PEMPHIGOID Jun Flores 130 Alina Tiraspolskaya 183 Joshua






- Slides: 21

PEMPHIGOID Jun Flores #130 Alina Tiraspolskaya #183 Joshua Cardwell #108 Jared Martin #147
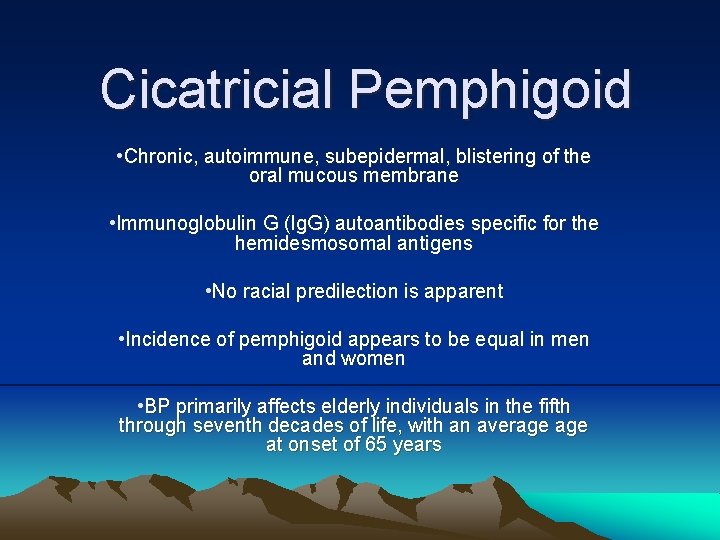
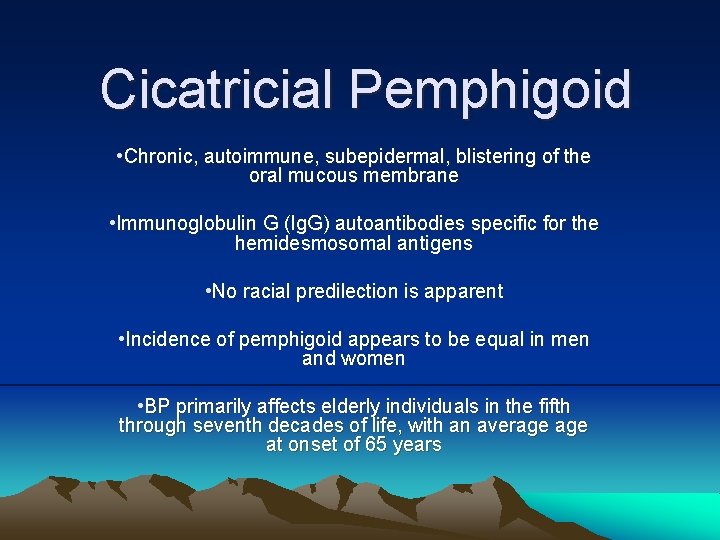
Cicatricial Pemphigoid • Chronic, autoimmune, subepidermal, blistering of the oral mucous membrane • Immunoglobulin G (Ig. G) autoantibodies specific for the hemidesmosomal antigens • No racial predilection is apparent • Incidence of pemphigoid appears to be equal in men and women • BP primarily affects elderly individuals in the fifth through seventh decades of life, with an average at onset of 65 years
Pathophysiology • Ig. G autoantibodies bind to the basement membrane • complement and inflammatory mediators • inflammatory cells to the basement membrane • release proteases • degrade hemidesmosomal proteins blister formation
Causes/Relevant factors: • Immunogenetics – Increased of specific HLA presentation of the target antigen by antigen-presenting cells in the initial development of the autoimmune response • Age – Intrinsic changes in the immune system with aging are factors in the initiation of an autoimmune