PELVIC FLOOR AND FUNCTIONAL ANATOMY Assoc Prof Gazi

- Slides: 76
PELVIC FLOOR AND FUNCTIONAL ANATOMY Assoc. Prof. Gazi YILDIRIM, M. D. Yeditepe University, Medical Faculty Dept of Ob&Gyn
Objectives • To define – Pelvic organ prolapsus • To learn – Risk factors for Pelvic organ prolapsus – Diagnosis of the prolapsus • To manage – A woman who has pelvic organ prolapsus
Functions of Pelvic Floor 1. Supportive function Pelvic viscera 2. Sphincteric function Vagina, Urethra, Rectum 3. Sexual function Proprioseptive sensation
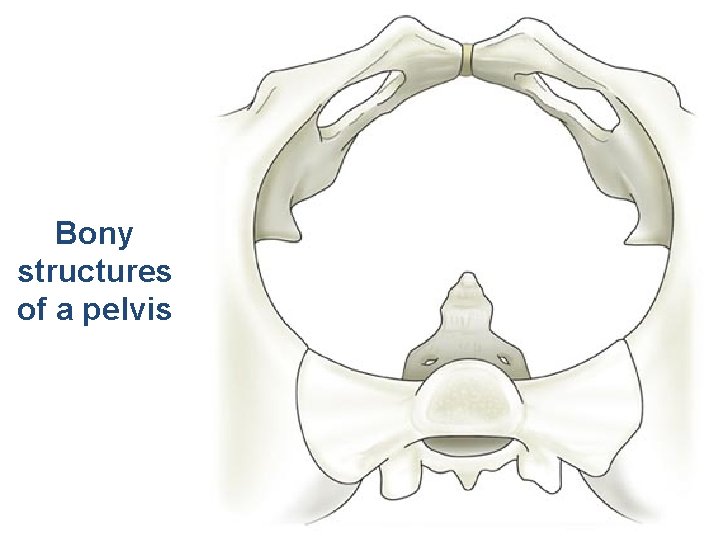
Elements comprising the Pelvis • Bones – Ilium, ischium and pubis fusion • Ligaments • Muscles – Obturator internis muscle – Arcus tendineus levator ani or white line – Levator ani muscles – Urethral and anal sphincter muscles
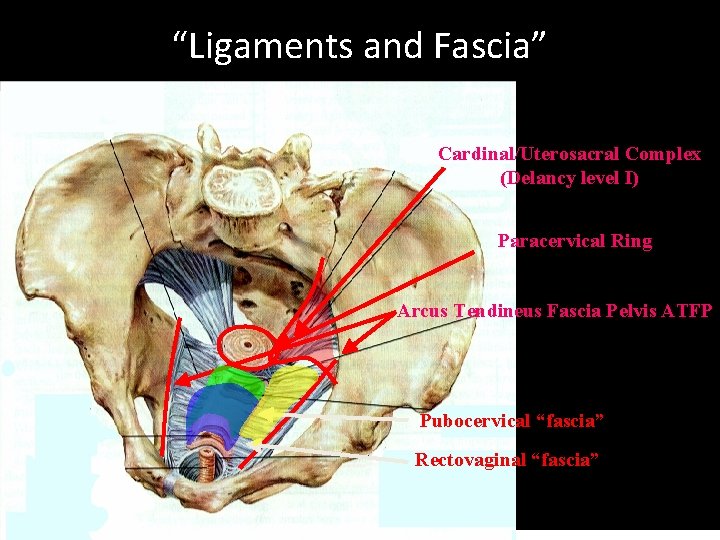
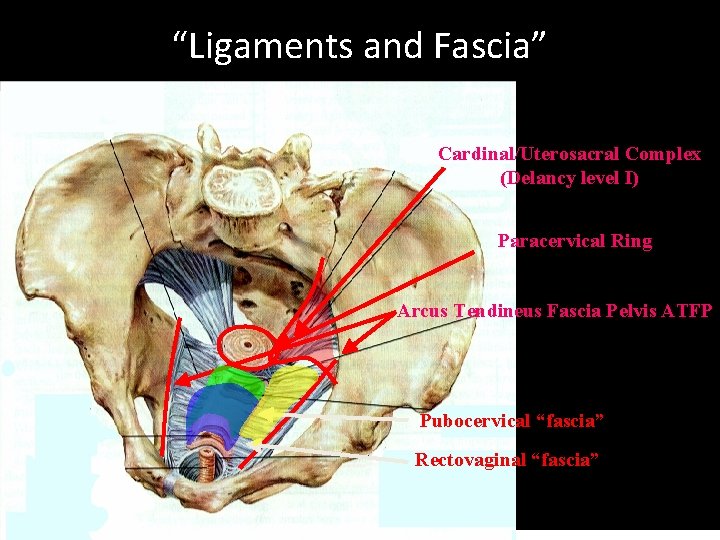
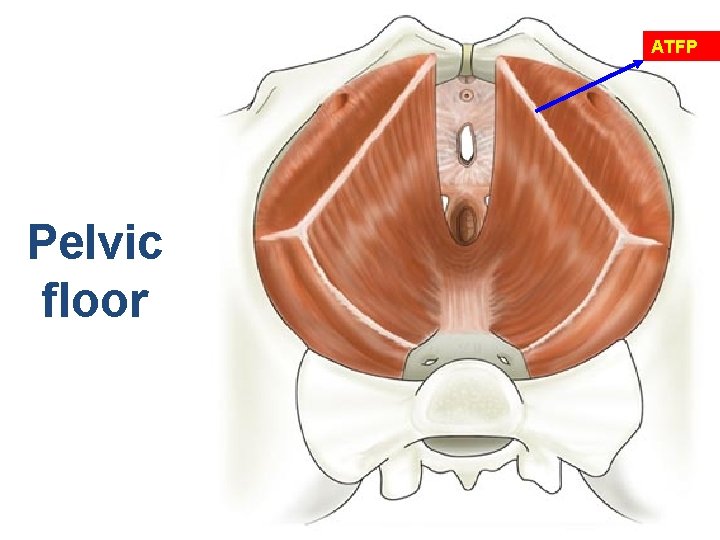
“Ligaments and Fascia” Cardinal/Uterosacral Complex (Delancy level I) Paracervical Ring Arcus Tendineus Fascia Pelvis ATFP Pubocervical “fascia” Rectovaginal “fascia”
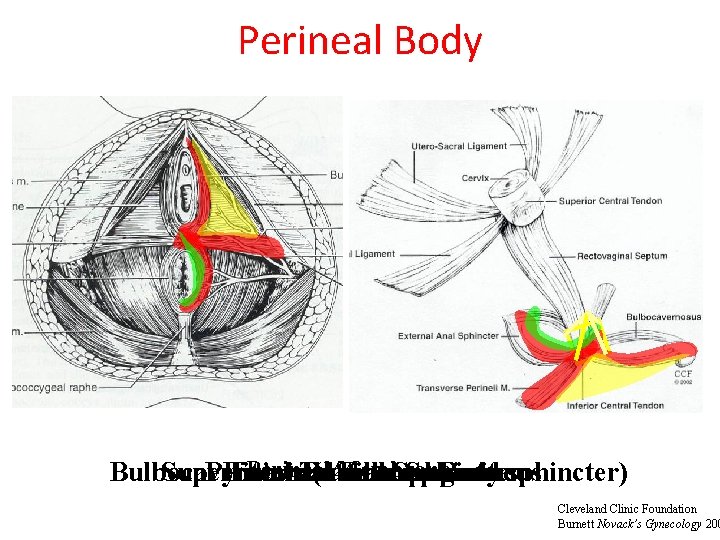
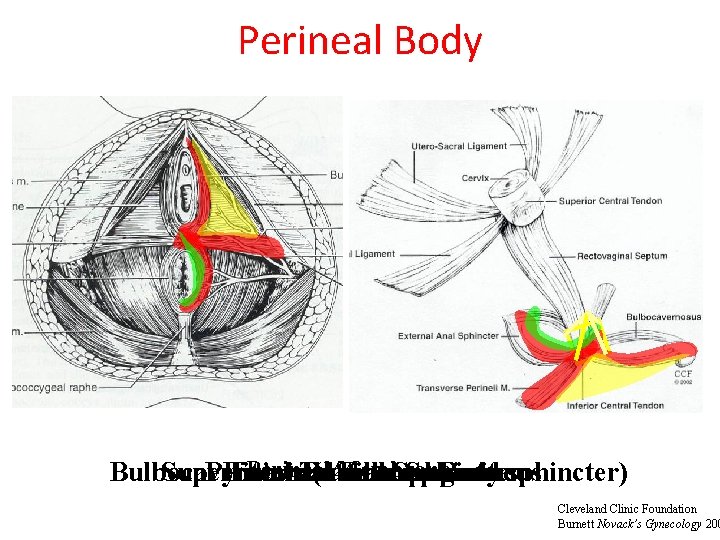
Perineal Body Perineal Membrane Superficial Pyramidal Internal External Transverse Anal Fibrous Anal. Sphincter Body perineus Bulbocavernosis (urethrovaginal sphincter) Cleveland Clinic Foundation Burnett Novack’s Gynecology 200
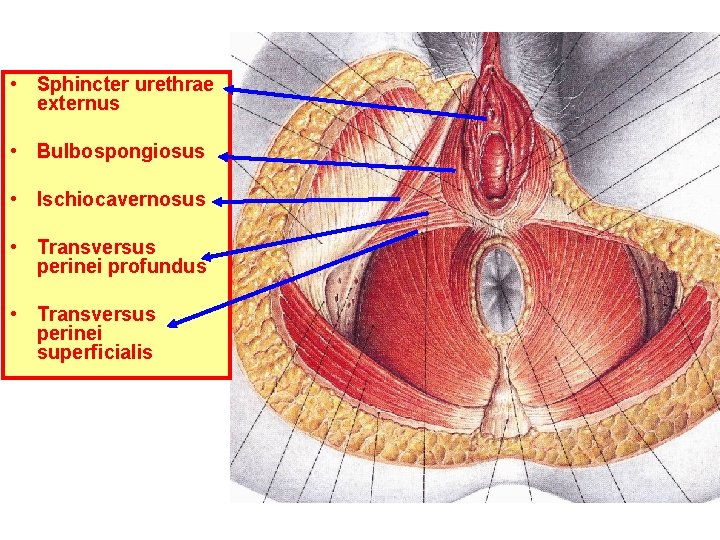
