Pediatric GastrointestinalGeniturinary Emergencies Leybie Ang PEM Fellow Aug
Pediatric Gastrointestinal/Geniturinary Emergencies Leybie Ang PEM Fellow Aug 6 2009
Pediatric Gastrointestinal Emergencies
Objectives Approach to GI Bleed DDx Common Causes Life threatening Causes Approach to Abdominal Pain Case Presentations
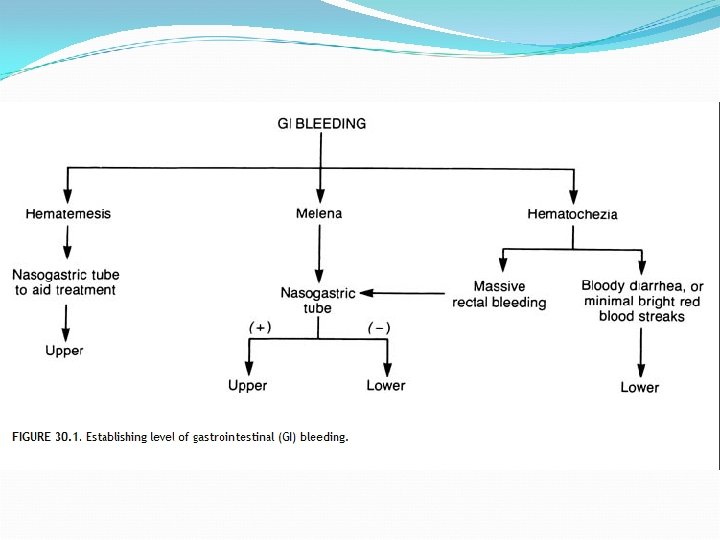
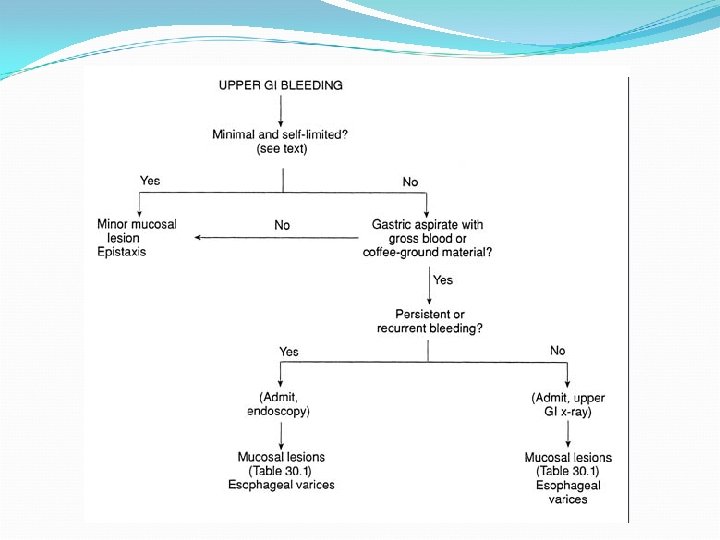
Approach to GI Bleed A B C Severity of the bleeding Site of the bleed
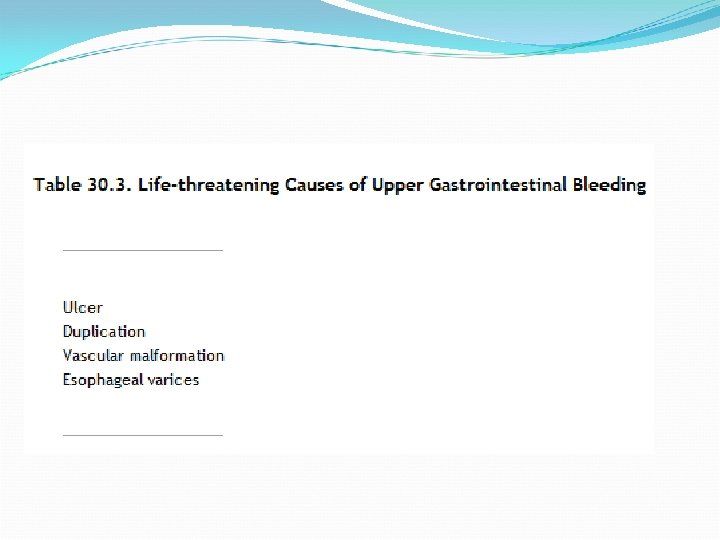
Common cause of UGI in neonatal period? Common cause of UGI in preschool age?
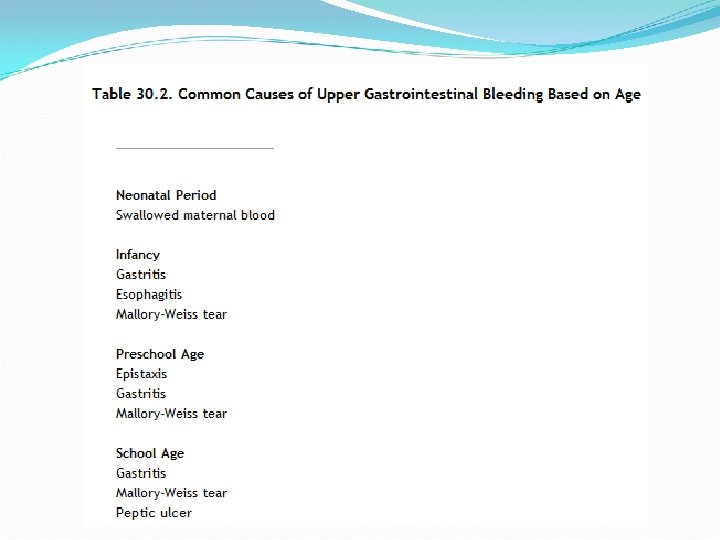
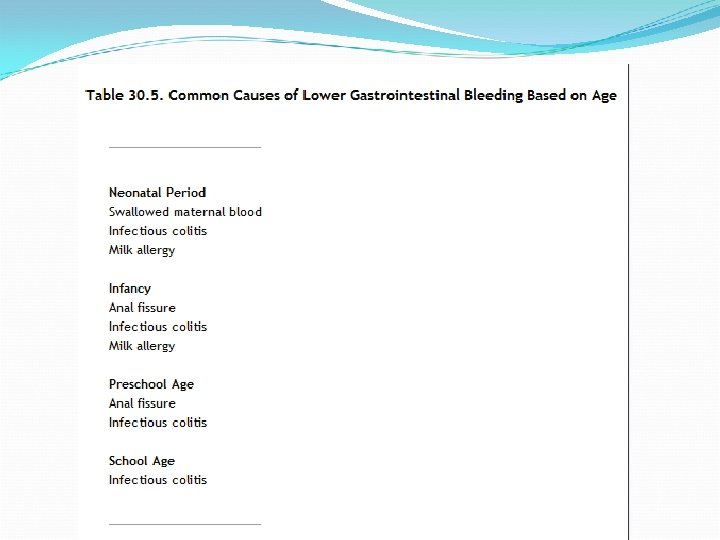
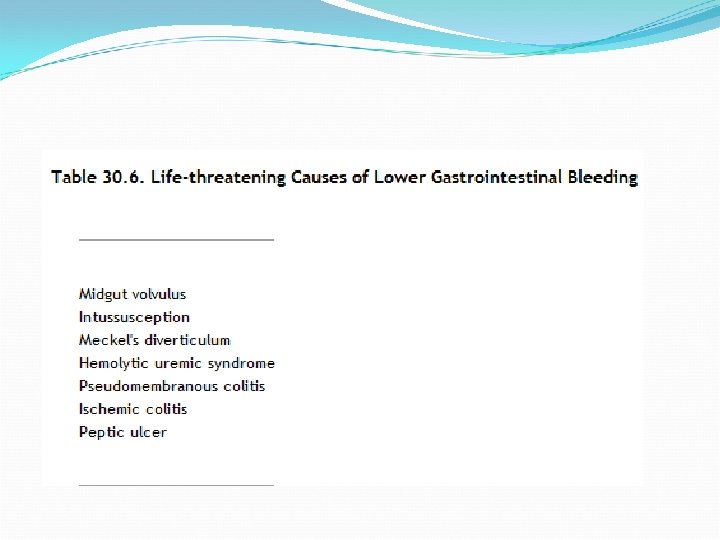
Common cause of LGI during neonatal period? Common cause of LGI during infancy?