response • Epitope spreading – Reports of bullous pemphigoid arising in patients with inflammatory skin diseases (psoriasis, lichen planus), or post- trauma (drug reactions) inflammation exposes sequestered skin basement membrane proteins and antigens leading to the development of an autoimmune response • Complement activation – Autoantibodies bind hemidesmosome/upper lamina lucida area of the skin basement membrane complement activation inflammatory cells release enzymes blister formation. • Chemokines – The histologic hallmark for bullous pemphigoid is the prominent eosinophil infiltration at the skin basement membrane area likely induced by chemokines

Pathogenesis (con’t) • Involves the mucosa in 10 -25% of patients • Limited oral intake secondary to dysphagia • Erosions secondary to rupture of the blisters, pain, functional limitations (palms, soles) • Bullous pemphigoid can be fatal in debilitated patients, mostly due to sepsis and adverse effects to treatment • Patients on high dose corticosteroids – increased risk for PUD, GI bleed, agranulocytosis, diabetes
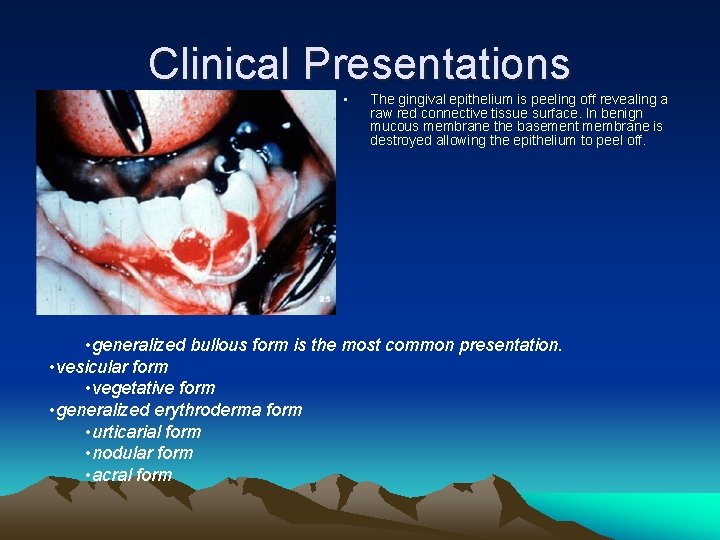
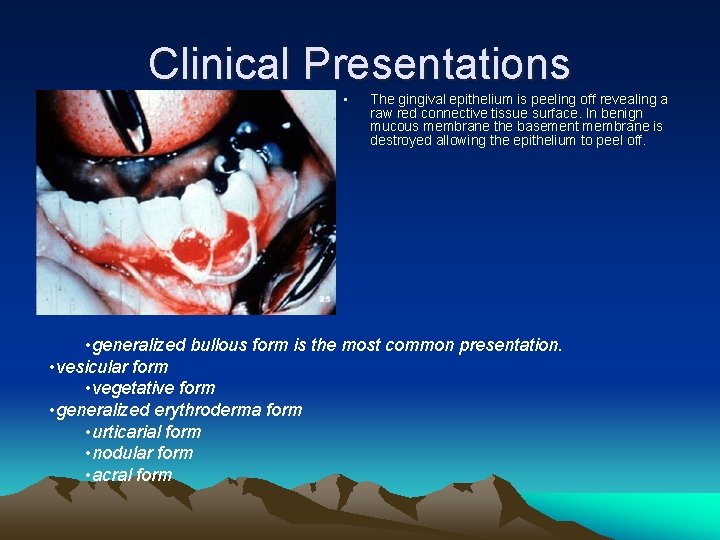