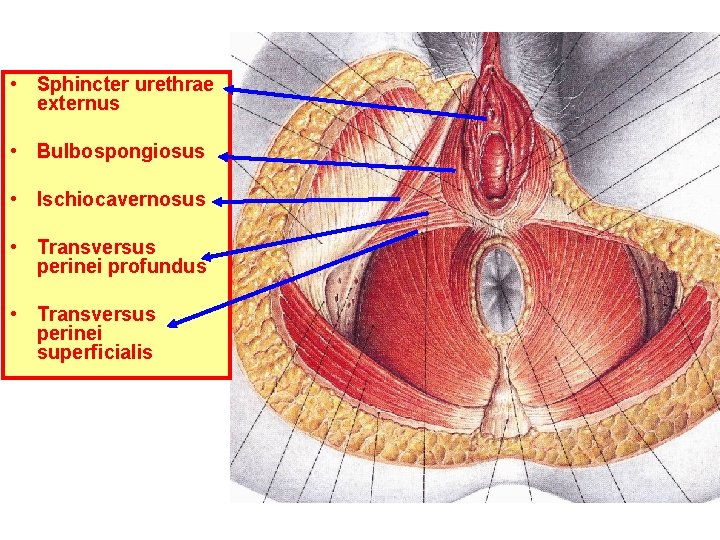
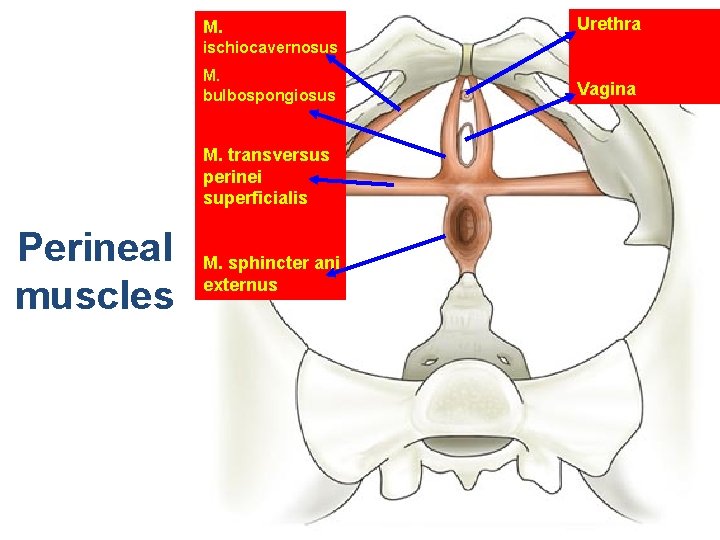
• Sphincter urethrae externus • Bulbospongiosus • Ischiocavernosus • Transversus perinei profundus • Transversus perinei superficialis
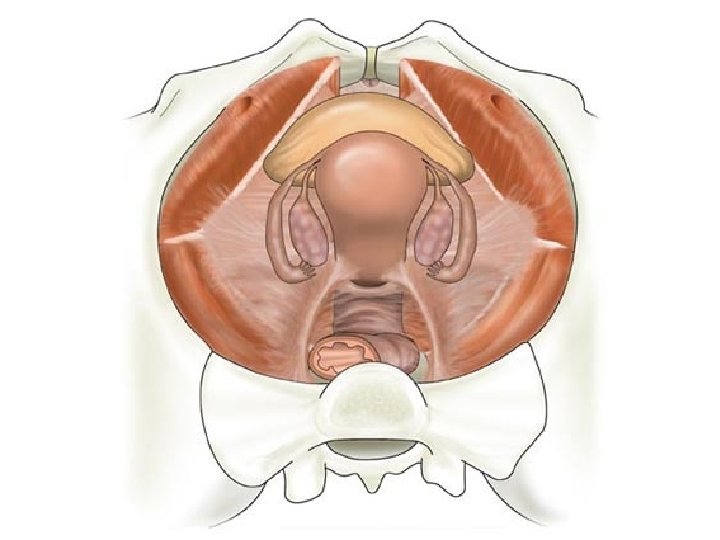
Lets ‘create’ a woman pelvis…
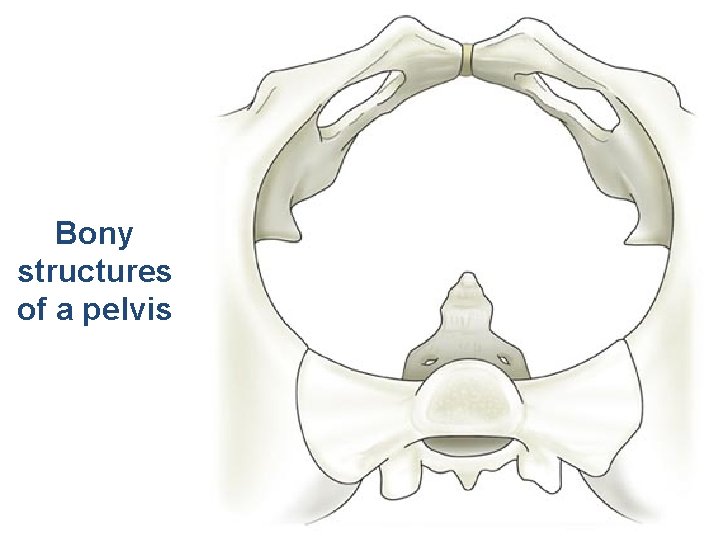
Bony structures of a pelvis
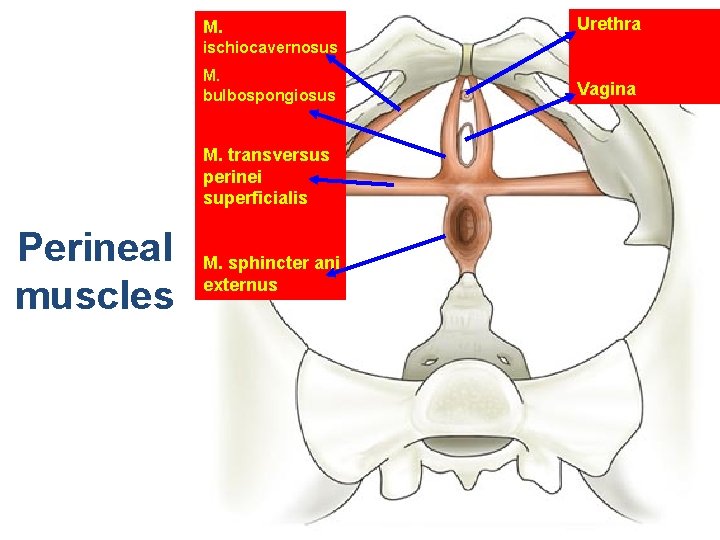
M. Urethra ischiocavernosus M. bulbospongiosus M. transversus perinei superficialis Perineal muscles M. sphincter ani externus Vagina
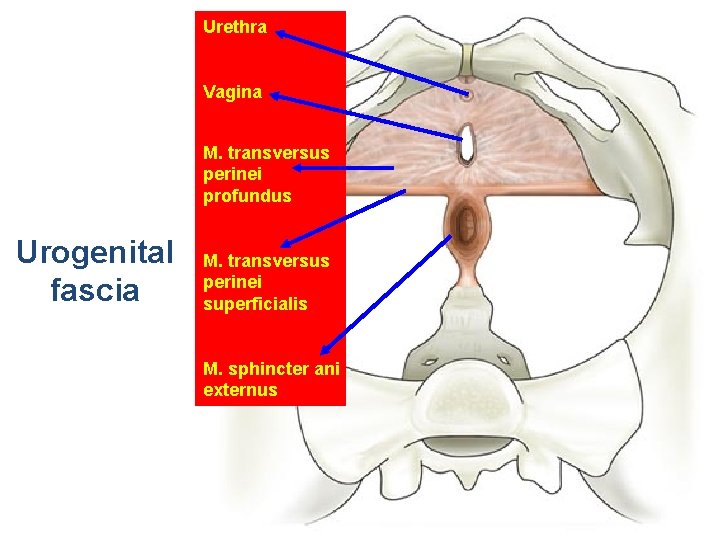
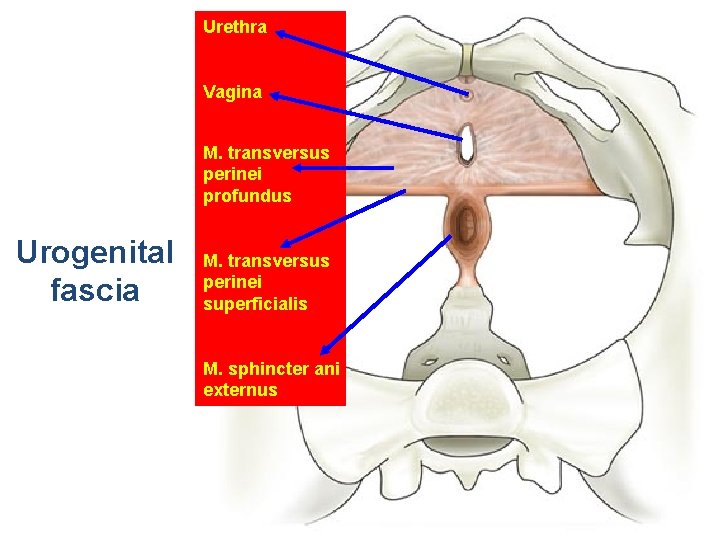
Urethra Vagina M. transversus perinei profundus Urogenital fascia M. transversus perinei superficialis M. sphincter ani externus
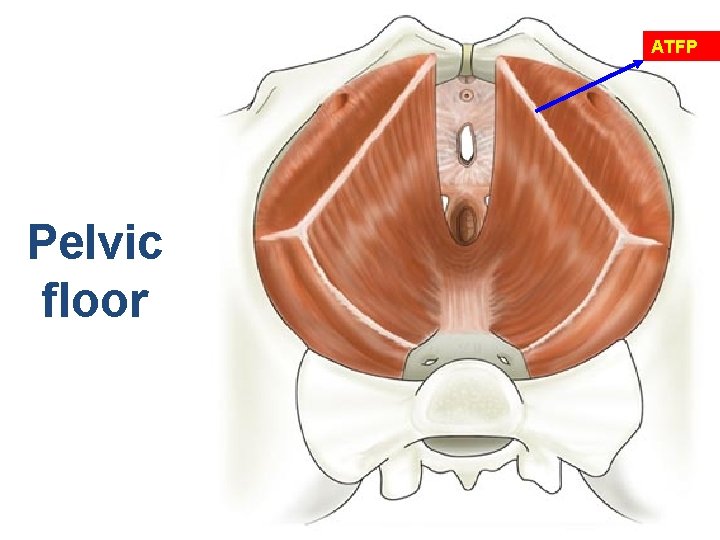
ATFP Pelvic floor
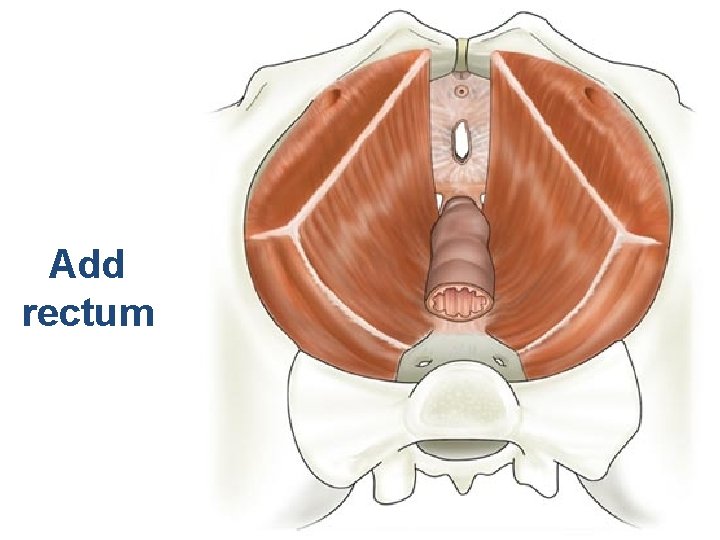
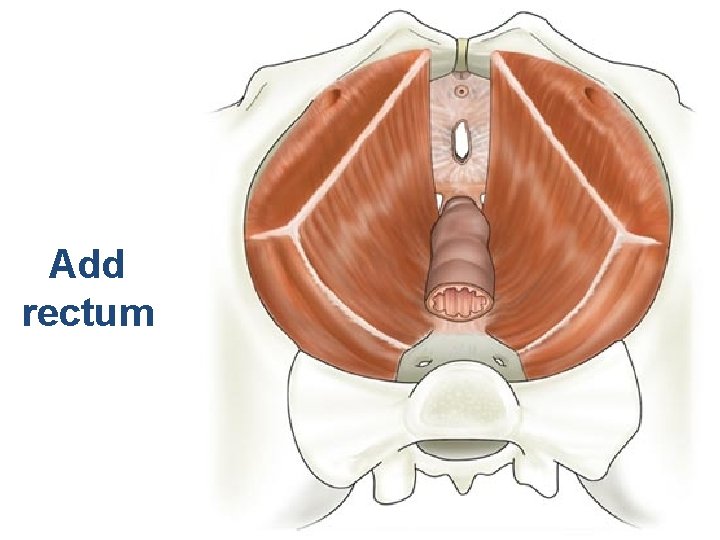
Add rectum
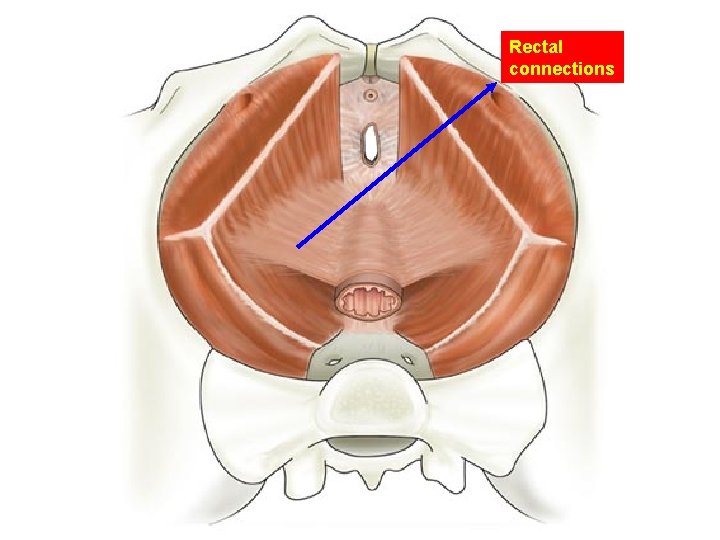
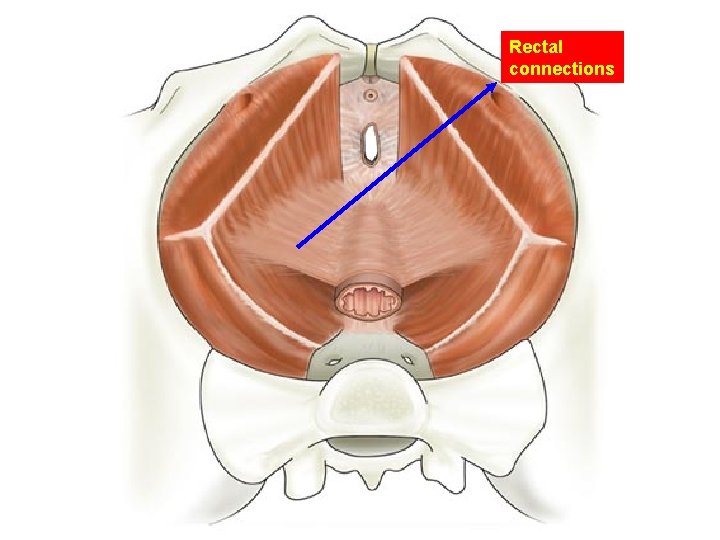
Rectal connections
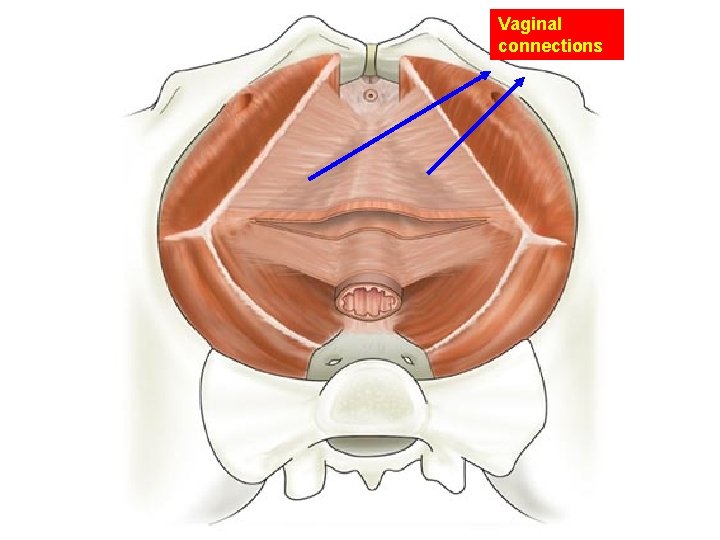
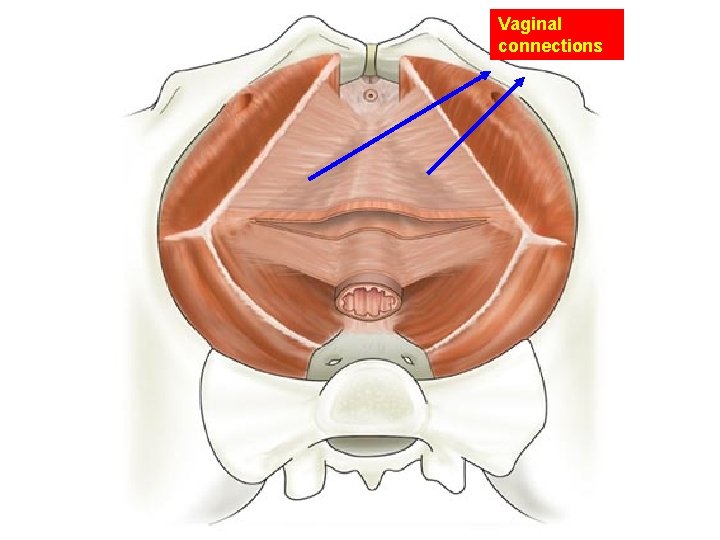
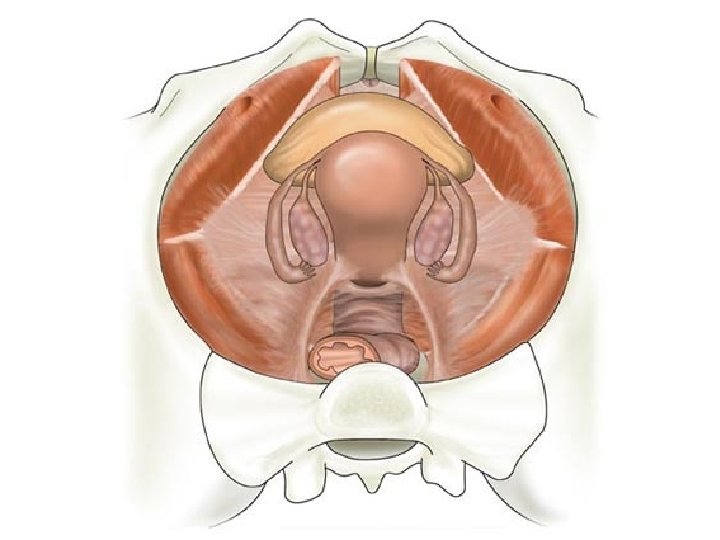
Vaginal connections
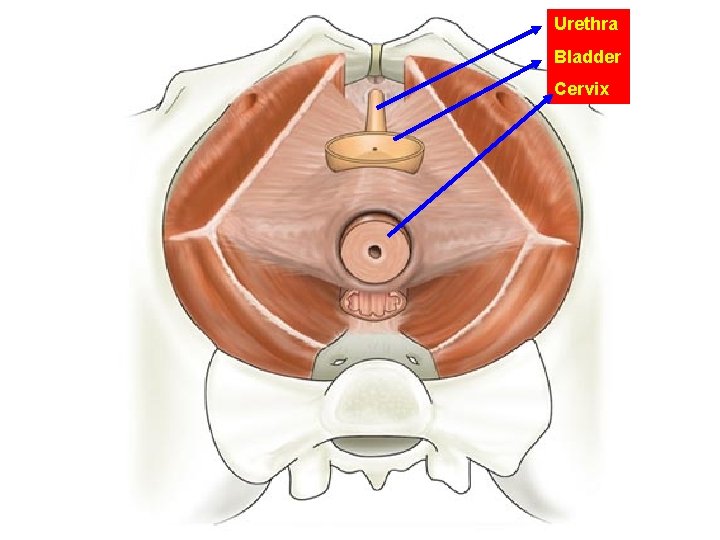
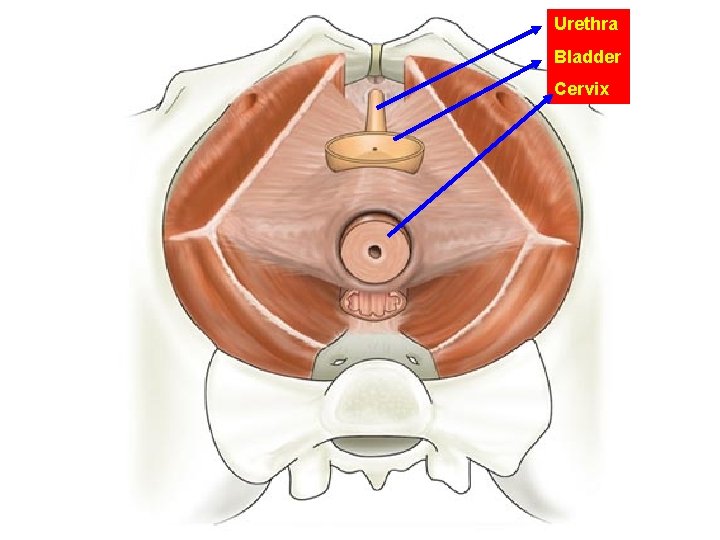
Urethra Bladder Cervix
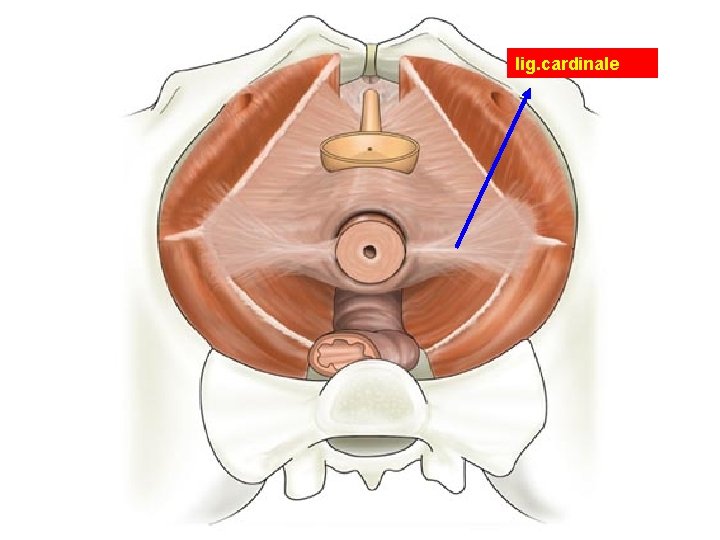
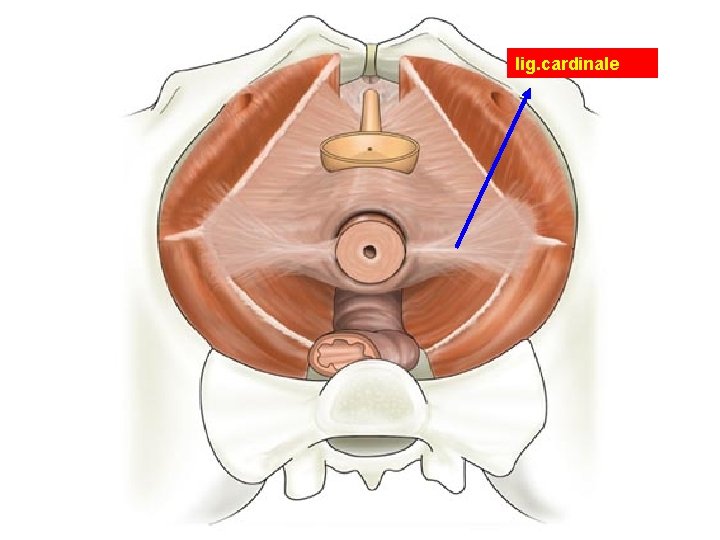
lig. cardinale
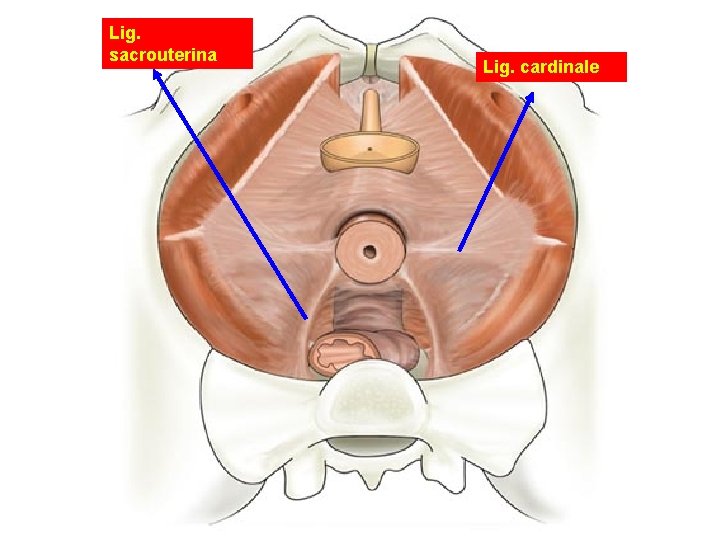
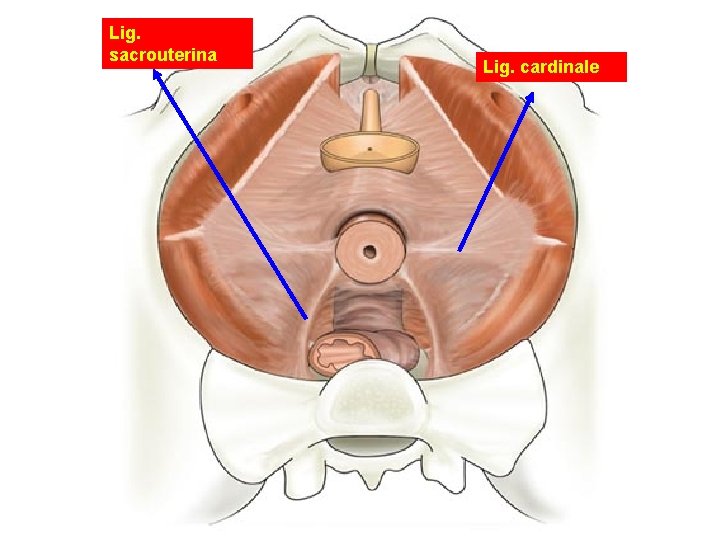
