PEDIATRIC CRRT THE PRESCRIPTION RATES DOSE FLUIDS Michael
- Slides: 20
PEDIATRIC CRRT THE PRESCRIPTION : RATES , DOSE, FLUIDS Michael Zappitelli, MD, MSc Montreal Children's Hospital Mc. Gill University Health Centre
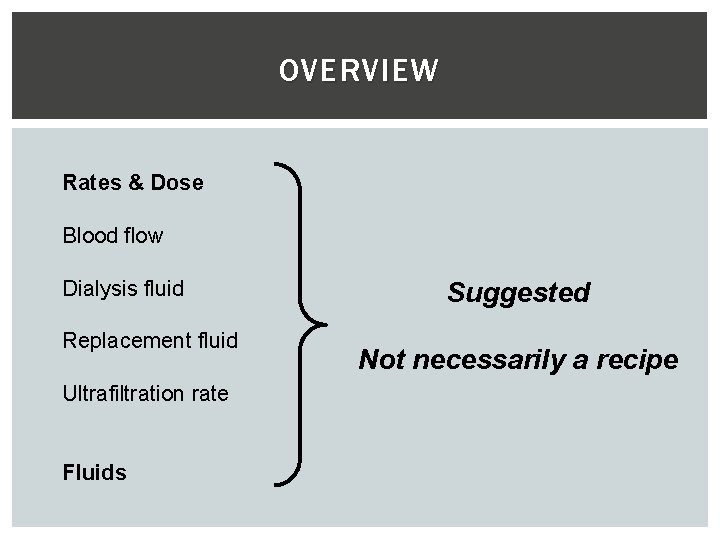
OVERVIEW Rates & Dose Blood flow Dialysis fluid Replacement fluid Ultrafiltration rate Fluids Suggested Not necessarily a recipe
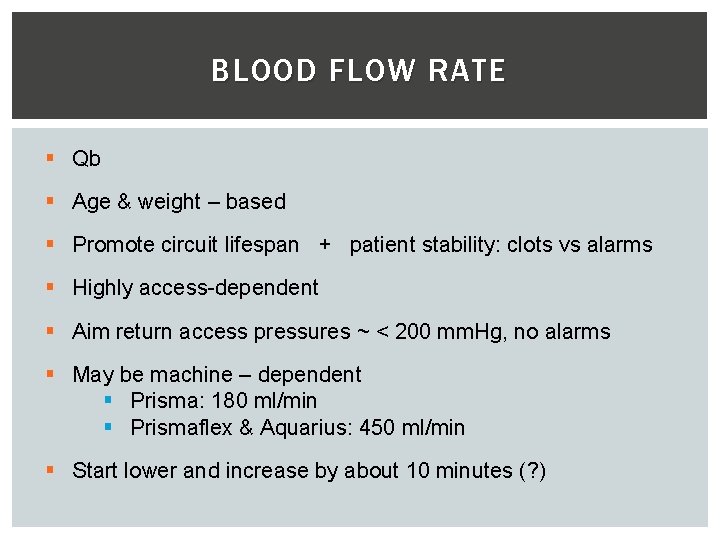
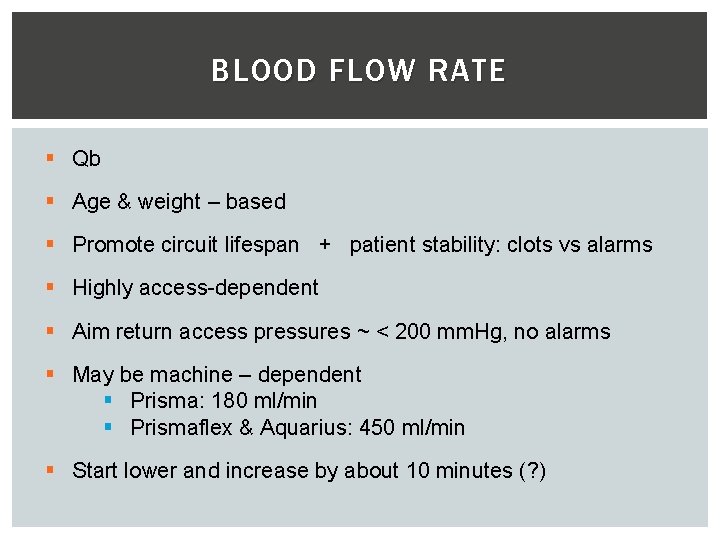
BLOOD FLOW RATE § Qb § Age & weight – based § Promote circuit lifespan + patient stability: clots vs alarms § Highly access-dependent § Aim return access pressures ~ < 200 mm. Hg, no alarms § May be machine – dependent § Prisma: 180 ml/min § Prismaflex & Aquarius: 450 ml/min § Start lower and increase by about 10 minutes (? )
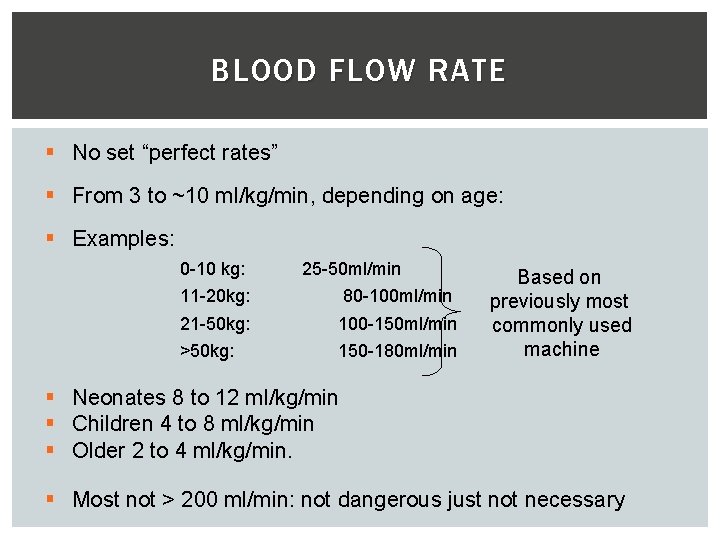
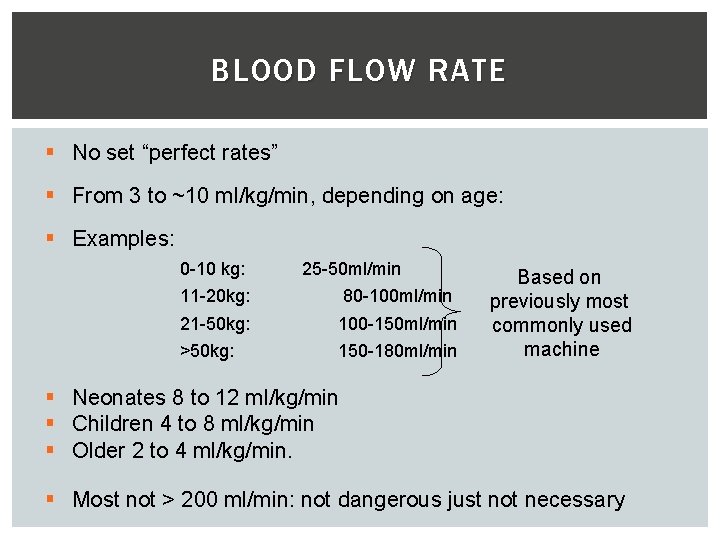