Clinical Presentations • The gingival epithelium is peeling off revealing a raw red connective tissue surface. In benign mucous membrane the basement membrane is destroyed allowing the epithelium to peel off. • generalized bullous form is the most common presentation. • vesicular form • vegetative form • generalized erythroderma form • urticarial form • nodular form • acral form
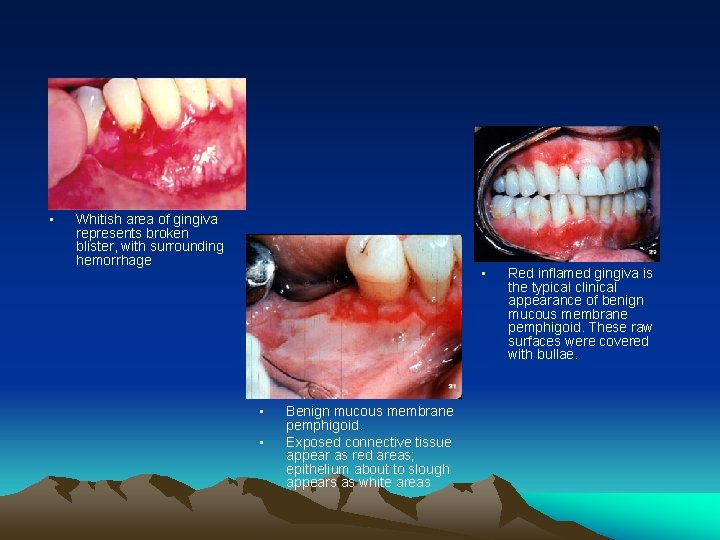
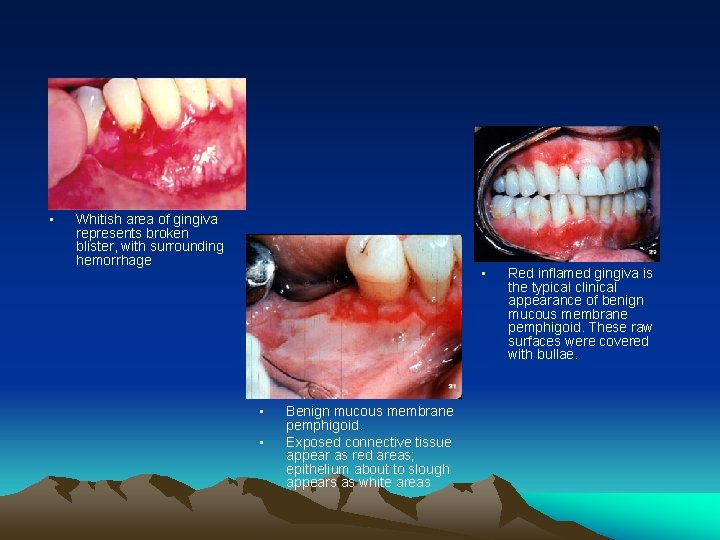
• Whitish area of gingiva represents broken blister, with surrounding hemorrhage • • • Benign mucous membrane pemphigoid. Exposed connective tissue appear as red areas; epithelium about to slough appears as white areas Red inflamed gingiva is the typical clinical appearance of benign mucous membrane pemphigoid. These raw surfaces were covered with bullae.

• Conjunctival involvement can be severe, resulting in loss of hair, of the lid itself, bulbar conjunctivitis and scar formation • • Ulcer bed of huge buccal mucosa bulla Bullae on external skin surfaces
Diagnostic Tests Positive Nikolsky Sign • With a blunt instrument (back of a mouth mirror), the investigator firmly places and pushes against the mucous membrane and twists. A positive Nikolsky sign presents as blister formation within a matter of minutes – Note: many other vesicular/bullous diseases have a positive nikolsky sign
