Pediatric gastrointestinal bleeding Saja Saraireh Abrar Areed Amer
Pediatric gastrointestinal bleeding Saja Saraireh Abrar Areed Amer al. Hajji Wael Alsanany
Introuduction �Gastrointestinal (GI) bleeding in infants and children occurs frequently. Fortunately, the majority of cases do not result in serious health consequences. �The initial approach to patients with significant GI bleeding should be to ensure patient stability, to establish adequate oxygen delivery, to place intravenous access, to initiate fluid and blood resuscitation, and to correct any underlying coagulopathies.
SYMPTOMS OF UPPER GI BLEED Symptoms of upper gastrointestinal bleeding include : - Hematemesis vomiting of blood which can be bright red blood or dark clots, or coffee ground-like material. - Melena passing black, tar-like stool
SYMPTOMS OF LOWER GI BLEED Symptoms of lower gastrointestinal bleeding include : - Hematochezia passing pure blood , Blood clots mixed with or in between stool. - Acute bloody diarrhea should be considered a medical emergency in preterm and infant ( NEC , Volvulus and intussusception).
Etiology Age-specific etiologies for GI bleeding :
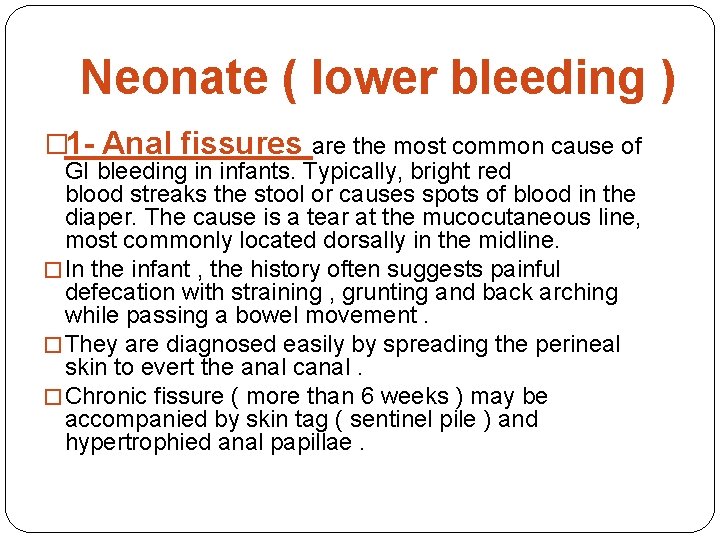
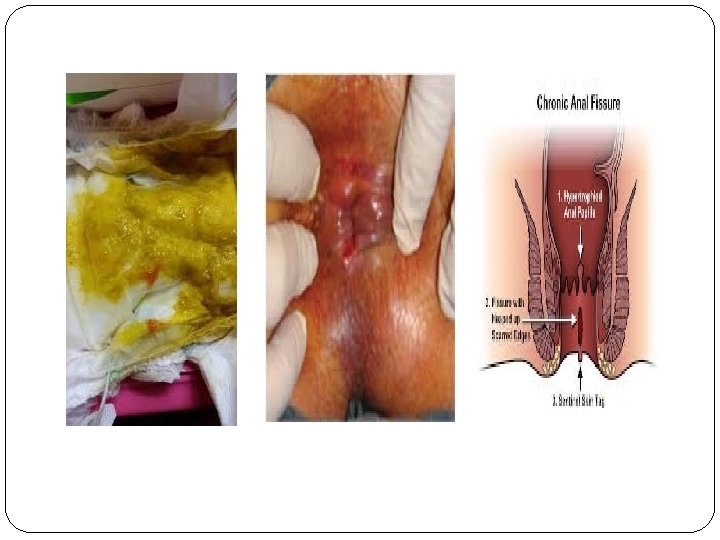
Neonate ( lower bleeding ) � 1 - Anal fissures are the most common cause of GI bleeding in infants. Typically, bright red blood streaks the stool or causes spots of blood in the diaper. The cause is a tear at the mucocutaneous line, most commonly located dorsally in the midline. � In the infant , the history often suggests painful defecation with straining , grunting and back arching while passing a bowel movement. � They are diagnosed easily by spreading the perineal skin to evert the anal canal. � Chronic fissure ( more than 6 weeks ) may be accompanied by skin tag ( sentinel pile ) and hypertrophied anal papillae.
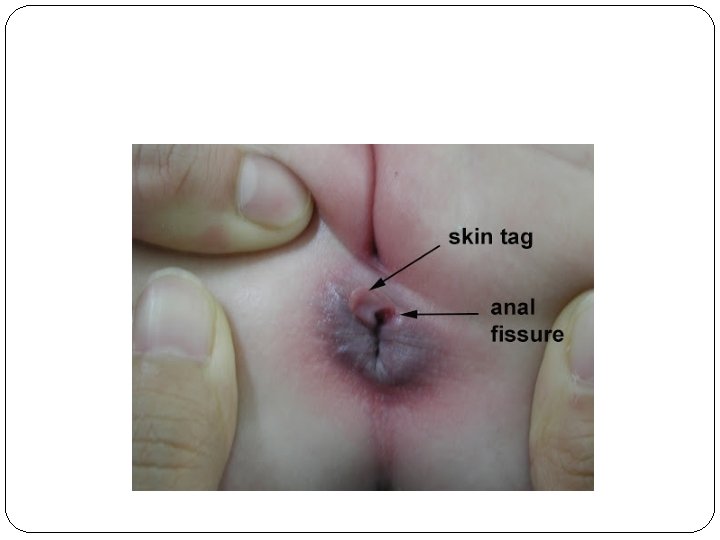
Treatment �Anal fissure usually respond to stool softener and lubricants such as vaseline �Vigorous wiping or use of glycerin suppositories should be avoided because they may further irritate the anal mucosa
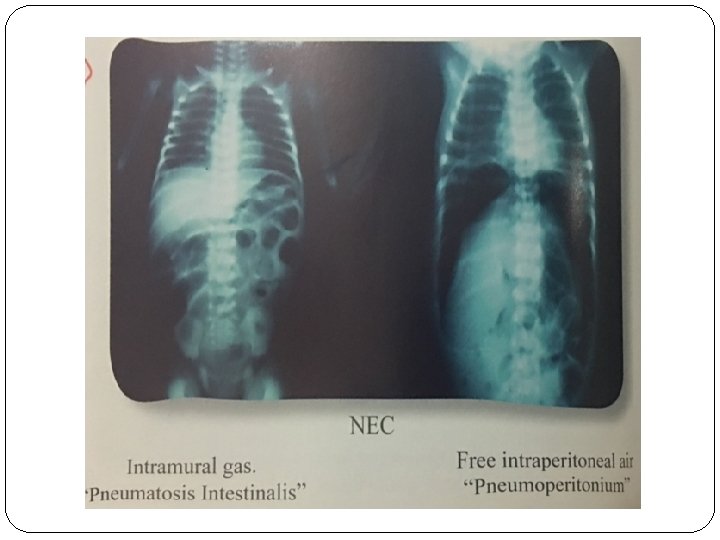
2 - Necrotizing enterocolitis (NEC) usually develops within 10 to 16 days after birth most commonly in premature infants and low birth weight ( less than 1. 5 kg ) , though can present in 13% of term infants. - It may involve single or multiple segment of the intestine , most comonly the terminal ileum. - Although the pathophysiology is currently unclear. the underlying mechanism is believed to involve a combination of poor blood flow and infection of the intestines.
- Symptoms of this condition include abdominal distension, poor feeding, vomiting, diarrhea, frank or occult bloody stools, lethargy and apnea. The baby may appear systemically ill : hypotention. Tachycardia , decrease urine output. - Abdominal examination : abdominal mass ( inflamed loop of bowel ) , tenderness , erythema and edema of anterior abdominal wall.
