Pediatric Epilepsy An Overview and Update on Treatment













- Slides: 68
Pediatric Epilepsy: An Overview and Update on Treatment Options Mitzi Payne, MD Pediatric Neurology Marshall University 1
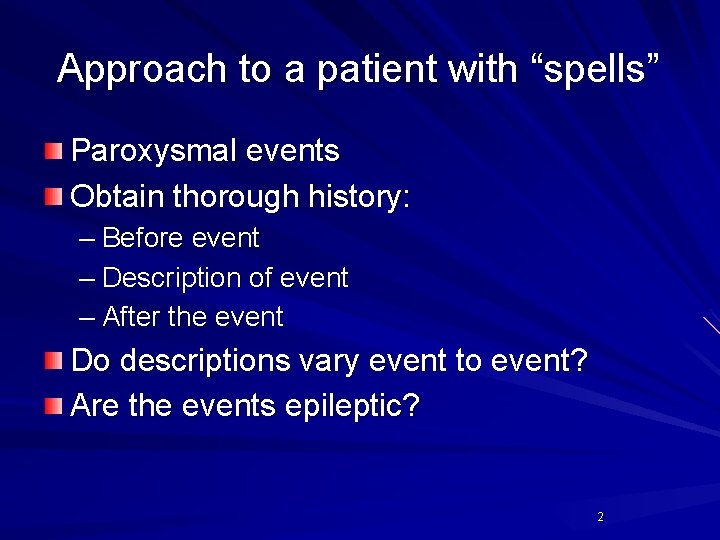
Approach to a patient with “spells” Paroxysmal events Obtain thorough history: – Before event – Description of event – After the event Do descriptions vary event to event? Are the events epileptic? 2
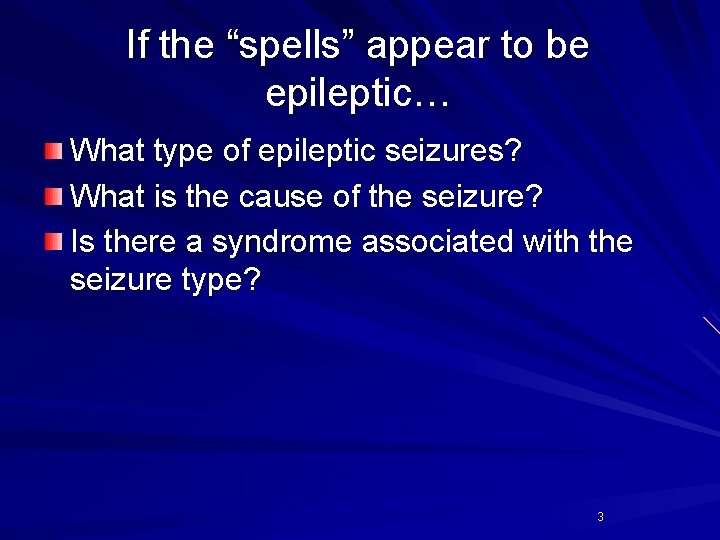
If the “spells” appear to be epileptic… What type of epileptic seizures? What is the cause of the seizure? Is there a syndrome associated with the seizure type? 3
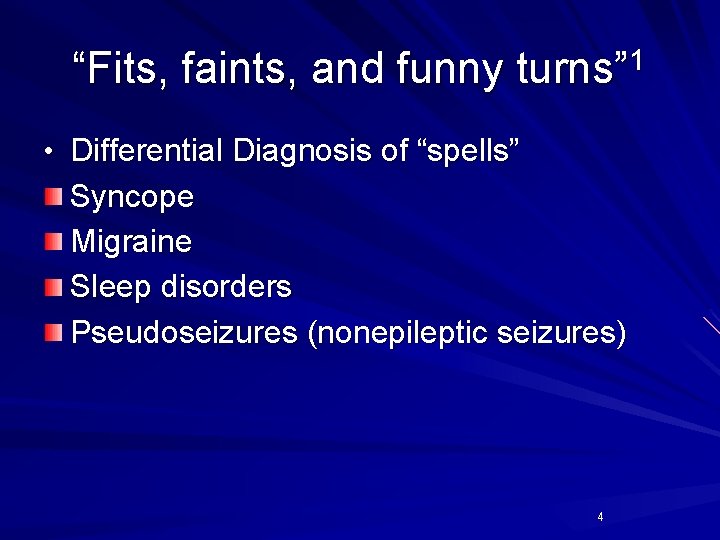
“Fits, faints, and funny turns” 1 • Differential Diagnosis of “spells” Syncope Migraine Sleep disorders Pseudoseizures (nonepileptic seizures) 4
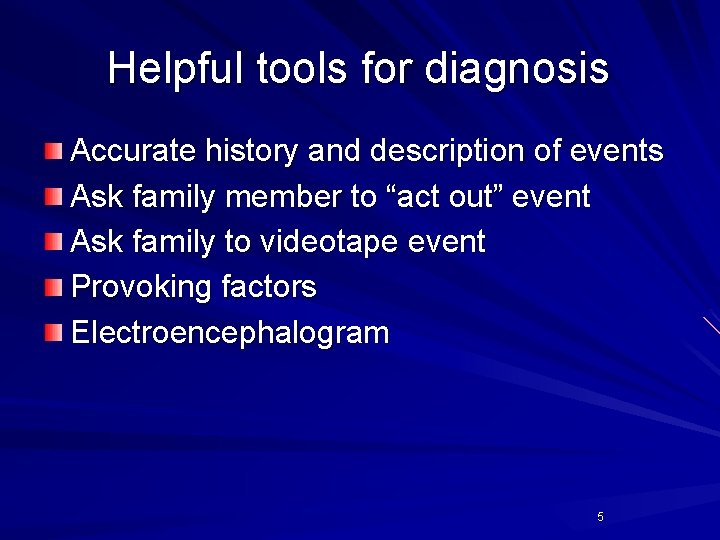
Helpful tools for diagnosis Accurate history and description of events Ask family member to “act out” event Ask family to videotape event Provoking factors Electroencephalogram 5

Some important points Classification(s) – seizure type an ictal event believed to represent a unique pathophysiological mechanism and anatomic substrate – epilepsy syndrome a complex of signs and symptoms that define a unique epilepsy condition Etiological categories of syndromes – idiopathic no underlying structural brain disease, presumed genetic – symptomatic seizures are the result of lesional or metabolic disease of the brain – probably symptomatic (cryptogenic) believed symptomatic but no etiology established 6
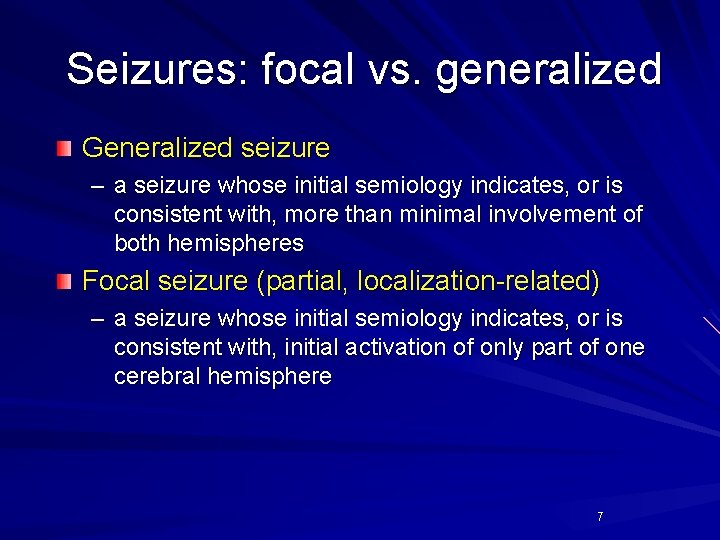
Seizures: focal vs. generalized Generalized seizure – a seizure whose initial semiology indicates, or is consistent with, more than minimal involvement of both hemispheres Focal seizure (partial, localization-related) – a seizure whose initial semiology indicates, or is consistent with, initial activation of only part of one cerebral hemisphere 7
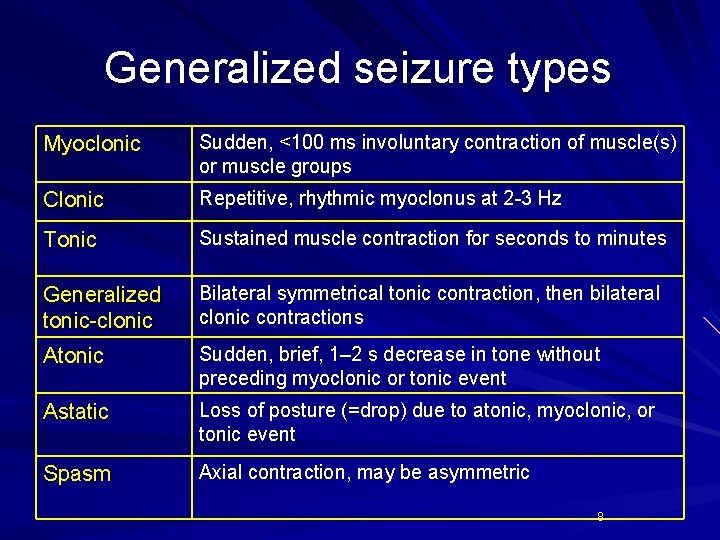
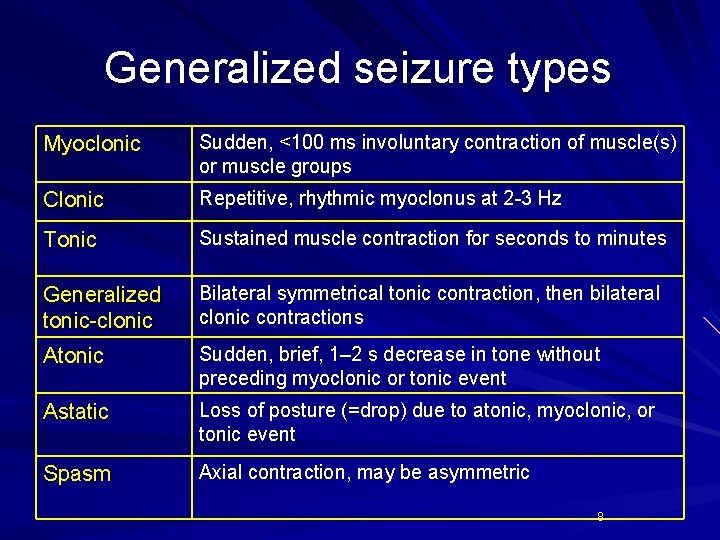
Generalized seizure types Myoclonic Sudden, <100 ms involuntary contraction of muscle(s) or muscle groups Clonic Repetitive, rhythmic myoclonus at 2 -3 Hz Tonic Sustained muscle contraction for seconds to minutes Generalized tonic-clonic Bilateral symmetrical tonic contraction, then bilateral clonic contractions Atonic Sudden, brief, 1– 2 s decrease in tone without preceding myoclonic or tonic event Astatic Loss of posture (=drop) due to atonic, myoclonic, or tonic event Spasm Axial contraction, may be asymmetric 8
