Pediatric Disaster Life Support PDLS A Course in



- Slides: 41
Pediatric Disaster © Life Support (PDLS ) A Course in Caring for Children During Disaster Continuing Medical Education University of Massachusetts Medical School
© PDLS : Psychosocial Issues: Children in Disasters
Disasters have Significant Psychological Impact on Children

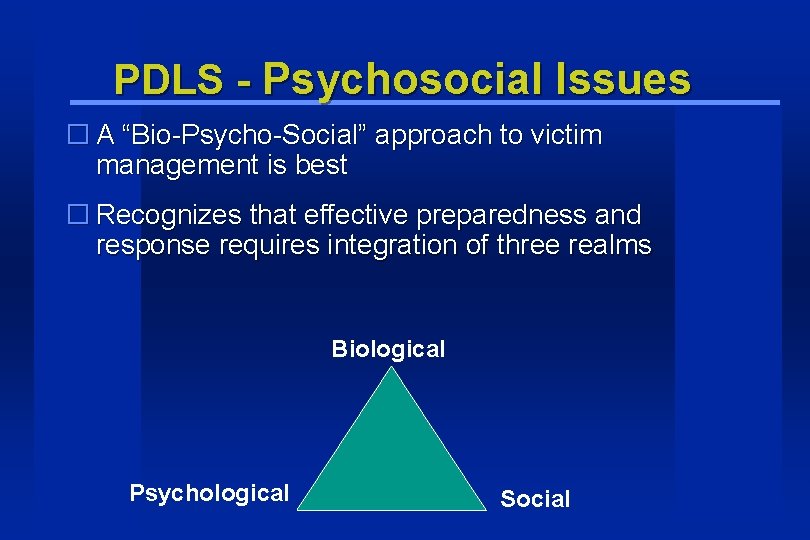
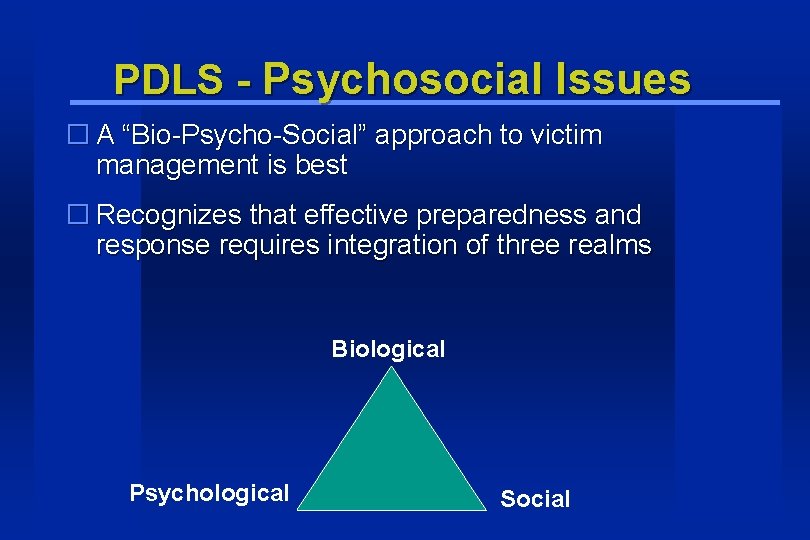
PDLS - Psychosocial Issues � A “Bio-Psycho-Social” approach to victim management is best � Recognizes that effective preparedness and response requires integration of three realms Biological Psychological Social
PDLS - Psychosocial Issues - Anatomy and Physiology unique to children - Focus on vulnerabilities of children, not on resuscitation - Discuss relationship to: Environmental exposure (heat, cold, entrapment) Decontamination Susceptibility to Chemicals, Toxins Behaviors that increase risk Immature immune systems Biological Lack of verbal skills Lack of self-preservation skills
PSYCHOLOGICAL - A child's emotional Response to Disaster - How to anticipate and recognize problems - How long do these disorders last? - Integrating these concepts into disaster preparedness and response plans
SOCIAL - Kids are irreversibly integrated into our society • If children are not accounted for, parents will not comply with officials - Adapting to the concept that children may be intentional targets of terrorism - Role of parents in disaster - Role of media in disaster, a double edged sword - Role of schools, where children spend the bulk of their time away from home - Children routinely cause increased stress in emergency providers

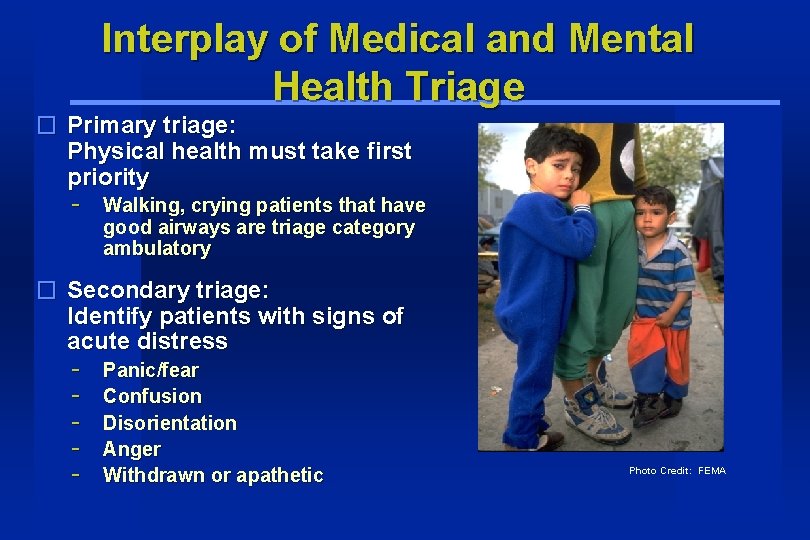
Interplay of Medical and Mental Health Triage � Separate mental health triage and treatment area may be established - Once medically cleared Separate child from adult mental health area Photo Credit: FEMA
Interplay of Medical and Mental Health Triage � Primary triage: Physical health must take first priority - Walking, crying patients that have good airways are triage category ambulatory � Secondary triage: Identify patients with signs of acute distress - Panic/fear Confusion Disorientation Anger Withdrawn or apathetic Photo Credit: FEMA
