Pediatric Case Conference 2007 8 31 R 2





- Slides: 25

Pediatric Case Conference 2007. 8. 31 R 2 施家祥 Supervisor: 吳孟書 醫師

Case 張X傑 10322186 n Age: 3 y 9 m/o, Gender: male n BW: 16 kg n 台北急診, 就診時間: 2007/8/15 16: 17 Vital signs: TPR: 36. 5 C/ 112/ 20, BP: ? /? mm. Hg GCS: E 4 V 5 M 6, Sa. O 2: 98% n 檢傷主訴: 腹痛. 嘔吐 n
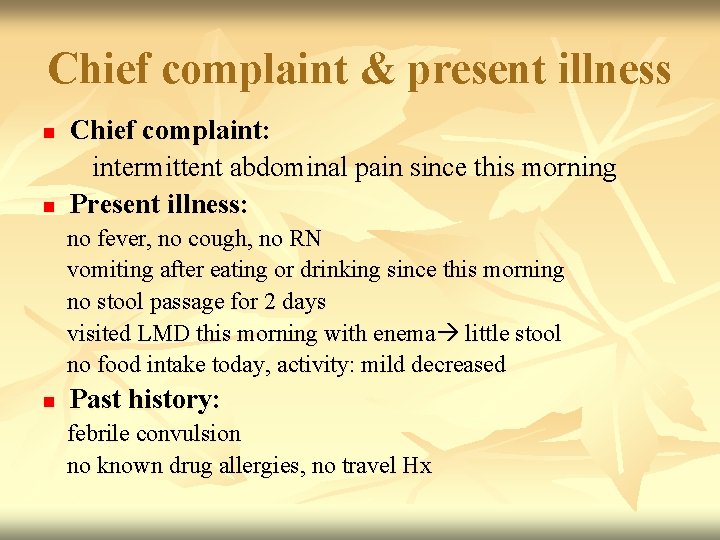
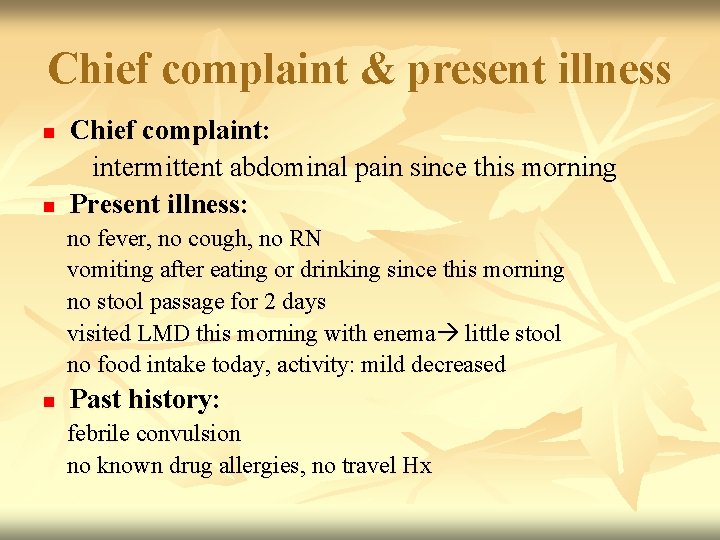
Chief complaint & present illness n n Chief complaint: intermittent abdominal pain since this morning Present