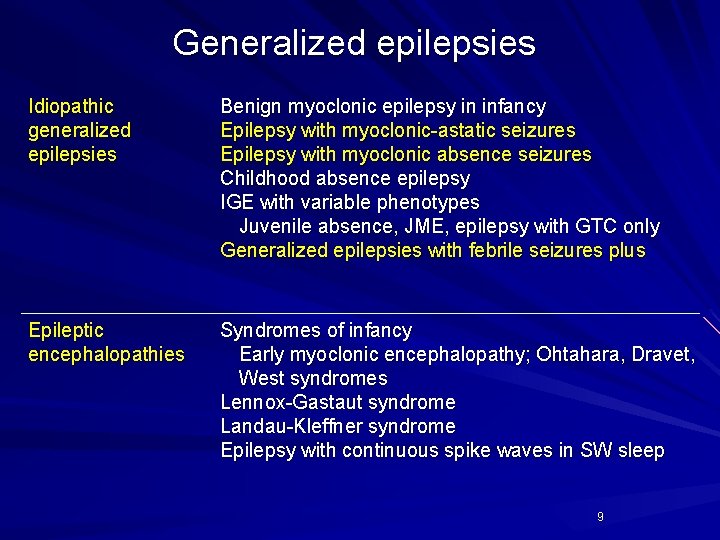
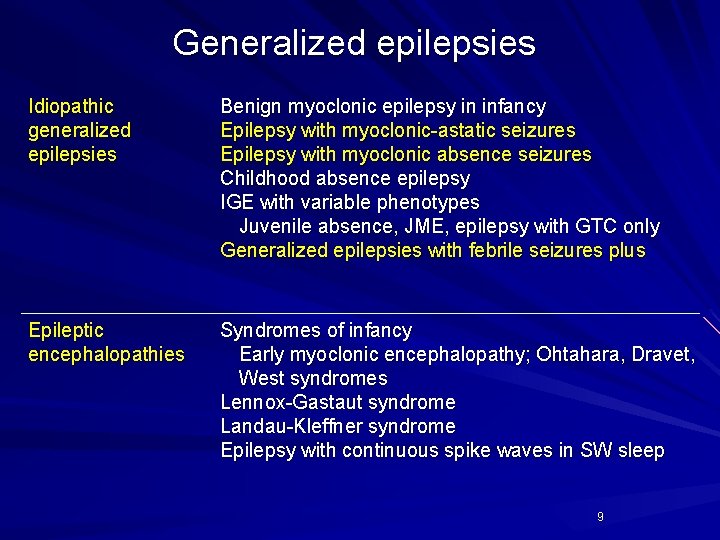
Generalized epilepsies Idiopathic generalized epilepsies Benign myoclonic epilepsy in infancy Epilepsy with myoclonic-astatic seizures Epilepsy with myoclonic absence seizures Childhood absence epilepsy IGE with variable phenotypes Juvenile absence, JME, epilepsy with GTC only Generalized epilepsies with febrile seizures plus Epileptic encephalopathies Syndromes of infancy Early myoclonic encephalopathy; Ohtahara, Dravet, West syndromes Lennox-Gastaut syndrome Landau-Kleffner syndrome Epilepsy with continuous spike waves in SW sleep 9
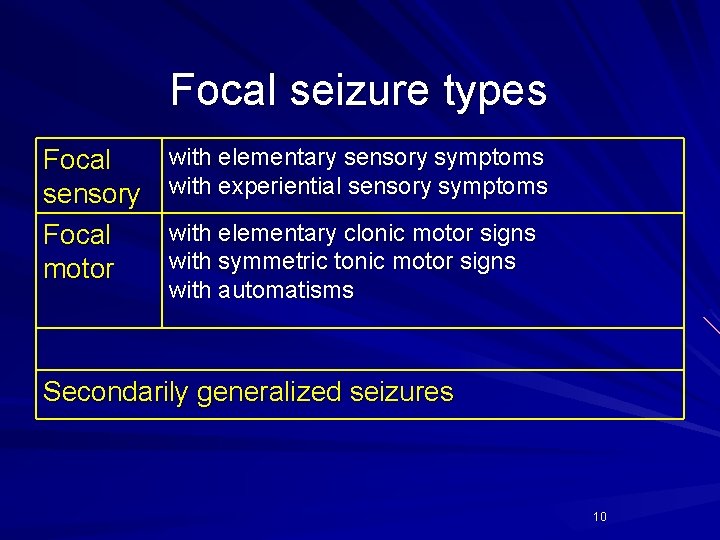
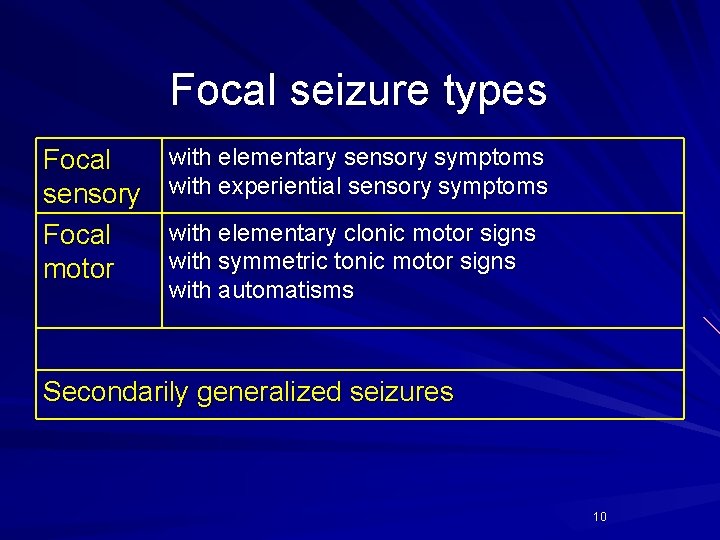
Focal seizure types Focal sensory Focal motor with elementary sensory symptoms with experiential sensory symptoms with elementary clonic motor signs with symmetric tonic motor signs with automatisms Secondarily generalized seizures 10
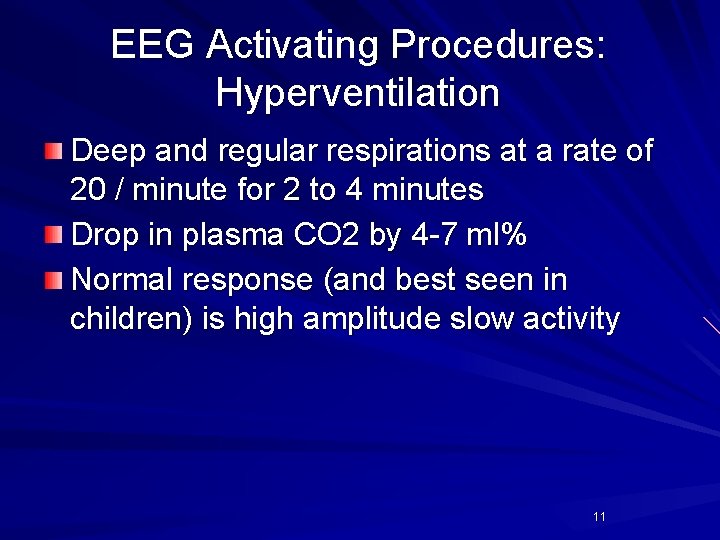
EEG Activating Procedures: Hyperventilation Deep and regular respirations at a rate of 20 / minute for 2 to 4 minutes Drop in plasma CO 2 by 4 -7 ml% Normal response (and best seen in children) is high amplitude slow activity 11
EEG Activating Procedures: Hyperventilation may induce diffuse sharp waves or spike-wave complexes Patients with generalized epilepsies are most likely to have these findings Actual seizures can be induced by hyperventilation – – Absence (petit mal) Temporal lobe seizures 12
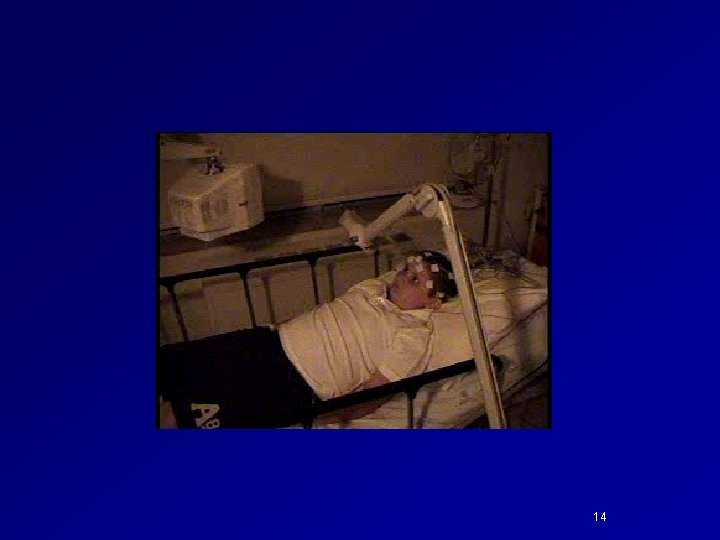
EEG Activating Procedures: Intermittent Photic Stimulation Strobe light flashes (1 -30 Hz) Photic driving Rhythmic activity over the posterior head regions Photomyoclonic response Repetitive muscle spikes over the anterior regions of the head Photoconvulsive (-paroxysmal) response Generalized spike and wave complexes 15 -20 Hz May have jerking or impairment of consciousness Photosensitive epilepsies 13
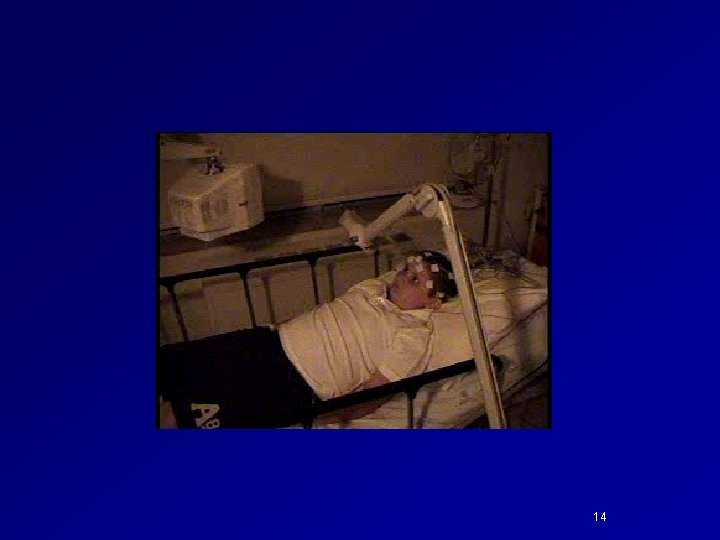
14
EEG Activating Procedures Somatosensory stimulation Electrical stimulation of peripheral nerves Epileptiform discharges in contralateral hemisphere Reenactment of a trigger Visual stimulation of geometric patterns Auditory stimulation Reading Hypoglycemia 15
Common Childhood Epilepsy Syndromes 16
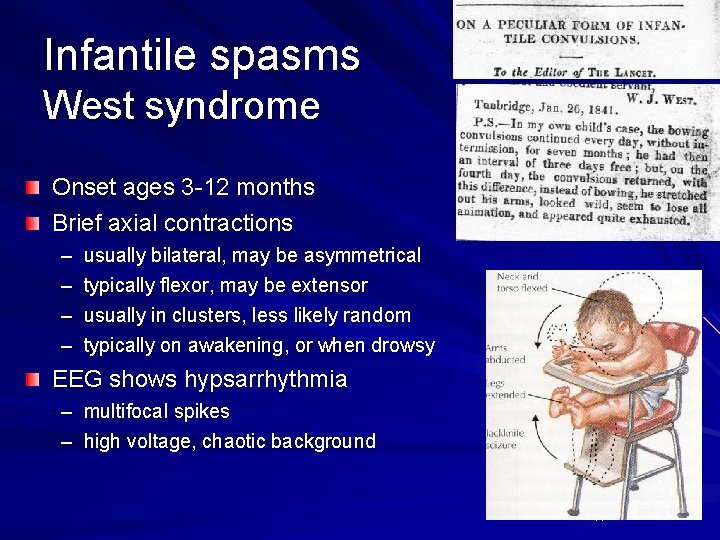
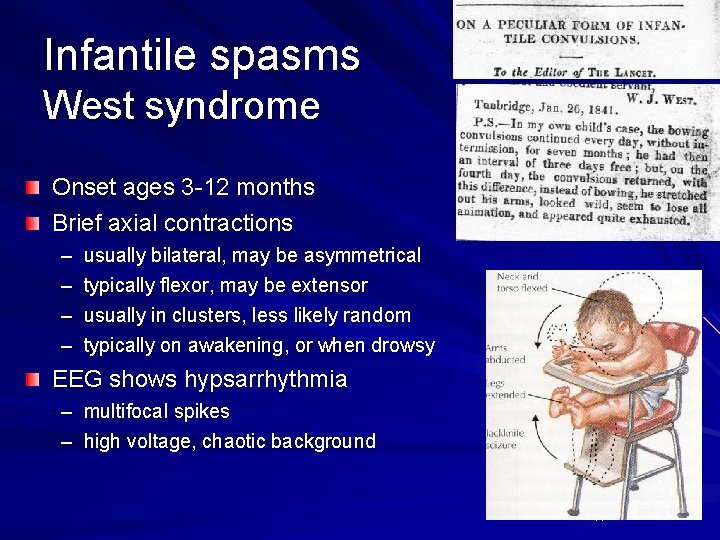
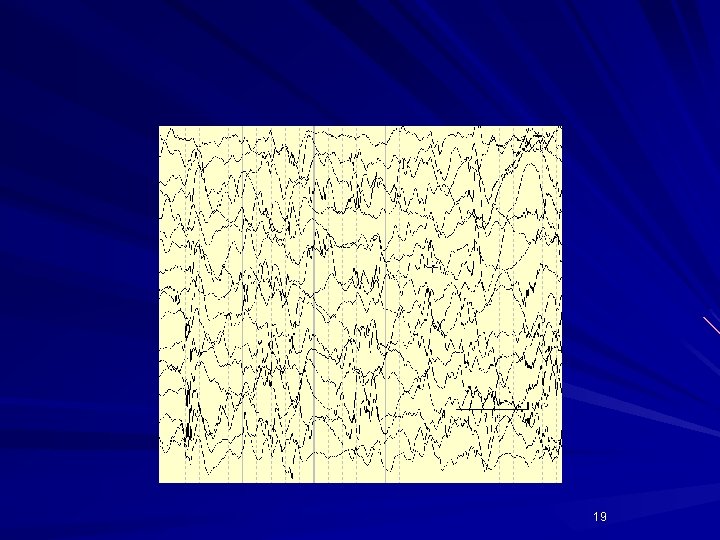
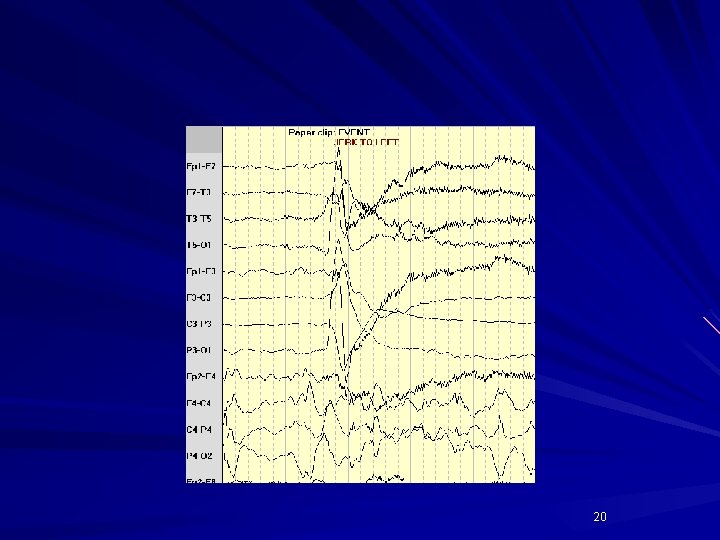
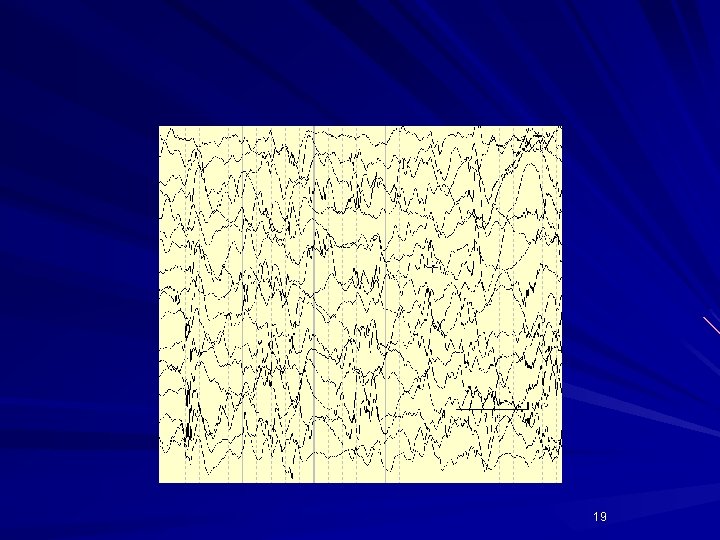
