Pediatric Inguinal and scrotal conditions Dr KHALED MADBOULY
Pediatric Inguinal and scrotal conditions Dr. KHALED MADBOULY, MD. Consultant Urologist. Urology Department, PMA HOSPITAL.
Pediatric Inguinal and scrotal conditions • Cryptorchidism (Undescended testis) • Varicocele • Hernias and Hydroceles • Acute scrotum • Epididymal, vasal and scrotal anomalies Dr. Khaled Madbouly, MD.
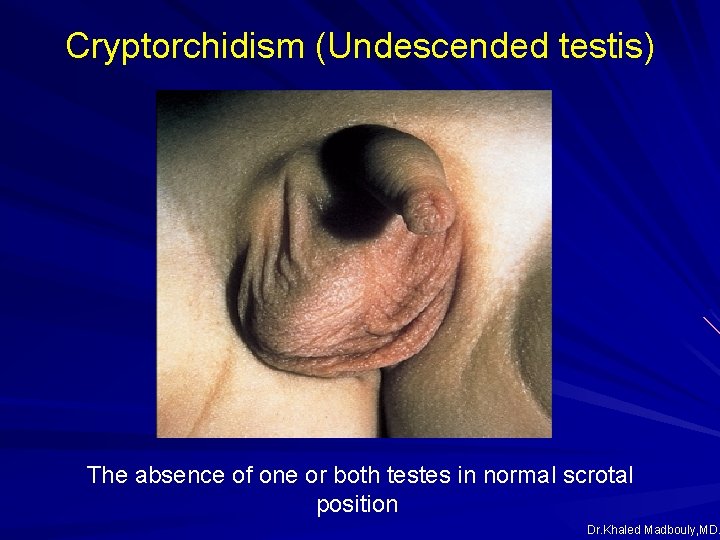
Cryptorchidism (Undescended testis) The absence of one or both testes in normal scrotal position Dr. Khaled Madbouly, MD.
Cryptorchidism (Undescended testis) Ø Incidence: One of the most common male developmental abnormalities The most common cong anomaly of male genitalia 3. 4% of full term infants Up to 45% of preterm male neonates 14% familial After birth: Testicular descend is possible due to the infantile LHRH surge that peaks at 3 months 0. 8 -1% of male children at 1 year of age 0. 8% of adult males 1/3 rd bilateral 2/3 rd unilateral : 70% : right testis 30% : left testis Dr. Khaled Madbouly, MD.
Classification Ø Undescended Ø Ectopic Ø Retractile Ø Gliding Ø Ascended Dr. Khaled Madbouly, MD.
Classification Ø Undescended : arrest of the testis in the normal pathway of its descent Abdominal 8% Canalicular 22% Prescrotal 70% Ø Ectopic : away from the normal pathway of its descent Ø Retractile : freely mobile testis can be manipulated into scrotum where it remains without tension Dr. Khaled Madbouly, MD.
Classification Ø Gliding: can be manipulated into upper scrotum but retracts when released Ø Ascended: previously descended, then “ascends” spontaneously Dr. Khaled Madbouly, MD.
Associated pathology Ø Testicular maldevelopment § Impaired transformation of gonocytes to spermatogonia § fewer spermatogonia § small semineferous tubules § increased peritubular tissue § collagen fibers deposition in spermatogonia& sertoli cells Ø Anomalies of epididymis § § § 35 - 75% caput and/or cauda epididymis fusion anomalies elongation and/or looping atresia Dr. Khaled Madbouly, MD.
Associated pathology Ø Anomalies of proc. vaginalis & gubernaculum § failure of closure of the processus vaginalis § failure of attachment of the gubernacular remnant Ø Other testicular anomalies § § § polyorchidism splenogonadal fusion transverse testicular ectopia Dr. Khaled Madbouly, MD.
Presentation Empty, undeveloped one or both scrotal compartments Ø Palpable testis 80% 2/3 rd unilateral (RT. > Lt. ) prescrotal canalicular ectopic retractile Ø Non palpable testis 20% abdominal or transinguinal (peeping) 25 – 50% complete atrophy (vanishing) 15 – 40% extra-abdominal, non palpable 10 – 30% Ø Inguinal hernia 70% Dr. Khaled Madbouly, MD.
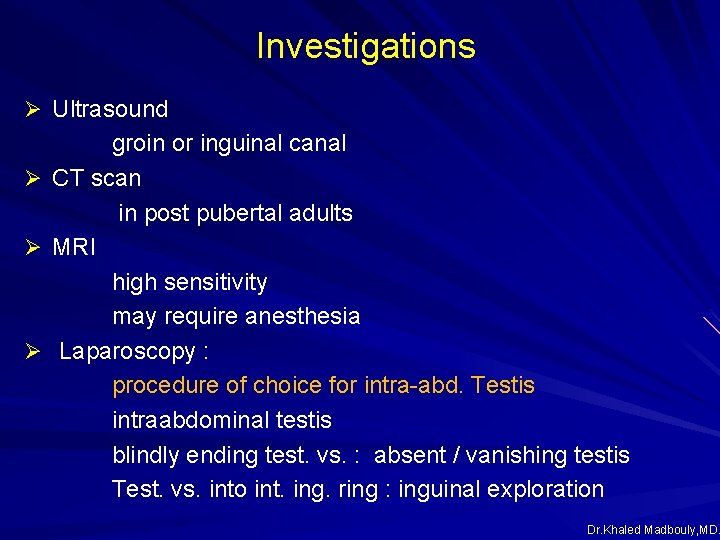
Investigations Ø Ultrasound groin or inguinal canal Ø CT scan in post pubertal adults Ø MRI high sensitivity may require anesthesia Ø Laparoscopy : procedure of choice for intra-abd. Testis intraabdominal testis blindly ending test. vs. : absent / vanishing testis Test. vs. into int. ing. ring : inguinal exploration Dr. Khaled Madbouly, MD.