BLOOD FLOW RATE § No set “perfect rates” § From 3 to ~10 ml/kg/min, depending on age: § Examples: 0 -10 kg: 25 -50 ml/min 11 -20 kg: 80 -100 ml/min 21 -50 kg: 100 -150 ml/min >50 kg: 150 -180 ml/min Based on previously most commonly used machine § Neonates 8 to 12 ml/kg/min § Children 4 to 8 ml/kg/min § Older 2 to 4 ml/kg/min. § Most not > 200 ml/min: not dangerous just not necessary
BLOOD FLOW RATE § May need to modify: § Be aware of access and return pressure § Visually inspect filter for clots § Transmembrane pressure – may need to increase blood flow § Filtration fraction
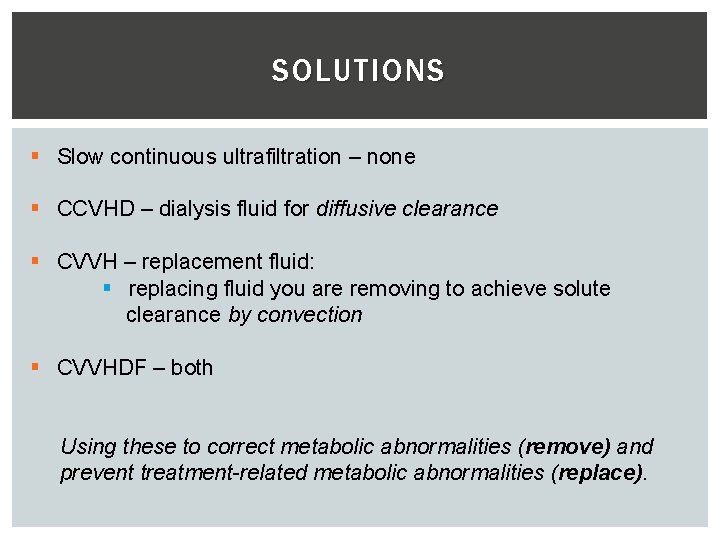
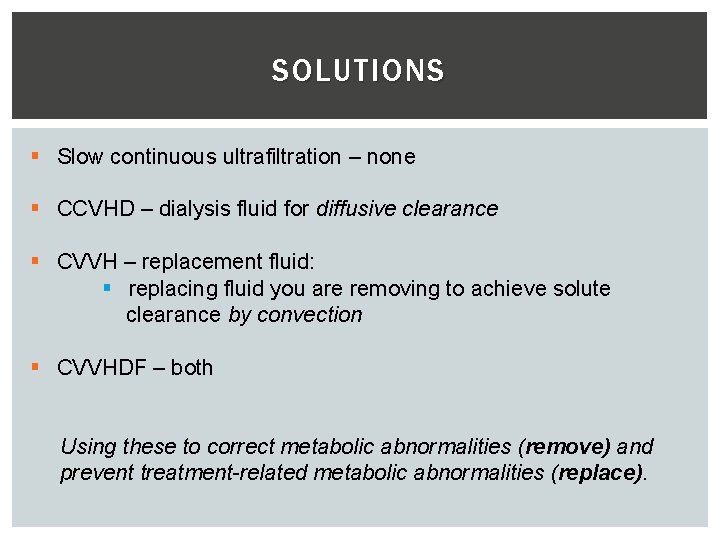
SOLUTIONS § Slow continuous ultrafiltration – none § CCVHD – dialysis fluid for diffusive clearance § CVVH – replacement fluid: § replacing fluid you are removing to achieve solute clearance by convection § CVVHDF – both Using these to correct metabolic abnormalities (remove) and prevent treatment-related metabolic abnormalities (replace).