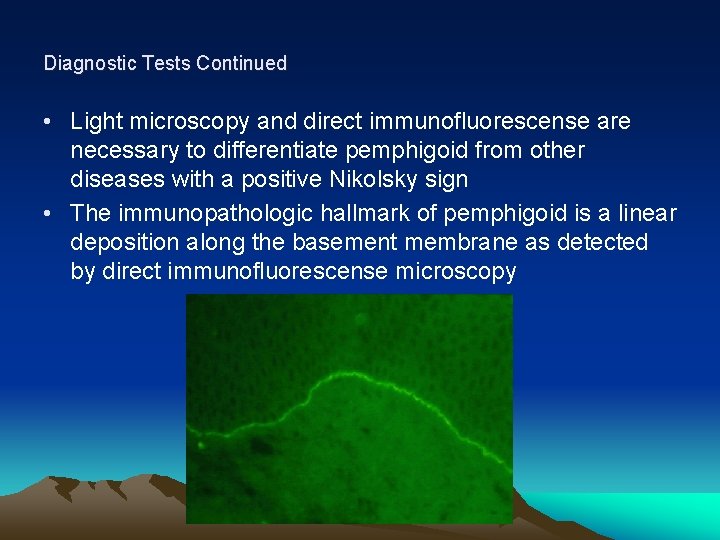
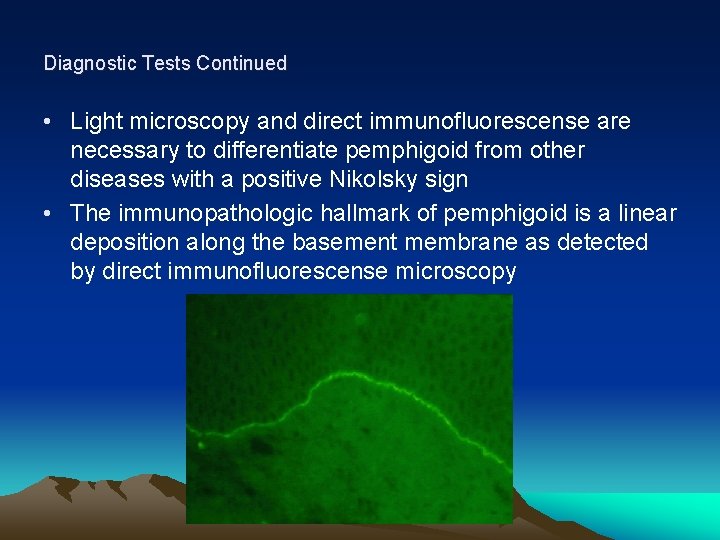
Diagnostic Tests Continued • Light microscopy and direct immunofluorescense are necessary to differentiate pemphigoid from other diseases with a positive Nikolsky sign • The immunopathologic hallmark of pemphigoid is a linear deposition along the basement membrane as detected by direct immunofluorescense microscopy
Histopathology • A separation of the epithelial and connective tissue layer at the level of the basement membrane • Immunofluorescence reveals a linear striation of Ig. G and C 3 at the level of the basement membrane (Chan and Cooper, 1994)
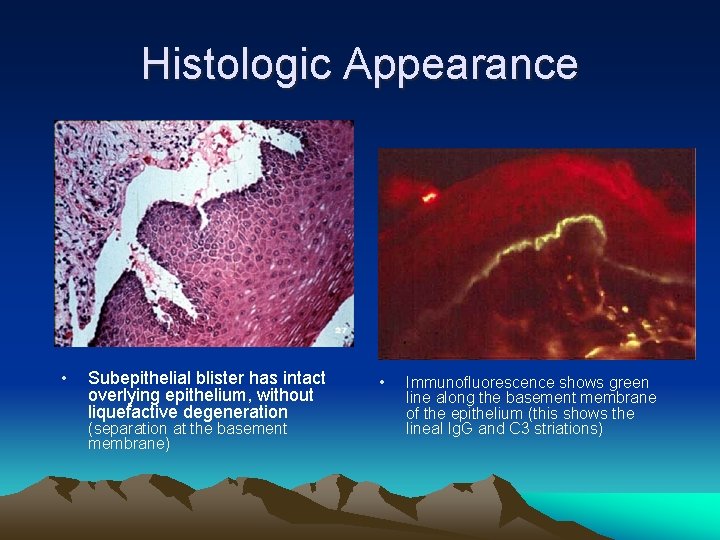
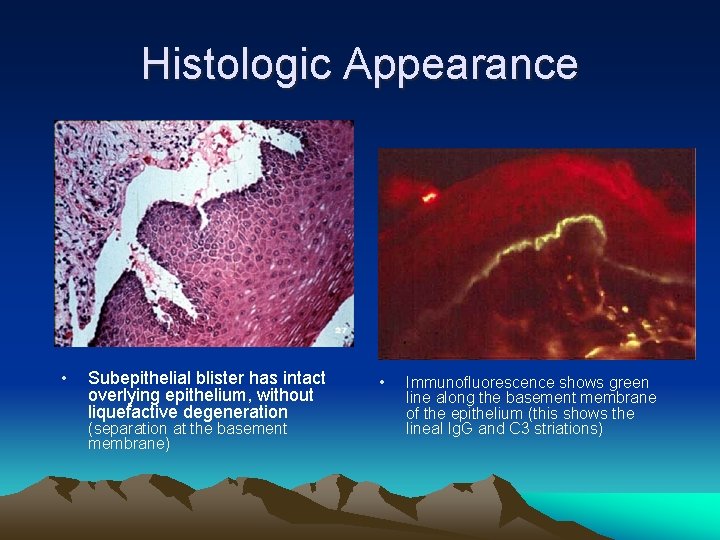
Histologic Appearance • Subepithelial blister has intact overlying epithelium, without liquefactive degeneration (separation at the basement membrane) • Immunofluorescence shows green line along the basement membrane of the epithelium (this shows the lineal Ig. G and C 3 striations)
