Pediatric Concepts Review Pediatric Airway Management Anatomical differences
- Slides: 27
Pediatric Concepts Review
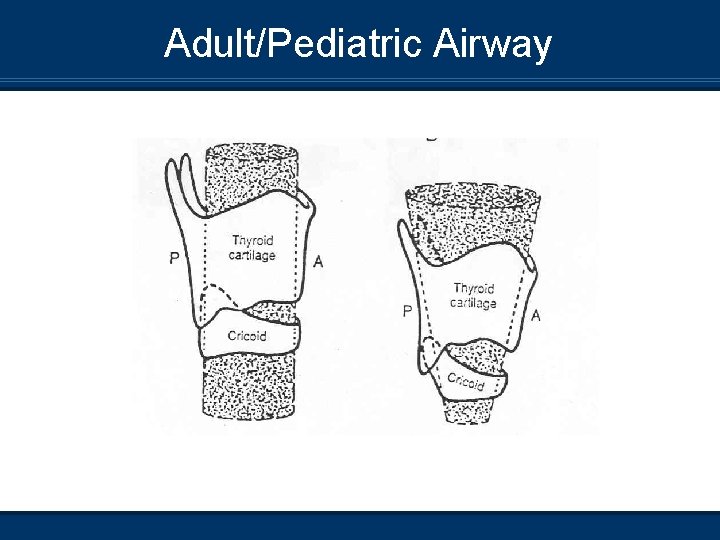
Pediatric Airway Management Anatomical differences n n n Large occiput Larger tongue compared to oropharygeal space Narrowest portion subglottic (cricoid funnel-shaped vs. cylinderical) Epiglottis typically floppier, articulates at a more acute angle with the larynx Larynx more anterior and cephalad (glottis C 3 -4 vs C 5 adult) Cords more inclined compared to flat
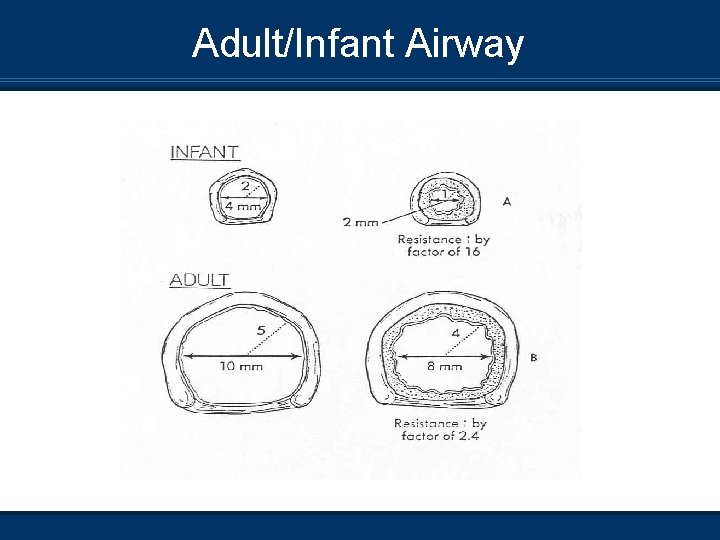
Differences cont. n Ribs more horizontal, loss of “bucket-handle” effect n Cartilage more compliant, with resp. distress the chest