PEDIATRIC EMERGENCE DELIRIUM AND THE USE OF PRECEDEX

- Slides: 31
PEDIATRIC EMERGENCE DELIRIUM AND THE USE OF PRECEDEX ADRIENNE DOMANICO RN, MSN, CRNA SOFA CONFERENCE FALL 2018
OBJECTIVES üDefine emergence delirium and its importance to anesthesia providers üIdentify risk factors for development of emergence delirium üIllustrate pharmacological properties of Precedex üExplain the use of Precedex in the treatment of pediatric emergence delirium
Agitation Delirium DEFINITIONS • “A more or less temporary disorder of the mental faculties, as in fevers, disturbances of consciousness, or intoxication, characterized by restlessness, excitement, delusions, hallucinations, etc. ; a state of violent excitement and emotion” – www. dictionary. com • “A neuropsychiatric condition that is secondary to a general medical condition and/or its treatments” (Schieveld and Janssen, 2014) • “To move or force into violent, irregular action; impart regular motion too; to disturb or excite emotionally, arouse, perturb; to call attention to with speech or writing; ruffle, fluster, roil” – www. dictionary. com So, what does the literature say…. .
… IT SAYS THIS • “A wide variety of behavioral disturbances seen in children following emergence from anesthesia” (Chandler et al 2012) • “A mental disturbance common in children during recovery of general anesthesia” (Mountain et al 2011) • “Characterized by a variety of presentations… during the early stage of emergence from anesthesia” (Dahmani et al. , 2010) • “A mental disturbance during the recovery from general anesthesia…” (Locatelli et al, 2012) • “A dissociative state of consciousness in which the child is irritable, uncompromising, uncooperative, incoherent, and inconsolably crying, moaning, kicking, or thrashing” (Reduque and Verghese, 2012) WHAT DOES IT ALL MEAN? !? !
IMPORTANCE • “Children get delirious so often and quickly that this is of no importance to us” ‐ Bleuler (1857‐ 1939) • So what does ED mean to us?
PEDIATRIC VS ADULT • Pediatrics • can last up to 30 minutes, in about 80% of pediatric cases!!! • Most commonly in ages 2‐ 8 • Adult • can be seen at any age • an incidence around 40% but this includes ICU psychosis, chronic illness, etc in addition to emergence
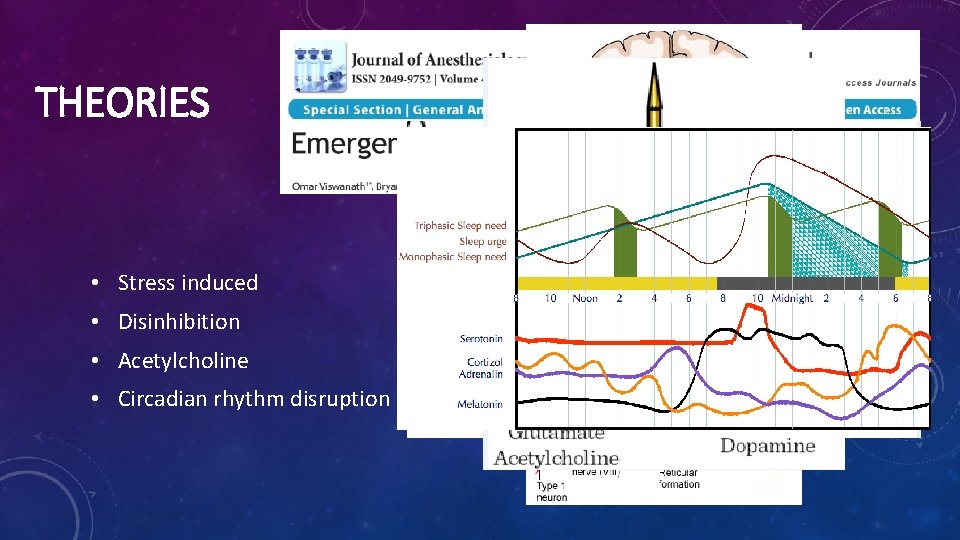
THEORIES • Stress induced • Disinhibition • Acetylcholine • Circadian rhythm disruption
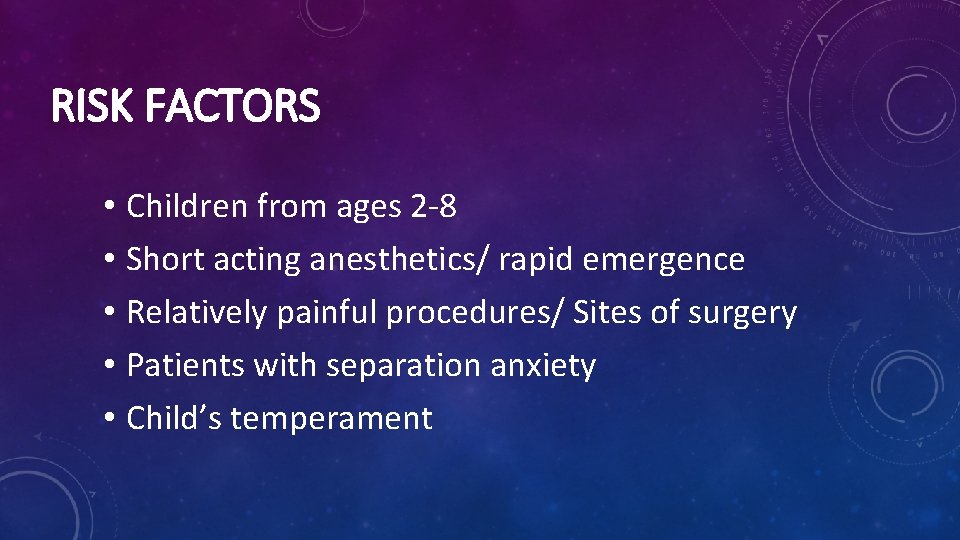
RISK FACTORS • Children from ages 2‐ 8 • Short acting anesthetics/ rapid emergence • Relatively painful procedures/ Sites of surgery • Patients with separation anxiety • Child’s temperament
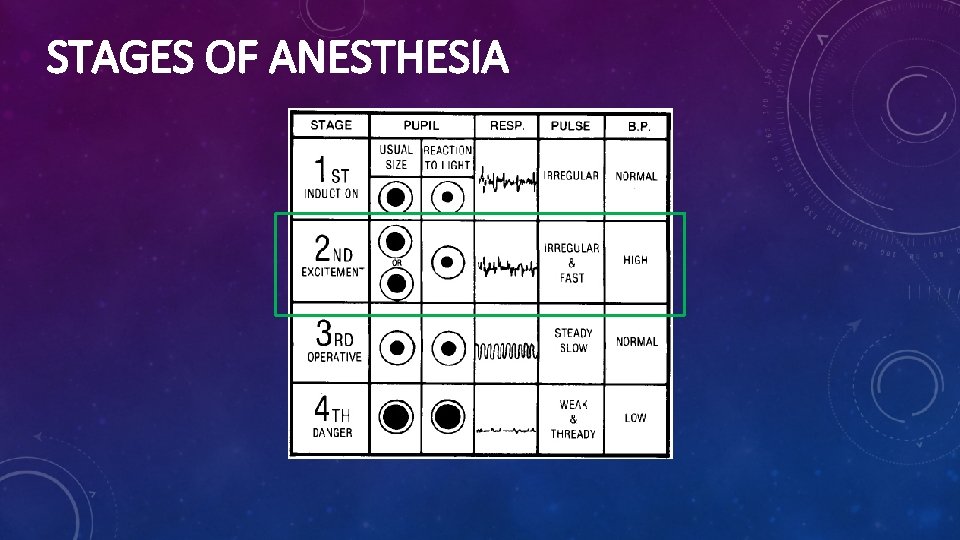
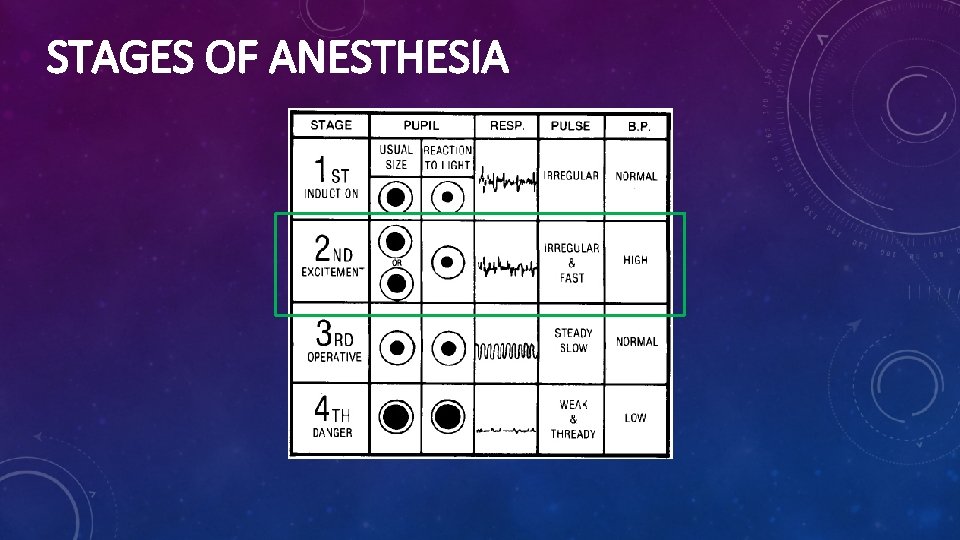
STAGES OF ANESTHESIA

Instead of this…. … We want this!!!
