Pediculosis and Scabies Pediculosis Pediculus humanus capitis head
Pediculosis and Scabies
Pediculosis Pediculus humanus capitis - head louse Pediculus humanus corpus - body louse Phthirus pubis - crab or pubic louse


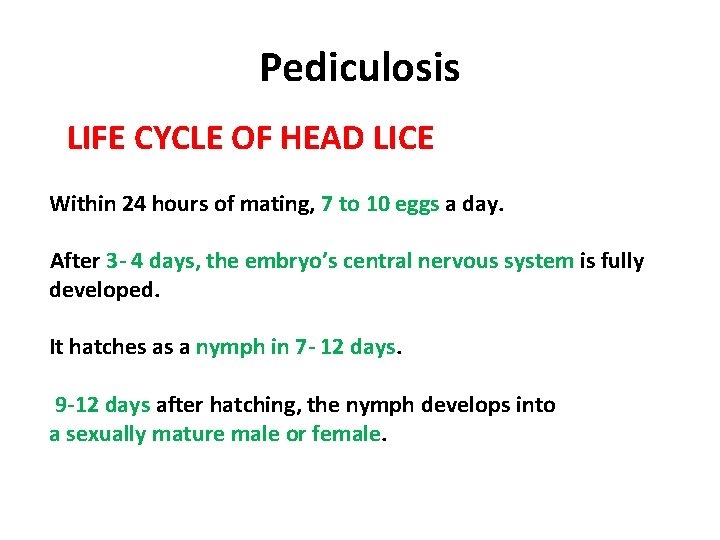
Pediculosis LIFE CYCLE OF HEAD LICE Within 24 hours of mating, 7 to 10 eggs a day. After 3 - 4 days, the embryo’s central nervous system is fully developed. It hatches as a nymph in 7 - 12 days. 9 -12 days after hatching, the nymph develops into a sexually mature male or female.
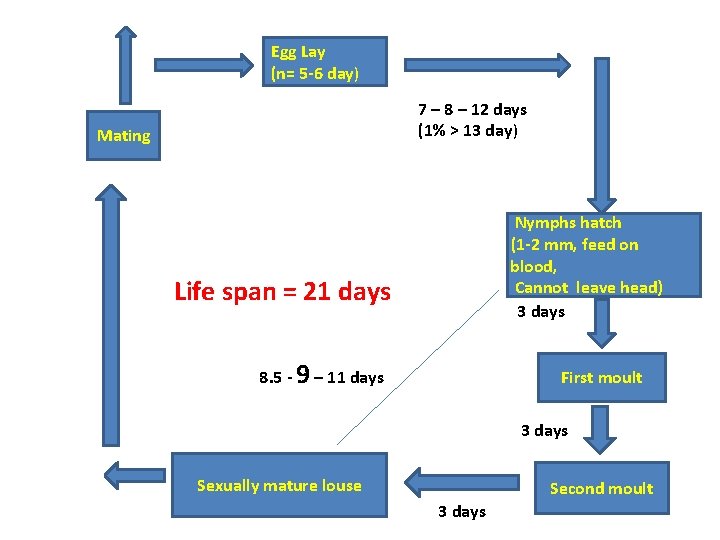
Egg Lay (n= 5 -6 day) 7 – 8 – 12 days (1% > 13 day) Mating Nymphs hatch (1 -2 mm, feed on blood, Cannot leave head) 3 days Life span = 21 days 8. 5 - 9 – 11 days First moult 3 days Sexually mature louse Second moult 3 days
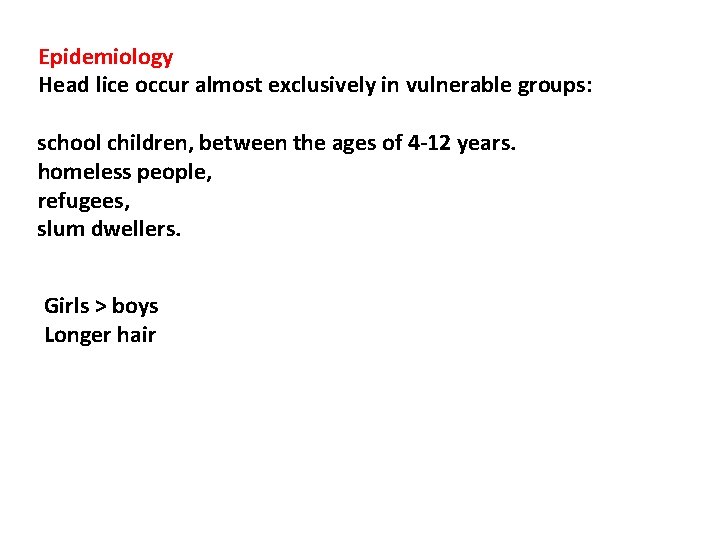
Epidemiology Head lice occur almost exclusively in vulnerable groups: school children, between the ages of 4 -12 years. homeless people, refugees, slum dwellers. Girls > boys Longer hair
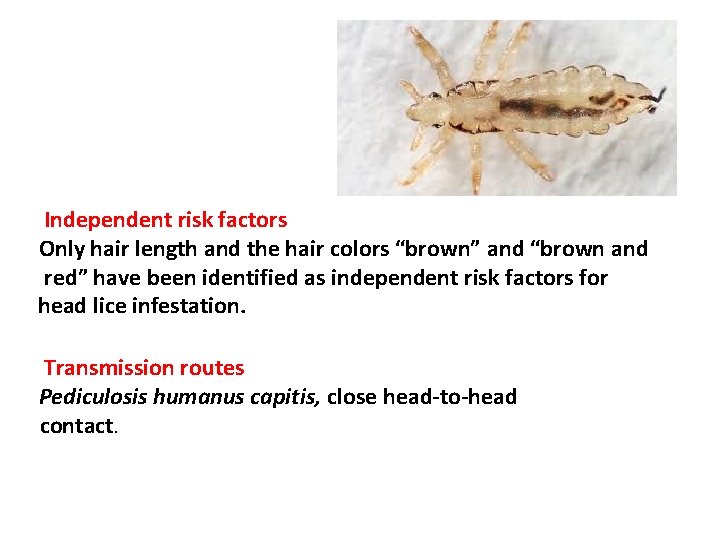
Independent risk factors Only hair length and the hair colors “brown” and “brown and red” have been identified as independent risk factors for head lice infestation. Transmission routes Pediculosis humanus capitis, close head-to-head contact.
