Pediatric Sepsis Dr S Veroukis Pediatric Critical Care

- Slides: 28

Pediatric Sepsis Dr. S. Veroukis Pediatric Critical Care Winnipeg Children’s Hospital Winnipeg, MB CANADA
Objective • Review of the 2007 Clinical Practice Guidelines on Pediatric and Neonatal Septic Shock
Guidelines • Aim to standardize care of the septic patient to decrease mortality • Expected mortality if guidelines adhered to are expected to be very low: – 0 -5% for previously healthy children – 10% for children with chronic illness
Recognizing Sepsis • Clinical triad: fever, tachycardia, vasodilation plus change in level of consciousness and urine output is the most common presentation of sepsis • Our hospital has a screening tool • Used for the febrile patient who also has changes in vital signs or level of consciousness
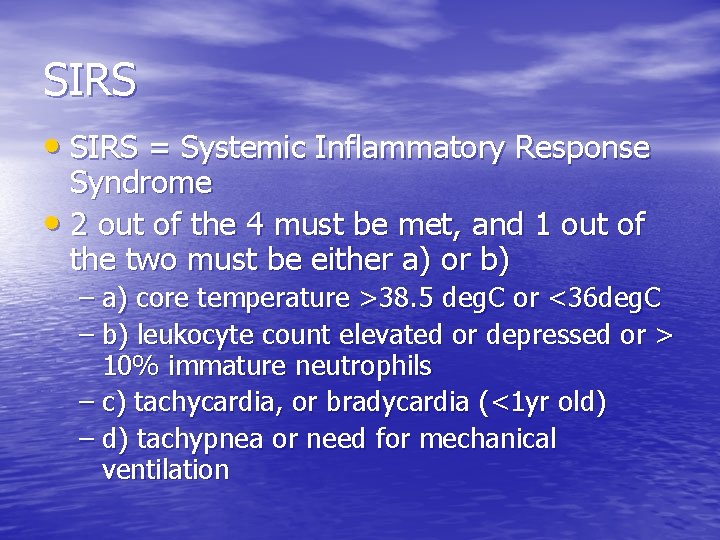
SIRS • SIRS = Systemic Inflammatory Response Syndrome • 2 out of the 4 must be met, and 1 out of the two must be either a) or b) – a) core temperature >38. 5 deg. C or <36 deg. C – b) leukocyte count elevated or depressed or > 10% immature neutrophils – c) tachycardia, or bradycardia (<1 yr old) – d) tachypnea or need for mechanical ventilation