Treatment �Feeding are discontinued , NG tube placed , broad spectrum parenteral antibiotic are given. �Intubation and mechanical ventilation may be required. �Surgical intervention may be required.
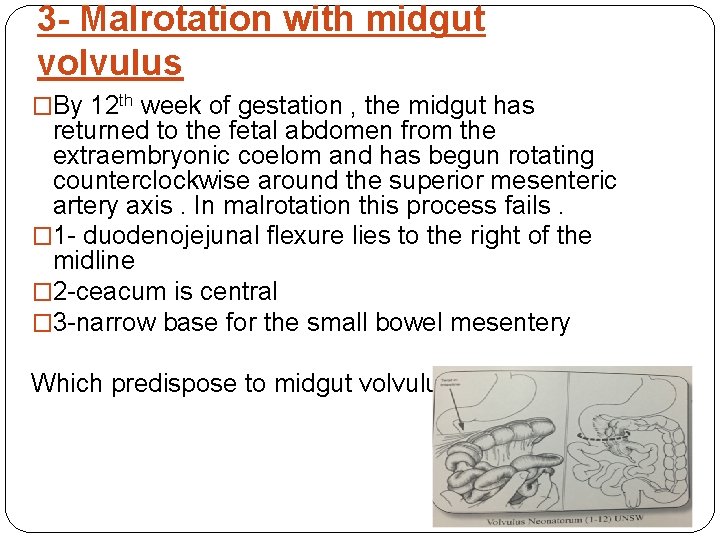
3 - Malrotation with midgut volvulus �By 12 th week of gestation , the midgut has returned to the fetal abdomen from the extraembryonic coelom and has begun rotating counterclockwise around the superior mesenteric artery axis. In malrotation this process fails. � 1 - duodenojejunal flexure lies to the right of the midline � 2 -ceacum is central � 3 -narrow base for the small bowel mesentery Which predispose to midgut volvulus
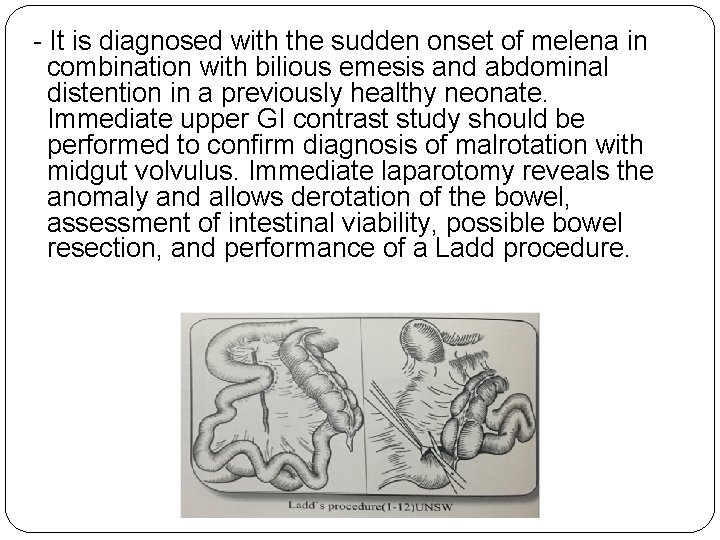
- It is diagnosed with the sudden onset of melena in combination with bilious emesis and abdominal distention in a previously healthy neonate. Immediate upper GI contrast study should be performed to confirm diagnosis of malrotation with midgut volvulus. Immediate laparotomy reveals the anomaly and allows derotation of the bowel, assessment of intestinal viability, possible bowel resection, and performance of a Ladd procedure.

Corkscrew sign
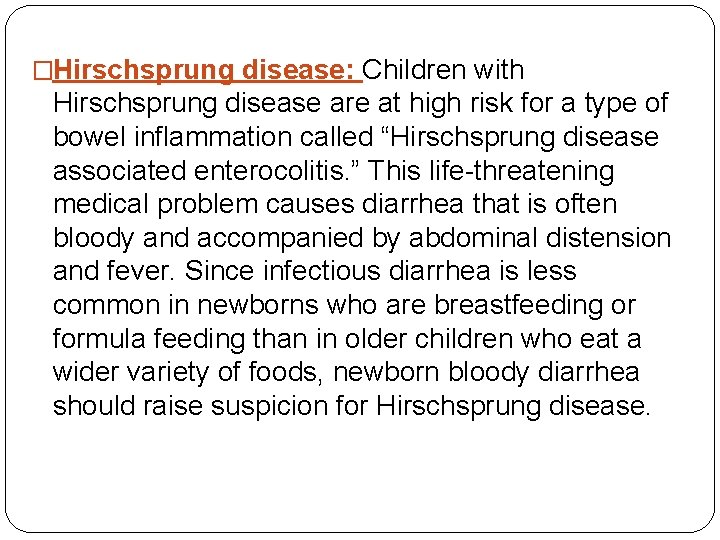
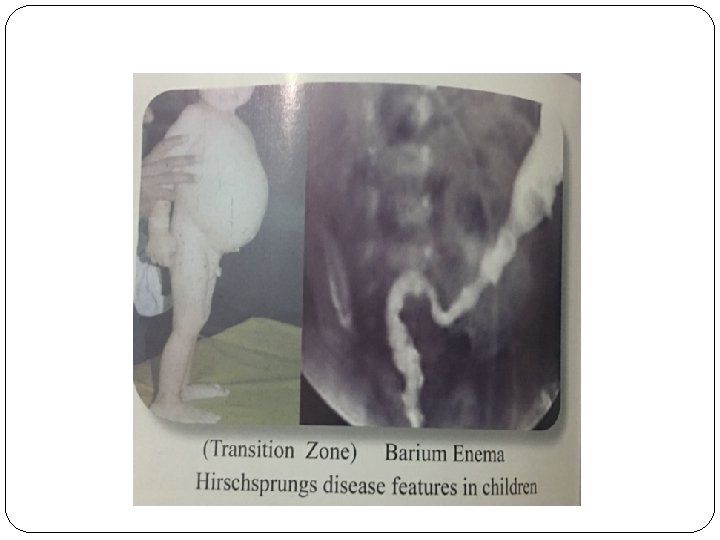
�Hirschsprung disease: Children with Hirschsprung disease are at high risk for a type of bowel inflammation called “Hirschsprung disease associated enterocolitis. ” This life-threatening medical problem causes diarrhea that is often bloody and accompanied by abdominal distension and fever. Since infectious diarrhea is less common in newborns who are breastfeeding or formula feeding than in older children who eat a wider variety of foods, newborn bloody diarrhea should raise suspicion for Hirschsprung disease.
Neonate ( upper bleeding ) 1 - Maternal blood ingestion - The most common cause of upper GI bleeding in neonates is due to maternal blood ingestion. This can also present as lower GI bleeding. This occurs when blood is swallowed during birth or from breast feeding ( cracked nipple ). The Apt tests differentiates between maternal and fetal hemoglobin.
2 - Stress gastritis is found mainly in neonates who are in the neonatal intensive care unit and it is highly correlated with prematurity, neonatal distress, and mechanical ventilation. Diagnosis is made by upper endoscopy in order to determine signs of erythema, diffuse bleeding, erosions or ulcerations of the gastric mucosa. - Stress ulcers in newborns are associated with dexamethasone, which can be used for fetal lung maturation.
3 - Hemorrhagic disease of the newborn resulting from a deficiency in vitamin K–dependent coagulation factors. levels of clotting factors II, VII, IX, and X decline rapidly after birth, reaching their nadir at 48 -72 hours of life. In 0. 25%-0. 5% of neonates, severe hemorrhage may result. - Addminstratiom of 1 mg vitamin k IV stop the bleeding with 2 hours.