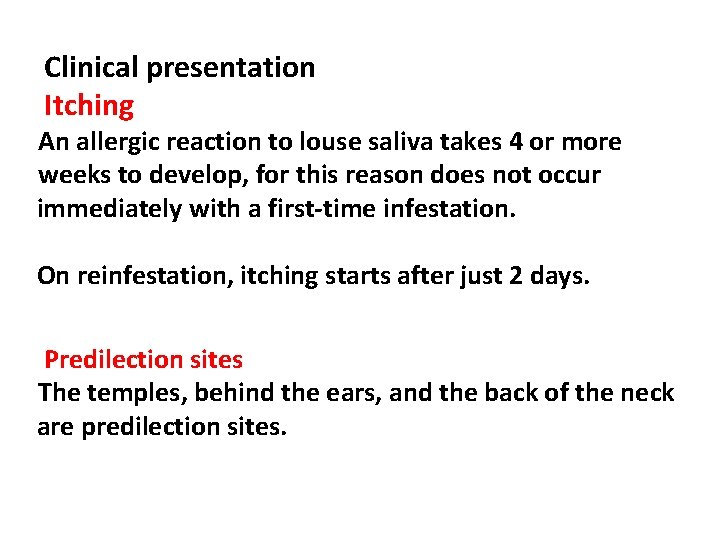
Clinical presentation Itching An allergic reaction to louse saliva takes 4 or more weeks to develop, for this reason does not occur immediately with a first-time infestation. On reinfestation, itching starts after just 2 days. Predilection sites The temples, behind the ears, and the back of the neck are predilection sites.

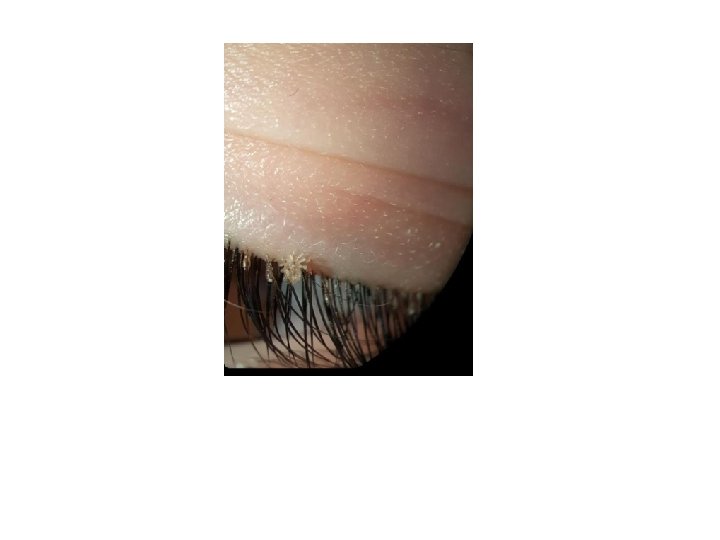

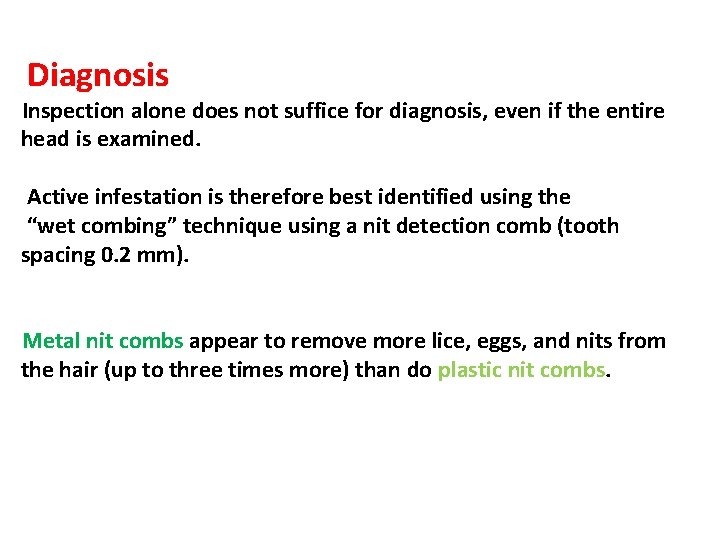
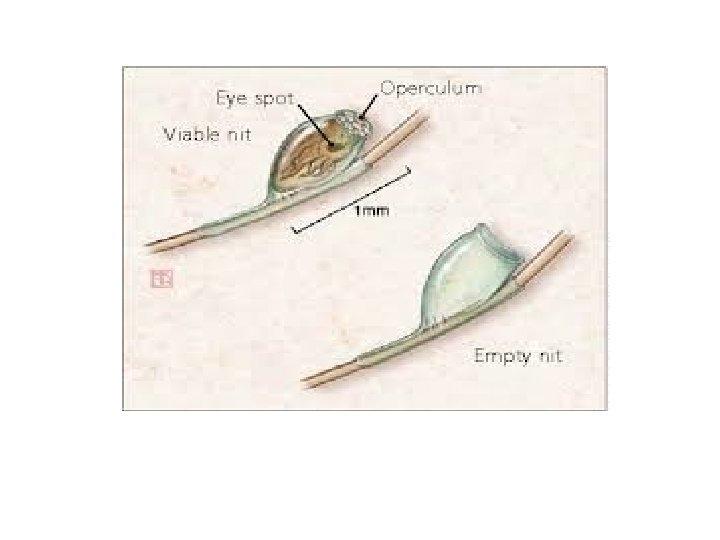
Diagnosis Inspection alone does not suffice for diagnosis, even if the entire head is examined. Active infestation is therefore best identified using the “wet combing” technique using a nit detection comb (tooth spacing 0. 2 mm). Metal nit combs appear to remove more lice, eggs, and nits from the hair (up to three times more) than do plastic nit combs.
Lice : Treatment Update Pharmacological treatment of head lice Nonpharmacological treatment of head lice
PHARMACOLOGIC TREATMENT OF HEAD LICE 3 mechanisms 1 -Neurotoxicity resulting in paralysis of the lice (Insecticidal), 2 -Suffocation via “coating” the lice, 3 -Dissolution of the wax covering on the exoskeleton(Noninsecticidal).