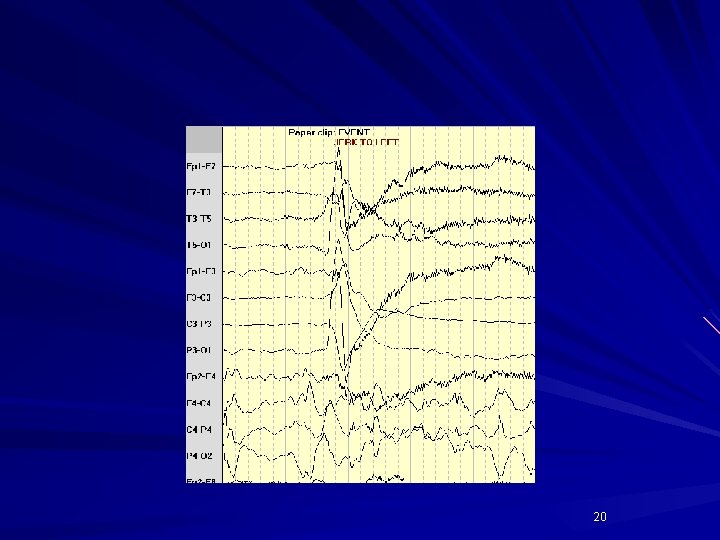
Infantile spasms West syndrome Onset ages 3 -12 months Brief axial contractions – – usually bilateral, may be asymmetrical typically flexor, may be extensor usually in clusters, less likely random typically on awakening, or when drowsy EEG shows hypsarrhythmia – multifocal spikes – high voltage, chaotic background 17

Flexor spasm 18
19
20
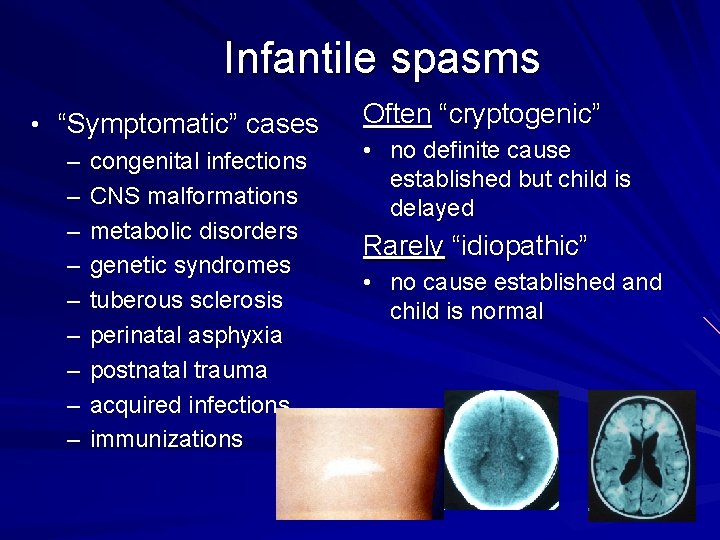
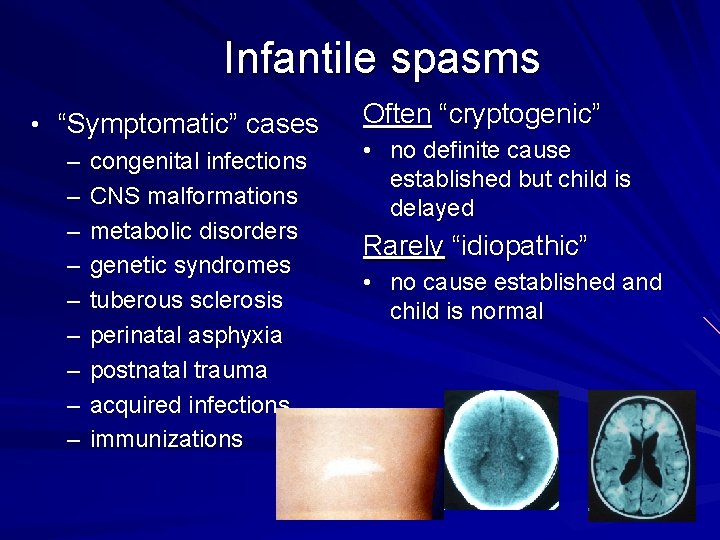
Infantile spasms • “Symptomatic” cases – congenital infections – CNS malformations – metabolic disorders – genetic syndromes – tuberous sclerosis – perinatal asphyxia – postnatal trauma – acquired infections – immunizations Often “cryptogenic” • no definite cause established but child is delayed Rarely “idiopathic” • no cause established and child is normal 21
Infantile spasms Short term treatment to stop spasms, improve EEG – ACTH effective, dose not established oral steroids not proven effective – Vigabatrin, especially in tuberous sclerosis not available in US, potential retinal toxicity Data insufficient to show early treatment or any treatment changes long term outcome 22
West Syndrome Infantile Spasms Hypsarrhythmia on EEG Developmental regression that begins concurrently with the onset of spasms 23
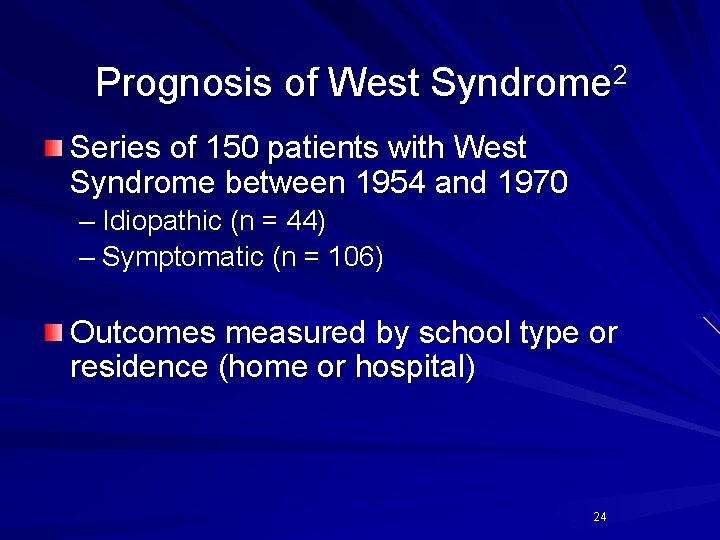
Prognosis of West Syndrome 2 Series of 150 patients with West Syndrome between 1954 and 1970 – Idiopathic (n = 44) – Symptomatic (n = 106) Outcomes measured by school type or residence (home or hospital) 24
Outcome Idiopathic cases: – Normal school 37% – Death 6% – Other seizure types 43% – Neurologic abnormality 31% 25

Outcome Symptomatic cases: – Normal school - none – Death 37% – Other seizure types 59% – Neurological abnormality 65% – Large number progress to develop Lennox Gastaut Syndrome 26
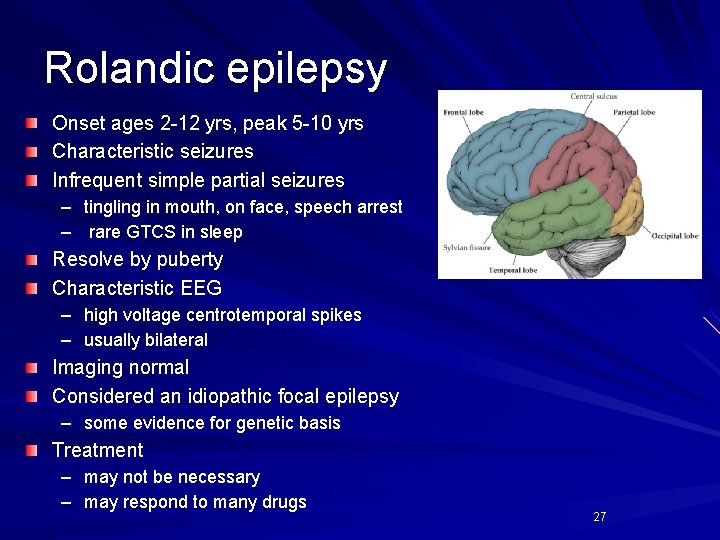
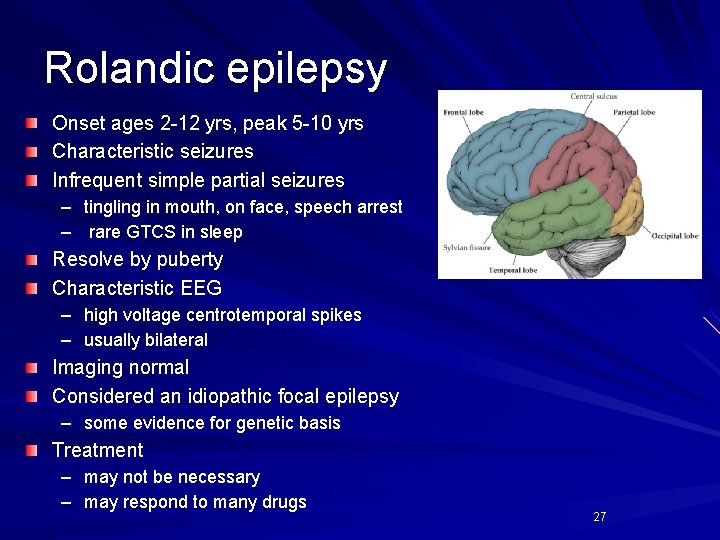
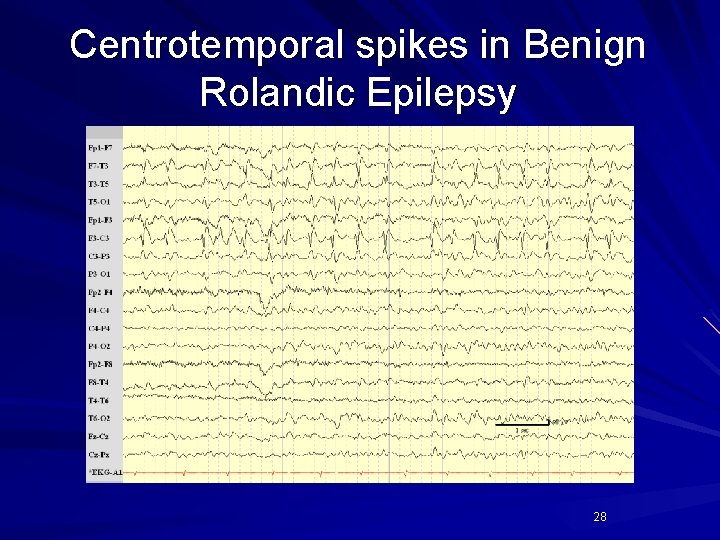
Rolandic epilepsy Onset ages 2 -12 yrs, peak 5 -10 yrs Characteristic seizures Infrequent simple partial seizures – tingling in mouth, on face, speech arrest – rare GTCS in sleep Resolve by puberty Characteristic EEG – high voltage centrotemporal spikes – usually bilateral Imaging normal Considered an idiopathic focal epilepsy – some evidence for genetic basis Treatment – may not be necessary – may respond to many drugs 27
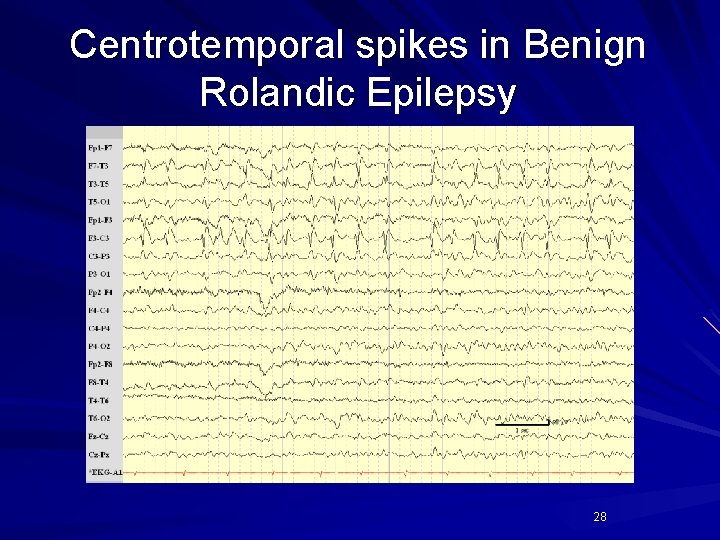
Centrotemporal spikes in Benign Rolandic Epilepsy 28
Presentation of “staring spells” • Complex partial seizures • Absence seizures • Behavior staring