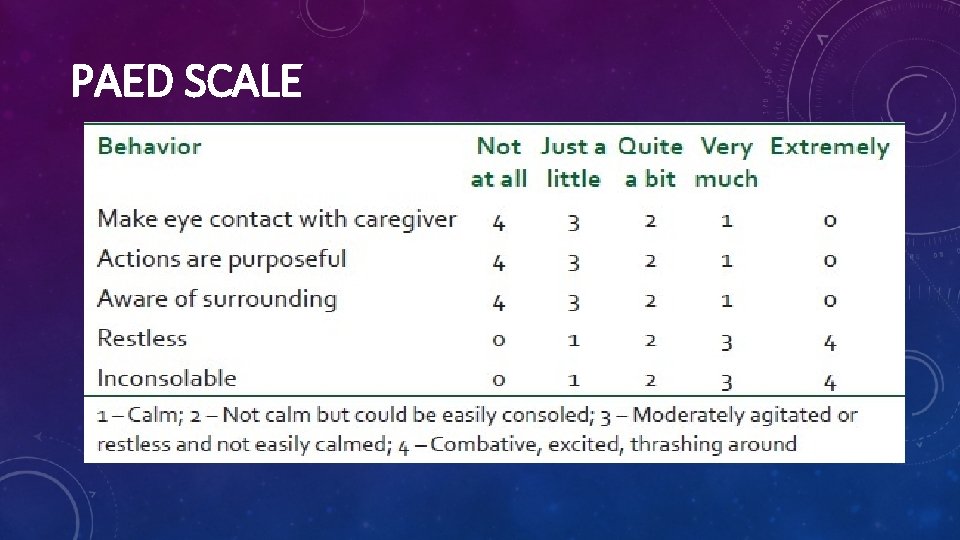
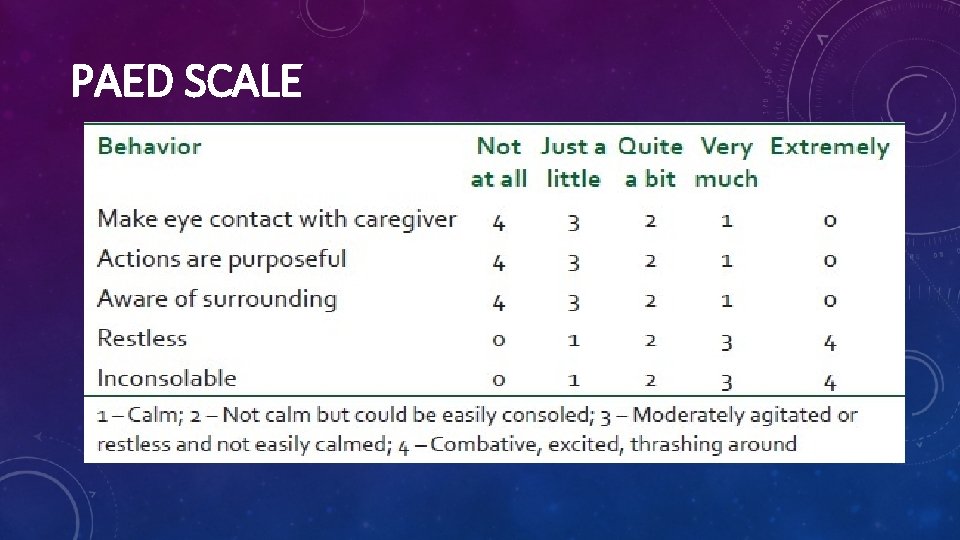
PAED SCALE
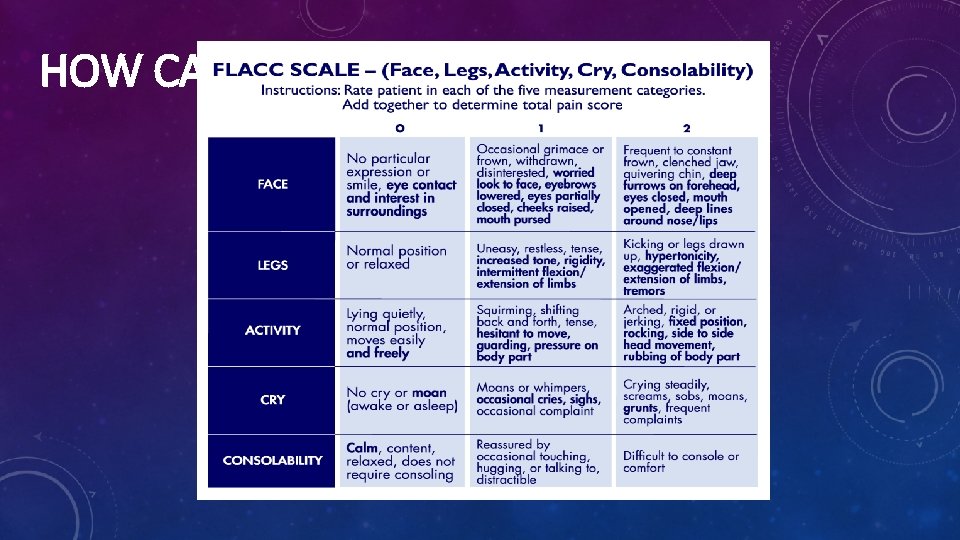
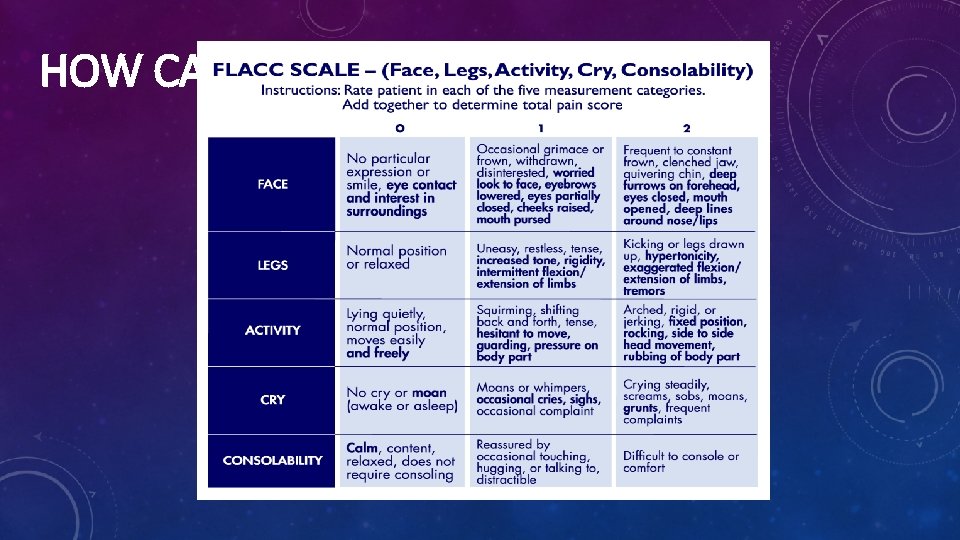
HOW CAN YOU TELL IF IT’S PAIN?