PHARMACOLOGIC TREATMENT OF HEAD LICE Insecticidal agents: neurotoxic to lice 1 -Permethrin 1% lotion or shampoo (Nix), 2 -Pyrethrins 0. 3%/piperonyl butoxide 4% shampoo (Rid), 3 -Malathion 0. 5% lotion (Ovide), 4 -Spinosad 0. 9% suspension (Natroba), 5 -Ivermectin 0. 5% lotion (Sklice), 6 -oral Ivermectin (Stromectol; off-label use).
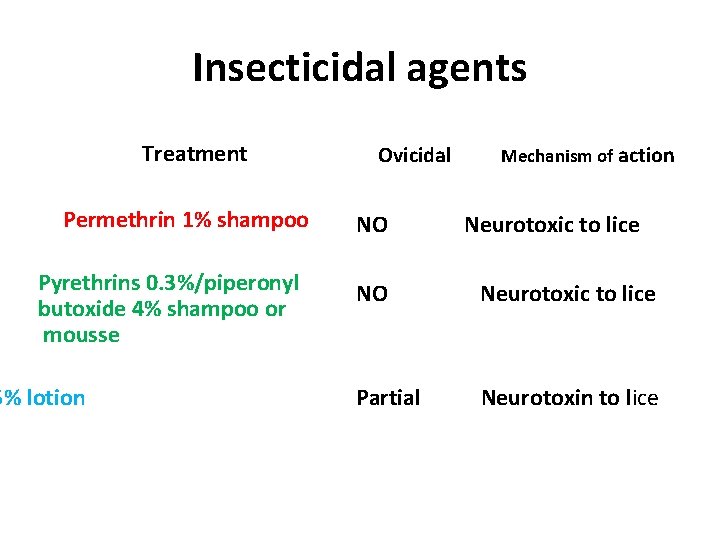
Insecticidal agents Treatment Permethrin 1% shampoo Pyrethrins 0. 3%/piperonyl butoxide 4% shampoo or mousse 5% lotion Ovicidal NO Mechanism of action Neurotoxic to lice NO Neurotoxic to lice Partial Neurotoxin to lice
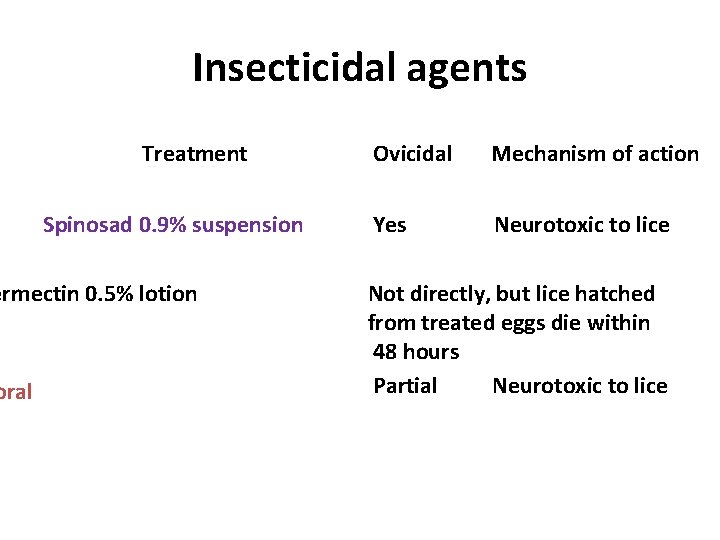
Insecticidal agents Treatment Spinosad 0. 9% suspension ermectin 0. 5% lotion oral Ovicidal Mechanism of action Yes Neurotoxic to lice Not directly, but lice hatched from treated eggs die within 48 hours Partial Neurotoxic to lice

Spinosad 0. 9% cream Topical pediculocidal agent It is a fermentation product of the soil bacterium sacchropolyspora spinosa - arthropod CNS, flaccid paralysis Apply on the scalp and hair for 10 min. and then rinsed
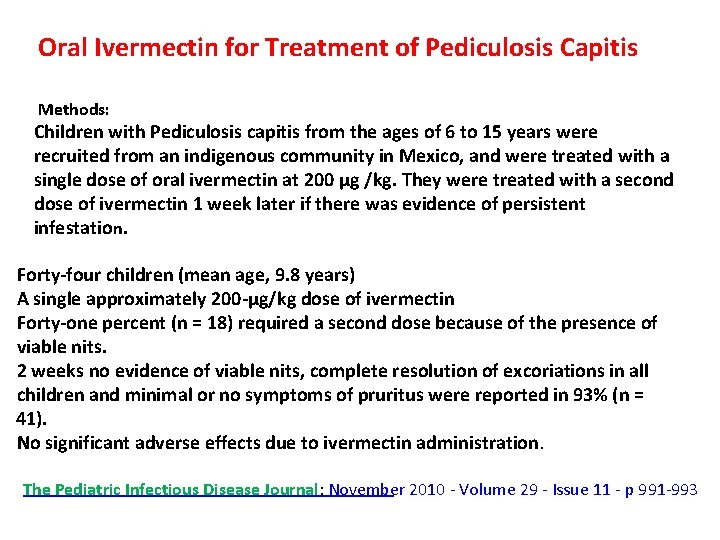
