Pediatric Trauma And Triage Overview of the Problem
Pediatric Trauma And Triage Overview of the Problem and Necessary Care for Positive Outcomes… Presented by: Jim Morehead, BS, NREMT-P 2003 Oklahoma EMSC Resource Center 0

OBJECTIVES • • Increase awareness of issues specific to children & trauma. Improve pediatric trauma Assessment & Intervention skills. • • 2003 Identify Mechanisms of Injury & key Assessment components Recognize differences btw adult & child priorities Identify & avoid common errors in the pediatric trauma care Provide appropriate interventions Oklahoma EMSC Resource Center 1
NATURE OF “BEAST” • Pediatrics account for 15 -25% of total • Trauma is approximately 50% of all pediatric emergencies emergent care patients. • • • Injury is the leading cause of death in children • 2003 Usually > 2 years old More medical cases < 2 years old MVC = 50% Oklahoma EMSC Resource Center 2

NATURE OF “BEAST” • Almost 70% of major pediatric trauma cases die due to severity of injury. • • NOT a deficit in emergent care When a child is injured, the whole family is injured too! • 2003 cont’d > 40% divorce rate within 1 year after a major trauma Oklahoma EMSC Resource Center 3
Clinical Pearls 2003 Oklahoma EMSC Resource Center 4
Consider Possibility of Child Abuse When you see an injured child • • • 2003 Common cause of injuries in children. 50% of second hospital visits for these children result in death Awareness of signs & symptoms of abuse helps identify cases Oklahoma EMSC Resource Center 5
General Principles of Pediatric Trauma • Priorities are similar to adults • • • Children have certain key differences • • 2003 All roads lead to the A-B-C (D-E)’s Start with “A”, not the most obvious Different energy transfer due to size Metabolism Ability to respond to words & give history History of accident may be critical in determining intervention plan Oklahoma EMSC Resource Center 6
Physical Differences • HEAD Is Larger • • • Brain injury increased during impacts More leverage on neck Occiput forces neck into flexion while lying flat • • NECK Is Shorter • • 2003 Airway tends to buckle & close on adult spine board without proper shoulder support Causes different injury patterns C 2 -C 4 more common injuries Oklahoma EMSC Resource Center 7
Physical Differences cont’d • CHEST More Pliable • • ABDOMINAL ORGANS Less Protection • • • 2003 Pulmonary contusion more likely Diaphragm motion essential for ventilation Energy transmitted to chest organs Liver not covered by the rib cage Less abdominal wall muscle mass Less Sub-Q tissue to absorb energy Oklahoma EMSC Resource Center 8
