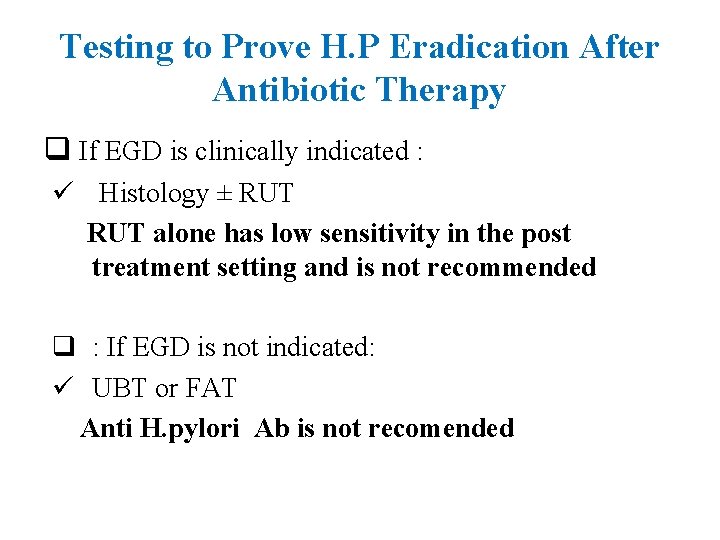
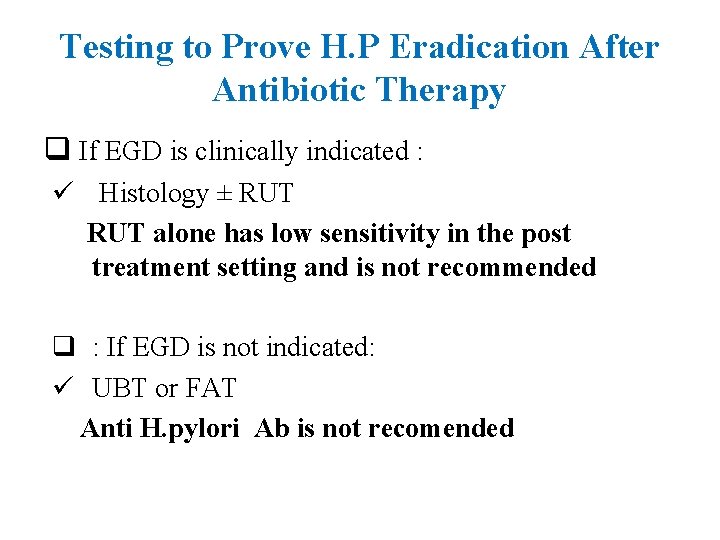
Testing to Prove H. P Eradication After Antibiotic Therapy q If EGD is clinically indicated : ü Histology ± RUT alone has low sensitivity in the post treatment setting and is not recommended q : If EGD is not indicated: ü UBT or FAT Anti H. pylori Ab is not recomended

Empirical H. Pylori eradication in PUD • In region that prevalence of H. pylori in DU is more than 90% H. Pylori eradication can be started without any H. pylori test
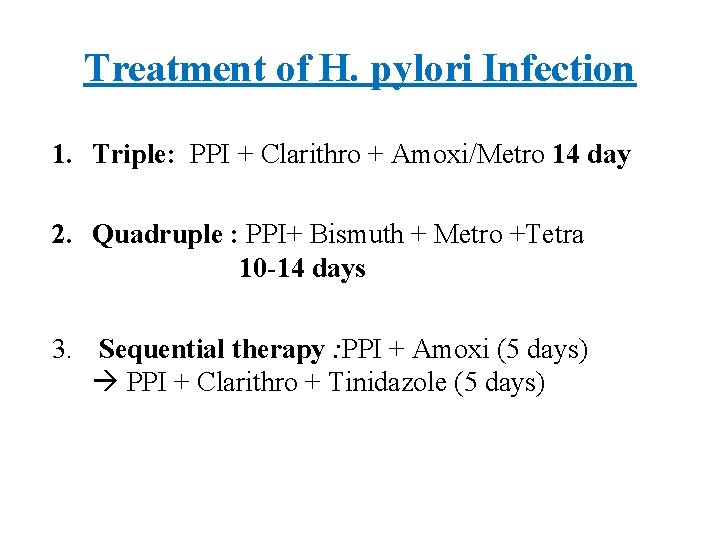
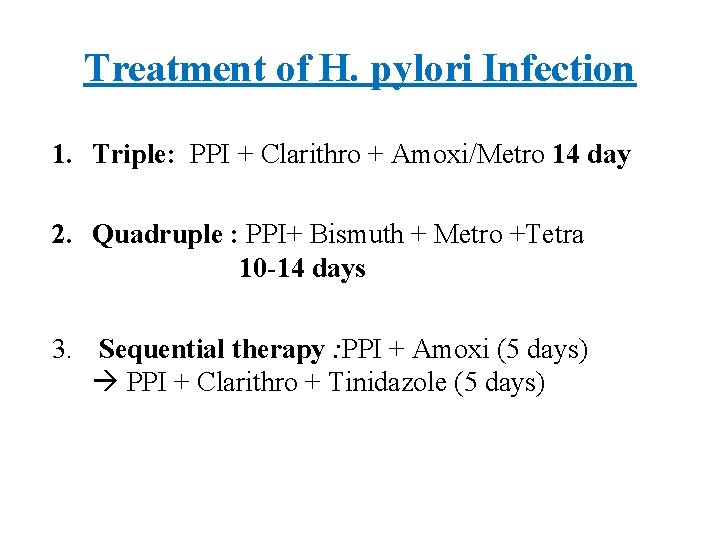
Treatment of H. pylori Infection 1. Triple: PPI + Clarithro + Amoxi/Metro 14 day 2. Quadruple : PPI+ Bismuth + Metro +Tetra 10 -14 days 3. Sequential therapy : PPI + Amoxi (5 days) PPI + Clarithro + Tinidazole (5 days)

