Peeing is a wonderful thing Acute Hemodialysis Jennifer













- Slides: 54

Peeing is a wonderful thing
Acute Hemodialysis Jennifer Stoddard Klenzak, MD Pinehurst Nephrology Associates 5/24/2011
w Who receives dialysis in the hospital? Acute kidney injury ESRD patients different populations, needs, meds, prescriptions for dialysis
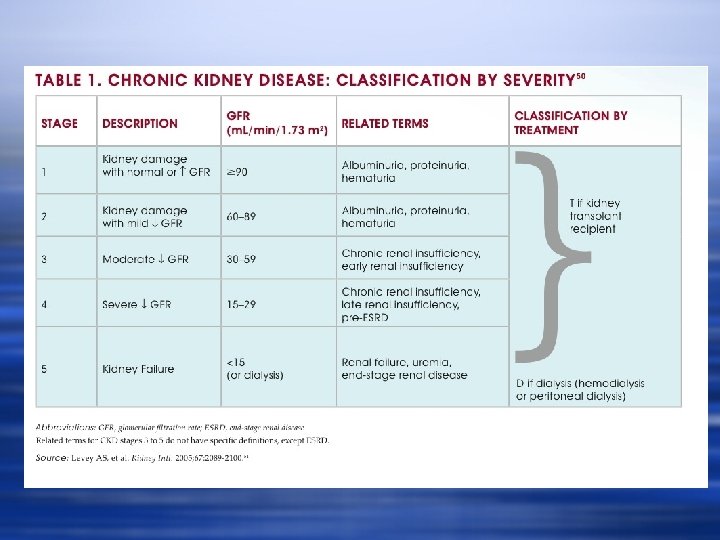
What is Acute Kidney Injury? w Decrease in GFR w Relative loss of clearance w And why do we care?
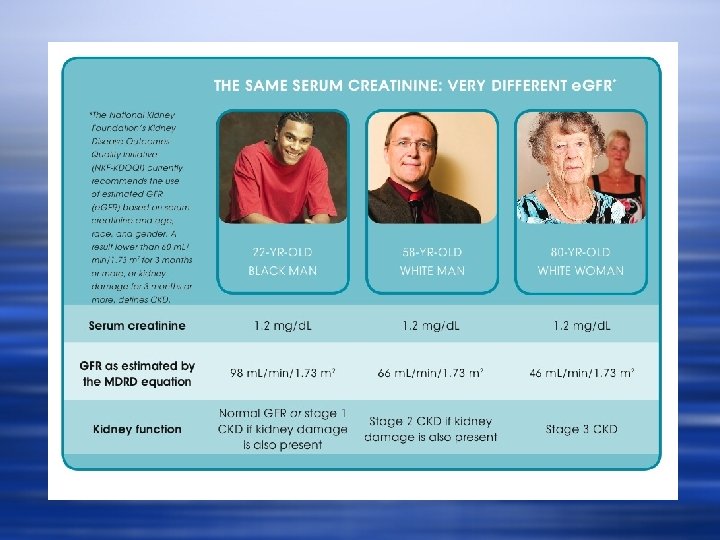
w Insert image

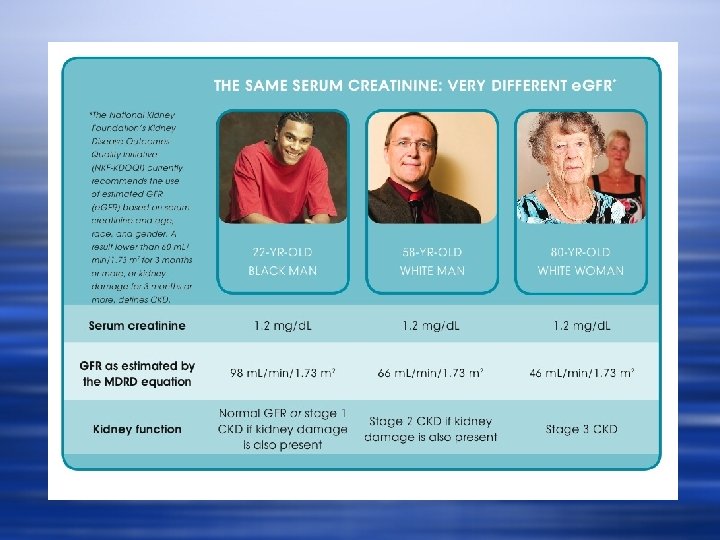
Variables affecting creatinine besides GFR w w w w Malnutrition Liver disease Pregnancy Body habitus Ethnicity Vegetarianism Volume status Age
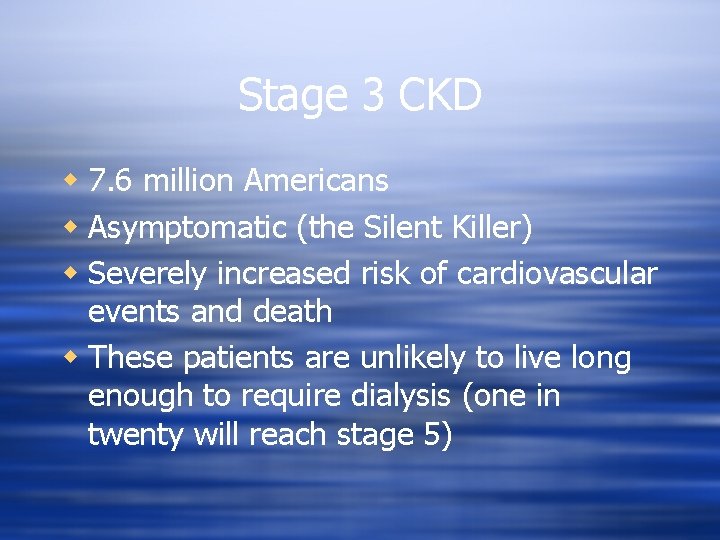
Stage 3 CKD w 7. 6 million Americans w Asymptomatic (the Silent Killer) w Severely increased risk of cardiovascular events and death w These patients are unlikely to live long enough to require dialysis (one in twenty will reach stage 5)



Causes of AKI w Acute Tubular Necrosis w Prolonged ischemic injury w Contrast nephropathy w SIRS w “post-operative” AKI w Other derangements of homeostasis leading to toxic or ischemic injury
