Pediatric Nutrition Management of SBR dehydration high ileostomy
Pediatric Nutrition: Management of SBR, dehydration, & high ileostomy output -The influential role of a Clinical Dietitian By Celina Chan
Dartmouth Hitchcock Medical Center- Lebanon �Founded 1893 �Teaching Hospital �Outpatient visits: 645, 857 �Employees 6, 724 Our Mission “We advance health through research, education, clinical practice and community partnerships, providing each person the best care, in the right place, at the right time, every time. ”
Dartmouth Hitchcock Medical Center- Lebanon � Beds: 396 � Mary Hitchcock Memorial Hospital � Geisel School of Medicine at Dartmouth � Children’s Hospital at Dartmouth-Hitchcock (Cha. D) � Norris Cotton Cancer Center
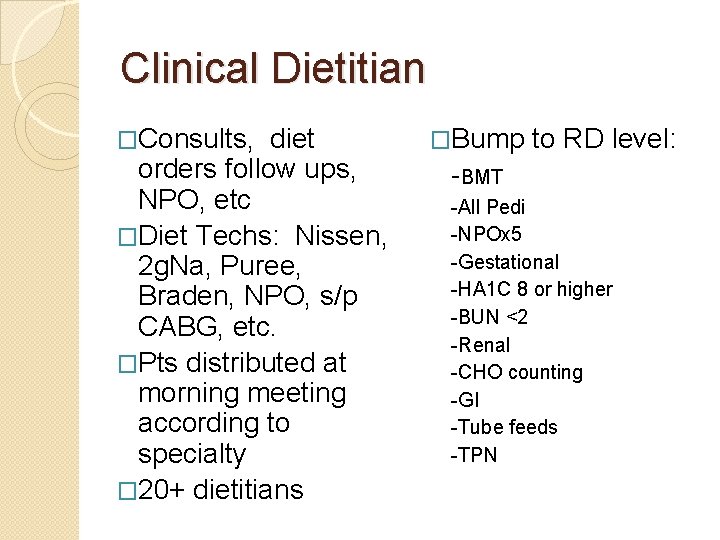
Clinical Dietitian �Consults, diet orders follow ups, NPO, etc �Diet Techs: Nissen, 2 g. Na, Puree, Braden, NPO, s/p CABG, etc. �Pts distributed at morning meeting according to specialty � 20+ dietitians �Bump to RD level: -BMT -All Pedi -NPOx 5 -Gestational -HA 1 C 8 or higher -BUN <2 -Renal -CHO counting -GI -Tube feeds -TPN
Outline �Pt introduction & history �Diagnosis �Assessment �Nutrition diagnosis �Intervention (MNT) �Monitoring �Evaluation
Patient History-Baby J �Male, Full term 38 wk �Birth date: 8/25/14 --- d/c 10/9 (~6 wk old) �Readmitted 10/12 �Gastroschisis �Ileal Atresia �Short Bowel Resection (SBR) �Ileostomy �Dehydration