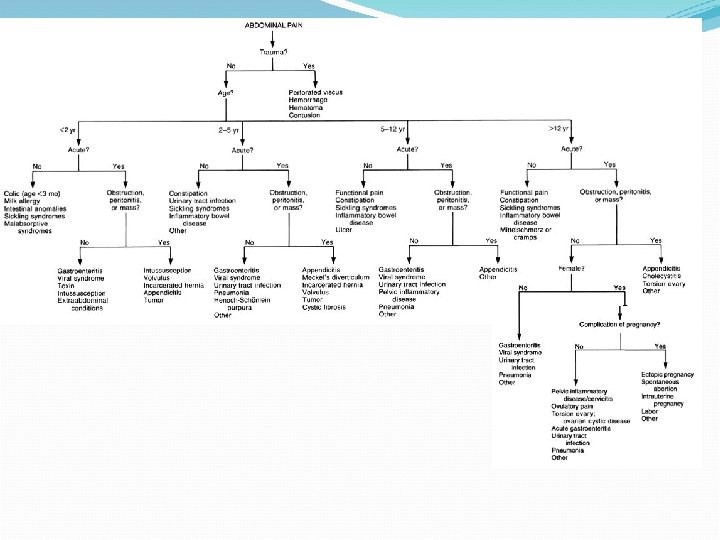
Approach to Abdominal Pain
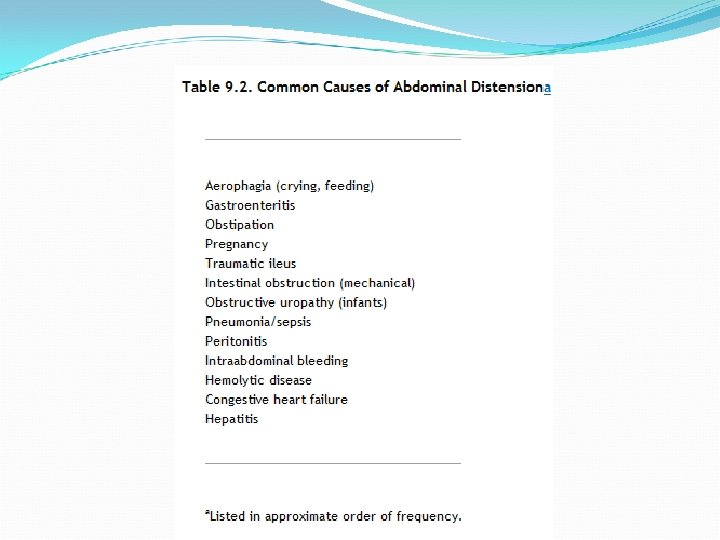
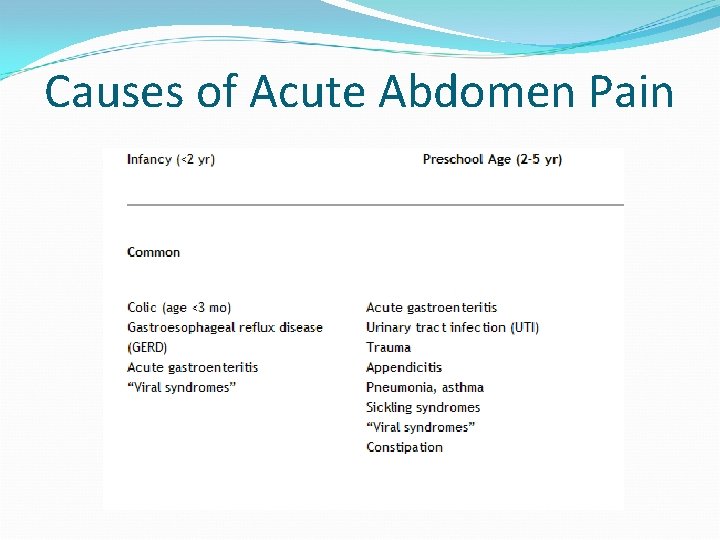
Causes of Acute Abdomen Pain
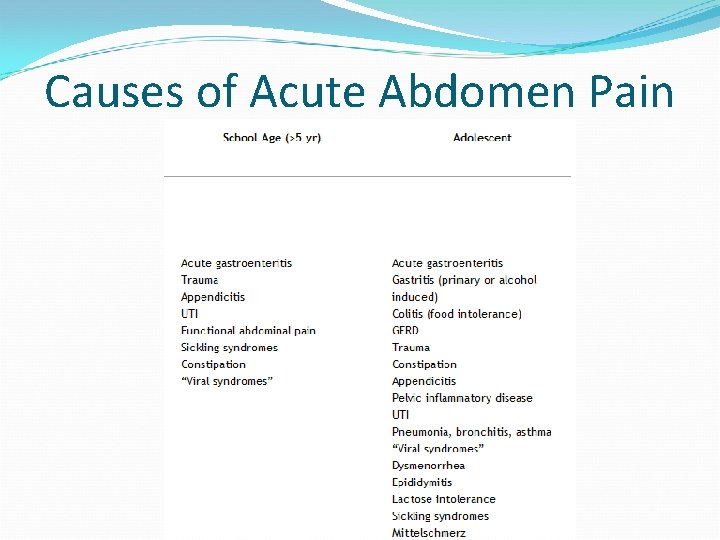
Causes of Acute Abdomen Pain
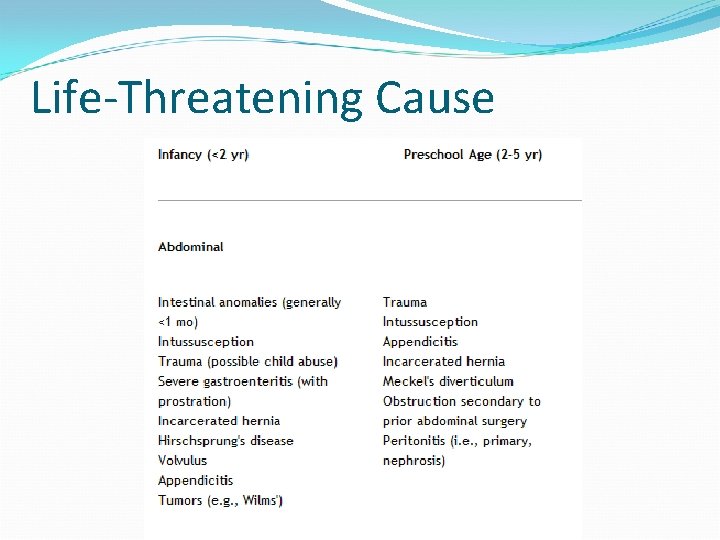
Life-Threatening Cause
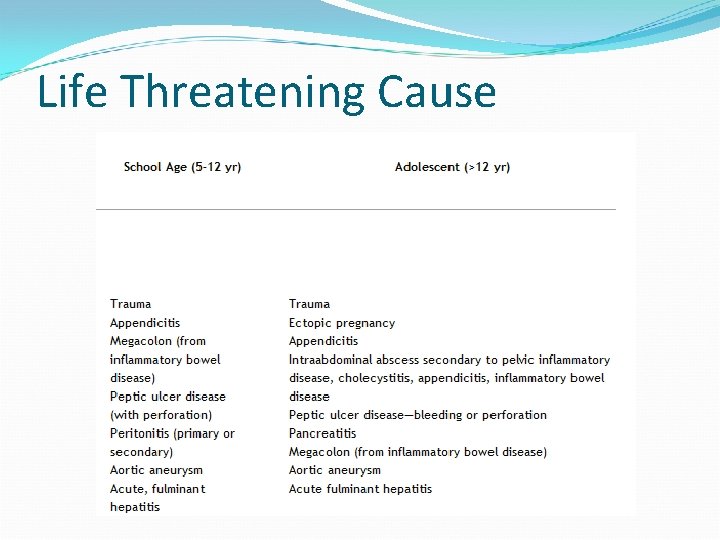
Life Threatening Cause
Case Presentation #1 2 week old male presented with abdominal distension At triage, noted to have bilious vomiting Former 37 weeker SVD SCN stay x 48 hr for ? TTN No sick contact Afebrile HR 200 RR 65 O 2 sat 98% RA Fussy but consolable GI exam revealed distended abdomen
Case Presentation #1 (con’t) Management priorities? Likely diagnosis?
