Pediatric Neurosurgery Baar Atalay M D Yeditepe University
Pediatric Neurosurgery Başar Atalay M. D. Yeditepe University Faculty of Medicine Department of Neurosurgery
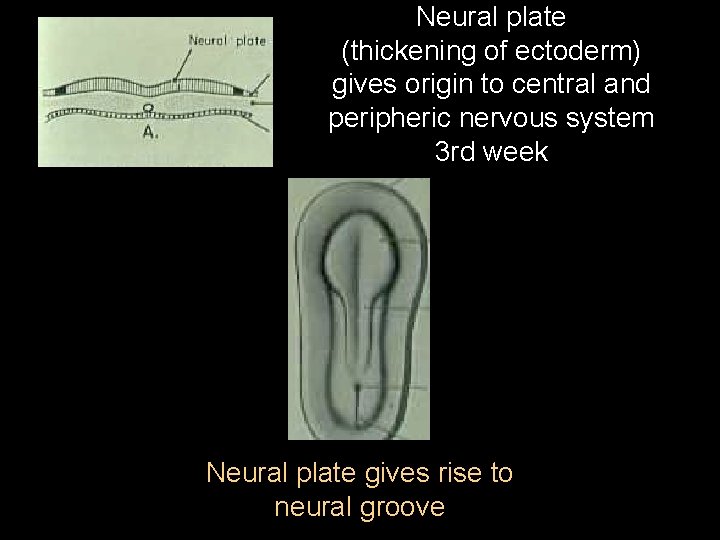
Neural plate (thickening of ectoderm) gives origin to central and peripheric nervous system 3 rd week Neural plate gives rise to neural groove
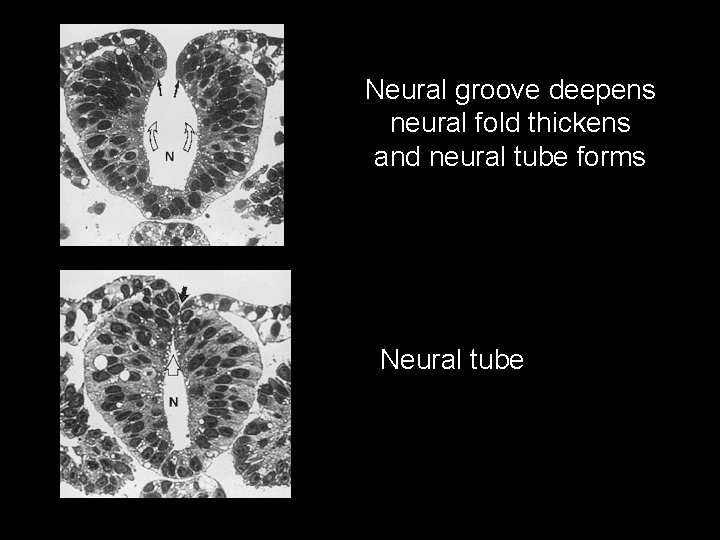
Neural groove deepens neural fold thickens and neural tube forms Neural tube
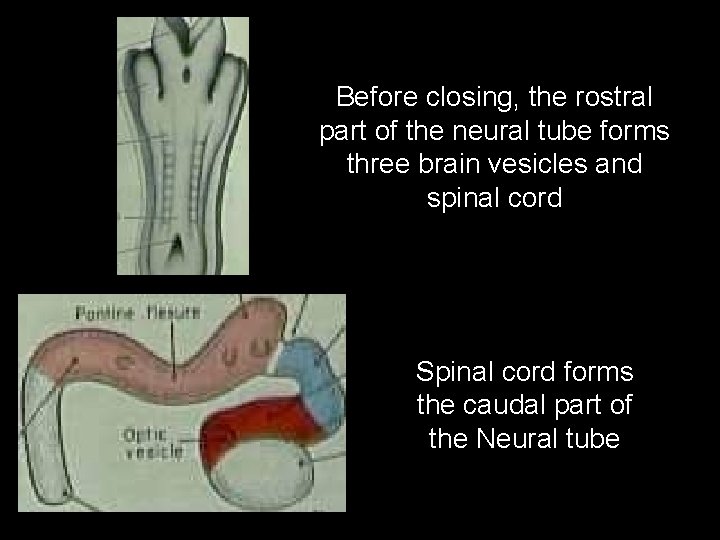
Before closing, the rostral part of the neural tube forms three brain vesicles and spinal cord Spinal cord forms the caudal part of the Neural tube
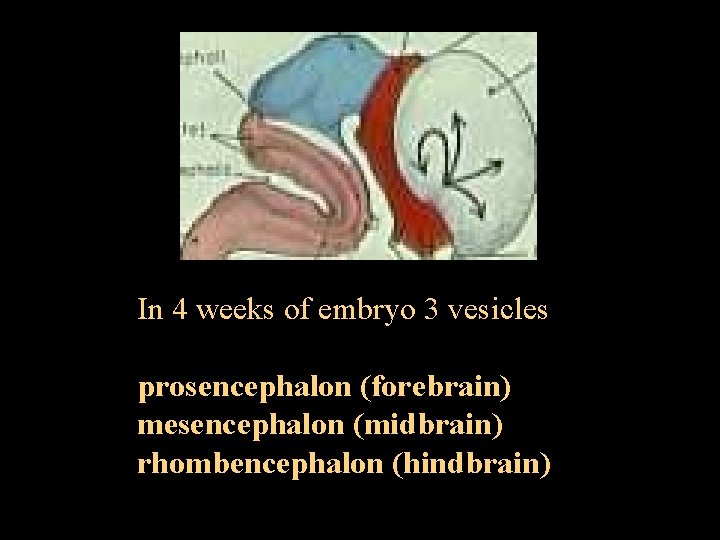
In 4 weeks of embryo 3 vesicles prosencephalon (forebrain) mesencephalon (midbrain) rhombencephalon (hindbrain)
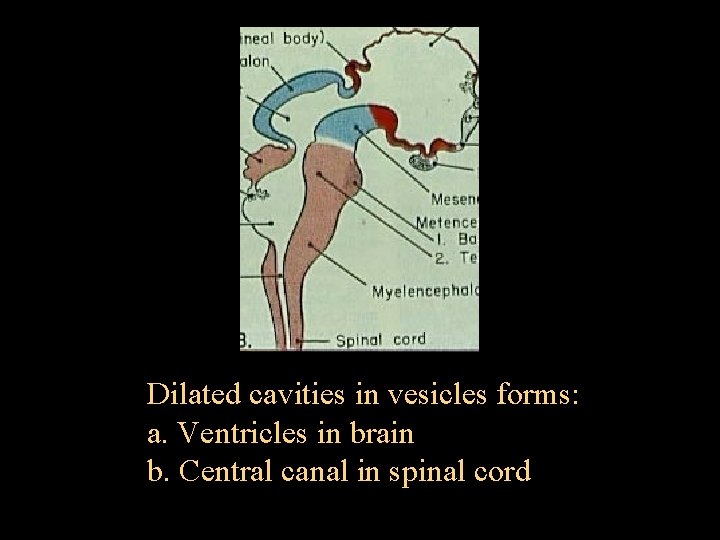