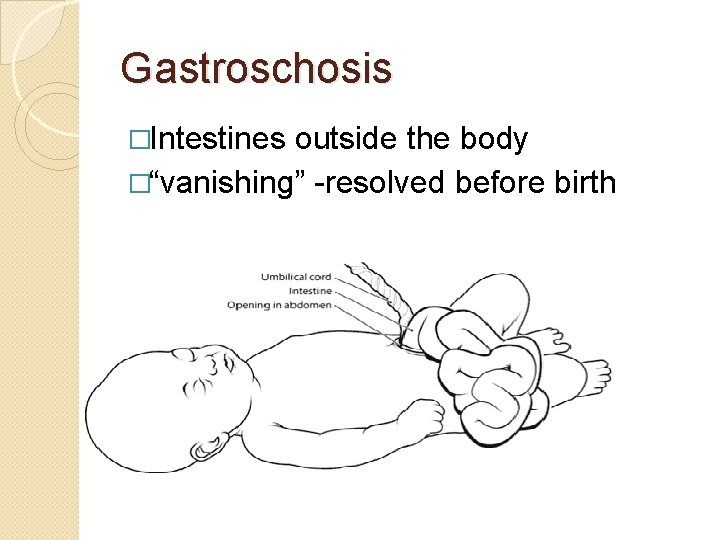
Gastroschosis �Intestines outside the body �“vanishing” -resolved before birth
Pathogenesis & Etiology ◦ ◦ Abdominal wall birth defect CDC estimates 1, 871 babies/yr Abdominal wall does not form correctly Intestines are outside the body (not covered by sac). Typically to the right of the umbilical cord ◦ Damage occurs from exposure to amniotic fluid (irritation, swelling, twisting, atreasia) ◦ Potential for future difficulty feeding pt
Pathogenesis & Etiology cont… ◦ Theories: �Failure of differentiation of embryonic cells �Rupture of amniotic membrane near umbilical cord �Abnormalities near umbilical cord �Necrosis of cord leading to gut herniation �Development failure at abdominal folds creating improper closure ◦ Many theories, but still unclear understanding of the disease ◦ Risk factors: young mother, alcohol & tobacco, poor nutrition (or failure to take prenatal supplements)
Treatment �Treatment ◦ Surgery ◦ “vanishing” – self resolves (surgery still needed to close the abdominal wall) ◦ Further complications requiring treatment may occur
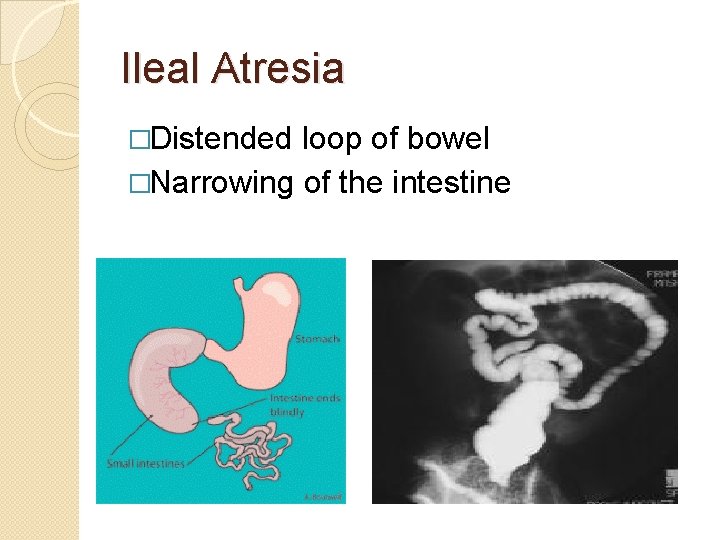
Ileal Atresia �Distended loop of bowel �Narrowing of the intestine
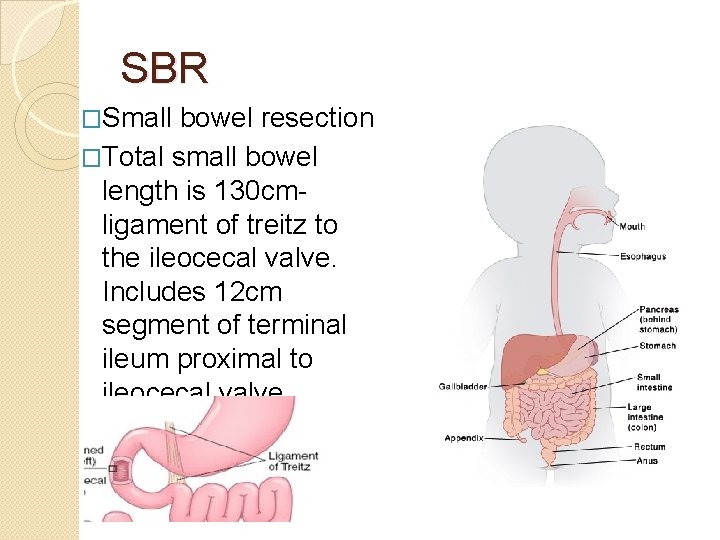
SBR �Small bowel resection �Total small bowel length is 130 cm- ligament of treitz to the ileocecal valve. Includes 12 cm segment of terminal ileum proximal to ileocecal valve.