Treatment of H. pylori Infection q PPI should be used b. i. d q H 2 RA can be substituted if a patient cannot tolerate PPI
Predictors of H. pylori Treatment Outcome q Most important predictors of failure are 1. Poor compliance 2. Antibiotic resistance. q There is limited evidence to suggest that smoking, alcohol , and diet may reduce successful eradication
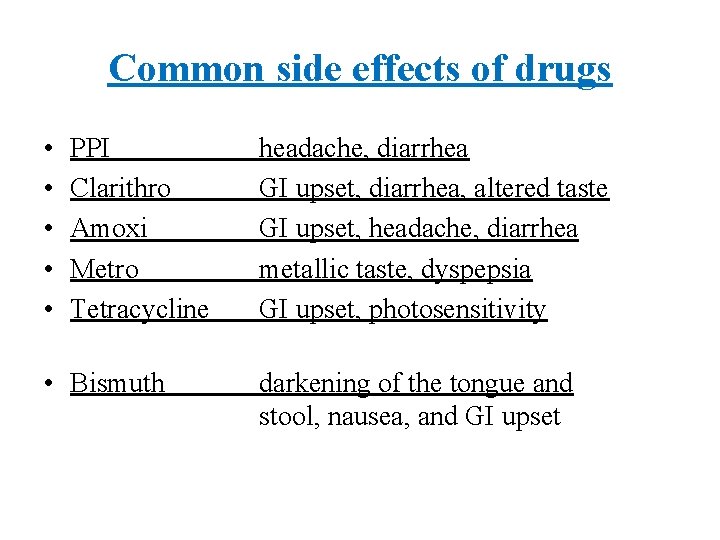
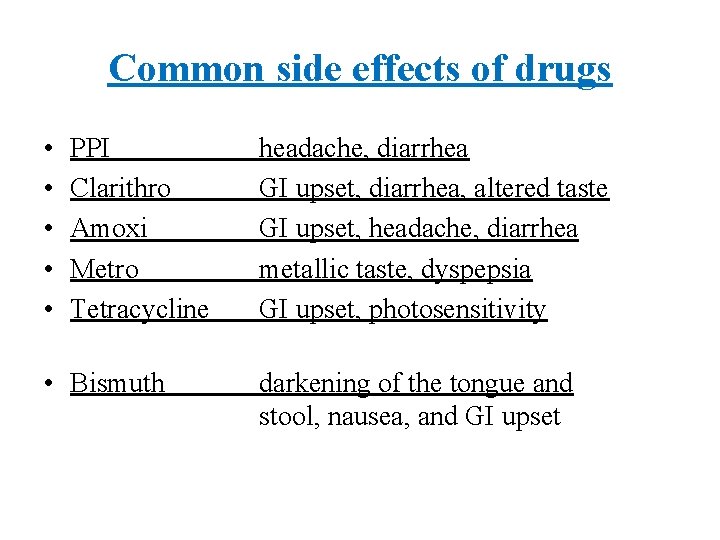
Common side effects of drugs • • • PPI Clarithro Amoxi Metro Tetracycline • Bismuth headache, diarrhea GI upset, diarrhea, altered taste GI upset, headache, diarrhea metallic taste, dyspepsia GI upset, photosensitivity darkening of the tongue and stool, nausea, and GI upset
Antibiotic resistance • • Metronidazole: 37% Clarithromycin: 10% Both antibiotics: 3. 9% Amoxicillin : 1. 4%. ü Metronidazole resistance can be overcome by use of higher doses(500 mg tds)
Antibiotic resistance q Previous treatment with a macrolide or metronidazole for any reason significantly increase resistance q In patients with persistent H. pylori ; avoidance from previously used antibiotics is recomended
culture and antibiotic sensitivity q Are typically not performed unless a patient has failed at least 2 courses of therapy. q Even in this circumstance, the usefulness of such testing is arguable.