Malrotation With Midgut Volvulus Congenital malrotation of the midgut During 5 th-8 th embryonic week, intestine projects out of cavity, rotates 270 degree and then returns If incomplete rotation, intestine does not anchor at the mesentry Volvulus is twisting of a loop of bowel about the mesentric attachment
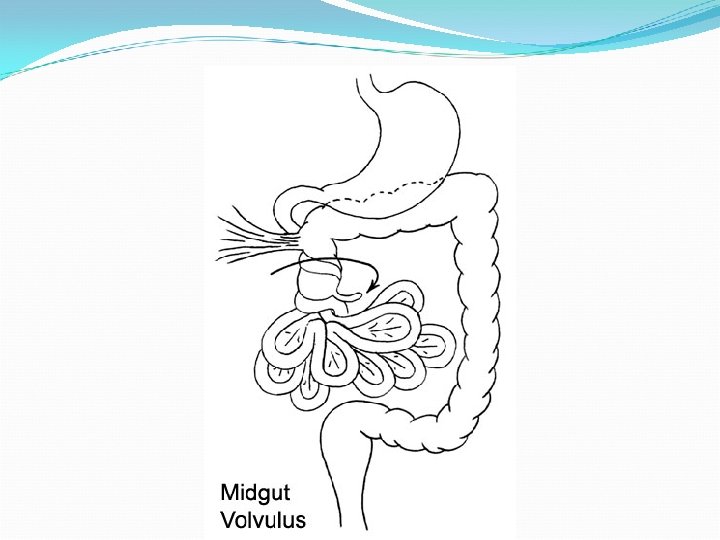
Malrotation with Volvulus Incidence 1 in 500 Male-to-female ratio 2: 1 Usually presents in the first year of life Bilious vomiting Abdominal distension Hematochezia
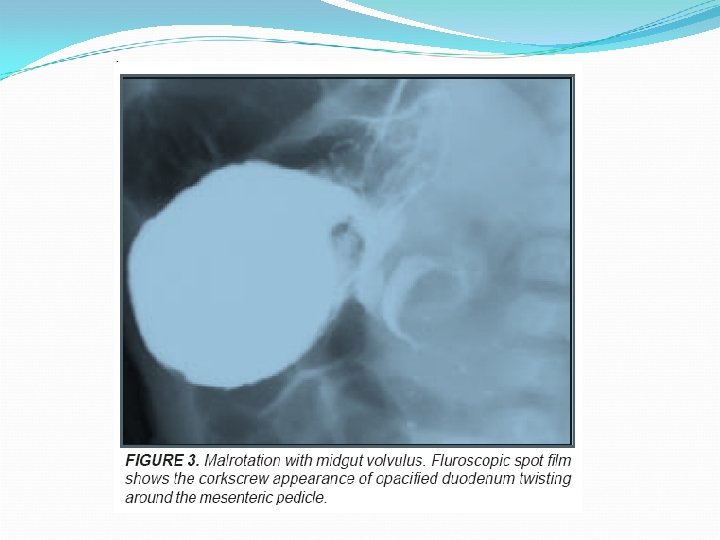
Imaging Abdominal films – Classic double bubble sign Upper GI (GOLD STD) – “cork-screwing”, spiraling of SB around SMA US – distended, fluid filled duodenum, with dilated loops of bowel to the right of the spinal column


Treatment SURGICAL CONSULT!!! IV hydration Correction of electrolytes NG tube
Case Presentation 2 1 yo female presents with vomiting, and intermittent abdominal cramping Noted to be lethargic PE revealed palpable mass in RUQ Heme positive stools
Most likely diagnosis? ? ? Management? ? ?
Intussusception Telescoping of a segment of bowel into an adjacent segment Mesentery and venous supply obstruct mucosal edema and increased pressure arterial flow obstruction Incidence: 6 mo to 2 yo
Intussusception Most common location ? ? ? Most common reported symptoms ? ? ?
Intussuception Idiopathic Meckel’s Diverticulum HSP Polyps Tumors Lymphoma
Intussusception Intermittent, colickly abdominal pain Currant jelly stools => late finding +/- RUQ mass Emesis -> bilious Heme positive stools
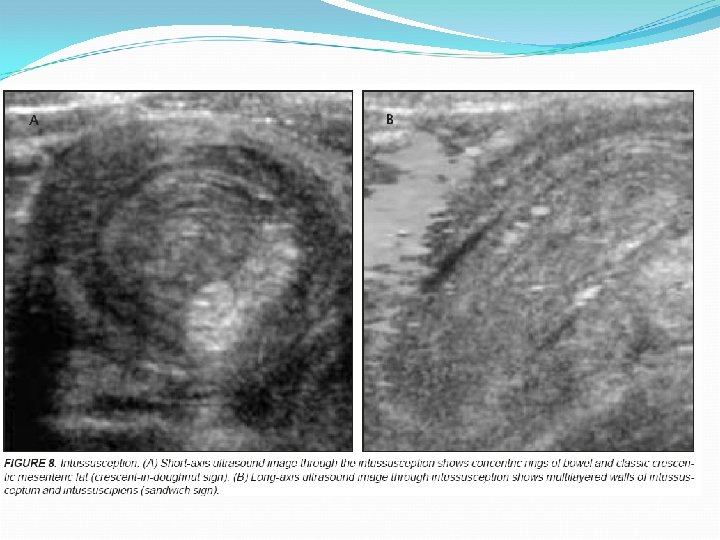
Intussusception - Dx AXR – may normal initially, but then may see signs of obstruction, paucity of air and dilated loops of bowel US – “target” or “donut” sign = single hypoechoic ring with hyperechoic center “pseudokidney” sign = superimposed hypo- and hyperechoic rings of edematous bowel and compressed mucosal layers

What is crescent sign? Please show it in the imaging below….


Air Enema vs Contrast Enema PROS Inert Rapid Less radiation Air perforation better than contrast perforation Easier to administer CONS May miss the lead point Poorer visualisation
Absolute contraindication? ? ?
Case Presentation 3 6 yo male presents with diffuse abdo pain, decreased appetite, fever, vomiting, increased pain with motion T 38 HR 120 bp 108/58 RR 22 In moderate discomfort Abdo exam revealed tenderness over periumbilical pain with rebound tenderness Differential diagnosis?