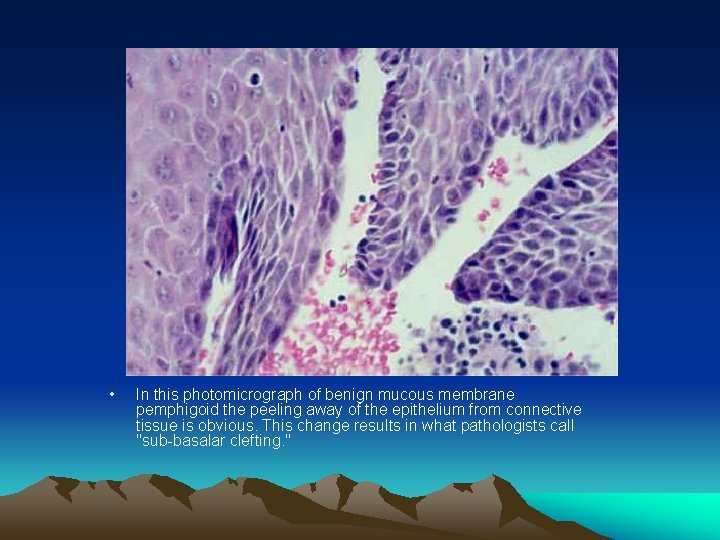
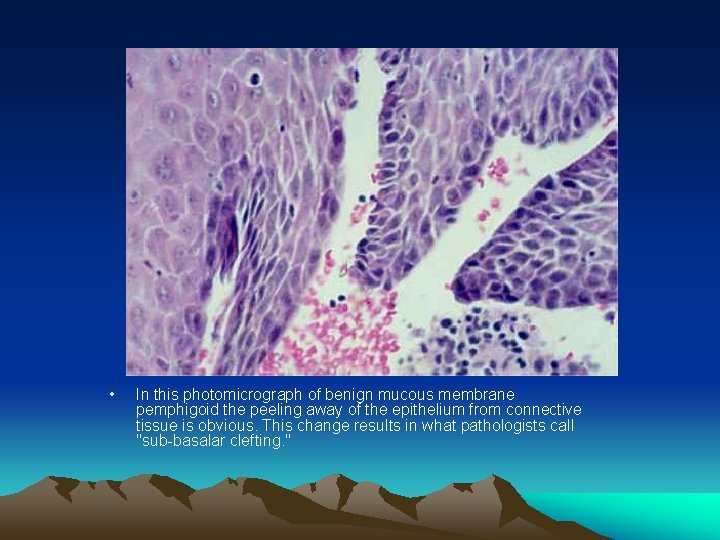
• In this photomicrograph of benign mucous membrane pemphigoid the peeling away of the epithelium from connective tissue is obvious. This change results in what pathologists call "sub-basalar clefting. "
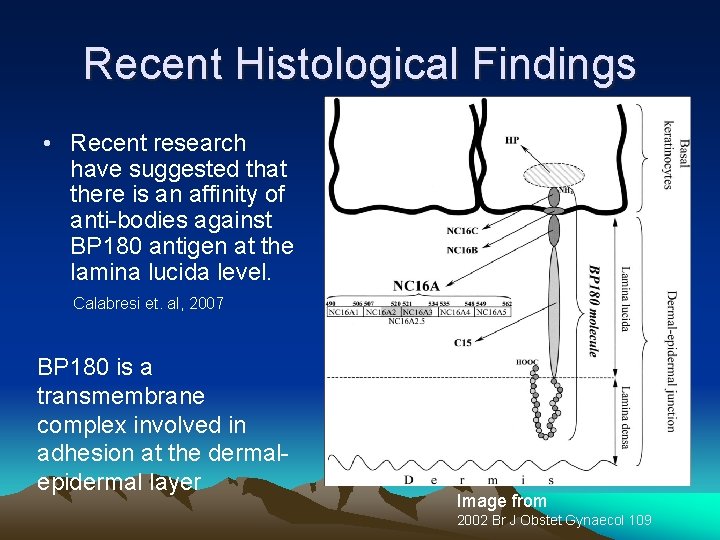
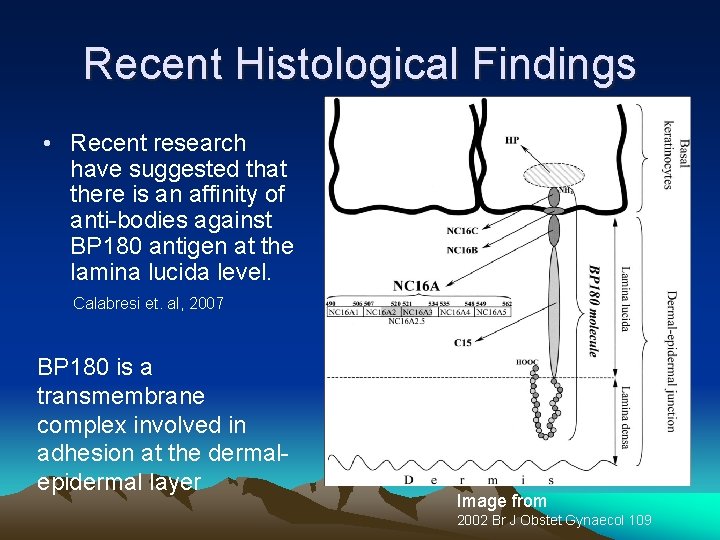
Recent Histological Findings • Recent research have suggested that there is an affinity of anti-bodies against BP 180 antigen at the lamina lucida level. Calabresi et. al, 2007 BP 180 is a transmembrane complex involved in adhesion at the dermalepidermal layer Image from 2002 Br J Obstet Gynaecol 109

Treatment Goal – decrease blister formation - promote healing of blisters and erosions - reduce inflammatory response and autoantibody production

Treatment (con’t) Medications -Anti-inflammatory agents – inhibit specific cytokine production and vascular permeability -Prednisone (1 mg/kg/d) -Tetracycline (500 mg qid) -Clobetasol – topical steroid (bid for up to 2 wk)
Treatment (con’t) -A recent article from Europe provided evidence that strong topical corticosteriods can achieve disease control while avoiding systemic adverse effects from systemic corticosteroids -Immunosuppressive agents – if antiinflammatory agents cause no response -Azathioprine (1 mg/kg/d bid, increase by 0. 5 mg/kg q 4 wk until response, do not exceed 2. 5 mg/kg/d)
Treatment (con’t) -For patients treated with systemic corticosteroid for longer than 1 month, a combined supplement of calcium and vitamin D should be instituted to prevent osteoporosis. -In addition to calcium and vitamin D supplementation, patients on long-term treatment with systemic corticosteroids should be taking bisphonate, a specific inhibitor for osteoclast-mediated bone resorption (eg, alendronate).

Before The remaining images are of the same patient. • Here the mucous membrane inside the lower lip shows the red and white desquamative areas so typical of benign mucous membrane pemphigoid. • After Within a week after starting systemic corticosteroid therapy, the patient showed significant improvement. Here the lesion on lip mucosa have resolved completely. • • In the same patient, the raw and sloughing process has affected the buccal mucosa. The improvement in the buccal mucous lesion after corticosteroid therapy is remarkable.