Infants and severely cognitively disabled don’t understand disaster Provide: § Feeding § Comfort § Familiar caretakers Photo Credit: FEMA
Toddlers, preschoolers and moderately cognitively disabled � Concerned about consequences of disaster � Reactions often are behavioral disturbances, mood changes and anxiety � Can comprehend absence of parents but not the permanence of death Photo Credit: FEMA
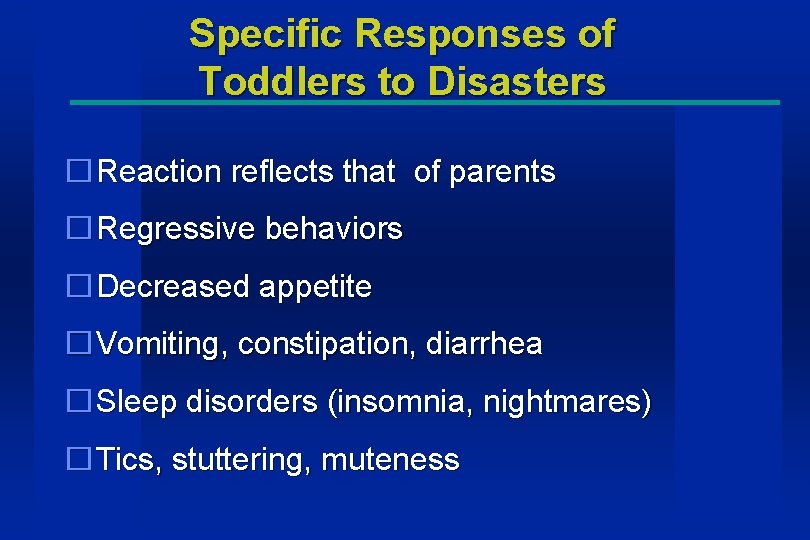
Specific Responses of Toddlers to Disasters �Reaction reflects that of parents �Regressive behaviors �Decreased appetite �Vomiting, constipation, diarrhea �Sleep disorders (insomnia, nightmares) �Tics, stuttering, muteness
Specific Responses of Preschoolers to Disasters �Clinging �Reenactment via play �Exaggerated startle response �Irritability �Posttraumatic stress disorder
Specific Responses of School Age Children to Disasters (5 -12) �Most marked reaction �Fear, anxiety �Increased hostility with siblings �Somatic complaints �Sleep disorders �School problems
School Age Children to Disasters (continued) �Social withdrawal �Reenactment via play �Apathy �Posttraumatic stress disorder �Decreased interest in peers, hobbies, school
Adolescents (13– 19) � Have full understanding of disaster’s causes and consequences � Tend to retain sense of omnipotence, boys > girls � May suffer depression and anxiety � May be aggressive to self or others, risk of suicide � May become sullen and withdrawn Photo Credit: FEMA
Specific Responses of Adolescents to Disasters � Decreased interest in social activities, peers, hobbies, school � Anhedonia (inability to experience pleasure) � Decline in responsible behaviors � Rebellion, behavior problems � Somatic complaints � Sleep disorders
Adolescents Response to Disasters (continued) �Eating disorders �Change in physical activity �Confusion �Lack of concentration �Risk-taking behaviors

Stress response in children �“Fight or flight” �Adrenaline/epinephrine mediated �Arousal state �Increased startle, response, agitation �Increased heart rate, respiratory rate, blood pressure
Alternate stress response �“Freeze and hide” �Vagal nerve stimulus �Opposite of “fight or flight” �Blunted reactions, affect, responses �Lowered heart rate, respiratory rate, blood pressure �Syncope may result
Short term reactions �Disbelief �Denial �Anxiety �Grief �Altruism �Relief