Other causes : �Some drugs are implicated in neonatal GI bleeds. These include NSAIDs, heparin, and tolazoline, which are used for persistent fetal circulation. �Indomethacin, used for patent ductus arteriosus in neonates, may cause GI bleeding through intestinal vasoconstriction and platelet dysfunction. �Maternal medications can cross the placenta and cause problems in the developing fetus and in the neonate on delivery. Aspirin, cephalothin, and phenobarbital are well-known causes of coagulation abnormalities in neonates.
Clinical scenario � 14 -day old term male baby , presented to the ER for evaluation of spitting up bright red blood , the baby is feeding well and behaving normally , the physical exam is completely unremarkable , the baby looks great! �There were no problems with pregnancy or labor!
Clinical scenario � 14 -day old female born at 30 weeks gestational age via vaginal delivery , BW was 1400 g , presented with poor feeding , abdominl distension, bilious vomiting with bloody stool. � Her urine output is decreased, she is lethargic and slightly toxic. � Exam : T 36 , RR 60 , BP 60/40 , HR 185. � Her abdomen is distended with redness , tenderness , and hypoactive bowel sound. � Cardiac exam demonstrate tachycardia � Her early hospital course was remarkable for RDS � Investigation reveals leukocytosis , thrombocytopenia , increase in BUN and plasma creatinine with metabolic acidosis on ABG
Causes of GI bleed in infants (1 month -1 year)
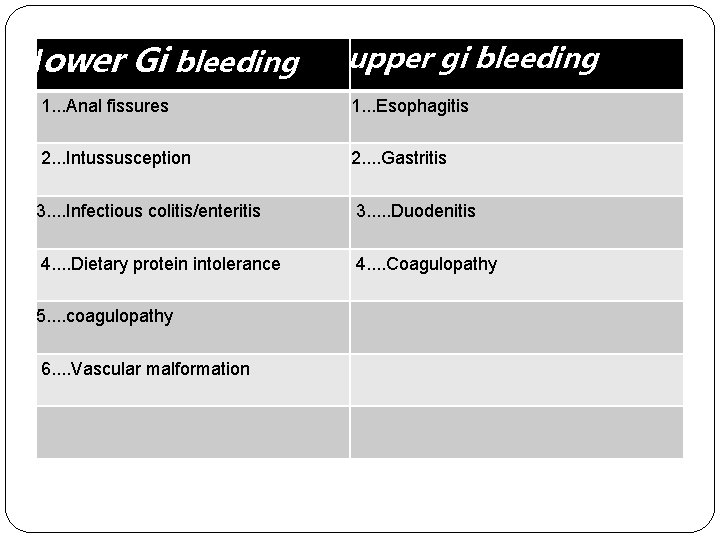
lower Gi bleeding upper gi bleeding 1. . . Anal fissures 1. . . Esophagitis 2. . . Intussusception 2. . Gastritis 3. . Infectious colitis/enteritis 3. . . Duodenitis 4. . Dietary protein intolerance 4. . Coagulopathy 5. . coagulopathy 6. . Vascular malformation
1. esophagitis 1 - Esophagitis (Peptic esophagitis) is the most common cause of bleeding in children aged 1 month to 1 year. This condition is caused by gastroesophageal reflux or esinophilic esophagitis , and is present in infants with regurgitation, dysphasia, odynophagia and failure to thrive. upper abdominal discomfort , crying , and vomiting following ingestion. respiratory distress and stridor can result from airway obstruction and glottic edema.
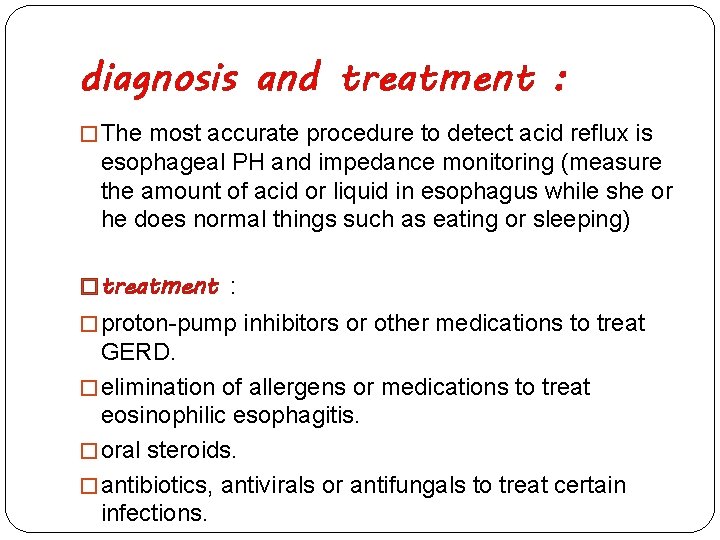
diagnosis and treatment : � The most accurate procedure to detect acid reflux is esophageal PH and impedance monitoring (measure the amount of acid or liquid in esophagus while she or he does normal things such as eating or sleeping) � treatment : � proton-pump inhibitors or other medications to treat GERD. � elimination of allergens or medications to treat eosinophilic esophagitis. � oral steroids. � antibiotics, antivirals or antifungals to treat certain infections.
2. gastritis �can be distinguished as primary or secondary in etiology: � 1. primary correlated withcauses: Helicobacter pylori infection and is the most common cause of gastritis in children. symptom : . an ache or burning pain in the abdomen. nausea. loss of appetite. unintentional weight loss
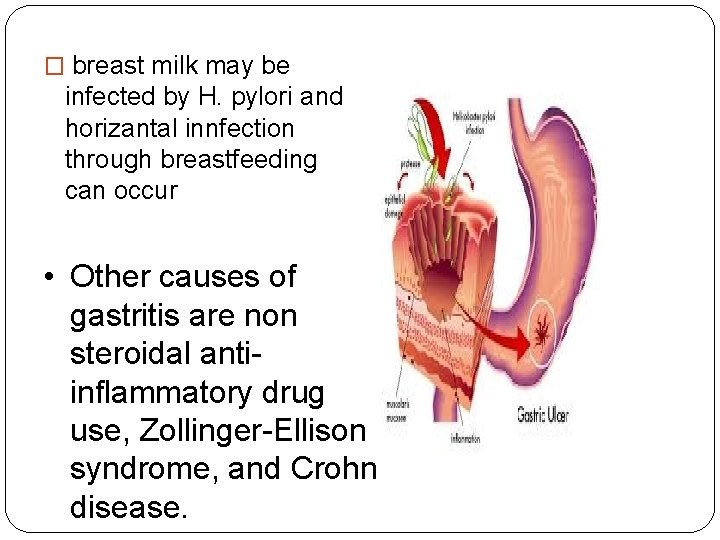
� breast milk may be infected by H. pylori and horizantal innfection through breastfeeding can occur • Other causes of gastritis are non steroidal antiinflammatory drug use, Zollinger-Ellison syndrome, and Crohn disease.