Dilated cavities in vesicles forms: a. Ventricles in brain b. Central canal in spinal cord
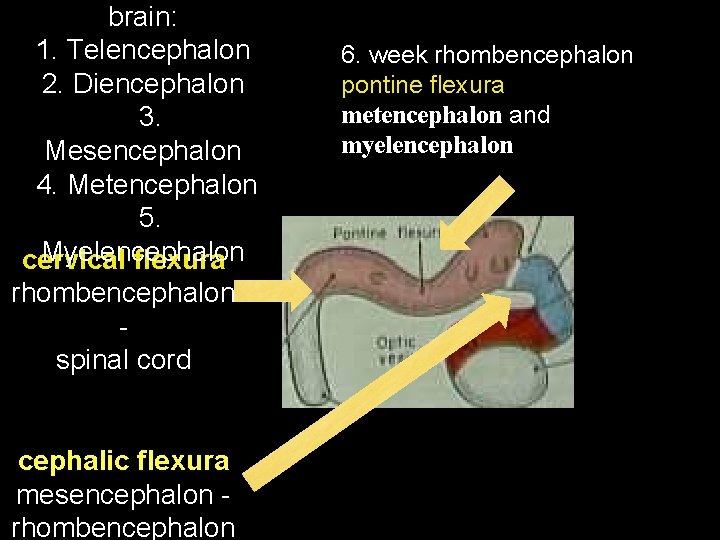
brain: 1. Telencephalon 2. Diencephalon 3. Mesencephalon 4. Metencephalon 5. Myelencephalon cervical flexura rhombencephalon spinal cord cephalic flexura mesencephalon rhombencephalon 6. week rhombencephalon pontine flexura metencephalon and myelencephalon
Neurilation defects Neurilation: completed on the 28. day incomplete neurilation : open lesions Myelomeningocele Anencephaly Total dysraphism

Neural tube defect
Postneurilation Defects (migration abnormality, skin-covered abnormalities) • CRANIAL: – Microcephalus – Hydranencephaly: bilateral ICA infarction – Holoprosencephaly – Lissencephaly: agyria, pachygyria – Porencephaly – Corpus callosum agenesia – Cerebellar hypoplasia/Dandy Walker Malfor. • SPINAL: – Split cord malformation, syringomyelia, tethered cord
