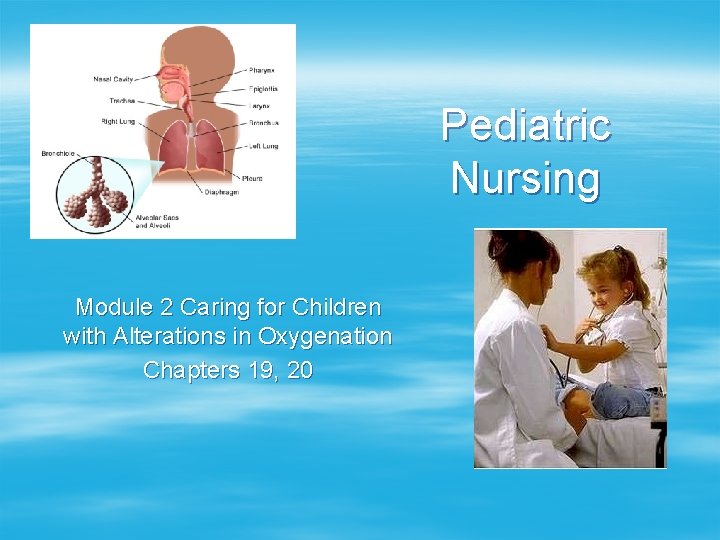
Pediatric Nursing Module 2 Caring for Children with




- Slides: 34
Pediatric Nursing Module 2 Caring for Children with Alterations in Oxygenation Chapters 19, 20
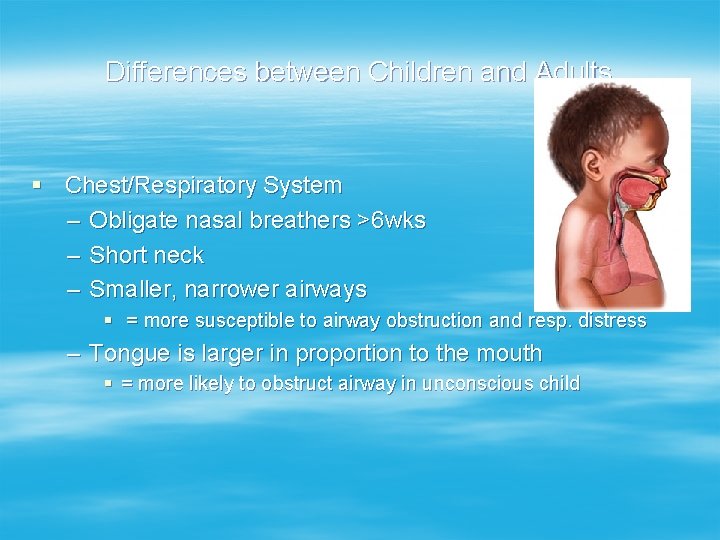
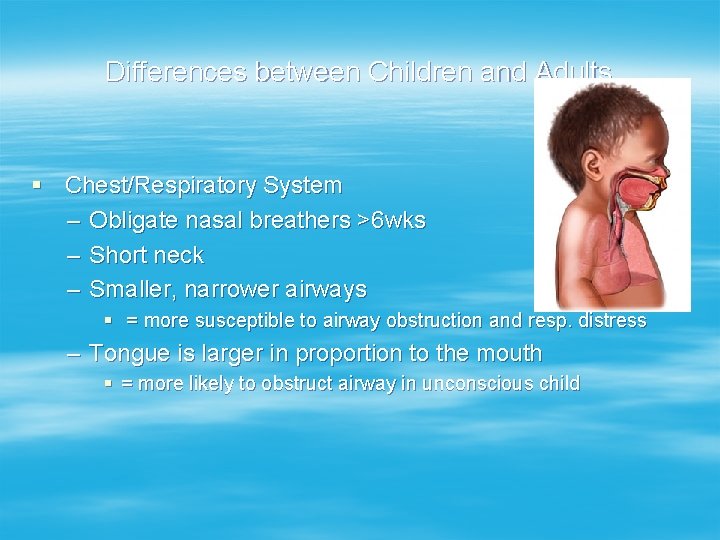
Differences between Children and Adults § Chest/Respiratory System – Obligate nasal breathers >6 wks – Short neck – Smaller, narrower airways § = more susceptible to airway obstruction and resp. distress – Tongue is larger in proportion to the mouth § = more likely to obstruct airway in unconscious child
Differences between Children and Adults § Chest/Respiratory System – Smaller lung capacity and underdeveloped intercostal muscles, poor chest musculature § = less pulmonary reserve, lung damage w/o fx – Children rely on diaphragm breathing § = high risk for resp. failure if the diaphragm unable to contract