treatment : �Your child's symptoms may go away without treatment. Treatment will depend on what is causing your child's gastritis. Symptoms caused by a toxic object such as a button battery need immediate treatment. Medications may be given to help treat a bacterial infection or decrease stomach acid. � 1. Taking antacids and other drugs (such as proton pump inhibitors or H-2 blockers) to reduce stomach acid. � 2. Avoiding hot and spicy foods
lower Gi bleeding � 1. anal fissure : �its common cause of rectal bleeding in patients younger than one year and also in children and adults and present with painfull defecation and constipation �produce bright red blood that streaks the stool or causes spots of blood in the diaper that is caused by a tear at the mucocutaneous line. Anal fissures can be diagnosed with an anal examination
treatment : �Have your child sit in a few centimetres of warm water (sitz bath) 3 times a day and after bowel movements �Avoid constipation: �Include fruits, vegetables, beans, and whole grains in your child's diet each day. These foods are high in fibre. �Have your child support his or her feet with a small step stool when sitting on the toilet. This helps flex the hips. It places the pelvis in a squatting position. �and use laxative
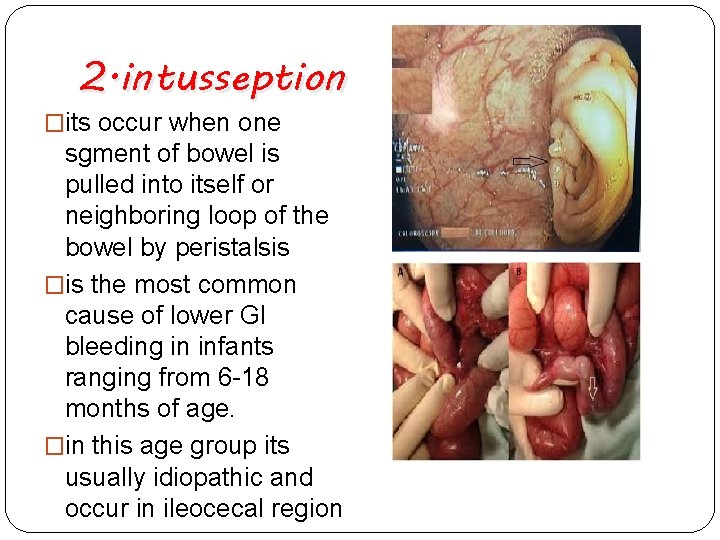
2. intusseption �its occur when one sgment of bowel is pulled into itself or neighboring loop of the bowel by peristalsis �is the most common cause of lower GI bleeding in infants ranging from 6 -18 months of age. �in this age group its usually idiopathic and occur in ileocecal region
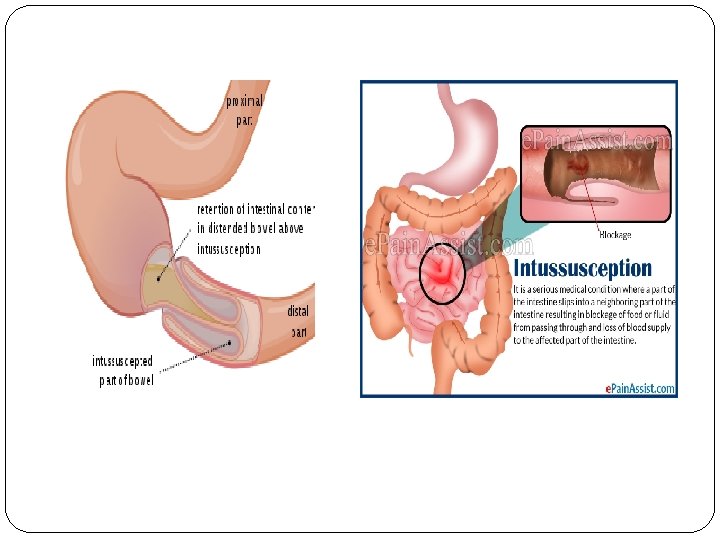
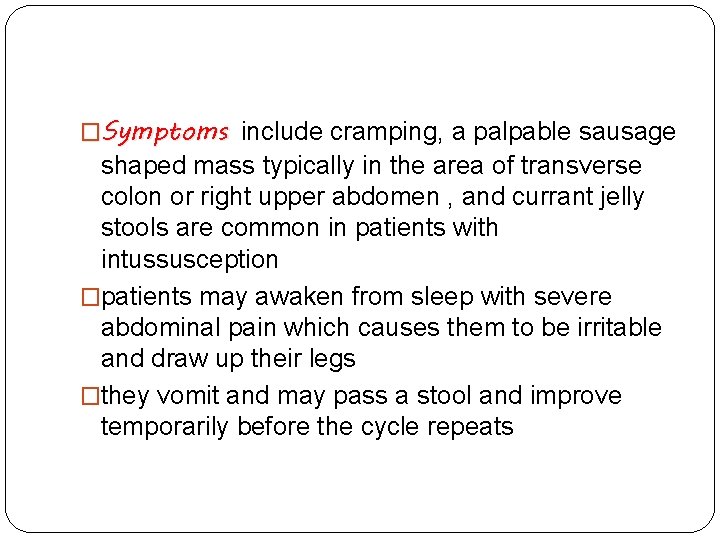
�Symptoms include cramping, a palpable sausage shaped mass typically in the area of transverse colon or right upper abdomen , and currant jelly stools are common in patients with intussusception �patients may awaken from sleep with severe abdominal pain which causes them to be irritable and draw up their legs �they vomit and may pass a stool and improve temporarily before the cycle repeats
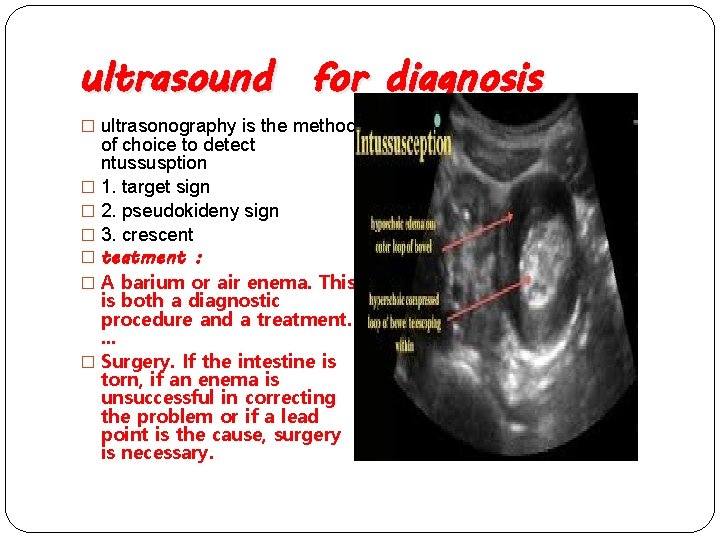
ultrasound for diagnosis � ultrasonography is the method of choice to detect ntussusption � 1. target sign � 2. pseudokideny sign � 3. crescent � teatment : � A barium or air enema. This is both a diagnostic procedure and a treatment. . � Surgery. If the intestine is torn, if an enema is unsuccessful in correcting the problem or if a lead point is the cause, surgery is necessary.
3. gangrenous �is the second most common cause of lower GI bleeding of this age group. Causes include malrotation with volvulus, omphalomesenteric remnant with volvulus, internal hernia with strangulation, segmental small-bowel volvulus, and on rarely, sigmoid volvulus.