LET’S REVIEW SOME A & P
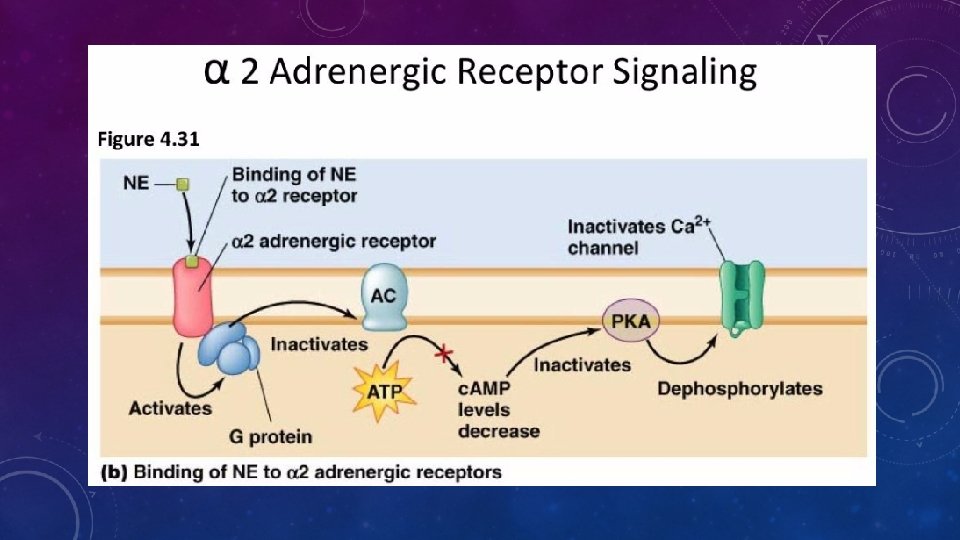
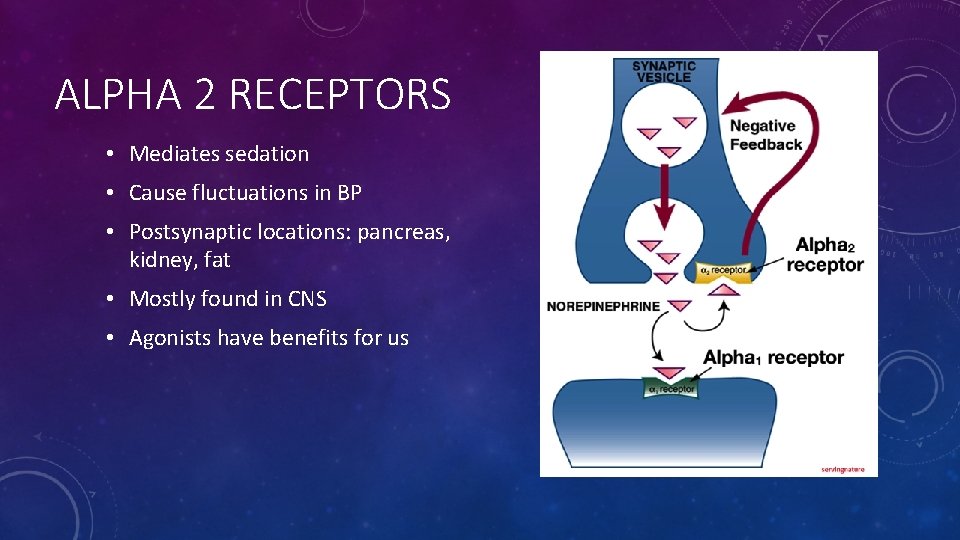
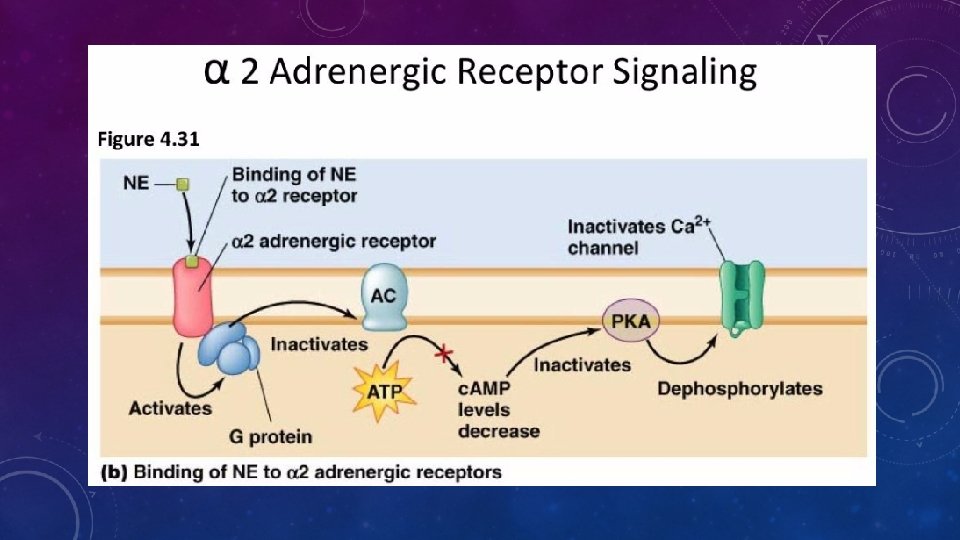
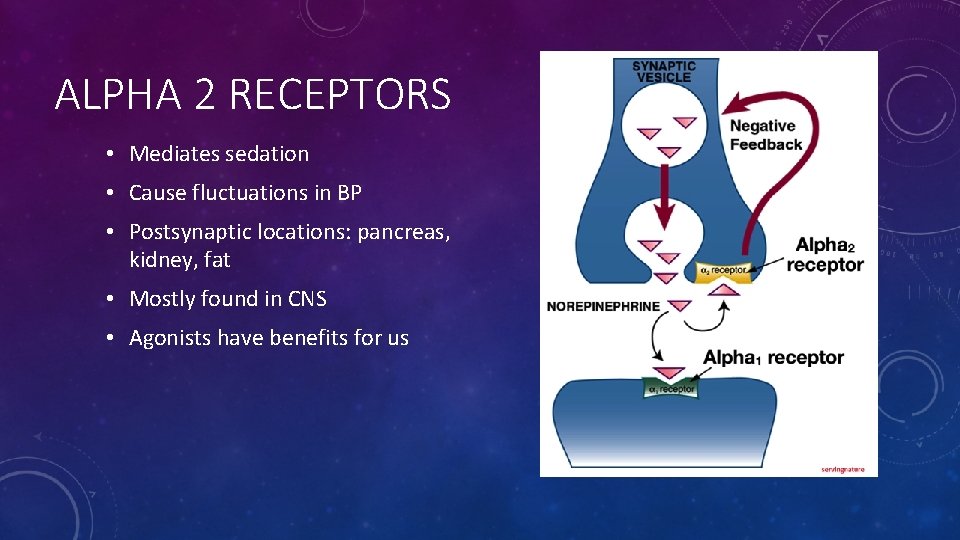
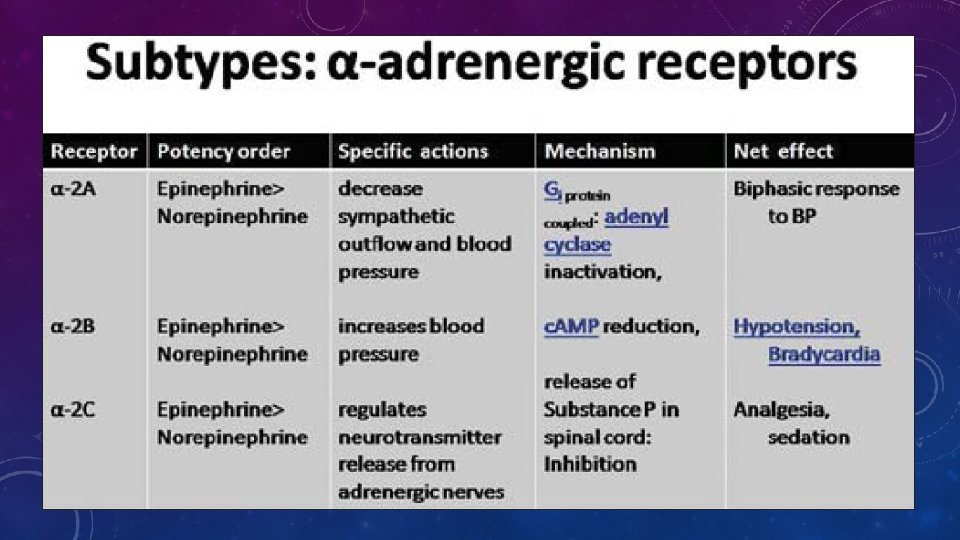
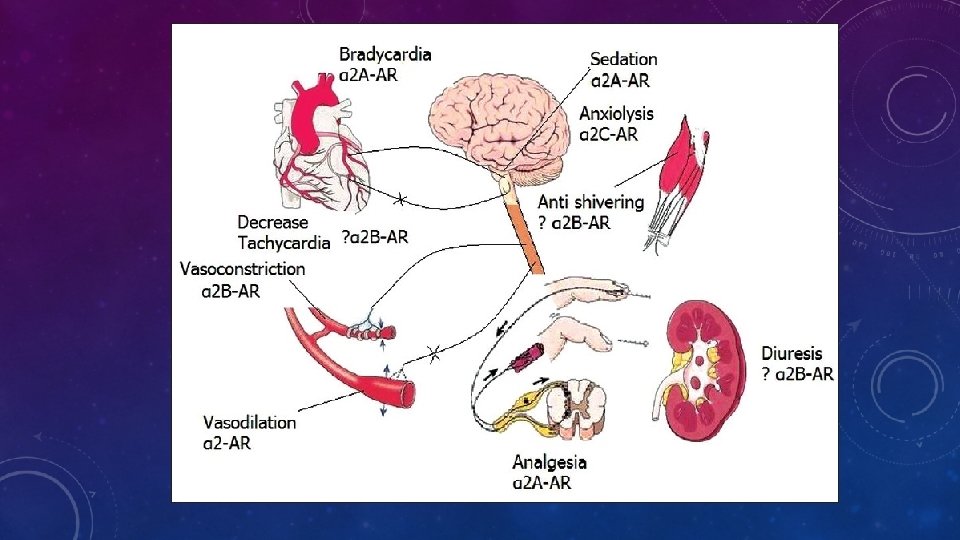
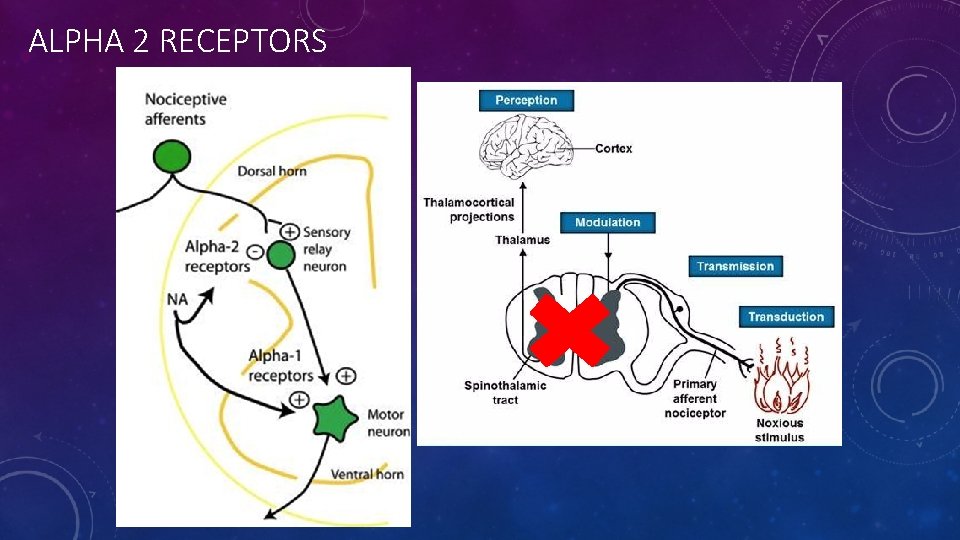
ALPHA 2 RECEPTORS • Mediates sedation • Cause fluctuations in BP • Postsynaptic locations: pancreas, kidney, fat • Mostly found in CNS • Agonists have benefits for us
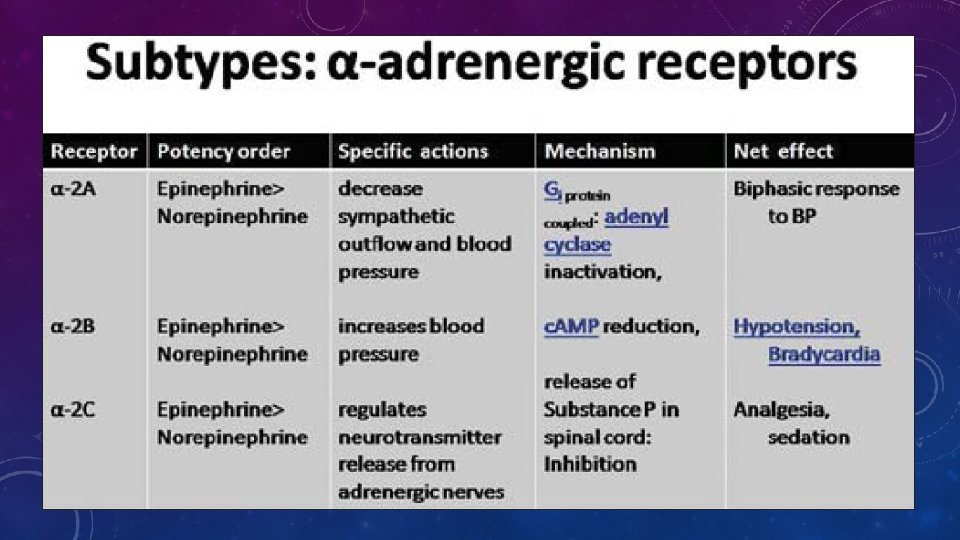
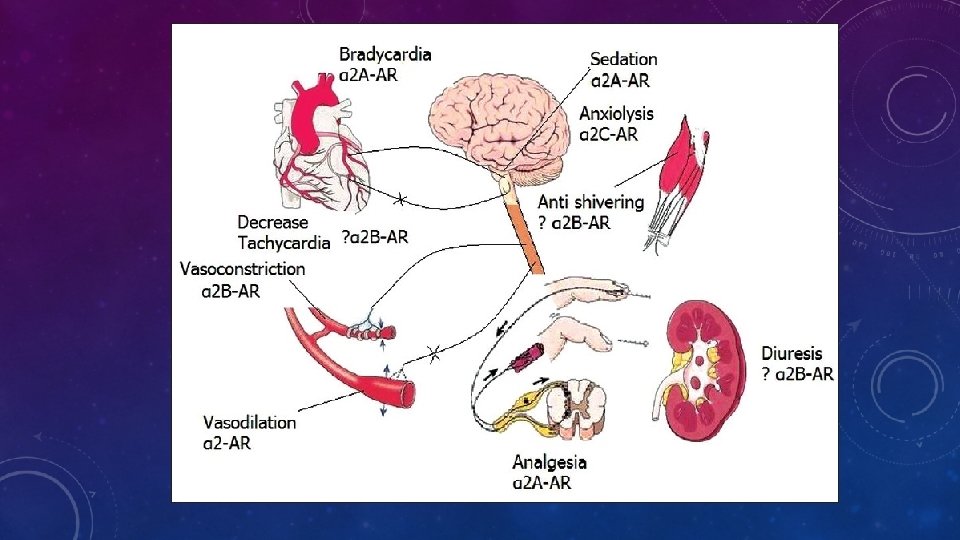