Sepsis Definition • Sepsis is defined as a condition meeting the SIRS definition in the presence of suspected or proven infection. • Septic shock is Sepsis with cardiovascular dysfunction (hypotension, poor perfusion, elevated lactate)
Recommendations for Pediatric Septic Shock
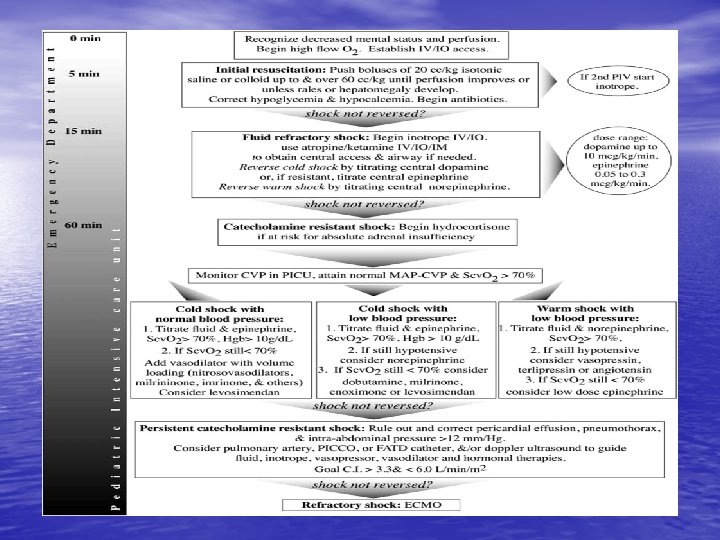
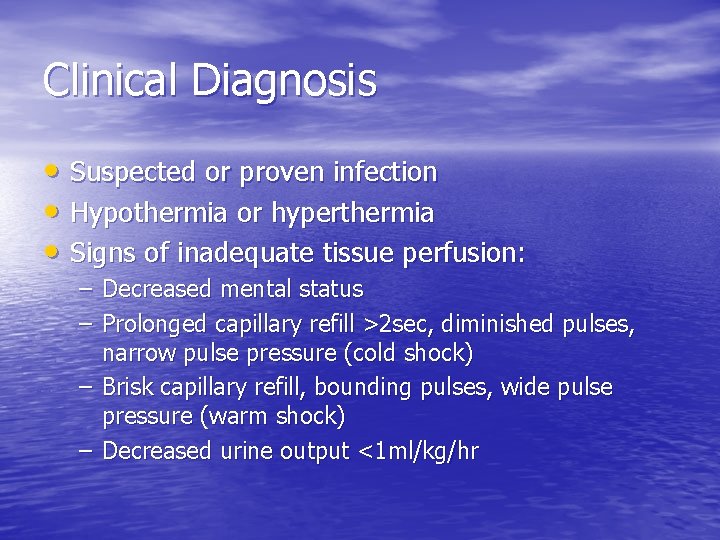
Clinical Diagnosis • Suspected or proven infection • Hypothermia or hyperthermia • Signs of inadequate tissue perfusion: – Decreased mental status – Prolonged capillary refill >2 sec, diminished pulses, narrow pulse pressure (cold shock) – Brisk capillary refill, bounding pulses, wide pulse pressure (warm shock) – Decreased urine output <1 ml/kg/hr
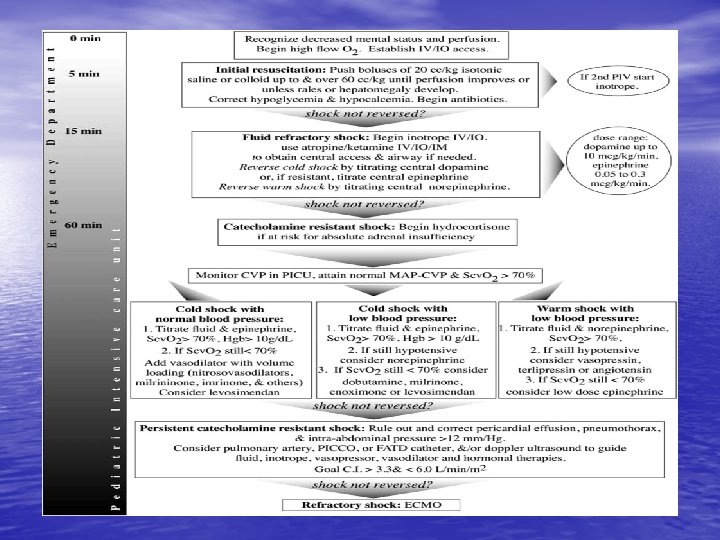
The First Hour of Resuscitation (Emergency Room) • Push 20 cc/kg of Crystalloid or Colloid up to 60 cc/kg IV or Intraosseous • Start antibiotics (eg. Vancomycin, Cefotaxime) • Correct hypoglycemia and hypocalcemia • Need to give fluids until capillary refill and peripheral pulses are normalized or until hepatomegaly and/or rales develop
Airway and Ventilation • During the first hour, the work of breathing may increase, oxygen saturation may decrease • May need to intubate • 40% of cardiac output is used for work of breathing • Recommended medications: atropine and ketamine(0. 5 -1. 5 mg/kg IV or IO)