Short-term reactions �Grief, loss, anger, guilt �Coping strategies - Regression – loss of developmental milestones - Clinging and increased dependency - Helpfulness – more useful in older children - Acting out – competing for attention
Second Stage: Immediate Post. Event Period Time �A few days to several weeks after disaster Reaction �Clinging, appetite changes, regressive symptoms, somatic complaints, sleep disturbances, apathy, depression, anger, and hostile delinquent acts
Aggressive/Defiant Behavior �Toddlers and preschoolers may exhibit hostile behaviors such as hitting and biting. �School age children may get involved in peer fights. �Adolescence may become delinquent or rebellious.
Aggressive/Defiant Behavior (continued) Recommendations �For the younger child, limit setting may be of help. �With adolescents, involving them in the rebuilding of the community or helping with younger children or elderly may aid recovery.
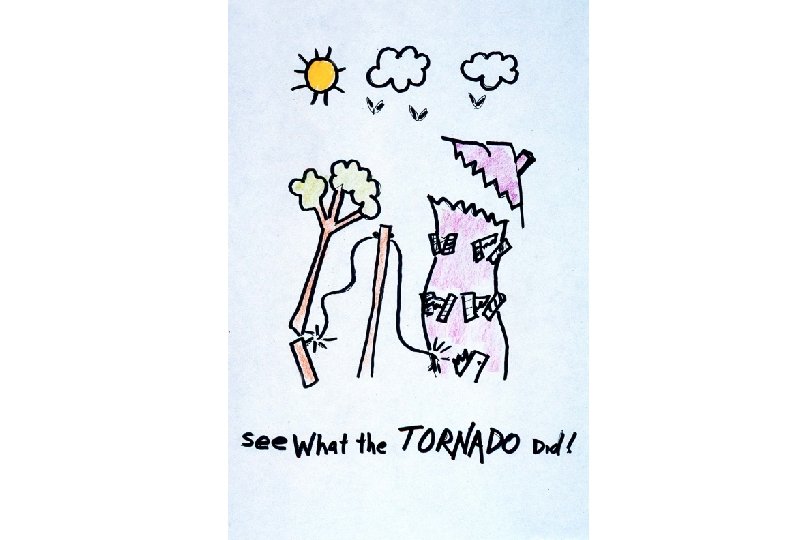
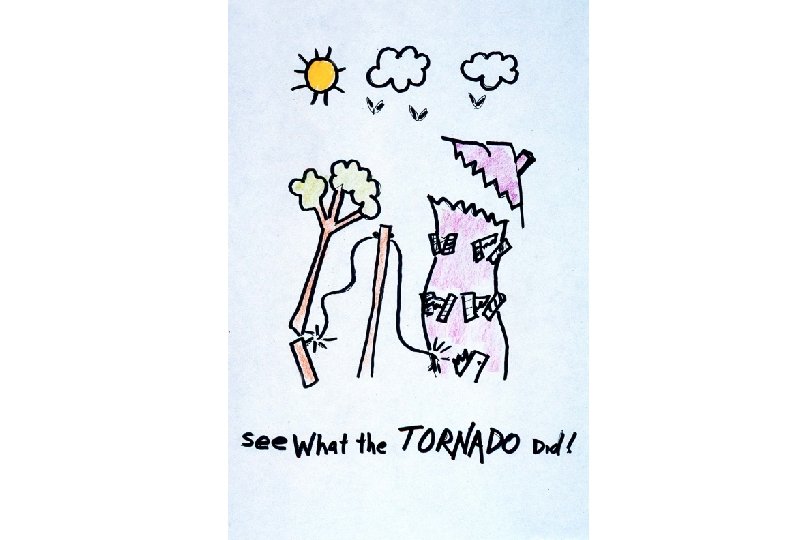
Repetitious Behavior �Most commonly seen in toddlers and preschoolers after disaster. �These children will reenact crucial details of the disaster. �Other repetitive behaviors are recurrent nightmares and frequent flashbacks. �The Healthcare worker should allow the child or preschooler to reenact the events as these are therapeutic and can help in recovery.
Somatic Symptoms �These include headaches, abdominal pain, and chest pain and are commonly observed in children and adolescents. �Reassurance by the healthcare worker can be of help after evaluation. �Counseling and mental health intervention may be necessary for the victims as well as the Healthcare workers.
Delayed Post-event Period (months) � Depression - More likely to manifest sleep, somatic and behavioral symptoms than adults Family and personal history of depression increase risk Exacerbated by re-exposure to venue of or media
Delayed Post-event Period � Post-Traumatic Stress Disorder (PTSD) - An anxiety disorder with psychological and physical symptoms including: Intrusive thoughts, memories and nightmares Exacerbation by anniversaries and reminders of the event Aggression, anger and fear Apathy, numbness