Lig. sacrouterina Lig. cardinale
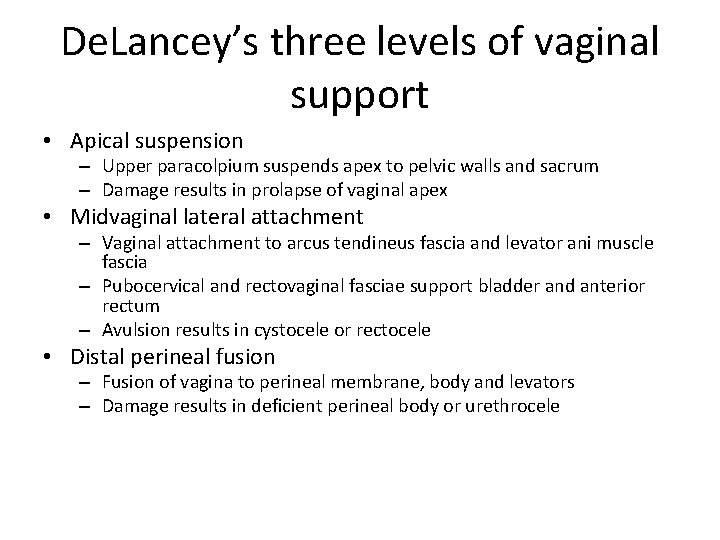
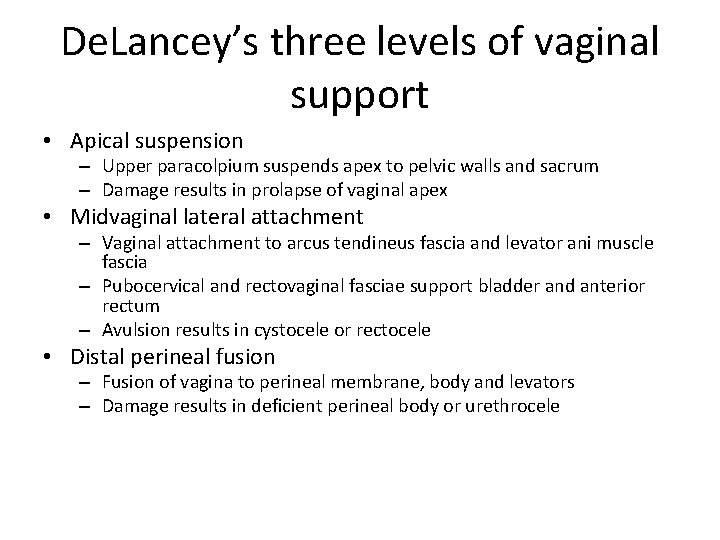
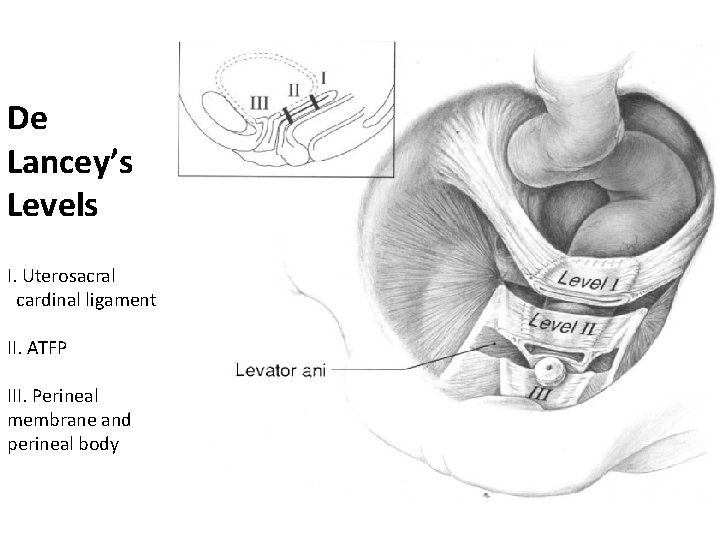
De. Lancey’s three levels of vaginal support • Apical suspension – Upper paracolpium suspends apex to pelvic walls and sacrum – Damage results in prolapse of vaginal apex • Midvaginal lateral attachment – Vaginal attachment to arcus tendineus fascia and levator ani muscle fascia – Pubocervical and rectovaginal fasciae support bladder and anterior rectum – Avulsion results in cystocele or rectocele • Distal perineal fusion – Fusion of vagina to perineal membrane, body and levators – Damage results in deficient perineal body or urethrocele
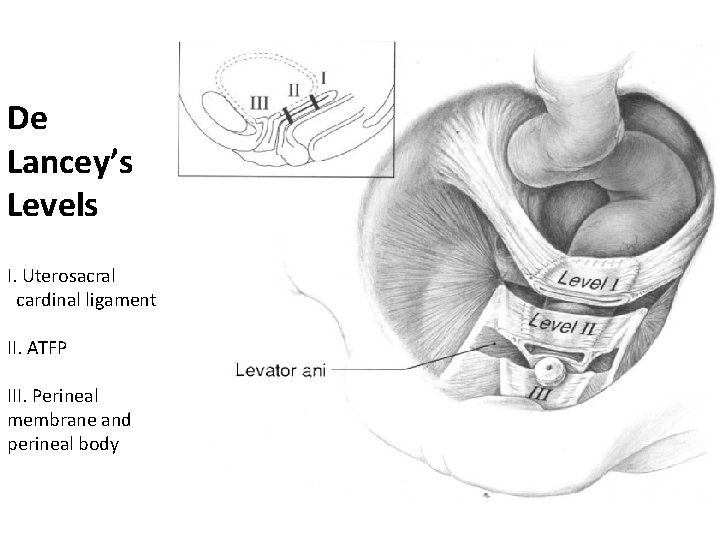
De Lancey’s Levels I. Uterosacral cardinal ligament II. ATFP III. Perineal membrane and perineal body
Factors associated with pelvic floor prolapse • • age parity big babies menopause obesity occupation home delivery family history
Pathogenesis • • • childbirth connective tissue disorders menopause chronic intra-abdominal pressure iatrogenic (hysterectomy)
Factors promoting prolapse • Erect posture causes increased stress on muscles, nerves and connective tissue • Acute and chronic trauma of vaginal delivery • Aging • Estrogen deprivation • Intrinsic collagen abnormalities • Chronic increase in intraabdominal pressure – heavy lifting – coughing – constipation