Oral Ivermectin for Treatment of Pediculosis Capitis Methods: Children with Pediculosis capitis from the ages of 6 to 15 years were recruited from an indigenous community in Mexico, and were treated with a single dose of oral ivermectin at 200 μg /kg. They were treated with a second dose of ivermectin 1 week later if there was evidence of persistent infestation. Forty-four children (mean age, 9. 8 years) A single approximately 200 -μg/kg dose of ivermectin Forty-one percent (n = 18) required a second dose because of the presence of viable nits. 2 weeks no evidence of viable nits, complete resolution of excoriations in all children and minimal or no symptoms of pruritus were reported in 93% (n = 41). No significant adverse effects due to ivermectin administration. The Pediatric Infectious Disease Journal: November 2010 - Volume 29 - Issue 11 - p 991 -993
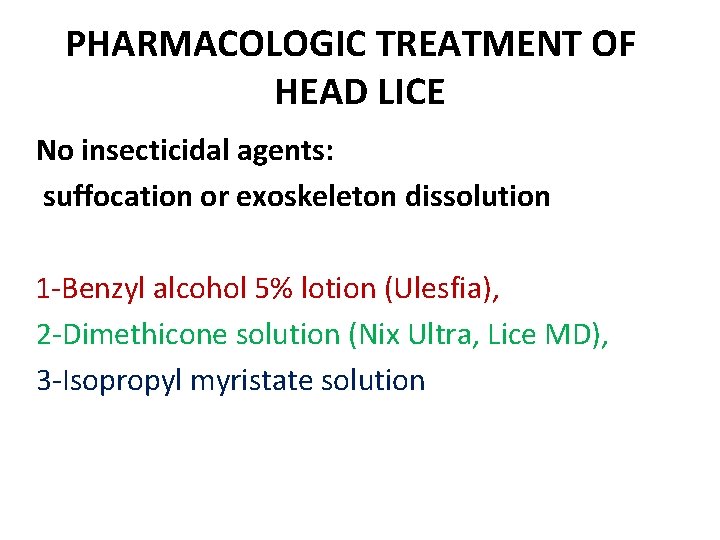
PHARMACOLOGIC TREATMENT OF HEAD LICE No insecticidal agents: suffocation or exoskeleton dissolution 1 -Benzyl alcohol 5% lotion (Ulesfia), 2 -Dimethicone solution (Nix Ultra, Lice MD), 3 -Isopropyl myristate solution
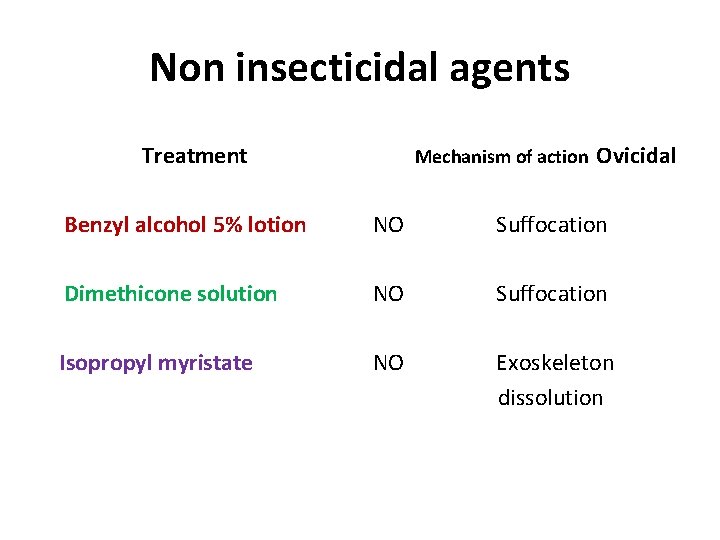
Non insecticidal agents Treatment Mechanism of action Ovicidal Benzyl alcohol 5% lotion NO Suffocation Dimethicone solution NO Suffocation Isopropyl myristate NO Exoskeleton dissolution