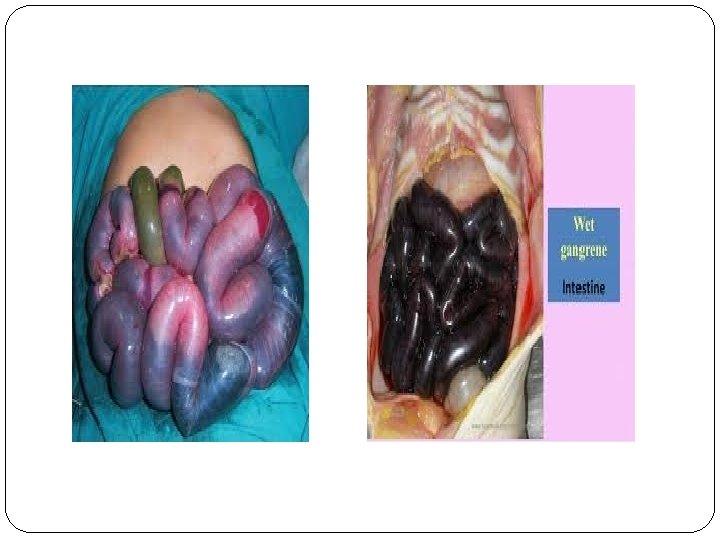
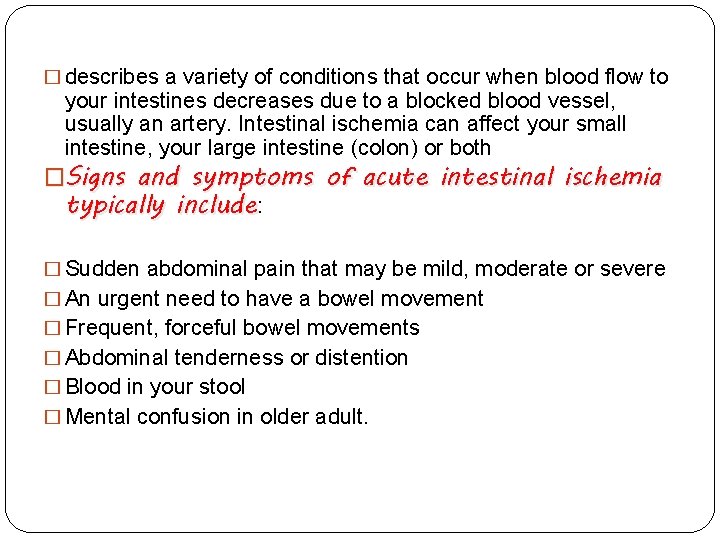
� describes a variety of conditions that occur when blood flow to your intestines decreases due to a blocked blood vessel, usually an artery. Intestinal ischemia can affect your small intestine, your large intestine (colon) or both �Signs and symptoms of acute intestinal ischemia typically include: � Sudden abdominal pain that may be mild, moderate or severe � An urgent need to have a bowel movement � Frequent, forceful bowel movements � Abdominal tenderness or distention � Blood in your stool � Mental confusion in older adult.
� 4 - Milk protein allergy causes a colitis that may be correlated with occult or gross lower GI bleeding. It is caused by an adverse immune reaction to cow’s milk and have additional symptoms that can include diarrhea (loose stool ) , weight loss, vomiting, and irritability. �it can occur in infant who are formula fed , or less commonly in brestfed infant because of cow milk in mother diet
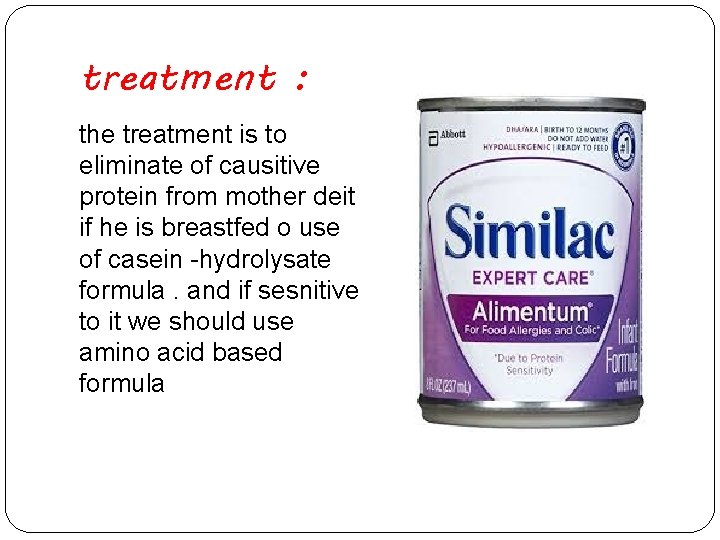
treatment : the treatment is to eliminate of causitive protein from mother deit if he is breastfed o use of casein -hydrolysate formula. and if sesnitive to it we should use amino acid based formula
5. gastrointestinal duplication cyst �Enteric duplication cysts, sometimes simply called duplication cysts, are rare congenital malformations of the gastrointestinal tract. [1] They most frequently occur in the small intestine, particularly the ileum, but can occur anywhere along the gastrointestinal tract. [1] They may be cystic or tubular in conformation. [2] �The condition of having duplication cysts has been called intestinal duplication. [3]
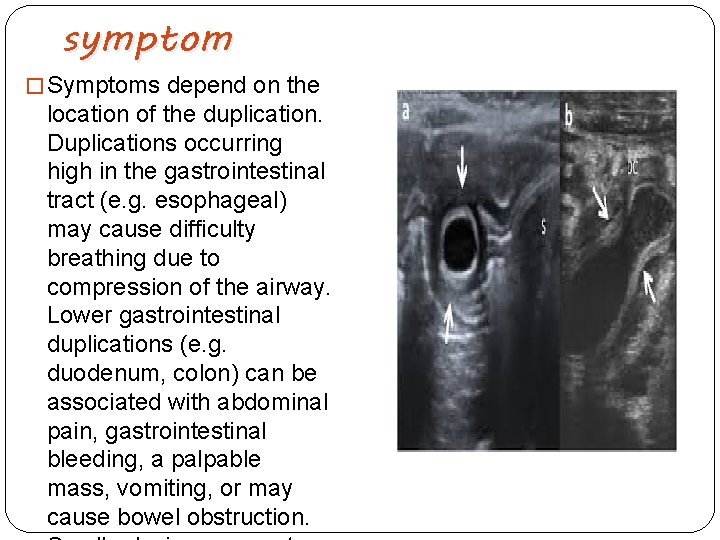
symptom � Symptoms depend on the location of the duplication. Duplications occurring high in the gastrointestinal tract (e. g. esophageal) may cause difficulty breathing due to compression of the airway. Lower gastrointestinal duplications (e. g. duodenum, colon) can be associated with abdominal pain, gastrointestinal bleeding, a palpable mass, vomiting, or may cause bowel obstruction.