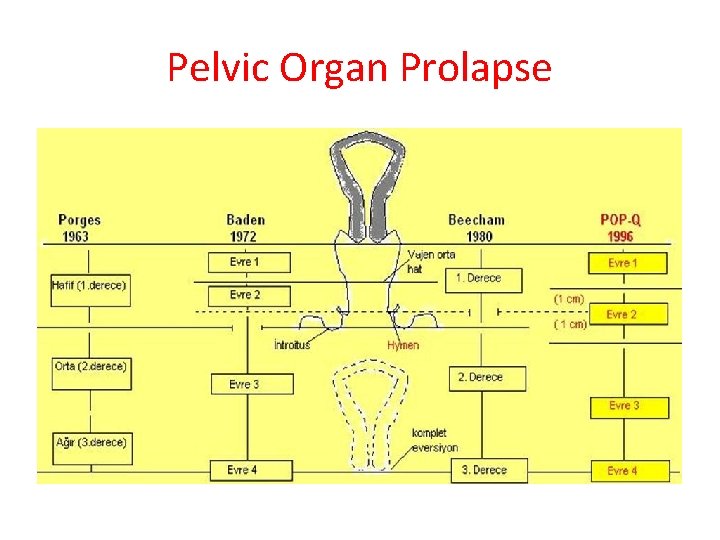
Pelvic Organ Prolapse
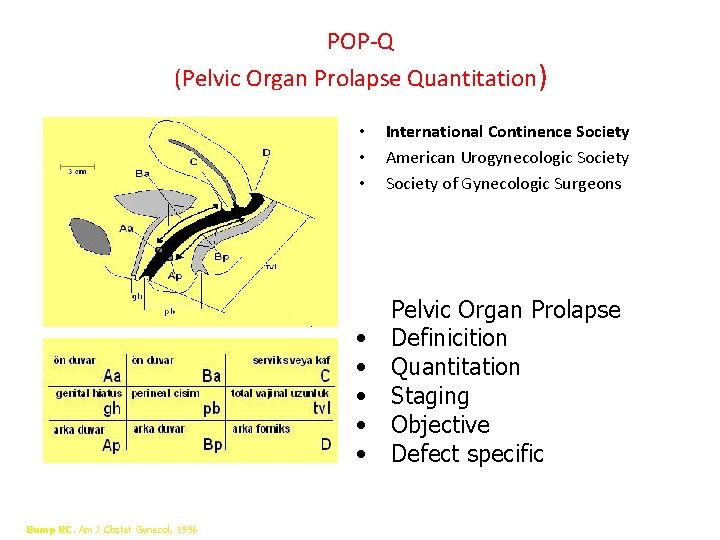
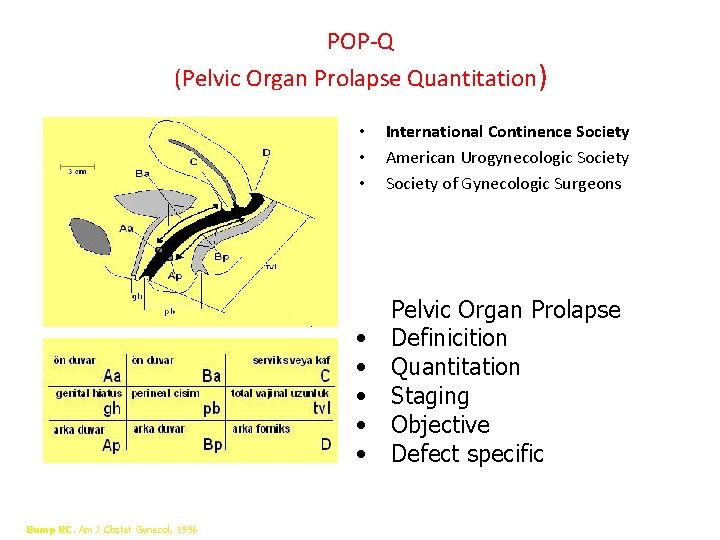
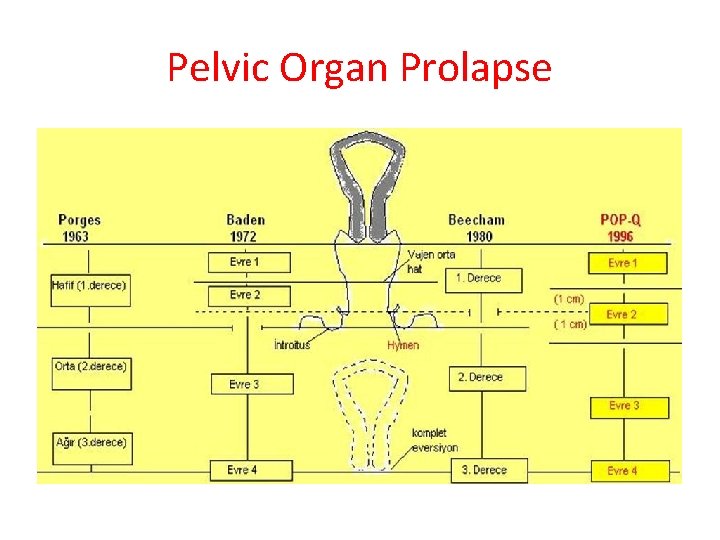
POP-Q (Pelvic Organ Prolapse Quantitation) Bump RC. Am J Obstet Gynecol, 1996 • • • International Continence Society American Urogynecologic Society of Gynecologic Surgeons • • • Pelvic Organ Prolapse Definicition Quantitation Staging Objective Defect specific
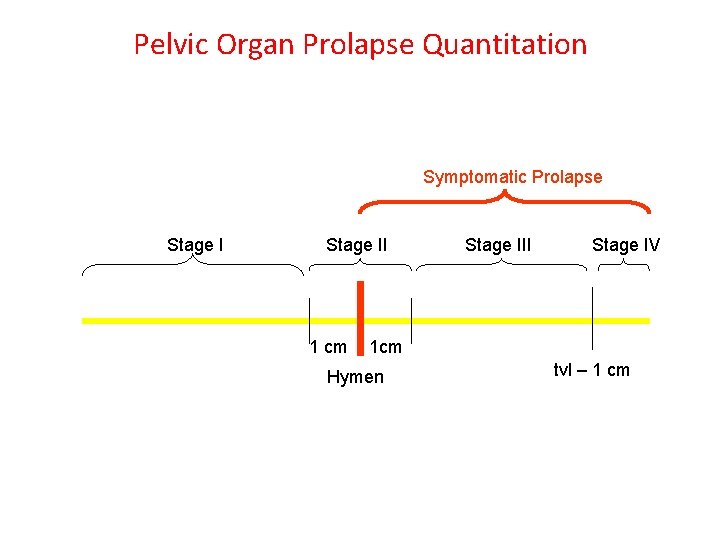
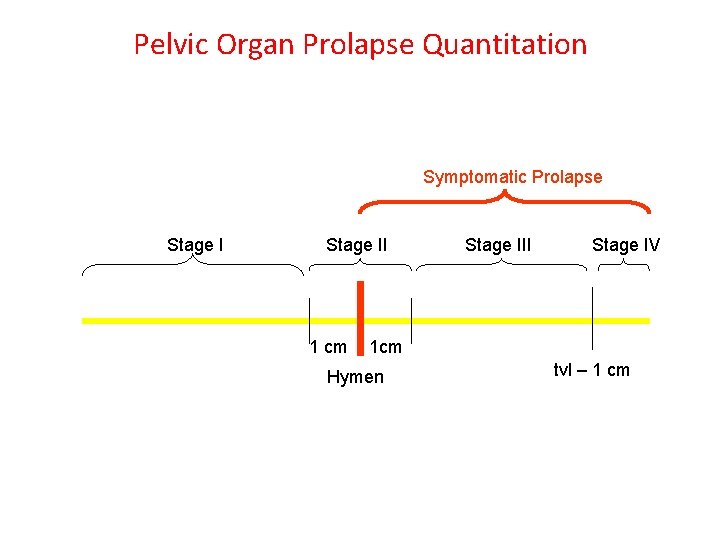
Pelvic Organ Prolapse Quantitation Symptomatic Prolapse Stage II 1 cm Stage III Stage IV 1 cm Hymen tvl – 1 cm
Pelvic Relaxation • • • Cystocele Stress urinary incontinence Rectocele Enterocele Uterine and vaginal prolapse – Result of weakness or defect in supporting tissues endopelvic fascia and neuromuscular damage
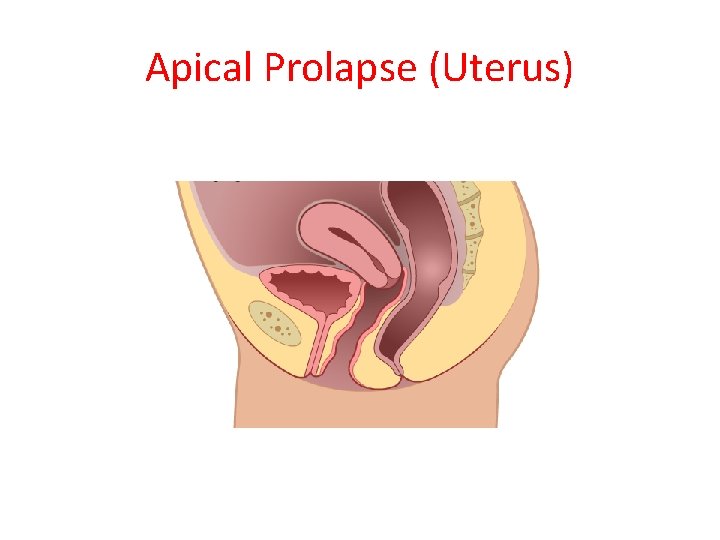
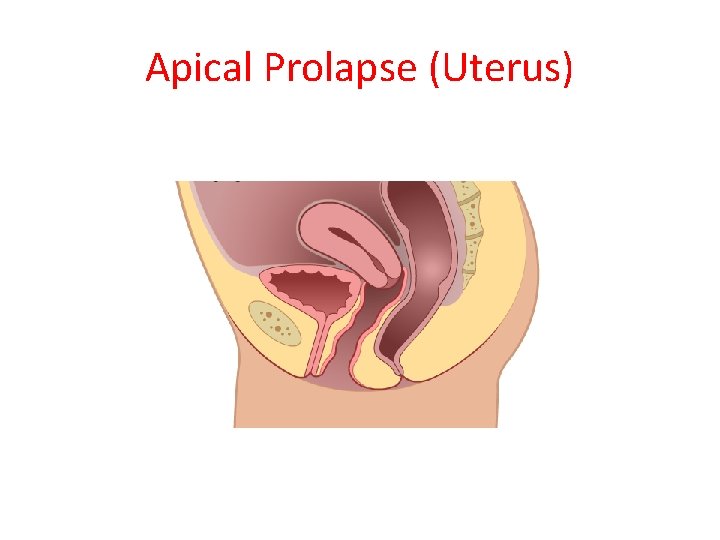
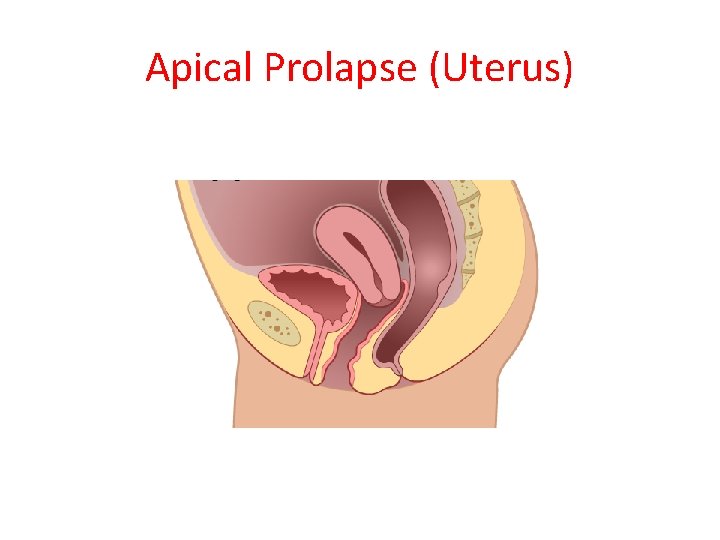
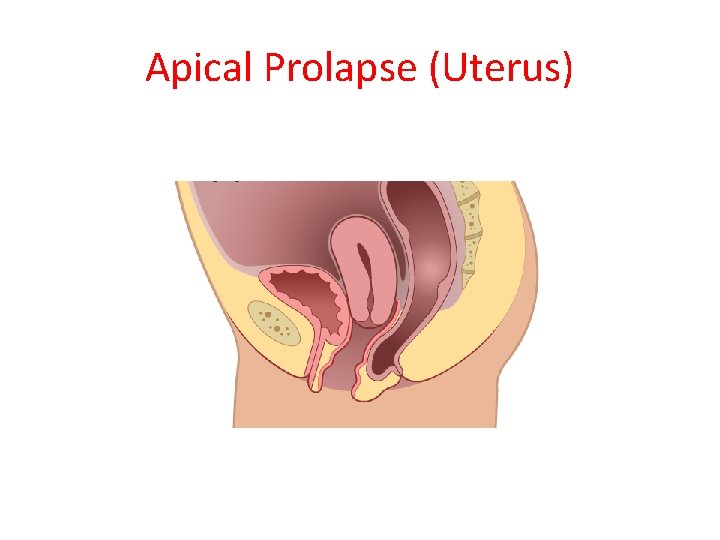
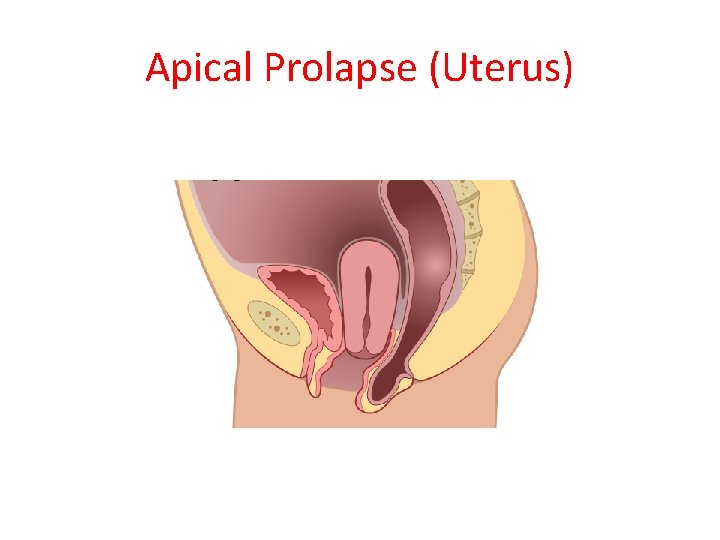
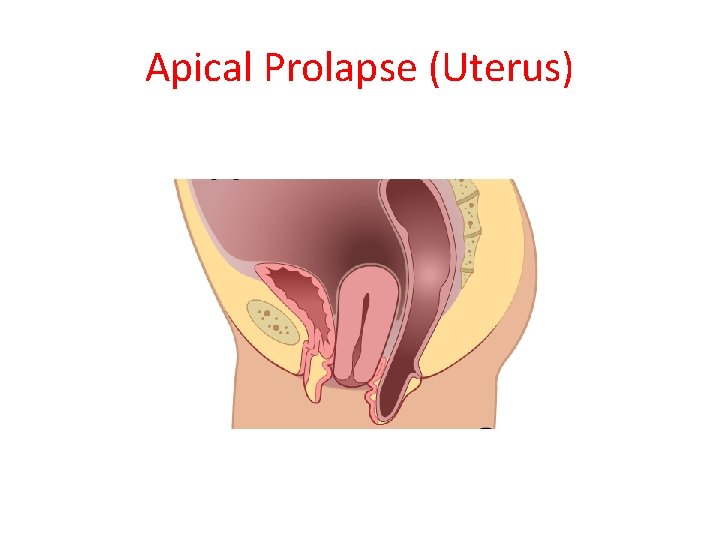
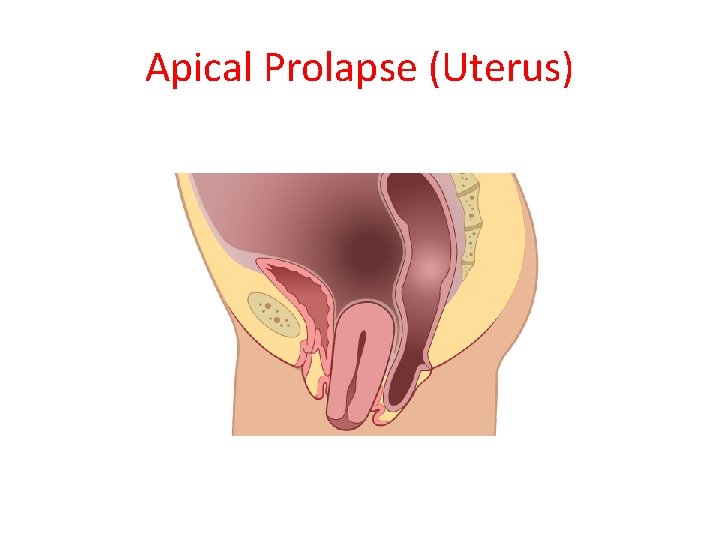
Apical Prolapse (Uterus)
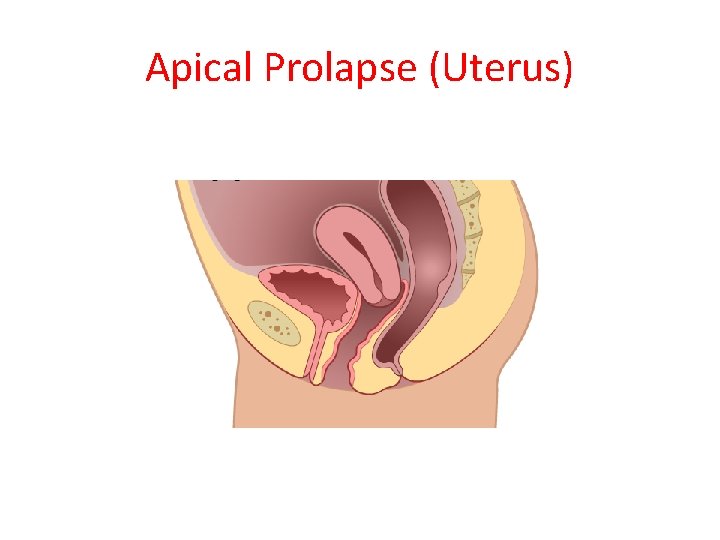
Apical Prolapse (Uterus)
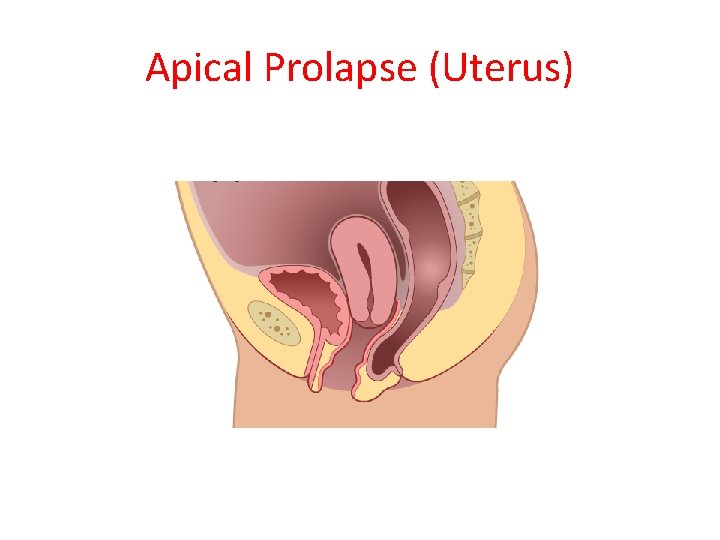
Apical Prolapse (Uterus)
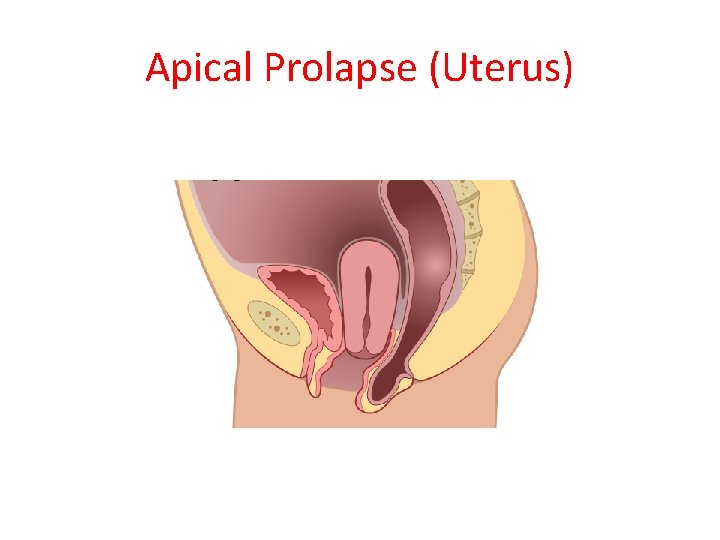
Apical Prolapse (Uterus)
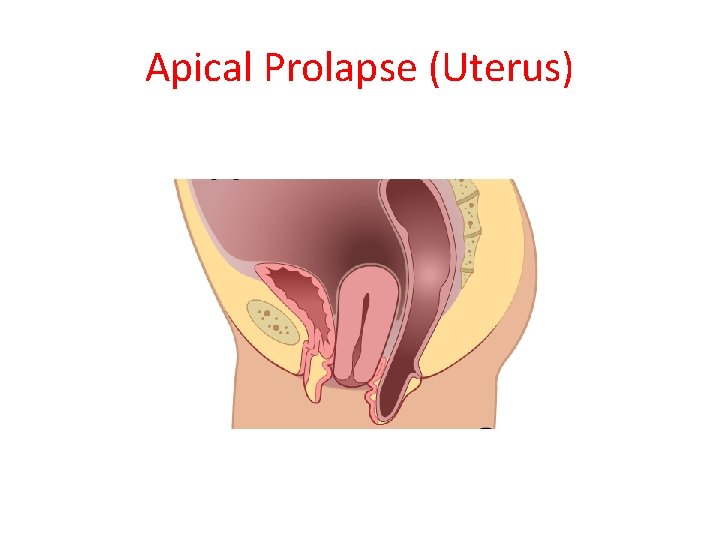
Apical Prolapse (Uterus)