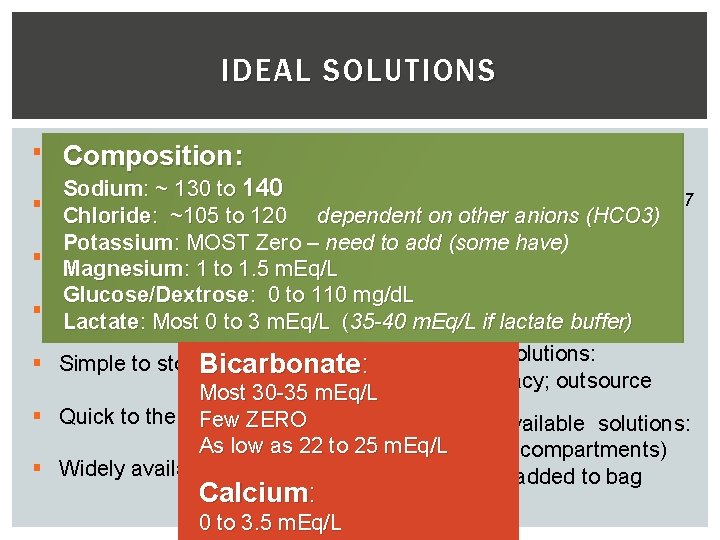
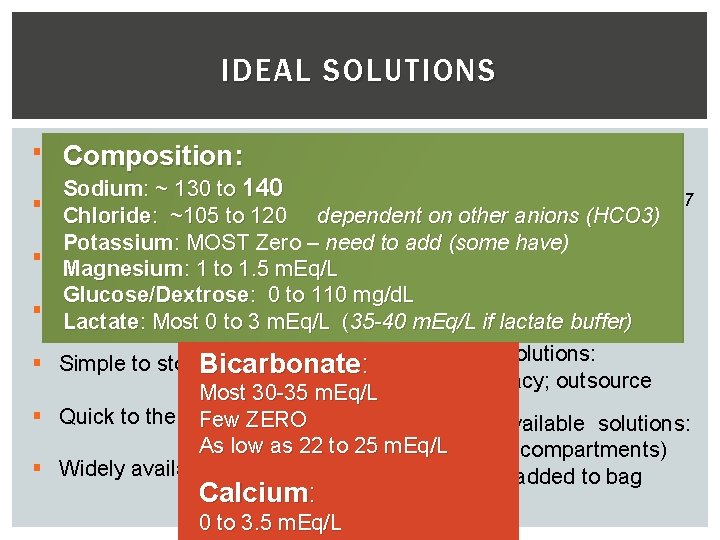
IDEAL SOLUTIONS § Physiological/ compatible Composition : § § § § Peritoneal dialysis fluid? § Hyperglycemia, metab acidosis Sodium: ~ 130 to 140 Soysal et al, Ped Neph, 2007 Reliable Chloride: ~105 to 120 dependent on other anions (HCO 3) § Pre-made IV solutions: Potassium: MOST Zero – need to add (some have) Inexpensive Magnesium: 1 to 1. 5 m. Eq/L § Saline, Lactated Ringers Glucose/Dextrose: 0 to 110 mg/d. L Easy to prepare Multi-bag systems: why? Lactate : Most 0 to 3 m. Eq/L §(35 -40 m. Eq/L if lactate buffer) § Custom-made solutions: Simple to store. Bicarbonate : § Local pharmacy; outsource Most 30 -35 m. Eq/L Quick to the bedside Few ZERO § Commercially available solutions: As low as 22 to 25 § m. Eq/L Ready-bags (compartments) Widely available § Concentrate added to bag Calcium: 0 to 3. 5 m. Eq/L
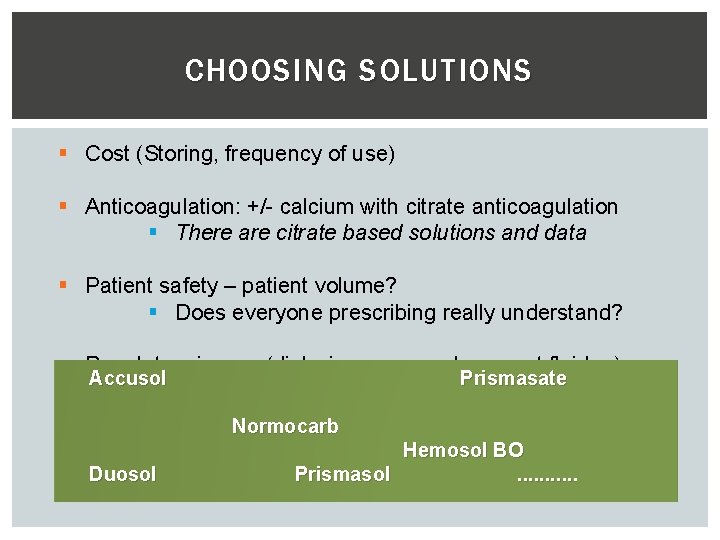
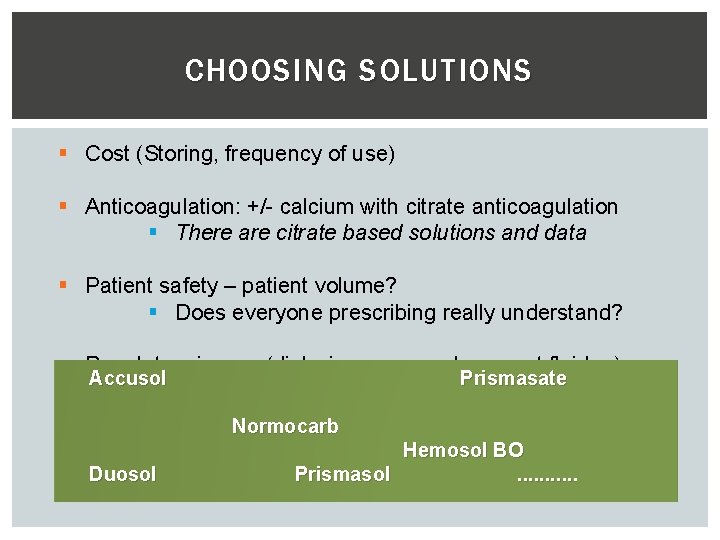
CHOOSING SOLUTIONS § Cost (Storing, frequency of use) § Anticoagulation: +/- calcium with citrate anticoagulation § There are citrate based solutions and data § Patient safety – patient volume? § Does everyone prescribing really understand? § Regulatory issues (dialysis versus replacement fluid. . ) Accusol Prismasate Some solutions are more flexible than others Normocarb Duosol Hemosol BO Prismasol. . .