Fluid Refractory Septic Shock • Dopamine IV or IO • May need to start second inotrope – Cold shock: (low CO, high SVR) choose epinephrine IV or IO – If warm shock (high CO, low SVR) choose norepinephrine • Need to establish central venous access soon in order to run inotropes at central concentrations
Cold Shock • Characterized by – Tachycardia – Cold extremities – Weak pulses, prolonged capillary refill – Elevated blood pressure with narrow pulse pressure – Usually Cardiac Output is low but Systemic Vascular Resistance (SVR) is high
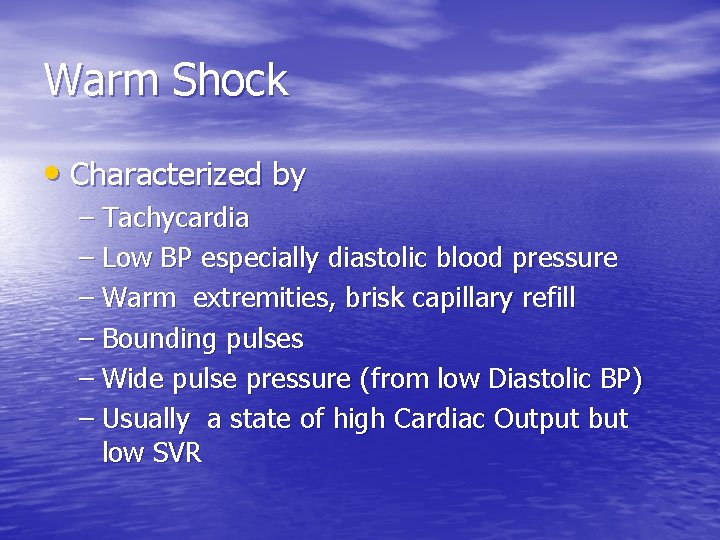
Warm Shock • Characterized by – Tachycardia – Low BP especially diastolic blood pressure – Warm extremities, brisk capillary refill – Bounding pulses – Wide pulse pressure (from low Diastolic BP) – Usually a state of high Cardiac Output but low SVR
Further Therapy • Maintenance fluids should be started : – D 10 WNS solution to run at maintenance – Ng if intubated – Foley to accurately measure urine output – Frequent vitals (hourly) – Treat temperature – If intubated needs sedation: most frequent fentanyl and midazolam infusions
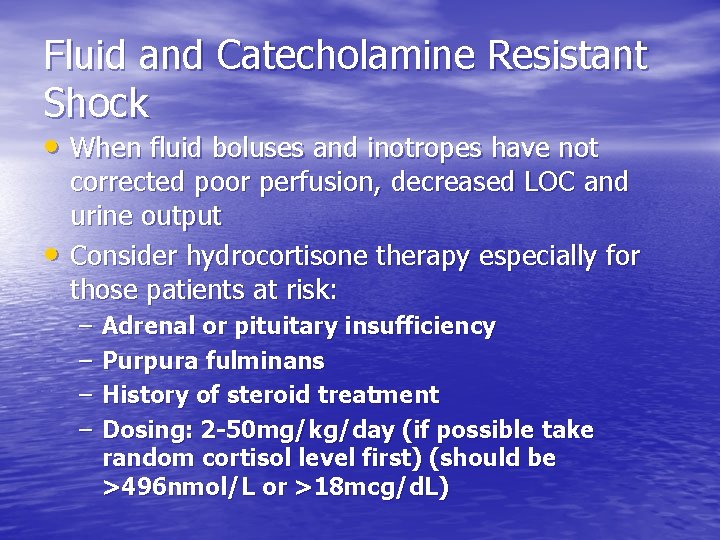