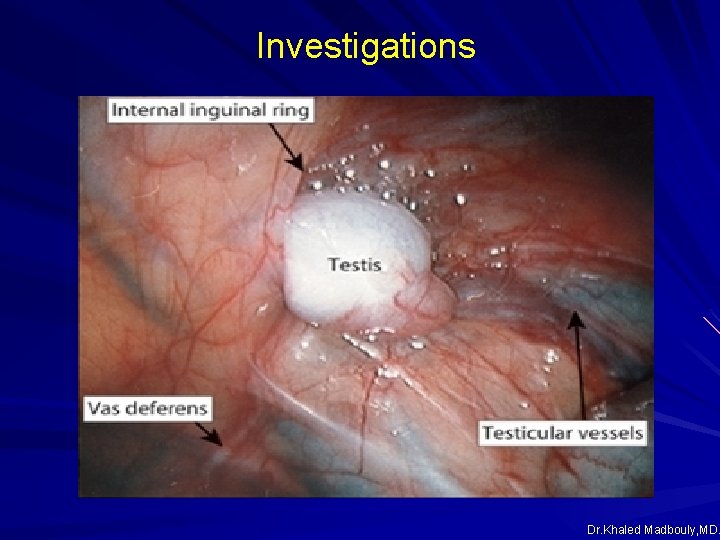
Investigations Dr. Khaled Madbouly, MD.
Differential diagnosis D. D. of empty scrotum Ø Cryptorchidism Ø Orchidectomy Ø Anorchia Dr. Khaled Madbouly, MD.

Complications Ø Neoplasia Ø Infertility Ø Torsion Ø Hernia Dr. Khaled Madbouly, MD.
Complications Ø Neoplasia • 10% of testicular tumors arise in undescended testis • The relative risk of malignant transformation is 2. 5 to 8 • 2– 3 folds in boys undergoing prepubertal orchidopexy • Prepubertal orchiopexy (<13 ys) may decrease the risk of testicular cancer • abdominal testis > inguinal testis (4 folds) • rare before the age of 10 Dr. Khaled Madbouly, MD.
Complications Ø Infertility 25% of unilateral cases : reduced sperm counts Majority of bilateral cases : reduced sperm count Unilateral UDT : 90% paternity rate Bilateral UDT : 50% paternity rate Testis arrest at higher position poorer fertility early orchidopexy (6 month-2 yrs): better fertility recovery Ø Torsion Ø Hernia 70% of cases 90% at surgery Dr. Khaled Madbouly, MD.
Treatment Ø Orchidopexy is recommended for testes that remain undescended after 6 months of age Rationale: to limit atrophic changes in the semineferous tubules to enhance future fertility to place the testis in an accessible site to avoid psychological trauma spontaneous descent is rare after 1 year of age ( 95% premature & 75% full term cryptorchid testis spontaneously descend by 1 yr) Ø hormone therapy is not recommended. Dr. Khaled Madbouly, MD
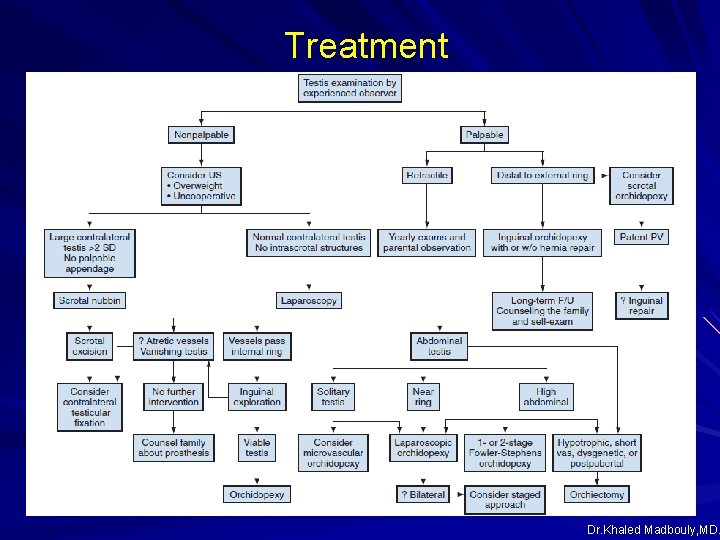
Treatment Dr. Khaled Madbouly, MD.
Pediatric Inguinal and scrotal conditions • Cryptorchidism (Undescended testis) • Varicocele • Hernias and Hydroceles • Acute scrotum • Epididymal, vasal and scrotal anomalies Dr. Khaled Madbouly, MD.