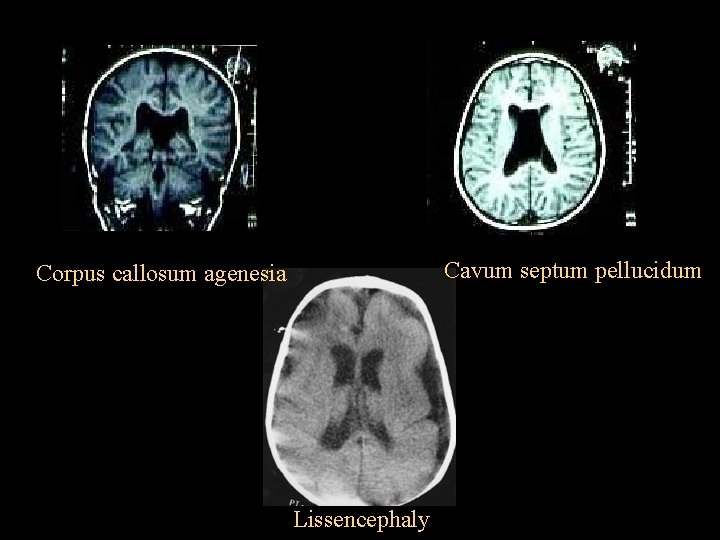
Cavum septum pellucidum Corpus callosum agenesia Lissencephaly
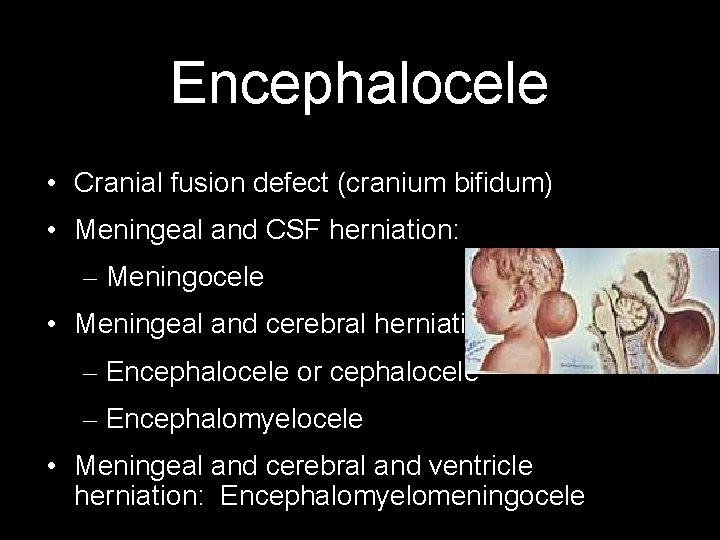
Encephalocele • Cranial fusion defect (cranium bifidum) • Meningeal and CSF herniation: – Meningocele • Meningeal and cerebral herniation: – Encephalocele or cephalocele – Encephalomyelocele • Meningeal and cerebral and ventricle herniation: Encephalomyelomeningocele
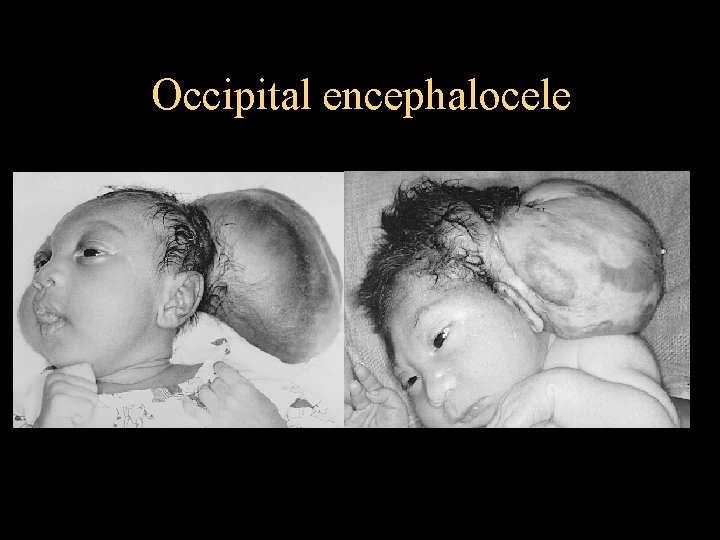
Occipital encephalocele
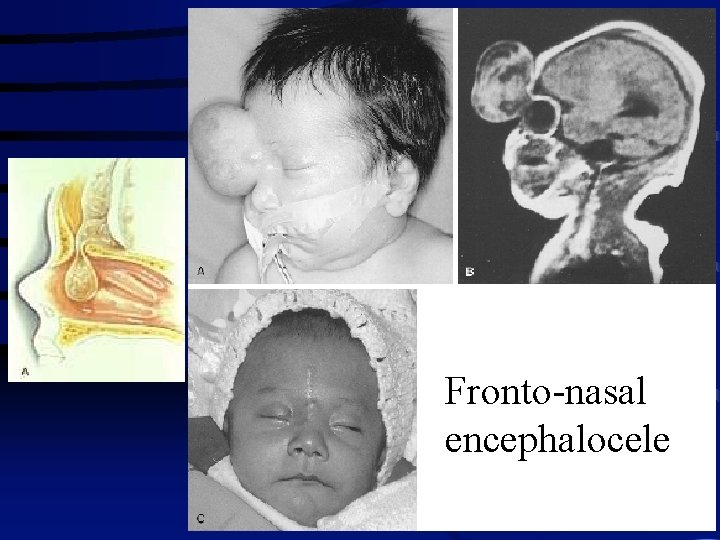
Fronto-nasal encephalocele
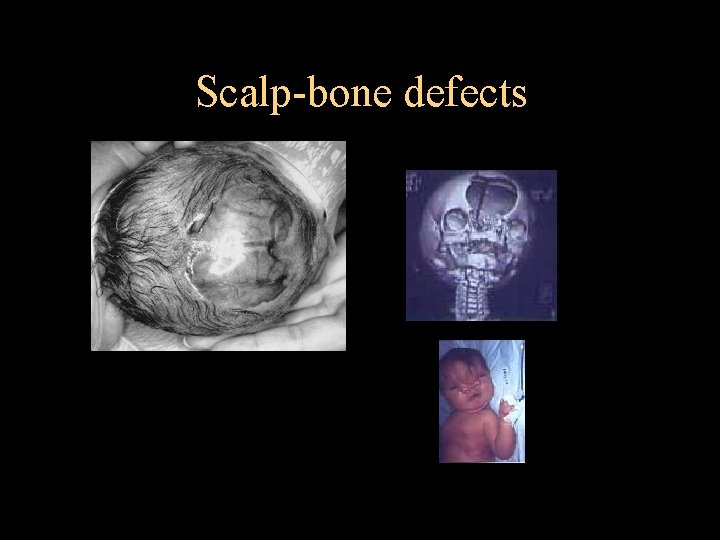
Scalp-bone defects
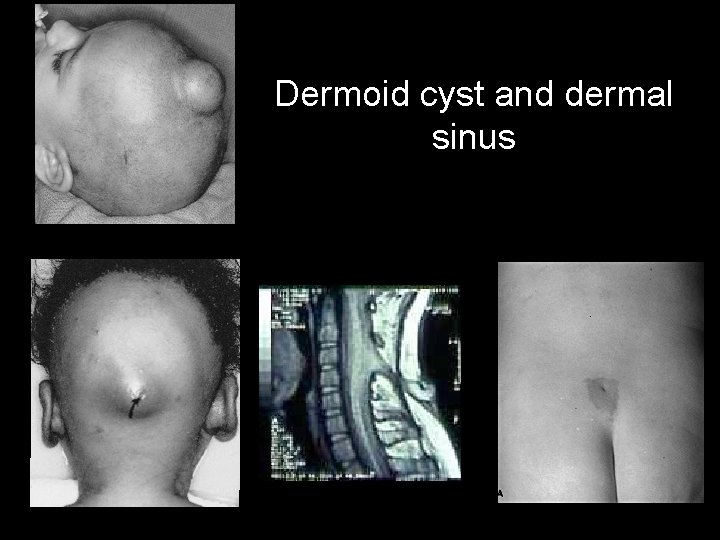
Dermoid cyst and dermal sinus
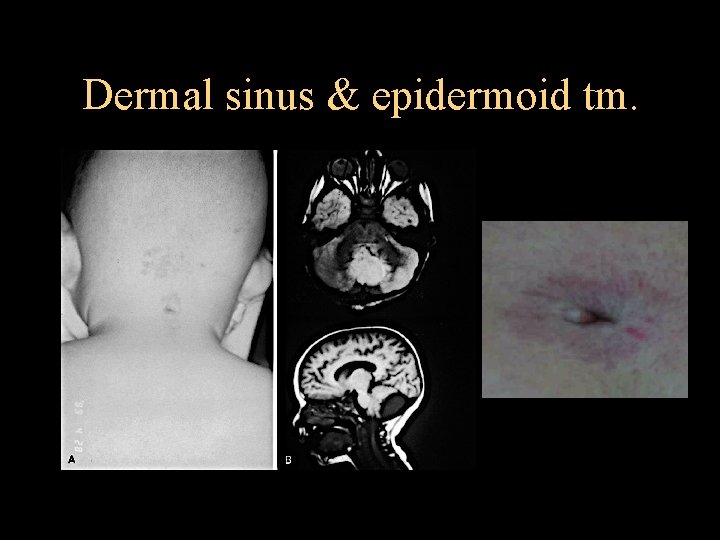
Dermal sinus & epidermoid tm.