PHOSPHATE § They WILL develop hypophosphatemia § Can replace: IV boluses, TPN § MANY add it to solutions – but no good data § Worry about precipitation, calcium-magnesium binding § How much too much? No good answer. Many 1. 2 -1. 5 mmol/L § Pharmacy versus nurse-based addition?
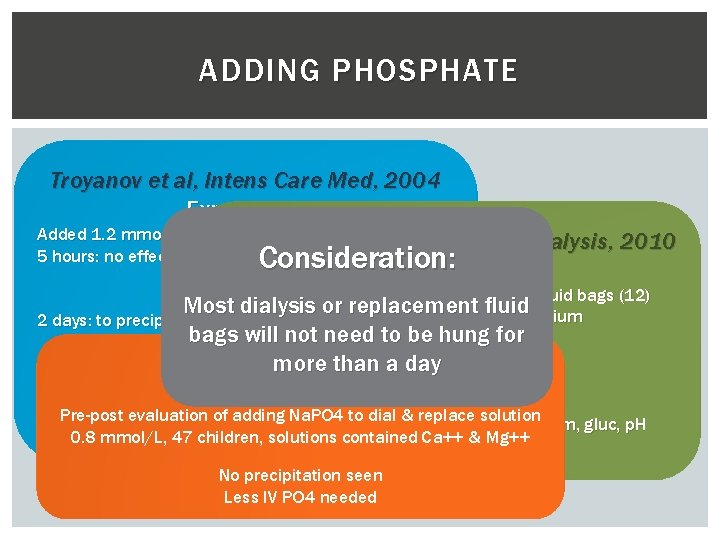
ADDING PHOSPHATE Troyanov et al, Intens Care Med, 2004 Experiment Added 1. 2 mmol/L PO 4 to calciumet – rich Santiago al, solutions Therap Apher & Dialysis, 2010 5 hours: no effect on calcium, Consideration: bicarb, p. H, p. CO 2 No visual precipitation Experiment Added Na. PO 4 to dialysis/replacement fluid bags (12) With and without filtering Most dialysis or replacement containing calcium andfluid magnesium 2 days: to precipitation bags will not need to 0. 8 bemmol/L hung for mmol/L Retrospective clinical Santiago more et al, KI, 2009 than a 1. 5 day 2. 5 mmol/L 14 adults CVVHDF Experiment KPO 4 addedevaluation when <1. 5 ofmmol/L (protocolized) Pre-post adding Na. PO 4 to dial & magnesium, replace solution No change inbicarb, calcium, sodium, gluc, p. H No negative effects caused on calcium, p. H 0. 8 mmol/L, 47 children, solutions contained Ca++ & Mg++ 2, 24 and 48 hours No precipitation seen Less IV PO 4 needed