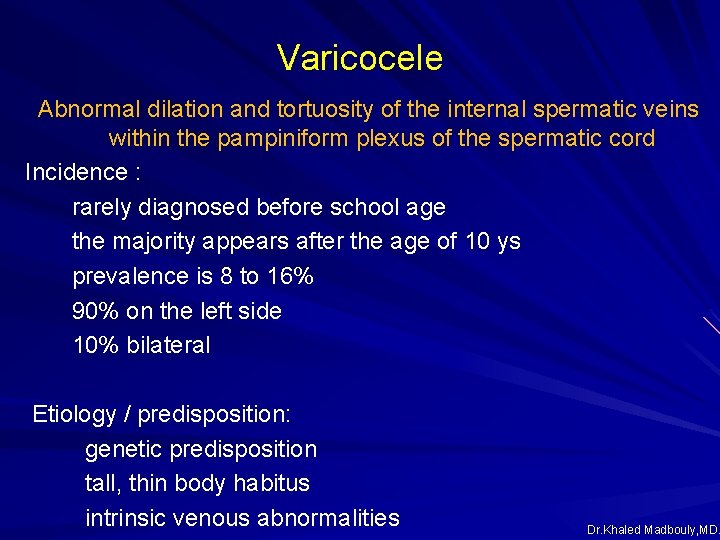
Varicocele Abnormal dilation and tortuosity of the internal spermatic veins within the pampiniform plexus of the spermatic cord Incidence : rarely diagnosed before school age the majority appears after the age of 10 ys prevalence is 8 to 16% 90% on the left side 10% bilateral Etiology / predisposition: genetic predisposition tall, thin body habitus intrinsic venous abnormalities Dr. Khaled Madbouly, MD.
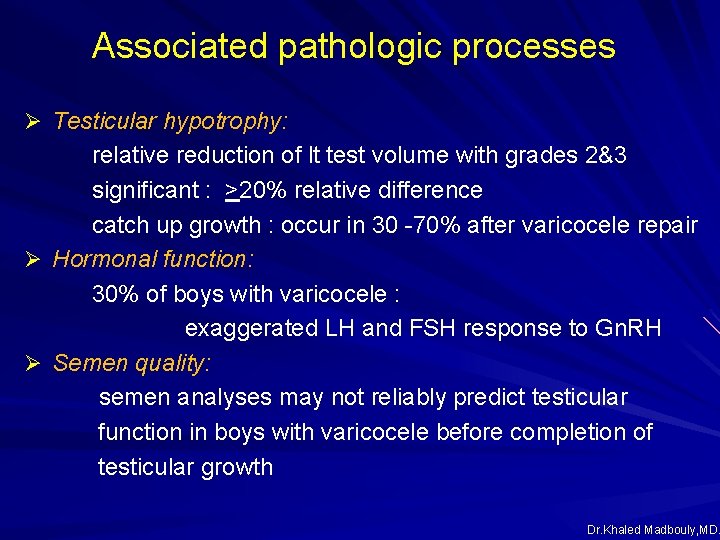
Associated pathologic processes Ø Testicular hypotrophy: relative reduction of lt test volume with grades 2&3 significant : >20% relative difference catch up growth : occur in 30 -70% after varicocele repair Ø Hormonal function: 30% of boys with varicocele : exaggerated LH and FSH response to Gn. RH Ø Semen quality: semen analyses may not reliably predict testicular function in boys with varicocele before completion of testicular growth Dr. Khaled Madbouly, MD.
Presentation Ø Asymptomatic Ø Pain : < 10% of cases Ø Infertility: later in life Ø Grading : 0 subclinical, not papable, detected by CDUS, 1 palpable only with valsalva 2 easily palpable, not visible 3 easily visible Ø Color Doppler ultrasound (CDUS) : vein diameter > 2 mm retrograde blood flow Dr. Khaled Madbouly, MD.
Treatment Ø Observation Ø Surgical repair Indications Pain significant left (≥ 20%) or bilateral testicular hypotroph y abnormal semen analysis (age> 18) Approaches: inguinal/subinguinal retroperitoneal laparoscopic venographic sclerotherapy / embolotherapy Dr. Khaled Madbouly, MD.
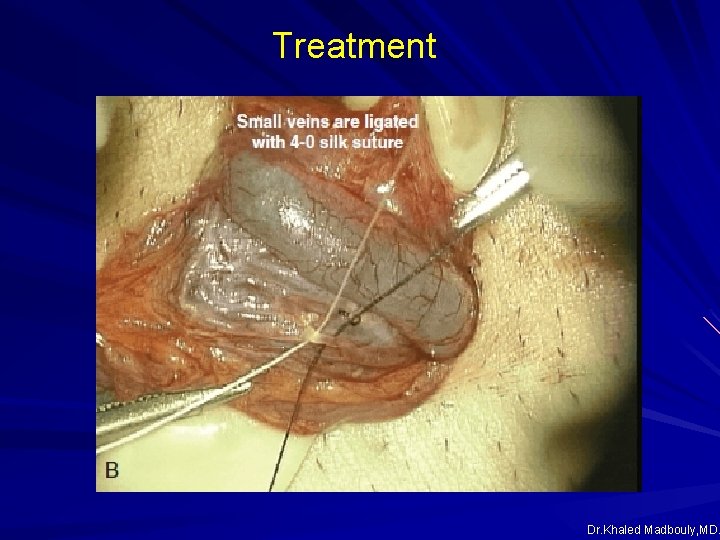
Treatment Dr. Khaled Madbouly, MD.