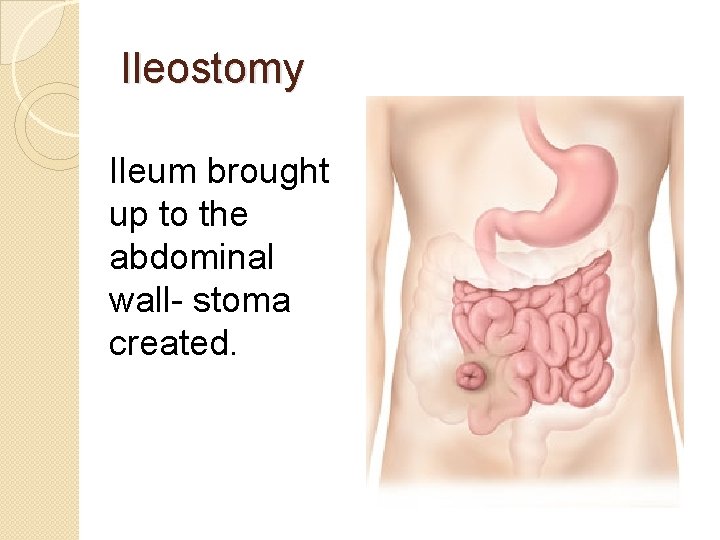
Ileostomy Ileum brought up to the abdominal wall- stoma created.
Dehydration � -watery stool, gassy, not taking bottle, no wet diaper for 12 hrs, mottling, lethargy, crying, irritable, vomiting, diarrhea, decreased urine volume, pallor � Took in about 300 -360 m. L formula at home. Parents unsure � Mom mixing wrong recipe � Current Weight: 2. 9 kg � Weight at previous discharge: 3. 34 kg � Na: 125 mmol/L (L) � K: 6. 8 mmol/L (H) � CL: 93 mmol/L (L) � CO 2: 10 mmol/L (L)
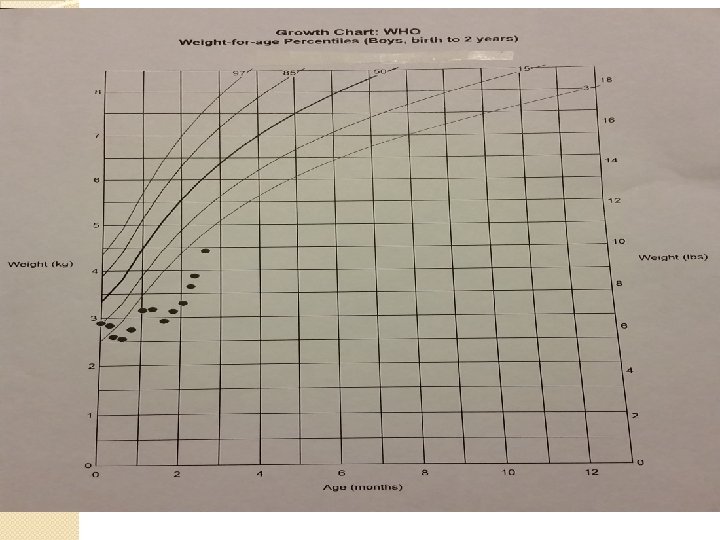
Nutrition Considerations �Weight �Growth Chart �Electrolytes �I’s & O’s �Ileostomy output �Food History �Needs �Formula

PES �Decreased energy intake related to inadequate oral consumption as evidenced by parent report of pts food refusal �Altered GI function related to SBR and ileostomy placement, as evidenced by increased ileostomy output of >2 ml/kg/hr and a positive fecal fat test. �*this is the primary PES statement.