infantile and very early onset IBD �develop definitions for pediatric inflammatory bowel disease (IBD). One important working group classified one subgroup of pediatric IBD patients to those presenting with symptoms at an age less than 10 years
clinical senario : A 7 -week-old baby presented to a district general hospital with a history of pallor, lethargy, vomiting and high pitched cry. She had vomited three times at home. It was reported that the last vomitus had a greenish tinge to it. In hospital, she had a non-bilious vomit. There was no history of fever, constipation or diarrhoea. Her birth history and medical history were unremarkable. She was noted to be pale, lethargic and quiet on examination. Her vital signs were unremarkable. She had a soft scaphoid abdomen on examination. No masses were palpable. Investigations for sepsis were done and antibiotics started. Results of all the investigations were normal apart from mildly raised blood glucose and neutrophilia. Later on she passed a small amount of blood per rectum. Examination revealed
� 1. esophagitis � 2. gatritis � 3. anal fissure � 4. intusseption � 5. gangenous � 6. milk protein allergy
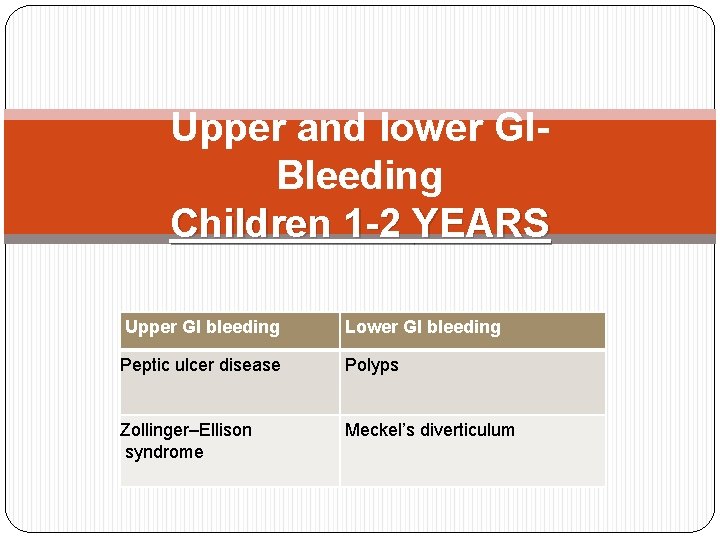
Upper and lower GIBleeding Children 1 -2 YEARS Upper GI bleeding Lower GI bleeding Peptic ulcer disease Polyps Zollinger–Ellison syndrome Meckel’s diverticulum
Peptic Ulcer v Peptic ulcers are sores that develop in the lining of the stomach, lower esophagus, or small intestine. They’re usually formed as a result of inflammation caused by the bacteria H. pylori, as well as from erosion from stomach acids. v The pathogenesis is multifactorial, but the final common pathway for the development of ulcers is the action of acid and pepsin-laden contents of the stomach on the gastric and duodenal mucosa and the inability of mucosal defense mechanisms to allay those effects. v According to the etiology, Ulcers can be classified to primary which are chronic and more often duodenal, or secondary, which are usually more acute in onset and are more often gastric. v Primary ulcers are most often associated with Helicobacter pylori infection , Secondary ulcers caused in respones to stress as sepsis and intracranial lesion and called cushing ulcer, or severe burn response and called curling ulcer, and most ofently can be caused by NSAID’S use. v Pathogenesis is directed to the imbalance between acid secretion and mucosal defense.
Clinical Manifestation v The presentation of peptic ulcer disease vary with the age of the patient. v Hematemesis and/or melena are presented in the most of cases. v Infants and younger children usually present with feeding difficulty, vomiting, crying episodes, hematemesis, or melena. v The classic symptom of peptic ulceration, epigastric pain alleviated by the ingestion of food, is present only in a minority of children. v Many pediatric patients present with poorly localized abdominal pain, which may be periumbilical. v Occasionally, bright red blood per rectum may be seen if the rate of bleeding is brisk and the intestinal transit time is short
Diagnosis v C-urea breath tests and stool antigen tests are reliable noninvasive methods of detecting H. pylori infection in patients who do not require endoscopic evaluation. v for symptomatic children with suspected H. pylori infection, an initial upper endoscopy is recommended to evaluate and confirm H. pylori disease , Esophagogastroduodenoscopy is the method of choice to establish the diagnosis of peptic ulcer disease. v It allows the direct visualization of esophagus, stomach, and duodenum, identifying the specific lesions. v Biopsy specimens must be obtained from the esophagus, stomach, and duodenum for histologic assessment as well as to screen for the presence of H. pylori infection.

Peptic ulcer
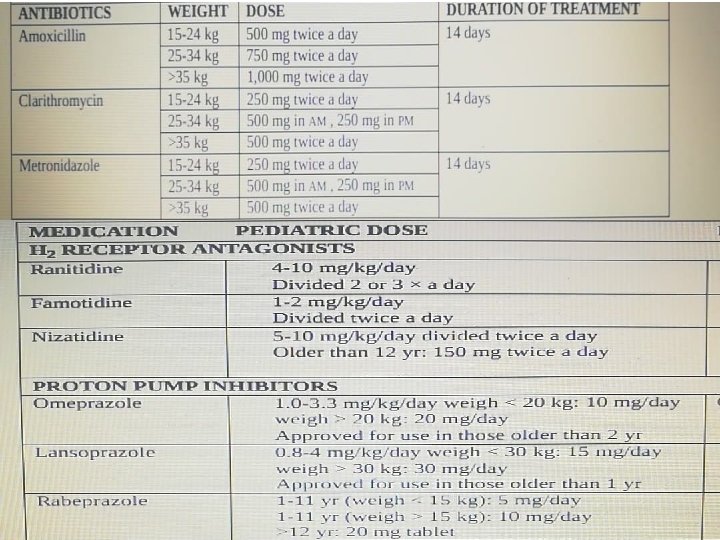
Managment v Ulcer therapy has two goals: ulcer healing and elimination of the primary cause. v Patients with suspected peptic ulcer hemorrhage should receive high-dose intravenous (IV) PPI therapy, which lowers the risk of rebleeding. v Once the patient is hemodynamically stable, endoscopy within 24 hr is indicated to identify the source of bleeding and to treat a potential bleeding site. v to achieve hemostasis include mechanical devices (clipping), injection therapy (diluted epinephrine 1: 10, 000), and thermal therapy (heater probe). v The first-line drugs for the treatment of gastritis and peptic ulcer disease in children are PPIs and H 2 receptor antagonists. v Antibiotics in combination with a PPI must be used for the treatment of H. pylori -associated ulcers.
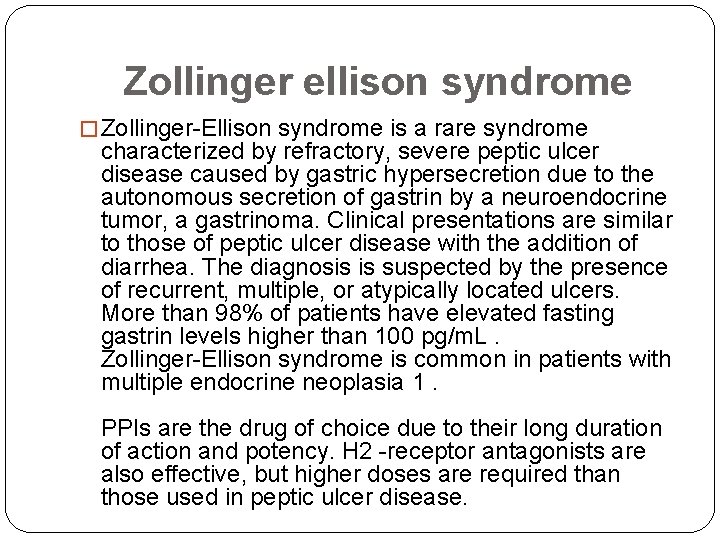
Zollinger ellison syndrome � Zollinger-Ellison syndrome is a rare syndrome characterized by refractory, severe peptic ulcer disease caused by gastric hypersecretion due to the autonomous secretion of gastrin by a neuroendocrine tumor, a gastrinoma. Clinical presentations are similar to those of peptic ulcer disease with the addition of diarrhea. The diagnosis is suspected by the presence of recurrent, multiple, or atypically located ulcers. More than 98% of patients have elevated fasting gastrin levels higher than 100 pg/m. L. Zollinger-Ellison syndrome is common in patients with multiple endocrine neoplasia 1. PPIs are the drug of choice due to their long duration of action and potency. H 2 -receptor antagonists are also effective, but higher doses are required than those used in peptic ulcer disease.
Lower GI bleeding

Polyps � abnormal tissue growths that most often look like small, flat bumps , most common in the colon. � In children and adolescents, approximately 85 percent or more of polyps are juvenile (hamartomas), 10 percent or less are adenomas � Juvenile polyps, usually present with painless rectal bleeding, with or without mucus , a few may have lower abdominal pain from traction on the polyp. � Juvenile polyps tend to be pedunculated rather than sessile, and may autoamputate, which results in significant bleeding � Approximately 60 to 80 percent of these polyps are in the rectosigmoid, and some of these can be palpated on rectal examination.