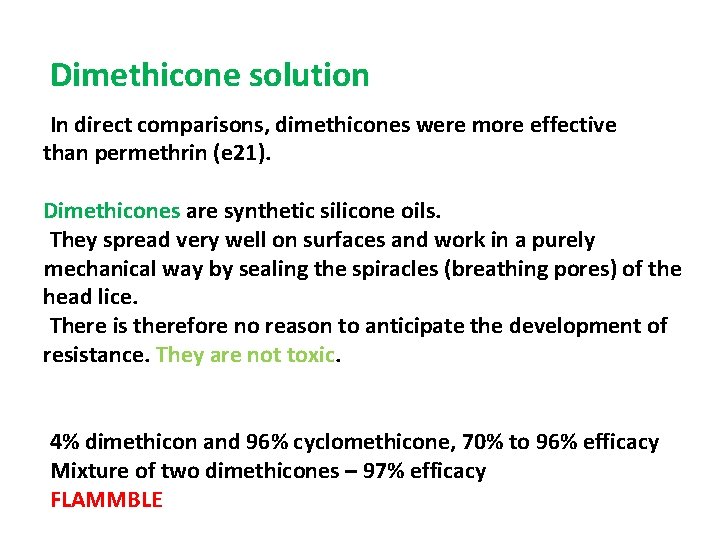
Dimethicone solution In direct comparisons, dimethicones were more effective than permethrin (e 21). Dimethicones are synthetic silicone oils. They spread very well on surfaces and work in a purely mechanical way by sealing the spiracles (breathing pores) of the head lice. There is therefore no reason to anticipate the development of resistance. They are not toxic. 4% dimethicon and 96% cyclomethicone, 70% to 96% efficacy Mixture of two dimethicones – 97% efficacy FLAMMBLE
Treatment Strategies Pediculicides organochlorines (DDT, lindane), Organophosphates malathion, carbamates (carbaryl), pyrethrins (pyrethrum), pyrethroids (permethrin, phenothrin, and bioallethrin)
Treatment Strategies Dichlorodiphenyltrichloroethane (DDT) and Lindane. Organochlorines (DDT and lindane) were the first of the synthetic organic insecticides used. DDT 1940 s
Trimethoprim-sulfamethoxazole - Is not toxic for head lice, instead, it acts by killing essential bacterial flora in the lice GI tract.
Scabies
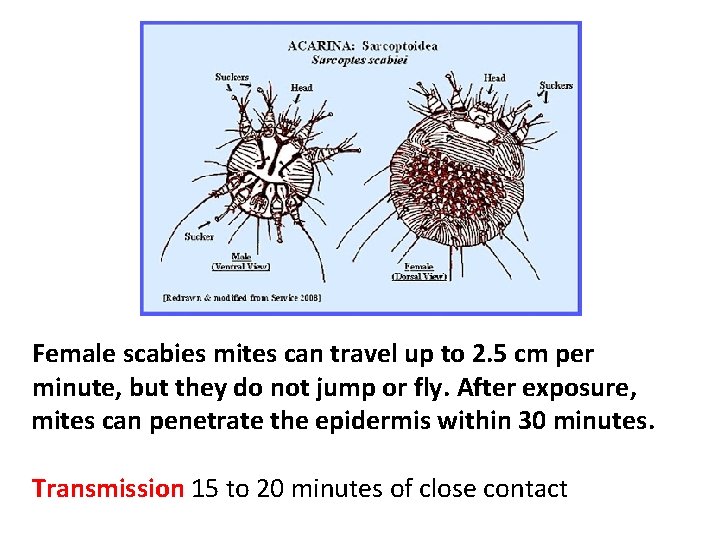
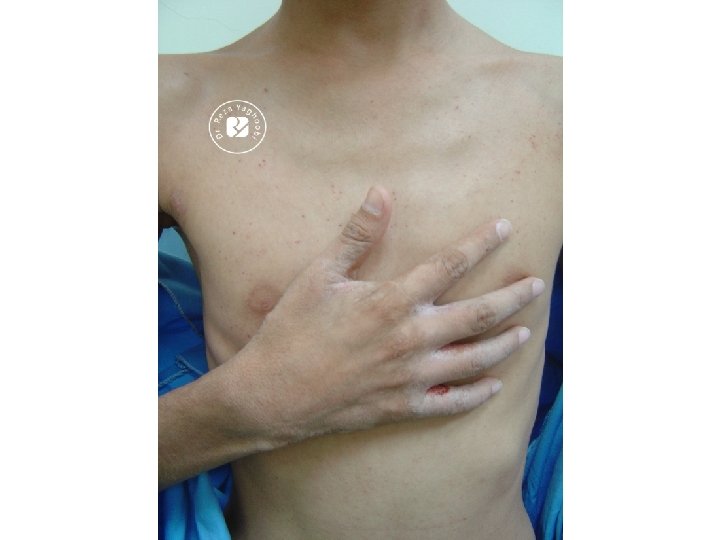