Pediatric Inguinal and scrotal conditions • Cryptorchidism (Undescended testis) • Varicocele • Hernias and Hydroceles • Acute scrotum • Epididymal, vasal and scrotal anomalies Dr. Khaled Madbouly, MD.
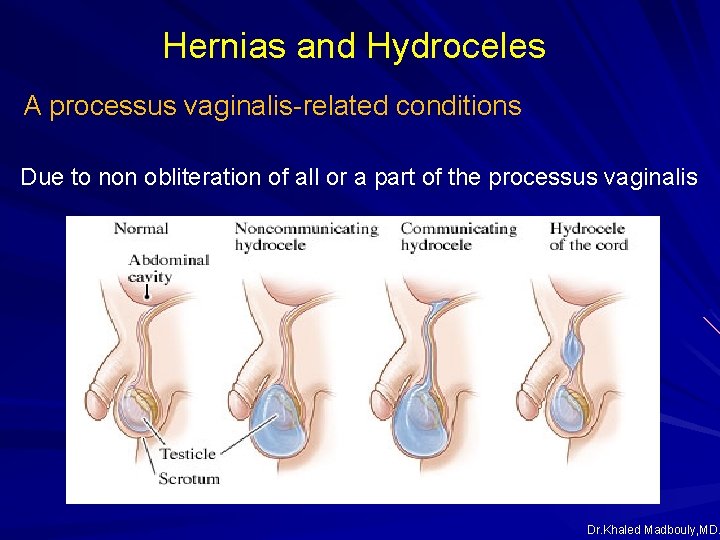
Hernias and Hydroceles A processus vaginalis-related conditions Due to non obliteration of all or a part of the processus vaginalis Dr. Khaled Madbouly, MD.
Inguinal Hernia Ø Incidence : 1 – 5% in full term infants up to 30% in premature infants male to female : 5 -10 to 1 75 -90% unilateral, more on the right side 28% familial Dr. Khaled Madbouly, MD.
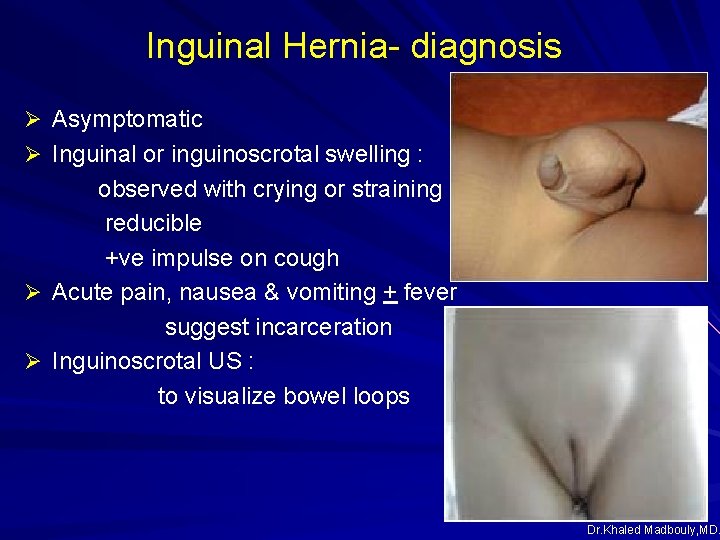
Inguinal Hernia- diagnosis Ø Asymptomatic Ø Inguinal or inguinoscrotal swelling : observed with crying or straining reducible +ve impulse on cough Ø Acute pain, nausea & vomiting + fever suggest incarceration Ø Inguinoscrotal US : to visualize bowel loops Dr. Khaled Madbouly, MD.
Inguinal Hernia Repair Ø Standard inguinal repair Ø Laparoscopic repair Ø Scrotal repair Dr. Khaled Madbouly, MD.
Hydrocele Ø Etiology Primary : communicating inguinoscrotal hydrocele: after birth non communicating scrotal hydrocele: after puberty Secondary Tumor Inflammation Dr. Khaled Madbouly, MD.
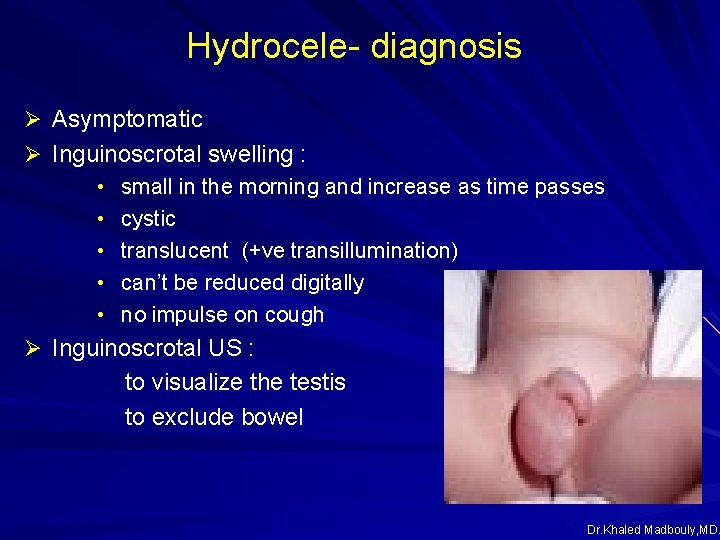
Hydrocele- diagnosis Ø Asymptomatic Ø Inguinoscrotal swelling : • small in the morning and increase as time passes • cystic • translucent (+ve transillumination) • can’t be reduced digitally • no impulse on cough Ø Inguinoscrotal US : to visualize the testis to exclude bowel Dr. Khaled Madbouly, MD.