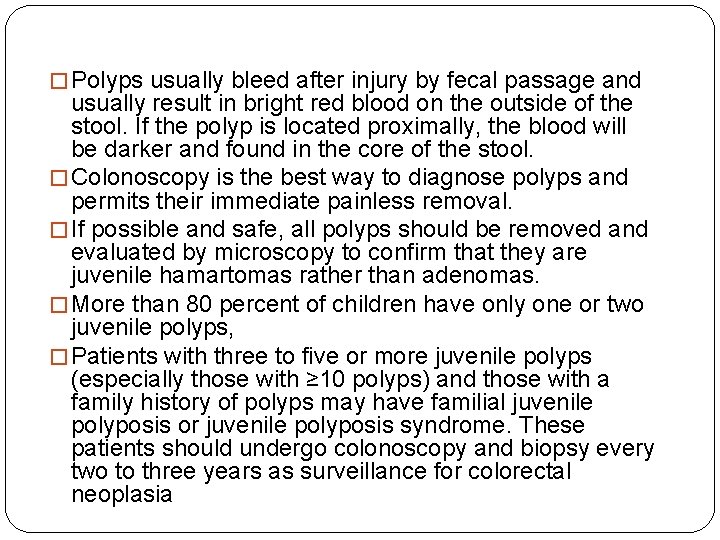
� Polyps usually bleed after injury by fecal passage and usually result in bright red blood on the outside of the stool. If the polyp is located proximally, the blood will be darker and found in the core of the stool. � Colonoscopy is the best way to diagnose polyps and permits their immediate painless removal. � If possible and safe, all polyps should be removed and evaluated by microscopy to confirm that they are juvenile hamartomas rather than adenomas. � More than 80 percent of children have only one or two juvenile polyps, � Patients with three to five or more juvenile polyps (especially those with ≥ 10 polyps) and those with a family history of polyps may have familial juvenile polyposis or juvenile polyposis syndrome. These patients should undergo colonoscopy and biopsy every two to three years as surveillance for colorectal neoplasia
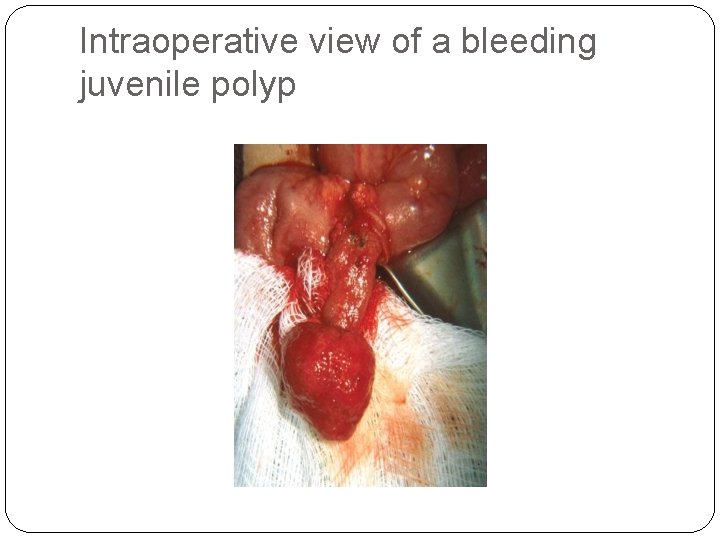
Intraoperative view of a bleeding juvenile polyp
Meckel diverticulum � Abnormal sac or pouch develops at a weak point in the intestines (usually in the ileum) , the only true congenital diverticulum (involves all layers of the bowel wall) � the most common congenital small-intestine anomaly that results from incomplete obliteration of the fetal vitelline (omphalomesenteric) duct that connects the midgut lumen and yolk sac cavity early in fetal life. � Most (~85%) diverticula contain heterotopic gastric tissue and less commonly contain pancreatic tissue. � The etiology of GI bleeding due to Meckel diverticulum is ileal ulceration caused by acid secretion from the ectopic gastric mucosa. Erosion into small arterioles leads to painless, brisk rectal bleeding
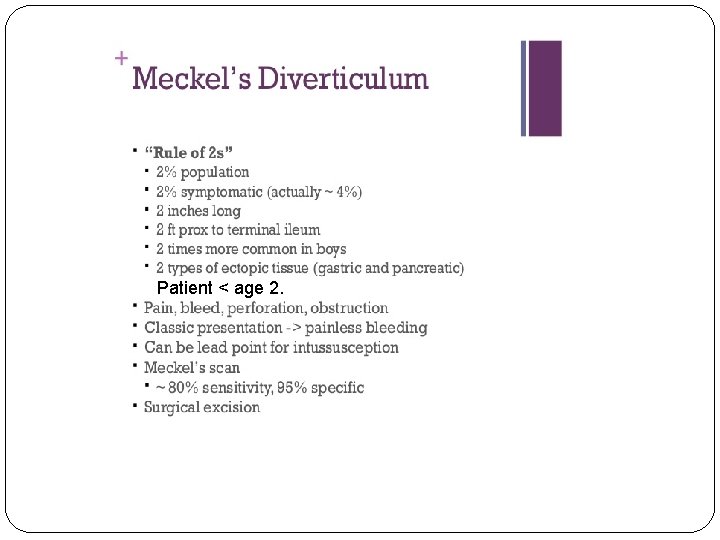
Patient < age 2.
Clinical presentation �The diverticulum is an asymptomatic, incidental finding in most patients. �Only 2% of diverticula become symptomatic, with painless hematochezia being the most common presentation. Ectopic gastric tissue secretes hydrochloric acid, causing mucosal ulceration of surrounding small bowel. The bleeding is often substantial and causes severe anemia or hemorrhagic shock. �the presentation is mainly a painless lower gastrointestinal bleeding. � present with dark red or maroon stools.