wall may actually retract n Predominantly nose breathers n Cartilage not fully formed, “floppy” n Smaller relative internal diameter of both upper and lower airways predisposes the child to higher Aw resistance
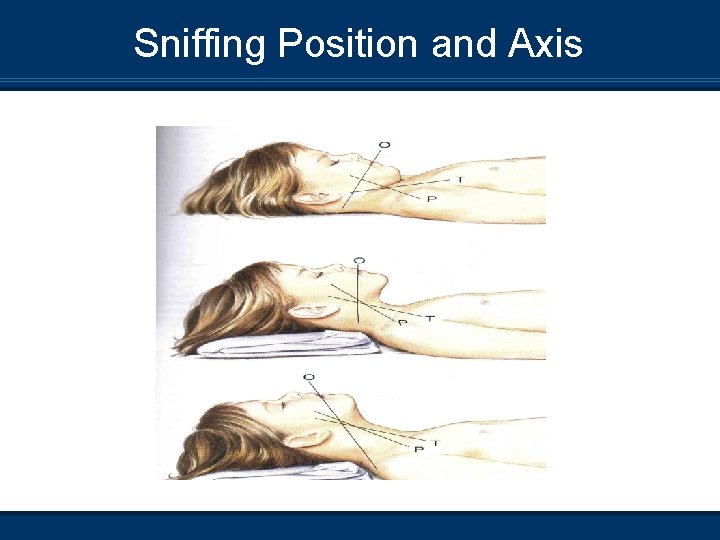
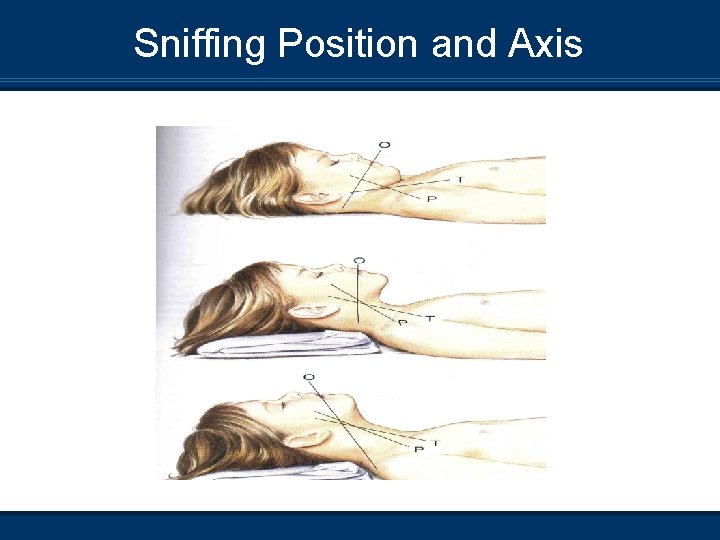
Sniffing Position and Axis
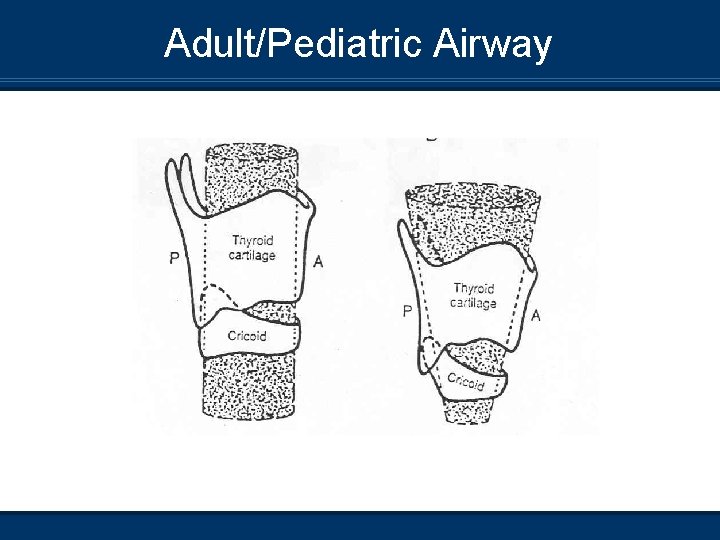
Adult/Pediatric Airway
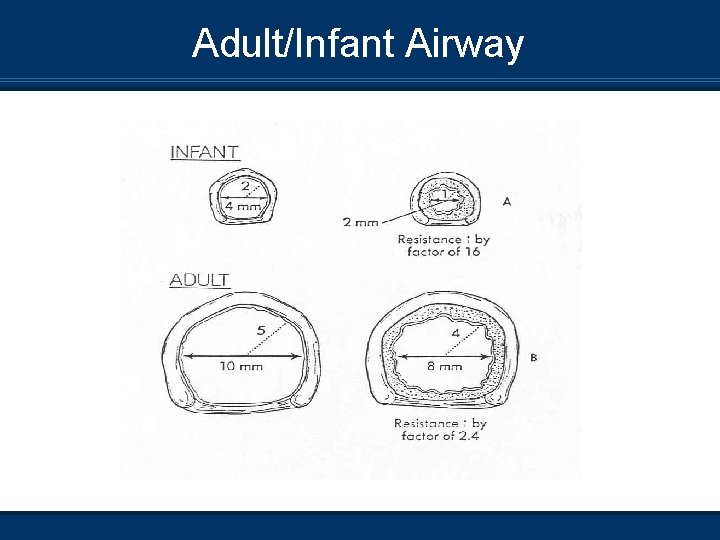
Adult/Infant Airway
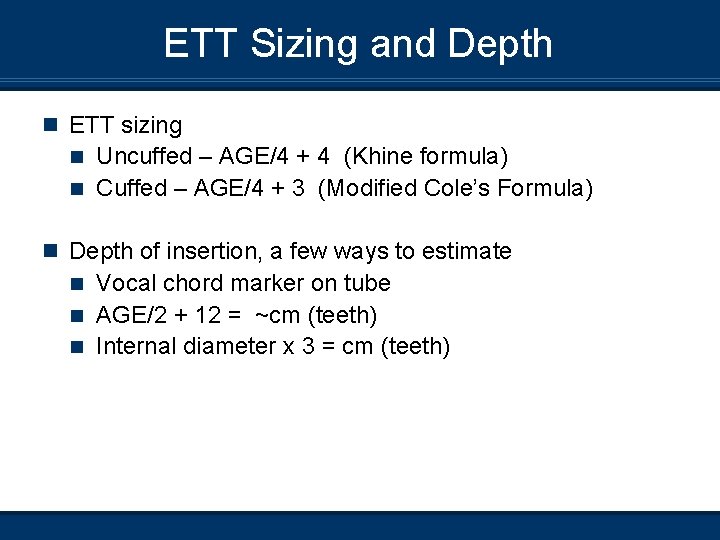
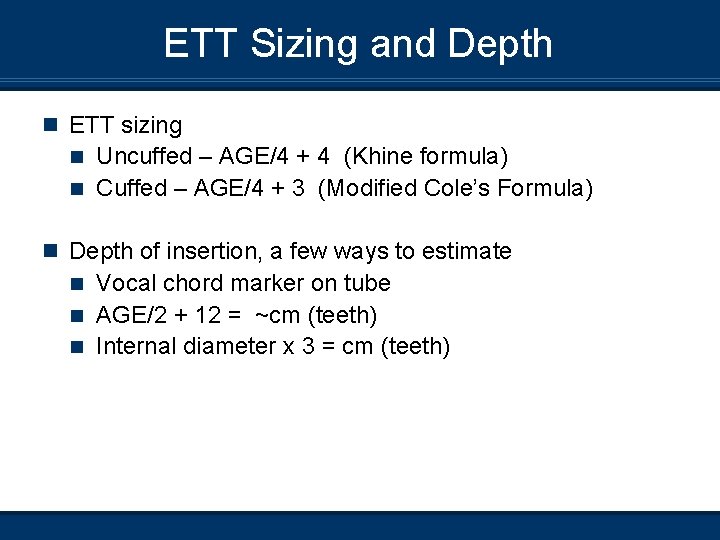
ETT Sizing and Depth n ETT sizing Uncuffed – AGE/4 + 4 (Khine formula) n Cuffed – AGE/4 + 3 (Modified Cole’s Formula) n n Depth of insertion, a few ways to estimate Vocal chord marker on tube n AGE/2 + 12 = ~cm (teeth) n Internal diameter x 3 = cm (teeth) n