illness: no fever, no cough, no RN vomiting after eating or drinking since this morning no stool passage for 2 days visited LMD this morning with enema little stool no food intake today, activity: mild decreased n Past history: febrile convulsion no known drug allergies, no travel Hx
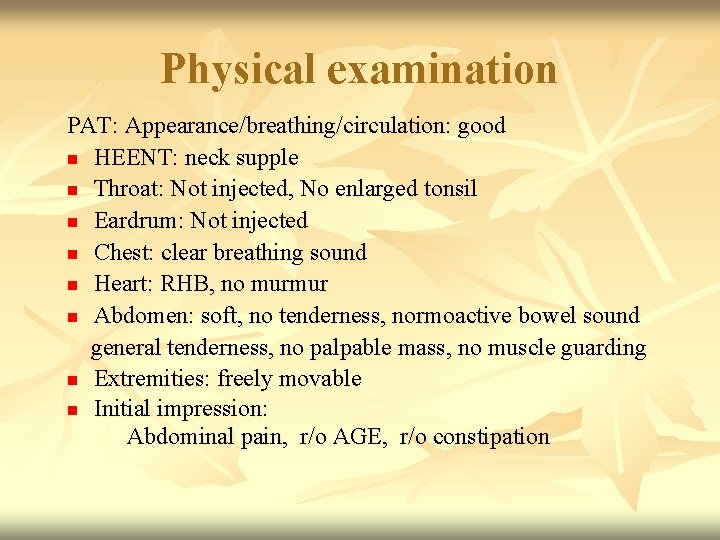
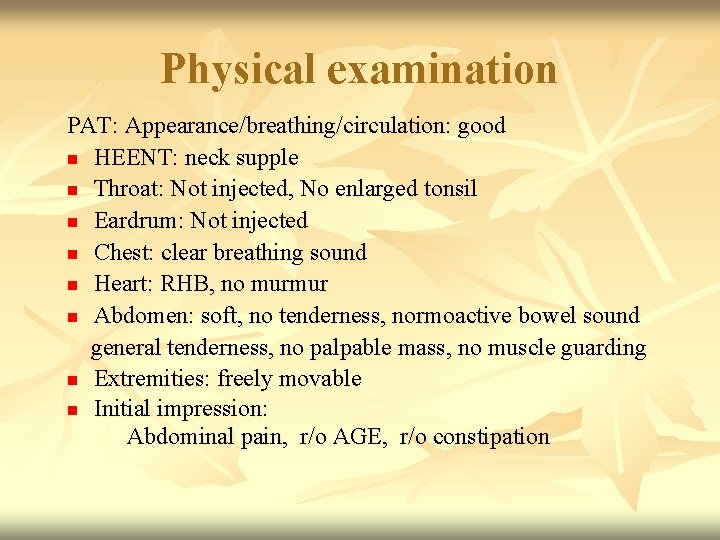
Physical examination PAT: Appearance/breathing/circulation: good n HEENT: neck supple n Throat: Not injected, No enlarged tonsil n Eardrum: Not