Hydrocele- treatment Inguinal exploration in communicating hydrocele Excision of the upper part Eversion of the lower part after 12 -24 months due to tendency for spontaneous resolution Scrotal exploration in non communicating hydrocele Dr. Khaled Madbouly, MD.
Pediatric Inguinal and scrotal conditions • Cryptorchidism (Undescended testis) • Varicocele • Hernias and Hydroceles • Acute scrotum • Epididymal, vasal and scrotal anomalies Dr. Khaled Madbouly, MD.
Acute scrotum § Spermatic cord torsion § § Intravaginal Extravaginal Appendage torsion Appendix testis Epididymitis Infectious : UTI, STD Traumatic Orchitis Trauma hematocele scrotal contusion testicular rupture Dr. Khaled Madbouly, MD.
Spermatic cord torsion Surgical emergency which if not managed rapidly : testicular atrophy Incidence : prevalence : 8. 6 / 100000 males aged 10 -19 years possible at any age peak age : 12 – 16 ys may occur at the neonatal period 90% after age 10 26% > 21 ys age undescended testis : higher risk Dr. Khaled Madbouly, MD.
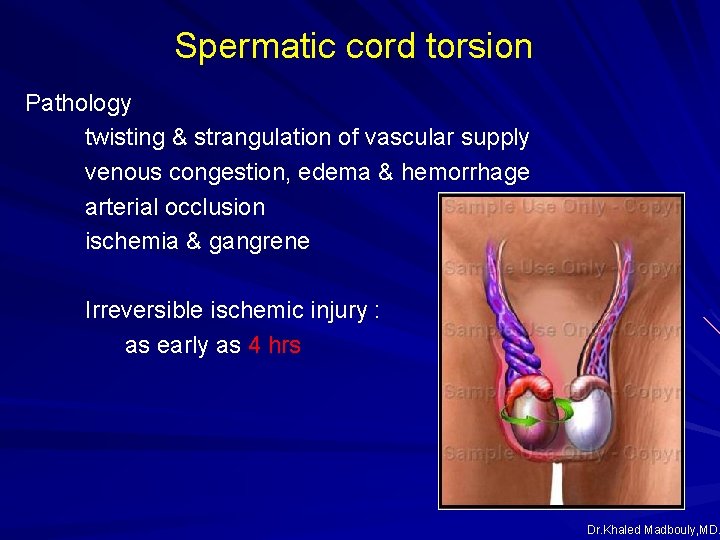
Spermatic cord torsion Pathology twisting & strangulation of vascular supply venous congestion, edema & hemorrhage arterial occlusion ischemia & gangrene Irreversible ischemic injury : as early as 4 hrs Dr. Khaled Madbouly, MD.
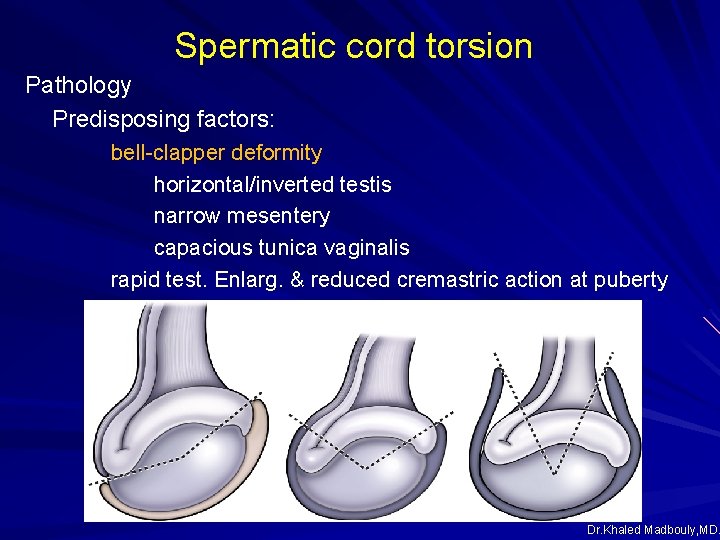
Spermatic cord torsion Pathology Predisposing factors: bell-clapper deformity horizontal/inverted testis narrow mesentery capacious tunica vaginalis rapid test. Enlarg. & reduced cremastric action at puberty Dr. Khaled Madbouly, MD.