Adjunct Assessments § Temperature – Febrile state increases oxygen consumption § Fluid Needs – Vomiting/diarrhea are commonly associated with respiratory illness – Increase respiratory efforts, increased fluid losses with decreased po intake requires an increase in fluid needs
Respiratory System § Inspection – Chest § Size, symmetry movement § Infancy shape is almost circular § < 6 -7 years respiratory movement primarily abdominal or diaphragmatic – Respirations § Rate, rhythm, depth, quality, effort § >60 /min in small children = significant respiratory distress
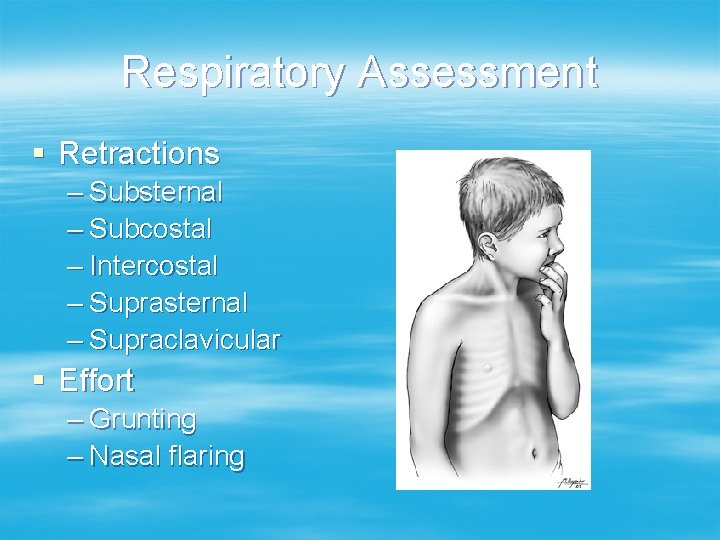
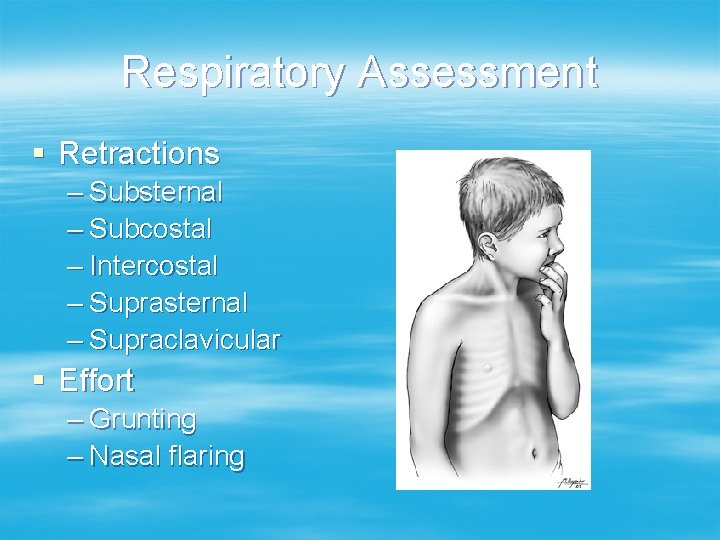
Respiratory Assessment § Retractions – Substernal – Subcostal – Intercostal – Suprasternal – Supraclavicular § Effort – Grunting – Nasal flaring
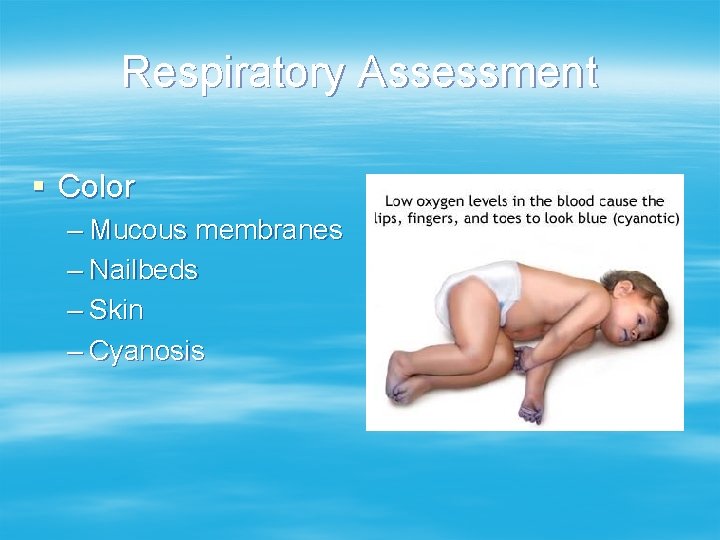
Respiratory Assessment § Color – Mucous membranes – Nailbeds – Skin – Cyanosis
Respiratory Assessment § Auscultation – Listen comparing one areas to the other § § § Equality of breath sounds Diminished Poor air exchange – Abnormal breath sounds § § Rales Rhonchi Wheezing Grunting – Present on inspiration or expiration