Appendicitis Most common etiology for surgical abdomen in children Third leading cause of pediatric hospitalisation Incidence 4 cases per 1000 children Male to female ratio 2: 1
Appendicitis Mortality in children 0. 1 -1% False positive rate 15 -20% Perforation rate 15 -40% in younger children due to delayed in diagnosis In younger children <5 yo, , perforation rate 50 -85% Morbidity in children treated with appendicitis results either from late diagnosis or negative appendectomy
Pathophysiology Blockage of lumen with stool, barium, food or parasites Swollen lymph glands Hyperplastic lymphoid tissue Edematous appendical mucosa Increase intraluminal pressure Persistence inflammation Exudate drainage
Pathophysiology (con’t) Exudate touches parietal peritoneum Pain (diffuse) Fecal bacteria grown within the obstructing material Worsening inflammation response Further increase intraluminal pressure perforation
Pathophysiology (con’t) Peritonitis develops In adult, the omentum can wall off inflamed or perforated appendix In child, less well developed omentum, hence decrease the ability to wall off perforation More likely to have peritonitis Severe blunt abdo trauma
History Classic history Anorexia, pain migrated from periumbilical to RLQ and vomiting Less than 60% patients Pain precedes vomiting Afebrile or low grade fever High grade – after perforation
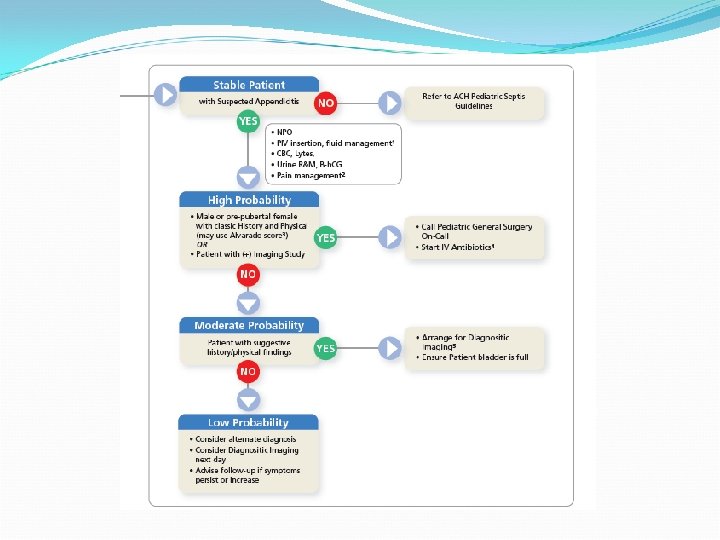
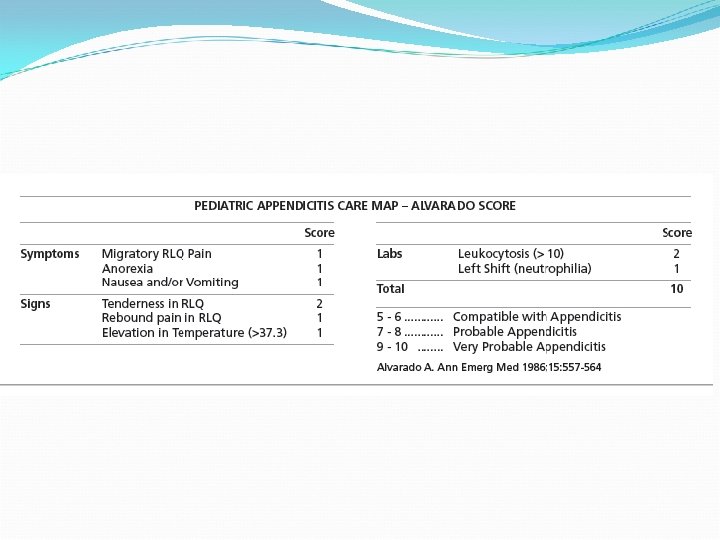
Appendicitis – Signs & Symptoms Am Emerg Med, 1986; 15: 557 -561 M – Migration of pain A – Anorexia N – Nausea/Vomiting T – Tenderness R – Rebound E – Elevated temperature L – Leukocytosis S – Shift (Bandemia)
Pain Meds? ? ? Green R et al. Pediatrics 2005 5 – 16 yo with acute abdominal pain requiring surgical consult 52 – IV morphine 56 – IV placebo Standardised form used to document clinical data and physician confidence in dx and 15 min after meds Surgeon see pt w/i 1 hr and same data collected Pt monitored for 2 weeks after enrollment
Conclusion Green R et al. Pediatrics 2005 No difference in MD confidence – ED or surgeon’s after morphine No difference in significant decrease in pain No difference in diagnosis
Management Emergency appendectomy (operation within 6 hr) in children has no advantages over urgent appendectomy (operation with 12 h) wrt gangrene and perforation rates, readmissions, postoperative complications, hospital stay, or hospital charges.
Pediatric Geniturinary Emergencies
Objectives Approach to hematuria DDx for testicular mass
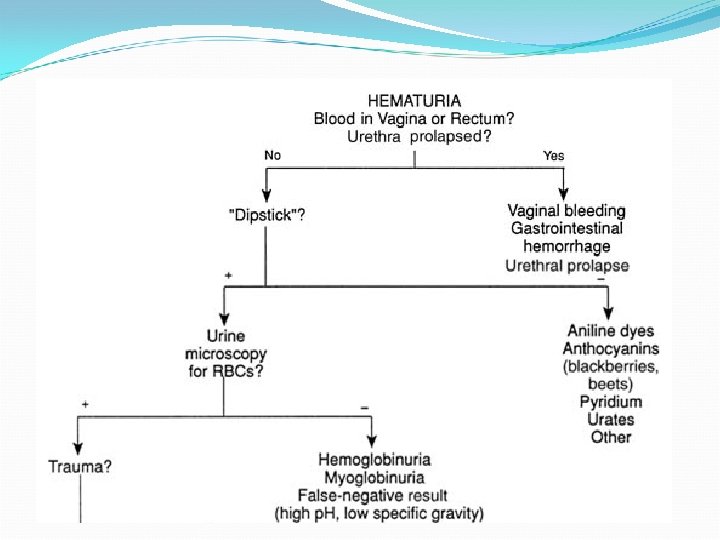
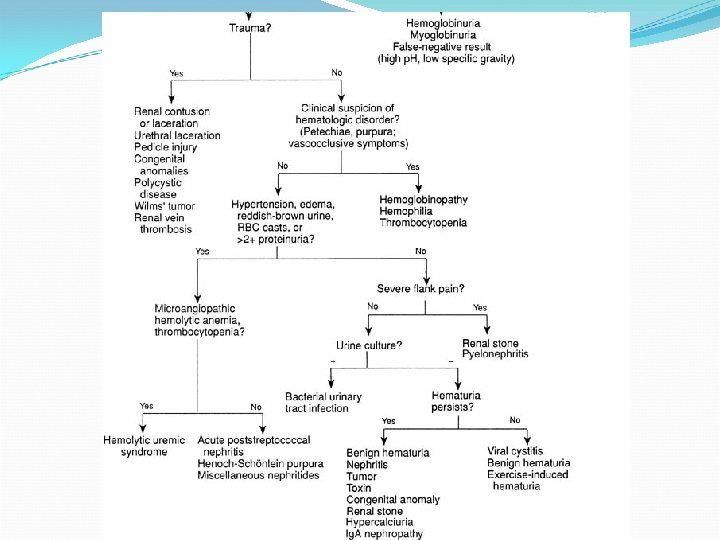
Approach To Hematuria Determine if the pigment in urine is from blood or other source. Are red blood cells present? Determine the source of bleeding, i. e. , kidney, bladder, urethra. Select those who will require referral versus those who simply require follow-up.