Complex Partial Seizures • Commonly temporal lobe focus • Begins in one area, then spreads enough to impair consciousness, but not to evoke a generalized tonic-clonic seizure • Staring is often part of the initial spread • Also can see automatisms…
Automatisms • • Coordinated involuntary movements Consciousness impaired Patient does not recall activity Simple – Lip smacking, chewing, uttering sounds, picking, tapping, walking straight or in circles • Complex (behavior involved) – Undressing, chewing inedible objects, wandering, aggression

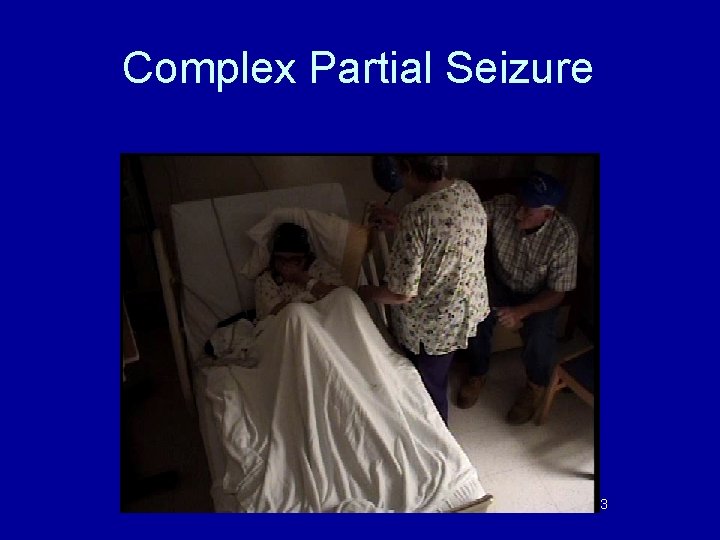
Complex Partial Seizure
Complex Partial Seizure 33

Complex Partial Seizure 34

Treatment of complex partial seizures • Use medications for focal onset seizures – Levetiracetam (Keppra) – Oxcarbamazepine (Trileptal) – Carbamazepine (Tegretol/ Carbatrol) – Lamotrigine (Lamictal) – Topiramate (Topamax) – Zonisimide (Zonegran) – Phenobarbital – Valproic Acid (Depakote) – Lacosamide (Vimpat)
Absence epilepsy
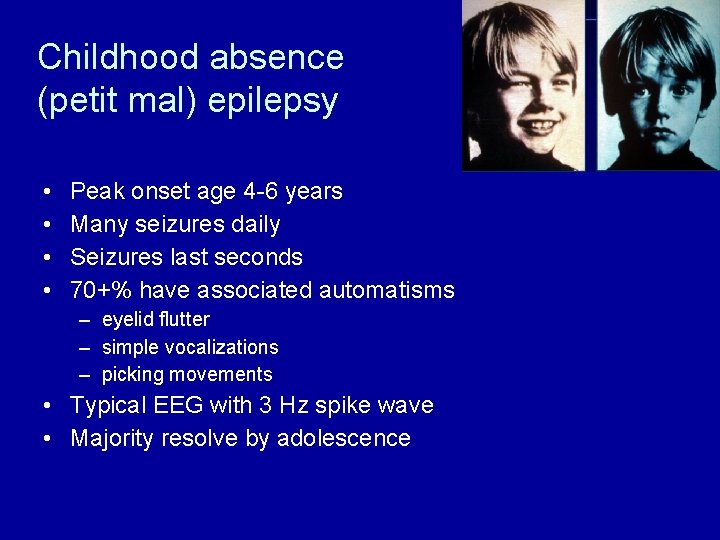
Childhood absence (petit mal) epilepsy • • Peak onset age 4 -6 years Many seizures daily Seizures last seconds 70+% have associated automatisms – eyelid flutter – simple vocalizations – picking movements • Typical EEG with 3 Hz spike wave • Majority resolve by adolescence
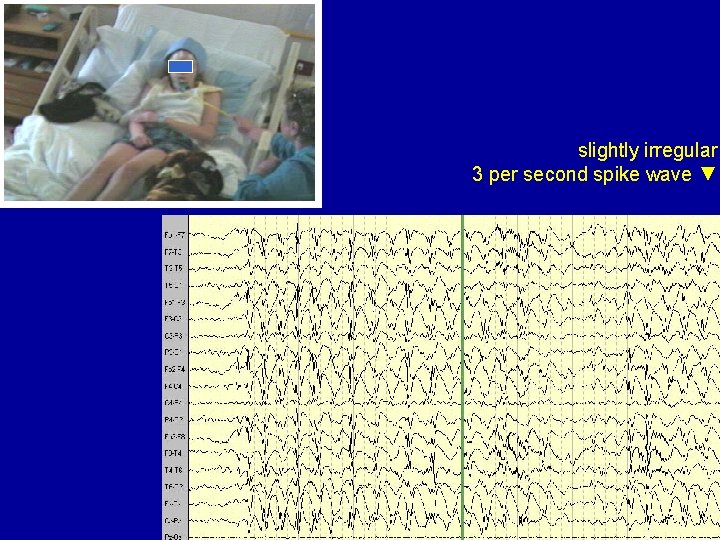
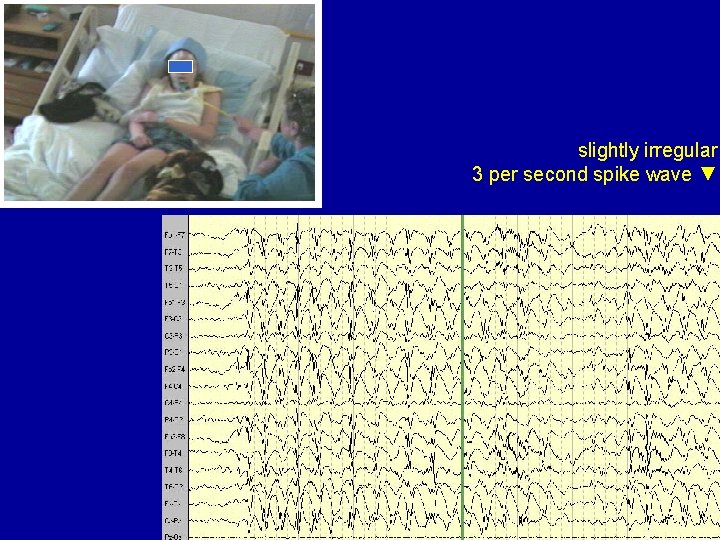
slightly irregular 3 per second spike wave ▼
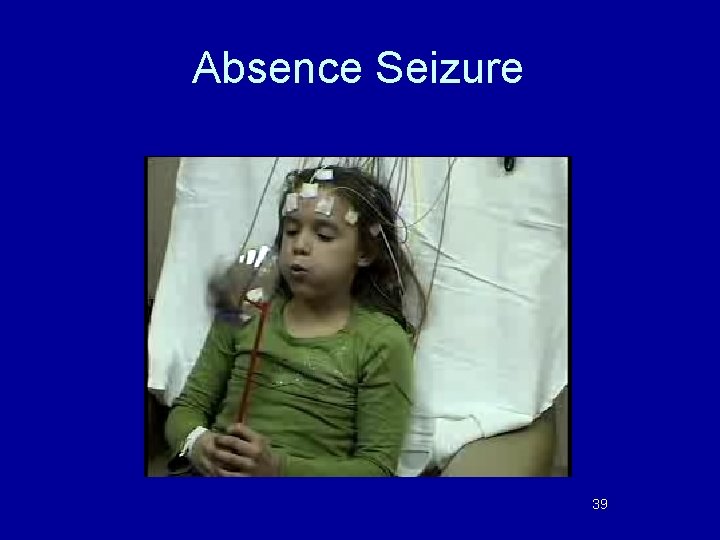
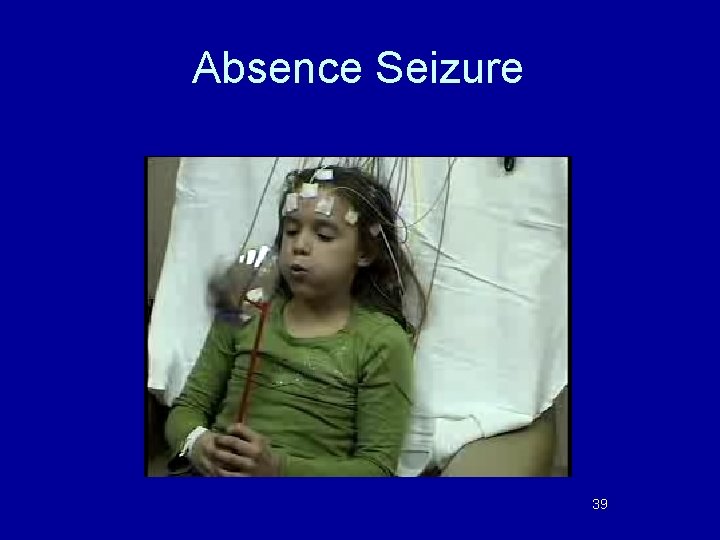
Absence Seizure 39
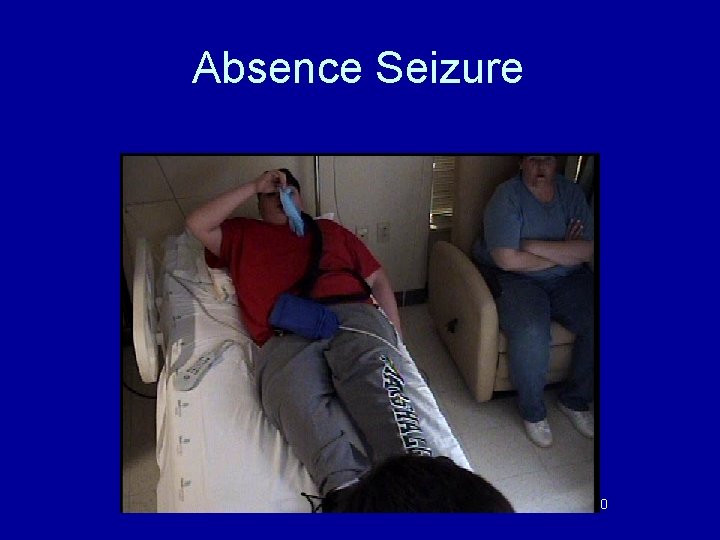
Absence Seizure 40
Absence Seizure 41
Pathophysiology of Absence Seizures • Generalized discharges occur from abnormal oscillatory rhythm in thalamocortical circuits • High density of T-type calcium channels in thalamus, thought to be involved

Treating absence seizures • • Ethosuximide (Zarontin) Valproic Acid (Depakote) Lamotrigine (Lamictal) Levetiracetam (Keppra)
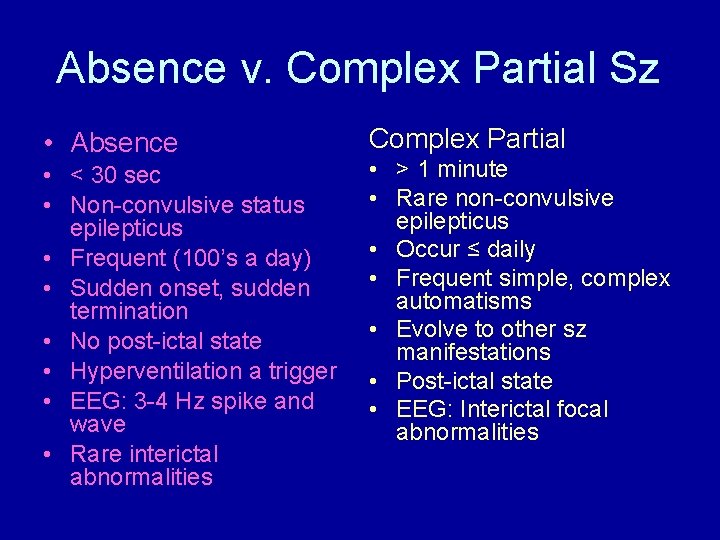
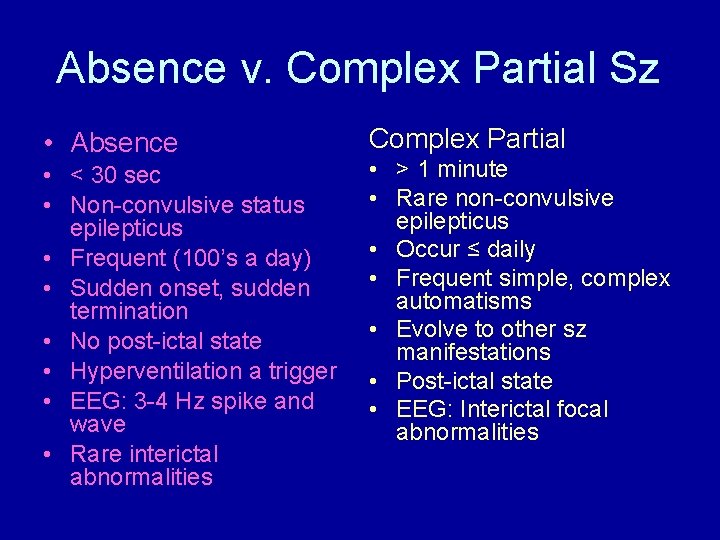
Absence v. Complex Partial Sz • Absence • < 30 sec • Non-convulsive status epilepticus • Frequent (100’s a day) • Sudden onset, sudden termination • No post-ictal state • Hyperventilation a trigger • EEG: 3 -4 Hz spike and wave • Rare interictal abnormalities Complex Partial • > 1 minute • Rare non-convulsive epilepticus • Occur ≤ daily • Frequent simple, complex automatisms • Evolve to other sz manifestations • Post-ictal state • EEG: Interictal focal abnormalities