w Systemic Inflammatory Response Syndrome w Release of interleukins, oxidative metabolites w Injury to renal tubular epithelial cells w Decreased perfusion related to hypotension
Causes of AKI, cont. w Rhabdomyolysis w Statin-induced w Heat stroke w Muscle injury w “Found down” w Compartment syndrome w Trauma
w Poisoning/Toxins/Overdose w Aspirin w Antifreeze/Ethylene glycol w Methanol w Hyperuricemia w Tumor Lysis Syndrome

w Rapidly Progressive Glomerulonephritis w Anca-associated disease w Lupus Nephritis w Goodpasture’s Syndrome (Anti-glomerular basement Antibody Syndrome) w Ig. A w Cryoglobulinemic Vasculitis w Myeloma Kidney w Cast nephropathy

Indications for hemodialysis w w w w Volume Overload Hyperkalemia Uremia Encephalopathy Pericarditis Metabolic Acidosis Toxin clearance Platelet dysfunction

Dialysis Prescription w Indication w Hemodynamic status w Chronicity of illness w Comorbidities

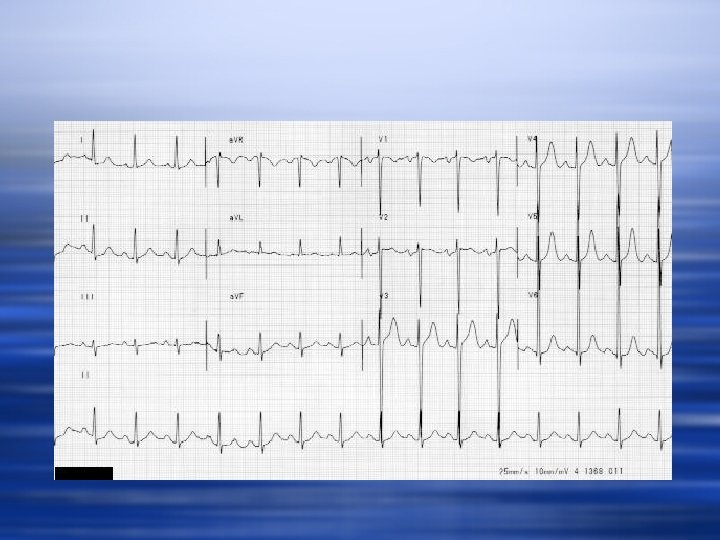
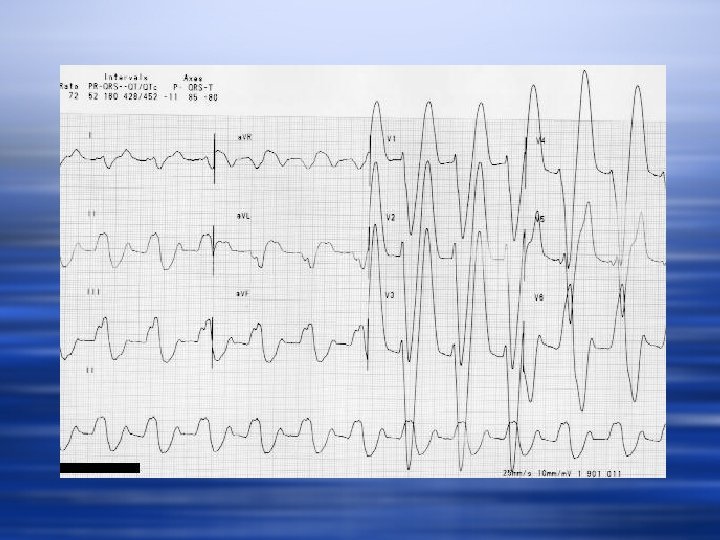
Case 1 w 52 year old female ESRD, MWF, patient missed Friday treatment. Saturday night presents to the ED with complaints of weakness.