Energy Transfer Effects of Size • Children are Smaller • • • More force per square inch of body Organs are closer together=multi-system injury rule Children are Softer (More Flexible / Bouncy) Bones don’t break but instead pass on energy • Internal organ damage without fractures is more common • • Larger Surface Area to Size Ratio • 2003 Lose heat more rapidly Oklahoma EMSC Resource Center 9
Metabolic Differences in Kids • Have Higher Metabolic Rates Nearly Twice as Rapid O 2 Consumption • Increased Blood Flow • More Frequent Feedings • More Fluid Intake per Size Ratio • 2003 Oklahoma EMSC Resource Center 10
Metabolic Differences cont’d • Children “SHOCK OUT” Differently • Children Compensate Better INITIALLY • • May show minimal signs & symptoms Children have less reserves than adults • Platinum Half-Hour in Trauma Resuscitation Rapid Intervention Critical • Once Reserves Exhausted • BAD THINGS HAPPEN!!! 2003 Oklahoma EMSC Resource Center 11

THE BAD THINGS • Decompensation can be rapid • • A conscious, crying child can become pulseless and apneic in less than 2 minutes Once decompensated, may be too late • Limited Reserves are gone; whole system collapses RAPID & EARLY RECOGNITION & INTERVENTION ARE CRITICAL!!! 2003 Oklahoma EMSC Resource Center 12
ASSESSMENT For Survival 2003 Oklahoma EMSC Resource Center 13
Safety First Bodily Substance Isolation • Potential Hazards on, around, or with Patient • Available Resources • 2003 Oklahoma EMSC Resource Center 14
Prepare Yourself • The first step in a cardiac arrest or other critical situation is to: Take your own pulse!!! • Assign roles ahead of time Respiratory Management • Spine Management • Circulatory Management • Hx, Equipment, etc. • 2003 Oklahoma EMSC Resource Center 15
Careful Attention Lots of b • lood Can’t breathe cryin g Fx’s Everyone scar ed Uncon. Quiet • 2003 Initial Assessment CRUCIAL • Don’t be distracted by the blood and screams A QUIET KID SHOULD SCARE the @$% of YOU!!! If practical, keep parents with child to help reduce child's fear Oklahoma EMSC Resource Center 16
Clinical Pearls 2003 Oklahoma EMSC Resource Center 17
Brilliance vs. Basics For every “BRILLIANT” maneuver/diagnosis you make which saves a life, you’ll save 10 by just doing a good, solid job. STAY FOCUSED ON THE BASICS IN THE HEAT OF THE MOMENT!!! 2003 Oklahoma EMSC Resource Center 18

Consider MOI Me cha nis m Of Inj ury 2003 Oklahoma EMSC Resource Center 19