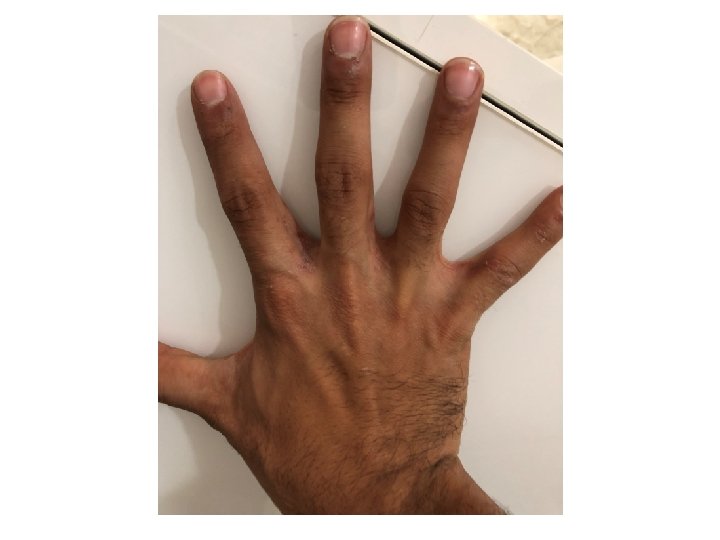
Female scabies mites can travel up to 2. 5 cm per minute, but they do not jump or fly. After exposure, mites can penetrate the epidermis within 30 minutes. Transmission 15 to 20 minutes of close contact
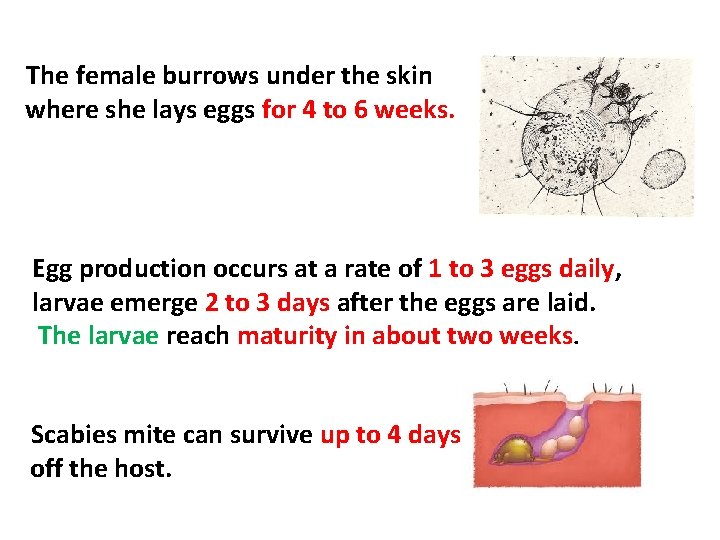
The female burrows under the skin where she lays eggs for 4 to 6 weeks. Egg production occurs at a rate of 1 to 3 eggs daily, larvae emerge 2 to 3 days after the eggs are laid. The larvae reach maturity in about two weeks. Scabies mite can survive up to 4 days off the host.
Risk factors for scabies infestation: overcrowded living conditions, poor hygiene, poor nutritional status, homelessness, dementia, sexual contact, living in a tropical region.














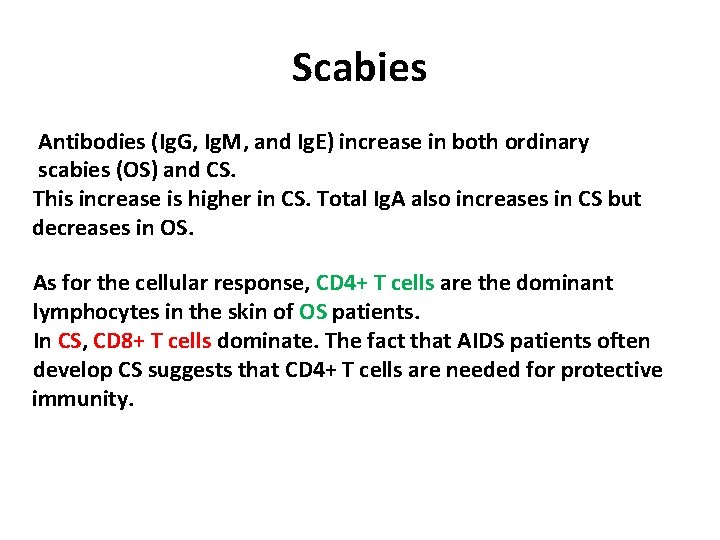
Scabies Antibodies (Ig. G, Ig. M, and Ig. E) increase in both ordinary scabies (OS) and CS. This increase is higher in CS. Total Ig. A also increases in CS but decreases in OS. As for the cellular response, CD 4+ T cells are the dominant lymphocytes in the skin of OS patients. In CS, CD 8+ T cells dominate. The fact that AIDS patients often develop CS suggests that CD 4+ T cells are needed for protective immunity.