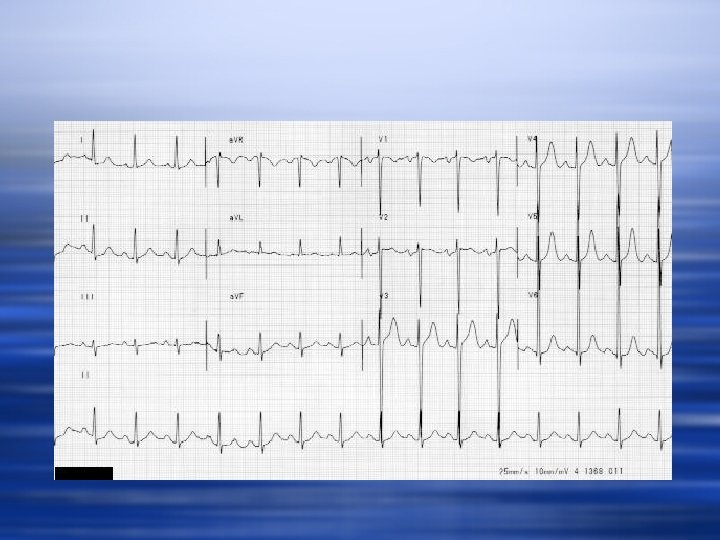
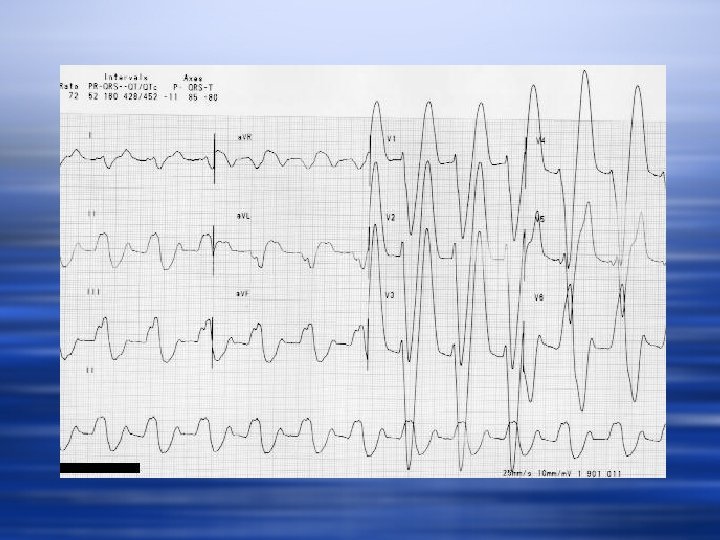
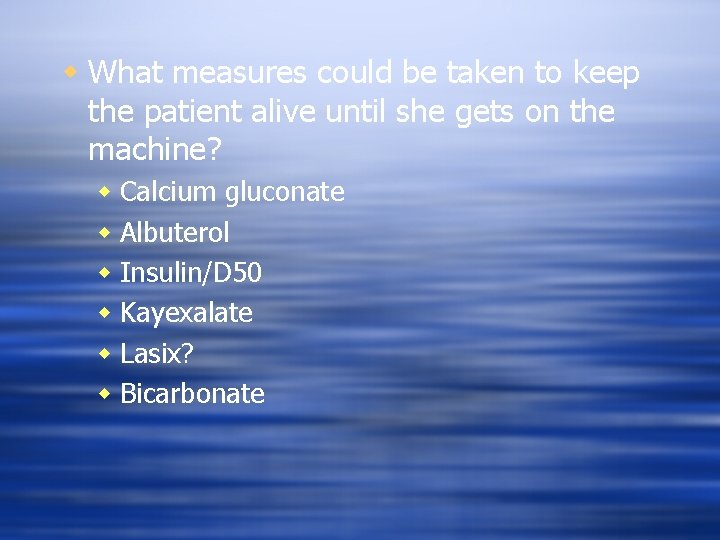
w What measures could be taken to keep the patient alive until she gets on the machine?
w What measures could be taken to keep the patient alive until she gets on the machine? w Calcium gluconate w Albuterol w Insulin/D 50 w Kayexalate w Lasix? w Bicarbonate
w What is the most likely complication of this acute dialysis treatment? w How can the dialysis prescription decrease the risk of this event?
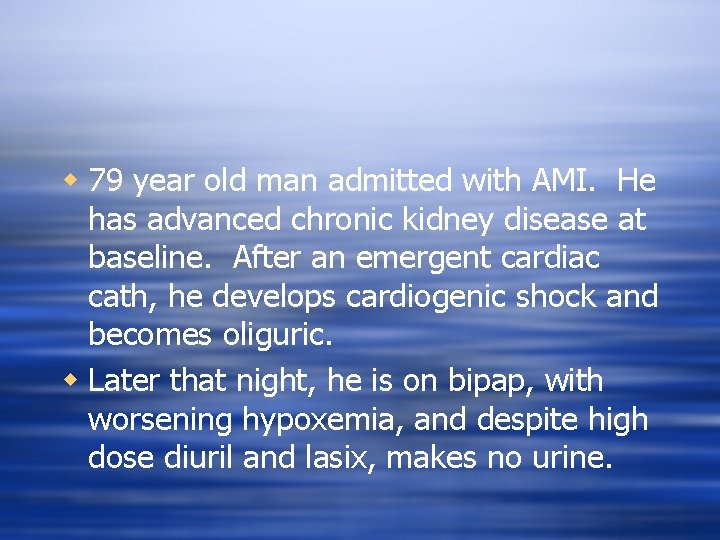
w 79 year old man admitted with AMI. He has advanced chronic kidney disease at baseline. After an emergent cardiac cath, he develops cardiogenic shock and becomes oliguric. w Later that night, he is on bipap, with worsening hypoxemia, and despite high dose diuril and lasix, makes no urine.
w Is dialysis indicated? Why? w What is the goal of treatment? w What are the expected risks? w Prescription?