Clinical Pearls 2003 Oklahoma EMSC Resource Center 20
Remember ‘s “Proper basic airway management is often performed inadequately if at all, apparently due to fear and panic. ” Theodore M. Barnett, M. D. Children's Mercy Hospital, Kansas City, MO 2003 Oklahoma EMSC Resource Center 21
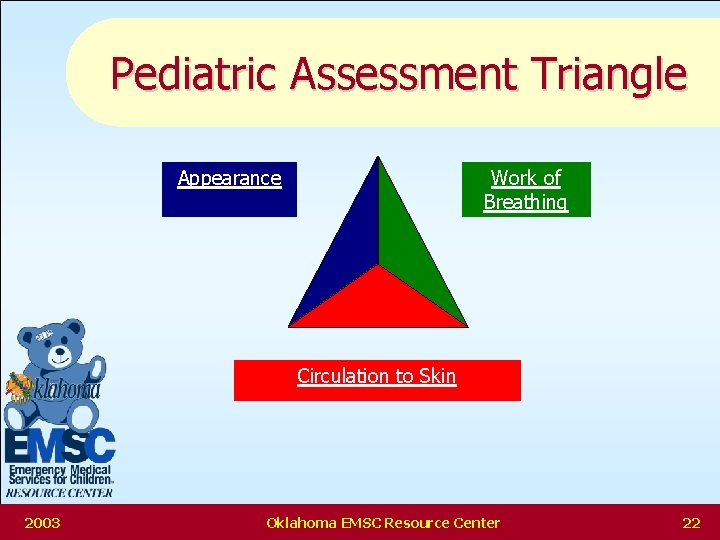
Pediatric Assessment Triangle Appearance Work of Breathing Circulation to Skin 2003 Oklahoma EMSC Resource Center 22
Appearance • 2003 Look at the patient from a slight distance - What do you see? • Mental Status • Color • Interaction / Movement • Recognition Oklahoma EMSC Resource Center STOP 23
Remember Quiet Kid is one that should, SCARE You!!! A 2003 Oklahoma EMSC Resource Center 24
Respiratory AIRWAY: Patent with Precautions • BREATHING: Respiratory Rate; too fast vs too slow, Abnormal Sounds • A slow or irregular respiratory rate in a child is an OMINOUS SIGN. (Bad JU JU) • Watch for the EFFORT NEEDED to BREATHE • • Chest, neck, or abdominal muscle retractions Flaring of the nostrils • Adventitious Sounds -Crackles, Crows, Grunts • 2003 (Rice Krispies, Rosters, Pigs) Oklahoma EMSC Resource Center 25
A=Airway: Control C-Spine • Unconscious kids can’t protect their airway • • • Infants in first 30 days of life are obligate nasal breathers • 2003 Tongue most common obstruction Little airways are easily blocked JAW THRUST: Neutral Alignment for kids includes Pad under the Shoulders May need Oral/Nasal Airway May need to suction out blood/mucus Oklahoma EMSC Resource Center 26
B=Breathing • All Children get Oxygen & LOTS OF IT • May need to assist with B-V-M Good mask seal is the KEY to bagging • Two people should bag when possible • Avoid distending the stomach • Cricoid pressure / Easy does it • Distended stomach = less room for air in lungs • Blue BAD - Oxygen GOOD 2003 Oklahoma EMSC Resource Center 27
C=Circulation: Peripheral vs Central Pulse • Color , Temperature, Texture of Skin • • CAPILLARY REFILL • < 2 seconds GOOD NEWS • 2 -4 seconds WATCH OUT • > 4 seconds DEEP DOODOO NOW!!! 2003 Oklahoma EMSC Resource Center 28
Clinical Pearls 2003 Oklahoma EMSC Resource Center 29
Pediatric Trauma Messages 1. A little bleeding is a lot the smaller you are. 2. BP often maintained until very late in hemorrhage by young patients because of their overactive vasoconstrictive responses. Tom Terndrup, MD Director of Pediatric Emergency Medicine University Hospital / Syracuse, N. Y. 2003 Oklahoma EMSC Resource Center 30