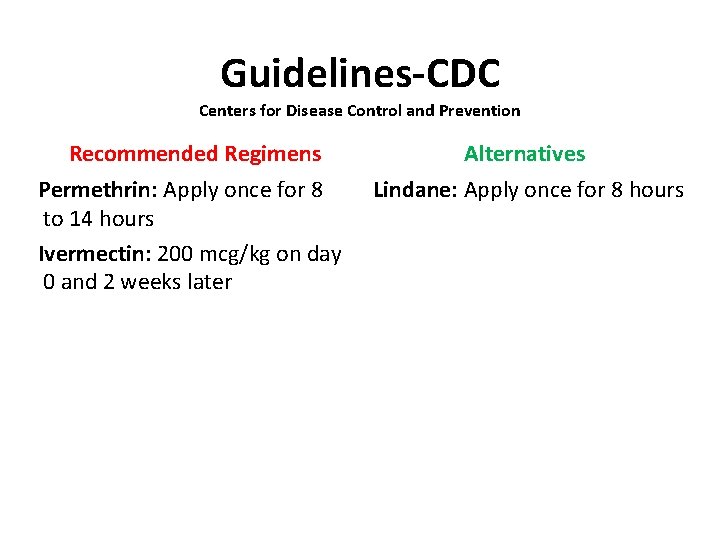
Guidelines-CDC Centers for Disease Control and Prevention Recommended Regimens Alternatives Permethrin: Apply once for 8 to 14 hours Ivermectin: 200 mcg/kg on day 0 and 2 weeks later Lindane: Apply once for 8 hours
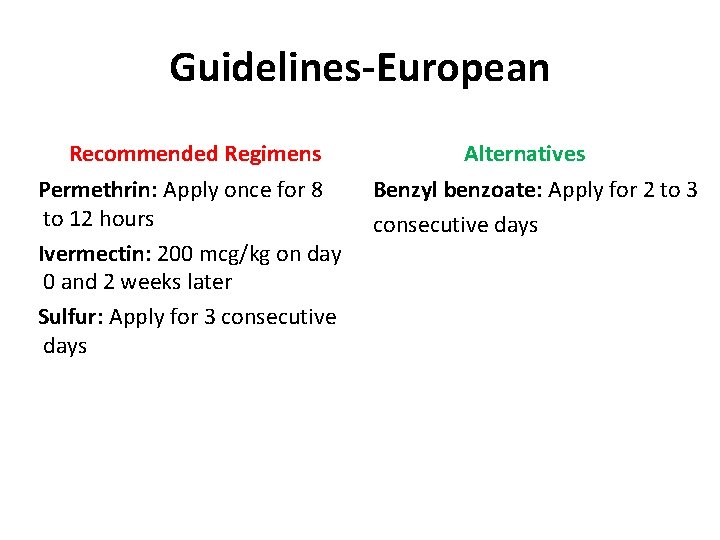
Guidelines-European Recommended Regimens Permethrin: Apply once for 8 to 12 hours Ivermectin: 200 mcg/kg on day 0 and 2 weeks later Sulfur: Apply for 3 consecutive days Alternatives Benzyl benzoate: Apply for 2 to 3 consecutive days
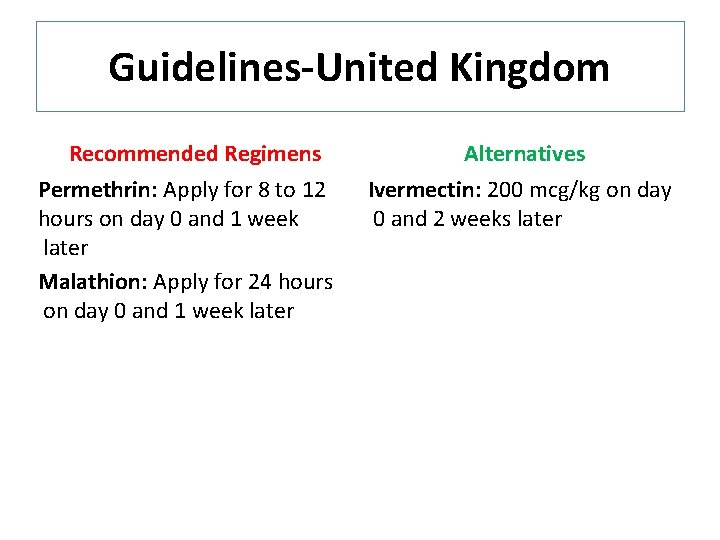
Guidelines-United Kingdom Recommended Regimens Permethrin: Apply for 8 to 12 hours on day 0 and 1 week later Malathion: Apply for 24 hours on day 0 and 1 week later Alternatives Ivermectin: 200 mcg/kg on day 0 and 2 weeks later
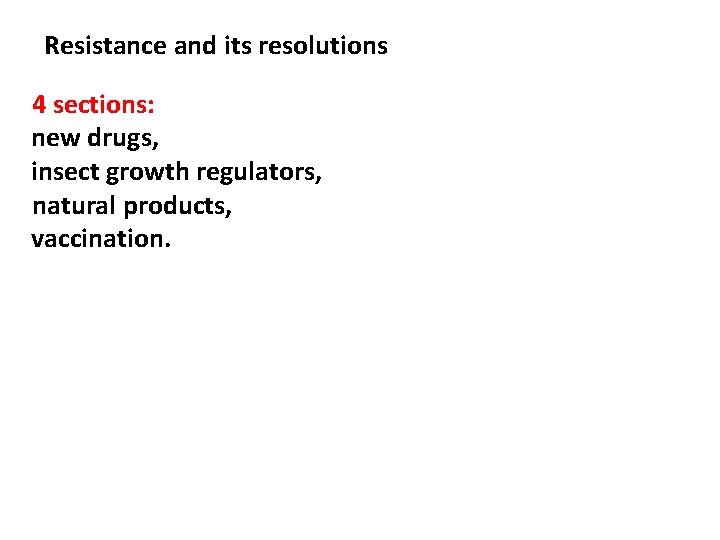
Resistance and its resolutions 4 sections: new drugs, insect growth regulators, natural products, vaccination.