Case Presentation #5 10 yo male presented with 24 hour of scrotal pain. Mom noted that patient was walking “funny” Afebrile HR 120 bp 120/75 RR 18 O 2 sat 97% RA PE exam revealed patient in moderate discomfort GI revealed benign exam GU revealed erythema, swollen right testes. High riding testes with absent cremasteric reflex on the right
Differential diagnosis PAINFUL SCROTAL PAIN Torsion of spermatic cord Torsion of testicular appendage Epididymitis Orchitis Incarcerated hernia Hematocele
Differential diagnosis PAINLESS SCROTAL SWELLING Hydrocele Variocele Testicular cancer Nonincarcerated inguinal hernia Spermatocele Localised edema from insect bites Nephrotic syndrome
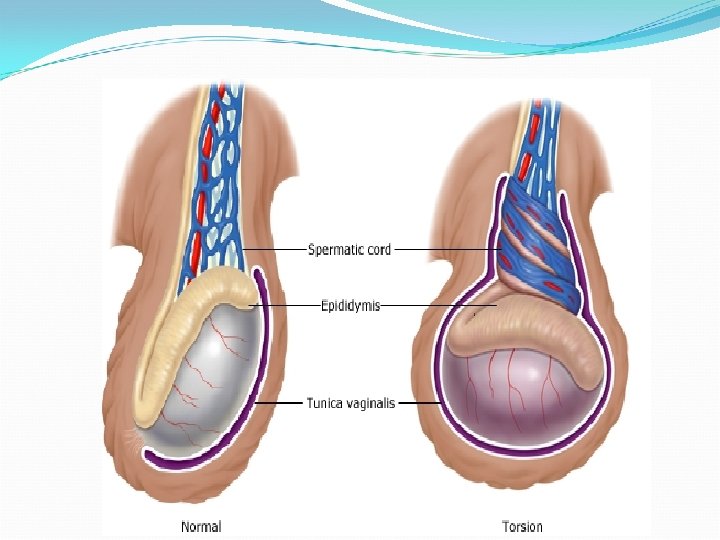
Testicular Torsion Most dramatic and potentially serious acute process affecting the scrotum Associated with anatomic anomaly of the tunica vaginalis Normally the tunica vaginalis inserts at the lower pole of testis (gubernaculum testes) Testes lack of the normal attachment to tunica vaginalis and rest transverse w/i scrotum
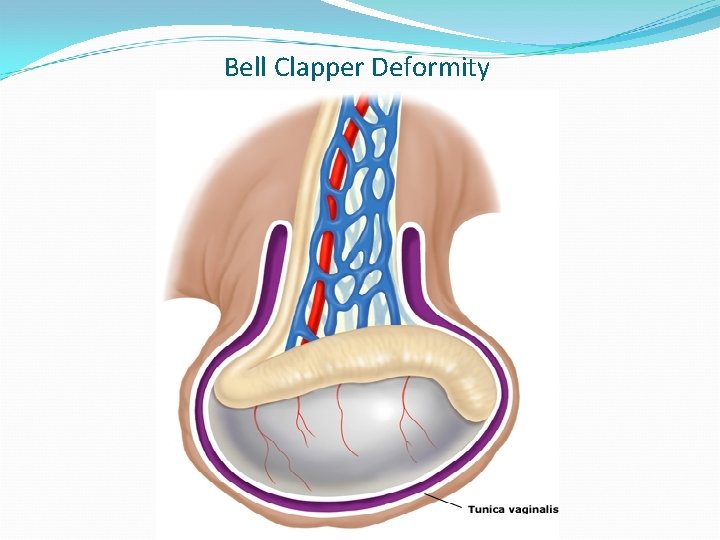
Bell Clapper Deformity
Testicular Torsion Deformity permits xs mobility of testis, increasing likelihood of torsion on its spermatic cord and compromise blood flow If bell clapper deformity, usually bilateral Twisting of spermatic cord w/i tunica vaginalis causes venous compression and subsequent edema of testicle and cord -> arterial occulsion ischemia
Testicular Torsion Can occur at any age Two peak incidence: neonatal period and puberty 1: 4000 in males <25 yo 65% cases in boys 12 -18 yo Increased incidence during adolescent - secondary to increase of weight of testes during puberty
Clinical Presentation Abrupt onset of severe scrotal pain Typical presentation: awaken from sleep with scrotal pain in the middle of night +/- radiation to lower abdomen Nausea/vomiting
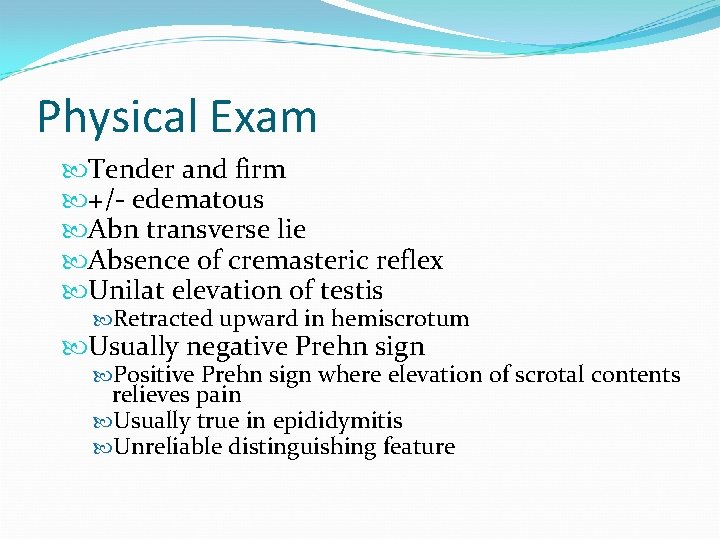
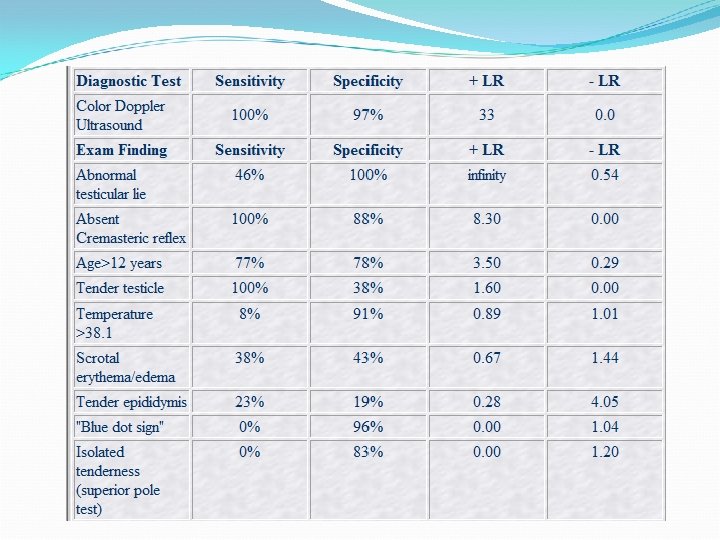
Physical Exam Tender and firm +/- edematous Abn transverse lie Absence of cremasteric reflex Unilat elevation of testis Retracted upward in hemiscrotum Usually negative Prehn sign Positive Prehn sign where elevation of scrotal contents relieves pain Usually true in epididymitis Unreliable distinguishing feature
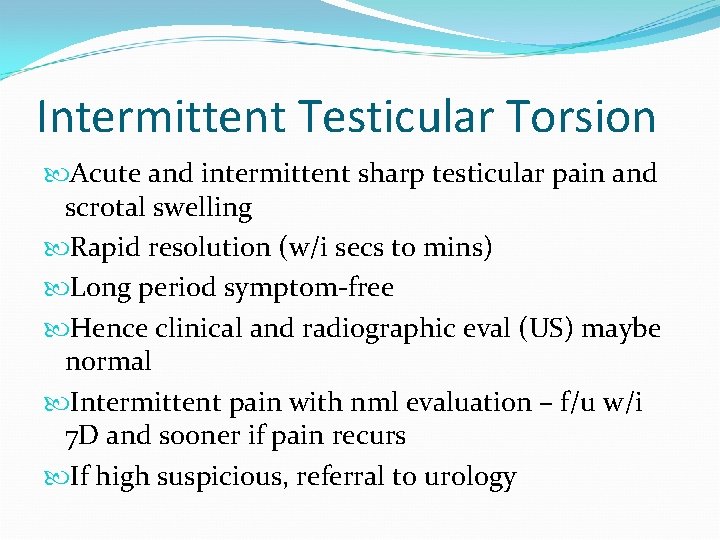
Intermittent Testicular Torsion Acute and intermittent sharp testicular pain and scrotal swelling Rapid resolution (w/i secs to mins) Long period symptom-free Hence clinical and radiographic eval (US) maybe normal Intermittent pain with nml evaluation – f/u w/i 7 D and sooner if pain recurs If high suspicious, referral to urology
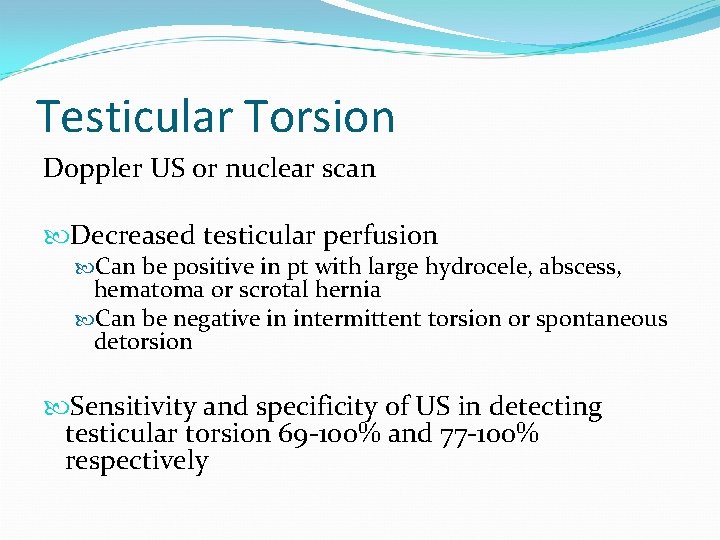
Testicular Torsion Doppler US or nuclear scan Decreased testicular perfusion Can be positive in pt with large hydrocele, abscess, hematoma or scrotal hernia Can be negative in intermittent torsion or spontaneous detorsion Sensitivity and specificity of US in detecting testicular torsion 69 -100% and 77 -100% respectively
Limited usefulness in doppler US in prepubertal pt due to lower blood flow Nuclear scan sensitivity and specificity 100 and 97% respectively
Management of Testicular Torsion SURGICAL EMERGENCY!!! Increased time in a state of torsion is inversely proportional to testis survival rates Urology/surgery consult Surgical detorsion of affected testes Orchiopexy of both testes Bell clapper deformity bilateral If nonviable orchiectomy
What is the viability if detorsion happens after 12 hr? ? ?