Fluid and Catecholamine Resistant Shock • When fluid boluses and inotropes have not • corrected poor perfusion, decreased LOC and urine output Consider hydrocortisone therapy especially for those patients at risk: – – Adrenal or pituitary insufficiency Purpura fulminans History of steroid treatment Dosing: 2 -50 mg/kg/day (if possible take random cortisol level first) (should be >496 nmol/L or >18 mcg/d. L)
Intensive Care • Patient can be transferred to Intensive Care at any point • Central venous access to be established • Obtain central venous oxygen saturation (Scv. O 2) • Surrogate for cardiac output and tissue oxygenation
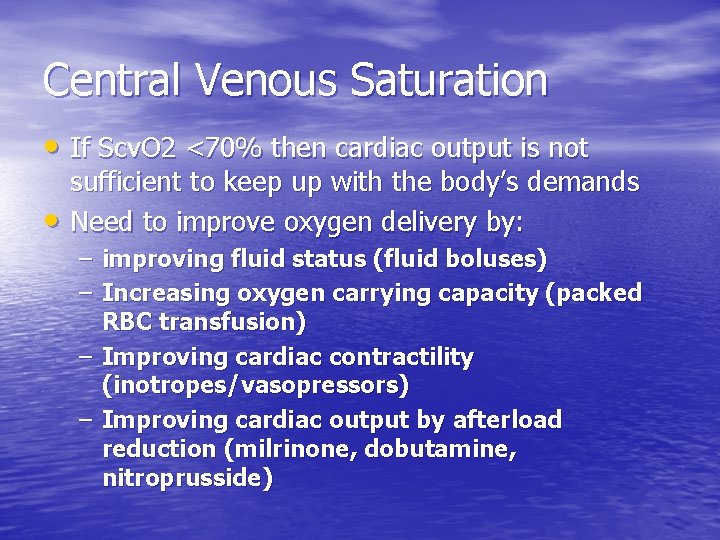
Central Venous Saturation • If Scv. O 2 <70% then cardiac output is not • sufficient to keep up with the body’s demands Need to improve oxygen delivery by: – improving fluid status (fluid boluses) – Increasing oxygen carrying capacity (packed RBC transfusion) – Improving cardiac contractility (inotropes/vasopressors) – Improving cardiac output by afterload reduction (milrinone, dobutamine, nitroprusside)
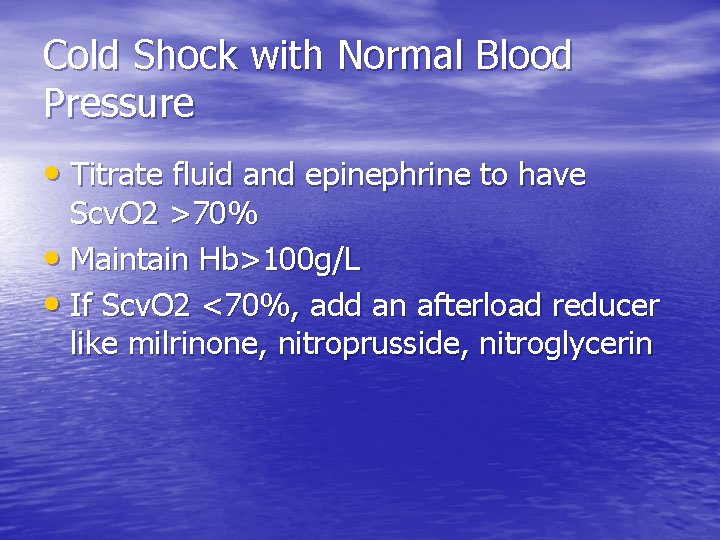
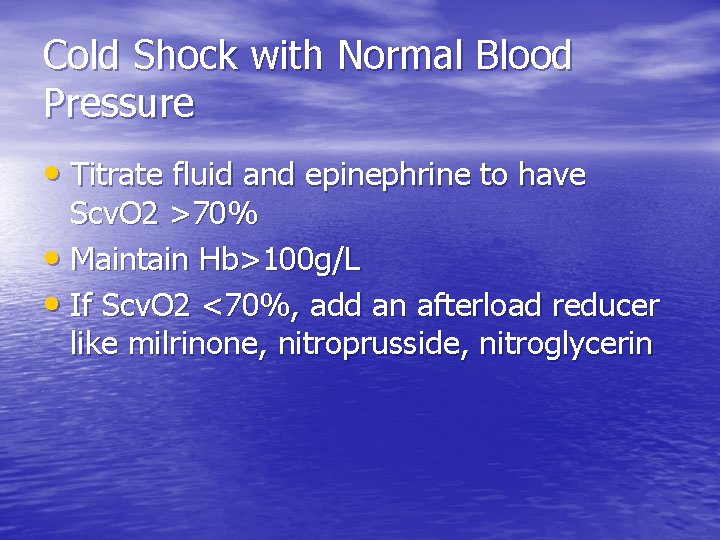