Behavioral Staring • Most commonly seen in children with ADD, PDD, MR • Occurs when “bored” or over-stimulated • Does not typically make the patient fall or stop an activity abruptly • Can be stopped with close contact / stimulation • Also can be seen in children with epilepsy!
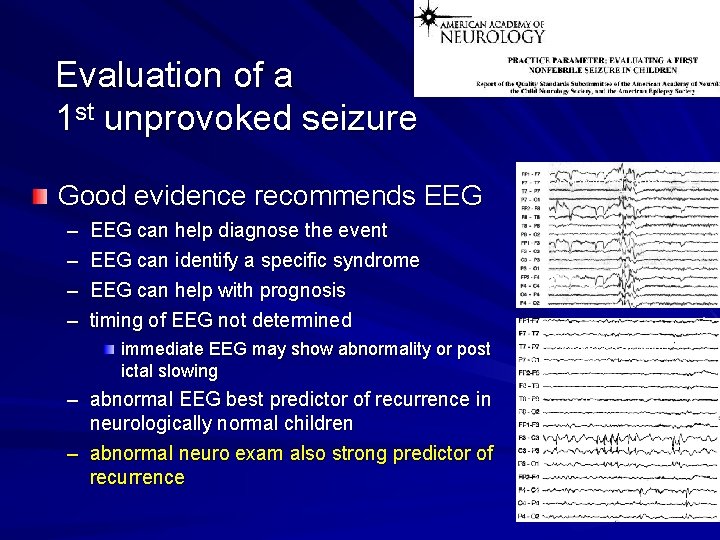
Evaluation of a 1 st unprovoked seizure Good evidence recommends EEG – – Generalized burst EEG can help diagnose the event EEG can identify a specific syndrome EEG can help with prognosis timing of EEG not determined immediate EEG may show abnormality or post ictal slowing Benign focal spike – abnormal EEG best predictor of recurrence in neurologically normal children – abnormal neuro exam also strong predictor of recurrence 46

Evaluation of a 1 st unprovoked seizure • Insufficient evidence for routine labs, LP, imaging – consider emergent imaging if postictal focal deficit, or not at baseline in several hours – consider nonurgent MRI with significant neuro abnormalities of unknown etiology a seizure of focal onset in children under 1 year of age – consider LP in the very young child (<6 months) in the patient who fails to return to baseline in any patient with meningeal signs if increased ICP suspected, image before LP 47
How likely is a 2 nd seizure? Evidence from multiple Class III studies Recurrence ranged from 14%-65% Most recurrences early (in 1 st year) Factors increasing recurrence risk – abnormal EEG – etiology remote symptomatic seizure recurrence >50% idiopathic seizure recurrence 30 -50% 48
Summary of evidence: Treatment of 1 st unprovoked seizure Most children with a 1 st seizure have few or no recurrences 10% will have many seizures regardless of initial Rx Rx after 1 st vs. 2 nd seizure does not affect long term prognosis Rx in adults and children leads to decreased recurrences 49
Recommendations: Treatment of a 1 st Seizure Anticonvulsant treatment after a 1 st seizure must be individualized – treatment is not indicated for prevention of epilepsy – treatment may be considered if risks of recurrent seizure out weigh risks of Rx Treatment must take into account patient and family preferences 50
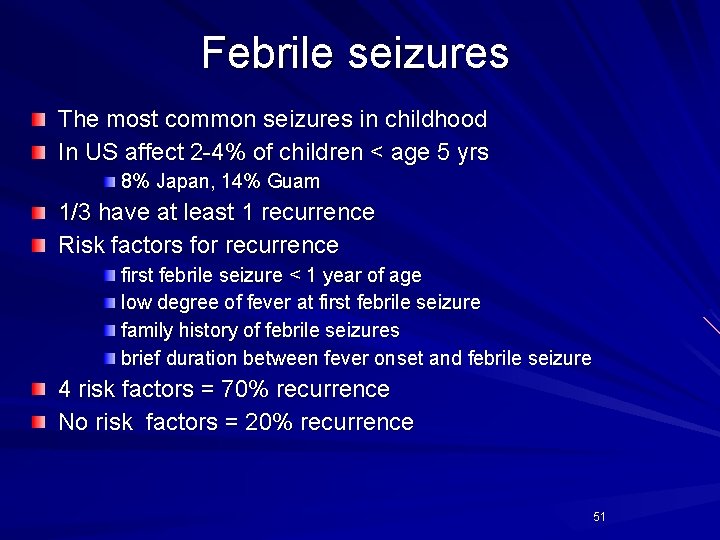
Febrile seizures The most common seizures in childhood In US affect 2 -4% of children < age 5 yrs 8% Japan, 14% Guam 1/3 have at least 1 recurrence Risk factors for recurrence first febrile seizure < 1 year of age low degree of fever at first febrile seizure family history of febrile seizures brief duration between fever onset and febrile seizure 4 risk factors = 70% recurrence No risk factors = 20% recurrence 51