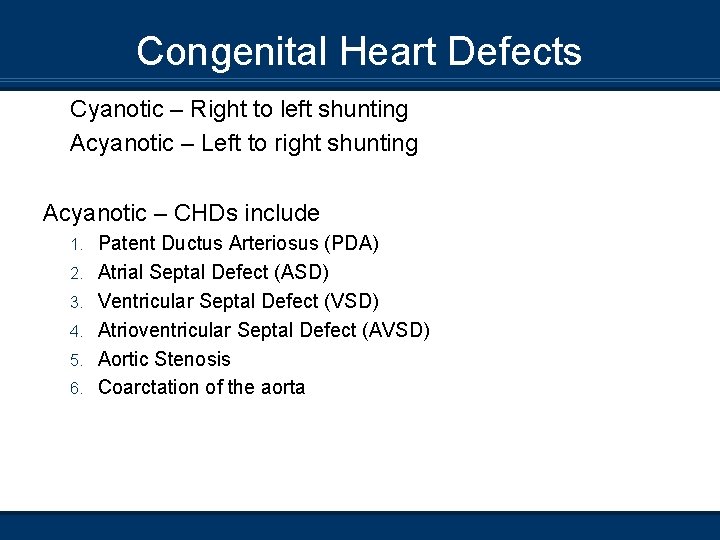
Congenital Heart Defects Cyanotic – Right to left shunting Acyanotic – Left to right shunting Acyanotic – CHDs include 1. 2. 3. 4. 5. 6. Patent Ductus Arteriosus (PDA) Atrial Septal Defect (ASD) Ventricular Septal Defect (VSD) Atrioventricular Septal Defect (AVSD) Aortic Stenosis Coarctation of the aorta
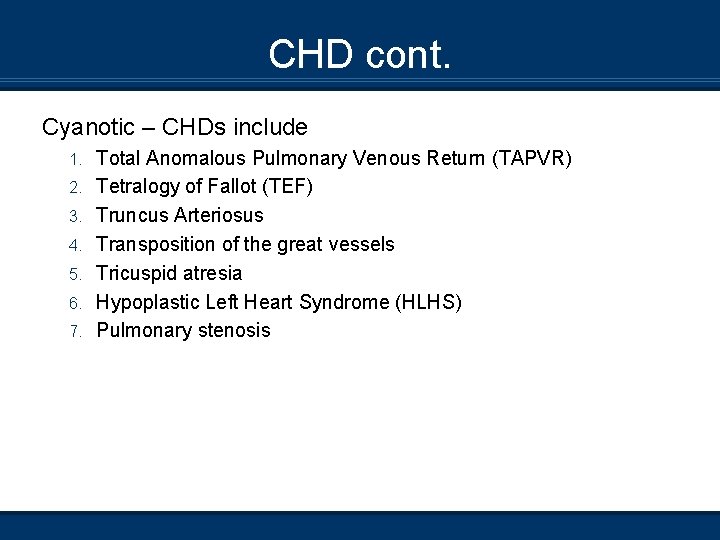
CHD cont. Cyanotic – CHDs include 1. 2. 3. 4. 5. 6. 7. Total Anomalous Pulmonary Venous Return (TAPVR) Tetralogy of Fallot (TEF) Truncus Arteriosus Transposition of the great vessels Tricuspid atresia Hypoplastic Left Heart Syndrome (HLHS) Pulmonary stenosis