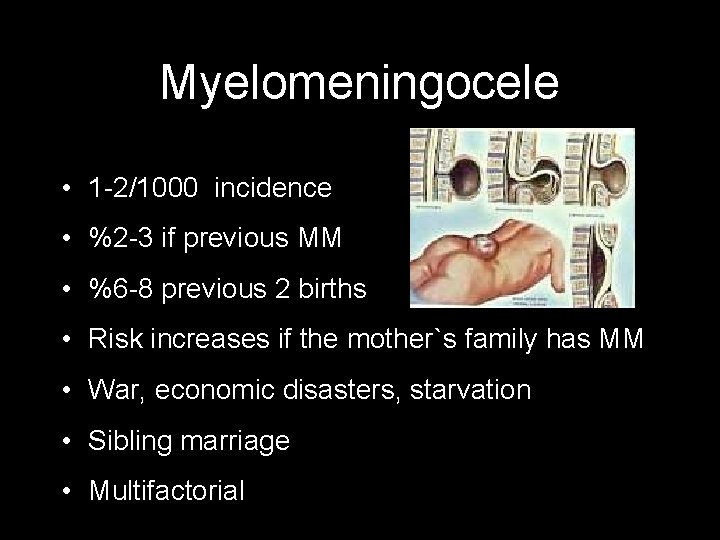
Myelomeningocele • 1 -2/1000 incidence • %2 -3 if previous MM • %6 -8 previous 2 births • Risk increases if the mother`s family has MM • War, economic disasters, starvation • Sibling marriage • Multifactorial

Myelomeningocele Early treatment No treatment 2 y survival: %95 5 y survival: %77 -85 %65 -75 death
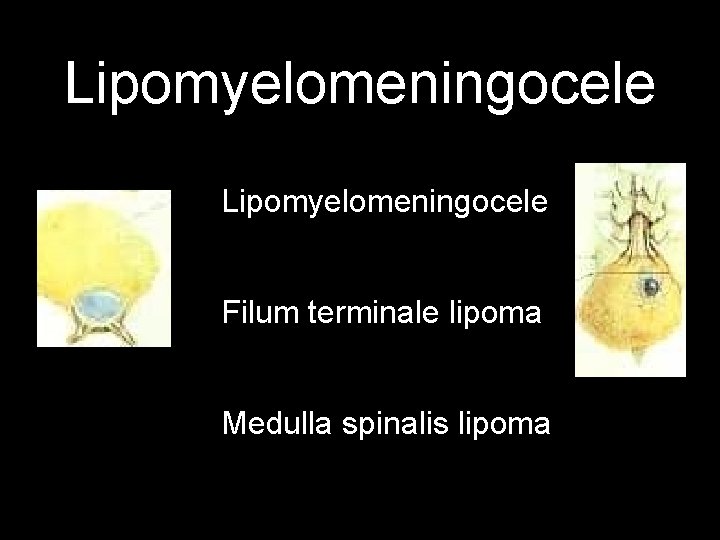
Lipomyelomeningocele Filum terminale lipoma Medulla spinalis lipoma
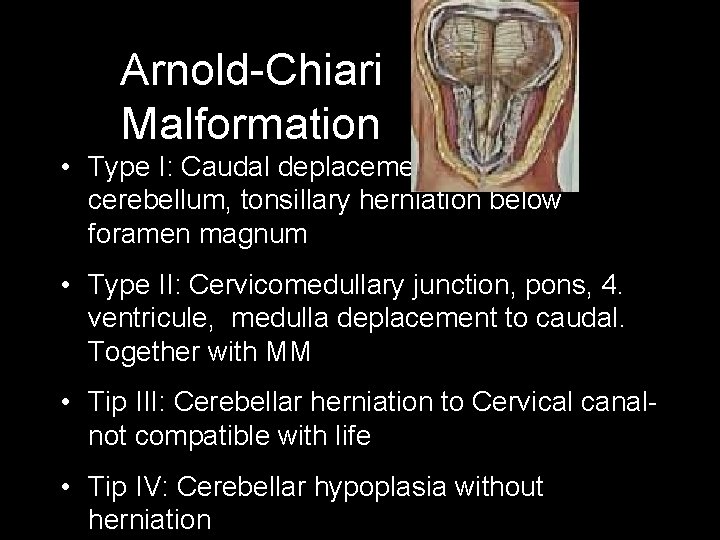
Arnold-Chiari Malformation • Type I: Caudal deplacement of the cerebellum, tonsillary herniation below foramen magnum • Type II: Cervicomedullary junction, pons, 4. ventricule, medulla deplacement to caudal. Together with MM • Tip III: Cerebellar herniation to Cervical canalnot compatible with life • Tip IV: Cerebellar hypoplasia without herniation