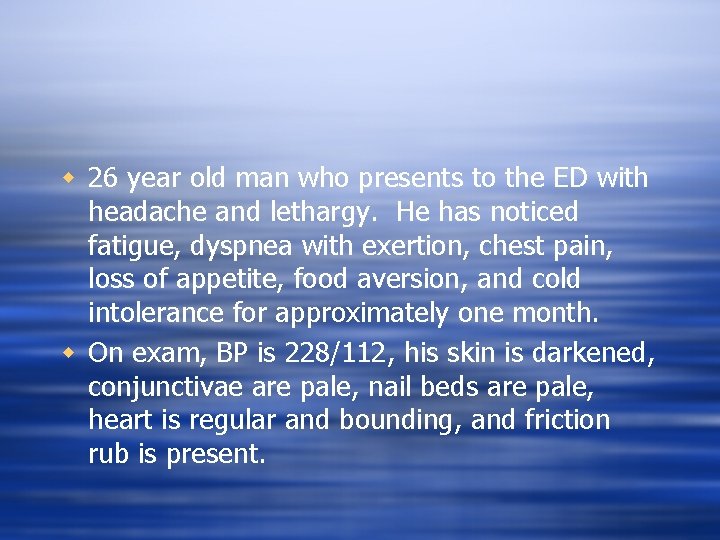
w 26 year old man who presents to the ED with headache and lethargy. He has noticed fatigue, dyspnea with exertion, chest pain, loss of appetite, food aversion, and cold intolerance for approximately one month. w On exam, BP is 228/112, his skin is darkened, conjunctivae are pale, nail beds are pale, heart is regular and bounding, and friction rub is present.
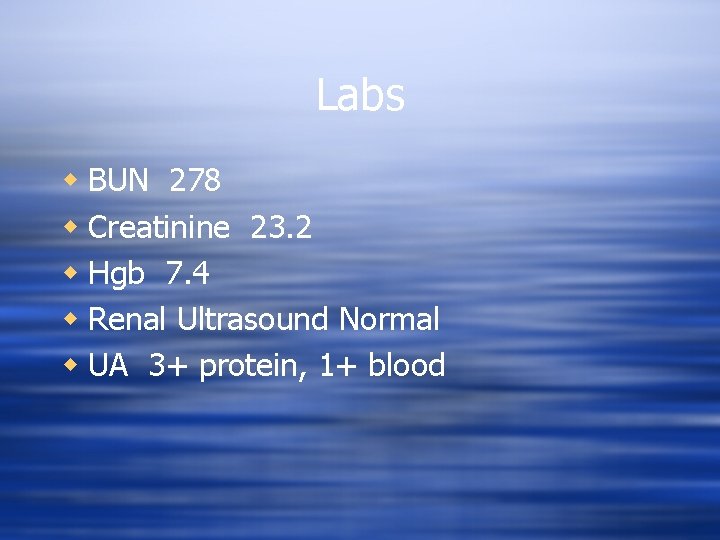
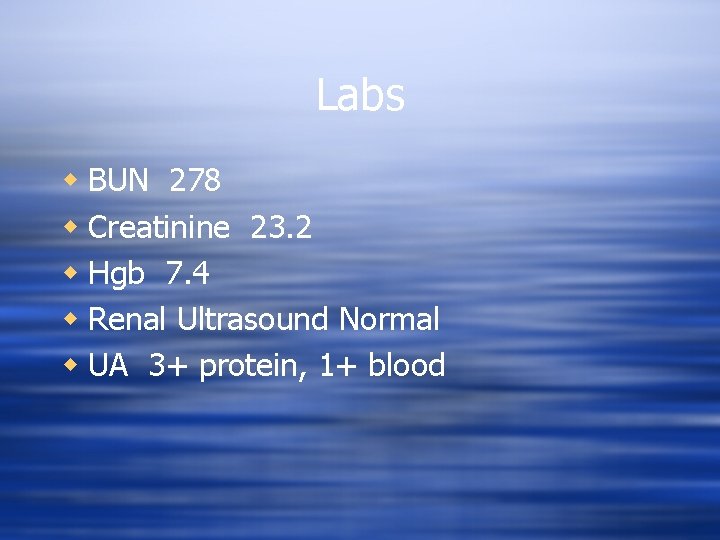
Labs w BUN 278 w Creatinine 23. 2 w Hgb 7. 4 w Renal Ultrasound Normal w UA 3+ protein, 1+ blood
w Is dialysis indicated? Why? w Is there an expectation of renal recovery? w Potential complications during dialysis? w Prescription?
w 18 year old female admitted with acute renal failure and hemoptysis. w She receives 1000 mg solumedrol and undergoes renal biopsy.
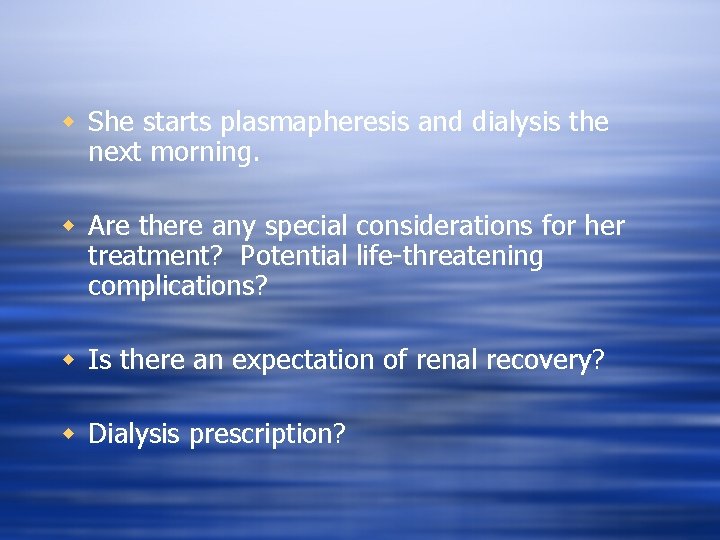
w She starts plasmapheresis and dialysis the next morning. w Are there any special considerations for her treatment? Potential life-threatening complications? w Is there an expectation of renal recovery? w Dialysis prescription?