Recommendations in persistent infection q If patient has not been previously treated with clarithro, triple therapy can be done q Levofloxacin-based triple therapy for 10 days is another option (Levofloxacin 500 mg daily+ Amoxi 1 gr BD+PPI) q Other antibiotic used include Rifabutin and Furazolidone.
Maintenance antisecretory therapy q. Is recommended in : ØHigh-risk patient who fail H. pylori eradication Ø H. pylori-negative ulcers With: • PPI or • Cimetidine 400 mg / Ranitidine 150 mg Famotidine 20 mg / Nizatidine 150 mg at bedtime

Maintenance antisecretory therapy q. Uncomplicated recurrent disease; stopping therapy after two years q Complicated disease; five-year may be more appropriate
Maintenance antisecretory therapy q Rebound acid-hypersecretion is important following abrupt cessation of PPI ü stepping-down to low dose PPI and then to full dose H 2 RA is an appropriate caution

H. pylori negative ulcers Ø Special attention to ensure that H. pylori infection and NSAID has been excluded Ø In confirmed non-H. pylori, non-NSAID ulcers; excluding acid hypersecretory states, such as ZES (fasting serum Gastrin )

H. pylori test&treat in NSAID user Ø Before starting NSAIDs or aspirin (even at low dose), consider testing for H. pylori Ø In NSAID users with ulcer complications and evidence of H. pylori , curing H. pylori does not reduce high risk of ulcer complications if NSAIDs are continued.
 Gastric ulcer
Gastric ulcer Objectives of peptic ulcer
Objectives of peptic ulcer Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Peptic ulcer disease
Peptic ulcer disease Peptic ulcer disease
Peptic ulcer disease Ajeerna symptoms
Ajeerna symptoms Pud
Pud Stomach ulcer
Stomach ulcer Modified johnson classification
Modified johnson classification Pathophysiology of peptic ulcer
Pathophysiology of peptic ulcer Mondor triad
Mondor triad Peptic ulcer case study
Peptic ulcer case study Peptic ulcer diseas
Peptic ulcer diseas Acholorhydria
Acholorhydria Mucosal atomizer device (mad)
Mucosal atomizer device (mad) Stomach mucosal barrier
Stomach mucosal barrier Tea pot deformity of stomach
Tea pot deformity of stomach Typhoid ulcer gross
Typhoid ulcer gross Types of gastric ulcer
Types of gastric ulcer Duodenal ulcer vs gastric ulcer
Duodenal ulcer vs gastric ulcer What is stablizing selection
What is stablizing selection Pengertian digital disruption
Pengertian digital disruption Big bang disruption examples
Big bang disruption examples From long disruption remained
From long disruption remained Millennial disruption index
Millennial disruption index Orointegratedcoop.com
Orointegratedcoop.com Accelerated disruption
Accelerated disruption Mis supply chain management
Mis supply chain management Communicable disease and non communicable disease
Communicable disease and non communicable disease Peptic cells secrete
Peptic cells secrete Induration of ulcer
Induration of ulcer Cryopathic ulcer meaning
Cryopathic ulcer meaning Periradicular tissue definition
Periradicular tissue definition Bulky disease definition
Bulky disease definition Hyprcapnia
Hyprcapnia Alzheimer disease definition
Alzheimer disease definition Pid discharge pictures
Pid discharge pictures Parkinson's disease definition
Parkinson's disease definition Mooren ulcer
Mooren ulcer Kennedy terminal ulcer presentation
Kennedy terminal ulcer presentation Sskin bundle hse
Sskin bundle hse Ulcer stool
Ulcer stool Haemtemesis
Haemtemesis Ischial pressure ulcer location
Ischial pressure ulcer location Ulcer bulbar definitie
Ulcer bulbar definitie Carmans meniscus sign
Carmans meniscus sign Thrombus fate
Thrombus fate Dulalax
Dulalax Mooren ulcer
Mooren ulcer Biopsy test
Biopsy test Dibetic shoes
Dibetic shoes Shelving edge ulcer
Shelving edge ulcer Corneal infiltration
Corneal infiltration Circumcorneal flush
Circumcorneal flush Iuliana ionascu cabinet veterinar
Iuliana ionascu cabinet veterinar Stress ulcer prophylaxis criteria
Stress ulcer prophylaxis criteria Stress ulcer prophylaxis criteria
Stress ulcer prophylaxis criteria Pressure ulcer safety cross template
Pressure ulcer safety cross template Pressure ulcer pico question
Pressure ulcer pico question Faecoloma
Faecoloma Hamptons line
Hamptons line Nasal cannula pressure ulcer prevention
Nasal cannula pressure ulcer prevention Voriconazole powder for eye drops
Voriconazole powder for eye drops Oral ulcer
Oral ulcer Parts of ulcer
Parts of ulcer Pressure ulcer query template
Pressure ulcer query template Oral ulcer
Oral ulcer Ulcer
Ulcer Category 4 pressure ulcer
Category 4 pressure ulcer Theme of 1984
Theme of 1984 Dentritic ulcer
Dentritic ulcer Mast cell stabilizer
Mast cell stabilizer Fibrin cuff theory
Fibrin cuff theory Amebiasis
Amebiasis 2232021
2232021 Ulcer
Ulcer Dendritic keratitis
Dendritic keratitis Duodenum ileum
Duodenum ileum Air pressure clipart
Air pressure clipart Depuap
Depuap