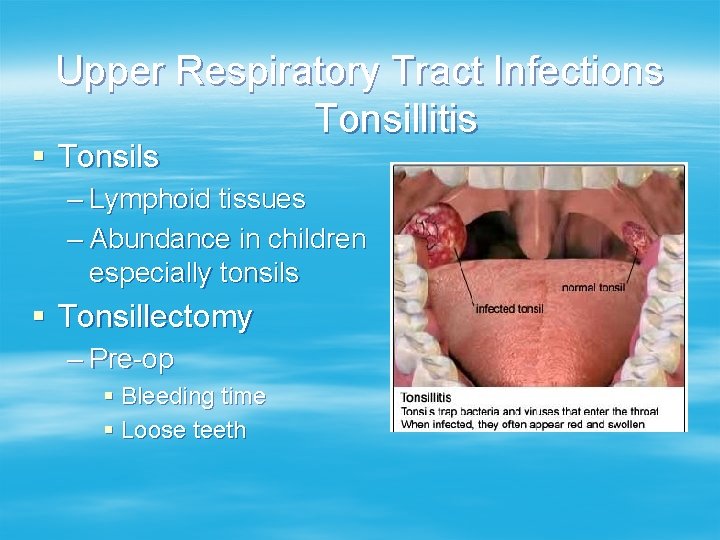
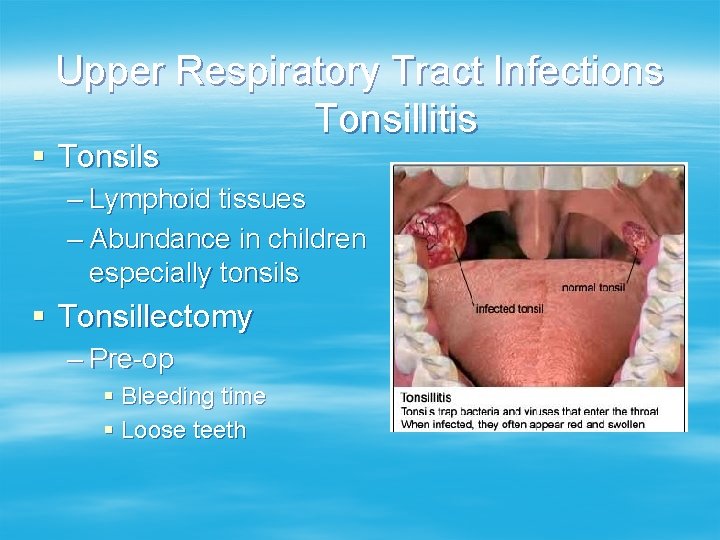
Upper Respiratory Tract Infections Tonsillitis § Tonsils – Lymphoid tissues – Abundance in children especially tonsils § Tonsillectomy – Pre-op § Bleeding time § Loose teeth
Tonsillectomy § Post-op – T & A position § Semi prone with head turned to the side – Monitor for bleeding § § § Frequent swallowing Persistent pulse of 120 or greater at rest Restlessness Pallor Vomiting bright red blood May bleed for 5 -10 days post-op – Home care § Diet
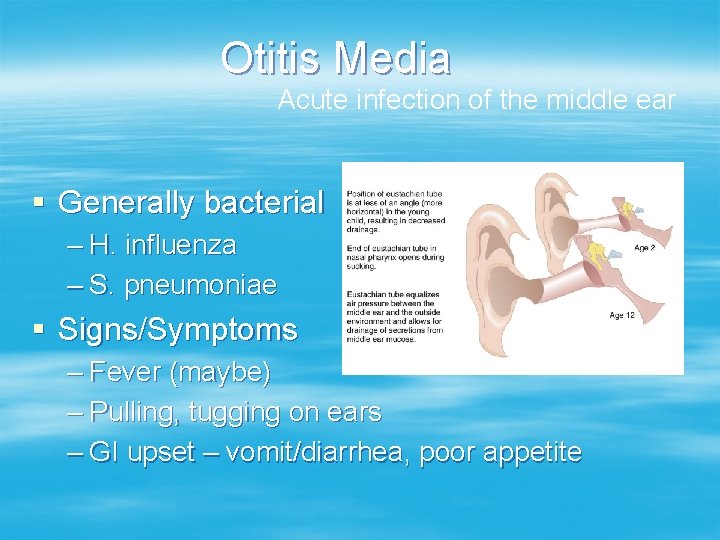
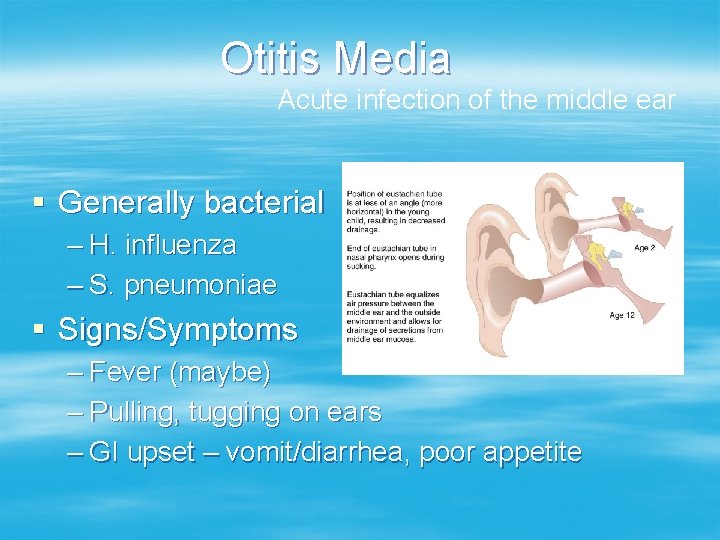
Otitis Media Acute infection of the middle ear § Generally bacterial – H. influenza – S. pneumoniae § Signs/Symptoms – Fever (maybe) – Pulling, tugging on ears – GI upset – vomit/diarrhea, poor appetite
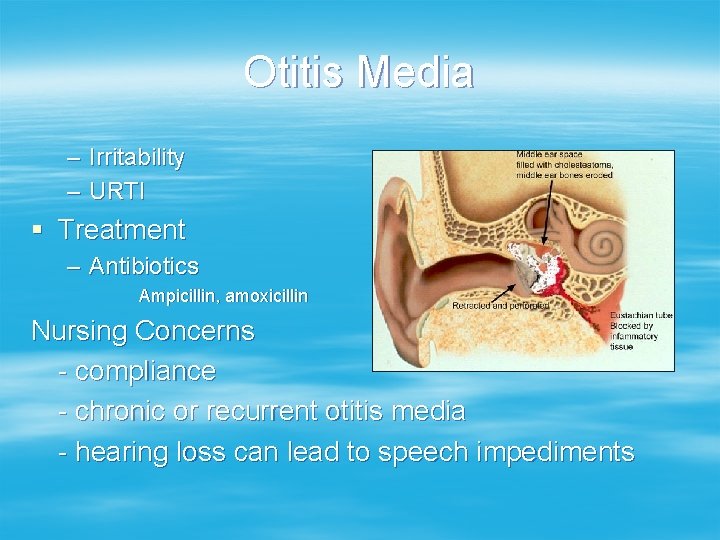
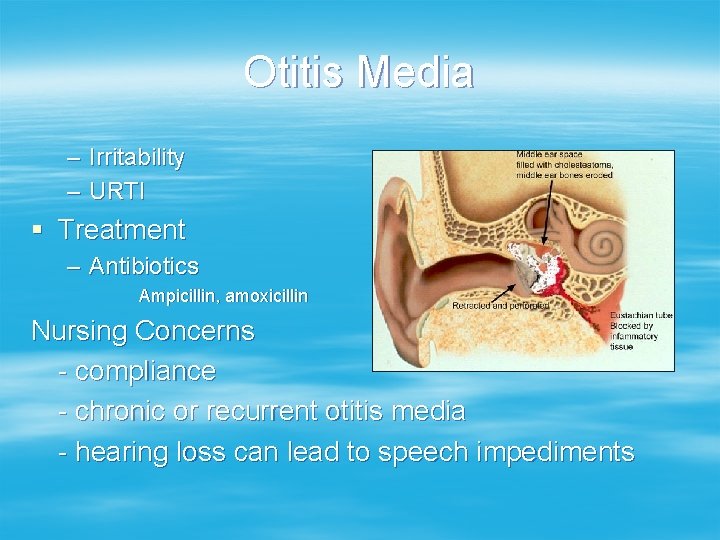