D=Disability: Neuro Eval • Use the AVPU system first – Avoid "lethargic“, "semi-conscious“, etc. because everyone has different meanings with these terms. • Use the Pediatric Glasgow Coma Scale – If time and circumstance permit – Age and behavior adjusted • TBI’s need adequate oxygen ! Hyperventilate only if they deteriorate • Otherwise High Flow O 2 • 2003 Oklahoma EMSC Resource Center 31
E=Exposure • • 2003 Kids lose heat quickly Keep them COVERED UP Expose only as you need If YOU are COMFORTABLE, it’s probably TOO COLD for them Oklahoma EMSC Resource Center 32
S-A-M-P-L-E Hx • • • 2003 S=Signs and Symptoms A=Allergies M=Medications currently taken P=Pertinent Past/ Present Illnesses L=Last Meal E=Events/environment related to the injury Oklahoma EMSC Resource Center 33
Positive Outcomes Resulting from early & rapid recognition, assessment, & management of shock… 2003 Oklahoma EMSC Resource Center 34
Pediatric Trauma Score (PTS) • • • 2003 All components are scored: • • • +2 +1 -1 • • • +12, the best - 6, the worst The threshold score is 8 Total score can range Anyone scoring < 8 send to Pediatric Trauma Center Oklahoma EMSC Resource Center 35
PTS Components • SIZE – The most obvious of all the components – Automatically weights the infant-toddler due to increased mortality associated to their smaller size • AIRWAY – Assesses functionability and management parameters – The more toys it takes, the lower the score 2003 Oklahoma EMSC Resource Center 36
PTS Components cont’d • SYSTOLIC B/P: Weighted to find the evolving shock patient (50 -90 mm. Hg). • New DOT EMT Basic uses capillary refill as an indicator of cardiovascular status. < 2 sec, 2 -4 sec, > 4 sec • Central vs Peripheral • • 2003 PALS recommends use of peripheral and central pulses as an indicator Oklahoma EMSC Resource Center 37
PTS Components cont’d • MENTAL STATUS – Any change in Mental Status warrants a lower score • SOFT TISSUE INJURY – Surface Area / Volume Issue • MUSCULO-SKELETAL INJURY/FX – High incidence in kids – Energy transmission instead of localized fracture MULTI-SYSTEMS TRAUMA IS RULE 2003 Oklahoma EMSC Resource Center 38
Recognizing Signs of Shock • Early signs can be subtle • May be minimal signs with under 20% blood loss 50% and over blood loss usually pulseless and unconscious (Read as DEAD) • Any injured kid who is Cool & Tachycardic is in SHOCK until proven otherwise!!! • 2003 Oklahoma EMSC Resource Center 39