Febrile seizures Simple – generalized – and <15 minutes duration Complex – – – focal or >15 minutes or recurrent within 24 hours 52
Evaluation of the child with simple febrile seizures Lumbar puncture – if meningeal signs – in infants < 12 months – with prior antibiotic Rx Blood studies not needed routinely Imaging not necessary EEG not necessary in simple febrile seizures 53
Treatment of the child with simple febrile seizures Effective in reducing recurrences but with potential toxicities – continuous phenobarbital or valproic acid – intermittent diazepam 54
Treatment options for pharmacoresistant epilepsy Ketogenic diet Vagus nerve stimulation Surgery 55

Ketogenic diet Very high fat, very low CHO, minimum RDA protein Vitamins, mineral supplements necessary Rigid compliance essential Effective in 1/3 -1/2 cases breakfast – all seizure types – all ages, but easiest to maintain in children lunch 56
Ketogenic diet formulations Formulated in fat: CHO ratios – generally between 4: 1 and 3: 1 – Atkins diet is about 2. 2: 1 Traditional diet – uses 40% cream, fatty foods MCT diet – adds oils to “normal foods” Tube feeding diet – CHO-free formula + microlipids or cooking oil 57
Surgical treatment of epilepsy Lobectomy – anterior temporal lobectomy most frequent procedure – 70% of selected patients become seizure-free Extratemporal resection – nature and extent of pathology determine results Hemispherectomy, multilobar resections – done in cases with extensive pathology Corpus callosotomy – rarely performed as sole procedure Multiple subpial transections – Palliative, done when focus is in “eloquent cortex” 58
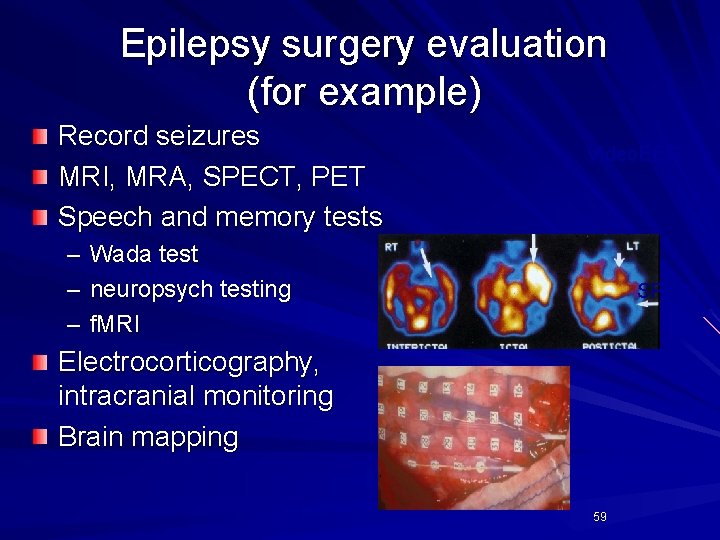
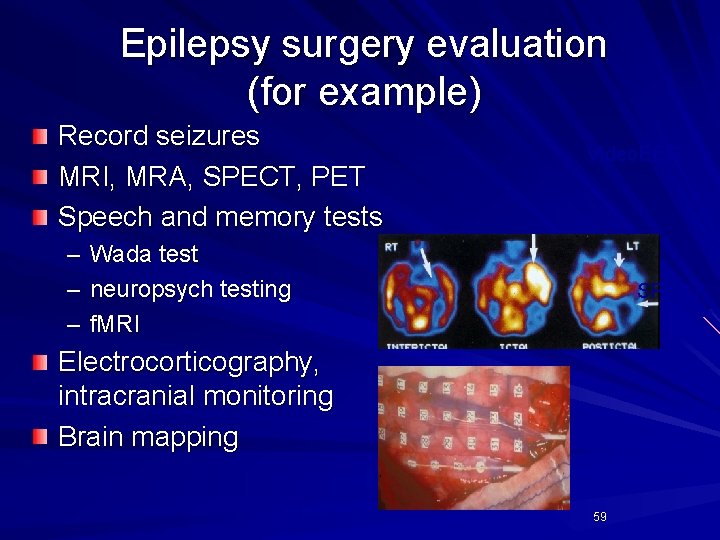
Epilepsy surgery evaluation (for example) Record seizures MRI, MRA, SPECT, PET Speech and memory tests – – – Video. EEG Wada test neuropsych testing f. MRI Electrocorticography, intracranial monitoring Brain mapping SPECT Intracranial grid 59
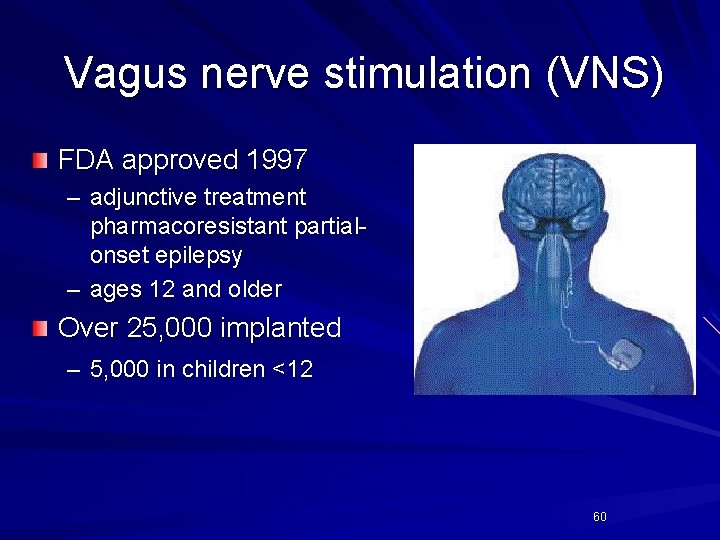
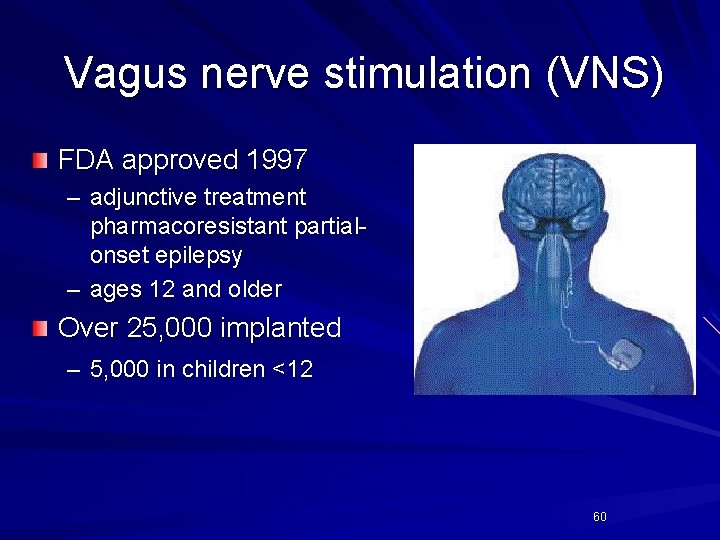
Vagus nerve stimulation (VNS) FDA approved 1997 – adjunctive treatment pharmacoresistant partialonset epilepsy – ages 12 and older Over 25, 000 implanted – 5, 000 in children <12 60
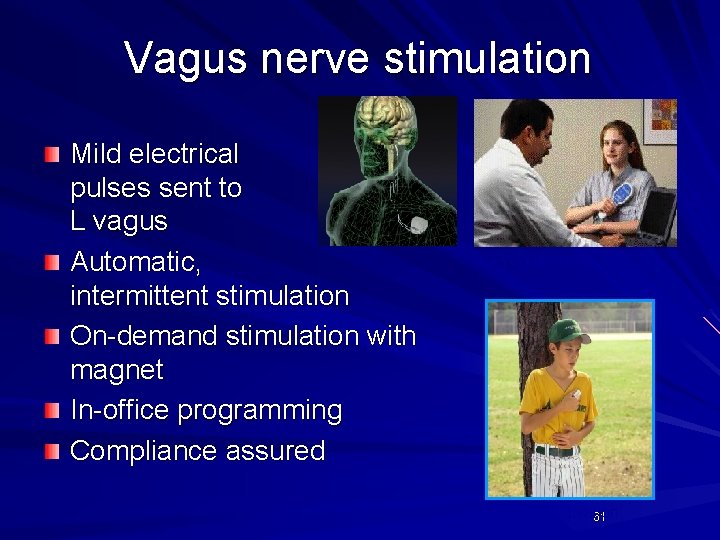
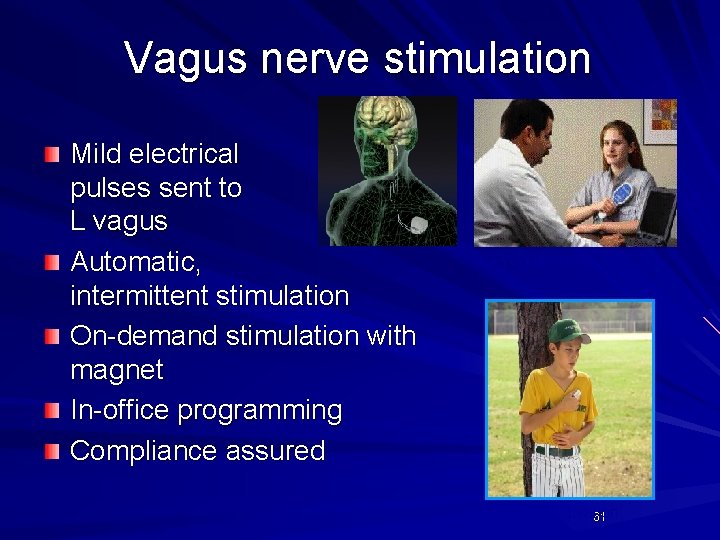
Vagus nerve stimulation Mild electrical pulses sent to L vagus Automatic, intermittent stimulation On-demand stimulation with magnet In-office programming Compliance assured Programming Magnet activation 61