Otitis Media – Irritability – URTI § Treatment – Antibiotics Ampicillin, amoxicillin Nursing Concerns - compliance - chronic or recurrent otitis media - hearing loss can lead to speech impediments
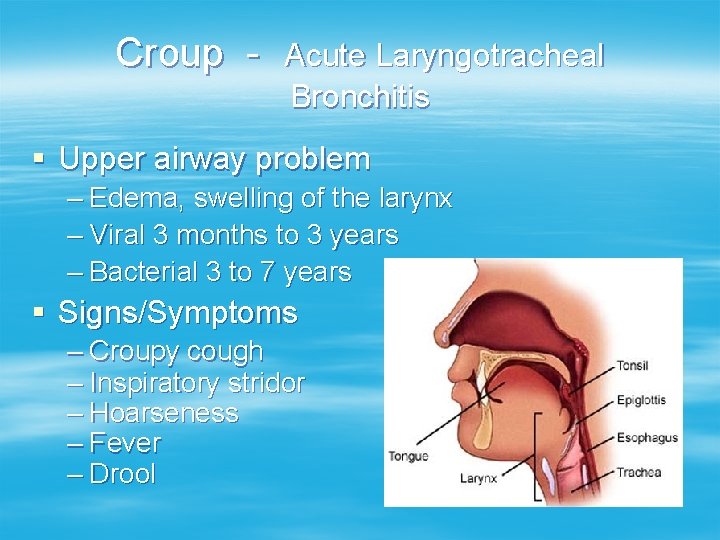
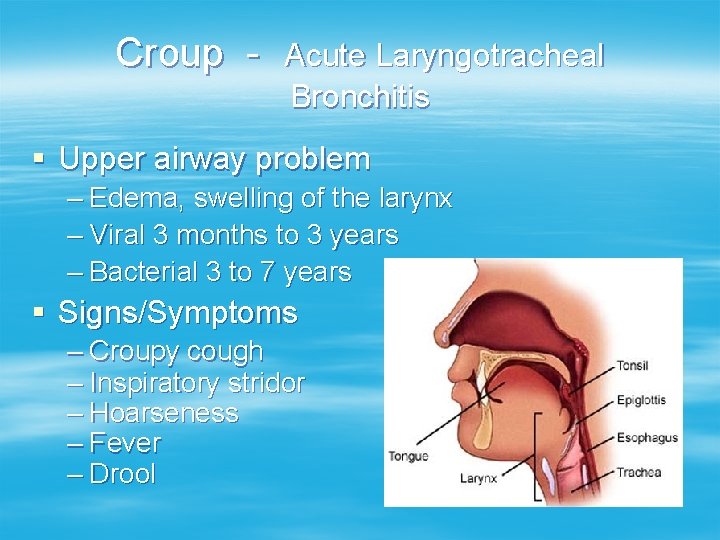
Croup - Acute Laryngotracheal Bronchitis § Upper airway problem – Edema, swelling of the larynx – Viral 3 months to 3 years – Bacterial 3 to 7 years § Signs/Symptoms – Croupy cough – Inspiratory stridor – Hoarseness – Fever – Drool
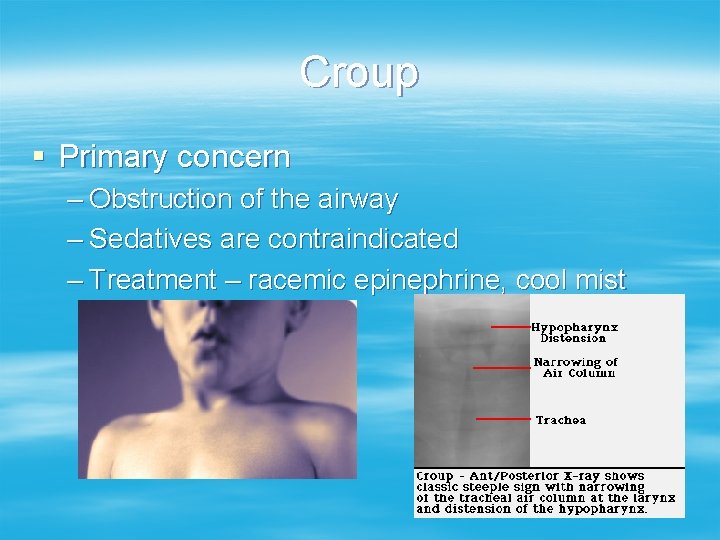
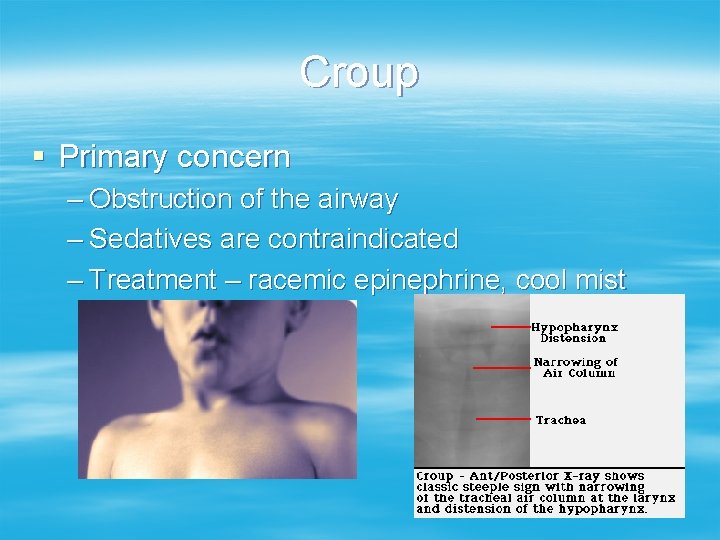
Croup § Primary concern – Obstruction of the airway – Sedatives are contraindicated – Treatment – racemic epinephrine, cool mist
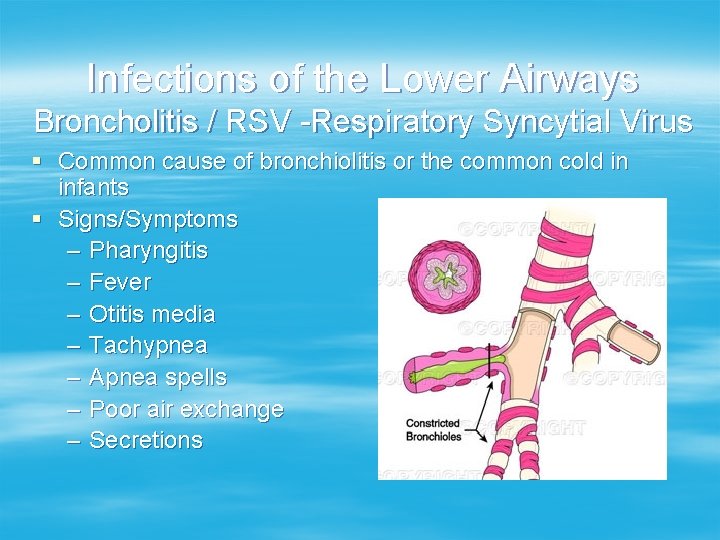
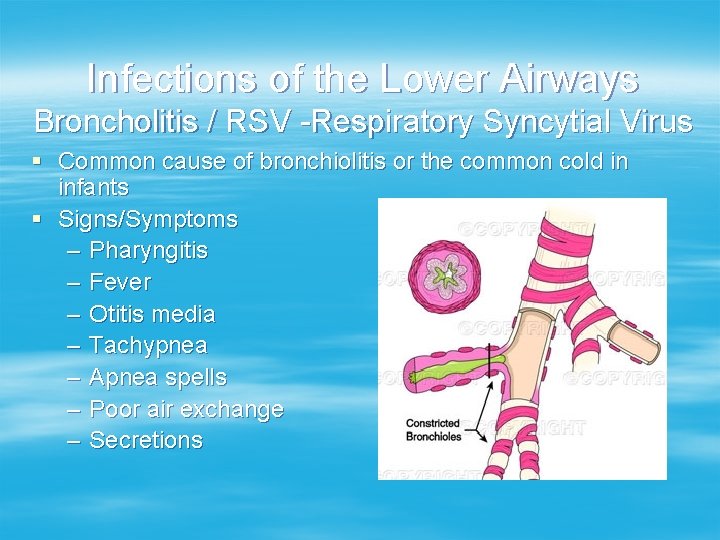
Infections of the Lower Airways Broncholitis / RSV -Respiratory Syncytial Virus § Common cause of bronchiolitis or the common cold in infants § Signs/Symptoms – Pharyngitis – Fever – Otitis media – Tachypnea – Apnea spells – Poor air exchange – Secretions