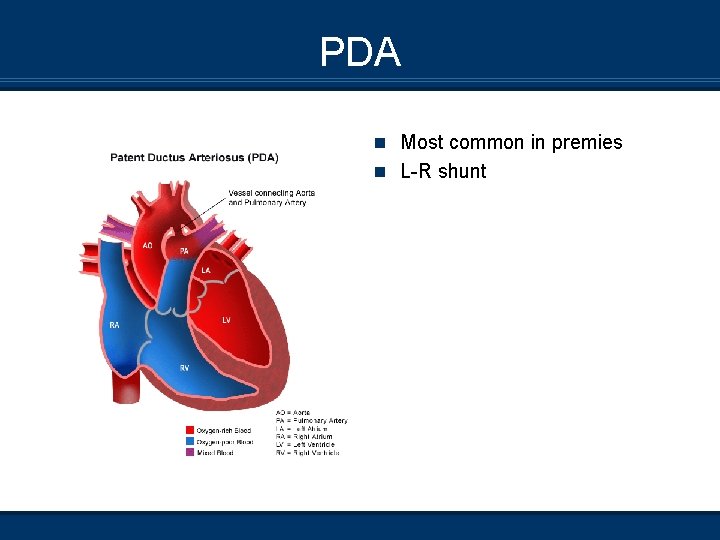
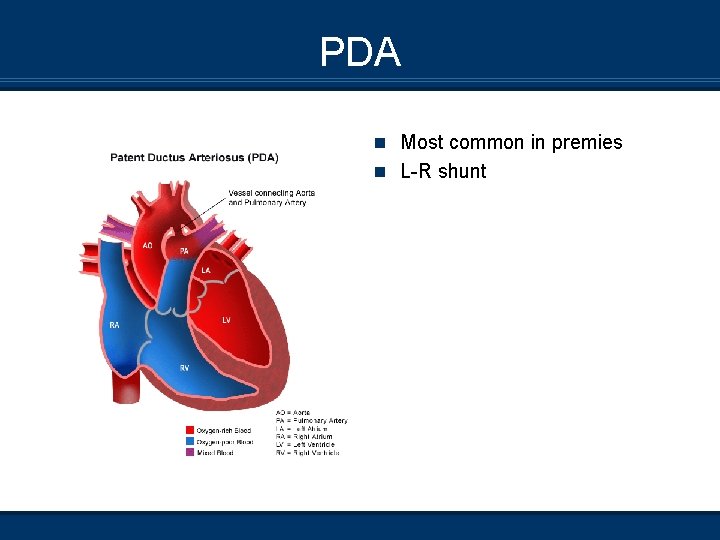
PDA n Most common in premies n L-R shunt
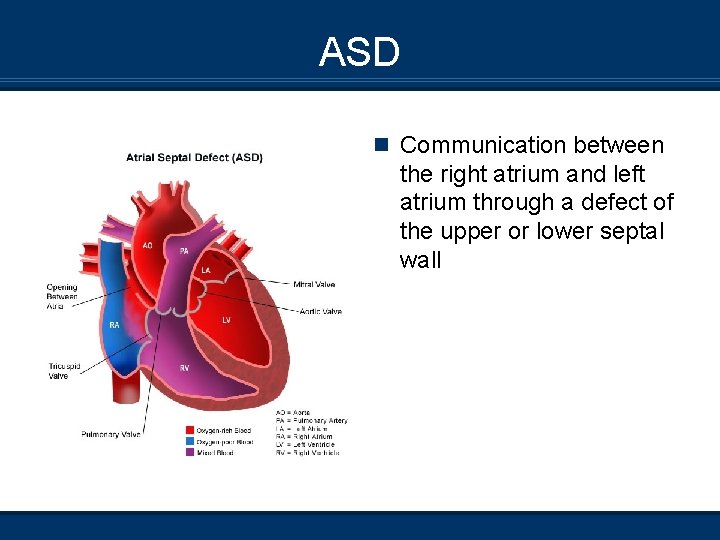
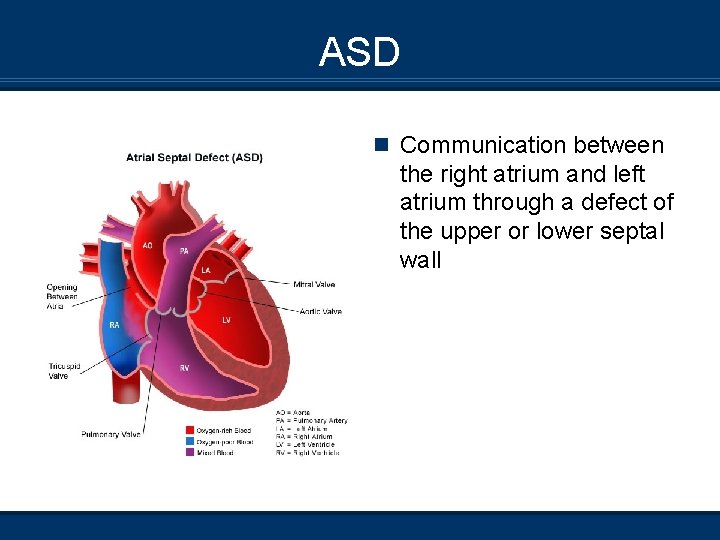
ASD n Communication between the right atrium and left atrium through a defect of the upper or lower septal wall
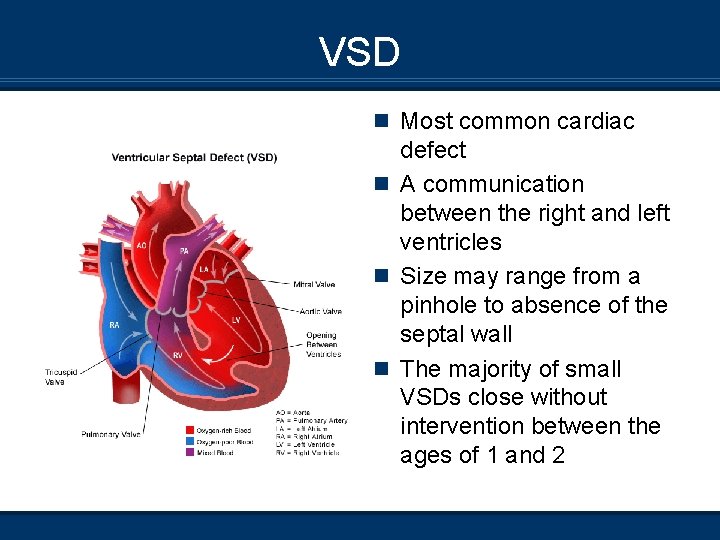
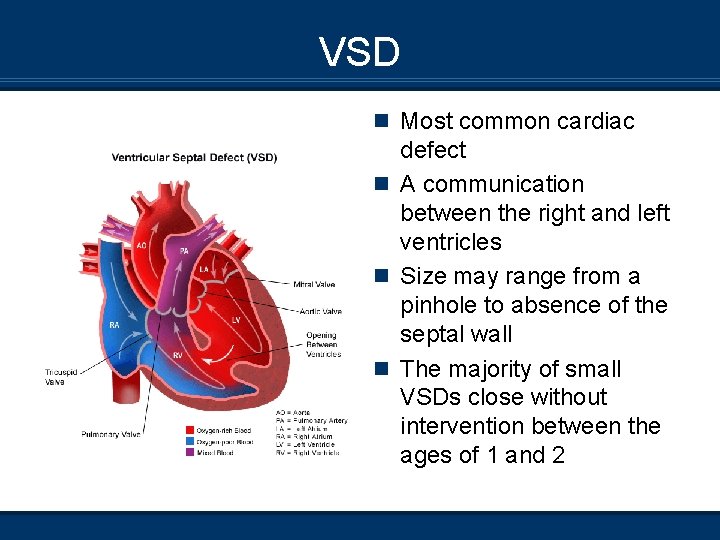
VSD n Most common cardiac defect n A communication between the right and left ventricles n Size may range from a pinhole to absence of the septal wall n The majority of small VSDs close without intervention between the ages of 1 and 2
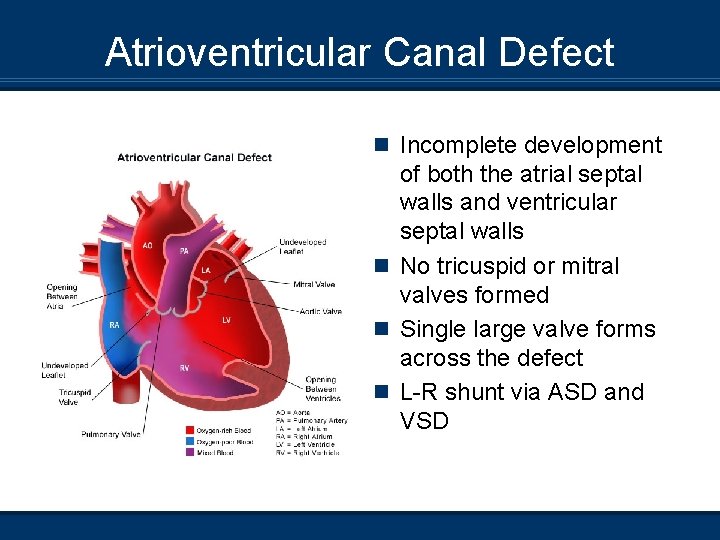