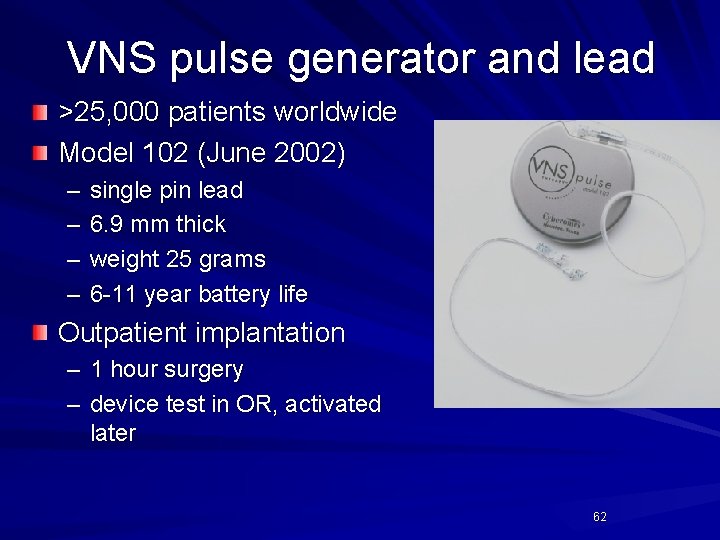
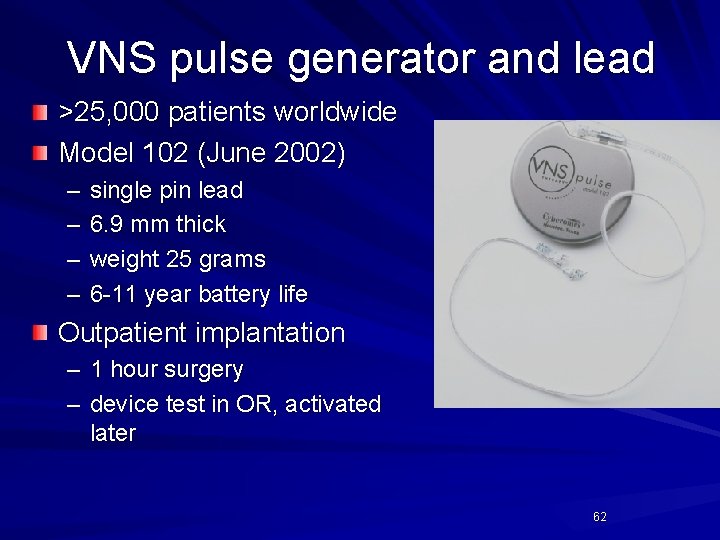
VNS pulse generator and lead >25, 000 patients worldwide Model 102 (June 2002) – – single pin lead 6. 9 mm thick weight 25 grams 6 -11 year battery life Outpatient implantation – 1 hour surgery – device test in OR, activated later 62

Seizure-response dogs How do they do it? Trained by several organizations 63

Diastat 64
Rectal diazepam - Given for seizures lasting longer than 5 minutes - Diastat is a safe way to give rescue seizure medication in the home or school environment - Dose varies by age and weight - If seizure continues 5 minutes after Diastat given, then EMS should be contacted - Some children have seizures that consistently are prolonged; in the case Diastat may be prescribed to be given at onset of seizure, instead of waiting 5 minutes. - Not FDA approved in children less than 2 years of age 65
Other Rescue Medication Options - Nasal midazolam - children refractory to Diastat - Oral lorazepam - seizure clusters - Routine seizure medications are NOT given as rescue medications - If a child routinely requires rescue medications on a consistent basis, then routine scheduled seizure medications need to be changed 66
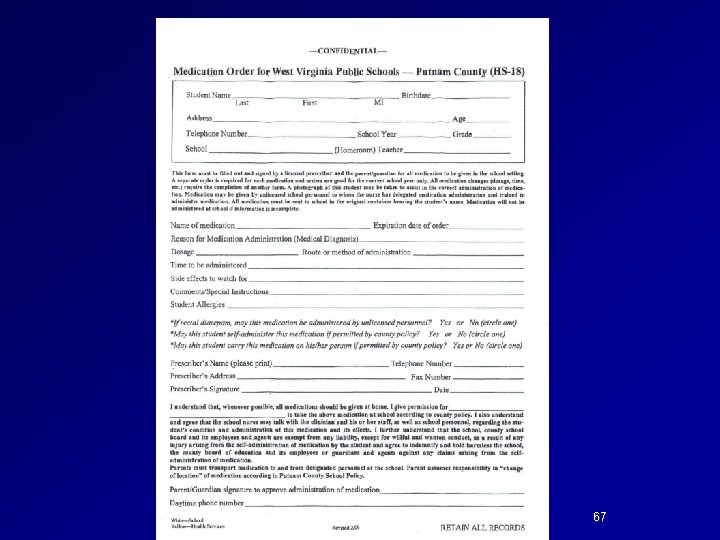
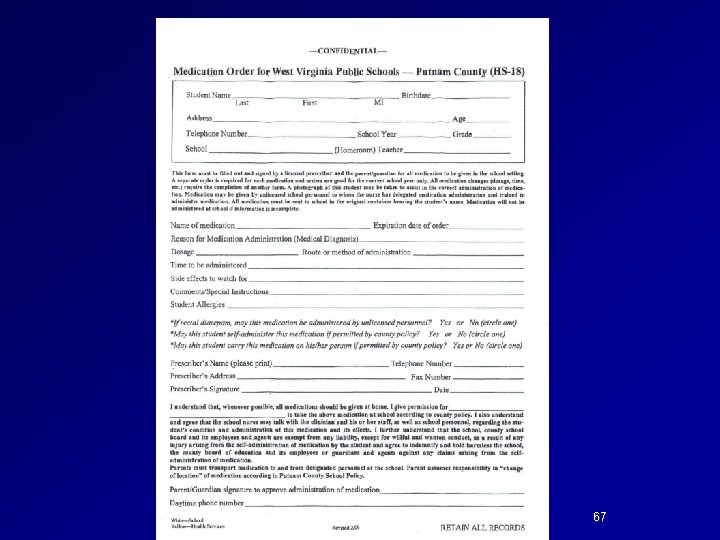
67

Thank you! 68
 Inflatable helmet for epilepsy
Inflatable helmet for epilepsy Which is an alternative of log based recovery
Which is an alternative of log based recovery Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Shaking vs seizure
Shaking vs seizure Epilepsy
Epilepsy Difference between seizure and epilepsy
Difference between seizure and epilepsy Catamenial epilepsy and birth control pills
Catamenial epilepsy and birth control pills Spina bifida and epilepsy
Spina bifida and epilepsy Develop and update food and beverage knowledge
Develop and update food and beverage knowledge Epilepsy ilae 2017
Epilepsy ilae 2017 Canadian league against epilepsy
Canadian league against epilepsy Migraine aura vs seizure aura
Migraine aura vs seizure aura Aremco epilepsy
Aremco epilepsy Vanderbilt nurse residency interview questions
Vanderbilt nurse residency interview questions Epilepsy
Epilepsy Epilepsy trigger
Epilepsy trigger European epilepsy database
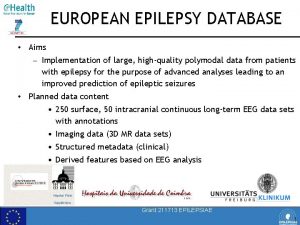
European epilepsy database Catastrophic epilepsy infancy
Catastrophic epilepsy infancy Post ictal phase