DIALYSIS FLUID? REPLACEMENT FLUID ? § Personal suggestion: use the same solution § If needed (e. g. alkalosis) can modify the replacement solution § Regulatory issues may hinder: § Replacement solution – saline, with additives
ALBUMIN DIALYSIS § Removes protein bound small substances: § e. g. copper/Wilson's, drugs, toxins of liver failure § Albumin live a scavenger Dialysis: § albumin-containing solution across highly permeable membrane § 25% albumin “added” to dialysis fluid bag: 2 -5% albumin solution § it's “single pass” - bags are changed § Shouldn't affect sodium – may affect (reduce) other electrolytes § Theoretically may affect citrate anticoagg rates § Allergic reaction Collins et al, Pediatr Nephrol, 2008 Askenazi et al, Pediatrics, 2004 Ringe, Pediatr Crit Care Med, 2011
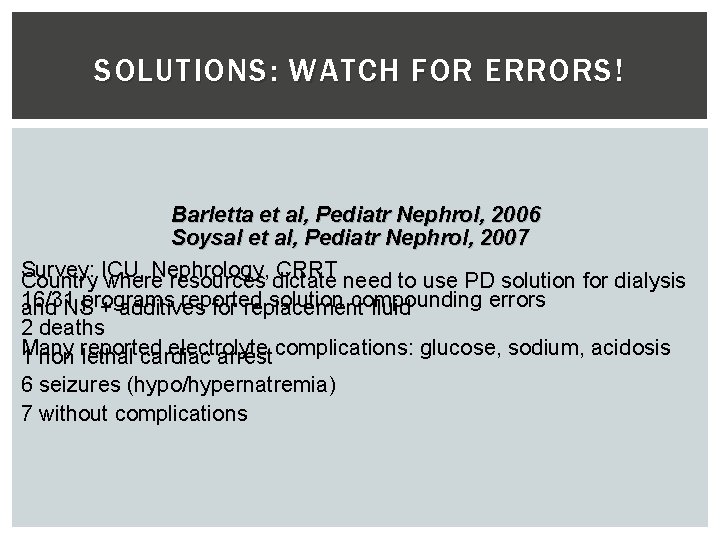
SOLUTIONS: WATCH FOR ERRORS ! Barletta et al, Pediatr Nephrol, 2006 Soysal et al, Pediatr Nephrol, 2007 Survey: Nephrology, CRRT need to use PD solution for dialysis Country ICU, where resources dictate 16/31 programs reported solution compounding errors and NS + additives for replacement fluid 2 deaths Many electrolyte 1 non reported lethal cardiac arrest complications: glucose, sodium, acidosis 6 seizures (hypo/hypernatremia) 7 without complications