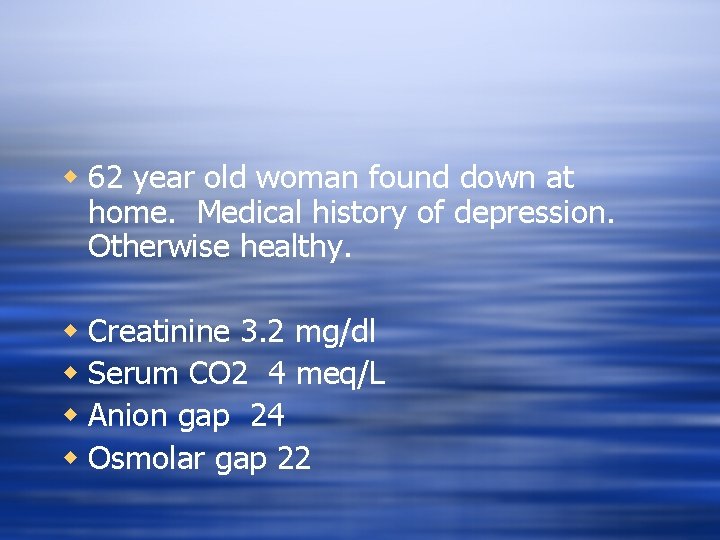
w 62 year old woman found down at home. Medical history of depression. Otherwise healthy. w Creatinine 3. 2 mg/dl w Serum CO 2 4 meq/L w Anion gap 24 w Osmolar gap 22

w Is dialysis indicated? Why? w What other measures should be taken here? w Do we expect renal recovery if she survives?

Interdisciplinary Team Approach to AKI w Nephrologist w Diagnosis and management of renal disease w Access management w Interventional radiologists and nephrologists w Vascular surgeons w General surgeons w Nurse w Floor nurse/ICU nurse w Hemodialysis nurse w PD nurse
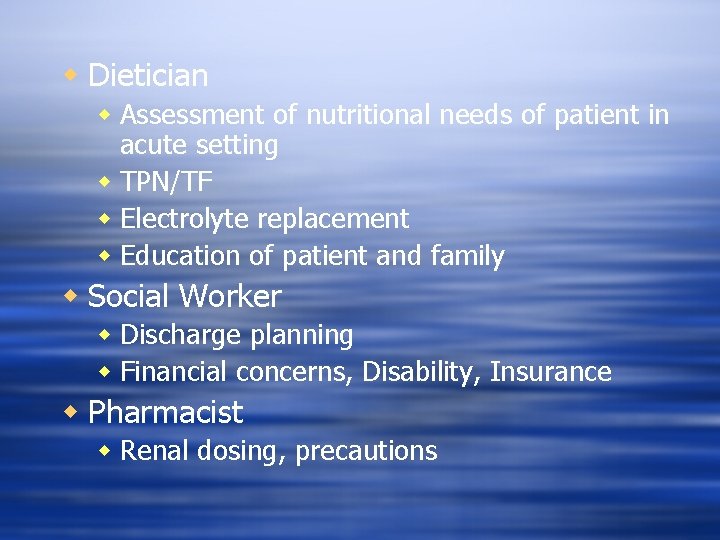
w Dietician w Assessment of nutritional needs of patient in acute setting w TPN/TF w Electrolyte replacement w Education of patient and family w Social Worker w Discharge planning w Financial concerns, Disability, Insurance w Pharmacist w Renal dosing, precautions
AKI: Role of the Nurse
The bedside nurse assessment the key ingredient w w w Blood Pressure Pulse rate Orthostasis Strength Mental Status Fever Oxygen requirements Access Bleeding Vomiting, diarrhea, constipation Cramping

w Ongoing assessments are the integral data w How do the bedside assessments affect the management of the patient? w The dialysis prescription? w Access plans?