Post ictal phase Cps epilepsy
Cps epilepsy What is epilepsy
What is epilepsy Convagran
Convagran Depakote epilepsy
Depakote epilepsy Epilepsy
Epilepsy Epilepsy
Epilepsy Spinocerebellar ataxia
Spinocerebellar ataxia Terratogenesis
Terratogenesis Northeast regional epilepsy
Northeast regional epilepsy Northeast regional epilepsy
Northeast regional epilepsy Epilepsy
Epilepsy Epilepsy death
Epilepsy death Snomed vs icd
Snomed vs icd Ykp epilepsy
Ykp epilepsy Epilepsy ppt
Epilepsy ppt Xl spikes on eeg
Xl spikes on eeg Seizures
Seizures Aremco epilepsy
Aremco epilepsy Susanne finn
Susanne finn Northeast regional epilepsy
Northeast regional epilepsy Young epilepsy
Young epilepsy American epilepsy society annual meeting 2017
American epilepsy society annual meeting 2017 Dr politsky epilepsy
Dr politsky epilepsy Sql insert update delete query
Sql insert update delete query Data redundancy and update anomalies
Data redundancy and update anomalies Pediatric first aid for caregivers and teachers
Pediatric first aid for caregivers and teachers Prof dr ayça vitrinel
Prof dr ayça vitrinel Overview of transcription and translation
Overview of transcription and translation Data quality and data cleaning an overview
Data quality and data cleaning an overview Chapter 17 elements and their properties answer key
Chapter 17 elements and their properties answer key Chicago time
Chicago time What is bioinformatics an introduction and overview
What is bioinformatics an introduction and overview An overview of data warehousing and olap technology
An overview of data warehousing and olap technology Data quality and data cleaning an overview
Data quality and data cleaning an overview Data quality and data cleaning an overview
Data quality and data cleaning an overview Overview of storage and indexing
Overview of storage and indexing Elements and their properties section 1 metals
Elements and their properties section 1 metals Zechariah stevenson update
Zechariah stevenson update What are these
What are these University community plan
University community plan Temporary update problem in dbms
Temporary update problem in dbms Www.sabupdate.com download
Www.sabupdate.com download Lnes
Lnes Dokumen deskripsi sdmk
Dokumen deskripsi sdmk Teacher prd examples
Teacher prd examples Position update formula
Position update formula Position update formula
Position update formula Fiberhome hg6243c firmware download
Fiberhome hg6243c firmware download Move update compliance
Move update compliance Mdh situation update
Mdh situation update