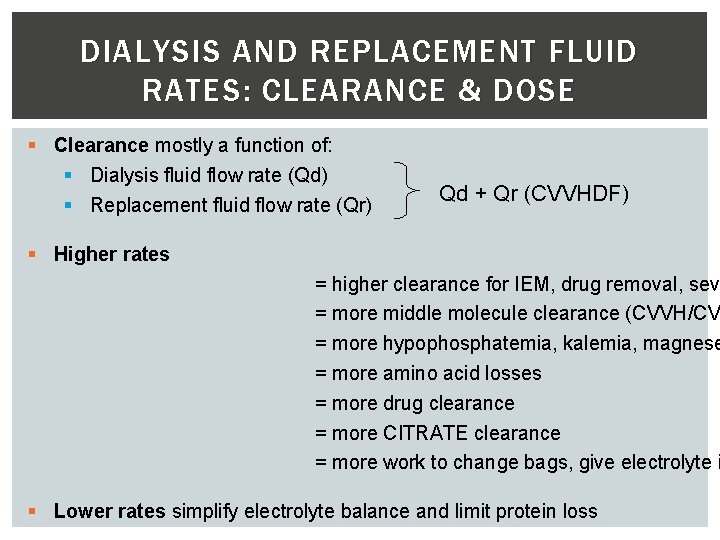
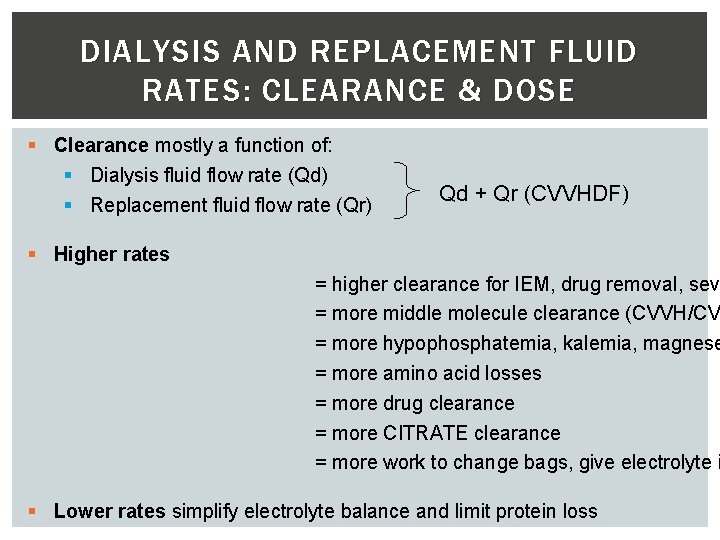
DIALYSIS AND REPLACEMENT FLUID RATES: CLEARANCE & DOSE § Clearance mostly a function of: § Dialysis fluid flow rate (Qd) § Replacement fluid flow rate (Qr) Qd + Qr (CVVHDF) § Higher rates = higher clearance for IEM, drug removal, seve = more middle molecule clearance (CVVH/CV = more hypophosphatemia, kalemia, magnese = more amino acid losses = more drug clearance = more CITRATE clearance = more work to change bags, give electrolyte i § Lower rates simplify electrolyte balance and limit protein loss
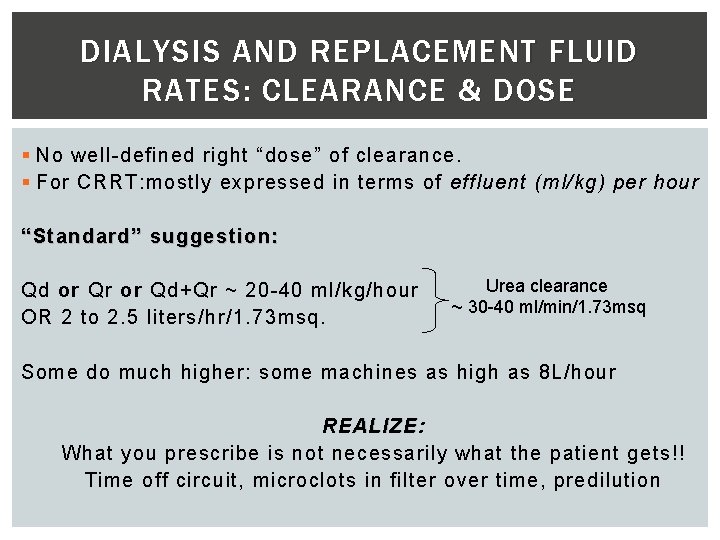
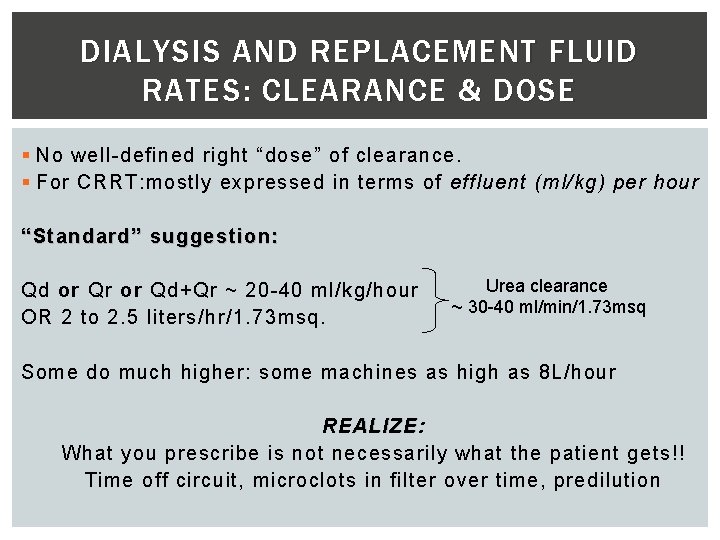
DIALYSIS AND REPLACEMENT FLUID RATES: CLEARANCE & DOSE § No well-defined right “dose” of clearance. § For CRRT: mostly expressed in terms of effluent (ml/kg) per hour “Standard” suggestion : Qd or Qr or Qd+Qr ~ 20 -40 ml/kg/hour OR 2 to 2. 5 liters/hr/1. 73 msq. Urea clearance ~ 30 -40 ml/min/1. 73 msq Some do much higher: some machines as high as 8 L/hour REALIZE: What you prescribe is not necessarily what the patient gets!! Time off circuit, microclots in filter over time, predilution