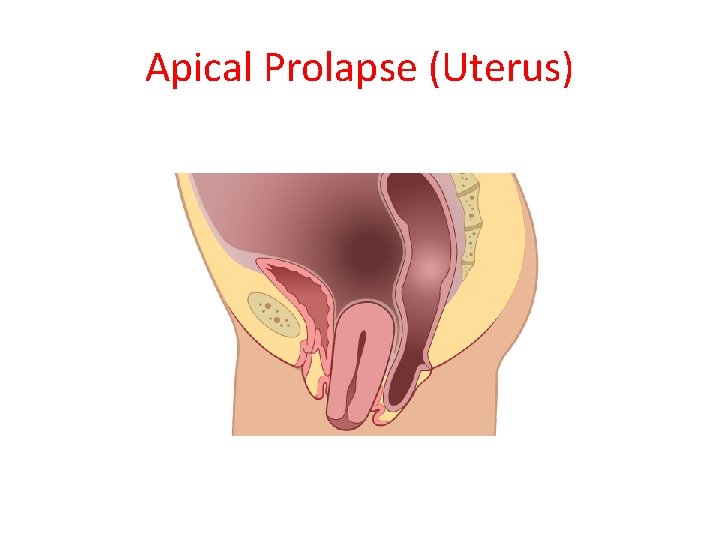
Apical Prolapse (Uterus)
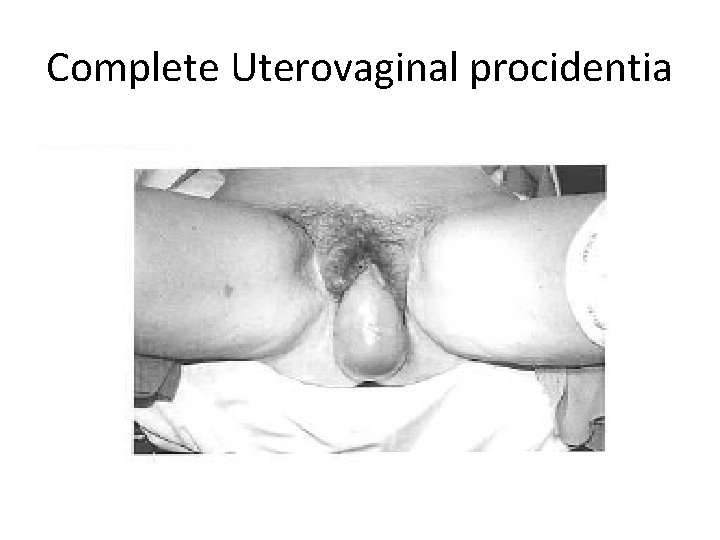
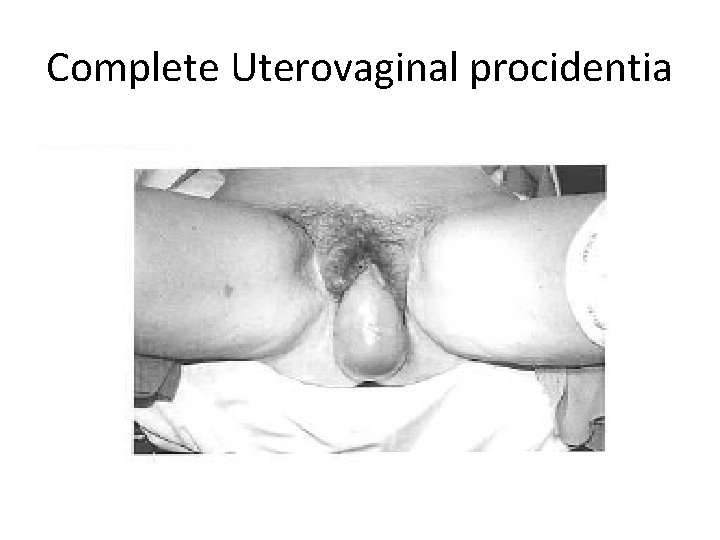
Complete Uterovaginal procidentia
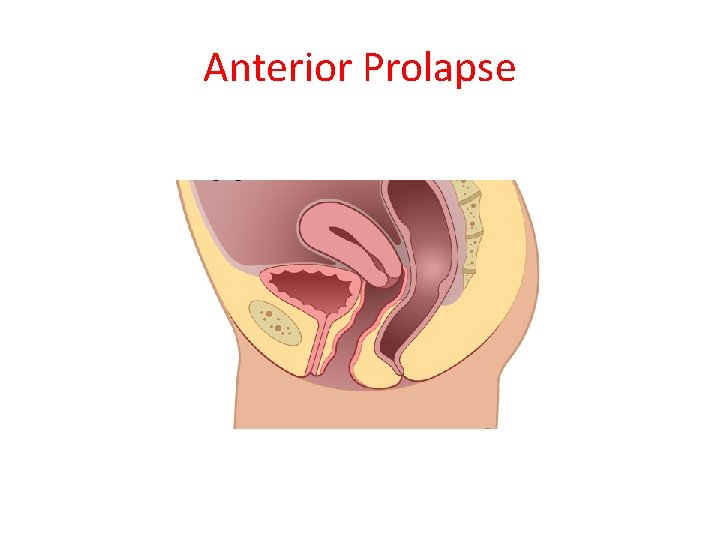
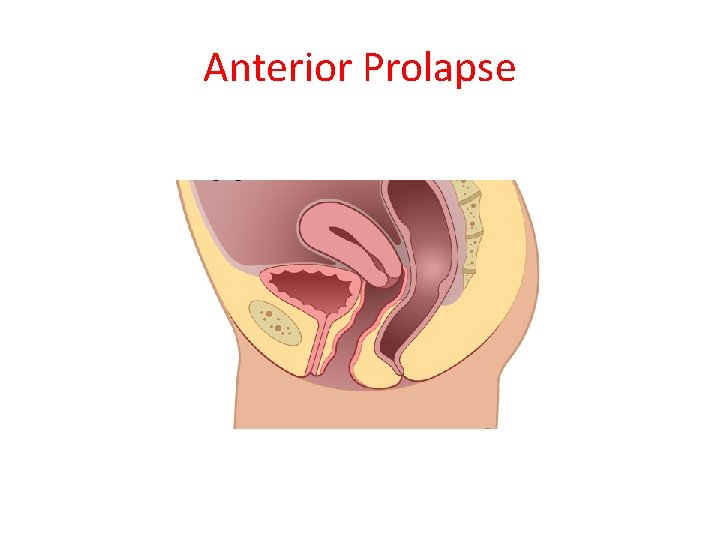
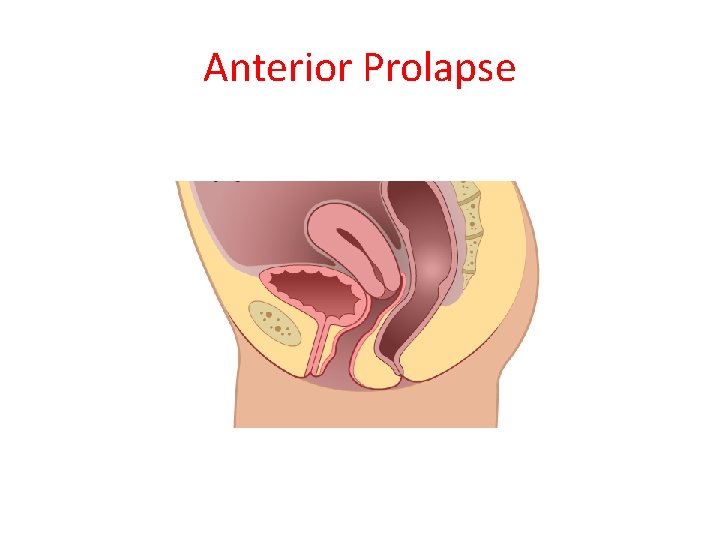
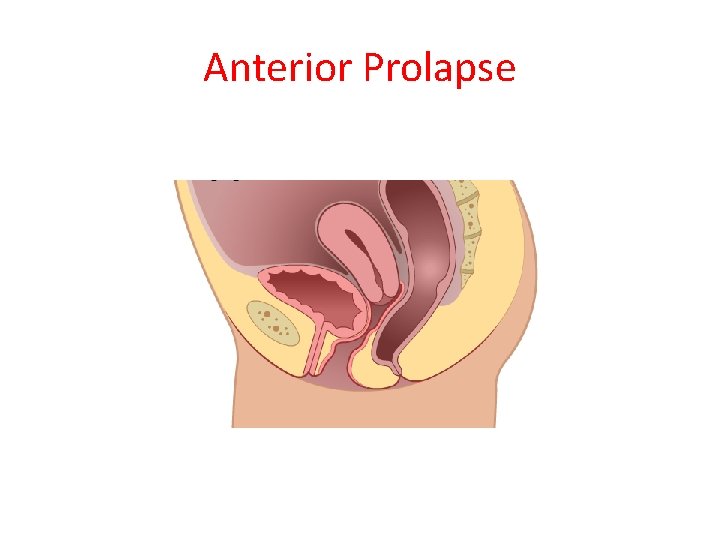
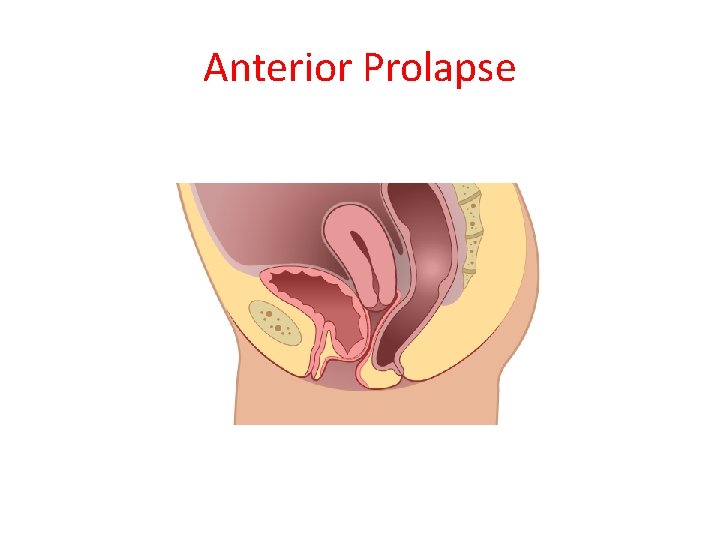
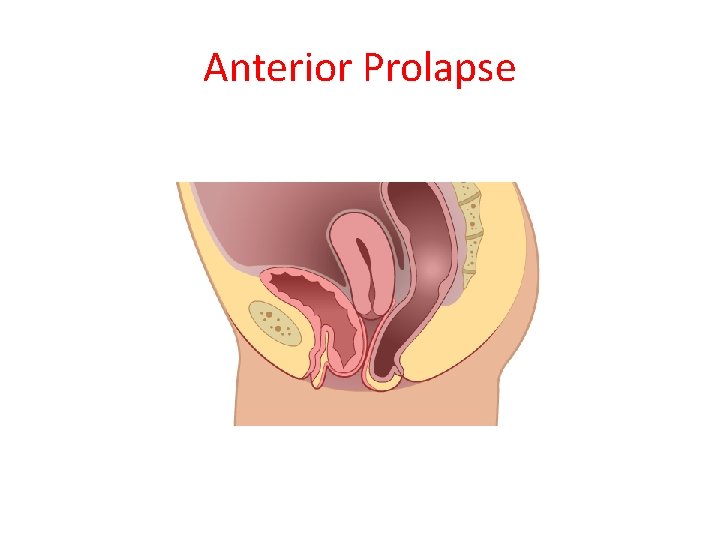
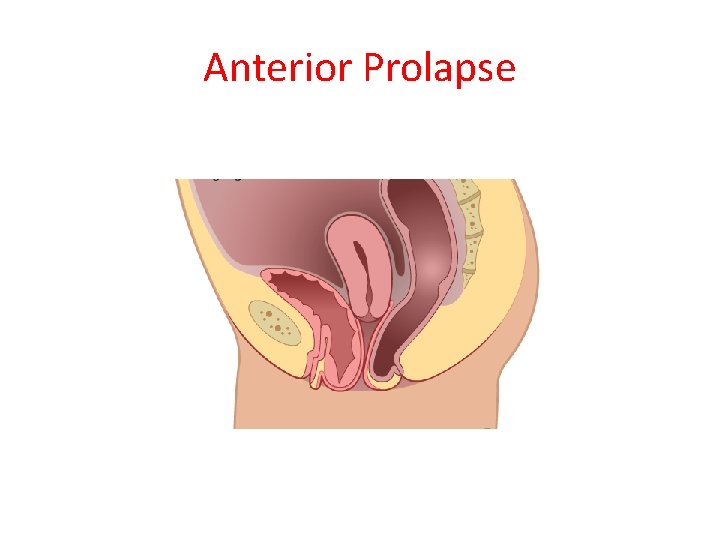
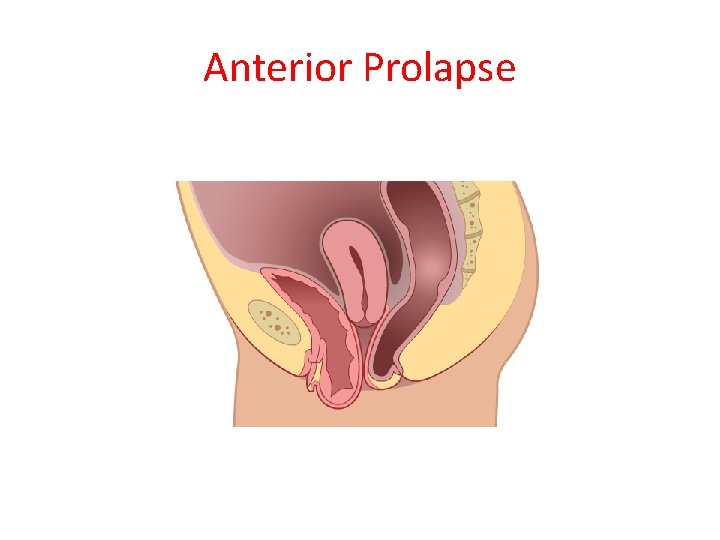
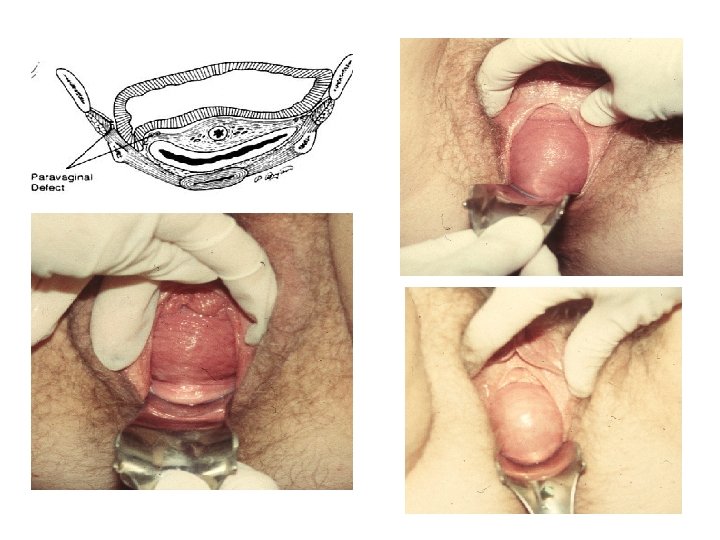
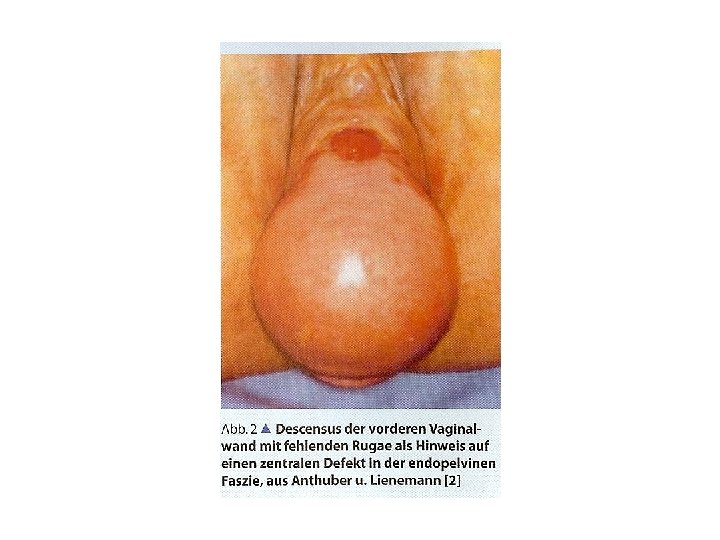
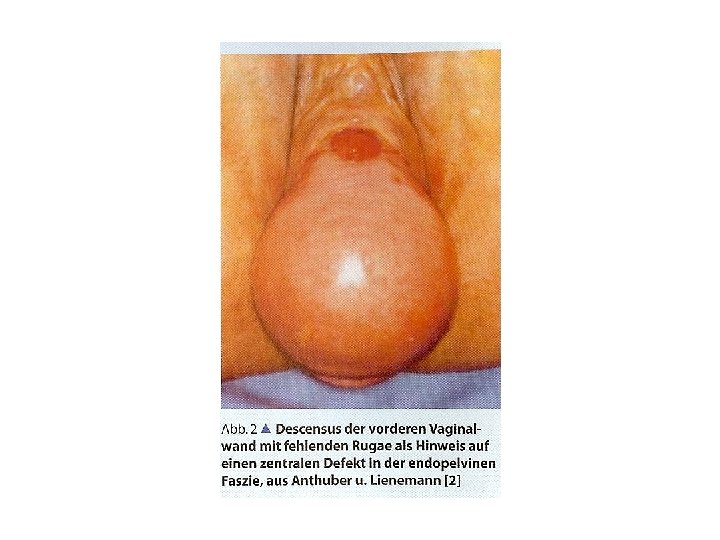
Anterior Prolapse
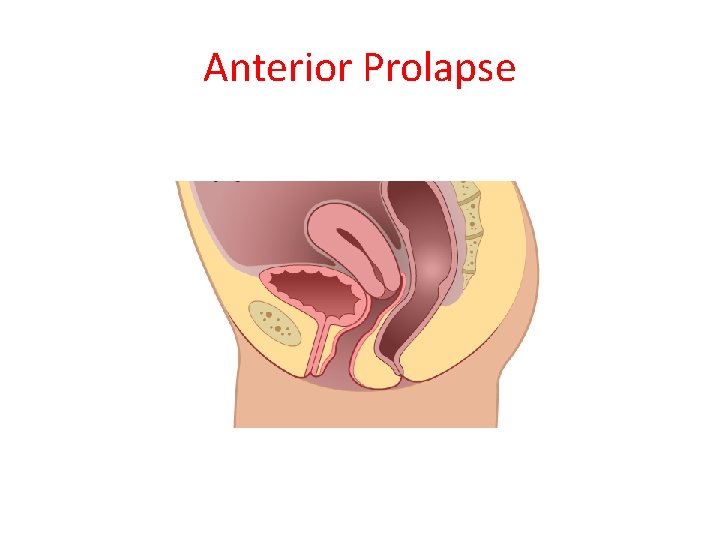
Anterior Prolapse
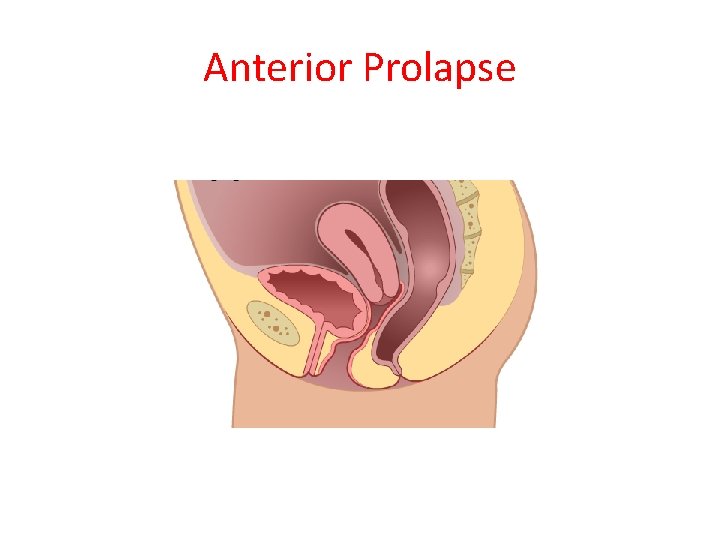
Anterior Prolapse
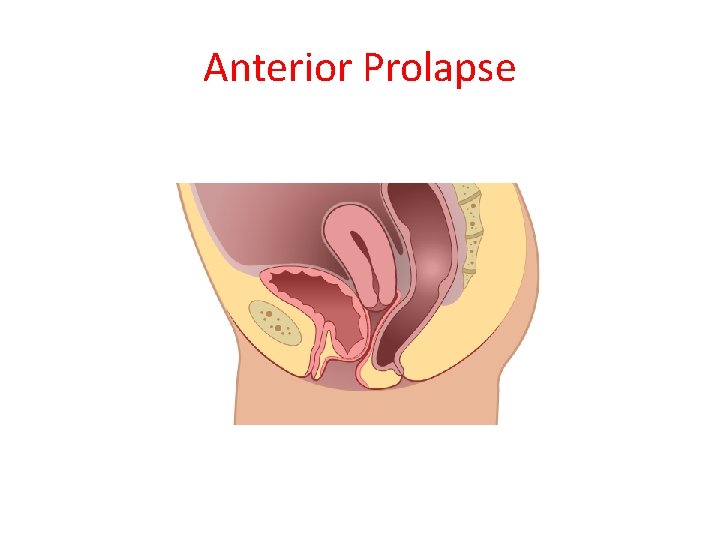
Anterior Prolapse
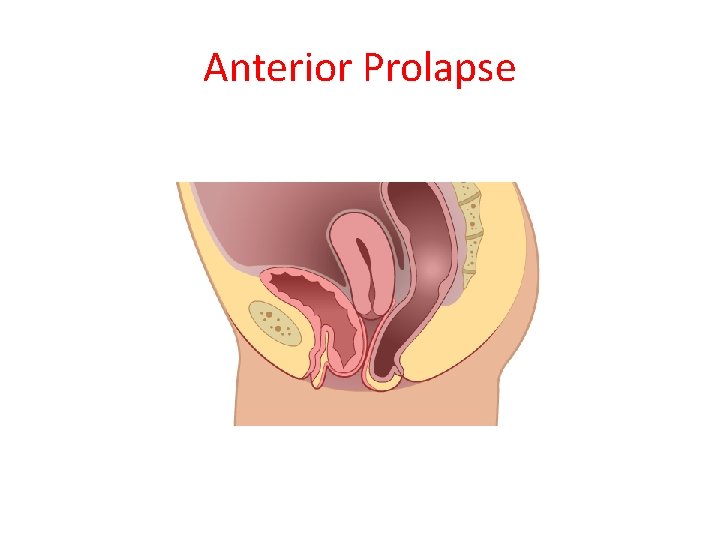
Anterior Prolapse
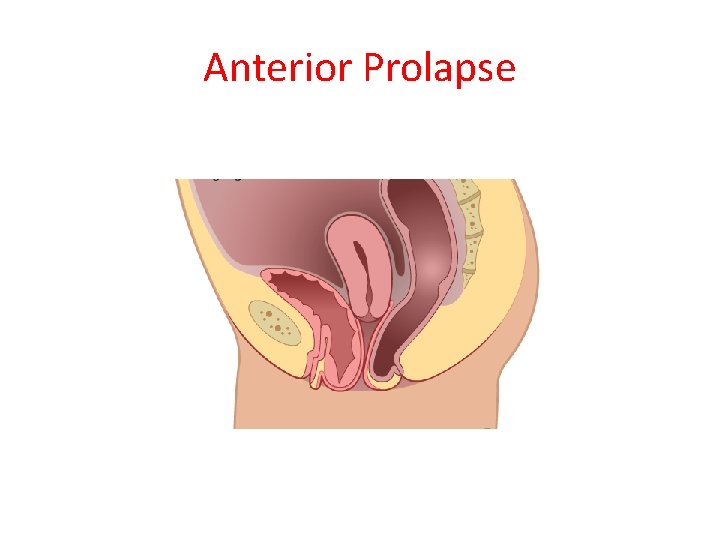
Anterior Prolapse
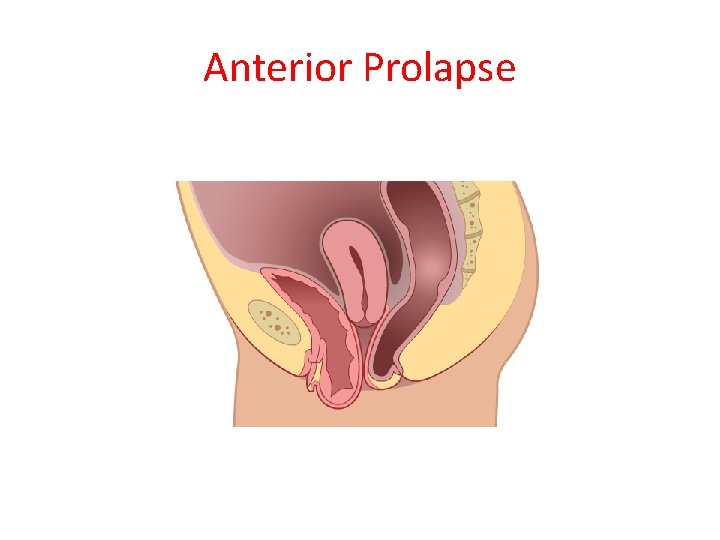
Anterior Prolapse
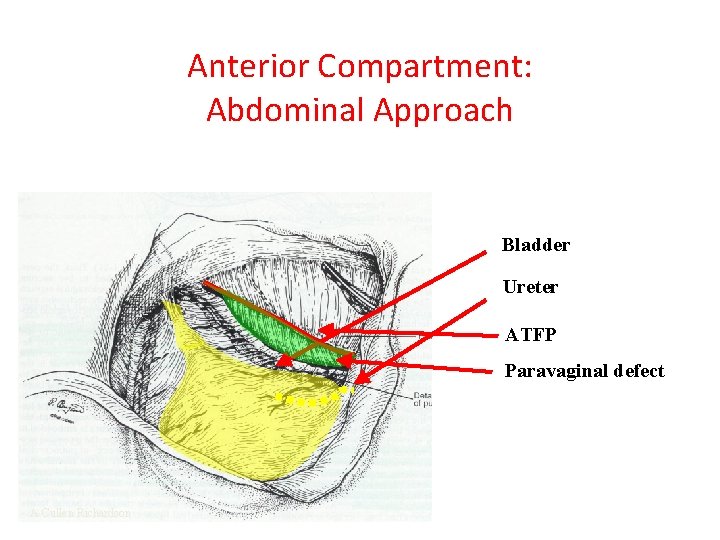
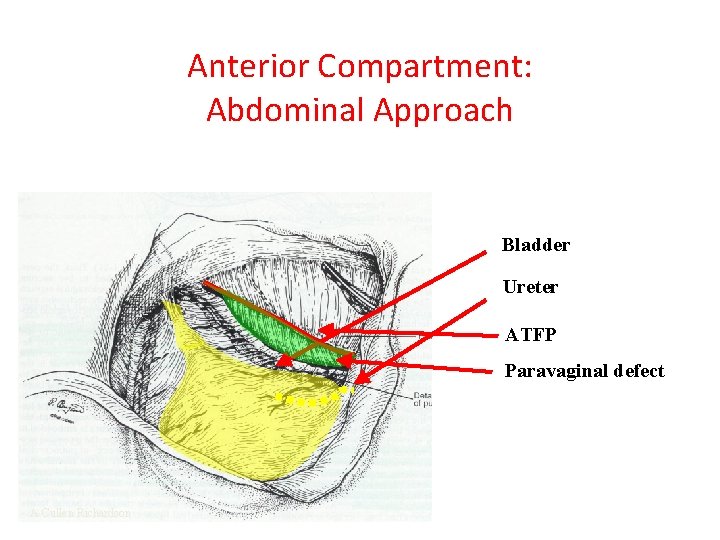
Anterior Compartment: Abdominal Approach Bladder Ureter ATFP Paravaginal defect A Cullen Richardson
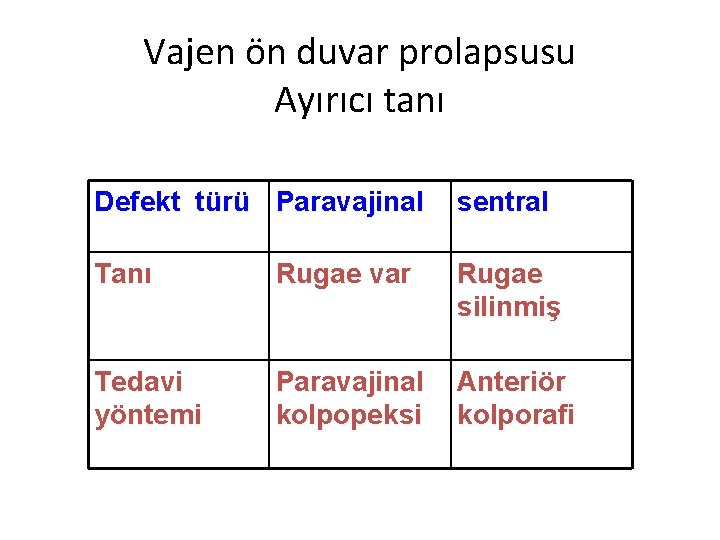
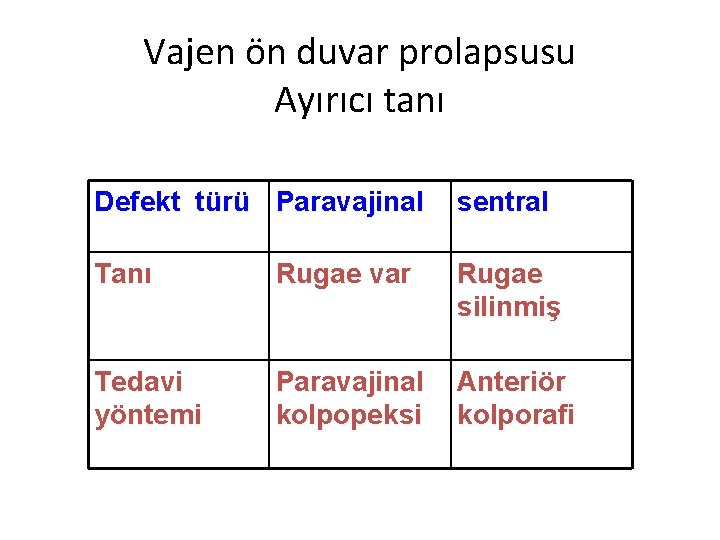
Vajen ön duvar prolapsusu Ayırıcı tanı Defekt türü Paravajinal sentral Tanı Rugae var Rugae silinmiş Tedavi yöntemi Paravajinal kolpopeksi Anteriör kolporafi