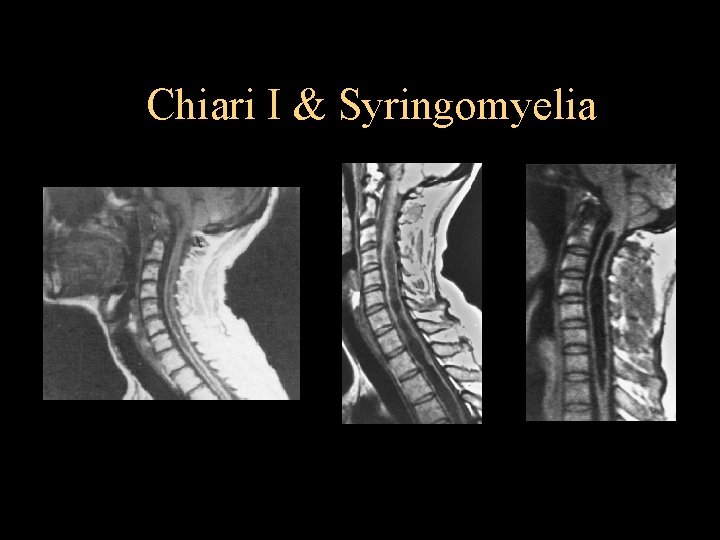
Chiari I & Syringomyelia
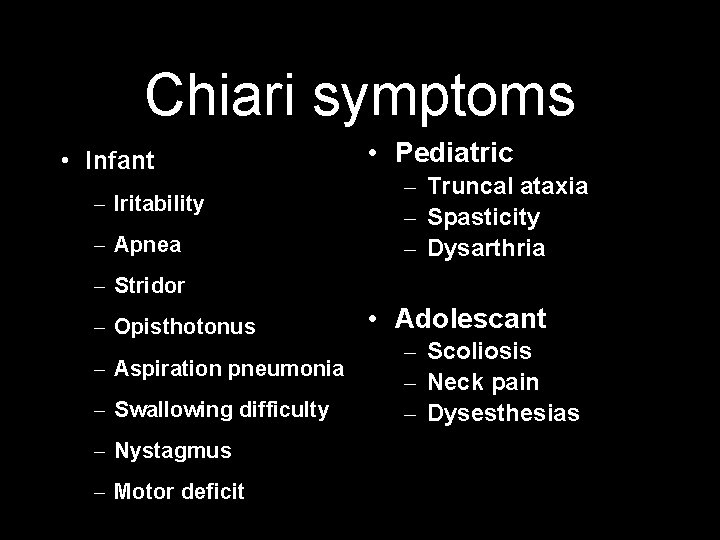
Chiari symptoms • Infant – Iritability – Apnea • Pediatric – Truncal ataxia – Spasticity – Dysarthria – Stridor – Opisthotonus – Aspiration pneumonia – Swallowing difficulty – Nystagmus – Motor deficit • Adolescant – Scoliosis – Neck pain – Dysesthesias
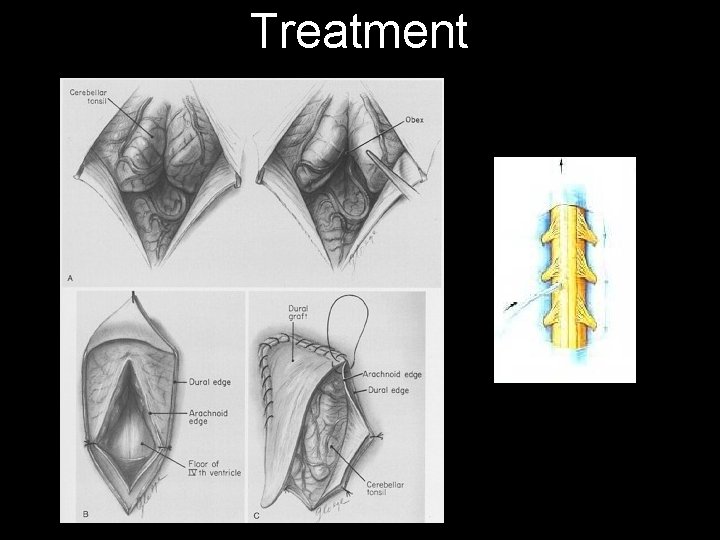
Treatment
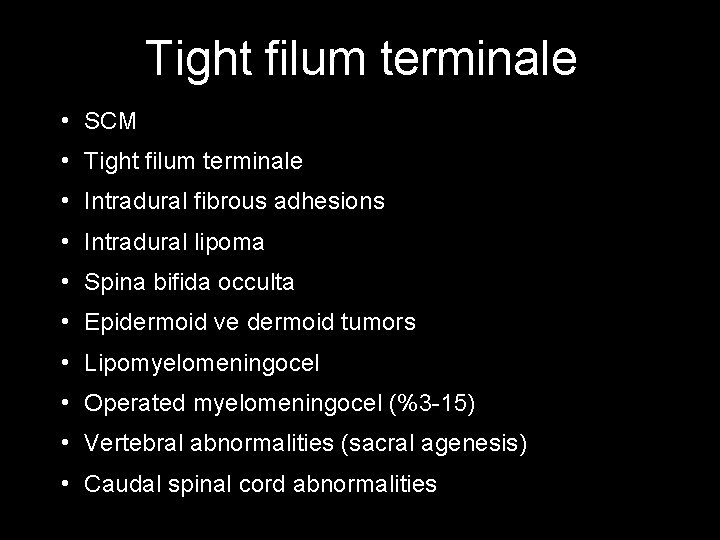
Tight filum terminale • SCM • Tight filum terminale • Intradural fibrous adhesions • Intradural lipoma • Spina bifida occulta • Epidermoid ve dermoid tumors • Lipomyelomeningocel • Operated myelomeningocel (%3 -15) • Vertebral abnormalities (sacral agenesis) • Caudal spinal cord abnormalities
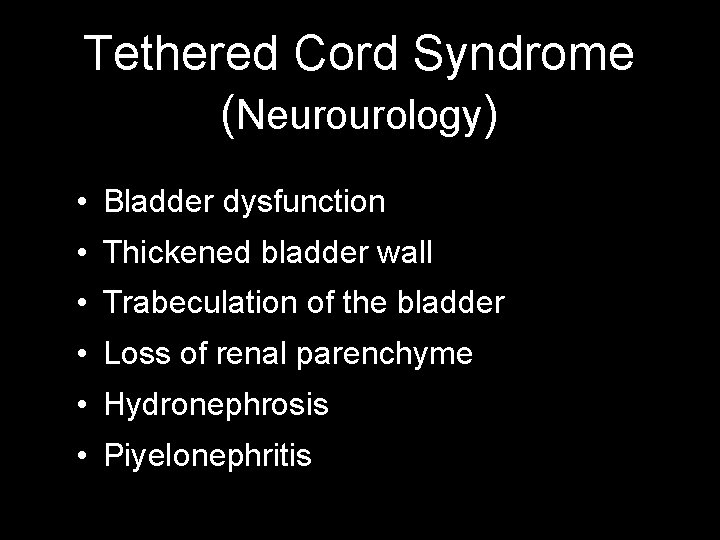