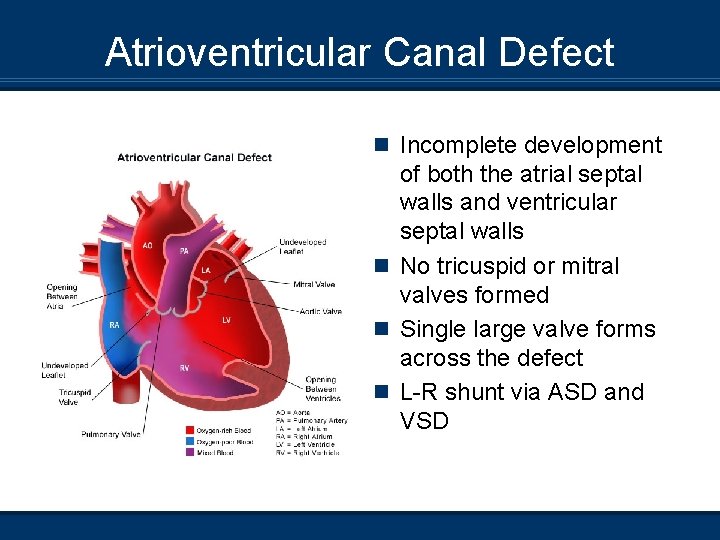
Atrioventricular Canal Defect n Incomplete development of both the atrial septal walls and ventricular septal walls n No tricuspid or mitral valves formed n Single large valve forms across the defect n L-R shunt via ASD and VSD
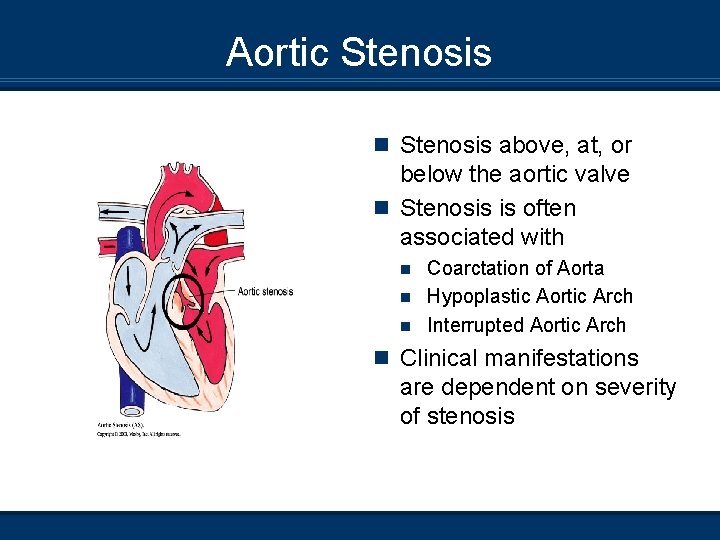
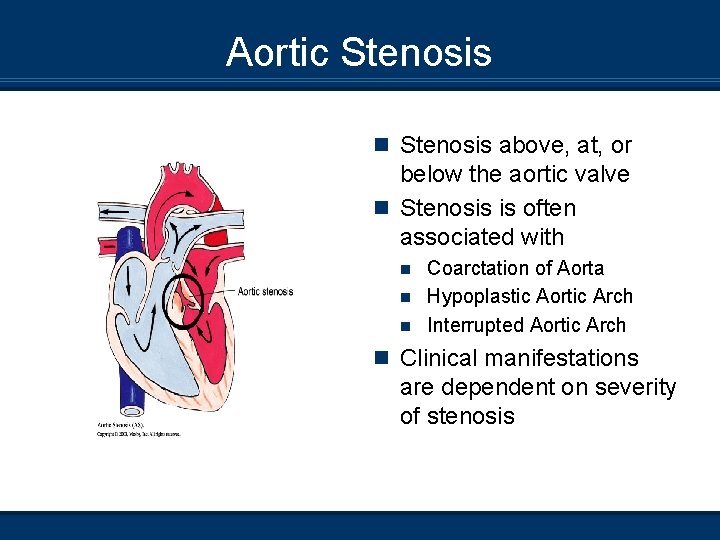
Aortic Stenosis n Stenosis above, at, or below the aortic valve n Stenosis is often associated with Coarctation of Aorta n Hypoplastic Aortic Arch n Interrupted Aortic Arch n n Clinical manifestations are dependent on severity of stenosis
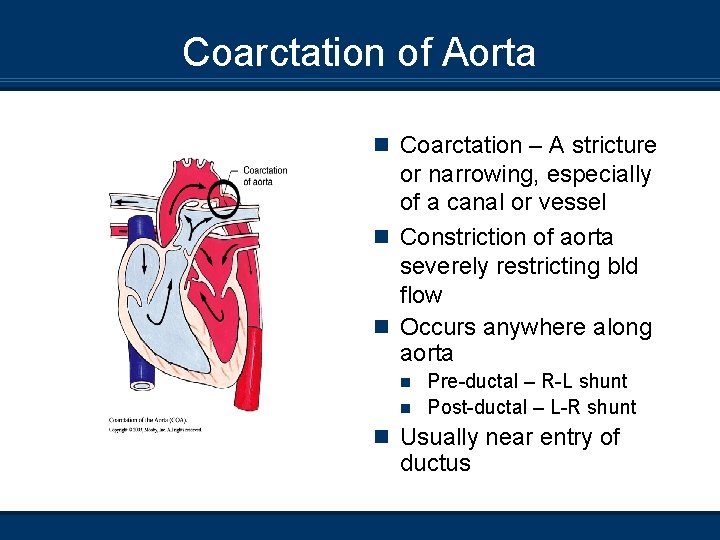
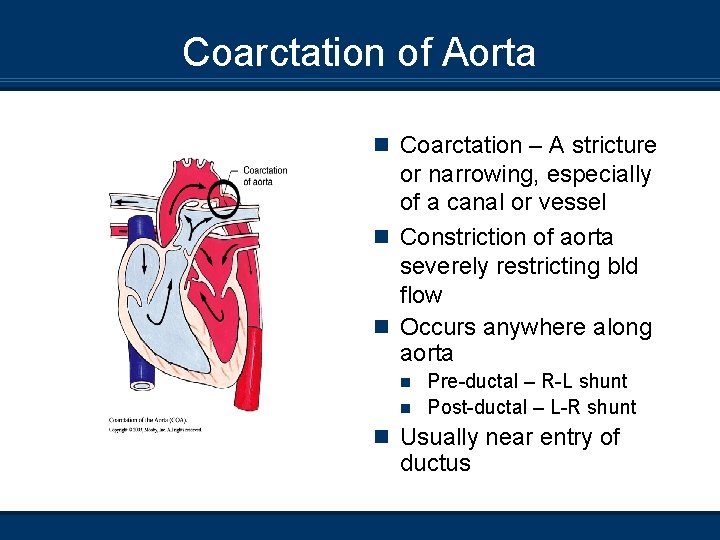