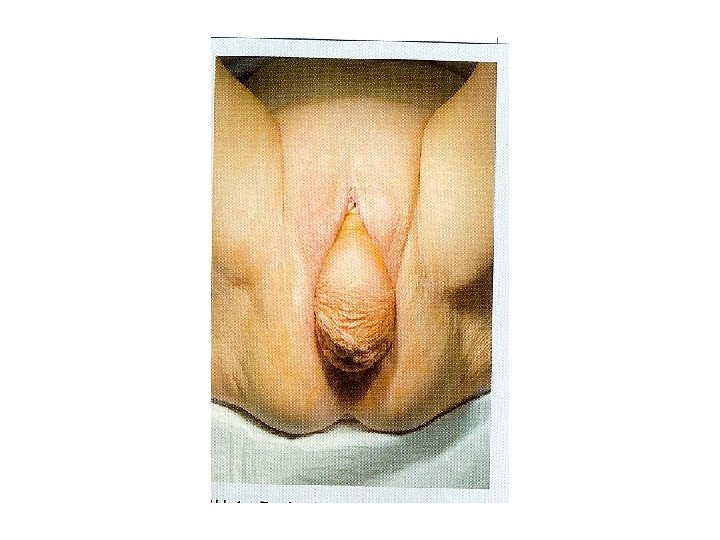
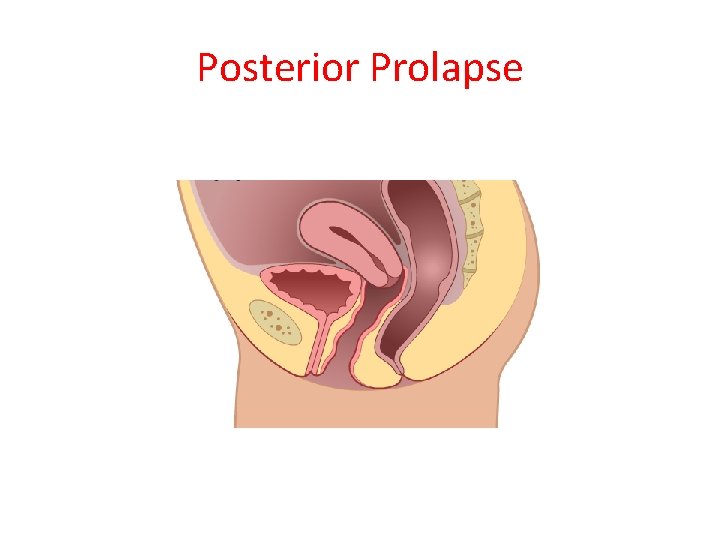
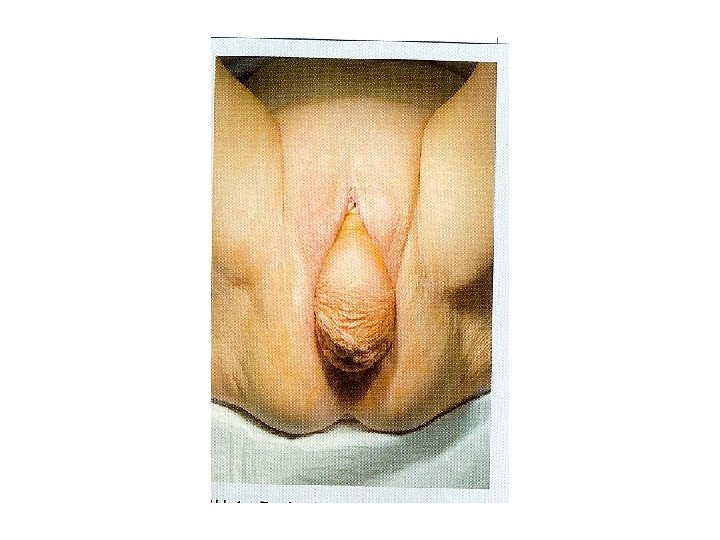
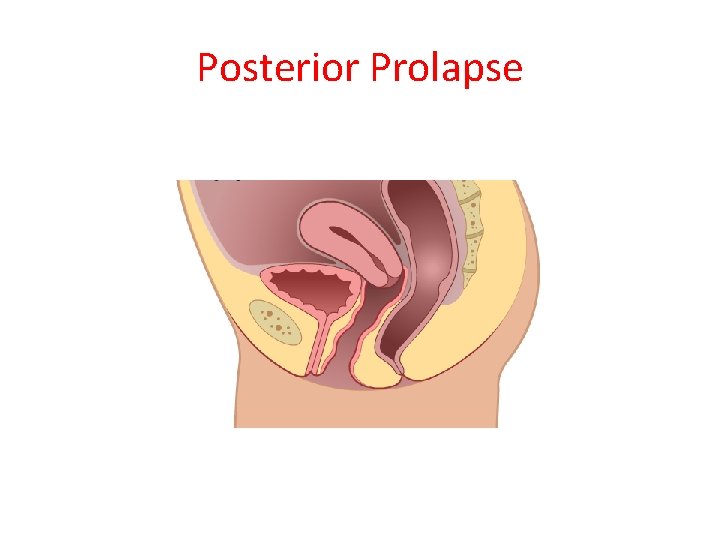
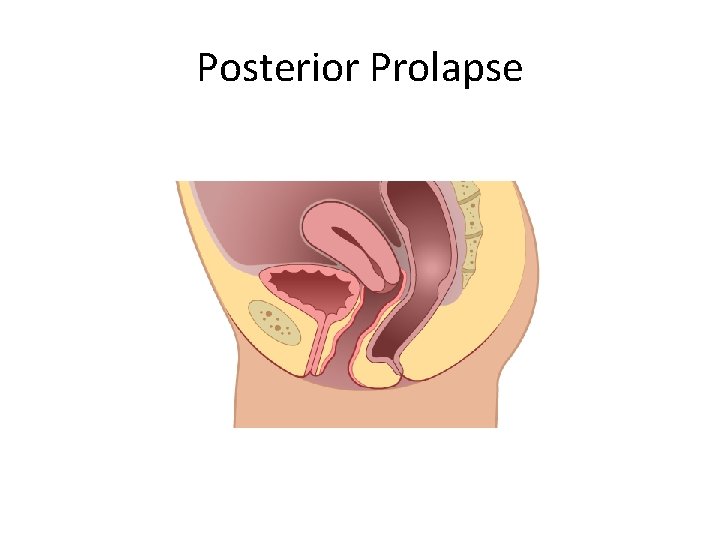
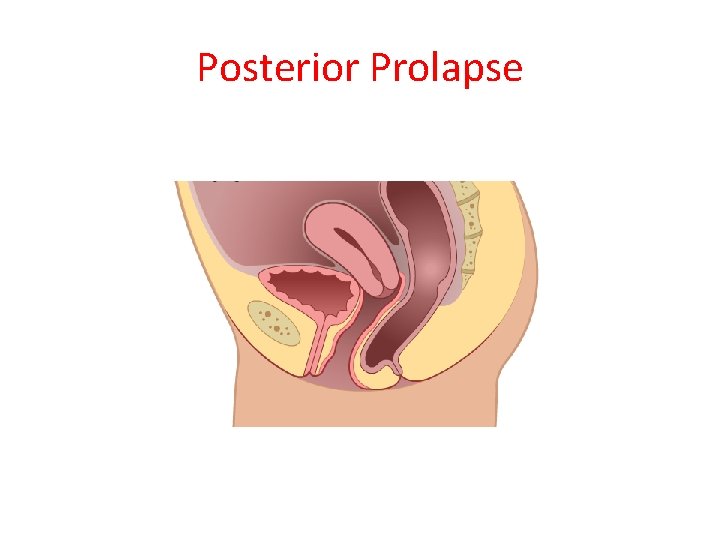
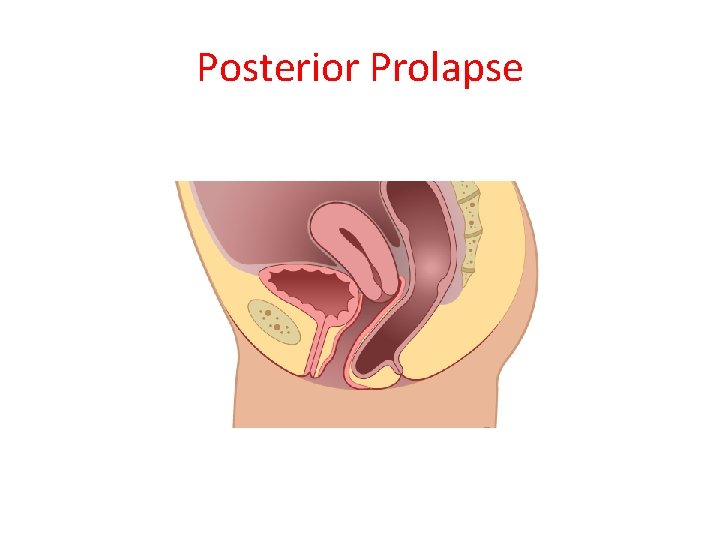
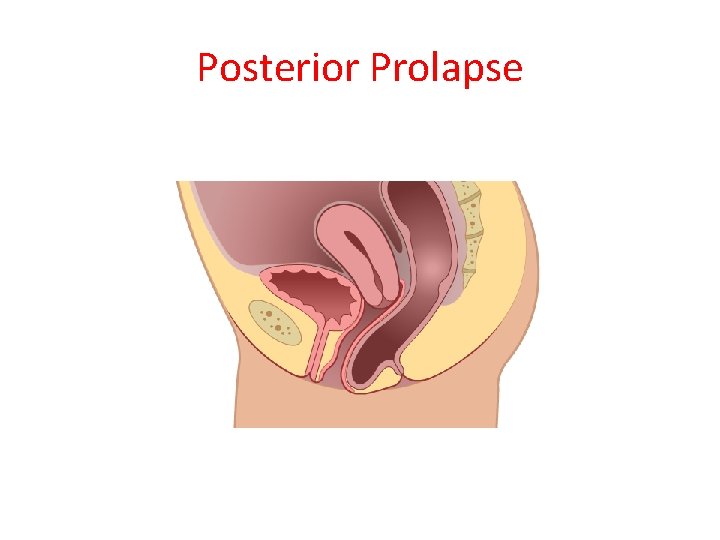
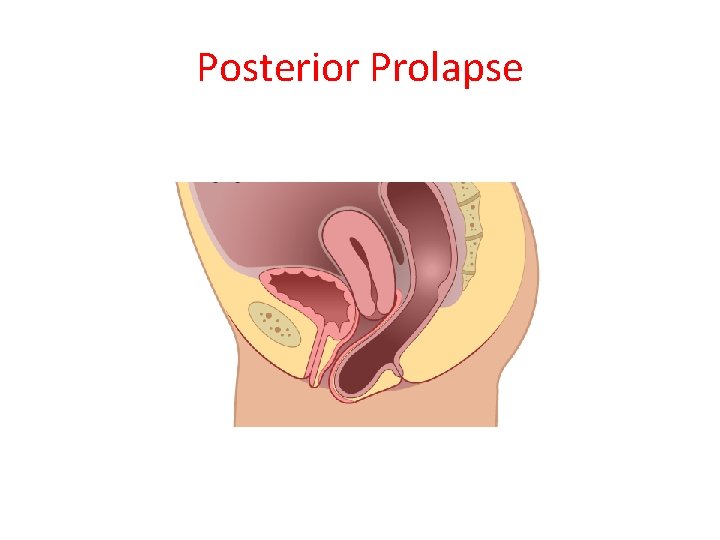
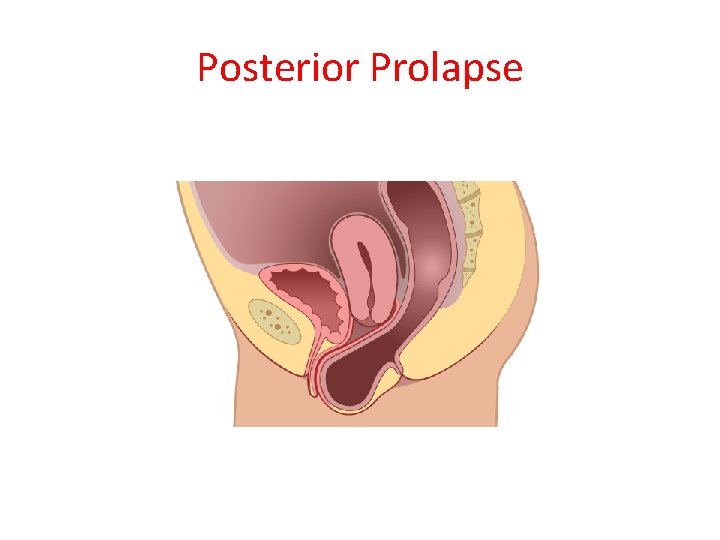
Posterior Prolapse
Posterior Prolapse
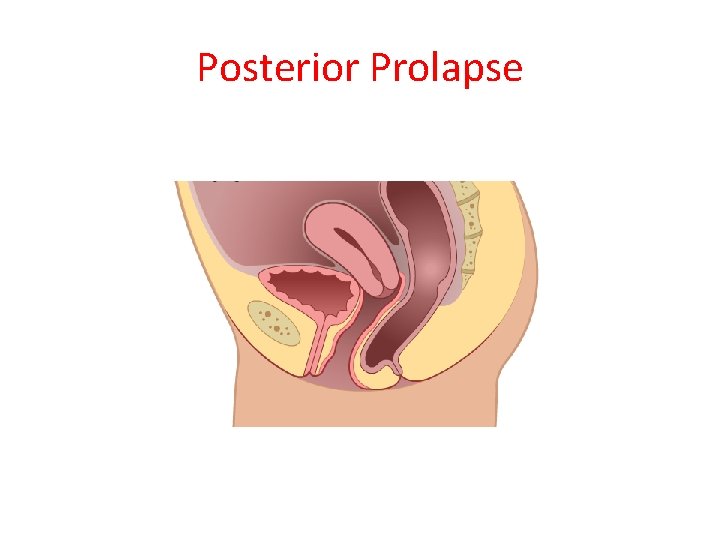
Posterior Prolapse
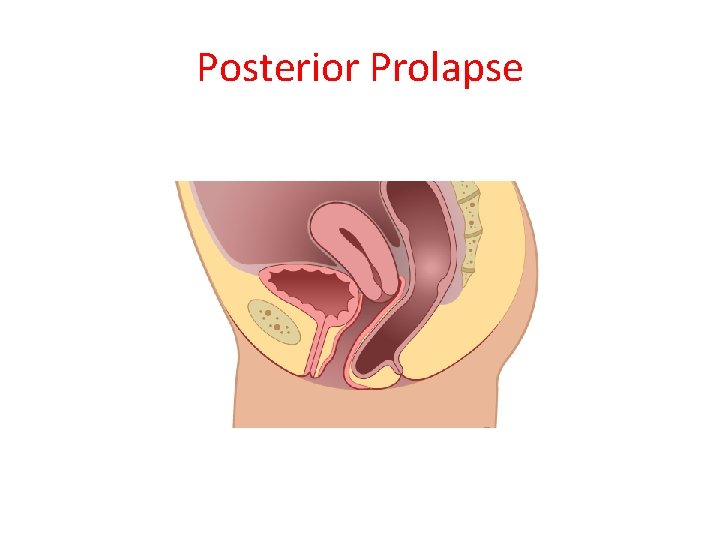
Posterior Prolapse
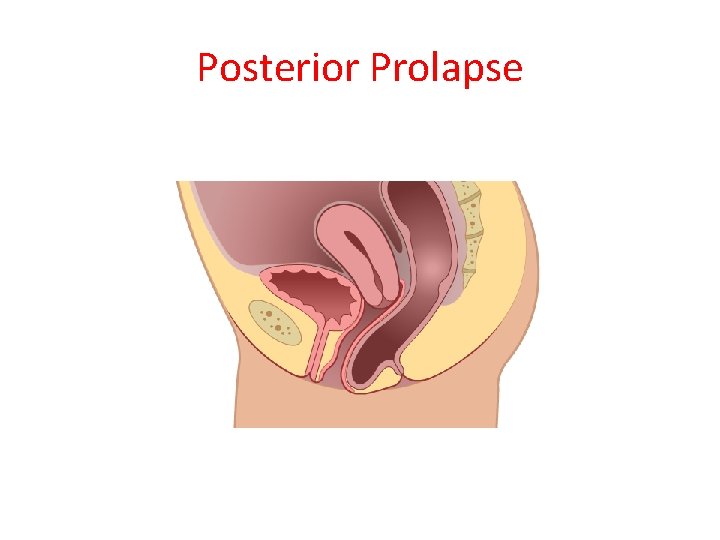
Posterior Prolapse
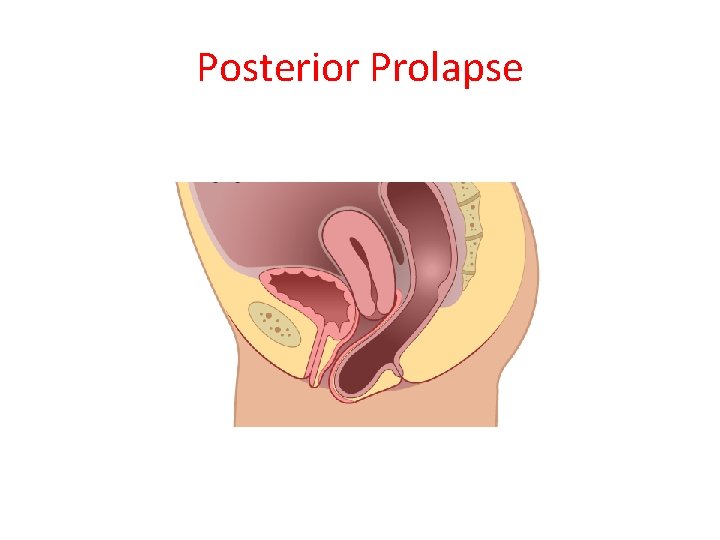
Posterior Prolapse
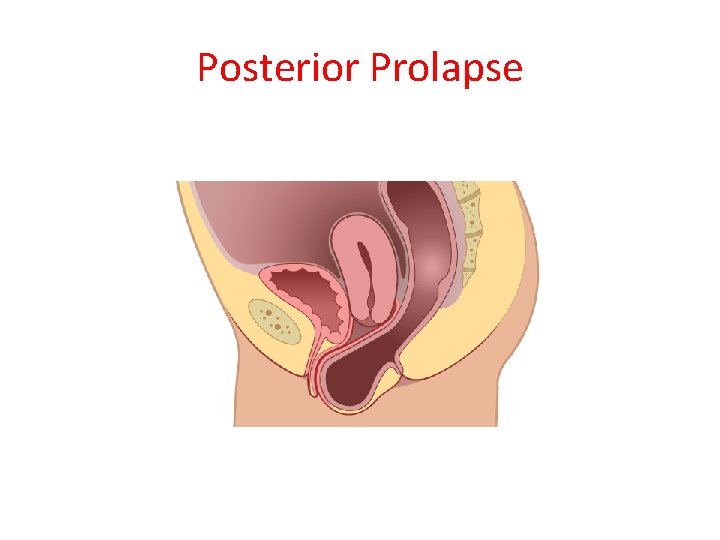
Posterior Prolapse
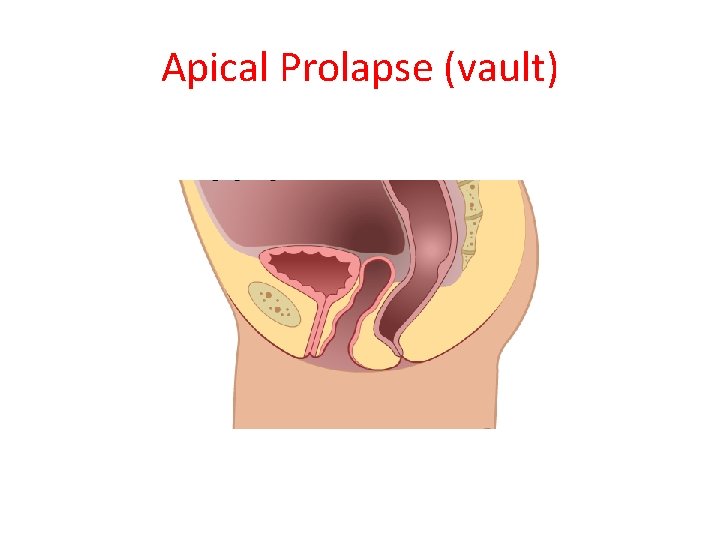
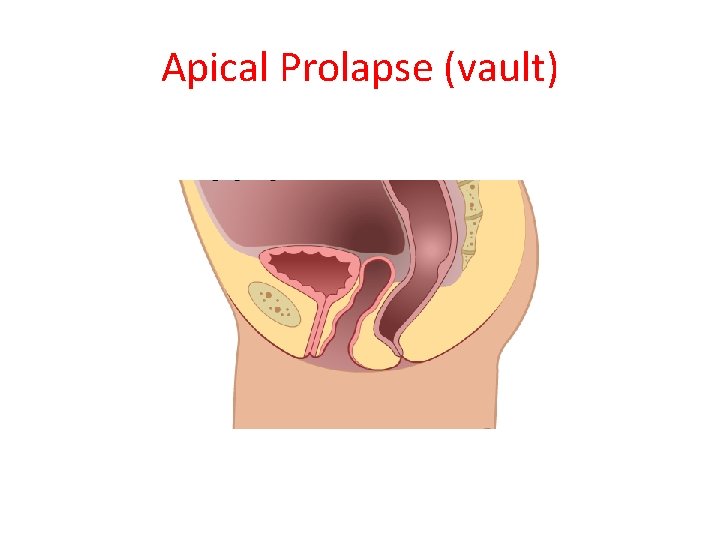
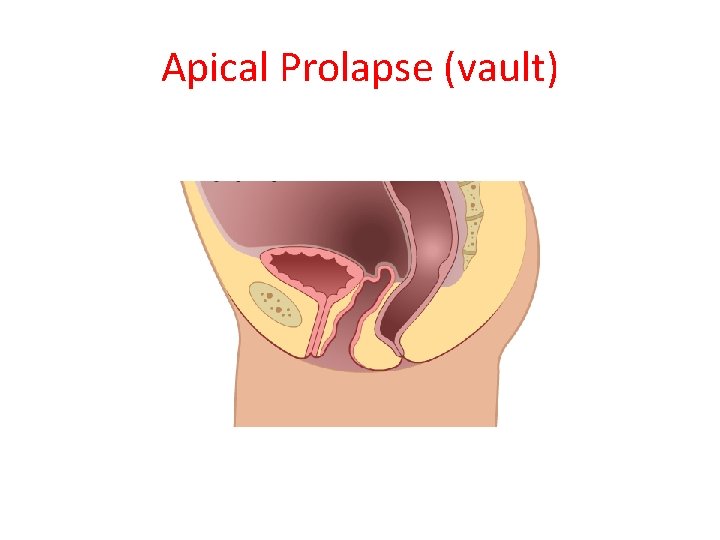
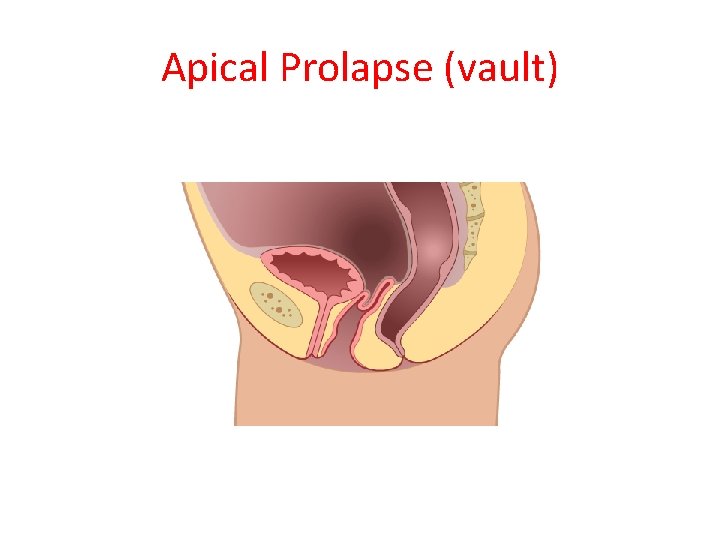
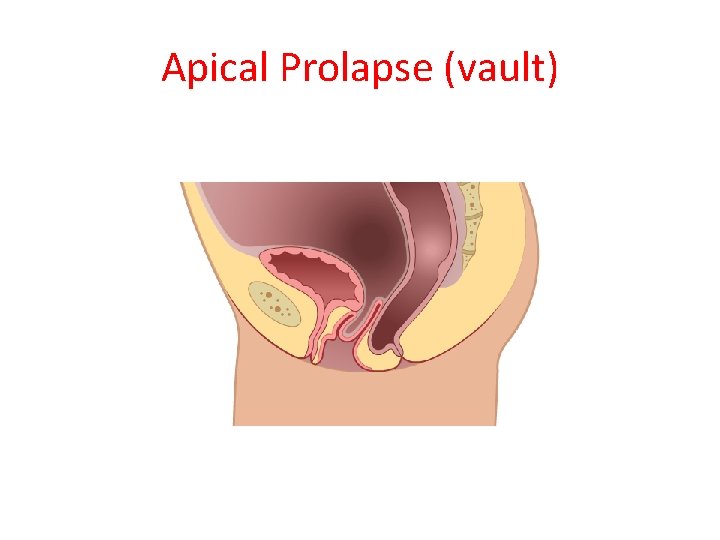
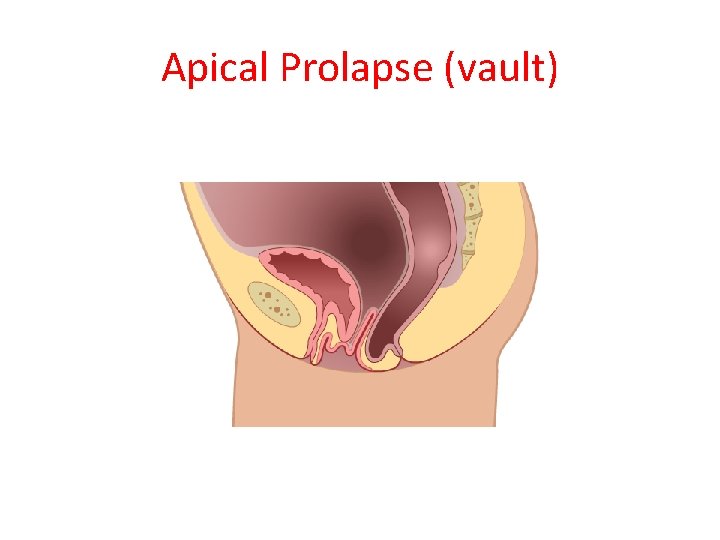
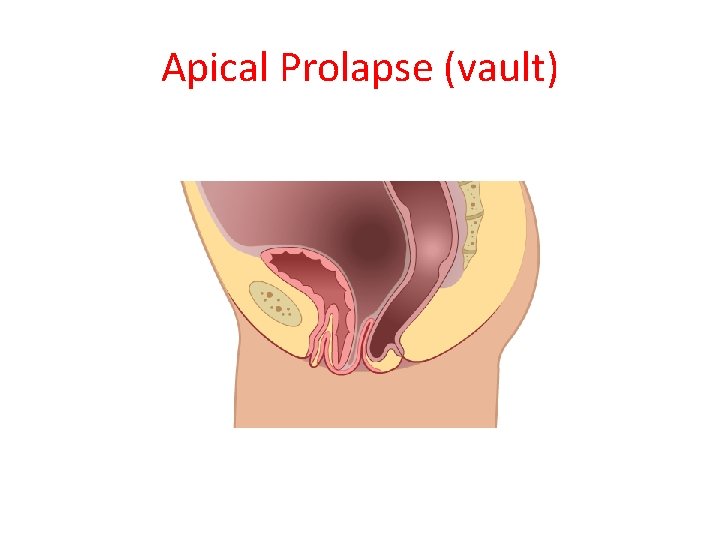
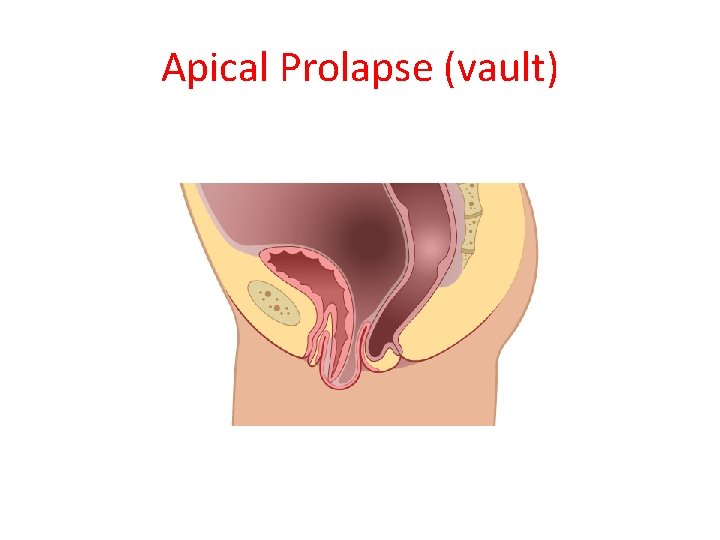
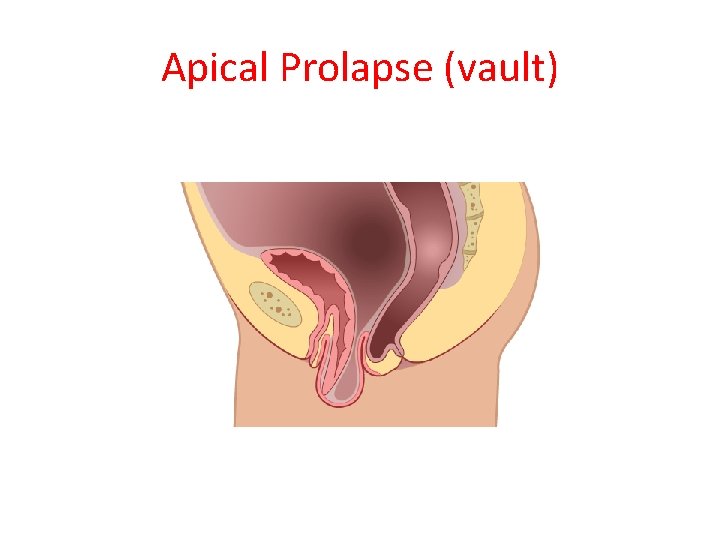
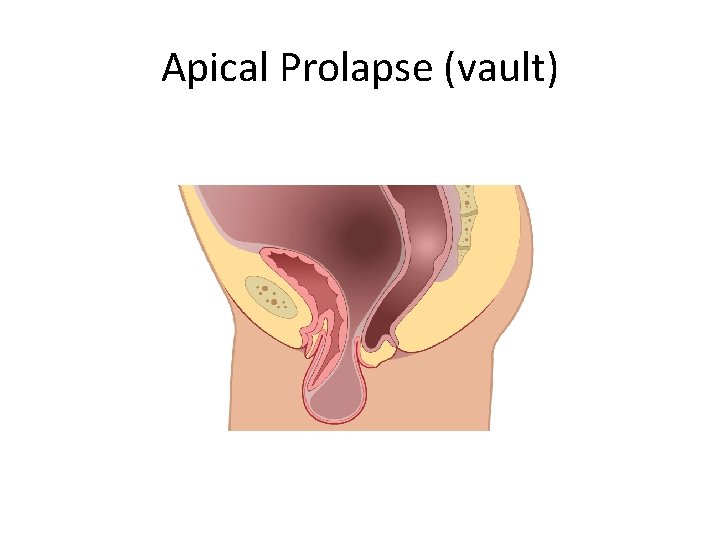
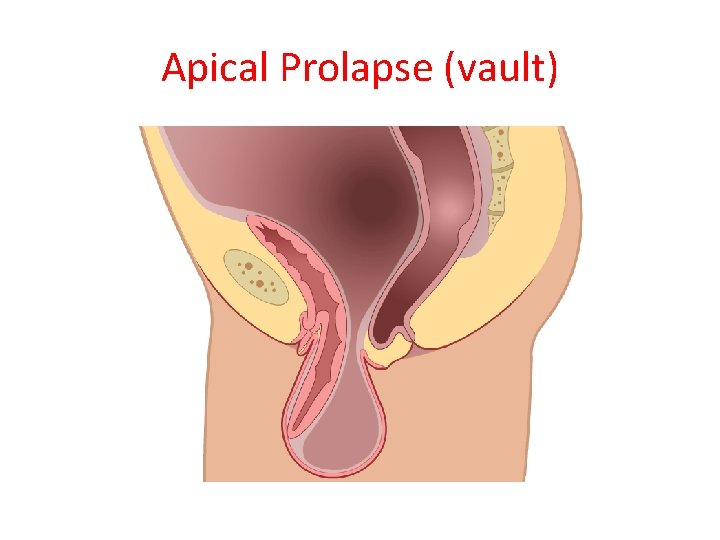
Apical Prolapse (vault)
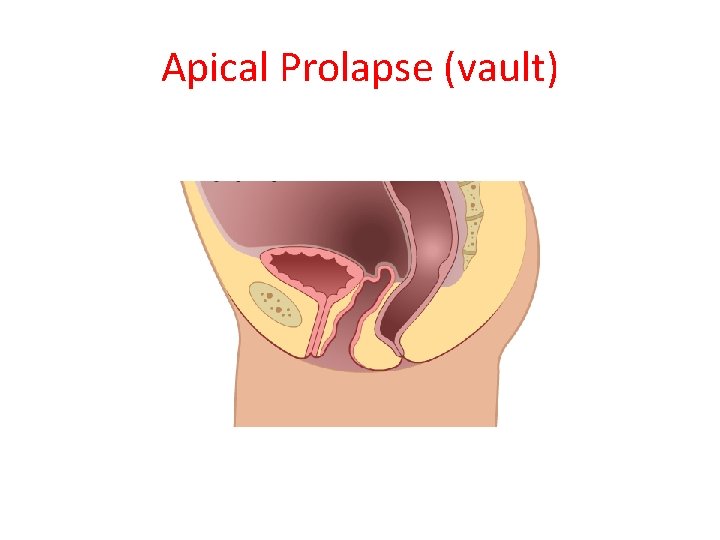
Apical Prolapse (vault)
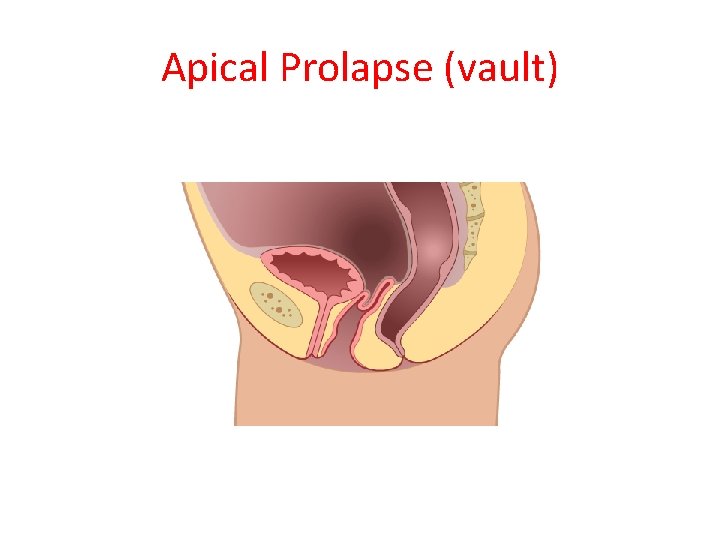
Apical Prolapse (vault)
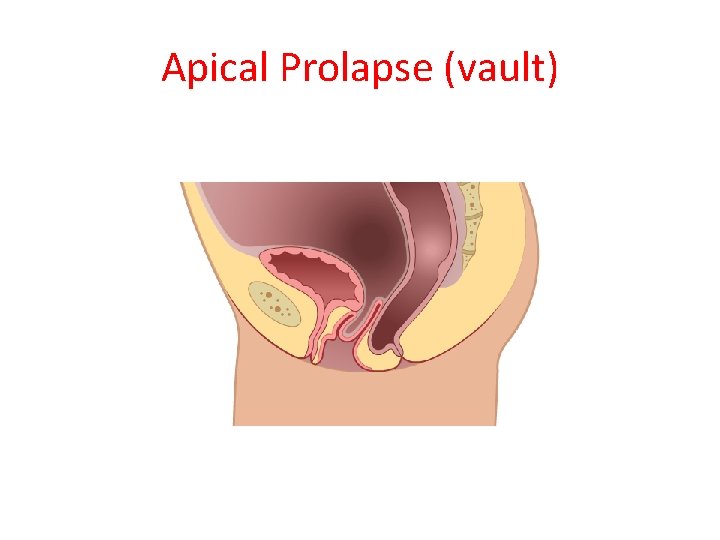
Apical Prolapse (vault)