injected n Chest: clear breathing sound n Heart: RHB, no murmur n Abdomen: soft, no tenderness, normoactive bowel sound general tenderness, no palpable mass, no muscle guarding n Extremities: freely movable n Initial impression: Abdominal pain, r/o AGE, r/o constipation
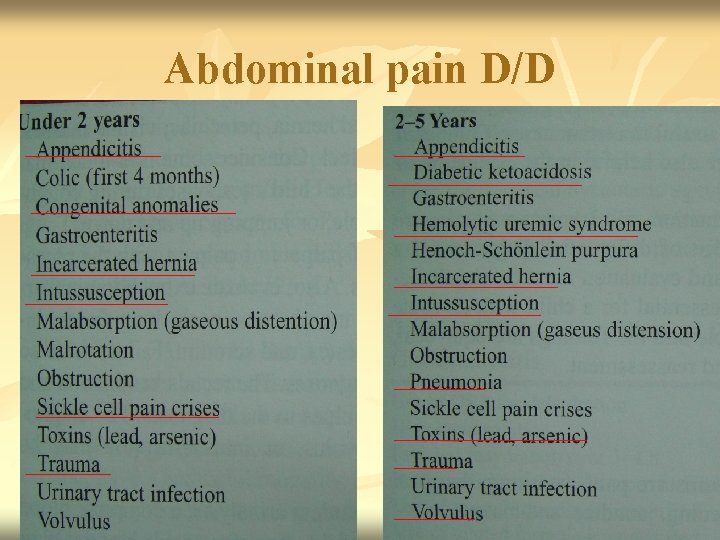
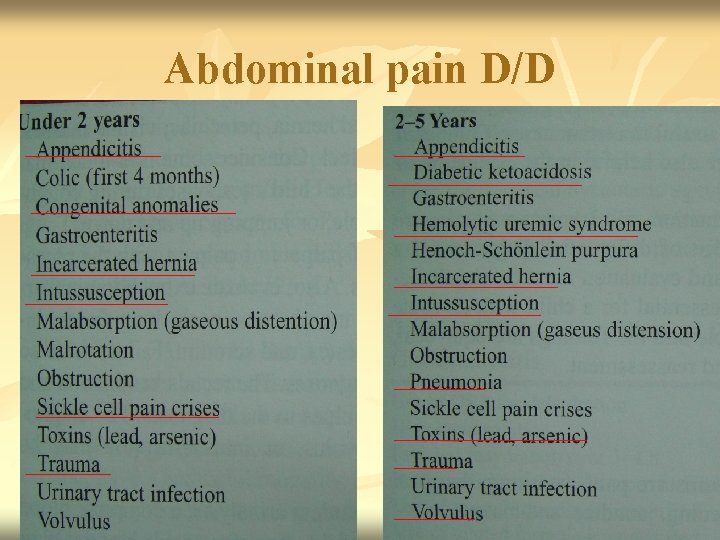
Abdominal pain D/D
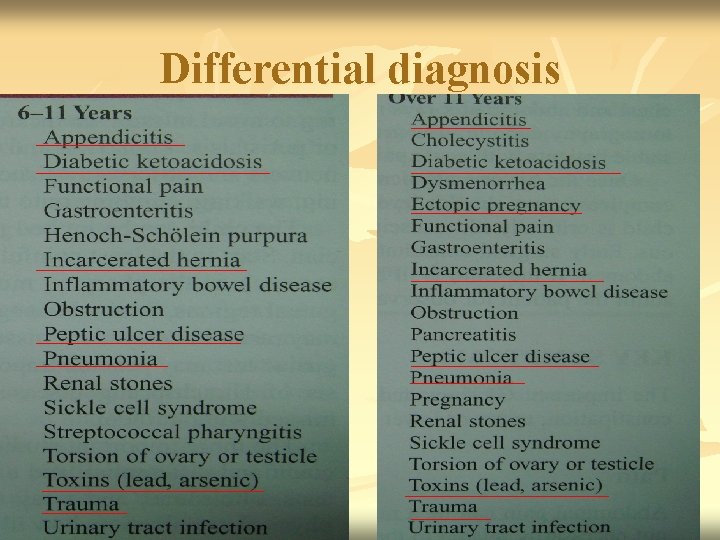
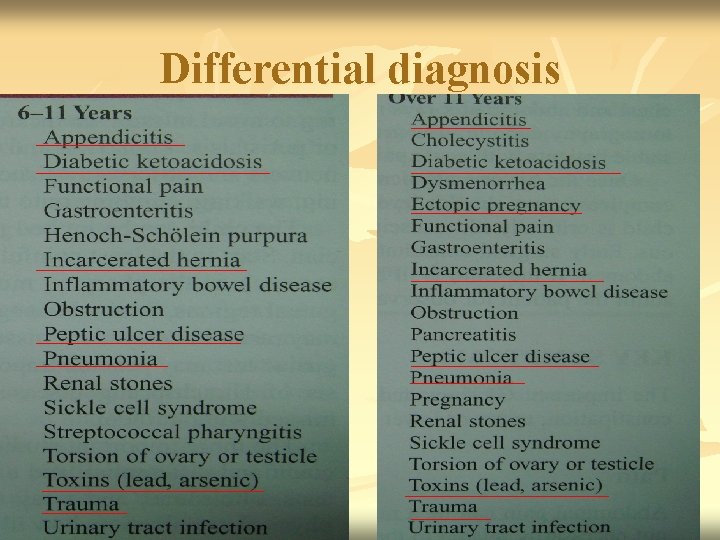
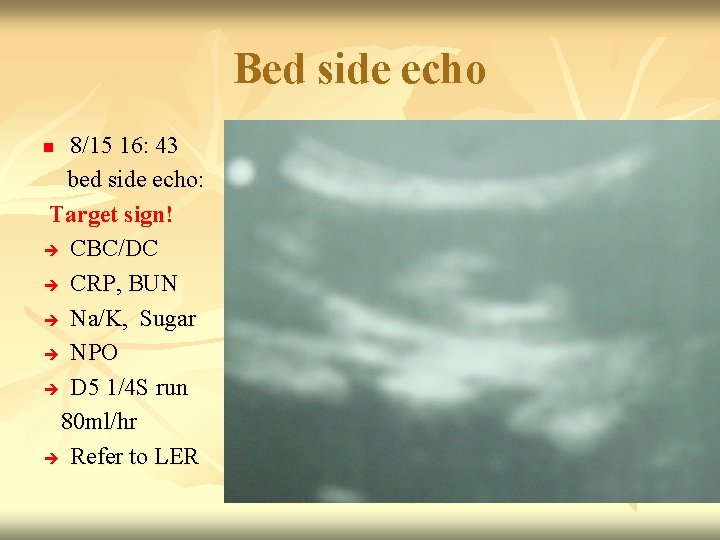
Differential diagnosis