Cold Shock with Normal Blood Pressure • Titrate fluid and epinephrine to have Scv. O 2 >70% • Maintain Hb>100 g/L • If Scv. O 2 <70%, add an afterload reducer like milrinone, nitroprusside, nitroglycerin
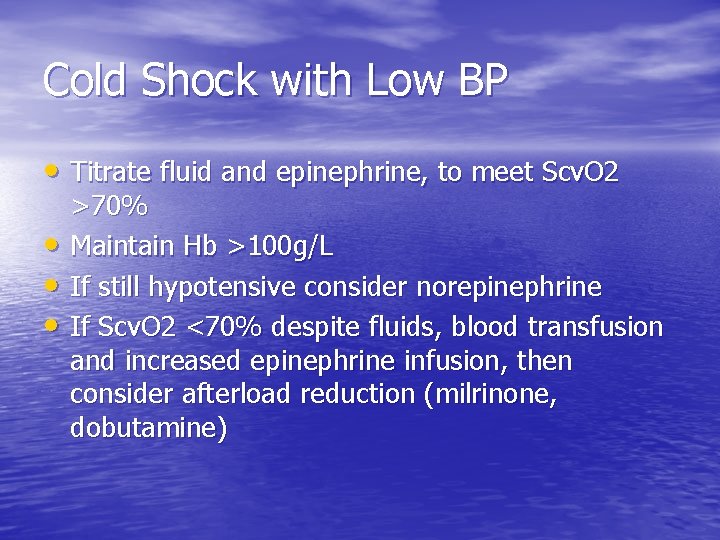
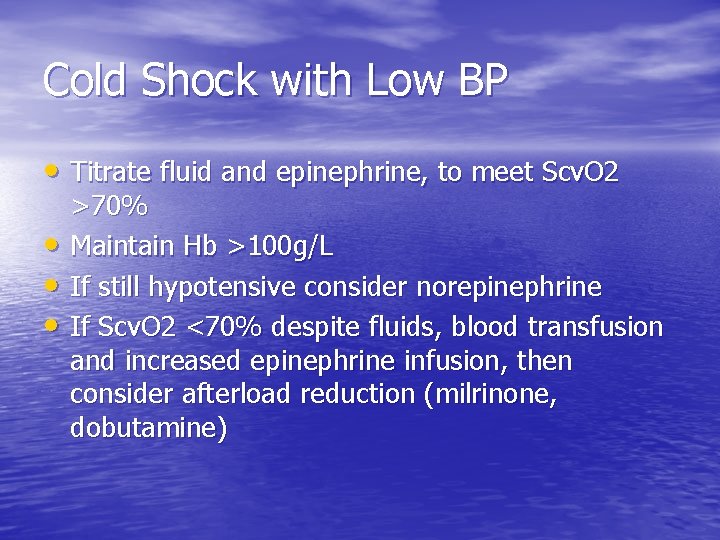
Cold Shock with Low BP • Titrate fluid and epinephrine, to meet Scv. O 2 • • • >70% Maintain Hb >100 g/L If still hypotensive consider norepinephrine If Scv. O 2 <70% despite fluids, blood transfusion and increased epinephrine infusion, then consider afterload reduction (milrinone, dobutamine)
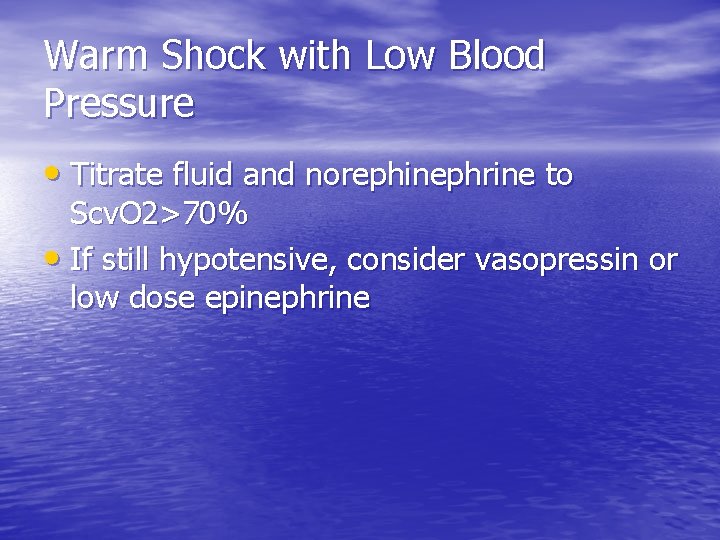
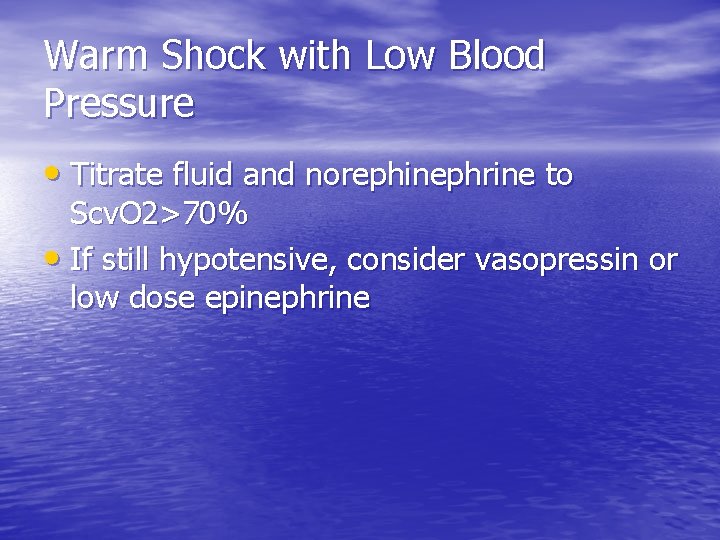
Warm Shock with Low Blood Pressure • Titrate fluid and norephinephrine to Scv. O 2>70% • If still hypotensive, consider vasopressin or low dose epinephrine
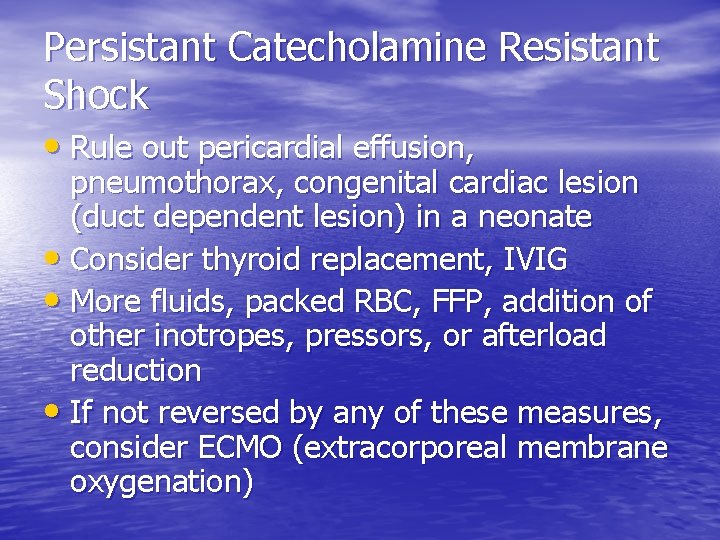
Persistant Catecholamine Resistant Shock • Rule out pericardial effusion, pneumothorax, congenital cardiac lesion (duct dependent lesion) in a neonate • Consider thyroid replacement, IVIG • More fluids, packed RBC, FFP, addition of other inotropes, pressors, or afterload reduction • If not reversed by any of these measures, consider ECMO (extracorporeal membrane oxygenation)