Tethered Cord Syndrome (Neurourology) • Bladder dysfunction • Thickened bladder wall • Trabeculation of the bladder • Loss of renal parenchyme • Hydronephrosis • Piyelonephritis
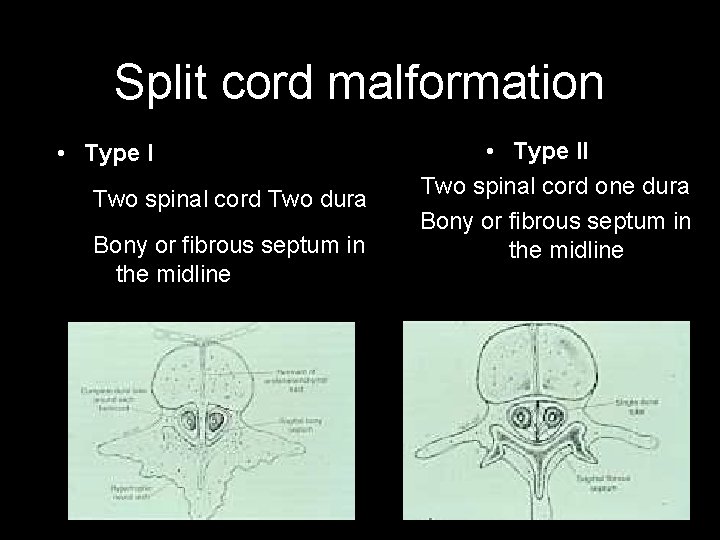
Split cord malformation • Type I Two spinal cord Two dura Bony or fibrous septum in the midline • Type II Two spinal cord one dura Bony or fibrous septum in the midline
SCM Clinic • Skin – Hypertricosis – Capillary hemangiom – dimple – Dermal sinus tract – Lipoma – Hyperpigmentation • Spinal deformity – Scoliosis – Kyphscoliosis – Pes kavus – Pes ekinovarus – Pes planus • Other – Meningocel – Myelomeningocel – Lipomyelomeningocel • Radiology – – – – Bifid lamina wide interpedicular distance Butterfly vertebra Block vertebra Bone spicule Hypertrophic lamina Sacral agenesia
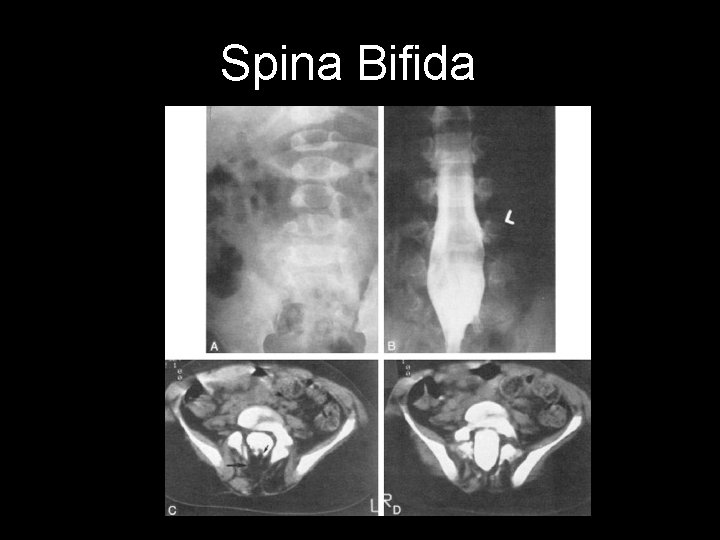
Spina Bifida