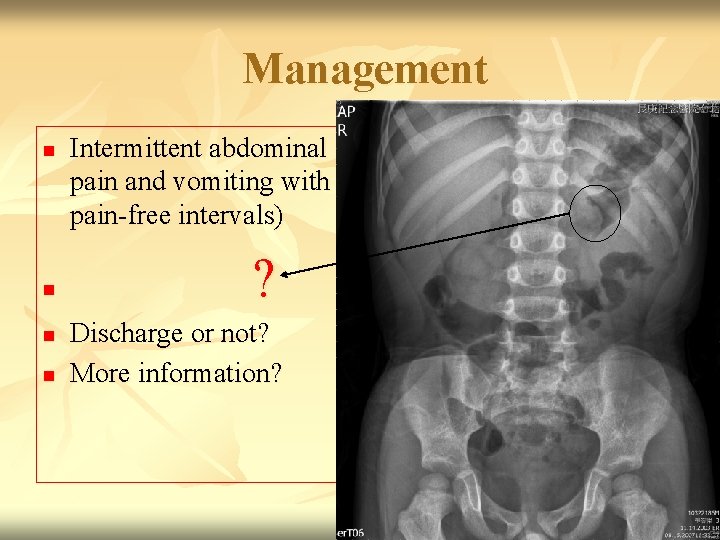
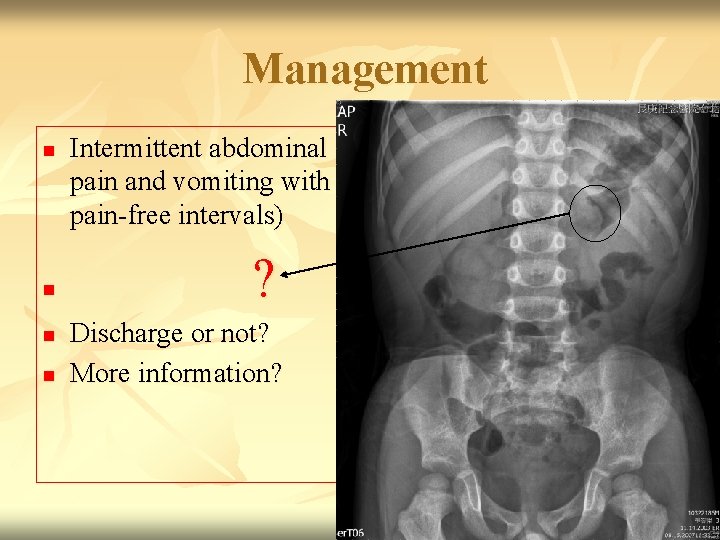
Management n n Intermittent abdominal pain and vomiting with pain-free intervals) ? Discharge or not? More information?
KUB n n n No hepatosplenomegaly. No obvious radiopaque stone along bilateral utrotracts Normal bowel gas pattern Unremarkable T-L spine alignment, disc spaces, no degenerative spur formation. Unremarkable other bony structures (including lower ribs, pelvic bones, bil SI joints, femoral head and necks).