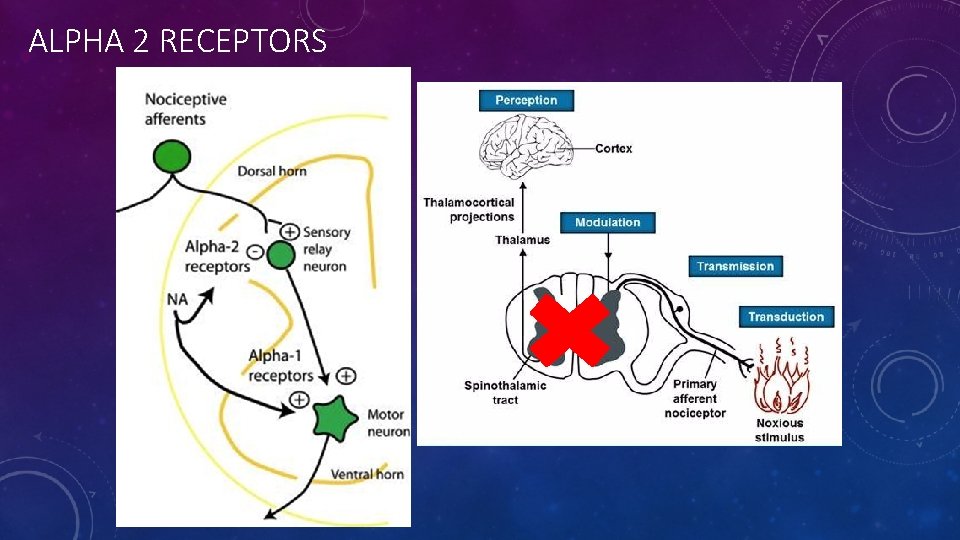
ALPHA 2 RECEPTORS
… Or sitting through this presentation
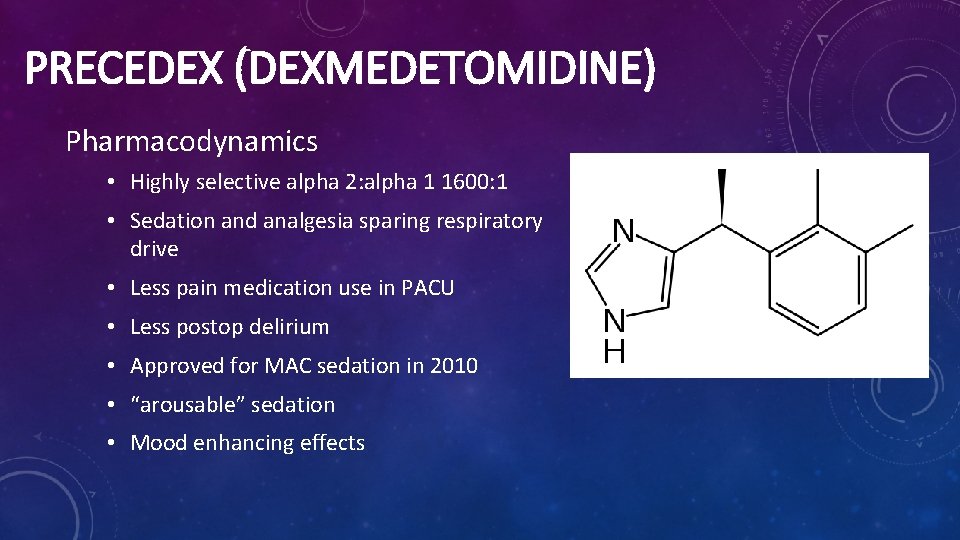
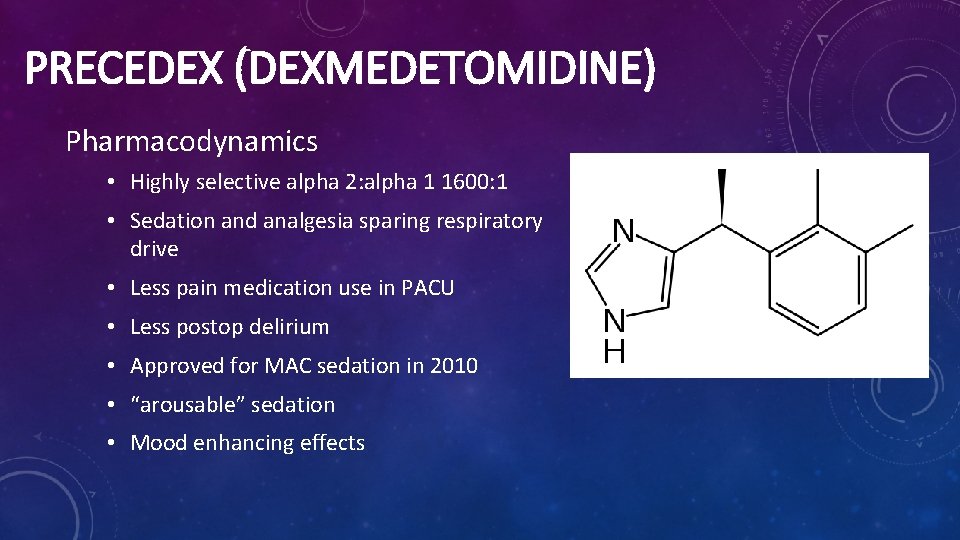
PRECEDEX (DEXMEDETOMIDINE) Pharmacodynamics • Highly selective alpha 2: alpha 1 1600: 1 • Sedation and analgesia sparing respiratory drive • Less pain medication use in PACU • Less postop delirium • Approved for MAC sedation in 2010 • “arousable” sedation • Mood enhancing effects
PRECEDEX Pharmacokinetics • Distribution half life = 6 mins • Terminal elimination half life = 2‐ 