Goals �Resolve dehydration— provide appropriate formula and monitor intake �Stool output <50 ml/kg/day or <2 ml/kg/hr �Electrolytes & labs wnl �Weight maintenance gain (recommend caloric goal of 150 kcal/kg) �*treated as a “functional” short gut pt
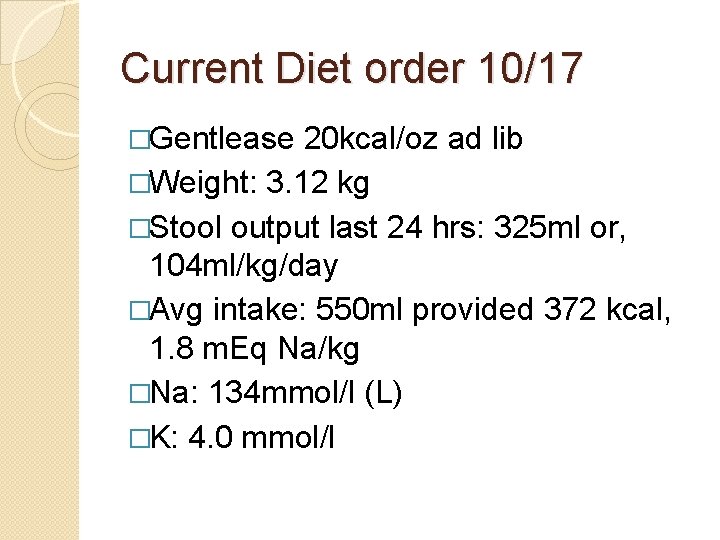
Current Diet order 10/17 �Gentlease 20 kcal/oz ad lib �Weight: 3. 12 kg �Stool output last 24 hrs: 325 ml or, 104 ml/kg/day �Avg intake: 550 ml provided 372 kcal, 1. 8 m. Eq Na/kg �Na: 134 mmol/l (L) �K: 4. 0 mmol/l
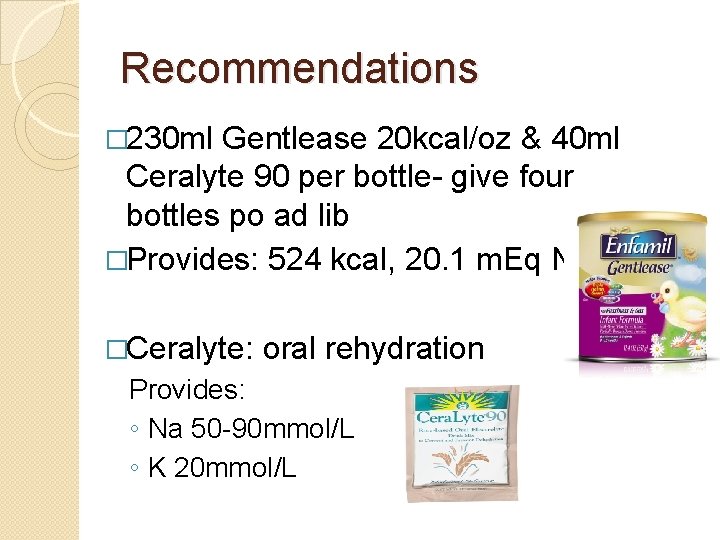
Recommendations � 230 ml Gentlease 20 kcal/oz & 40 ml Ceralyte 90 per bottle- give four bottles po ad lib �Provides: 524 kcal, 20. 1 m. Eq Na �Ceralyte: oral rehydration Provides: ◦ Na 50 -90 mmol/L ◦ K 20 mmol/L

Follow up- 10/21 � 230 ml Gentlease 20 kcal/oz & 40 ml Ceralyte 90 per bottle- give four bottles po ad lib �Provides: 524 kcal, 20. 1 m. Eq Na �Previous weight: 3. 12 kg �Current Weight: 3. 17 kg �Na: 135 mmol/L �Stool output: 257 m. L = 3. 3 ml/kg/hr