Shock Recognition cont’d Altered mental status may be first sign of shock • Another early sign is DELAYED CAPILLARY • REFILL • Next comes a decrease in pulse pressure • • Drop in Blood Pressure is a LATE SIGN • 2003 Systolic minus Diastolic Systolic should be > [ 70 + 2(age in years)] but it rarely falls below this until 25 -30% blood loss Oklahoma EMSC Resource Center 40
Shock Recognition cont’d • Anxiety, fear, and cold weather can all mimic early shock • • • History alone can be a good enough reason • 2003 Increased heart rate Decreased capillary refill Pale, cool extremities Weak peripheral pulses Remember the MOI Oklahoma EMSC Resource Center 41
Shock Intervention • • 2003 O 2 (shoot the juice) Protection • • Spinal Stabilization/Immobilization Preserve Body Temperature • • Crystalloids (NS/LR) 20 m. L/kg Length-Based Resuscitation Tape Hemorrhage Control Volume Replacement Oklahoma EMSC Resource Center 42
Clinical Pearls 2003 Oklahoma EMSC Resource Center 43
Infant Transport by EMS • “Keep infants in car seats unless treatment of injuries requires removal (IV, ETT, BVM, control of hemorrhage). If they survived the crash in an intact car seat, they are usually better off to stay in it for the ride to the hospital. ” William E. Hauda, II, MD Pediatric Emergency Medicine Fellow Attending Emergency Medicine Physician Fairfax Hospital, Falls Church, VA 2003 Oklahoma EMSC Resource Center 44
Trauma Management Kids are large headed and may have cervical spine injury without evidence • Ideal immobilization is a hard collar, spine board with pads & head-straps. • TBI’s need adequate oxygen! • Hyperventilate only if they deteriorate • Otherwise High Flow O 2 • 2003 Oklahoma EMSC Resource Center 45
Pediatric Trauma Triage Identifying a possible tool to accomplish task… 2003 Oklahoma EMSC Resource Center 46
Pediatric Problems in Triage • Children often not triaged as well as adults in traumatic MCI’s • Currently no published or widely utilized Multi. Casualty Triage Tools that take into account physiology differences between children & adults 2003 Oklahoma EMSC Resource Center 47
Triage Problems cont’d • Pediatric Multi-Casualty triage may be affected by the emotional states of providers • May be tendencies to upgrade triage categories out of compassion or lack of confidence in pediatric assessment & intervention skills 2003 Oklahoma EMSC Resource Center 48

May 3, 1999 2003 Oklahoma EMSC Resource Center 49
May 3, 1999 cont’d 2003 Oklahoma EMSC Resource Center 50
Multi-Casualty Triage Goal “To do the BEST for the MOST with the LEAST. ” 2003 Oklahoma EMSC Resource Center 51
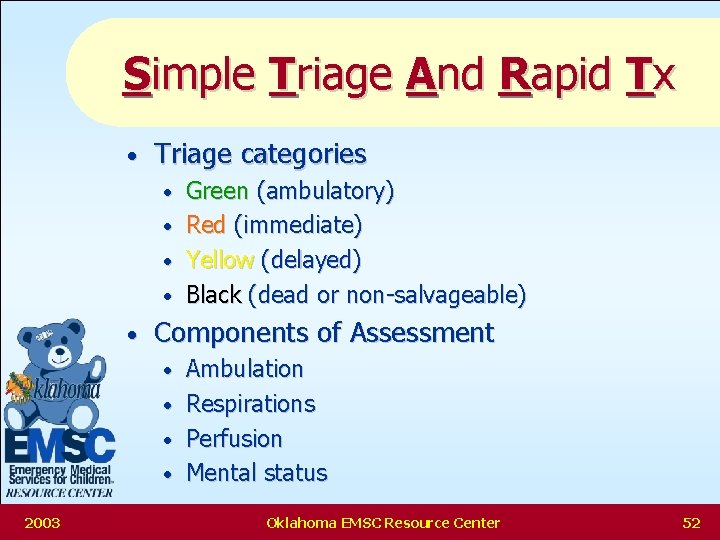