w Dialysis Nursing Assessments: with the patient during the riskiest time w w w w Bleeding Hypotension Tachyarrhythmias Seizure Loss of consciousness Cramping Pain Access assessment
AKI Dialysis Nursing Interventions w w w Fluids Medications Changes in Qb Lytic instillation for catheters Removing catheters Stopping treatment w Returning blood
AKI Pharmacology w “Nephrotoxic Agents” w NSAIDS w Iodinated Contrast Dye w Gentamicin w IV acyclovir
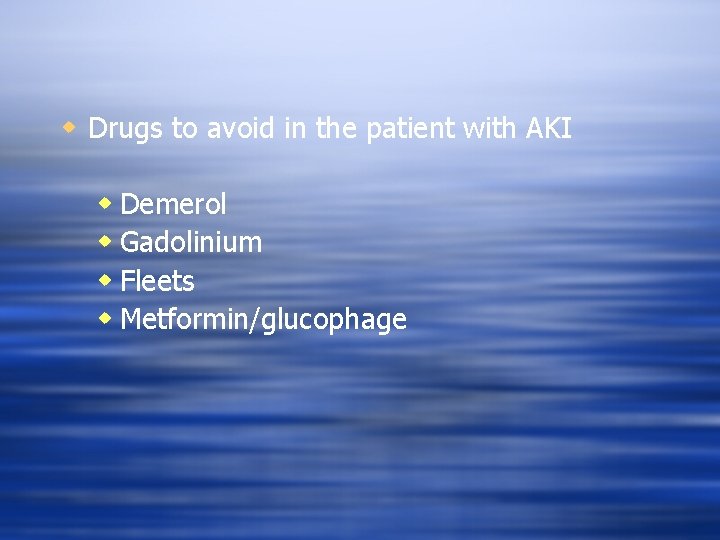
w Drugs to avoid in the patient with AKI w Demerol w Gadolinium w Fleets w Metformin/glucophage
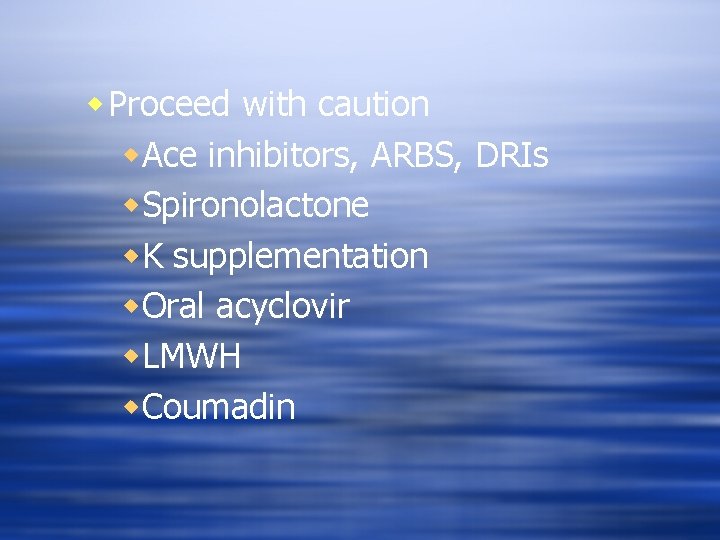
w Proceed with caution w. Ace inhibitors, ARBS, DRIs w. Spironolactone w. K supplementation w. Oral acyclovir w. LMWH w. Coumadin
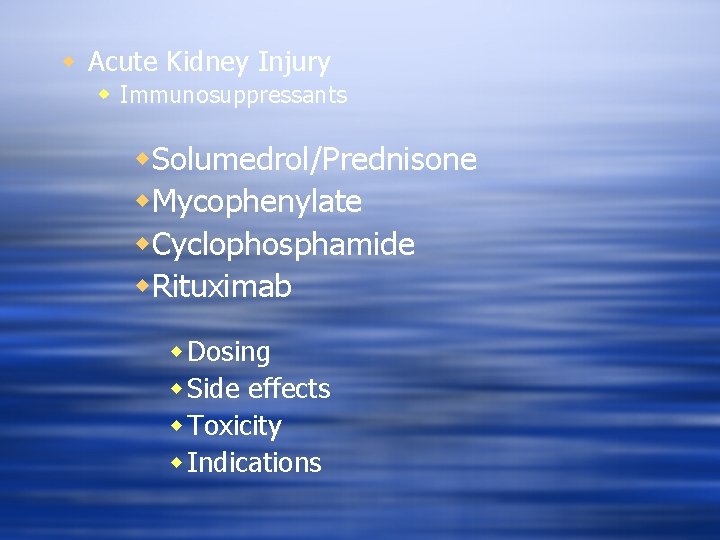
w Acute Kidney Injury w Immunosuppressants w. Solumedrol/Prednisone w. Mycophenylate w. Cyclophosphamide w. Rituximab w Dosing w Side effects w Toxicity w Indications

w IVF w When to give? w Compositions w Bicarbonate based solutions w Rhabdomyolysis w Tumor Lysis Syndrome w Metabolic acidosis w Diuretics w Loop diuretics w Thiazides w Acetozolamide w Antihypertensives w Others w Rasburicase w Fomepizole
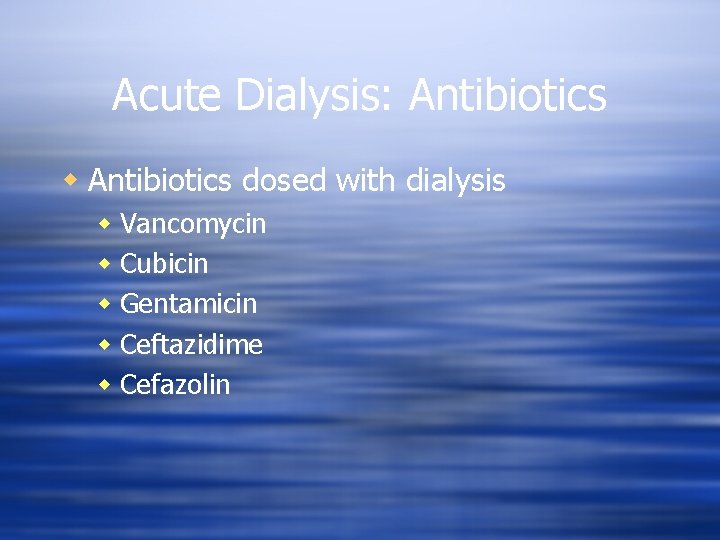
Acute Dialysis: Antibiotics w Antibiotics dosed with dialysis w Vancomycin w Cubicin w Gentamicin w Ceftazidime w Cefazolin
Acute Dialysis: ESAs w Epogen, Aranesp, Procrit w Iron Supplementation w Oral vs. IV w To give or not to give in the acute setting? w Pressure from outpatient units to “keep hgb in goal range” at discharge
Bone and Mineral Metabolism w Vitamin D 3 w Activated Vitamin D w Binders w Calcium-based vs. calcium-free w Calcimimetics (Sensipar) w Calciphylaxis w Thiosulfate w Bisphosphanates
Transition to Chronic Setting w Communication between Acute Dialysis Nurse and Outpatient Dialysis Nurse w Crucial for success w What was patient’s diagnosis during hospitalization? w For the outpatient nurse: w How will the hospitalization affect the outpatient dialysis prescription? w If the patient is actively listed for transplant, how does this event affect his/her candidacy?