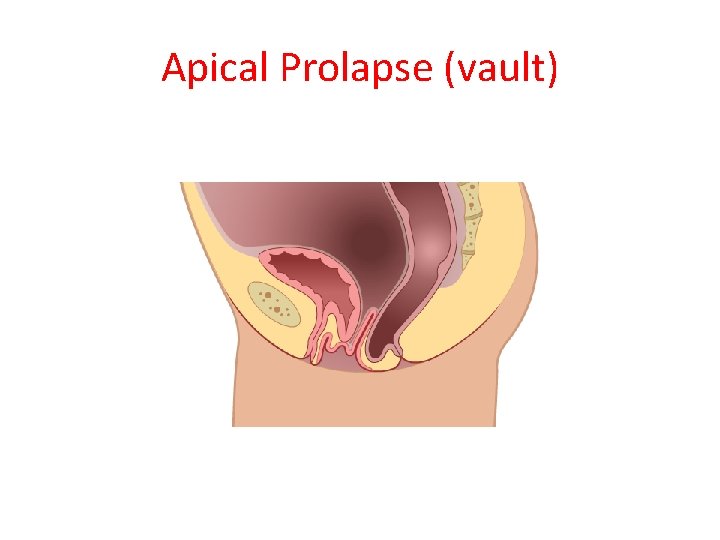
Apical Prolapse (vault)
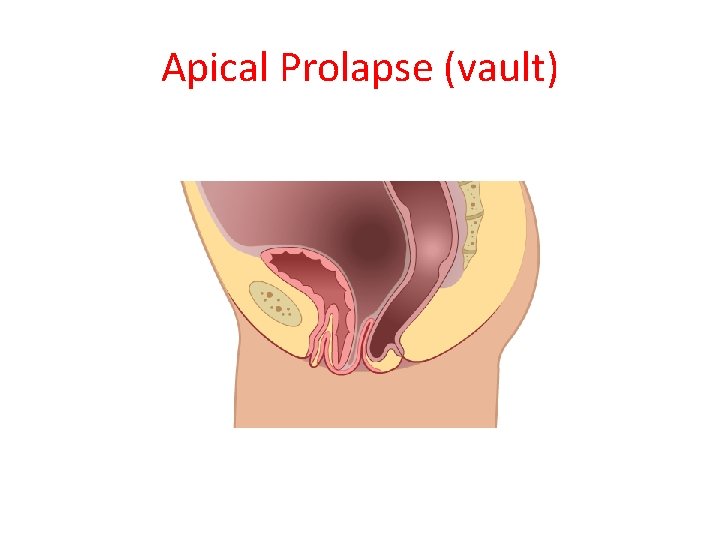
Apical Prolapse (vault)
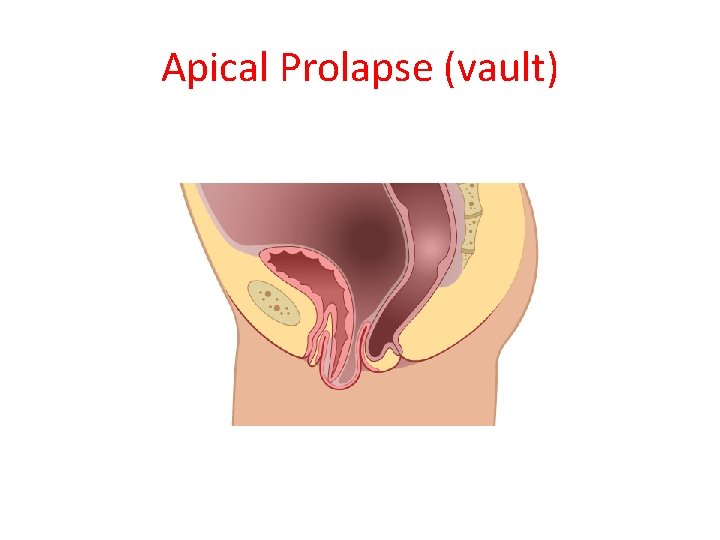
Apical Prolapse (vault)
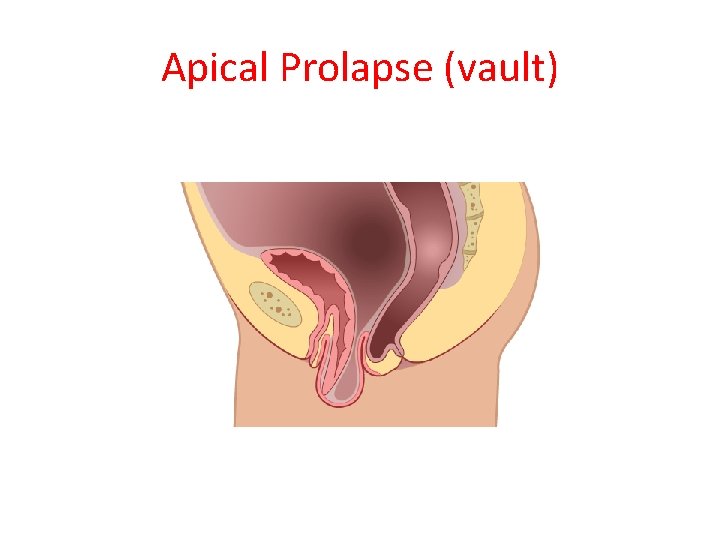
Apical Prolapse (vault)
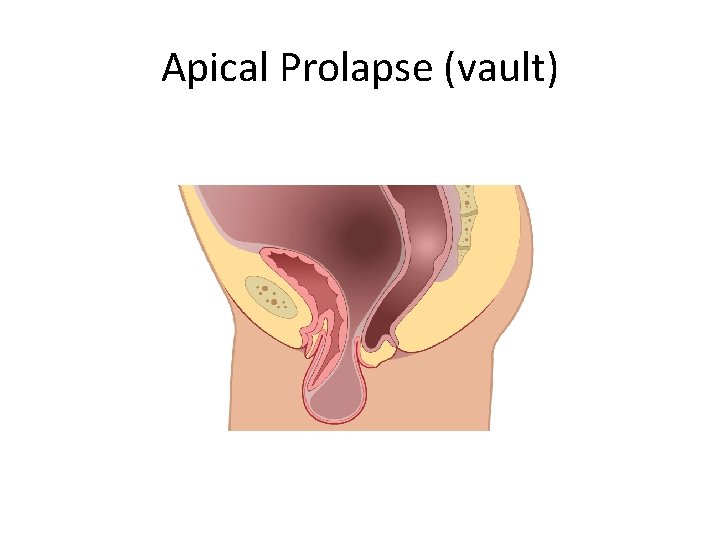
Apical Prolapse (vault)
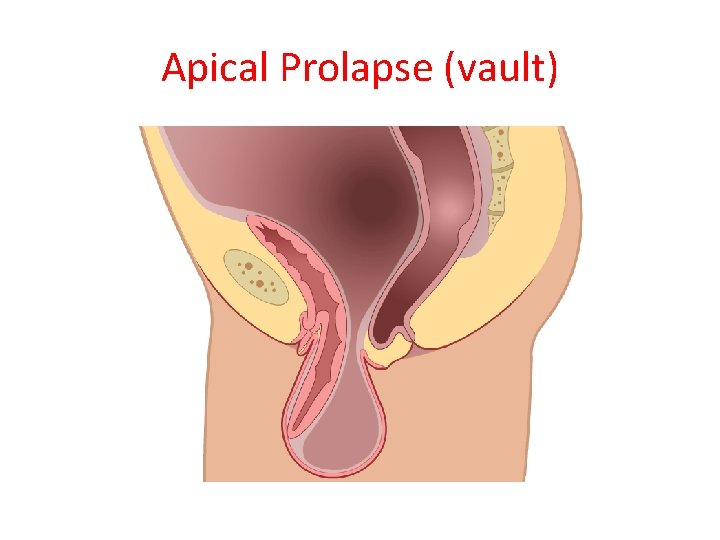
Apical Prolapse (vault)

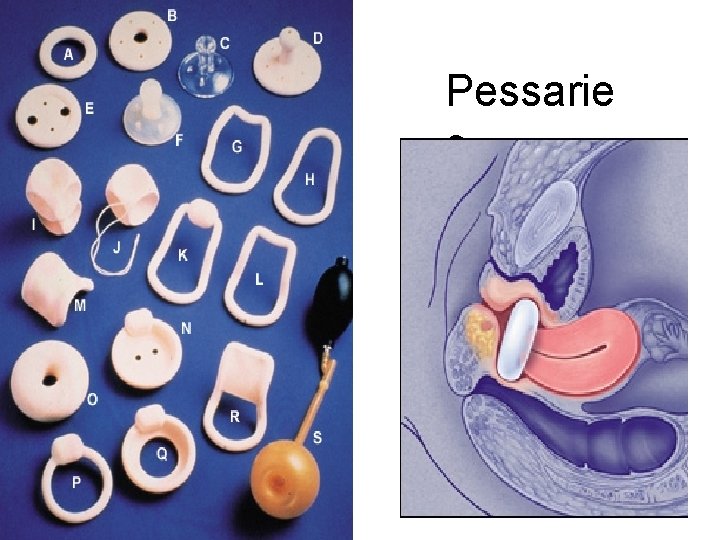
Are effective non-surgical treatments available for women with pelvic organ prolapse • Pessary. • Pelvic Floor Muscle Rehabilitation. • Symptom-Directed Therapy No data supporting their use to prevent prolapse progression.
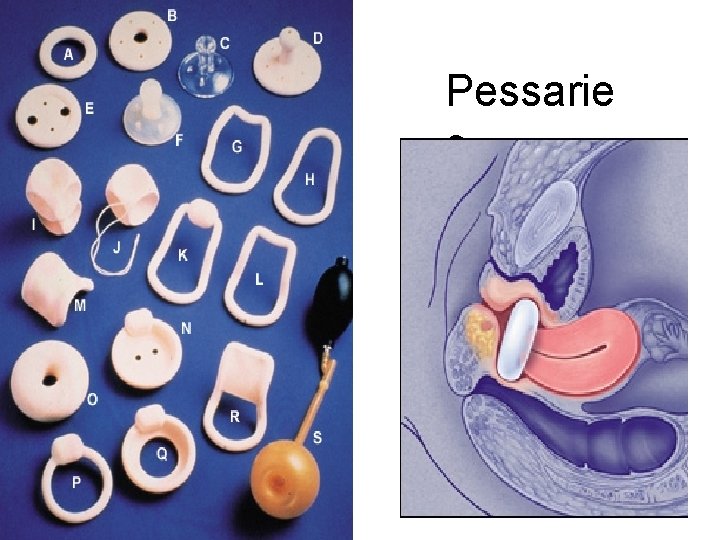
Pessarie s
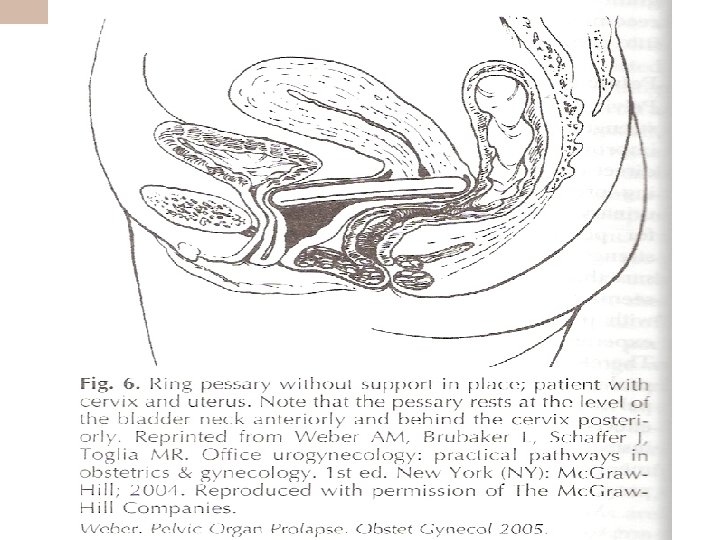
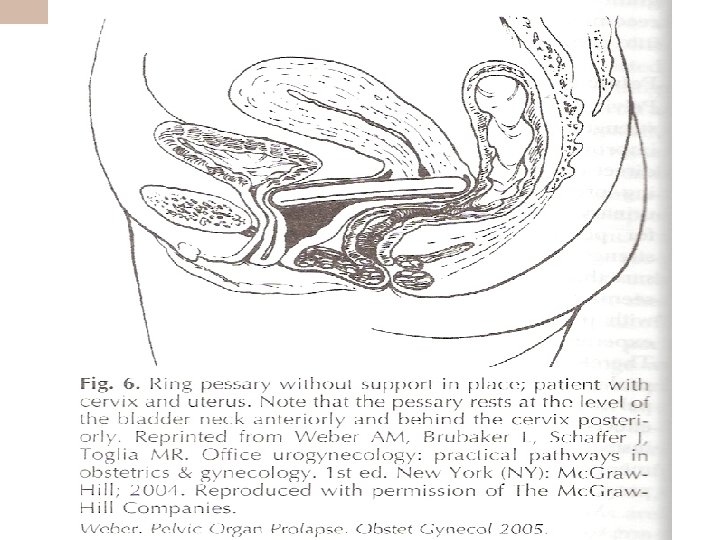
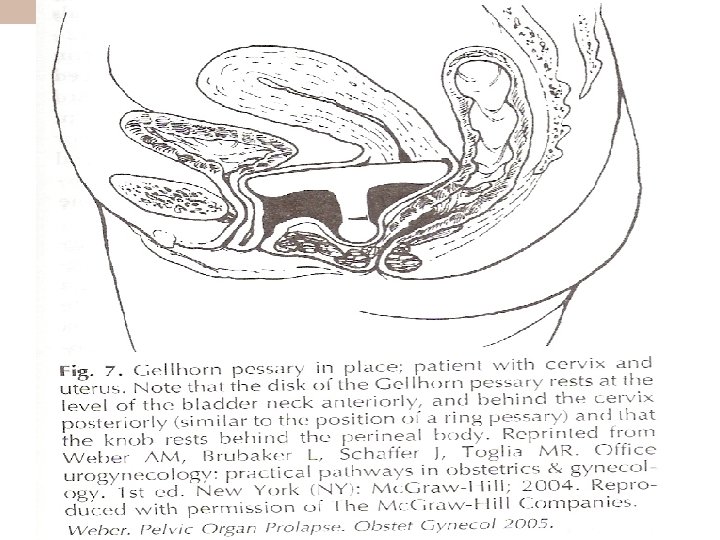
Nonsurgical Management
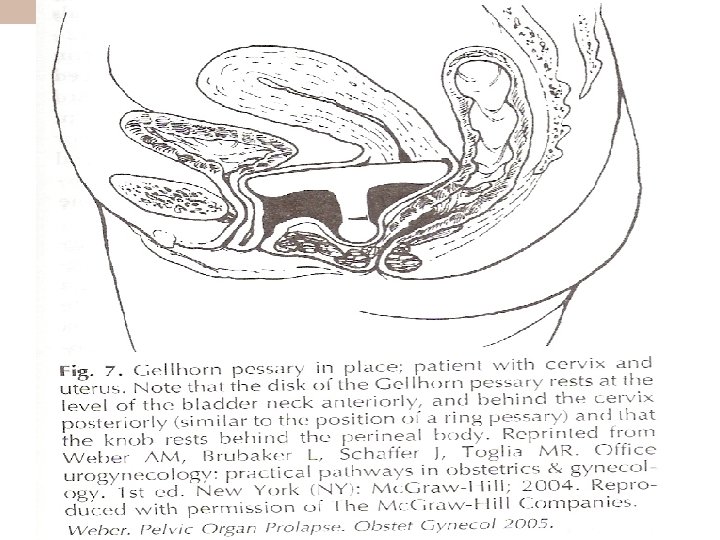
Nonsurgical Management
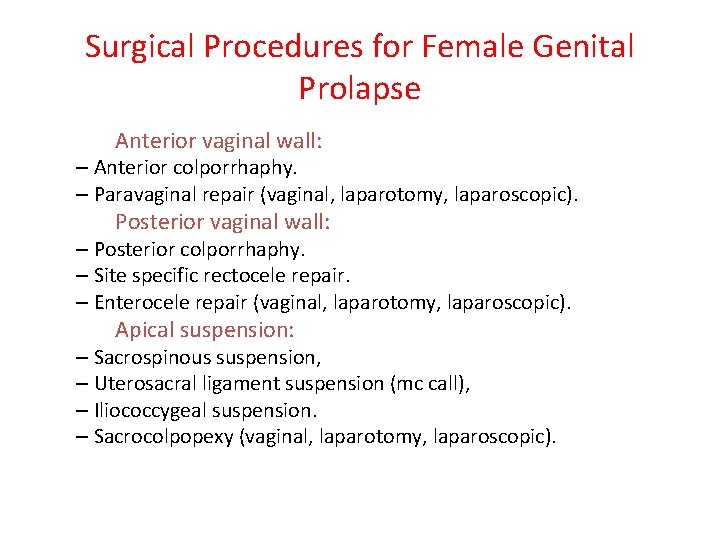
Surgical Procedures for Female Genital Prolapse Anterior vaginal wall: – Anterior colporrhaphy. – Paravaginal repair (vaginal, laparotomy, laparoscopic). Posterior vaginal wall: – Posterior colporrhaphy. – Site specific rectocele repair. – Enterocele repair (vaginal, laparotomy, laparoscopic). Apical suspension: – Sacrospinous suspension, – Uterosacral ligament suspension (mc call), – Iliococcygeal suspension. – Sacrocolpopexy (vaginal, laparotomy, laparoscopic).