3 hrs • Plasma binding is 94% and significantly decreased in hepatic impaired subjects • Metabolism = glucuronodation and cytochrome p 450 metabolism to undergo almost complete biotransformation and excreted almost entirely through kidneys • No difference in pharmacokinetics for impaired renal patients
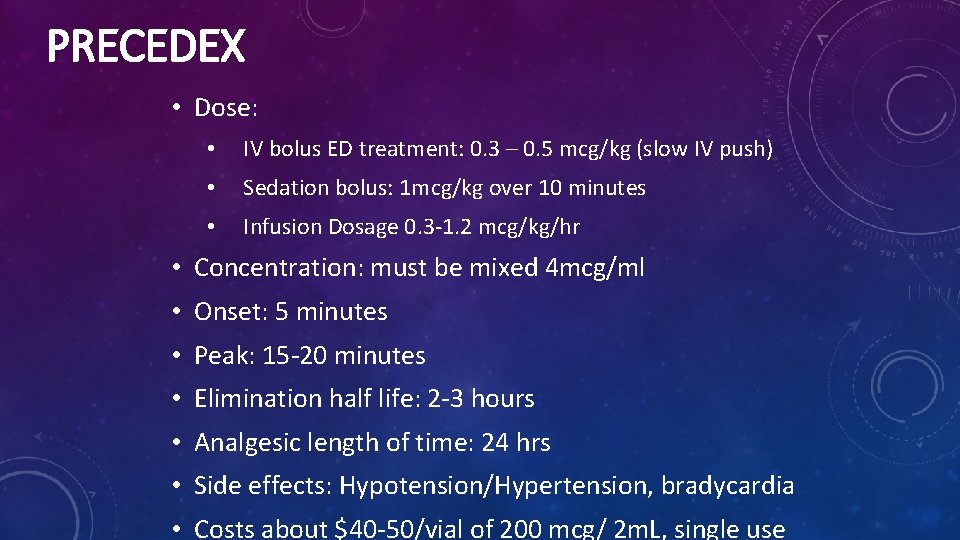
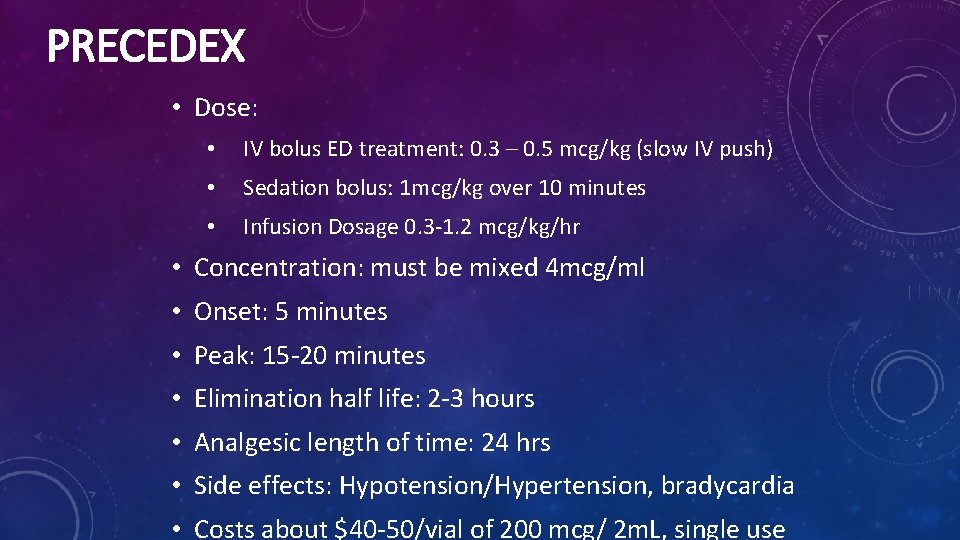
PRECEDEX • Dose: • IV bolus ED treatment: 0. 3 – 0. 5 mcg/kg (slow IV push) • Sedation bolus: 1 mcg/kg over 10 minutes • Infusion Dosage 0. 3‐ 1. 