Spinal lipoma-Tethered cord
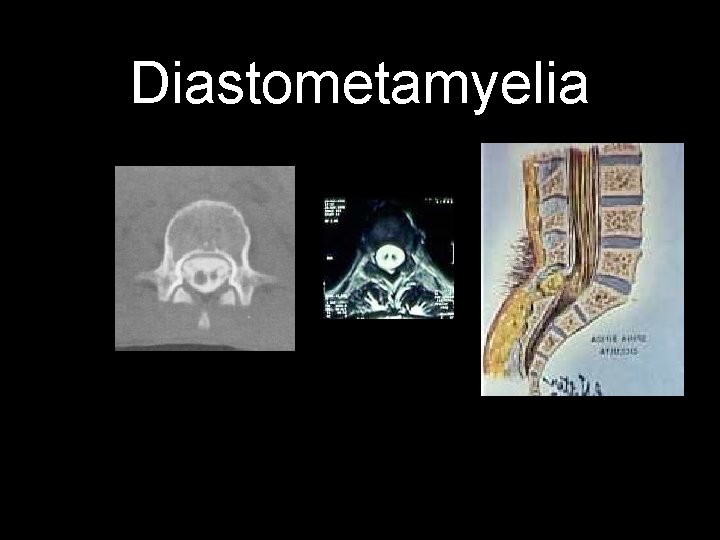
Diastometamyelia
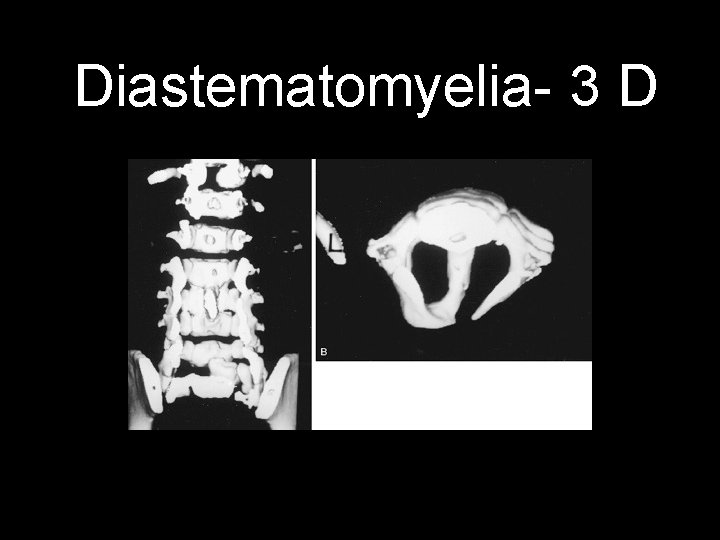
Diastematomyelia- 3 D

Treatment of SCM is surgical excision of the bone spicule
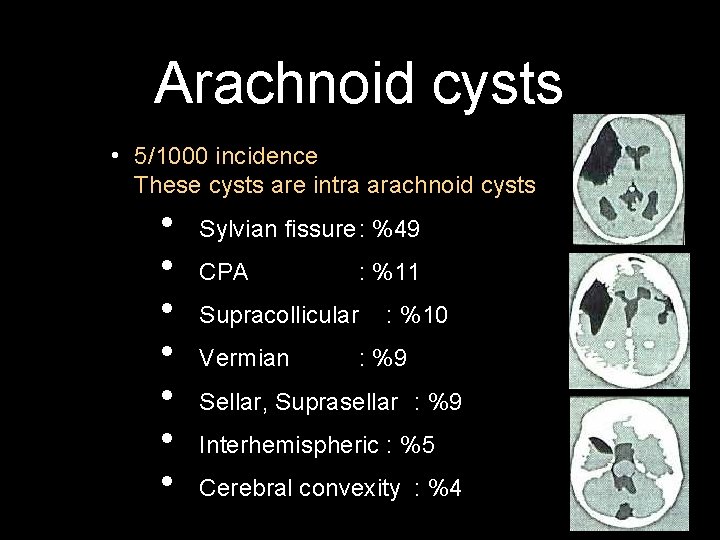
Arachnoid cysts • 5/1000 incidence These cysts are intra arachnoid cysts • • Sylvian fissure: %49 CPA : %11 Supracollicular Vermian : %10 : %9 Sellar, Suprasellar : %9 Interhemispheric : %5 Cerebral convexity : %4
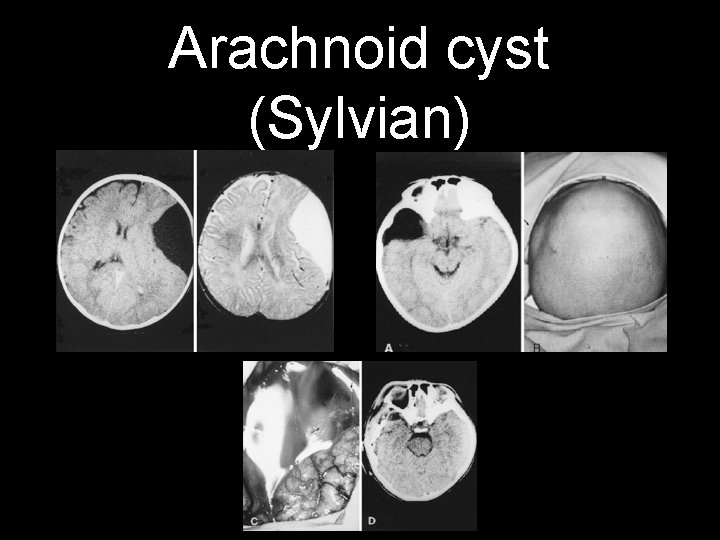
Arachnoid cyst (Sylvian)
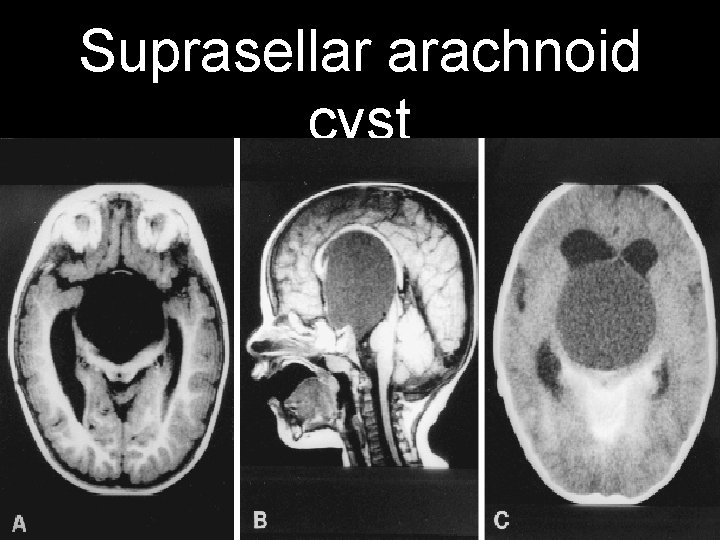
Suprasellar arachnoid cyst
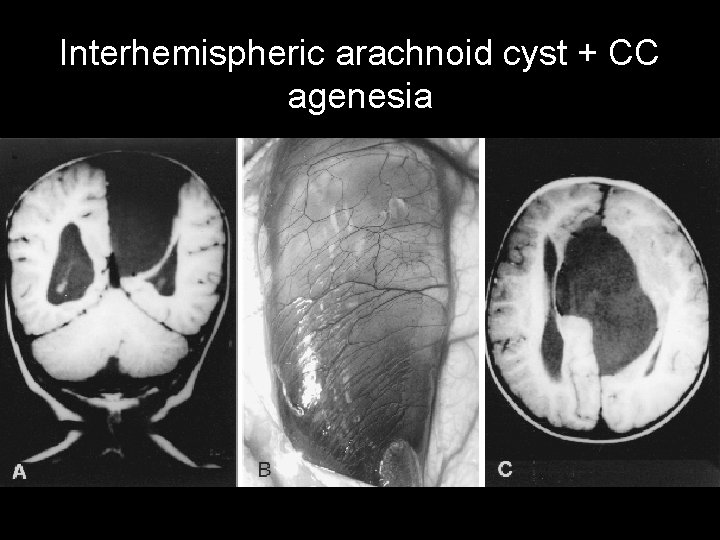
Interhemispheric arachnoid cyst + CC agenesia

Fontanelles • Anterior fontanelle : close 2. 5 years • Posterior fontanelle : 2 -3 months • Sphenoid fontanelle : 2 -3 months • Mastoid fontanelle : 1 year