Viability & Fertility Studies have shown: Detorsion w/i 4 -6 hr 100% viability Detorsion after 12 hr 20% viability Detorsion after 24 hr 0% viability Fertility controversial issues Decreased fertility after unilat torsion (immune-mediated damage) No evidence of decreased fertility or anti-sperm antibodies Heindel et al The effect of unilateral spermatic cord torsion on fertility in the rat JUrol 1990 Aug; 144: 366 -9 If torsion >720 degree or more causes a significant reduction of subsequent fertility
Manual Detorsion Manual detorsion if experienced clinician available, definitive care hours away and appropriate sedation and analgesics Textbook teaching: Testes rotates medially normally To detorse, rotate outward towards the thigh. Retrospective study showed pt with surgical detorsion, 1/3 has lateral rotation Successful detorsion if pain relief, lower position of testes and return of normal arterial pulsations (US) Still need to have orchiopexy
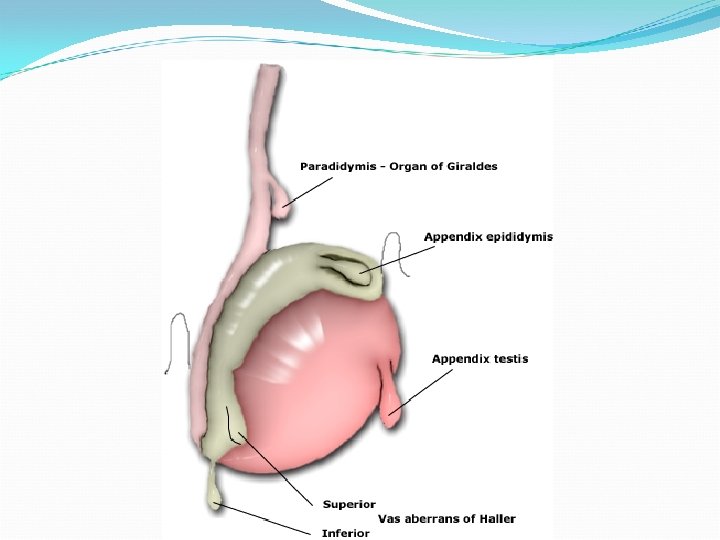
Torsion of Appendix Testes Sudden onset pain Less severe pain Usually tender localised palpable mass at superior/inferior pole Tiny, localised swelling pain localised to upper portion of testis Blue dot sign gangrenous/black appendix through scortal skin (esp in lightly pigmented skin pt)
Torsion of Appendix Testes Nearly always able to elicit cremasteric reflex +/- Reactive hydrocele US showed nml or increased blood flow to affected testis (2 nd to inflammation) Lesion of low echogenicity with central hypoechogenic area Unable to visible involved appendage In prepubertal, US unreliable (low baseline testicular perfusion)
Management Supportive management Analgesics Bed rest Pain resolve in 5 -10 D If persistent pain -> surgery to remove testicular appendix Contralateral hemiscrotum need not to be explored
Epididymitis Inflammation of epididymis Common among adolescents Often caused by infections Sexually active – Chlamydia, N. gonorrhea and viruses Less commonly - Ureaplasma, Mycobacterium, CMV/Cryptococcus in pt with HIV
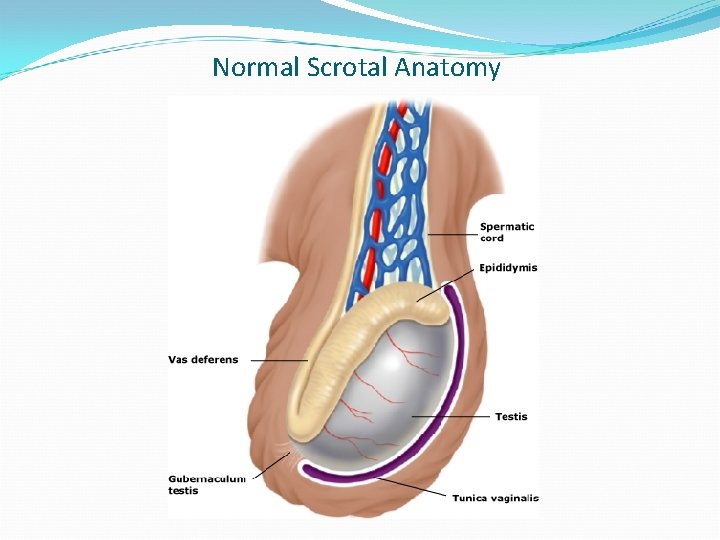
Normal Scrotal Anatomy
Epididymitis Occur in younger boys who deny sexual activity Other causes: heavy physical exertion, bicycle/motorcycle riding, structural anomalies of UT Noninfectious – chemical inflammation swelling ductal obstruction reflux of sterile urine through ejaculatory ducts and vas into epididymis
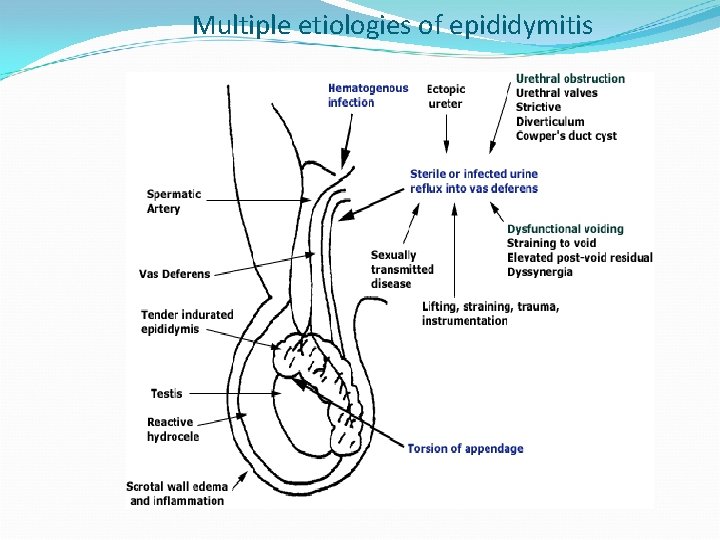
Multiple etiologies of epididymitis
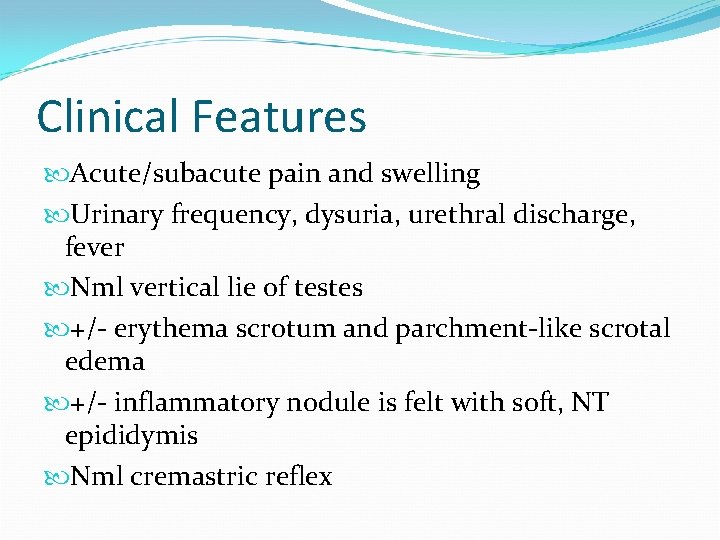