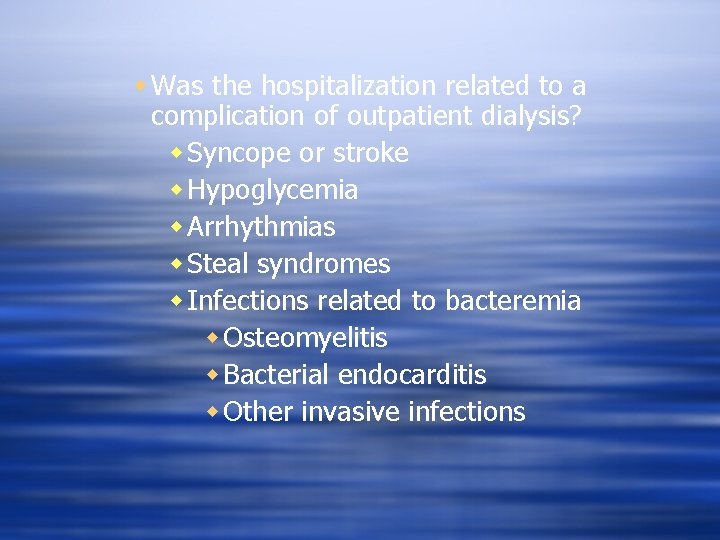
w Was the hospitalization related to a complication of outpatient dialysis? w Syncope or stroke w Hypoglycemia w Arrhythmias w Steal syndromes w Infections related to bacteremia w Osteomyelitis w Bacterial endocarditis w Other invasive infections
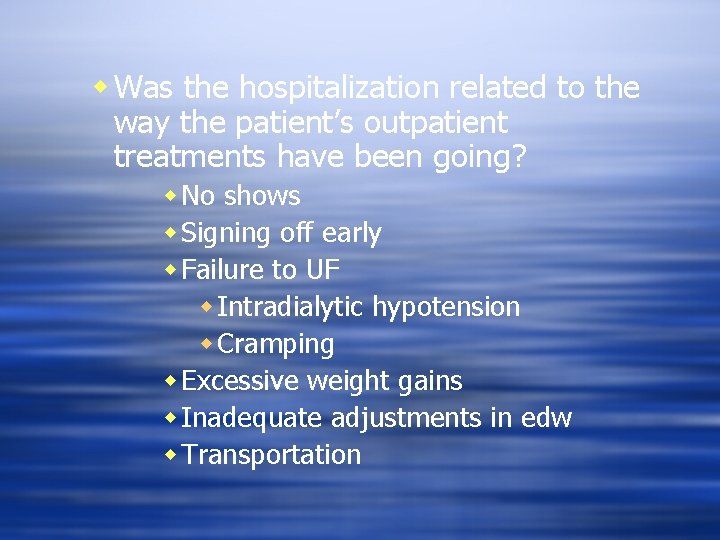
w Was the hospitalization related to the way the patient’s outpatient treatments have been going? w No shows w Signing off early w Failure to UF w Intradialytic hypotension w Cramping w Excessive weight gains w Inadequate adjustments in edw w Transportation
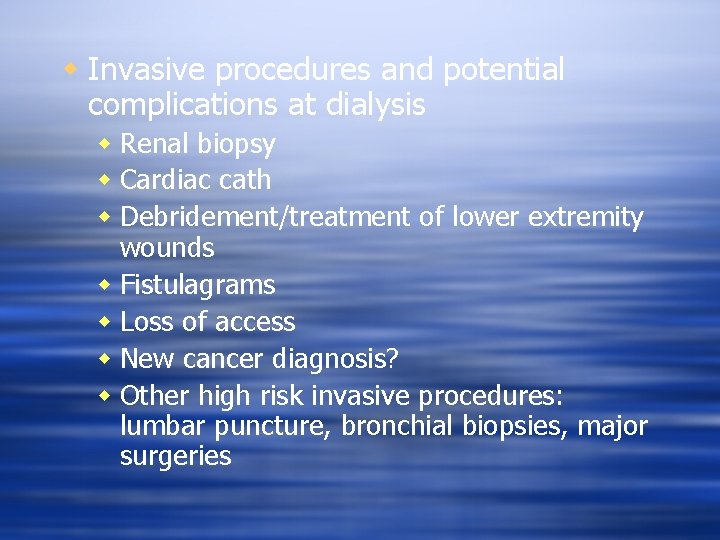
w Invasive procedures and potential complications at dialysis w Renal biopsy w Cardiac cath w Debridement/treatment of lower extremity wounds w Fistulagrams w Loss of access w New cancer diagnosis? w Other high risk invasive procedures: lumbar puncture, bronchial biopsies, major surgeries
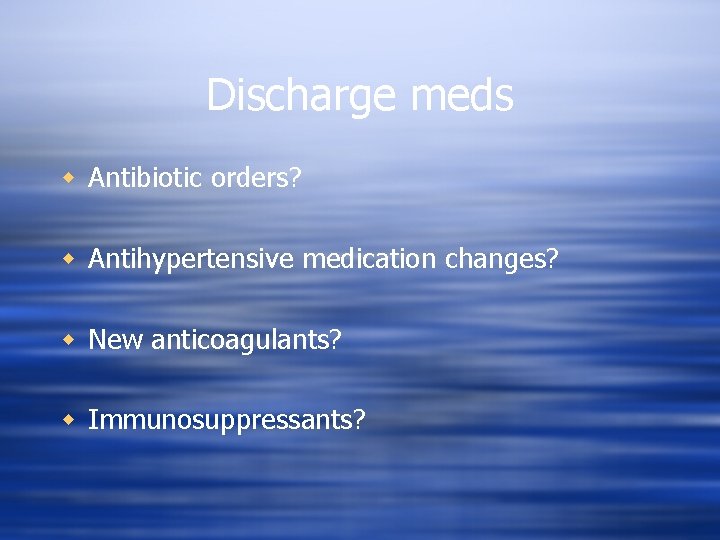
Discharge meds w Antibiotic orders? w Antihypertensive medication changes? w New anticoagulants? w Immunosuppressants?