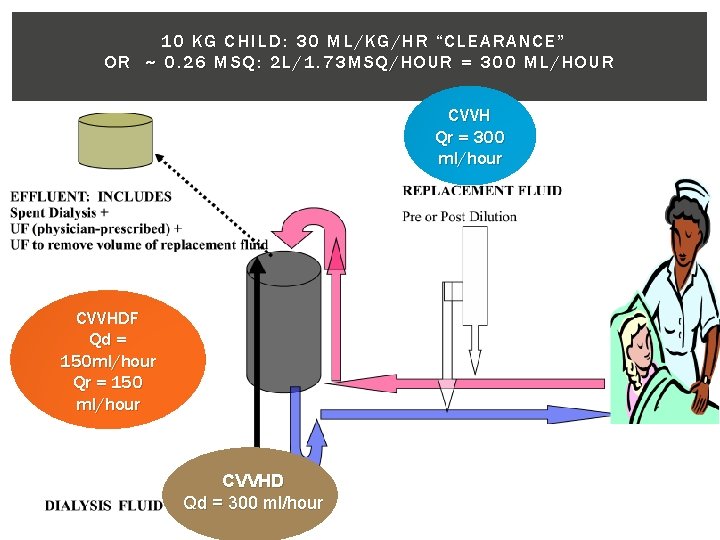
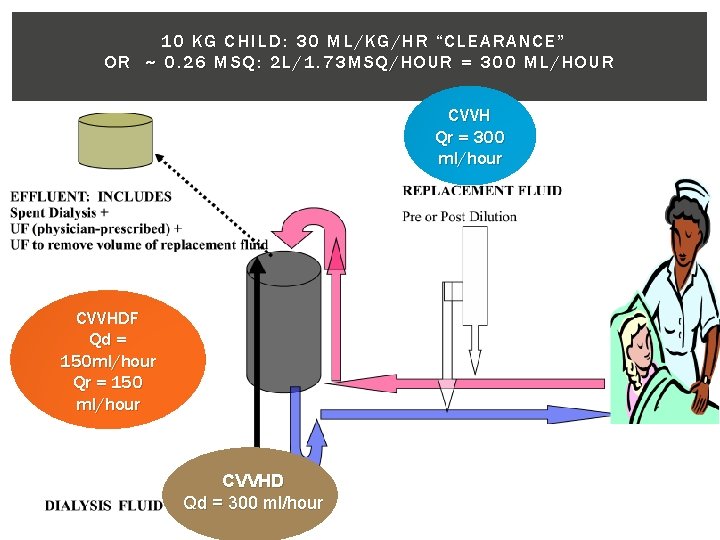
10 KG CHILD: 30 ML/KG/HR “CLEARANCE” OR ~ 0. 26 MSQ: 2 L/1. 73 MSQ/HOUR = 300 ML/HOUR CVVH Qr = 300 ml/hour CVVHDF Qd = 150 ml/hour Qr = 150 ml/hour CVVHD Qd = 300 ml/hour
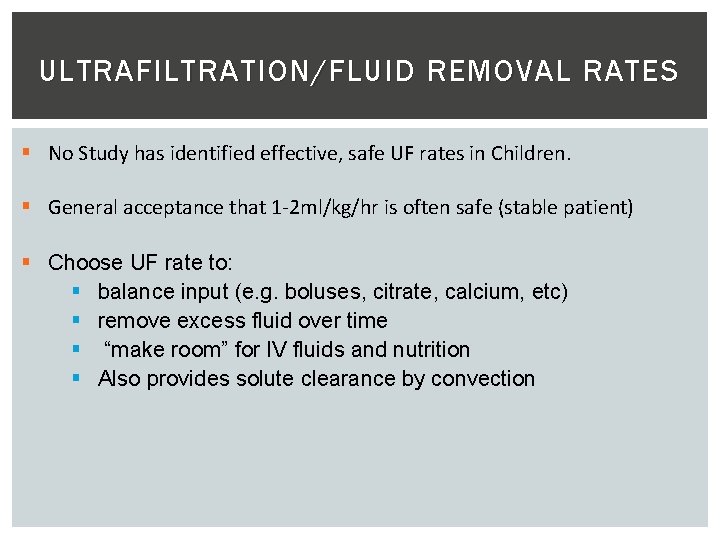
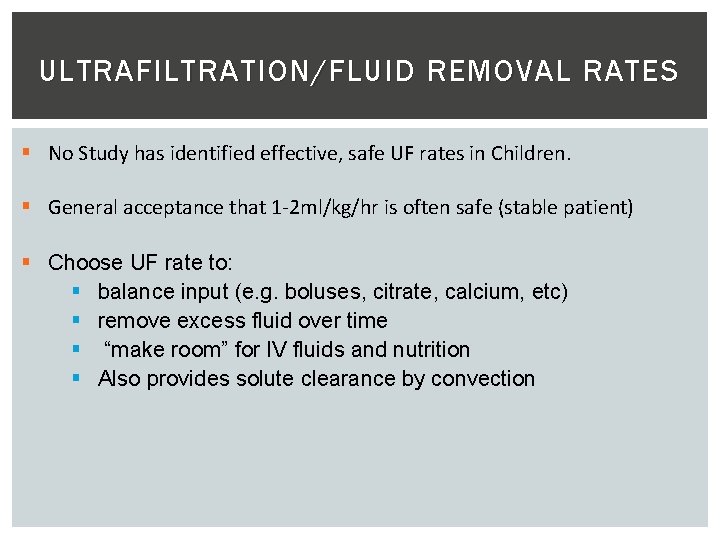
ULTRAFILTRATION/FLUID REMOVAL RATES § No Study has identified effective, safe UF rates in Children. § General acceptance that 1 -2 ml/kg/hr is often safe (stable patient) § Choose UF rate to: § balance input (e. g. boluses, citrate, calcium, etc) § remove excess fluid over time § “make room” for IV fluids and nutrition § Also provides solute clearance by convection
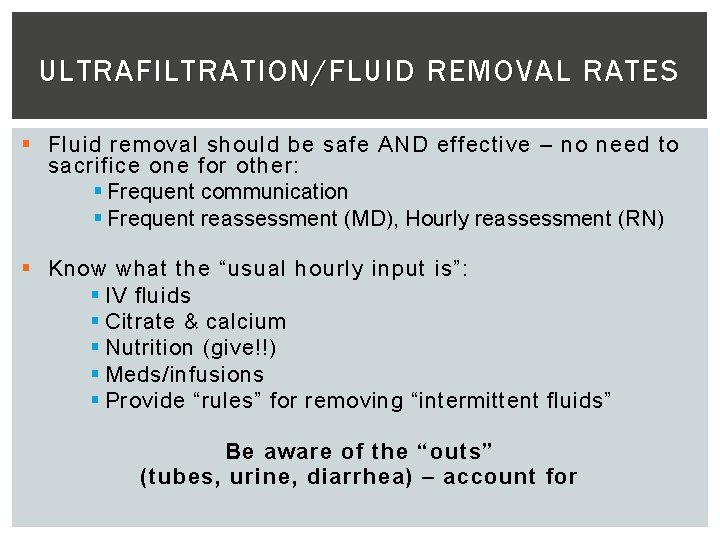
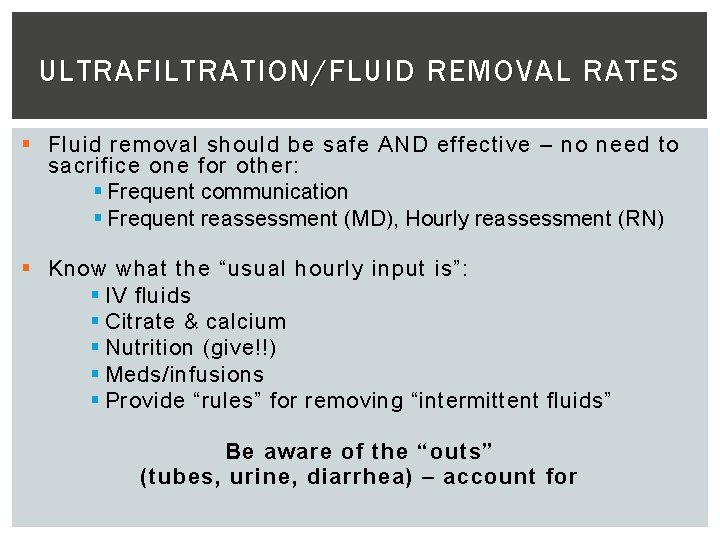
ULTRAFILTRATION/FLUID REMOVAL RATES § Fluid removal should be safe AND effective – no need to sacrifice one for other: § Frequent communication § Frequent reassessment (MD), Hourly reassessment (RN) § Know what the “usual hourly input is”: § IV fluids § Citrate & calcium § Nutrition (give!!) § Meds/infusions § Provide “rules” for removing “intermittent fluids” Be aware of the “outs” (tubes, urine, diarrhea) – account for