RSV § Treatment – Aerosol respiratory treatments – Supplemental 02 – Vaccine for high risk infants
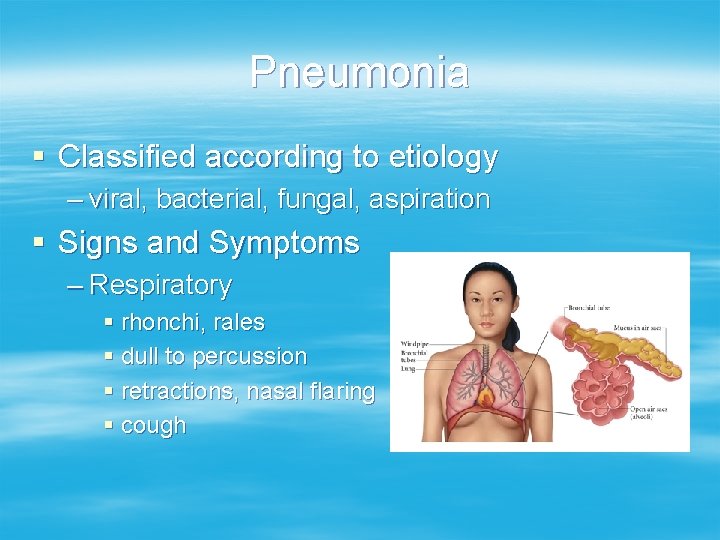
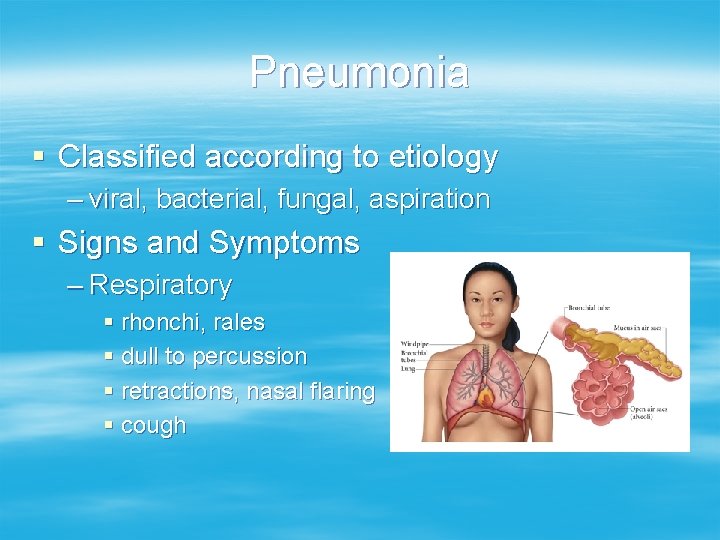
Pneumonia § Classified according to etiology – viral, bacterial, fungal, aspiration § Signs and Symptoms – Respiratory § rhonchi, rales § dull to percussion § retractions, nasal flaring § cough
Pneumonia – Systemic § high fever – Neurological § irritable, restless, lethargic § pain – Gastrointestinal § a/v/d § abdominal pain
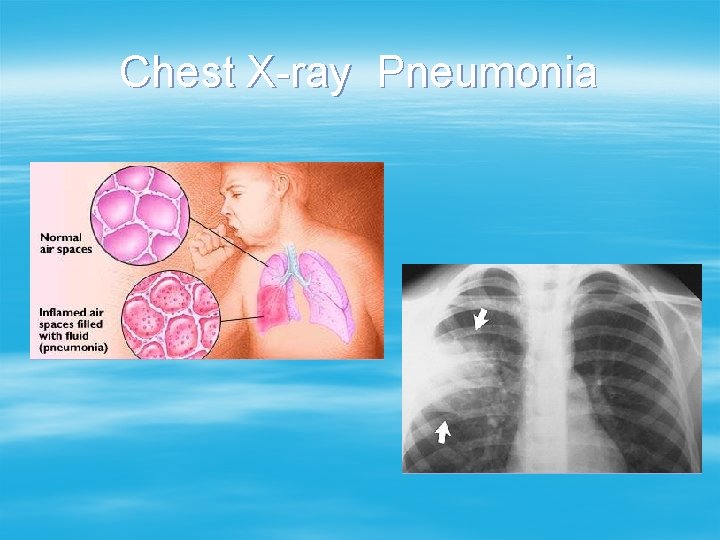
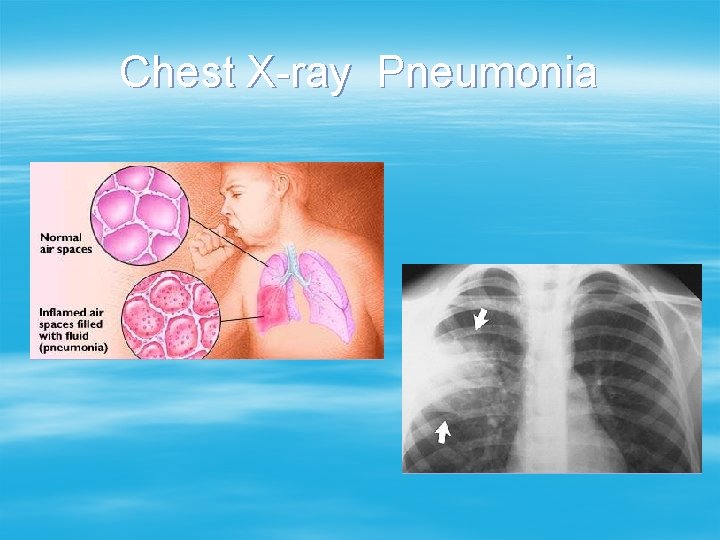
Chest X-ray Pneumonia
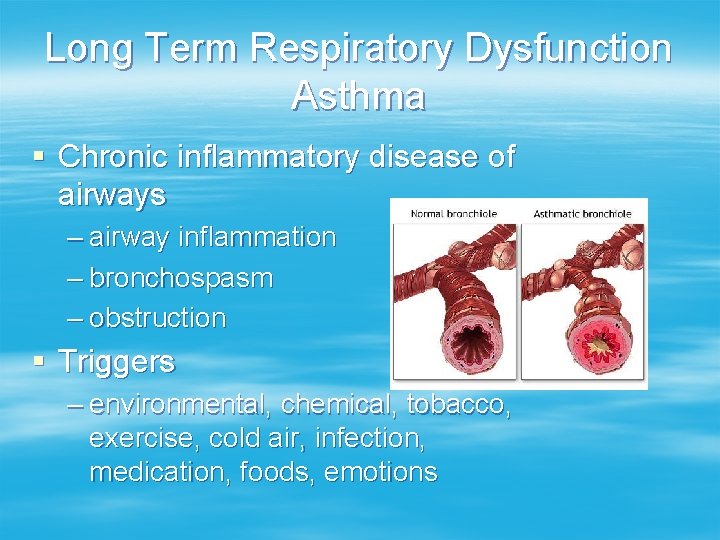
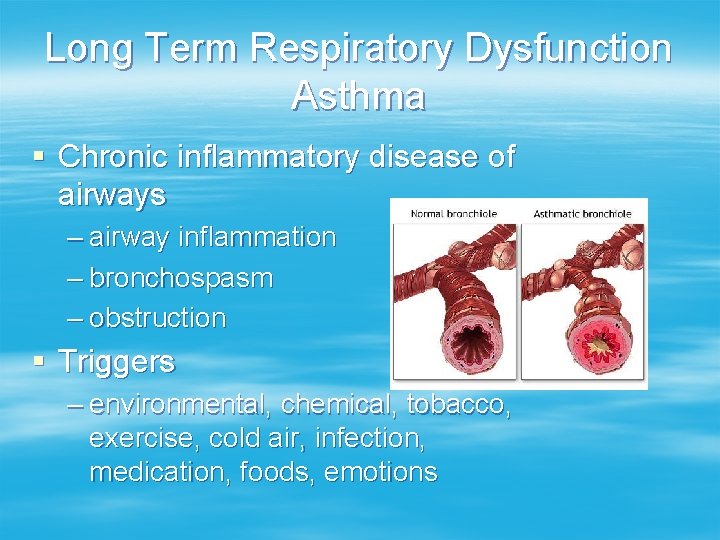
Long Term Respiratory Dysfunction Asthma § Chronic inflammatory disease of airways – airway inflammation – bronchospasm – obstruction § Triggers – environmental, chemical, tobacco, exercise, cold air, infection, medication, foods, emotions
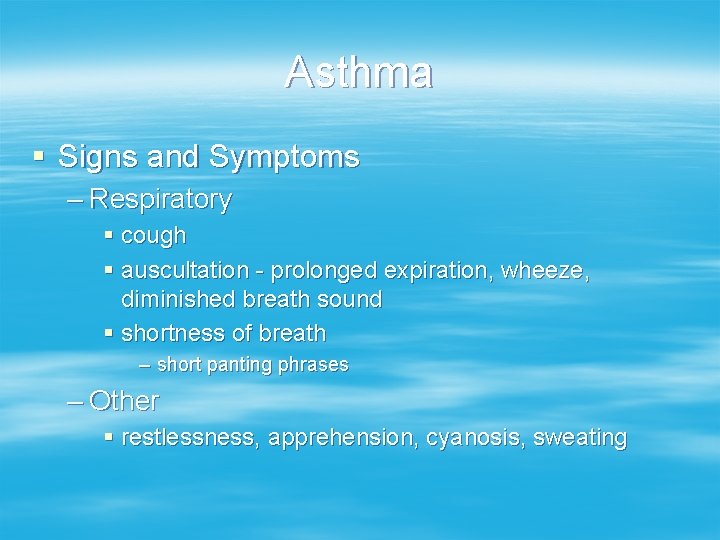