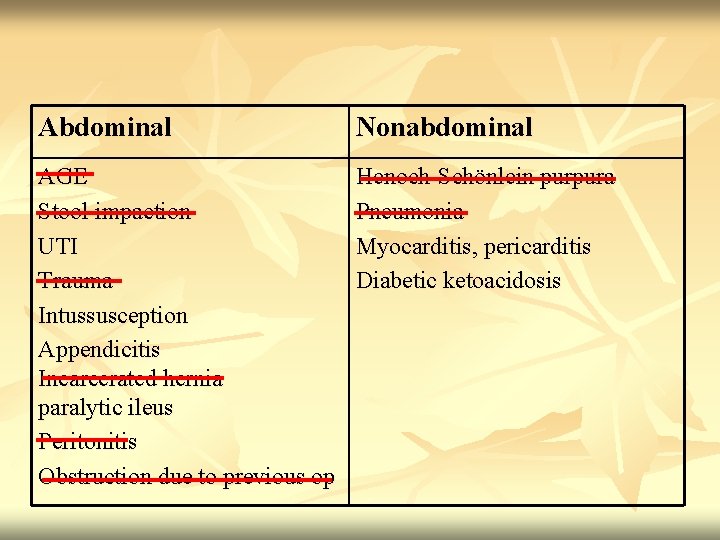
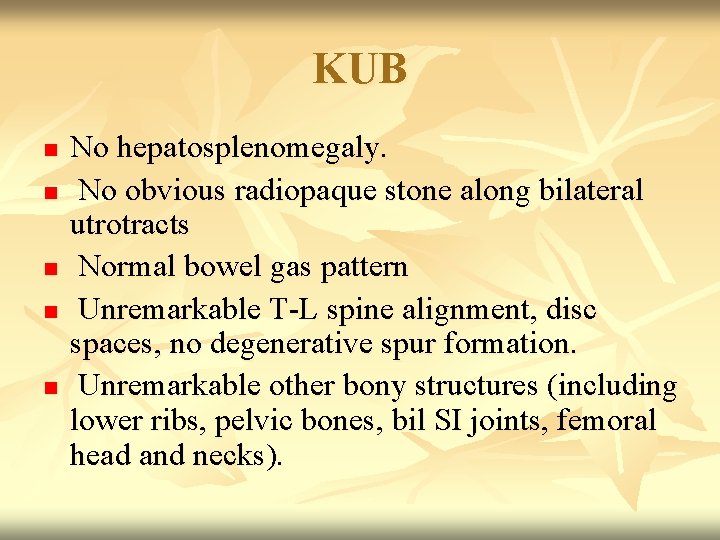
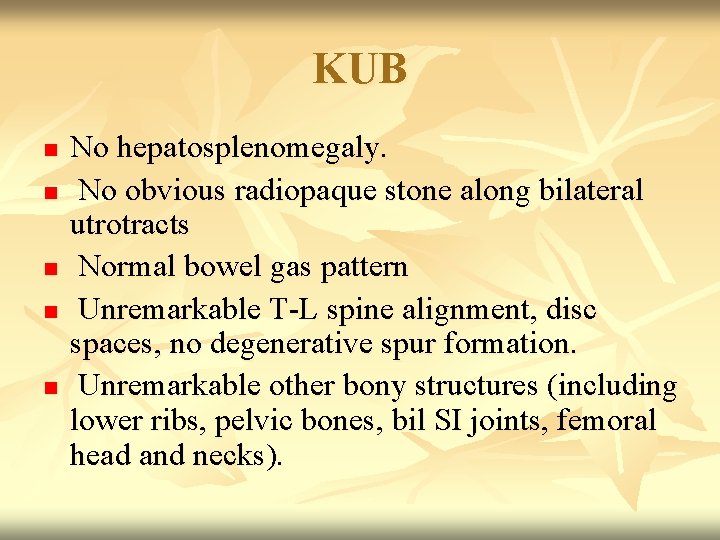
Abdominal Nonabdominal AGE Stool impaction UTI Trauma Intussusception Appendicitis Incarcerated hernia paralytic ileus Peritonitis Obstruction due to previous op Henoch-Schönlein purpura