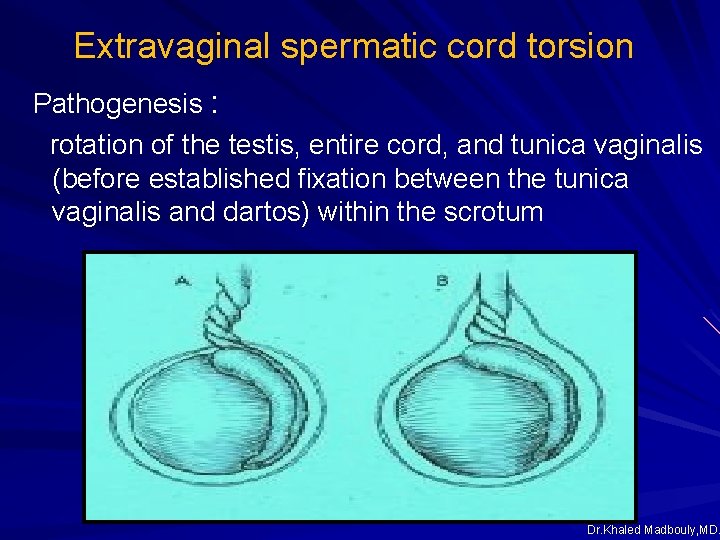
Extravaginal spermatic cord torsion Pathogenesis : rotation of the testis, entire cord, and tunica vaginalis (before established fixation between the tunica vaginalis and dartos) within the scrotum Dr. Khaled Madbouly, MD.
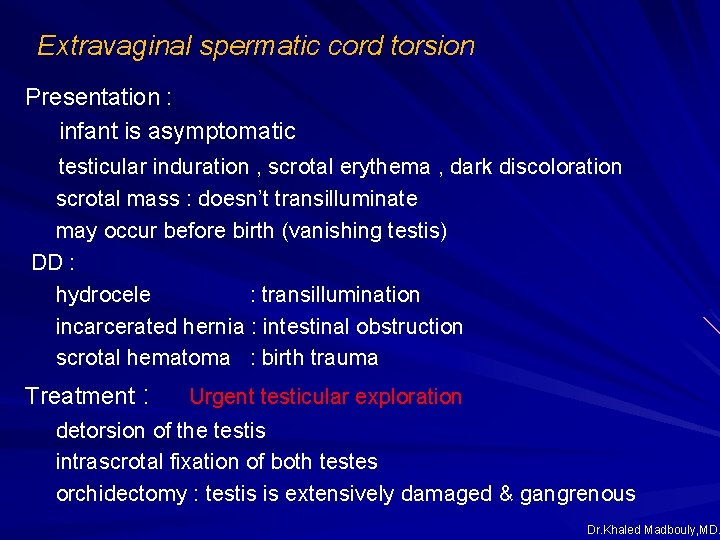
Extravaginal spermatic cord torsion Presentation : infant is asymptomatic testicular induration , scrotal erythema , dark discoloration scrotal mass : doesn’t transilluminate may occur before birth (vanishing testis) DD : hydrocele : transillumination incarcerated hernia : intestinal obstruction scrotal hematoma : birth trauma Treatment : Urgent testicular exploration detorsion of the testis intrascrotal fixation of both testes orchidectomy : testis is extensively damaged & gangrenous Dr. Khaled Madbouly, MD.
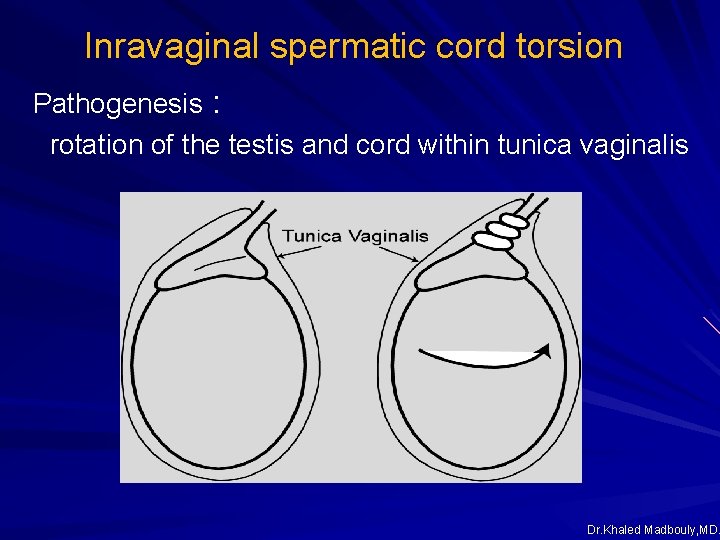
Inravaginal spermatic cord torsion Pathogenesis : rotation of the testis and cord within tunica vaginalis Dr. Khaled Madbouly, MD.
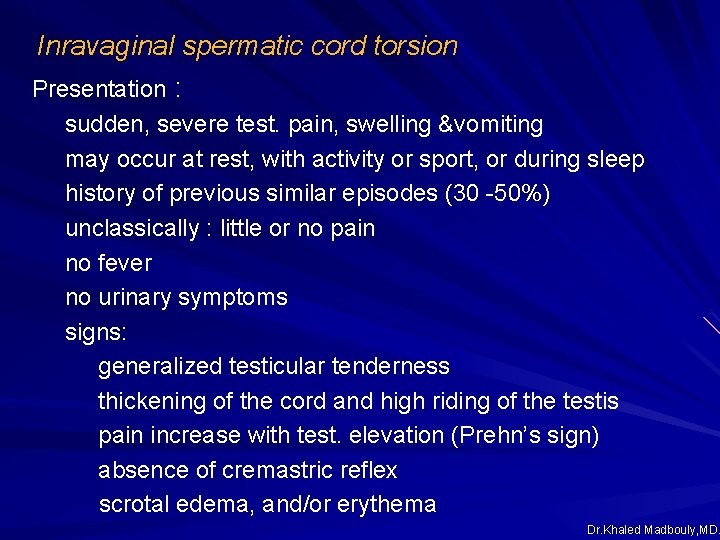
Inravaginal spermatic cord torsion Presentation : sudden, severe test. pain, swelling &vomiting may occur at rest, with activity or sport, or during sleep history of previous similar episodes (30 -50%) unclassically : little or no pain no fever no urinary symptoms signs: generalized testicular tenderness thickening of the cord and high riding of the testis pain increase with test. elevation (Prehn’s sign) absence of cremastric reflex scrotal edema, and/or erythema Dr. Khaled Madbouly, MD.