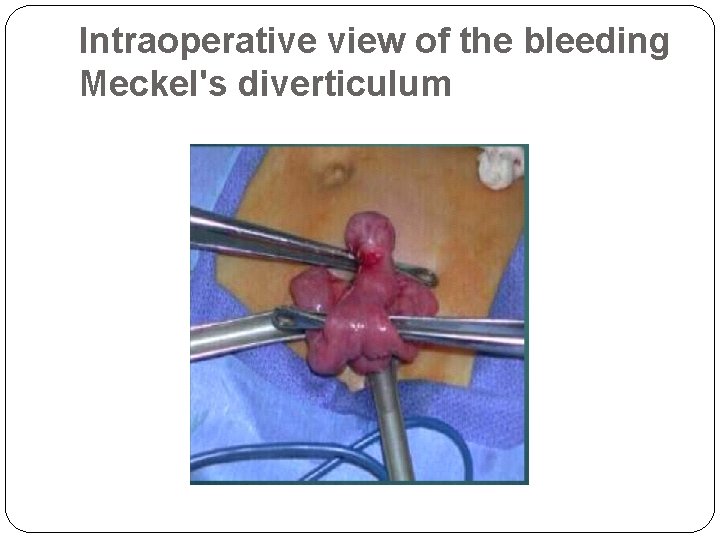
Intraoperative view of the bleeding Meckel's diverticulum
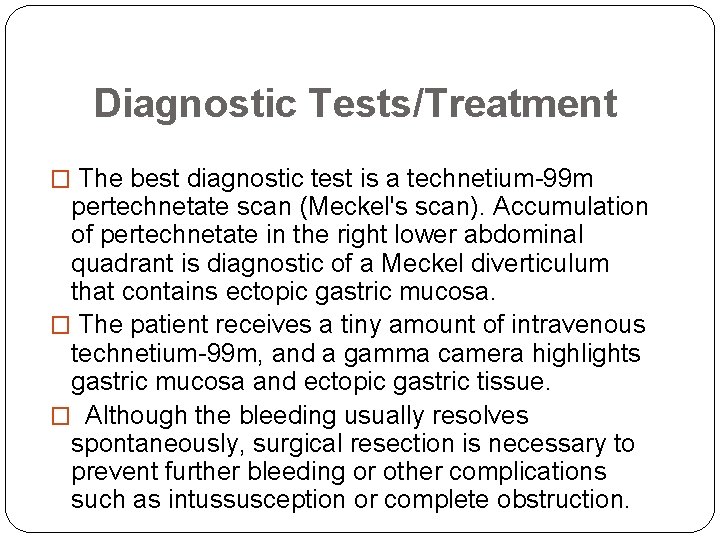
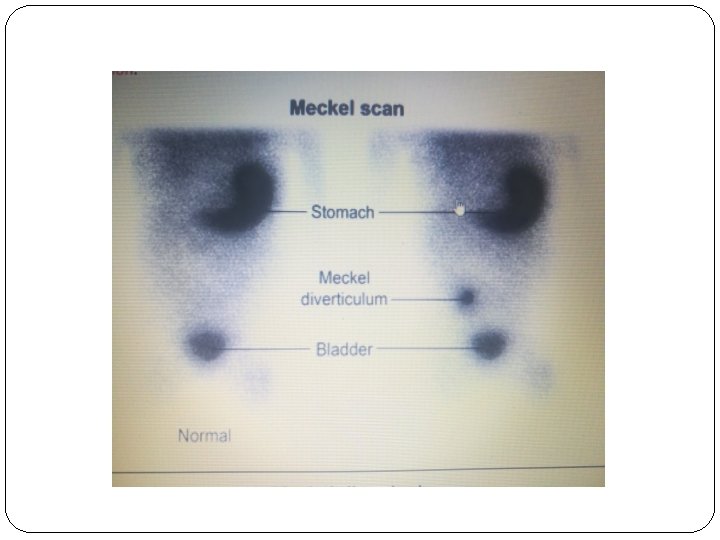
Diagnostic Tests/Treatment � The best diagnostic test is a technetium-99 m pertechnetate scan (Meckel's scan). Accumulation of pertechnetate in the right lower abdominal quadrant is diagnostic of a Meckel diverticulum that contains ectopic gastric mucosa. � The patient receives a tiny amount of intravenous technetium-99 m, and a gamma camera highlights gastric mucosa and ectopic gastric tissue. � Although the bleeding usually resolves spontaneously, surgical resection is necessary to prevent further bleeding or other complications such as intussusception or complete obstruction.
Common causes of GI bleeding in children (2 years and above)
Esophageal varices �Esophageal varices are abnormally enlarged veins in the lower part of this tube. �Esophageal varices are often a complication of serious liver diseases(portal vein thrombosis, biliary atrasia) �. Esophageal varices can develop when normal blood flow to the liver through the portal vein is blocked.
�Symptoms of esophageal varices are: -Vomiting blood -Black, tarry or bloody stools -Decreased urination from unusually low blood pressure -Lightheadedness
�INVESTIGATION: 1 -Upper endoscopy is the preferred diagnostic test for esophageal varices, as it provides definitive diagnosis. 2 -Also we can use US, Barium contrast studies, CT !! �The management of acute variceal bleeding must include : 1 -hemodynamic stability through blood transfusion. 2 -vasoactive drugs. 3 - short-term antibiotic use, and 4 - endoscopy to perform or sclerotherapy, as
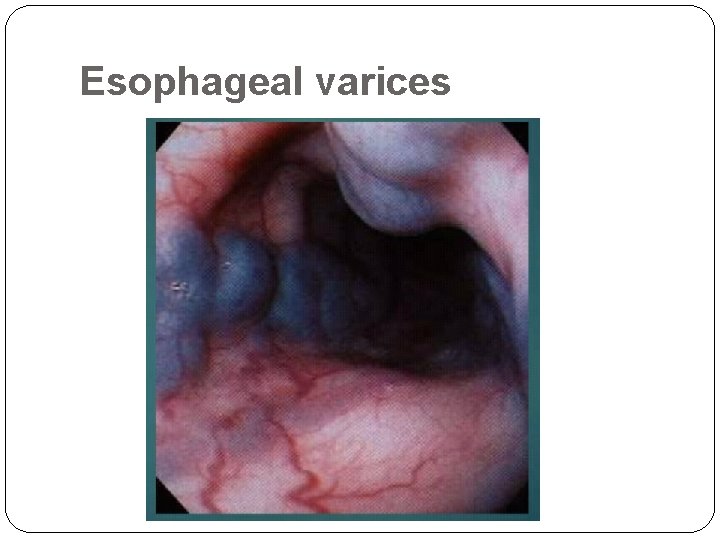
Esophageal varices
Inflammatory Bowel Disease (IBD) � Inflammatory bowel disease (IBD) is an inflammation or swelling in the gastrointestinal tract. � IBD: 1 - ulcerative colitis 2 - Crohn's disease � Causes of IBD unknown !! � Symptoms : Ulcerative colitis and Crohn’s disease have many similar symptoms, including: -Diarrhea -Rectal bleeding -Abdominal (belly) pain -Decreased appetite -Weight loss -Fever
�Diagnosing these diseases requires several tests: 1 - Laboratory 2 -barium and radiological studies 3 -Endoscopy • Managment: 1 -Dietary changes 2 -Medications(5 -ASAs, , Immunomodulators, , Biologics) 3 -Surgery
Infectious Diarrhea �is suspected when lower GI bleeding occurs in association with profuse diarrhea. �Common bacterium cause of infectious diarrhea are E. coli & Shigella. �Diagnosis is clinically + stool analysis. �Initial management should always focus on rehydration. �Antibiotics
Vascular lesions �consist of a variety of malformations that include hemangiomas , arteriovenous malformations, and vasculitis. �Lesions located in the colon can be diagnosed with colonoscopy. However, bleeding can cause this to be challenging making localizing the bleeding practically impossible.
� Treatment of GI bleeding : � should begin with an initial assessment, rapid stabilization, and a logical sequence of diagnostic tests. � When a treatable cause is identified, specific therapy should be started. � In many cases, the amount of blood is small, and no resuscitation is required. � For children with large-volume bleeds, the ABCs of resuscitation (airway, breathing, circulation) should be addressed first. � Oxygen should be administered and the airway protected with an endotracheal tube if massive hematemesis is present � cardiopulmonary and urine output monitoring.
INITIAL MANAGEMENT The initial approach to all patients with significant GI bleed is : - to establish adequate oxygen delivery. - to place intravenous line. - to initiate fluid and blood resuscitation - to correct any underlying coagulopathies.
Therapy Supportive care : begin promptly - Bowel Rest and NG decompression (esp. in NEC) - IV fluids - Blood products (FFPs, RCC)
Specific care : - H 2 receptor antagonists (cimetidine, ranitidine, etc. ) - Proton pump inhibitors (omeprazole, lansoprazole) - Vasoconstrictors (somatostatine analogue[ Octreotide ], vasopressin, Beta Blockers) -Inj Vitamin K (HDN) - Stool Softeners (Anal Fissure) - Antibiotics (for enteritis, Cl. Difficile ass. Colitis) - H. pylori Eradication ( triple therapy)
Endoscopic treatments include the application of clips, coagulation, banding, injection, sclerotherapy, and the use of tissue adhesives angiography is indicated when endoscopic therapy is unsuccessful.
Surgical options If all medical measures fail - Laprotomy - Laproscopy - Vagotomy - Pyloroplasty - Fissurotomy, fistulectomy - Diverticulectomy
- Slides: 81