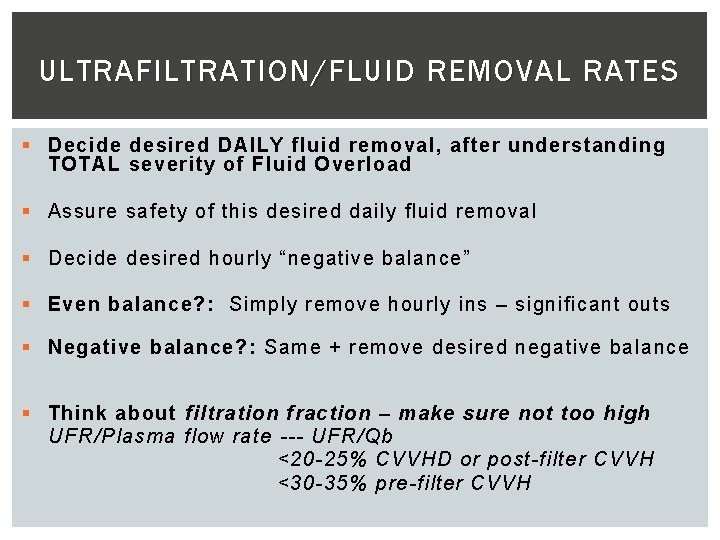
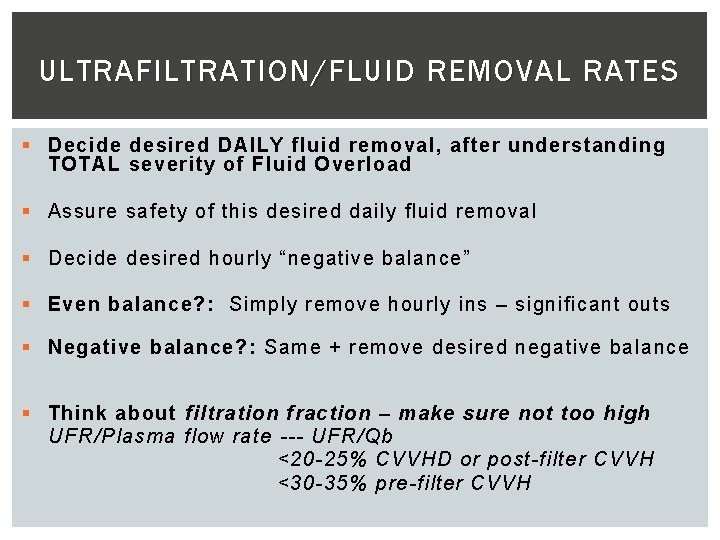
ULTRAFILTRATION/FLUID REMOVAL RATES § Decide desired DAILY fluid removal, after understanding TOTAL severity of Fluid Overload § Assure safety of this desired daily fluid removal § Decide desired hourly “negative balance” § Even balance? : Simply remove hourly ins – significant outs § Negative balance? : Same + remove desired negative balance § Think about filtration fraction – make sure not too high UFR/Plasma flow rate --- UFR/Qb <20 -25% CVVHD or post-filter CVVH <30 -35% pre-filter CVVH
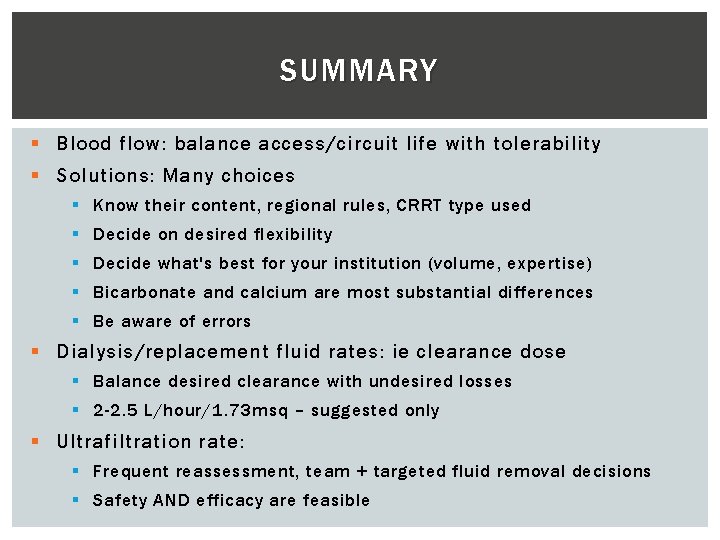
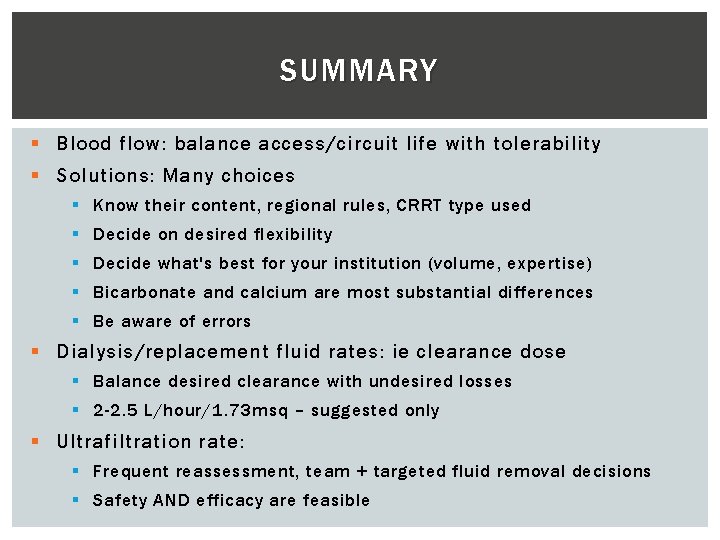
SUMMARY § Blood flow: balance access/circuit life with tolerability § Solutions: Many choices § Know their content, regional rules, CRRT type used § Decide on desired flexibility § Decide what's best for your institution (volume, expertise) § Bicarbonate and calcium are most substantial differences § Be aware of errors § Dialysis/replacement fluid rates: ie clearance dose § Balance desired clearance with undesired losses § 2 -2. 5 L/hour/1. 73 msq – suggested only § Ultrafiltration rate: § Frequent reassessment, team + targeted fluid removal decisions § Safety AND efficacy are feasible