Simple Triage And Rapid Tx • Triage categories • • • Components of Assessment • • 2003 Green (ambulatory) Red (immediate) Yellow (delayed) Black (dead or non-salvageable) Ambulation Respirations Perfusion Mental status Oklahoma EMSC Resource Center 52
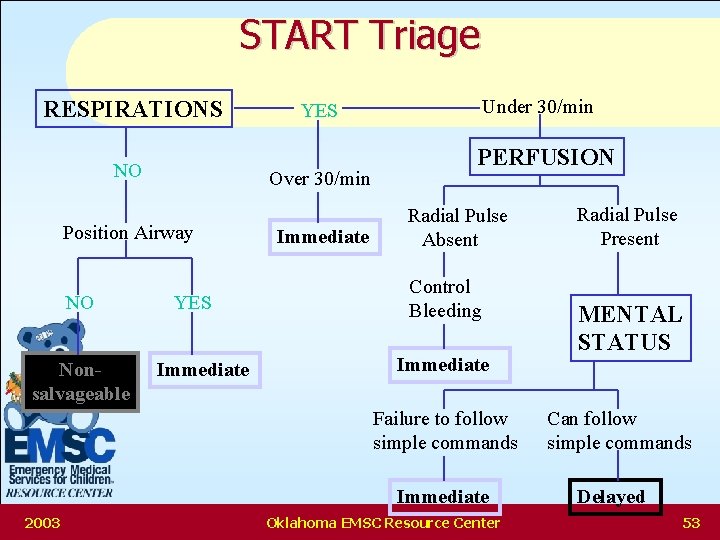
START Triage RESPIRATIONS NO Over 30/min Position Airway NO Nonsalvageable YES Immediate Under 30/min YES Immediate PERFUSION Radial Pulse Absent Control Bleeding Immediate Failure to follow simple commands Immediate 2003 Oklahoma EMSC Resource Center Radial Pulse Present MENTAL STATUS Can follow simple commands Delayed 53
Pediatric Problems with START Apneic child more likely to have a primary respiratory problem than adult • Perfusion may be maintained for a short time & child may be salvageable • RR +/- 30 may either over-triage or under-triage a child, depending on age • 2003 Oklahoma EMSC Resource Center 54
Problems with START cont’d • Capillary refill may not adequately reflect peripheral hemodynamic status in a cool environment • • 2003 In fact START has changed to reflect peripheral pulse checks instead of cap refill Obeying commands may not be an appropriate gauge of mental status for younger children Oklahoma EMSC Resource Center 55
JUMPSTART Goals • • 2003 Modify an existing tool for use with children Utilize decision points that are flexible enough to serve children of all ages & reflective of the unique points of pediatric physiology Reduce over- and under-triage Accomplish triage for most patients within 15 second/pt goal Oklahoma EMSC Resource Center 56
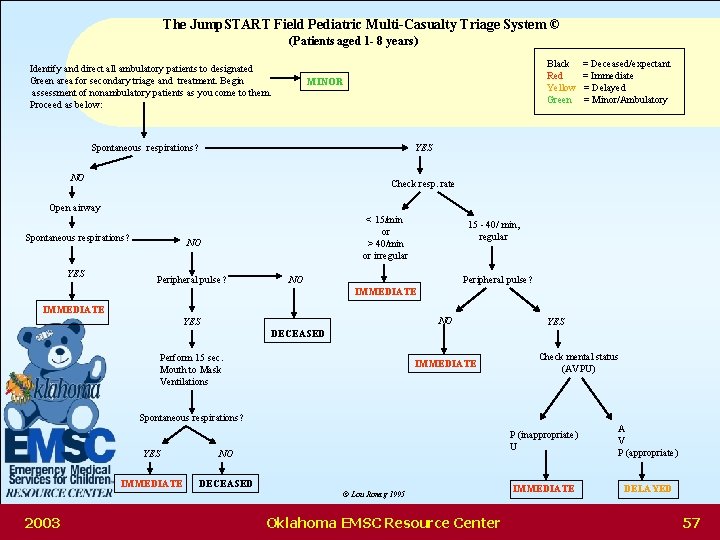
The Jump. START Field Pediatric Multi-Casualty Triage System © (Patients aged 1 - 8 years) Identify and direct all ambulatory patients to designated Green area for secondary triage and treatment. Begin assessment of nonambulatory patients as you come to them. Proceed as below: Black Red Yellow Green MINOR Spontaneous respirations? = Deceased/expectant = Immediate = Delayed = Minor/Ambulatory YES NO Check resp. rate Open airway Spontaneous respirations? YES < 15/min or > 40/min or irregular NO Peripheral pulse? 15 - 40/ min, regular NO Peripheral pulse? IMMEDIATE NO YES DECEASED Perform 15 sec. Mouth to Mask Ventilations IMMEDIATE Check mental status (AVPU) Spontaneous respirations? YES NO IMMEDIATE DECEASED © Lou Romig 1995 2003 Oklahoma EMSC Resource Center P (inappropriate) U A V P (appropriate) IMMEDIATE DELAYED 57