Clinical Features Acute/subacute pain and swelling Urinary frequency, dysuria, urethral discharge, fever Nml vertical lie of testes +/- erythema scrotum and parchment-like scrotal edema +/- inflammatory nodule is felt with soft, NT epididymis Nml cremastric reflex
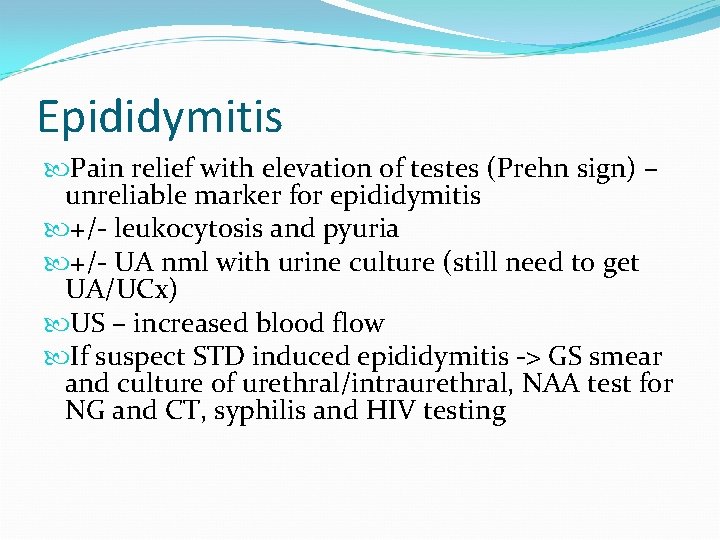
Epididymitis Pain relief with elevation of testes (Prehn sign) – unreliable marker for epididymitis +/- leukocytosis and pyuria +/- UA nml with urine culture (still need to get UA/UCx) US – increased blood flow If suspect STD induced epididymitis -> GS smear and culture of urethral/intraurethral, NAA test for NG and CT, syphilis and HIV testing
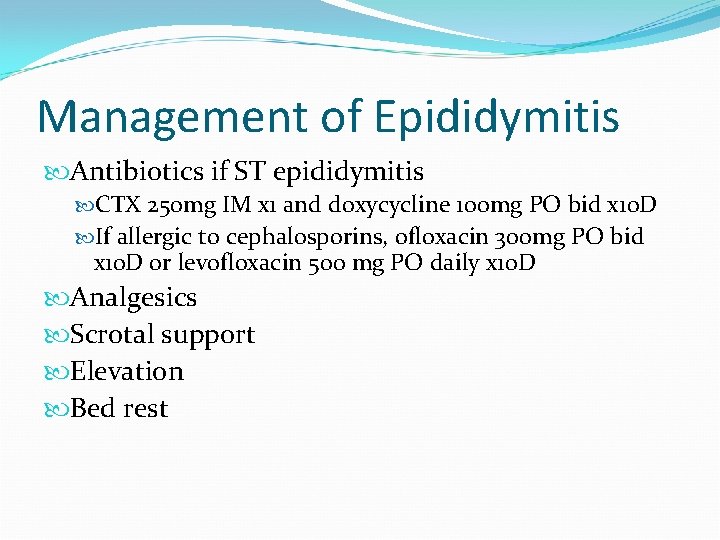
Management of Epididymitis Antibiotics if ST epididymitis CTX 250 mg IM x 1 and doxycycline 100 mg PO bid x 10 D If allergic to cephalosporins, ofloxacin 300 mg PO bid x 10 D or levofloxacin 500 mg PO daily x 10 D Analgesics Scrotal support Elevation Bed rest
Orchitis Acute inflammation reaction of the testes Mostly associated with viral infection
Bacterial Orchitis rare usually associated with a concurrent epididymitis (epididymo-orchitis) occur in sexually active males > 15 yo Unilateral testicular edema occurs in 90% of cases Bugs in immunocompromised pt?
Clinical features Testicular pain and swelling course variable and ranges from mild discomfort to severe pain. Fatigue Malaise Myalgias Fever and chills Nausea Headache Mumps orchitis follows the development of parotitis by 47 days. complicated by a reactive hydrocele or pyocele
Physical exam Testicular enlargement and tenderness Induration of the testis Erythematous scrotal skin Edematous scrotal skin Enlarged epididymis If associated with epididymo-orchitis Rectal examination Soft boggy prostate (prostatitis) often associated with epididymo-orchitis Parotitis
Diagnosis based on history and physical examination if concerns for epididymo-orchitis UA and culture urethral cultures serum immunofluorescence antibody testing Color Doppler ultrasound to rule out testicular torsion. inflammation of the testis or the epididymis
Management Rule out testicular torsion Supportive treatment (viral) Analgesics Bed rest Hot or cold packs If highly suspicious for epididymo-orchitis, treat appropriately. If a significant hydrocele or pyocele is detected or suspected surgical tapping Bacterial orchitis or epididymo-orchitis requires appropriate antibiotic coverage
Complications ~60% with orchitis Unilateral testicular atrophy Sterility is rarely a consequence of unilateral orchitis. little evidence supports an increased likelihood of developing a testicular tumor after an episode of orchitis.