Cranial Development • 90 % of the adult in one year • 95 % in 6 years
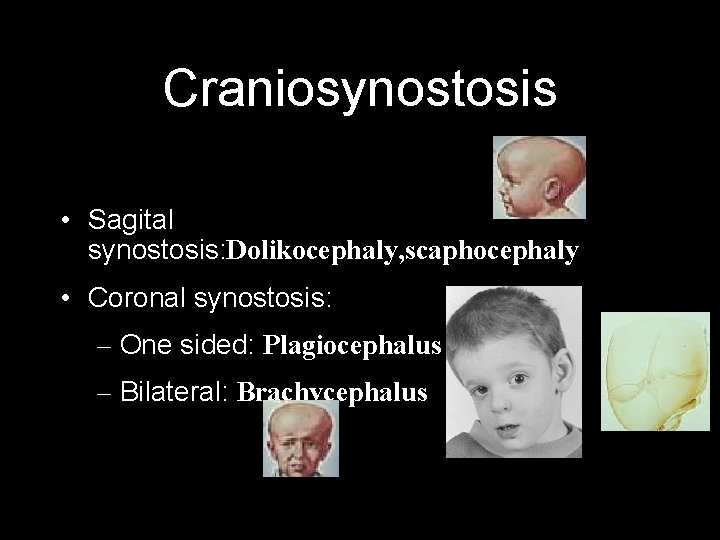
Craniosynostosis • Sagital synostosis: Dolikocephaly, scaphocephaly • Coronal synostosis: – One sided: Plagiocephalus – Bilateral: Brachycephalus
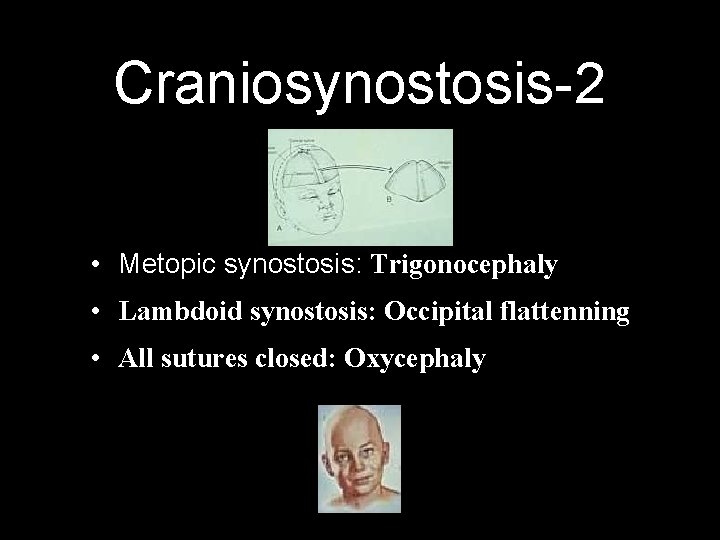
Craniosynostosis-2 • Metopic synostosis: Trigonocephaly • Lambdoid synostosis: Occipital flattenning • All sutures closed: Oxycephaly
Dandy Walker • Atresia of Foramen Magendi ve Lushka • Agenesis of Cerebellar vermis • IV. ventricule connected cyst in posterior fossa • Hydrocephalus (%90) • Corpus callosum agenesia (%17) • Occipital encephalocell (%7) • Spina bifida, syringomyelia, microcephalus, dermoid cyst, porencephalus, Klippel-Feil, etc.
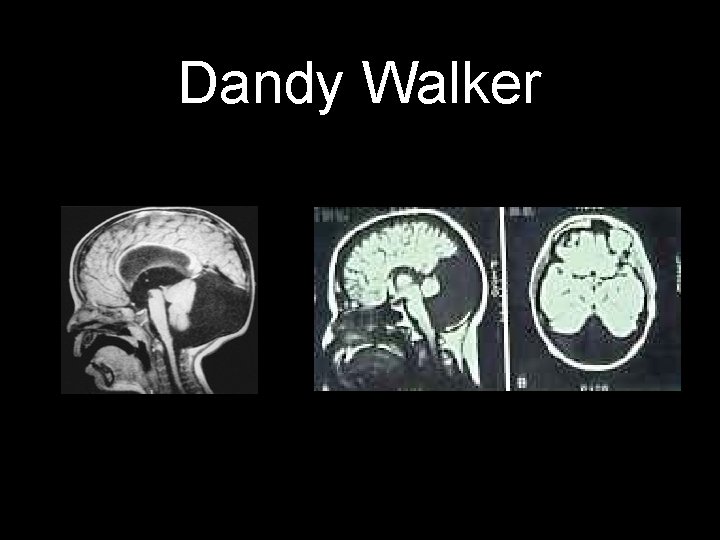
Dandy Walker
- Slides: 43