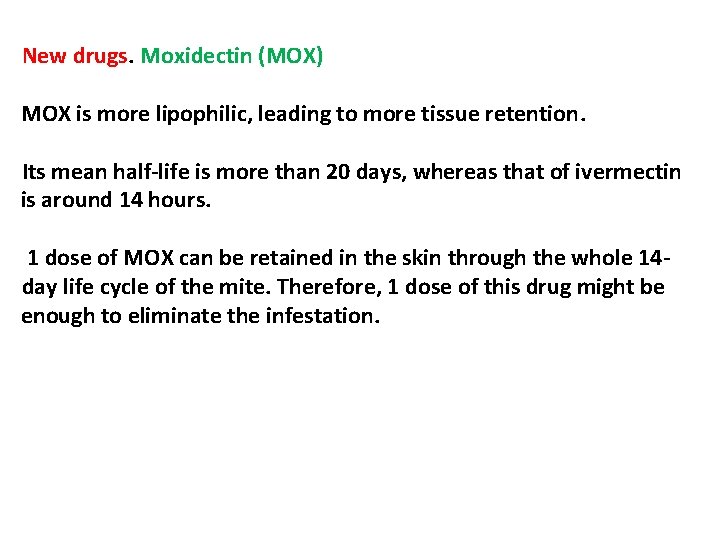
New drugs. Moxidectin (MOX) MOX is more lipophilic, leading to more tissue retention. Its mean half-life is more than 20 days, whereas that of ivermectin is around 14 hours. 1 dose of MOX can be retained in the skin through the whole 14 day life cycle of the mite. Therefore, 1 dose of this drug might be enough to eliminate the infestation.
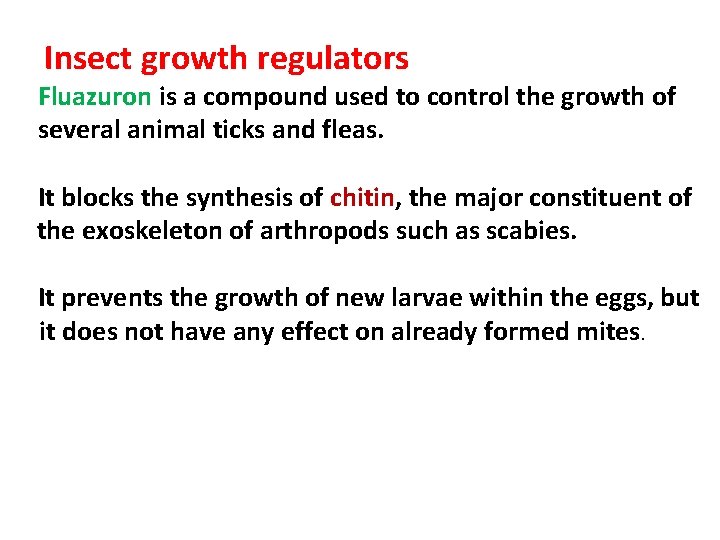
Insect growth regulators Fluazuron is a compound used to control the growth of several animal ticks and fleas. It blocks the synthesis of chitin, the major constituent of the exoskeleton of arthropods such as scabies. It prevents the growth of new larvae within the eggs, but it does not have any effect on already formed mites.
Natural products Tea tree oil derives from the plant Melaleuca alternifolia - a shorter median survival time of the mites when compared to permethrin and ivermectin. Vaccination

- Slides: 57