JUMPSTART Ages 1 -8 years chosen • <1 year of age is less likely to be ambulatory • These children can be triaged using JUMPSTART but should be fully screened – If all “DELAYED” criteria satisfied & without significant external injuries, the child may be classified as “AMBULATORY” – • 2003 Pertinent pediatric physiology (specifically airway) approaches that of adults by approximately eight years of age Oklahoma EMSC Resource Center 58
JUMPSTART Ambulatory • Identify & direct all ambulatory patients to designated GREEN area for secondary triage & treatment • Begin assessment of non-ambulatory patients as you come to them 2003 Oklahoma EMSC Resource Center 59
JUMPSTART Breathing • If breathing spontaneously, go on to the next step, assessing respiratory rate • If apneic or with very irregular breathing, open the airway using standard positioning techniques • If positioning results in resumption of spontaneous respirations, tag the patient IMMEDIATE & move on 2003 Oklahoma EMSC Resource Center 60
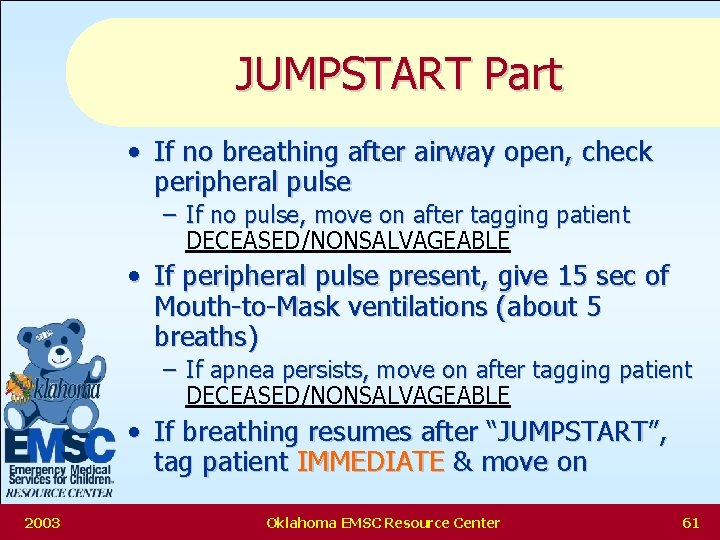
JUMPSTART Part • If no breathing after airway open, check peripheral pulse – If no pulse, move on after tagging patient DECEASED/NONSALVAGEABLE • If peripheral pulse present, give 15 sec of Mouth-to-Mask ventilations (about 5 breaths) – If apnea persists, move on after tagging patient DECEASED/NONSALVAGEABLE • If breathing resumes after “JUMPSTART”, tag patient IMMEDIATE & move on 2003 Oklahoma EMSC Resource Center 61
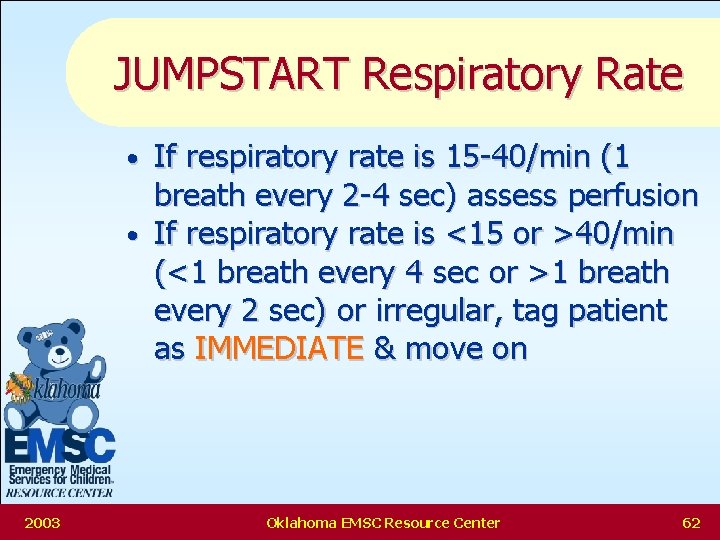
JUMPSTART Respiratory Rate If respiratory rate is 15 -40/min (1 breath every 2 -4 sec) assess perfusion • If respiratory rate is <15 or >40/min (<1 breath every 4 sec or >1 breath every 2 sec) or irregular, tag patient as IMMEDIATE & move on • 2003 Oklahoma EMSC Resource Center 62
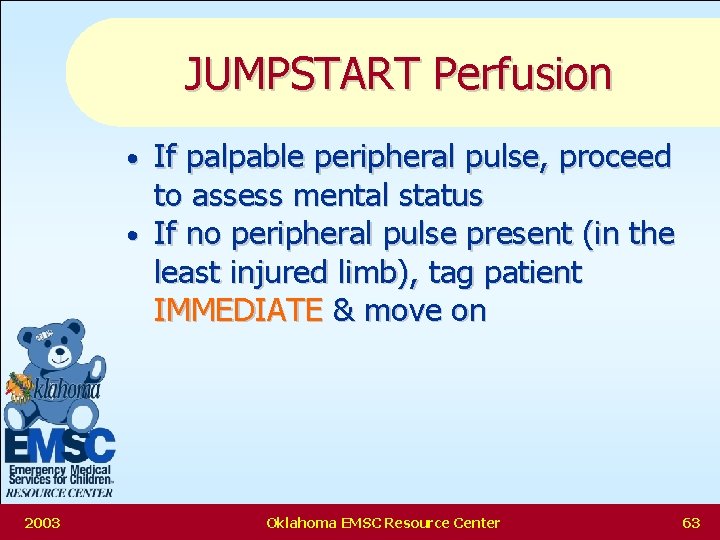
JUMPSTART Perfusion If palpable peripheral pulse, proceed to assess mental status • If no peripheral pulse present (in the least injured limb), tag patient IMMEDIATE & move on • 2003 Oklahoma EMSC Resource Center 63
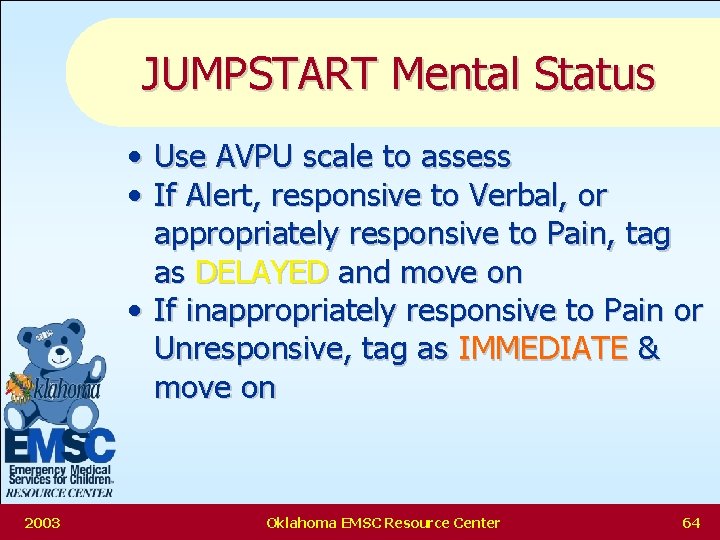
JUMPSTART Mental Status • Use AVPU scale to assess • If Alert, responsive to Verbal, or appropriately responsive to Pain, tag as DELAYED and move on • If inappropriately responsive to Pain or Unresponsive, tag as IMMEDIATE & move on 2003 Oklahoma EMSC Resource Center 64
START/JUMPSTART Similarities As soon as a definitive triage category determined further assessment STOPS • Ambulatory patients are immediately moved away for secondary triage • To be in the DELAYED category pt’s must have adequate respirations & perfusion & mental status that is unlikely to compromise the airway • 2003 Oklahoma EMSC Resource Center 65