Coarctation of Aorta n Coarctation – A stricture or narrowing, especially of a canal or vessel n Constriction of aorta severely restricting bld flow n Occurs anywhere along aorta Pre-ductal – R-L shunt n Post-ductal – L-R shunt n n Usually near entry of ductus
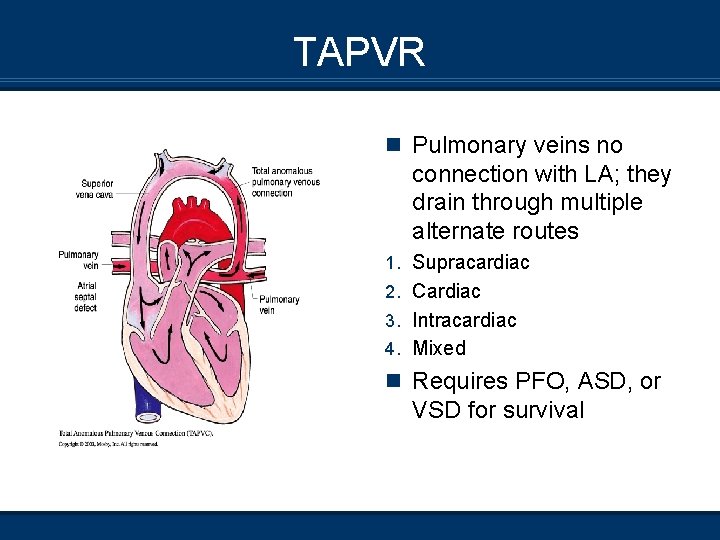
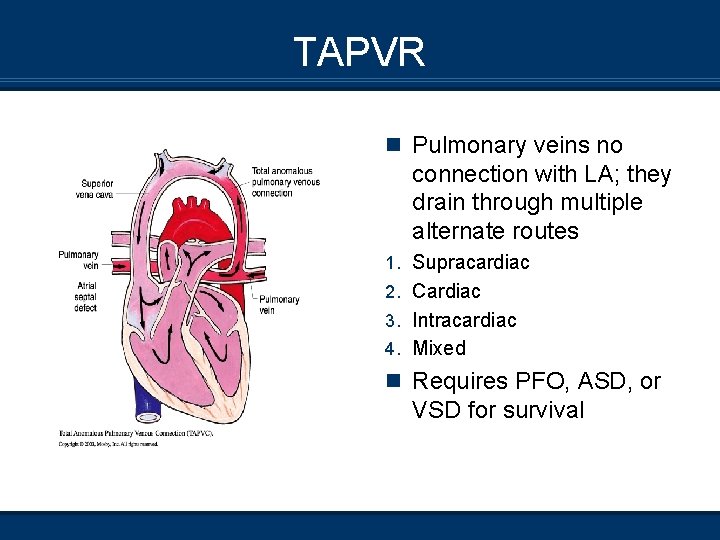
TAPVR n Pulmonary veins no connection with LA; they drain through multiple alternate routes 1. Supracardiac 2. Cardiac 3. Intracardiac 4. Mixed n Requires PFO, ASD, or VSD for survival
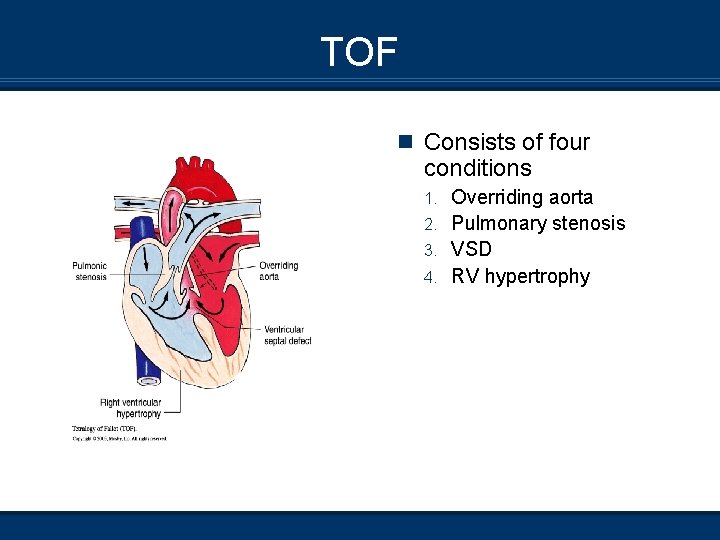
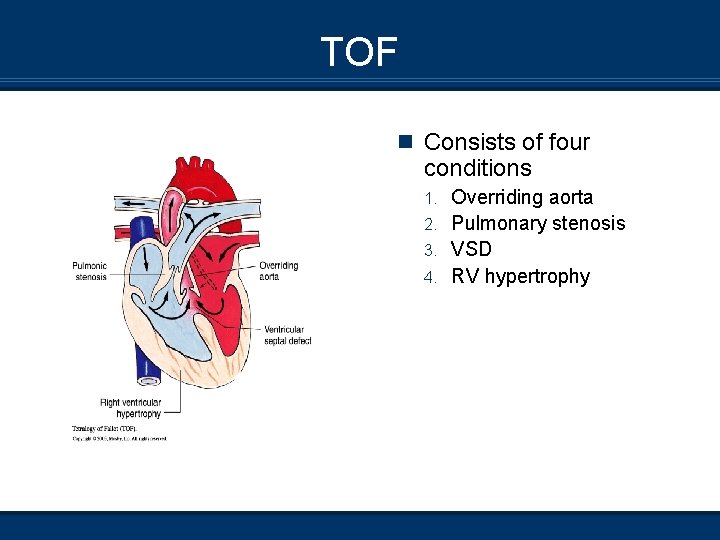
TOF n Consists of four conditions Overriding aorta 2. Pulmonary stenosis 3. VSD 4. RV hypertrophy 1.