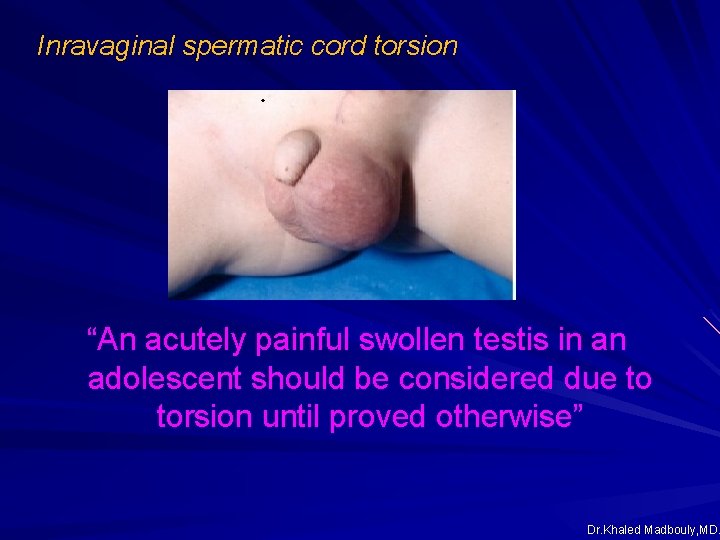
Inravaginal spermatic cord torsion “An acutely painful swollen testis in an adolescent should be considered due to torsion until proved otherwise” Dr. Khaled Madbouly, MD.
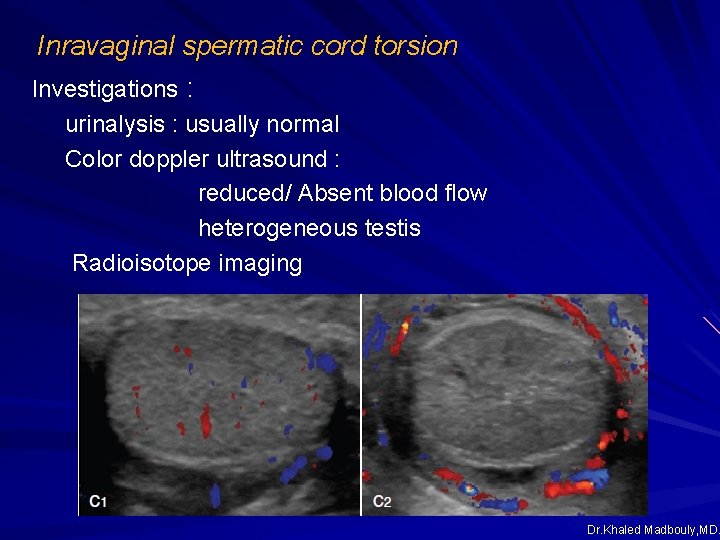
Inravaginal spermatic cord torsion Investigations : urinalysis : usually normal Color doppler ultrasound : reduced/ Absent blood flow heterogeneous testis Radioisotope imaging Dr. Khaled Madbouly, MD.
Inravaginal spermatic cord torsion “When findings support or are suspicious for spermatic cord torsion, emergent scrotal exploration is indicated and should not be delayed to obtain scrotal ultrasonography or any other diagnostic test” Dr. Khaled Madbouly, MD.
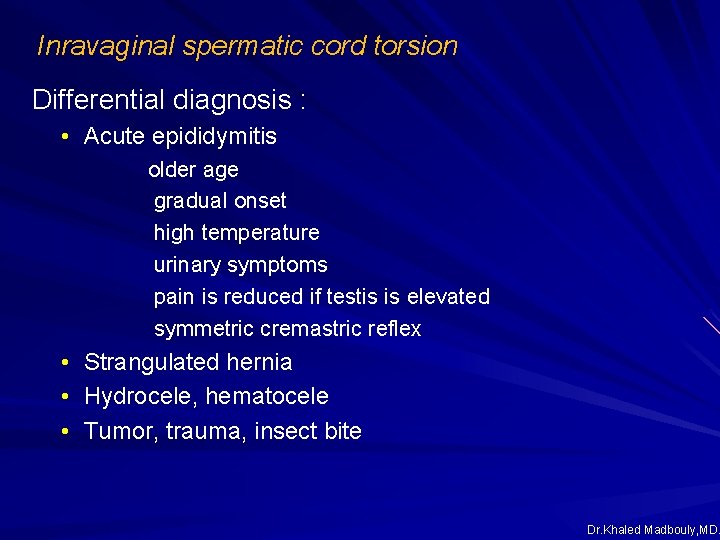
Inravaginal spermatic cord torsion Differential diagnosis : • Acute epididymitis older age gradual onset high temperature urinary symptoms pain is reduced if testis is elevated symmetric cremastric reflex • Strangulated hernia • Hydrocele, hematocele • Tumor, trauma, insect bite Dr. Khaled Madbouly, MD.