START/JUMPSTART Differences • Apneic children are rapidly assessed for sustained circulation • • • Respiratory rates are adjusted Peripheral pulse is substituted for Cap Refill • • 2003 Apneic children with circulation receive a brief ventilatory trial as an additional airway opening & stimulating maneuver This is now done in START too AVPU is used to assess mental status Oklahoma EMSC Resource Center 66

POTENTIAL JUMPSTART DISADVANTAGES 2003 Oklahoma EMSC Resource Center 67
Disadvantages Extra steps for apneic children add time to the triage process • Mouth-to-Mask ventilation increases the risk of cross-contamination between patients • Additional equipment must be carried by triage personnel • • • 2003 TOO COMPLICATED NO PROOF IT WILL WORK Oklahoma EMSC Resource Center 68
POTENTIAL JUMPSTART ADVANTAGES 2003 Oklahoma EMSC Resource Center 69
Advantages Provides rapid triage system specifically designed for children, taking into consideration their unique physiology • Algorithm modified from an existing system widely accepted for adult triage • For most patients, triage can be accomplished within the 15 sec goal • 2003 Oklahoma EMSC Resource Center 70
Advantages cont’d Objective criteria for children will help eliminate role of emotions in triage process • Objective criteria will provide emotional support for personnel forced to make life or death decisions for children in the MCI setting • 2003 Oklahoma EMSC Resource Center 71
Transport Decisions Oklahoma ‘s Trauma Triage and Transport Guidelines 2003 Oklahoma EMSC Resource Center 72

Air Medical Services MEDIFLIGHT OF OKLAHOMA • 1 -800 -522 -0212 AIR EVAC LIFE TEAM • 1 -918 -426 -4081 TULSA LIFE FLIGHT • 1 -888 -4 TRAUMA EAGLEMED • 2003 1 -800 -525 -5220 Oklahoma EMSC Resource Center 73

Pediatric Special Care Facilities Children’s Hospital at OU Med Center, OKC (405) 271 - 4876 University Hospital at OU Med Center, OKC (405) 271 - 4363 Children’s Center of St. Francis Hospital, Tulsa (918) 584 -5433 2003 Oklahoma EMSC Resource Center 74
Summary • The more critical the patient, the more important it is to focus on the basics IN ORDER • • • Rapid Recognition & Intervention for Shock Airway Oxygen Proper Immobilization Keep Warm • Assign roles ahead of time 2003 Oklahoma EMSC Resource Center 75
OK-EMSC Resource Center To Contact Us: Phone: 405 -271 -3307 Fax: 405 -271 -2421 e-mail: emsc@ouhsc. edu Web Page: www. oumedicine. com/emsc 2003 Oklahoma EMSC Resource Center 76
- Slides: 77