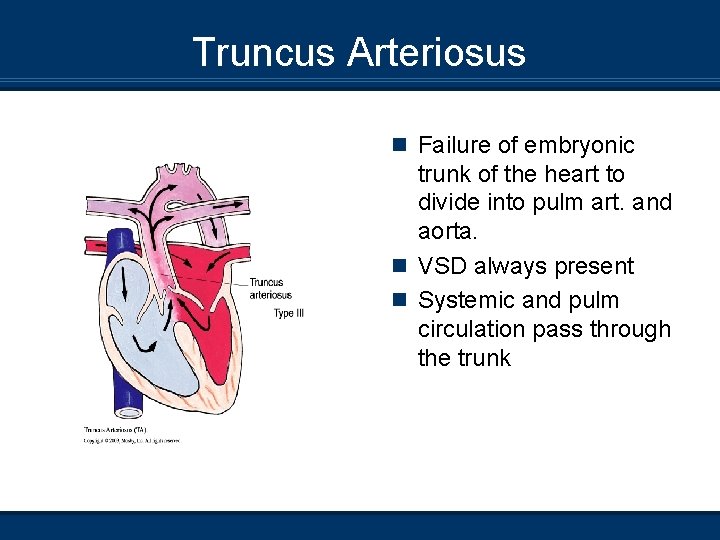
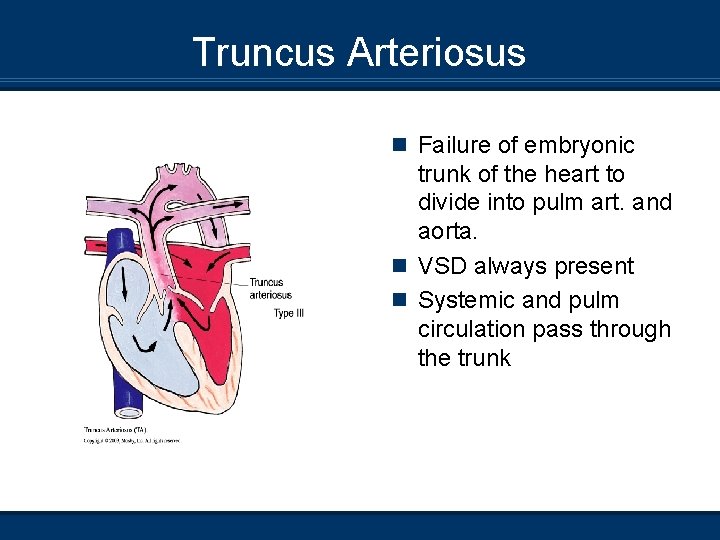
Truncus Arteriosus n Failure of embryonic trunk of the heart to divide into pulm art. and aorta. n VSD always present n Systemic and pulm circulation pass through the trunk
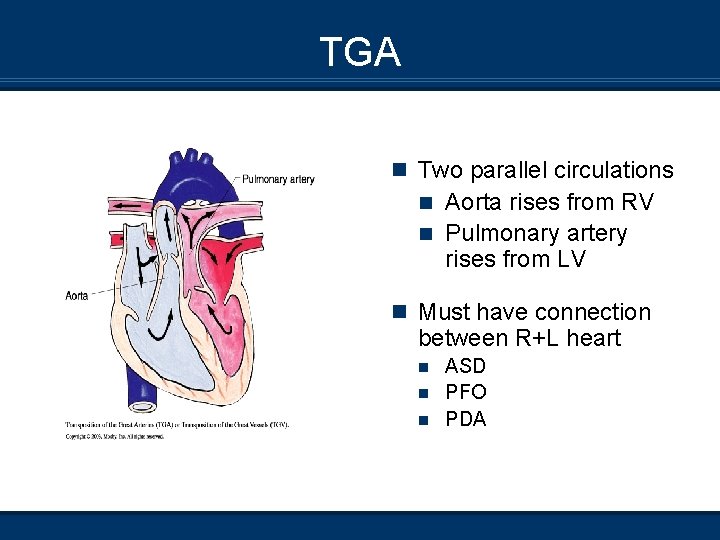
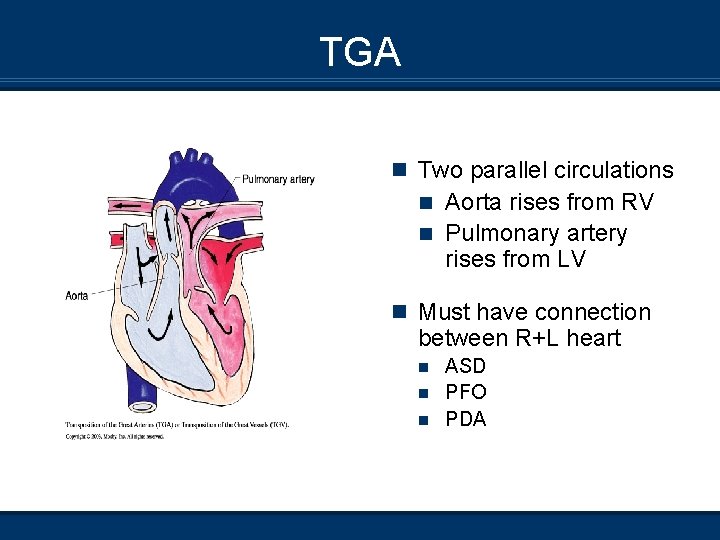
TGA n Two parallel circulations Aorta rises from RV n Pulmonary artery rises from LV n n Must have connection between R+L heart ASD n PFO n PDA n
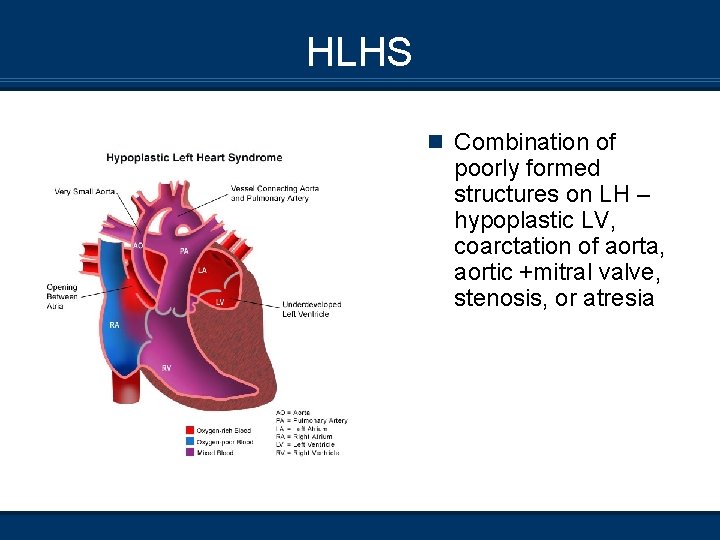
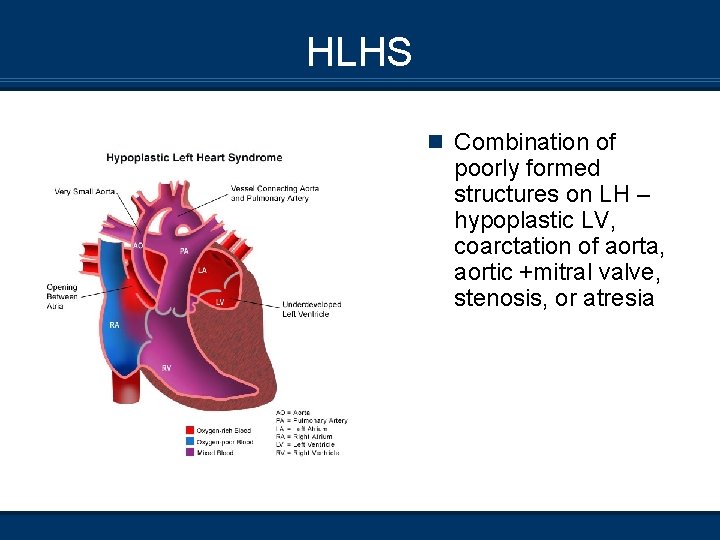
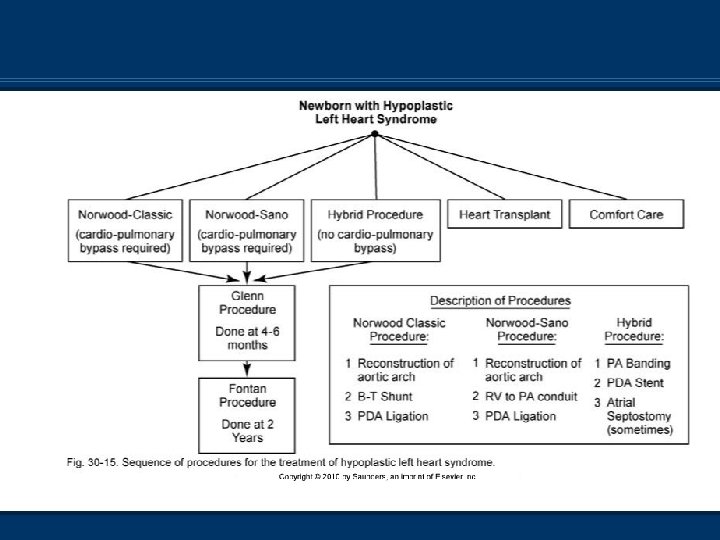
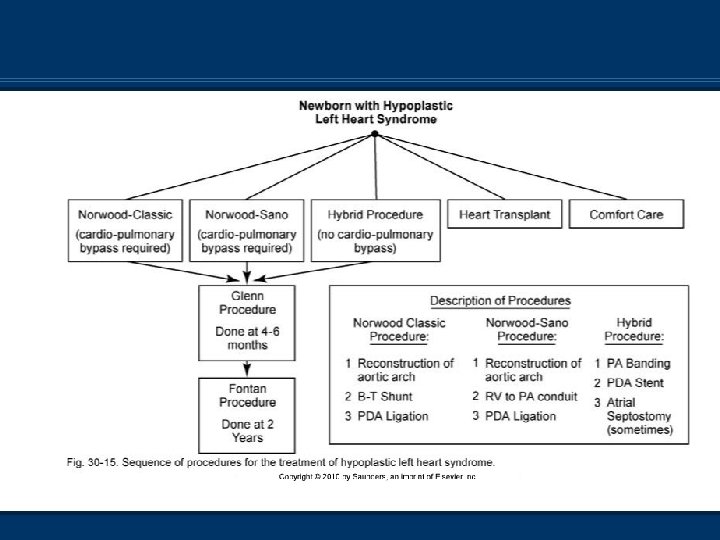
HLHS n Combination of poorly formed structures on LH – hypoplastic LV, coarctation of aorta, aortic +mitral valve, stenosis, or atresia
Croup (LTB) Clinical presentation n 6 months - 4 years (Peak incidence fall and winter) n Several day Hx of upper respiratory tract symptoms progressing to hoarseness n Barky cough, stridor, low-grade fever, usually clear o/a n Severe – Biphasic stridor, nasal flaring, accessory muscle use, low Sp. O 2
Diagnostics n Most common cause – Parainfluenza virus type 1 n Also caused by types 2 and 3, RSV, adenovirus n Usually based on clinical diagnosis n X-ray – Steeple sign (More noticeable on insp) n Usually normal WBC; leukocytosis with viral differential