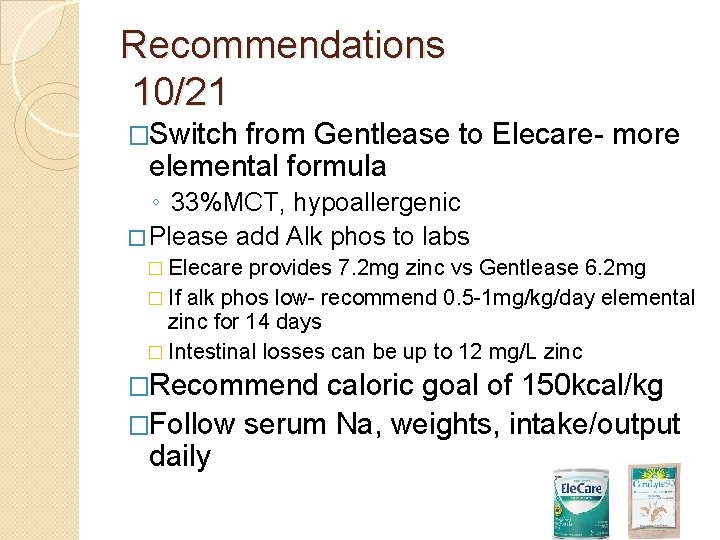
Recommendations 10/21 �Switch from Gentlease to Elecare- more elemental formula ◦ 33%MCT, hypoallergenic � Please add Alk phos to labs � Elecare provides 7. 2 mg zinc vs Gentlease 6. 2 mg � If alk phos low- recommend 0. 5 -1 mg/kg/day elemental zinc for 14 days � Intestinal losses can be up to 12 mg/L zinc �Recommend caloric goal of 150 kcal/kg �Follow serum Na, weights, intake/output daily
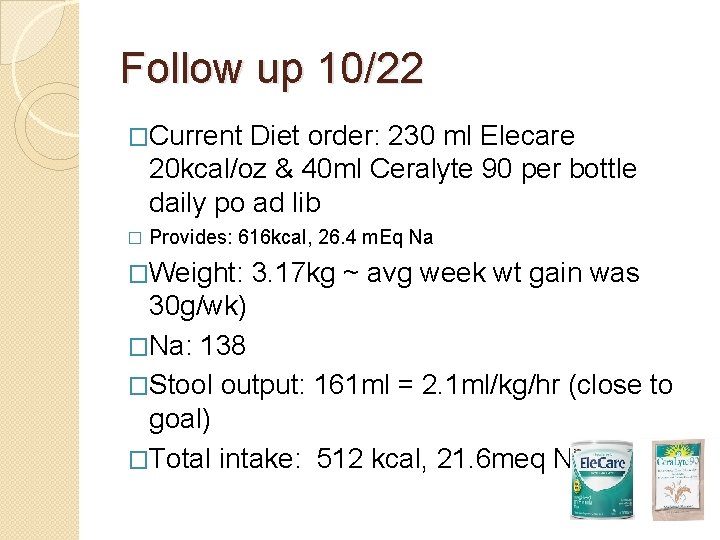
Follow up 10/22 �Current Diet order: 230 ml Elecare 20 kcal/oz & 40 ml Ceralyte 90 per bottle daily po ad lib � Provides: 616 kcal, 26. 4 m. Eq Na �Weight: 3. 17 kg ~ avg week wt gain was 30 g/wk) �Na: 138 �Stool output: 161 ml = 2. 1 ml/kg/hr (close to goal) �Total intake: 512 kcal, 21. 6 meq Na
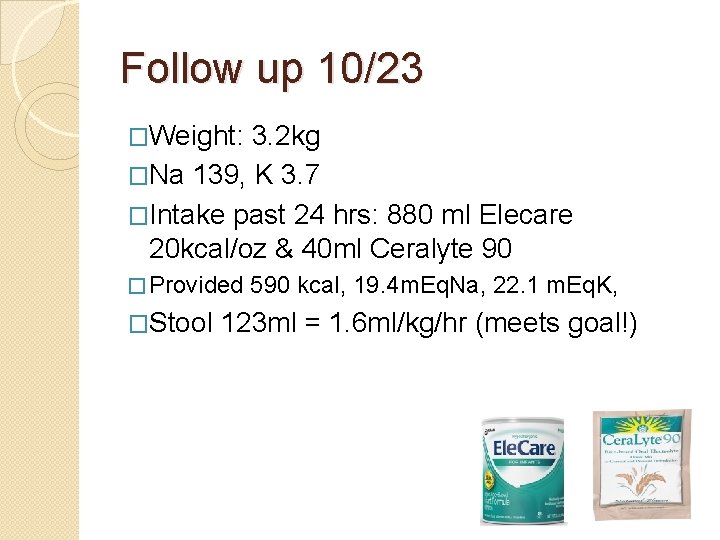
Follow up 10/23 �Weight: 3. 2 kg �Na 139, K 3. 7 �Intake past 24 hrs: 880 ml Elecare 20 kcal/oz & 40 ml Ceralyte 90 � Provided 590 kcal, 19. 4 m. Eq. Na, 22. 1 m. Eq. K, �Stool 123 ml = 1. 6 ml/kg/hr (meets goal!)