2 mcg/kg/hr • Concentration: must be mixed 4 mcg/ml • Onset: 5 minutes • Peak: 15‐ 20 minutes • Elimination half life: 2‐ 3 hours • Analgesic length of time: 24 hrs • Side effects: Hypotension/Hypertension, bradycardia • Costs about $40‐ 50/vial of 200 mcg/ 2 m. L, single use
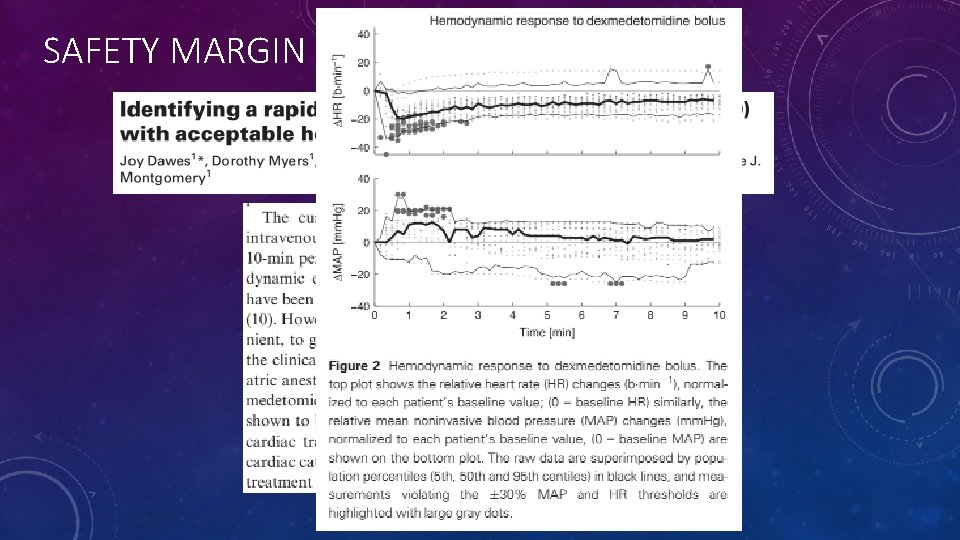
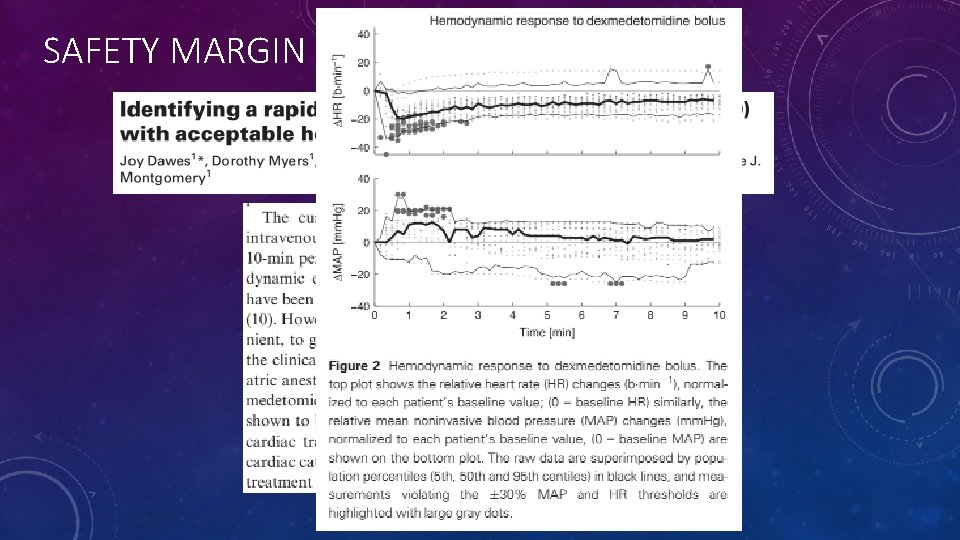
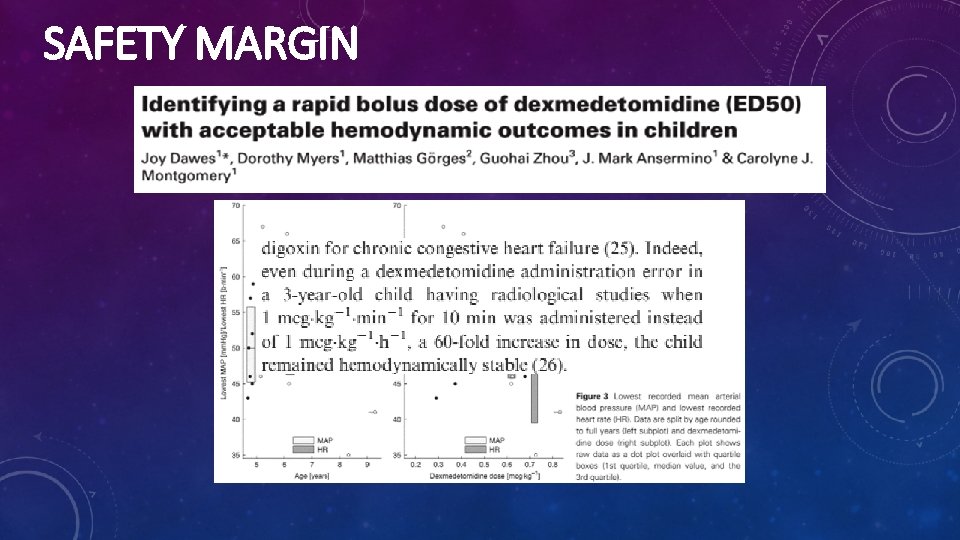
SAFETY MARGIN
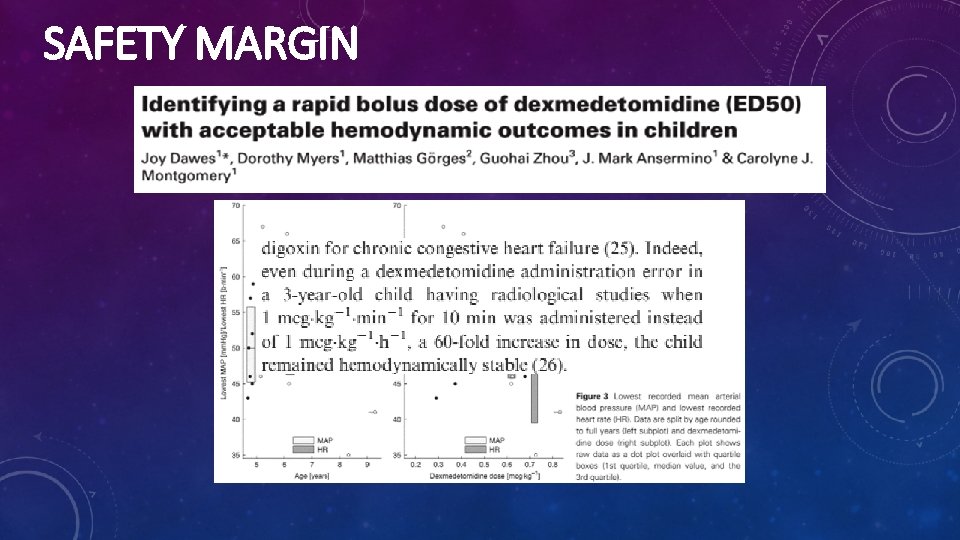
SAFETY MARGIN
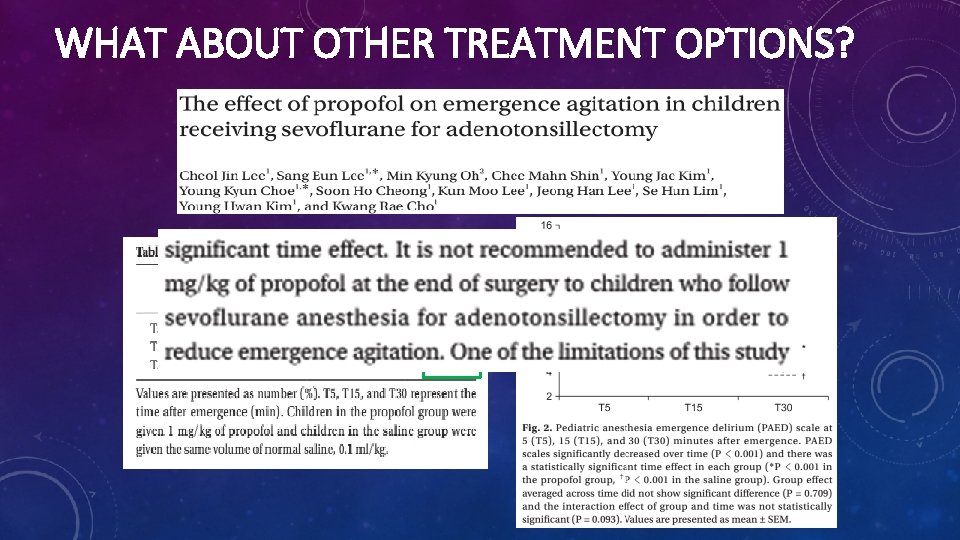
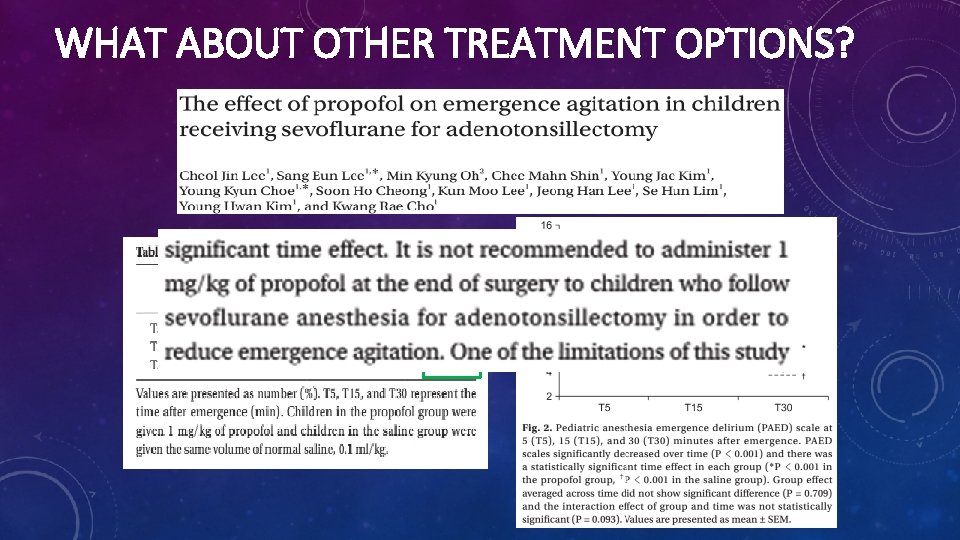
WHAT ABOUT OTHER TREATMENT OPTIONS?