Epiglottitis Clinical presentation Since H flu vaccine, decrease in # of cases Cellulitis of supraglottic structures (Life-threatening) Can occur at any age, usually 2 - 8 years Toxic looking and anxious, tripod position 4 Ds – Drooling, dyspnea, dysphagia, dysphonia Symptoms show rapid progression after a matter of hours n Stridor a late finding – Indicates impending complete AW obstruction n n n
Diagnostics n Haemophilus influenza type B most common n Also viruses, group B hemolytic strep, pneumococci n ↑ WBC with neutrophil predominance n X-ray – Thumb sign n Visualization – Edema and erytherma of supraglottic structures
Bronchiolitis RSV n High risk of mortality in prem infants, infants with chronic lung disease, immunocompromised patients n Infection in infancy predisposes children to reactive AW and asthma later on n Nosocomial infection common; droplets may remain infectious up to 12 hours
Clinical Presentation n Peak epidemic Nov - Apr; most children affected are <2 n n years old Mild to moderate nasal congestion Low-grade fever Productive cough 30 - 50% develop lower resp. tract infection in 2 - 3 days n Coughing more severe, copious secretions, resp distress, tachypnea, nasal flaring, retractions, prolonged exh n Crackles t/o; wheezing in half n CXR – Hyperinflation; interstitial infiltrates n Very young infants may only present with lethargy and poor feeding; apnea and bradycardia frequently