Recommendations �D/c Ceralyte…try with pectin �Start with 0. 6 ml pectin/120 ml Elecare can increase to 1. 2 ml/120 ml if stool still has not thickened
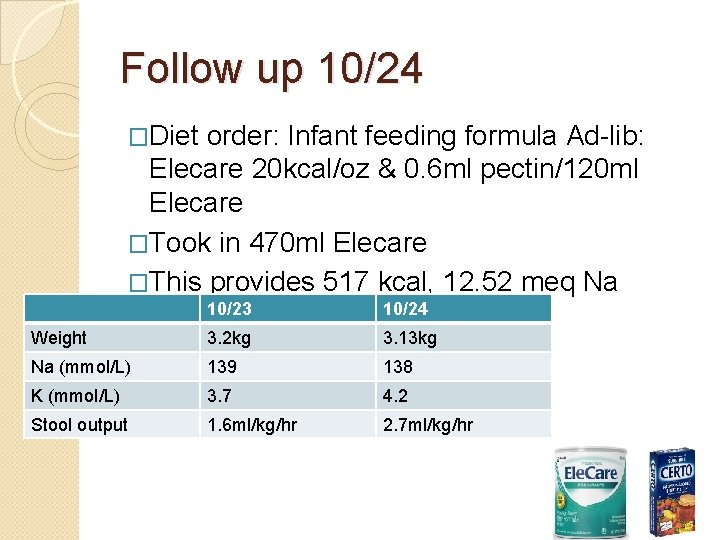
Follow up 10/24 �Diet order: Infant feeding formula Ad-lib: Elecare 20 kcal/oz & 0. 6 ml pectin/120 ml Elecare �Took in 470 ml Elecare �This provides 517 kcal, 12. 52 meq Na 10/23 10/24 Weight 3. 2 kg 3. 13 kg Na (mmol/L) 139 138 K (mmol/L) 3. 7 4. 2 Stool output 1. 6 ml/kg/hr 2. 7 ml/kg/hr
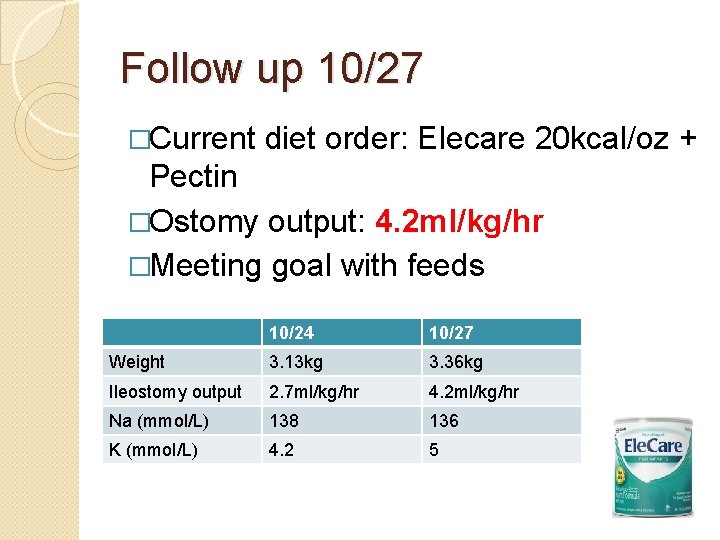
Follow up 10/27 �Current diet order: Elecare 20 kcal/oz + Pectin �Ostomy output: 4. 2 ml/kg/hr �Meeting goal with feeds 10/24 10/27 Weight 3. 13 kg 3. 36 kg Ileostomy output 2. 7 ml/kg/hr 4. 2 ml/kg/hr Na (mmol/L) 138 136 K (mmol/L) 4. 2 5
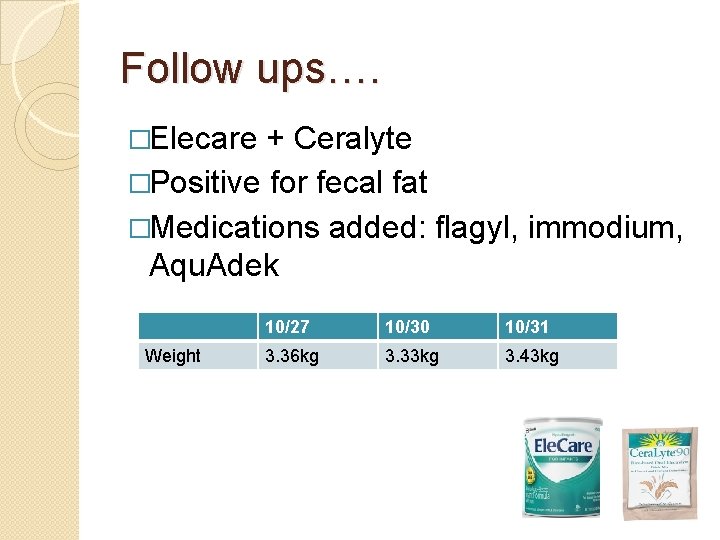
Follow ups…. �Elecare + Ceralyte �Positive for fecal fat �Medications added: flagyl, immodium, Aqu. Adek Weight 10/27 10/30 10/31 3. 36 kg 3. 33 kg 3. 43 kg