References • • Calabresi V, Carrozzo M, Cozzani E, Arduino P, Bertolusso G, Tirone F, Parodi A, Zambruno G, Di Zenzo G. Oral pemphigoid autoantibodies preferentially target BP 180 ectodomain. Clin Immunol. 2007 Feb; 122(2): 207 -13. Epub 2006 Dec 1. Chan LS, Cooper. A novel immune-mediated subepidermal bullous dermatosis characterized by Ig. G autoantibodies to a lower lamina lucida component. Arch Dermatol. 1994 Mar; 130(3): 343 -7. Chan LS, Yancey KB, Hammerberg C. Immune-mediated subepithelial blistering diseases of mucous membranes. Arch Dermatol. 1993 Apr; 129(4): 448 -55. Sapp, J. P. , Eversole, L. R. , Wysocki, G. P. Contemproary Oral and Maxillofacial Pathology. Mosby 2004, p. 262 -265.
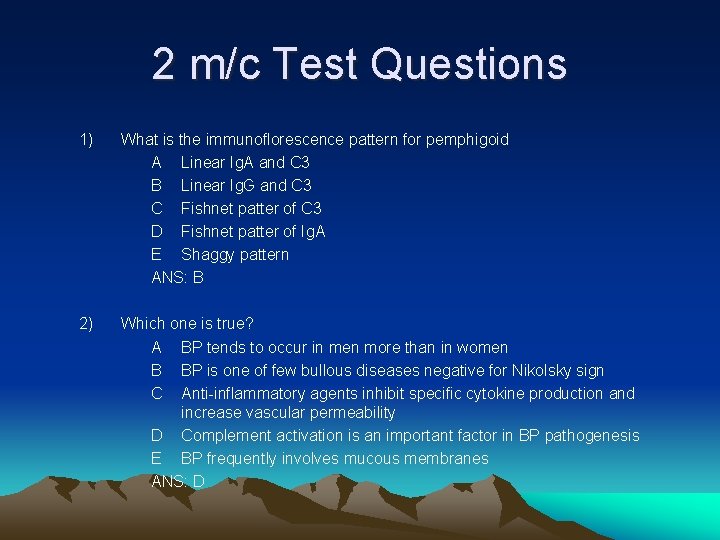
2 m/c Test Questions 1) What is the immunoflorescence pattern for pemphigoid A Linear Ig. A and C 3 B Linear Ig. G and C 3 C Fishnet patter of C 3 D Fishnet patter of Ig. A E Shaggy pattern ANS: B 2) Which one is true? A BP tends to occur in men more than in women B BP is one of few bullous diseases negative for Nikolsky sign C Anti-inflammatory agents inhibit specific cytokine production and increase vascular permeability D Complement activation is an important factor in BP pathogenesis E BP frequently involves mucous membranes ANS: D
 Dr alina tiraspolskaya
Dr alina tiraspolskaya Dr alina tiraspolskaya
Dr alina tiraspolskaya Alina
Alina Dr alina tiraspolskaya
Dr alina tiraspolskaya Jun flores
Jun flores Kristine krafts
Kristine krafts Pemphigus vulgaris vs bullous pemphigoid
Pemphigus vulgaris vs bullous pemphigoid Beng 183
Beng 183 Gül kerman
Gül kerman Ki kd al qur'an hadits ma kma 183
Ki kd al qur'an hadits ma kma 183 Eecs 183 lab 8
Eecs 183 lab 8 Eecs 183
Eecs 183 Where is the bermuda located
Where is the bermuda located Eecs 183
Eecs 183 Eecs 183
Eecs 183 Convenio 183
Convenio 183 Convenção 183 oit
Convenção 183 oit Cs183b stanford
Cs183b stanford Pkj 183
Pkj 183 School revision 101
School revision 101 Jun akizaki
Jun akizaki Slide to doc.com
Slide to doc.com