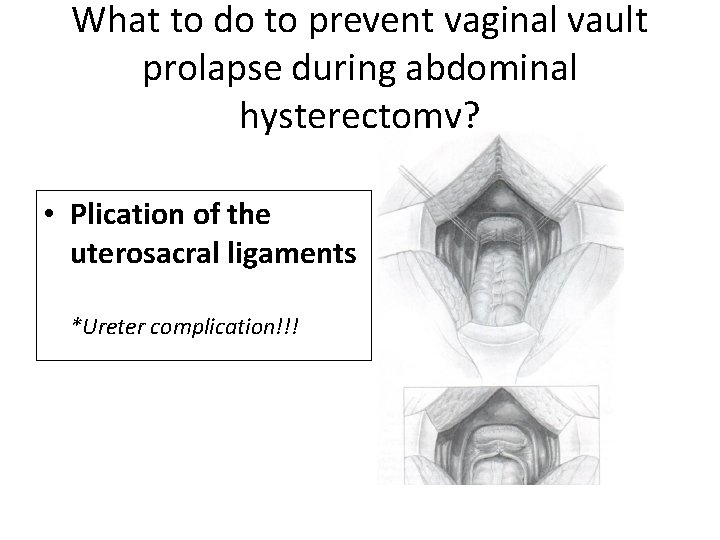
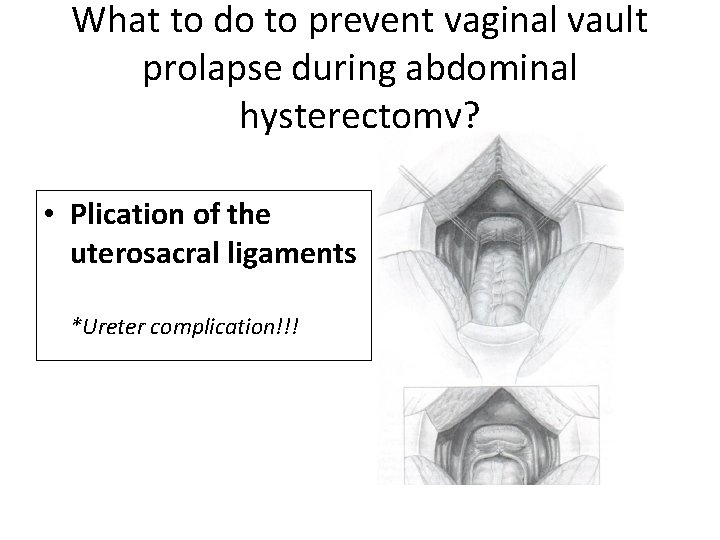
What to do to prevent vaginal vault prolapse during abdominal hysterectomy? • Plication of the uterosacral ligaments *Ureter complication!!!
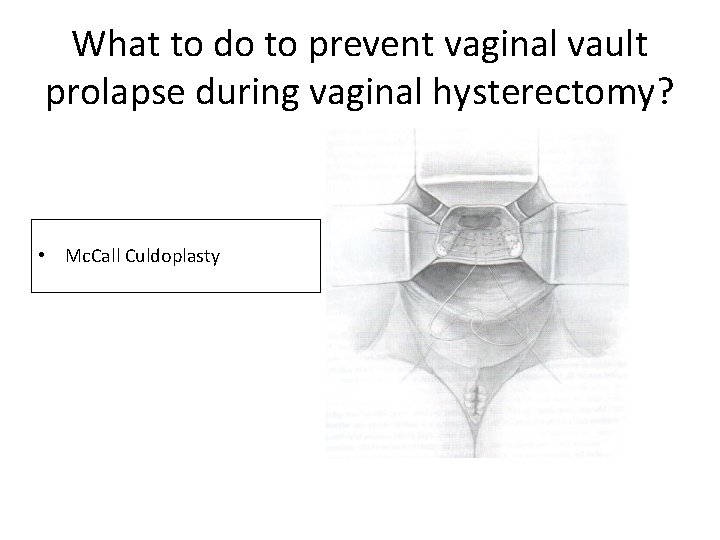
What to do to prevent vaginal vault prolapse during vaginal hysterectomy? • Mc. Call Culdoplasty
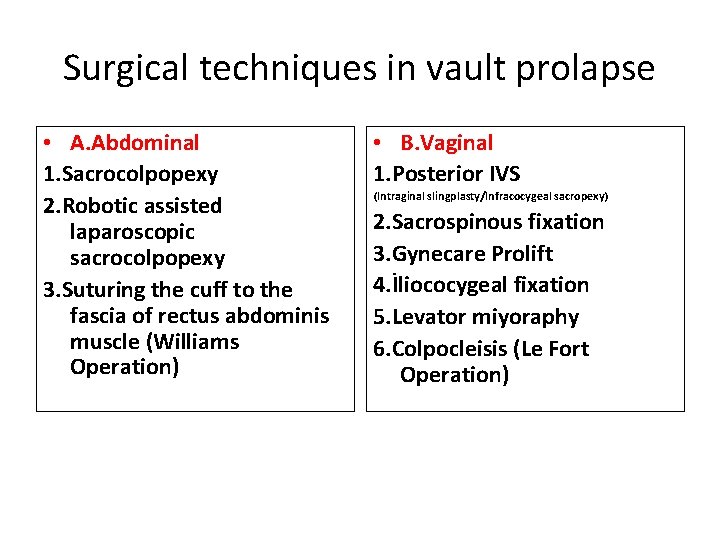
Surgical techniques in vault prolapse • A. Abdominal 1. Sacrocolpopexy 2. Robotic assisted laparoscopic sacrocolpopexy 3. Suturing the cuff to the fascia of rectus abdominis muscle (Williams Operation) • B. Vaginal 1. Posterior IVS (Intraginal slingplasty/Infracocygeal sacropexy) 2. Sacrospinous fixation 3. Gynecare Prolift 4. İliococygeal fixation 5. Levator miyoraphy 6. Colpocleisis (Le Fort Operation)
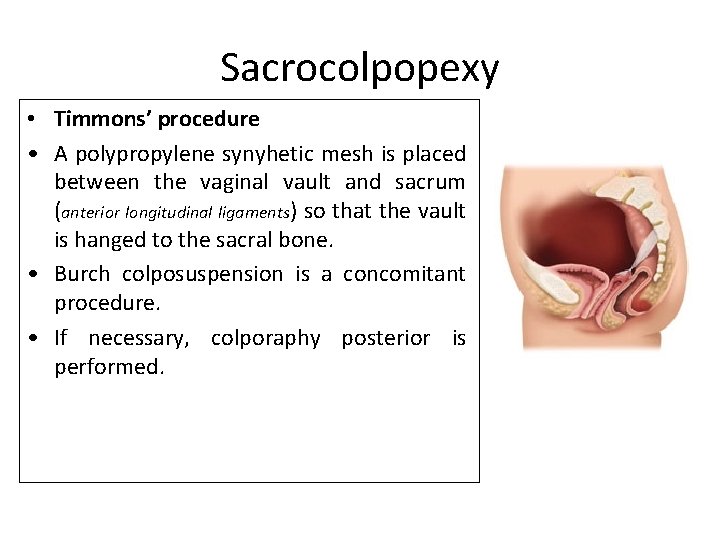
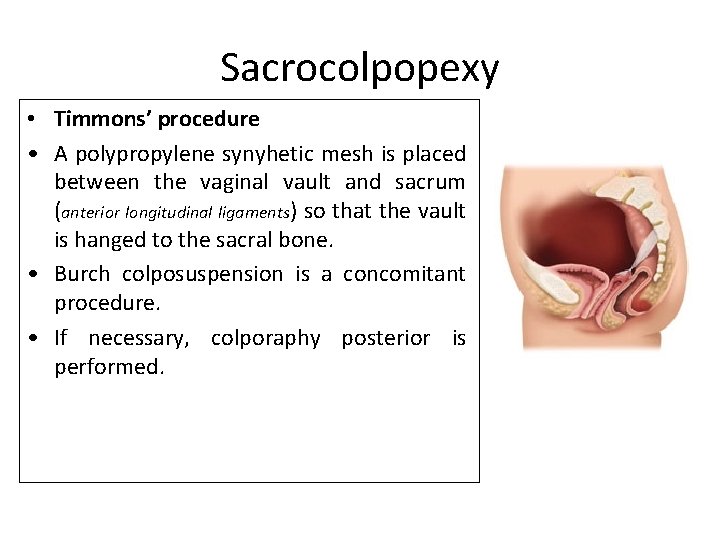
Sacrocolpopexy • Timmons’ procedure • A polypropylene synyhetic mesh is placed between the vaginal vault and sacrum (anterior longitudinal ligaments) so that the vault is hanged to the sacral bone. • Burch colposuspension is a concomitant procedure. • If necessary, colporaphy posterior is performed.
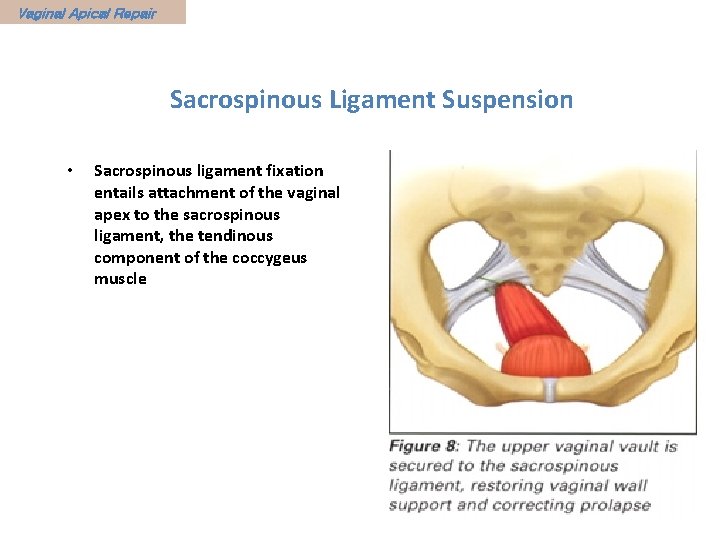
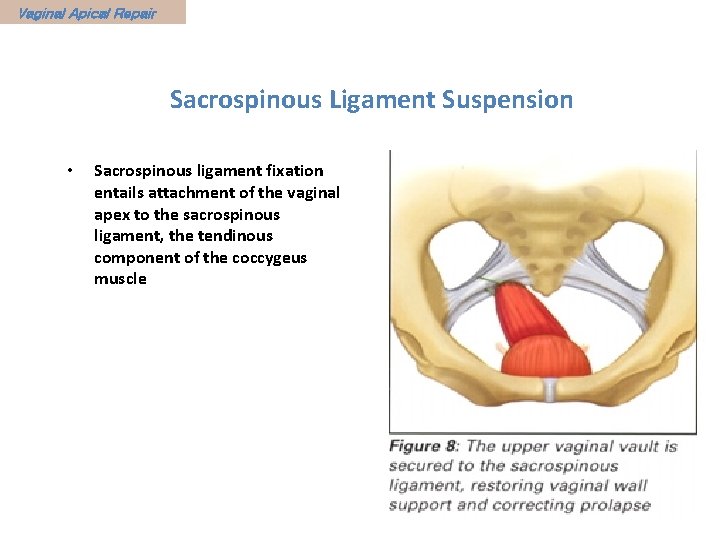
Vaginal Apical Repair Sacrospinous Ligament Suspension • Sacrospinous ligament fixation entails attachment of the vaginal apex to the sacrospinous ligament, the tendinous component of the coccygeus muscle
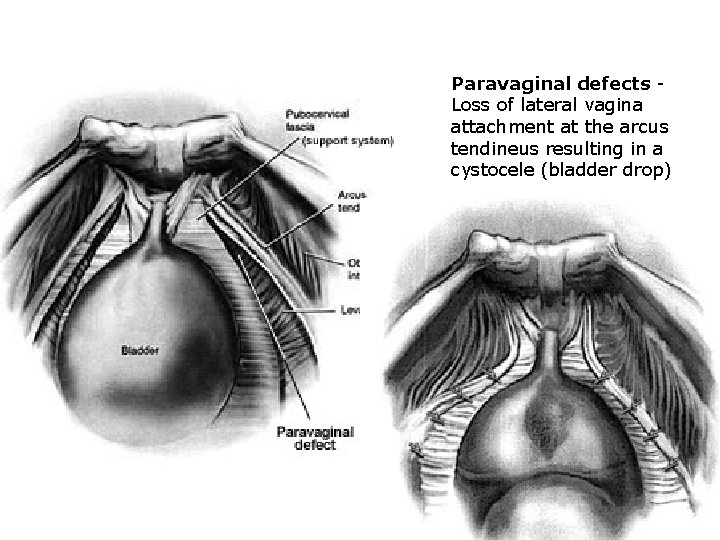
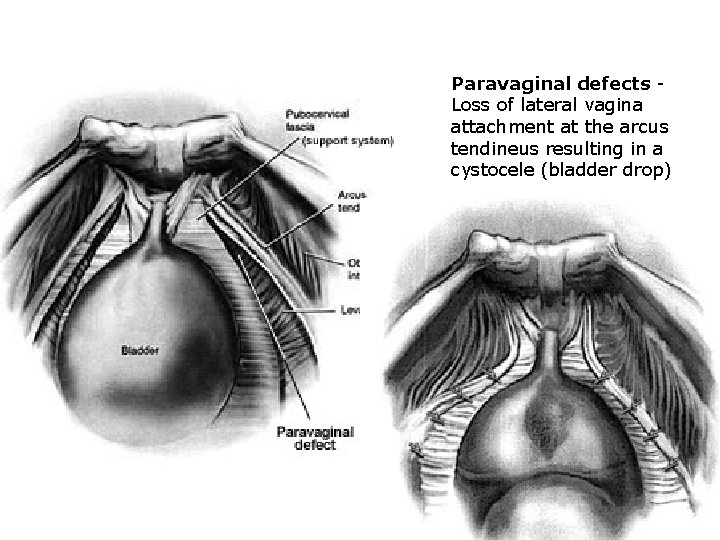
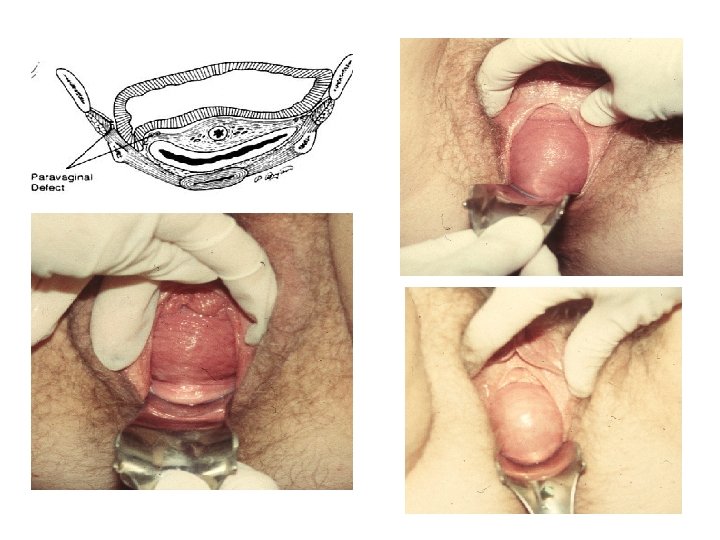
Paravaginal defects Loss of lateral vagina attachment at the arcus tendineus resulting in a cystocele (bladder drop)
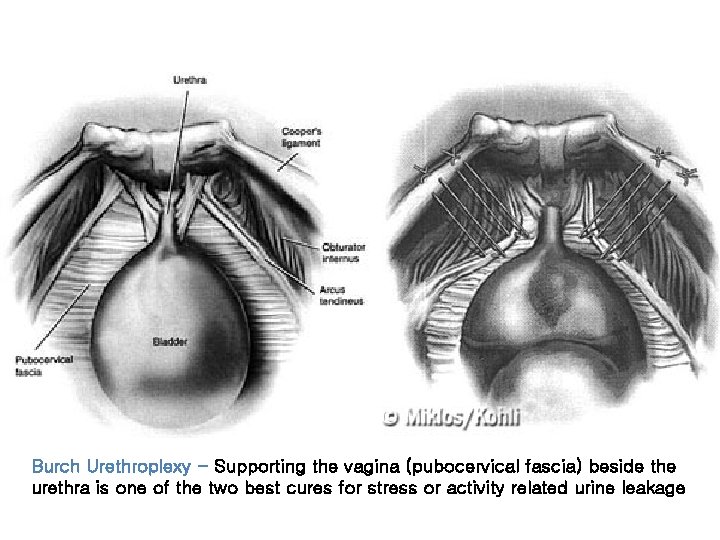
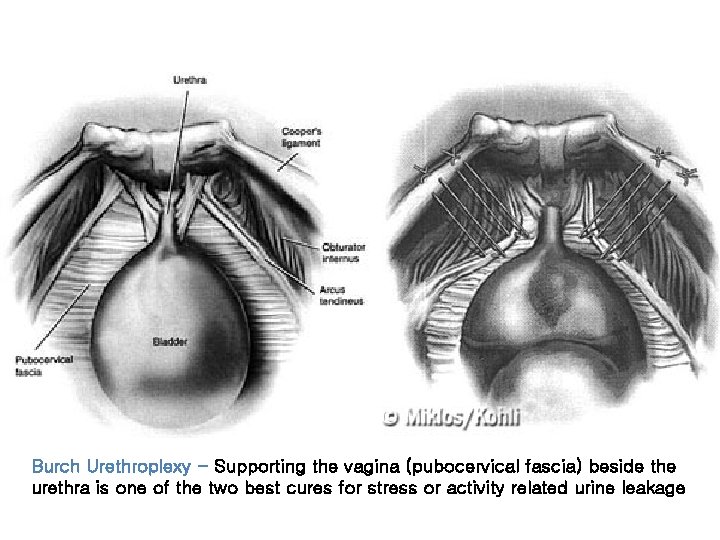
Burch Urethroplexy - Supporting the vagina (pubocervical fascia) beside the urethra is one of the two best cures for stress or activity related urine leakage