Hydrocele Collection of peritoneal fluid between the parietal and visceral layers of tunica vaginalis Communicating vs noncommunicating Communicating result of failure of the processus vaginalis to close during development fluid around testes is peritoneal fluid
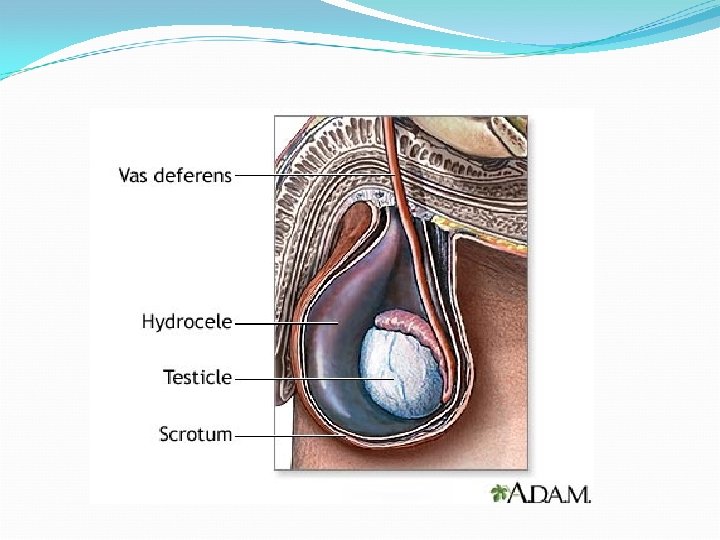
Hydrocele Noncommunicating no connection to the peritoneum; the fluid comes from the mesothelial lining of tunica vaginalis Common in newborns and majority spontaneously resolve In older children and adolescents Idiopathic secondary to epididymitis, orchitis, testicular torsion, torsion of the appendix testes/epididymis, trauma or tumor (reactive hydrocele)
Communicating usually cystic scrotal mass Reducible increase mass in size during the day or with valsalva maneuver Non communicating not reducible no change in size or shape with crying/straining Transillumination of scrotum cystic fluid collection US of testes to r/o primary causes
In newborns – spontaneously resolution by 1 year of age If communicating, rarely resolve and risk of incarcerated inguinal hernia If tense scrotum – concerns for reduce circulation to testes surgical repair at time of diagnosis If secondary causes, treat underlying condition

Varicocele Collection of dilated and tortuous veins in the pampiniform plexus surrounding the spermatic cord in scrotum Result from increased venous pressure and incompetent valves Commonly on left side (85 -95%) Left spermatic vein entering left renal vein to a 90 degree angle Right spermatic vein drains more obtuse angle directly in IVC – more continuous flow 10 -15% varicoceles - infertility
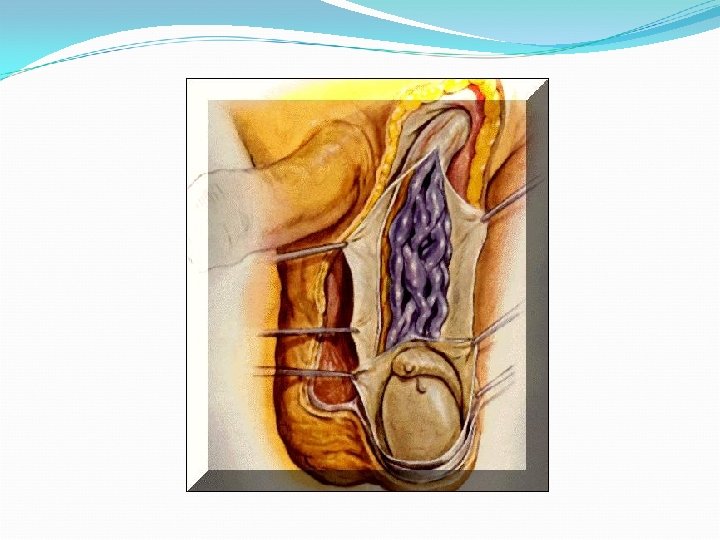
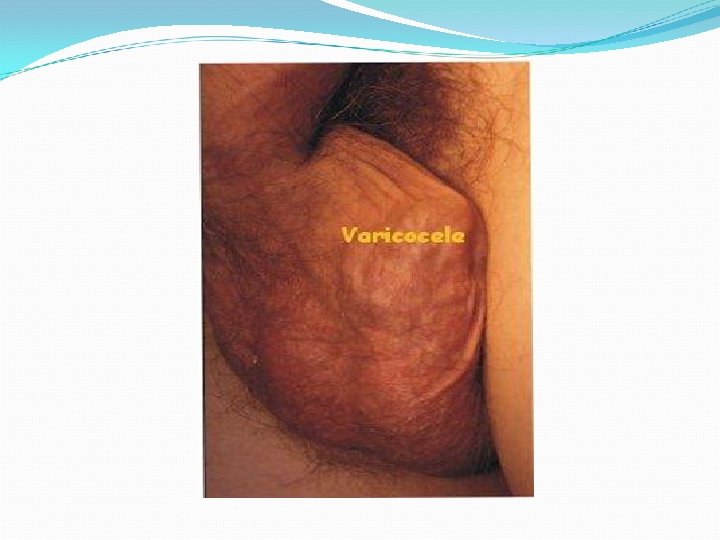
Varicocele Asymptomatic c/o dull ache in scrotum upon standing Gr I (small) – palpable only with valsalva maneuver Gr II (mod) – nonvisivible on inspection, but palpable upon standing Gr III (large) - Visible distention around spermatic cord Palpable varicocele – texture of “a bag of worms”
Varicocele Examined in both supine and standing position If idiopathic – prominent when upright and disappears in supine If secondary – no change in size with change of position US r/o IVC thrombus, right renal vein thrombosis with clot propagation down IVC and abdo mass
Varicocele Conservative management Observation Surgical ligation / Testicular vein embolization Affected testicular vol < unaffected testicle (diff in size of >10 -15% or >2 m. L by US) Presence of bilat varicoceles Large varicoceles (Gr III) Presence of scrotal pain
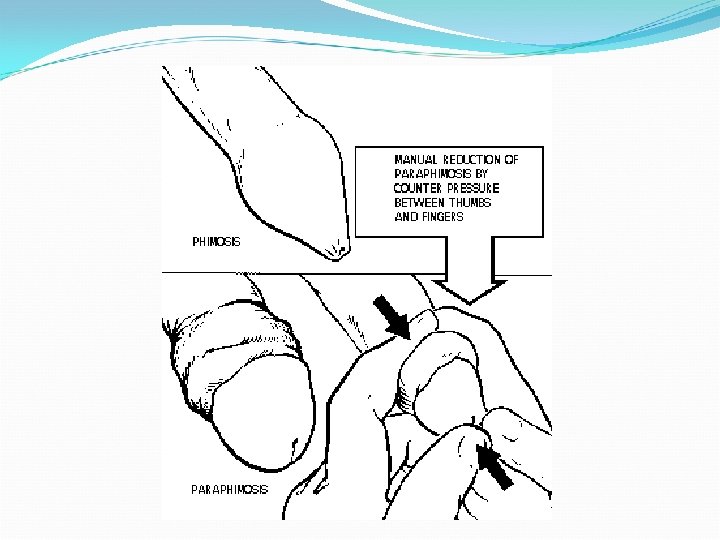
Paraphimosis SURGICAL EMERGENCY occurs when a phimotic ring of foreskin is retracted, becoming trapped proximal to the coronal sulcus Significant edema of the glans penis Ischemic injury to the glans
Paraphimosis - Management Reduction of the foreskin Manually after applying gentle constant pressure to the edematous foreskin with or without local anesthesia Surgically by division of the phimotic ring. Circumcision is advisable at some point after the occurrence
Hair Tourniquet Syndrome SURGICAL EMERGENCY Circumferential strangulation of an appendages or genitalia by human hairs or fibers Ischemic injury to the glans may occur if not relieved promptly by division and removal of the hair strand
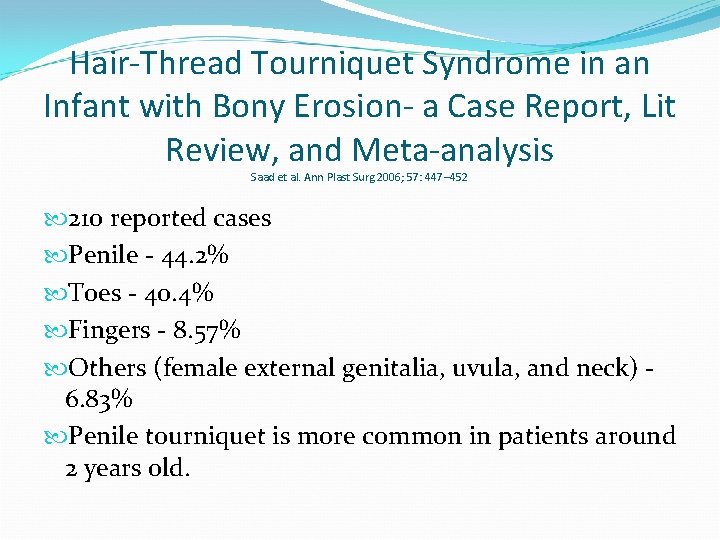
Hair-Thread Tourniquet Syndrome in an Infant with Bony Erosion- a Case Report, Lit Review, and Meta-analysis Saad et al. Ann Plast Surg 2006; 57: 447– 452 210 reported cases Penile - 44. 2% Toes - 40. 4% Fingers - 8. 57% Others (female external genitalia, uvula, and neck) 6. 83% Penile tourniquet is more common in patients around 2 years old.


What product would you use to remove hair torniquet on finger/toe non-operatively? ? ?
Post-Circumcision Bleeding remains the commonest complication encountered during and after circumcision Reported incidence ranges from 0· 1 to 35 per cent Majority is minor bleed Required to achieve haemostasis is gentle pressure
Post-Circumcision Bleed Excessive bleeding Anomalous vessels Bleeding disorder 13 000 circumcisions reported in two large series, no patient required blood transfusion for bleeding In the event of a bleeding disorder, appropriate clotting factors may have to be administered.
Circumferential bandage may be used to aid haemostasis May cause a degree of urethral obstruction which in severe cases, leads to urinary retention and may dispose thus dispose to urinary tract infection

- Slides: 124