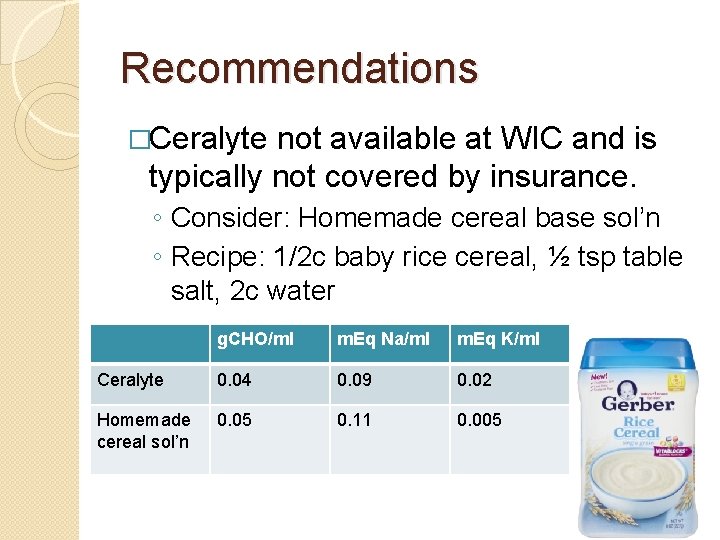
Recommendations �Ceralyte not available at WIC and is typically not covered by insurance. ◦ Consider: Homemade cereal base sol’n ◦ Recipe: 1/2 c baby rice cereal, ½ tsp table salt, 2 c water g. CHO/ml m. Eq Na/ml m. Eq K/ml Ceralyte 0. 04 0. 09 0. 02 Homemade cereal sol’n 0. 05 0. 11 0. 005
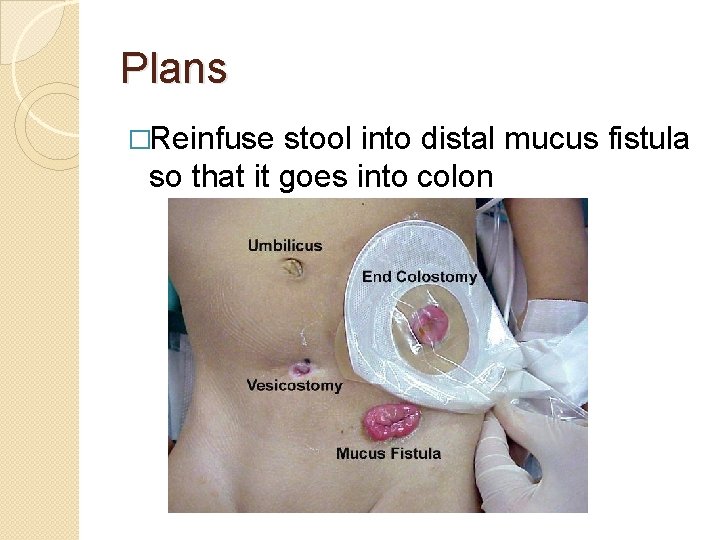
Plans �Reinfuse stool into distal mucus fistula so that it goes into colon
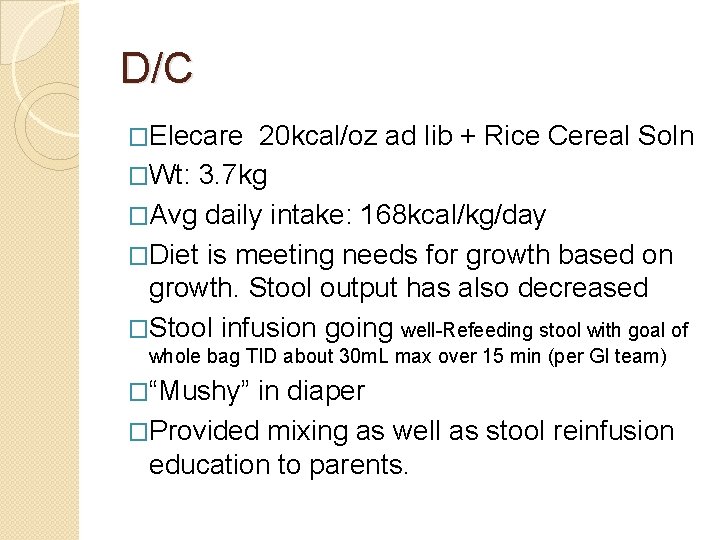
D/C �Elecare 20 kcal/oz ad lib + Rice Cereal Soln �Wt: 3. 7 kg �Avg daily intake: 168 kcal/kg/day �Diet is meeting needs for growth based on growth. Stool output has also decreased �Stool infusion going well-Refeeding stool with goal of whole bag TID about 30 m. L max over 15 min (per GI team) �“Mushy” in diaper �Provided mixing as well as stool reinfusion education to parents.