Asthma § Signs and Symptoms – Respiratory § cough § auscultation - prolonged expiration, wheeze, diminished breath sound § shortness of breath – short panting phrases – Other § restlessness, apprehension, cyanosis, sweating

Cystic Fibrosis
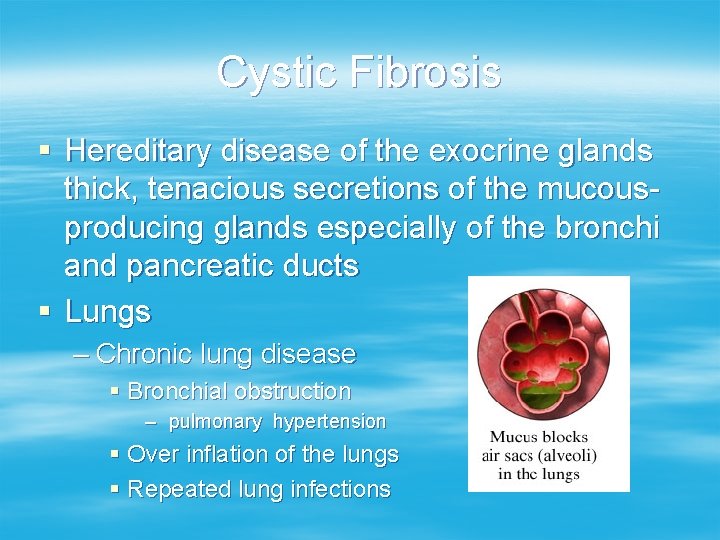
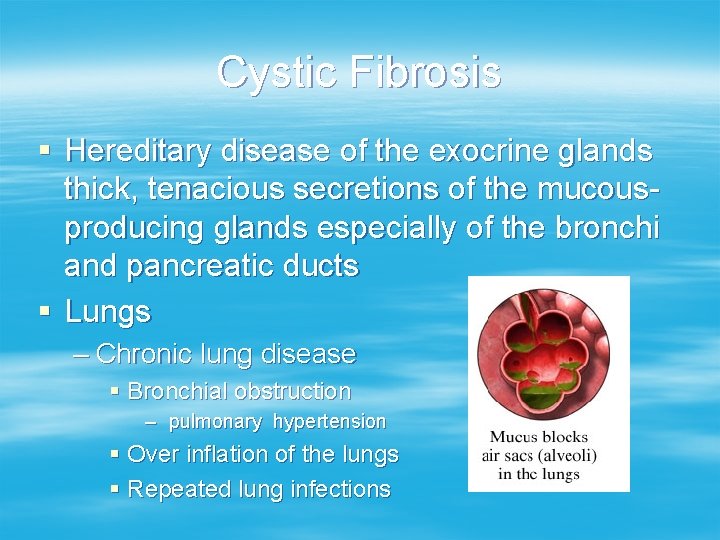
Cystic Fibrosis § Hereditary disease of the exocrine glands thick, tenacious secretions of the mucousproducing glands especially of the bronchi and pancreatic ducts § Lungs – Chronic lung disease § Bronchial obstruction – pulmonary hypertension § Over inflation of the lungs § Repeated lung infections
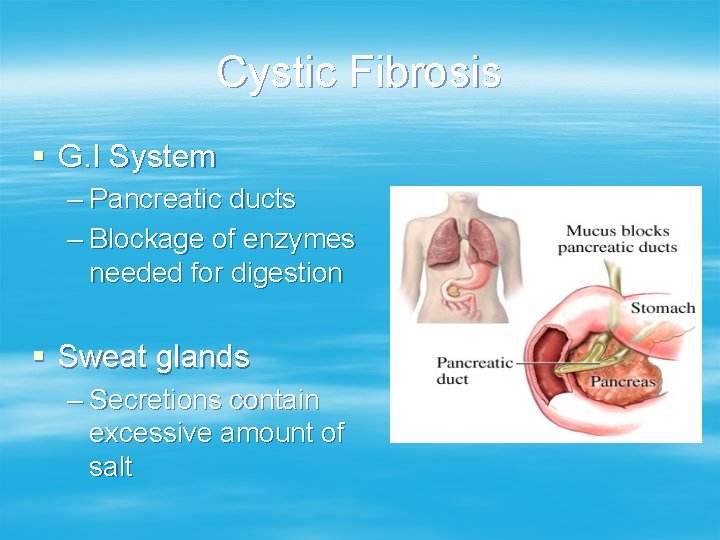
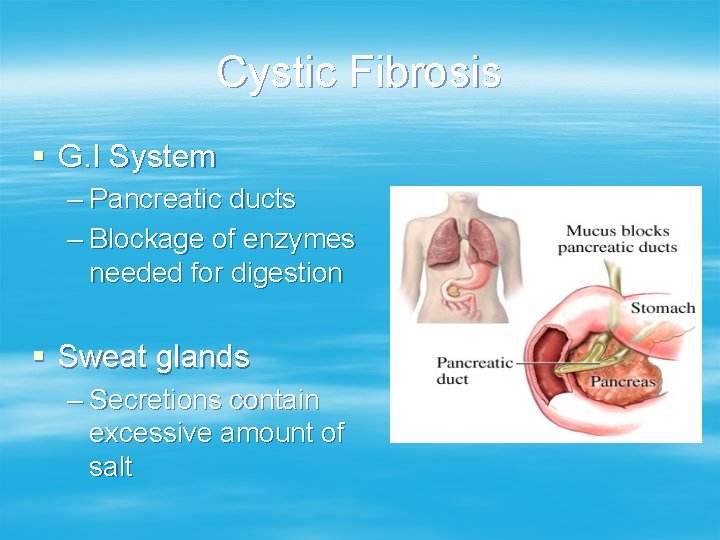
Cystic Fibrosis § G. I System – Pancreatic ducts – Blockage of enzymes needed for digestion § Sweat glands – Secretions contain excessive amount of salt
Cystic Fibrosis § Signs/symptoms – Newborn meconium ileus – Tastes salty when kissed – Recurrent respiratory illnesses – Failure to gain weight with a good appetite – Malasbsorption of fats and proteins § Stools are foul smelling, frothy and bulky § Pot belly with wasted buttocks