Inravaginal spermatic cord torsion Treatment : Early (1 hr. ) manual detorsion testis rotates medially : twist it laterally 1% lidocain inflitration of the cord if successful : intrascrotal fixation of both testes later ( 40% chance of torsion in contra lateral testis) Dr. Khaled Madbouly, MD.
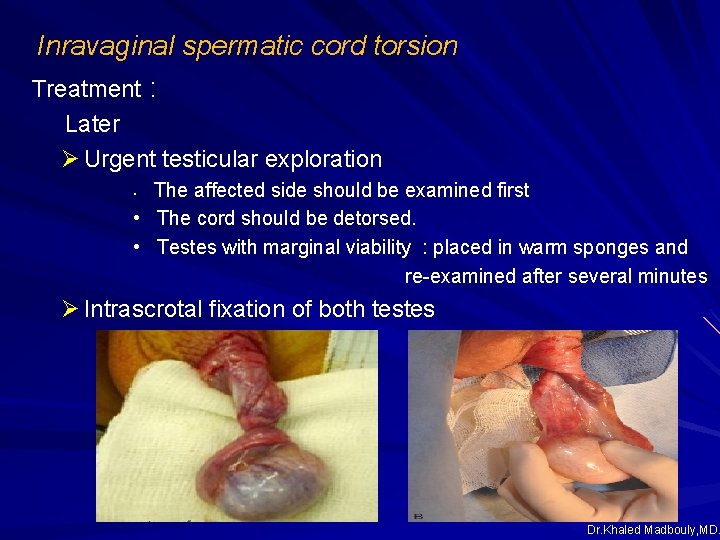
Inravaginal spermatic cord torsion Treatment : Later Ø Urgent testicular exploration The affected side should be examined first • The cord should be detorsed. • Testes with marginal viability : placed in warm sponges and re-examined after several minutes • Ø Intrascrotal fixation of both testes Dr. Khaled Madbouly, MD.

Inravaginal spermatic cord torsion Treatment : Orchidectomy : testis is extensively damaged & gangrenous Dr. Khaled Madbouly, MD.
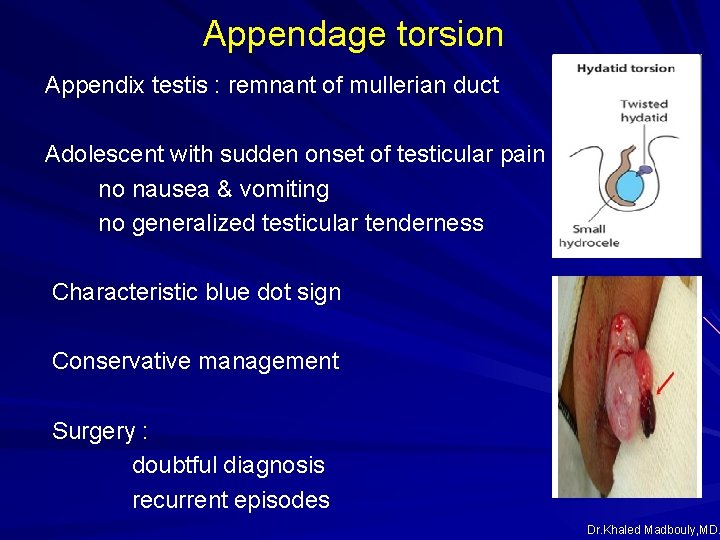
Appendage torsion Appendix testis : remnant of mullerian duct Adolescent with sudden onset of testicular pain no nausea & vomiting no generalized testicular tenderness Characteristic blue dot sign Conservative management Surgery : doubtful diagnosis recurrent episodes Dr. Khaled Madbouly, MD.
Epididymitis Incidence : poorly defined in children Risk factors : neurogenic and non-neurogenic voiding dysfunction clean intermittent catheterization (CIC) urethral abnormalities hypospadias urethrorectal fistula stricture congenital anomalies of the ejaculatory duct STD : in postpubertal sexually active males Dr. Khaled Madbouly, MD.
Epididymitis Presentation : Acute scrotal pain : gradual onset no nausea and vomiting fever Voiding symptoms Localized epididymal enlargement and tenderness Cremasteric reflex is symmetric. Dr. Khaled Madbouly, MD.
Epididymitis Investigations : Urine : pyuria 20 – 40% +ve urine culture Blood : leucocytosis Color doppler ultrasound : increased epididymal size increased blood flow in the epididymis / testis Dr. Khaled Madbouly, MD.
Epididymitis Treatment : Documented UTI with epididymitis / epididymo-orchitis IV antibiotics Hospitalization Renal ultrasonography VCUG after resolution of infection No documented UTI Symptomatic treatment Ultrasound if repeated Dr. Khaled Madbouly, MD.
Orchitis Ø Non specific Ø Specific Mumps orchitis Mumps is a contagious viral disease (RNA virus) Painful swelling of the parotid gland (parotitis) Orchitis in 20 -30%, 1 -2 weeks after parotitis Rare in prepubertal ~30% epididymoorchitis in adolescents and adults 50% will result in reduced testicular size (atrophy) 25% will result in abnormalities of semen analysis Subfertility is common, sterility is rare Dr. Khaled Madbouly, MD.
- Slides: 54