TEAM PROPOFOL… MAYBE
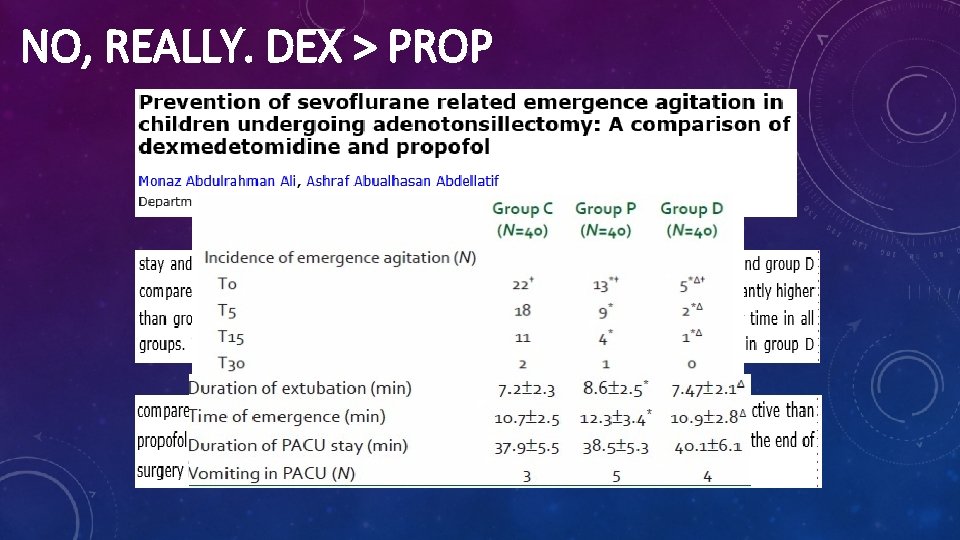
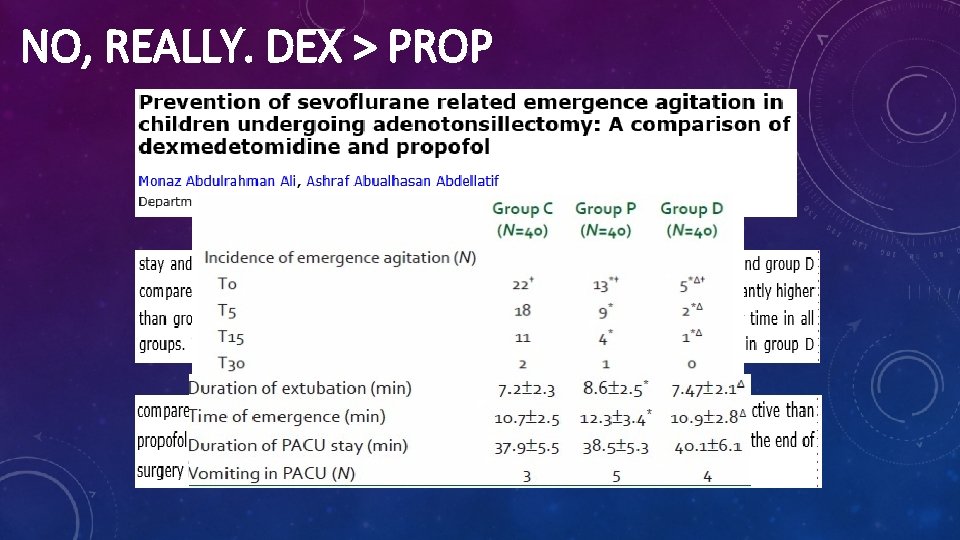
NO, REALLY. DEX > PROP
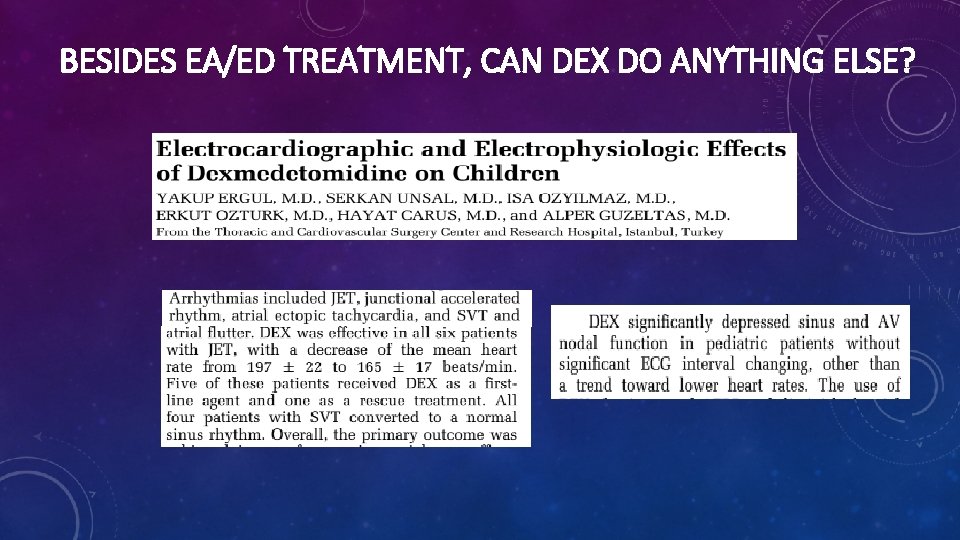
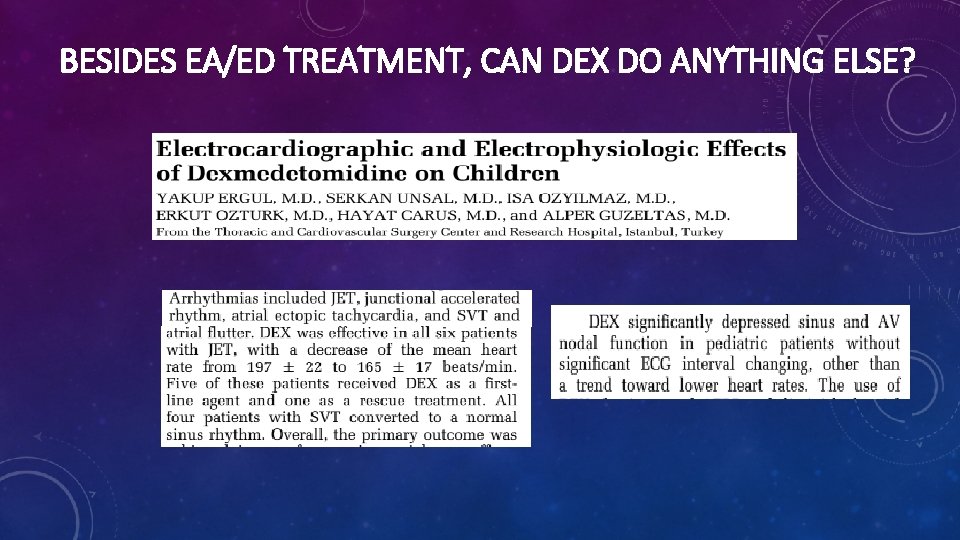
BESIDES EA/ED TREATMENT, CAN DEX DO ANYTHING ELSE?