Summary w Acute hemodialysis creates specific needs related to optimal patient outcome and patient safety w Protection of renal function and chances of recovery w High risk medications and procedures w Transition to outpatient setting w Short and long term outcomes perspective
GO HEELS!!!!
 It a wonderful world no need to run and hide
It a wonderful world no need to run and hide Wonderful so wonderful is your unfailing love
Wonderful so wonderful is your unfailing love Wonderful wonderful jesus
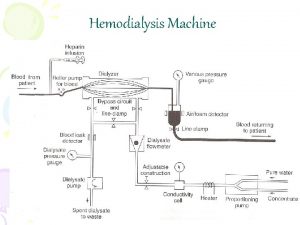
Wonderful wonderful jesus Hemodialysis machine parts and function
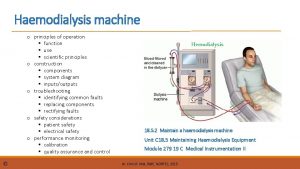
Hemodialysis machine parts and function Haemodialysis
Haemodialysis Hemodialysis cito indication
Hemodialysis cito indication Urea reduction ratio formula
Urea reduction ratio formula Hd ultrafiltration
Hd ultrafiltration Hemosorption vs hemodialysis
Hemosorption vs hemodialysis If you want joy real joy wonderful joy
If you want joy real joy wonderful joy The wonderful name of jesus
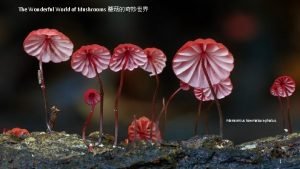
The wonderful name of jesus The wonderful world of mushrooms
The wonderful world of mushrooms What a wonderful performance
What a wonderful performance Wonderful plan
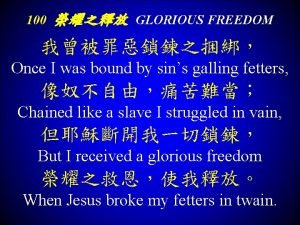
Wonderful plan Glorious freedom wonderful freedom
Glorious freedom wonderful freedom The wonderful cross
The wonderful cross Marvelous monday terrific tuesday wonderful wednesday
Marvelous monday terrific tuesday wonderful wednesday Dynamics of what a wonderful world
Dynamics of what a wonderful world What a wonderful change
What a wonderful change I hope you had a great summer break
I hope you had a great summer break Come
Come A wonderful savior is jesus my lord
A wonderful savior is jesus my lord Quavers marvellous world of music
Quavers marvellous world of music Lewis carroll wonderful
Lewis carroll wonderful He hideth my soul
He hideth my soul Irregular adverbs of manner
Irregular adverbs of manner Internet is a wonderful
Internet is a wonderful The wonderful world of computers
The wonderful world of computers Isnt the love of jesus something wonderful
Isnt the love of jesus something wonderful Is proudly a adverb
Is proudly a adverb Mary devenport o'neill poems
Mary devenport o'neill poems Cats make wonderful house pets
Cats make wonderful house pets Wonderful
Wonderful Wonderful world meme
Wonderful world meme Smarty smarty had a party poem
Smarty smarty had a party poem Turtles are wonderful creatures subject and predicate
Turtles are wonderful creatures subject and predicate Wonderful words of life song
Wonderful words of life song Central idea
Central idea Mv wonderful grace
Mv wonderful grace Line of poetry
Line of poetry Poems with literary devices highlighted
Poems with literary devices highlighted Wonderful jesus bright morning star
Wonderful jesus bright morning star How marvelous how wonderful
How marvelous how wonderful Genre of poems
Genre of poems How to make spaghetti
How to make spaghetti All the vain things that charm me most
All the vain things that charm me most Wonderful grace
Wonderful grace When does her wonderful adventure begin?
When does her wonderful adventure begin? Inventions inspired by nature
Inventions inspired by nature Acute subacute chronic
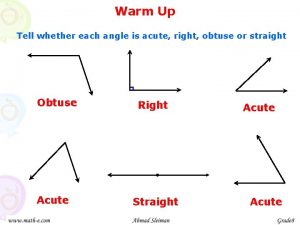
Acute subacute chronic Name an angle or angle pair that satisfies each condition
Name an angle or angle pair that satisfies each condition Tubotympanic
Tubotympanic Redha meaning
Redha meaning Name of angles
Name of angles Acute upper respiratory infection unspecified คือ
Acute upper respiratory infection unspecified คือ