Fluid Removal • Patients will get lots of fluid, even up to • • 200 cc/kg in 24 hr period Capillary leak from SIRS edematous skin, pulmonary edema, ascites and risk of abdominal compartment syndrome If kidneys can not produce enough urine, and patient is 10% fluid overloaded, may use diuretics, peritoneal dialysis, CRRT to remove fluid
Outcomes • Early initiated, goal directed therapy has made great improvement in pediatric sepsis survival • Oliveira et al showed that by following the recommendations, mortality in pediatric sepsis was reduced from 39% to 12%
Summary • Recognizing Sepsis early is important in decreasing mortality – Consider sepsis in the patient with fever, tachycardia, and altered mental status • Fluid boluses to begin within 5 minutes of suspecting sepsis – Bolus 20 cc/kg up to 60 cc/kg in 15 -20 mins – Start antibiotics as soon as possible
Summary • Start peripheral or central dopamine if fluid refractory shock – IV or IO; establish central venous access if possible • Titrate fluids, norepinephrine, packed red blood cells to ensure – Tachycardia, capillary refill, pulses and BP normalize – Lactate within normal, Scv. O 2>70% – Urine output >1 mg/kg/hr
Summary • For persistent severe septic shock consider the following: – Hydrocortisone – Thyroid replacement – ECMO – IVIG
Thank-you!