Delayed Post-event Period � Children have special susceptibility to certain risk factors - Witnessing terror in parents and loved ones - Repeated exposure to media of the disaster Photo Credit: FEMA � Little data about preventing and treating PTSD in children
People with Special Healthcare Needs (PSHCN) Cognitive and/or Emotional Disabilities � Reaction to disaster similar to typical children with important differences � May be and feel particularly vulnerable due to technology dependence and impaired mobility - Cognitively impaired children may respond similarly to chronologically younger children Emotionally disabled children are at increased risk for acute and chronic negative disaster responses Photo Credit: FEMA
Caring for Disaster Mental Health Adapted mental health first aid: Strategy for identifying children in need of help �Introduce yourself in a developmentally appropriate way �Explain that you are trying to help �Remain non-threatening but be honest and direct - Preserve credibility Avoid unrealistic promises or false statements Photo Credit: FEMA
Caring for Disaster Mental Health �Listen for anxiety, fear about location of care-takers and immediate needs - Acknowledge the child’s emotions Give reassurance and information �If available, guide child to mental health triage/treatment facility �Encourage self-help strategies - Guided imagery Exercise Preservation of routine
Caring For Disaster Mental Health �Play �Home �Drawings �Nightmares Guided play/imagery to take control of scenario and make a happy ending.
Caring For Disaster Mental Health Treatment/Recommendations � Parents, teachers, and Healthcare workers should create and maintain a predictable schedule for children. � Night lights, stuffed animals, and reassurance are helpful. � Compassion is helpful but punishment is not. � Consultation with psychiatrist or psychiatric social worker may be a benefit.
Responding to children’s needs �Parents should know age appropriate responses �Monitor and limit media exposure to disaster coverage �Early counseling may reduce long term negative effects
Responding to children’s needs �Rehearsal of plan reduces anxiety and gives a sense of control - Rehearsal of plan with a live drill that has children acting out roles Step #1 exercise – school bus accident Step #2 exercise – school evacuation
Normal Recovery �Talking with others �Coping mechanisms - Learning healthy mechanisms �Counseling