PEARLS I’VE LEARNED • • • 0. 3‐ 0. 4 mcg/kg is the sweet spot Time it for extubation Works really well in patients with MR, autism, ADHD Careful with a pre‐med There is no alligator rolling Some providers are still not comfortable with it but…
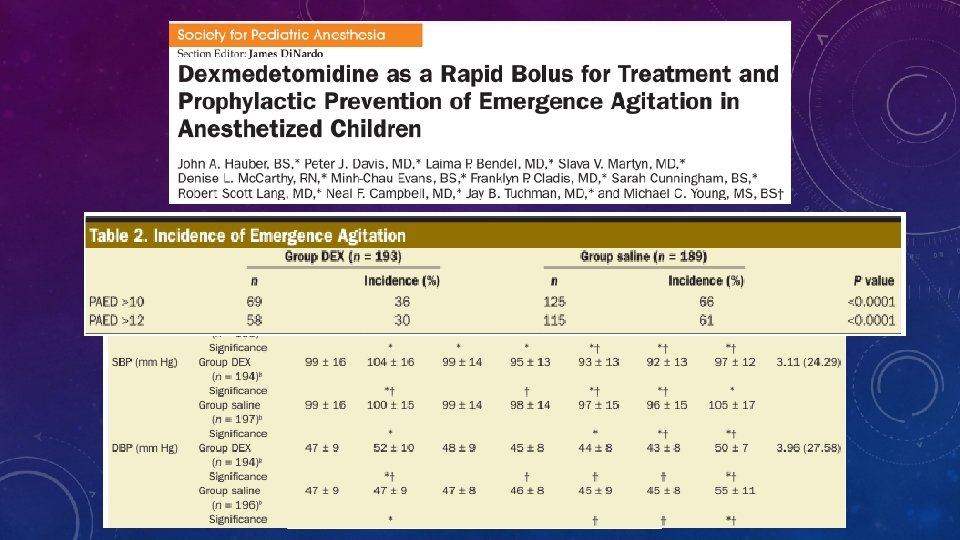
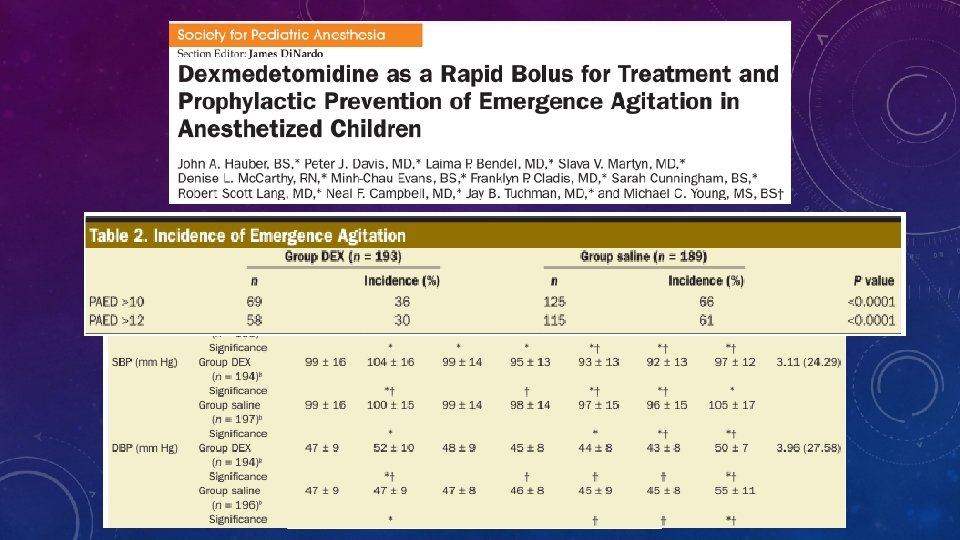
REFERENCES • Ali, M. A. , & Abdellatif, A. A. (2013). Prevention of sevoflurane related emergence agitation in children undergoing adenotonsillectomy: A comparison of dexmedetomidine and propofol. Saudi journal of anaesthesia. 7(3), 296. • Chen, J. Y. , Jia, J. E. , Liu, T. J. , Qin, M. J. , & Li, W. X. (2013). Comparison of the effects of dexmedetomidine, ketamine, and placebo on emergence agitation after strabismus surgery in children. Canadian Journal of Anesthesia, 60(4), 385‐ 392 • Dawes, J. , Myers, D. , Görges, M. , Zhou, G. , Ansermino, J. M. , & Montgomery, C. J. (2014). Identifying a rapid bolus dose of dexmedetomidine (ED 50) with acceptable hemodynamic outcomes in children. Pediatric Anesthesia 24(12), 1260‐ 1267 • Enlow, W. M. , & Ardizzone, L. L. (2008). A systematic review: dexmedetomidine versus placebo to decrease the incidence of emergence delirium/emergence agitation (ED/EA) in pediatric patients. Clinical Scholars Review, 1(2). 89‐ 94 • Ergul, Y. , Unsal, S. , Ozyilmaz, I. , Ozturk, E. , Carus, H. , & Guzeltas, A. (2015). Electrocardiographic and electrophysiologic effects of dexmedetomidine on children. Pacing and Clinical Electrophysiology, 38(6), 682‐ 687 • Hauber, J. A. , Davis, P. J. , Bendel, L. P. , Martyn, S. V. , Mc. Carthy, D. L. , . . . & Tuchman, J. B. (2015) Dexmedetomidine as a rapid bolus for treatment and prophylactic prevention of emergence agitation in anesthetized children. Anesthesia & Analgesia, 121(5). 1308‐ 1315 • Hoff, S. L. , O'Neill, E. S. , Cohen, L. C. , & Collins, B. A. (2015). Does a prophylactic dose of propofol reduce emergence agitation in children receiving anesthesia? A systematic review and meta‐analysis. Pediatric Anesthesia, 25(7). 668‐ 676 • Lee, C. J. , Lee, S. E. , Oh, M. K. , Shin, C. M. , Kim, Y. J. , Choe, Y. K. , . . . & Kim, Y. H. (2010). The effect of propofol on emergence agitation in children receiving sevoflurane for adenotonsillectomy. Korean journal of anesthesiology, 59(2). 75‐ 81 • Sato, M. , Shirakami, G. , Tazuke‐Nishimura, M. , Matsuura, S. , Tanimoto, K. , & Fukuda, K. (2010). Effect of single‐dose dexmedetomidine on emergence agitation and recovery profiles after sevoflurane anesthesia in pediatric ambulatory surgery. Journal of anesthesia, 24(5). 675‐ 682 • Sun, L. , & Guo, R. (2014). Dexmedetomidine for preventing sevoflurane‐related emergence agitation in children: a meta‐analysis of randomized controlled trials. Acta Anaesthesiologica Scandinavica, 58(6), 642‐ 650 • Tobias, J. D. (2006). Clinical uses of dexmedetomidine in pediatric anesthesiology and critical care. Seminars in Anesthesia, Perioperative Medicine and Pain. 25(2) 57‐ 64 • Viswanath O, Kerner B, Jean Y‐K, Soto R and Rosen G. (2015) Emergence delirium: a narrative review. Journal of Anesthesiolical Clinical Science. 4(2) • Wagner, D. S. , & Brummett, C. M. (2006). Dexmedetomidine: as safe can be. Seminars in Anesthesia, Perioperative Medicine and Pain. 25(2) 77‐ 83) • Wilson, J. T. (2014). Pharmacologic, physiologic, and psychological characteristics associated with emergence delirium in combat veterans. AANA journal, 82(5) • Yu, M. , Han, C. , Jiang, X. , Wu, X. , Yu, L. , & Ding, Z. (2015). Effect and placental transfer of dexmedetomidine during caesarean section under general anaesthesia. Basic and clinical pharmacology & toxicology. 117(3). 204‐ 208 • Zhang, C. , Hu, J. , Liu, X. , & Yan, J. (2014). Effects of intravenous dexmedetomidine on emergence agitation in children under sevoflurane anesthesia: a meta‐analysis of randomized controlled trials. Plo. S one, 9(6)