Summary �Gentlease + Ceralyte Elecare + Ceralyte Elecare + Pectin Elecare + Rice Sol’n (to mimic ceralyte) � Flagyl, aquadek
Final Thoughts �Initiation of Elecare �Pectin? �Complicated situation: ◦ more than one solution: “many right answers, obvious wrong answers” ◦ Team effort (Pedi MDs, Dietitians, GI team, pedi, etc)
References Pediatric Nutrition Care Manual � Hendricks, KM, Duggan, C. Chp 36 - Short Bowel Syndrome. In Manual of pediatric nutrition. Hamilton, Ontario: BC Decker; 2005: 718 -735. https: //www. childrenshospital. org/~/media/Centers%20 and%20 Serv ices/Programs/A_E/Center%20 for%20 Advanced%20 Intestinal% 20 Rehabilitation/Hendricks%20 Ch%2036. ashx � Mattei, P. Fundamentals of pediatric surgery. New York: Springer; 2011. � Weaver LT, Austin S, Cole TJ. Small intestinal length: a factor essential for gut adaptation. Gut 1991; 32(11): 1321 -1323. � Leonberg, BL. ADA pocket guide to pediatric nutrition assessment. Chicago: American Dietetic Association; 2008. � Groh-Wargo, S, Thompson, M, Cox, JH. ADA pocket guide to neonatal nutrition. Chicago, IL: American Dietetic Association; 2009. � Wong, KKY, Lan, LCL, Lin, SCL, Chan, AWS, Tam, PKH. Mucous Fistula Refeeding in Premature Neonates With Enterostomies. Journal of Pediatric Gastroenterology and Nutrition. 2004; 39(1): 43 -45. doi: 10. 1097/00005176 -20040700000009. �
References (photos) � http: //acareotc. caraudio. netdna- cdn. com/media/catalog/product/cache/1/image/500 x 500/9 df 78 eab 33525 d 08 d 6 e 5 fb 8 d 27 136 e 95/4/0/404925. Jpg � http: //www. convatec. com/media/12324/ileostomy-copy. jpg � http: //www. columbusfetalmedicine. org/images/gastroschisis-1. png � http: //img. medscape. com/pi/emed/ckb/radiology/336139 -409746 -10248 tn. jpg � https: //www. luriechildrens. org/en-us/care-services/conditions-treatments/fetal-intestinal- atresia/Publishing. Images/Low. Atresia_sm_new. gif � http: //fce-study. netdna-ssl. com/2/images/upload-flashcards/60/80/54/5608054_m. jpg � http: //www. uofmchildrenshospital. org/fv/groups/public/documents/images/95145. jpg � http: //static. abbottnutrition. com/cms-prod/abbottnutrition. com/img/06 -07 -2011 -01 -16 - 05_Ele. Care_Infant. jpg � http: //g-ecx. images-amazon. com/images/G/01/hpc/detail-page/c 26 -B 0026 RHUO 4 -1 - l. jpg � http: //www. jocosarblog. org/. a/6 a 0105364 e 2 a 0 e 970 b 01157193 be 95970 b-pi � http: //c 4. diapers. com/images/products/p/ns/ns-688_1 z. jpg � http: //www. chadkids. org/images/DHMC_location. jpg � http: //www. brplusa. com/images/projects/healthcare/dhmc_aerial_fs. jpg
- Slides: 35