Cystic Fibrosis § Diagnosis – Family history of CF – Repeated illnesses/hospitalization with respiratory problems or failure to thrive – Absence of pancreatic enzyme or stool studies – + sweat chloride tests § Concentration of Cl > 60 m. Eq/L
Cystic Fibrosis § Treatment – Nutritional § Pancreatic enzymes with meals and snacks § Vitamin replacement – A, D, E, K § High protein, high calorie diet – Pulmonary § Thin the secretions, keep them mobile – CPT – Aerosol Treatment § bronchodilators, D-nase
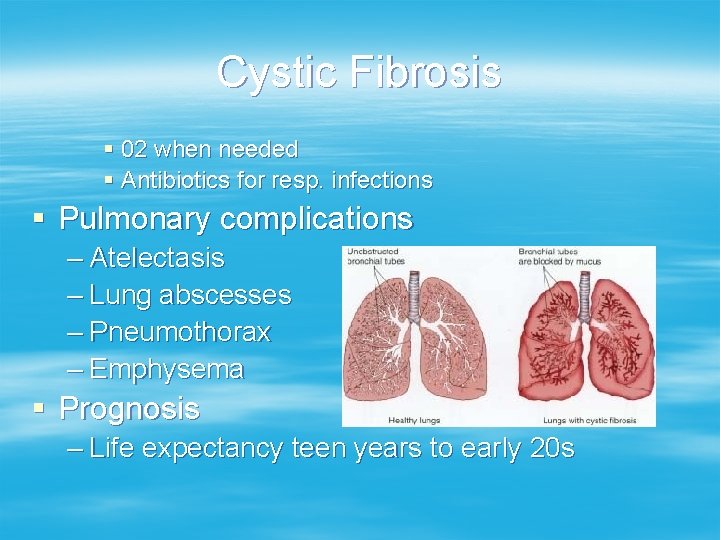
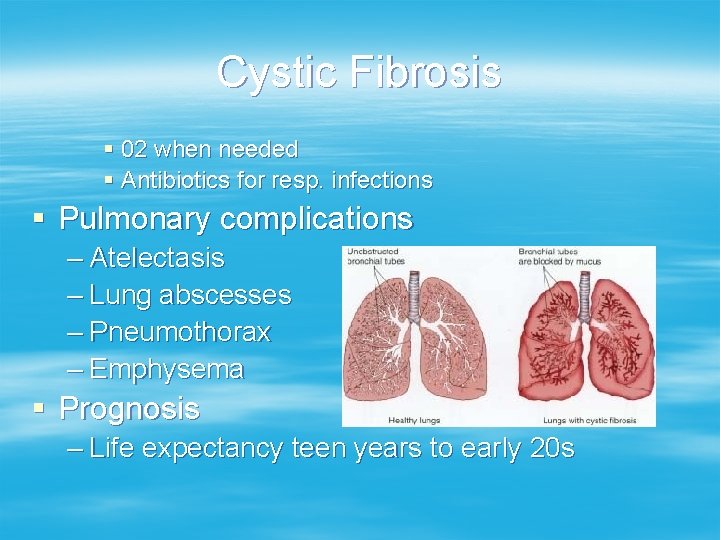
Cystic Fibrosis § 02 when needed § Antibiotics for resp. infections § Pulmonary complications – Atelectasis – Lung abscesses – Pneumothorax – Emphysema § Prognosis – Life expectancy teen years to early 20 s

Respiratory – Nursing Diagnosis § § § § § Impaired gas exchange Ineffective airway clearance Ineffective breathing pattern High risk fluid volume deficit Altered tissue perfusion Anxiety Activity Intolerance Altered growth/development Knowledge deficit
Respiratory – Nursing Diagnosis § § PC: Atelectasis/Pneumonia PC: Electrolyte Imbalance PC: Hemorrhage PC: Hypoxia
Nursing Interventions § Assess respiratory status – Tachypnea, labored breathing, shallow breathing – Effort § Retractions § Nasal flaring § Head bobbing – Grunting – Apnea – Poor air exchange – 02 saturation

Nursing Interventions § Oxygenation/ventilation needs – Administer O 2 § Incubator/oxygen hood § Nasal prongs § Mist tent – Tracheotomy – croup § Decrease respiratory efforts § Infant car seat § Knee-chest position
Nursing Interventions § Maintain airway – Head tilt – do not hyper extend neck – Aerosol treatment – CPT – Suction bulb syringe, BBG or tracheal bronchial § Fluids – IV or po

Nursing Interventions § § § Labs Medications Conserve energy – Organize care § Monitor vital signs § Teaching