Pneumonia Myocarditis, pericarditis Diabetic ketoacidosis
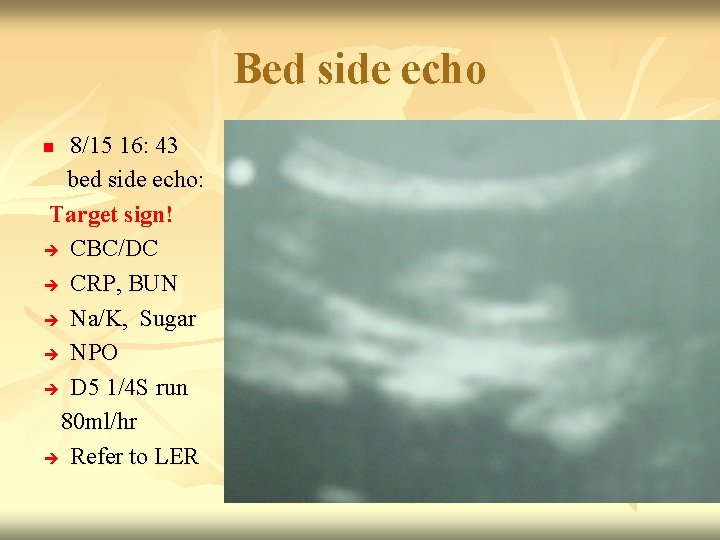
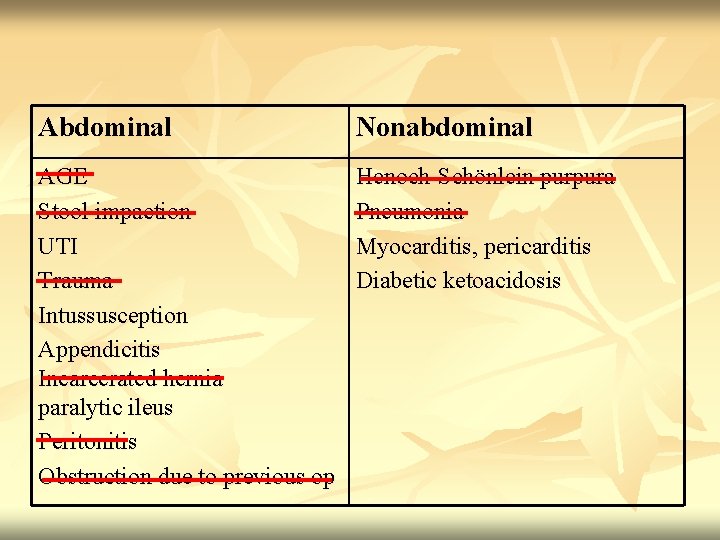
Bed side echo 8/15 16: 43 bed side echo: Target sign! CBC/DC CRP, BUN Na/K, Sugar NPO D 5 1/4 S run 80 ml/hr Refer to LER n
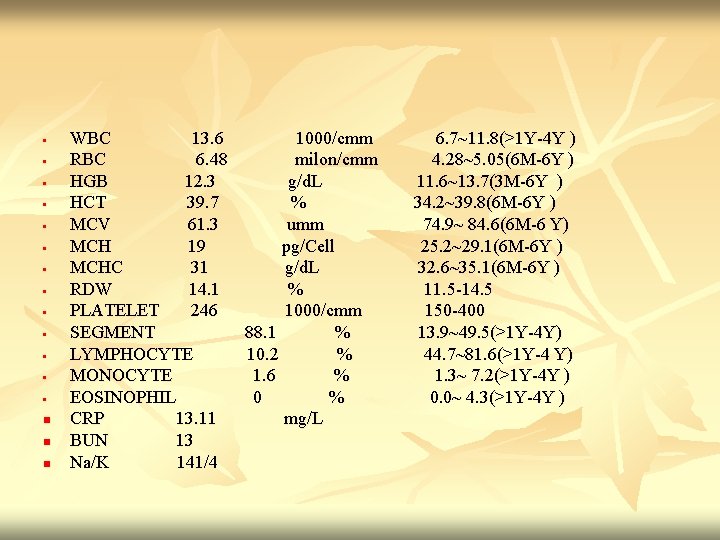
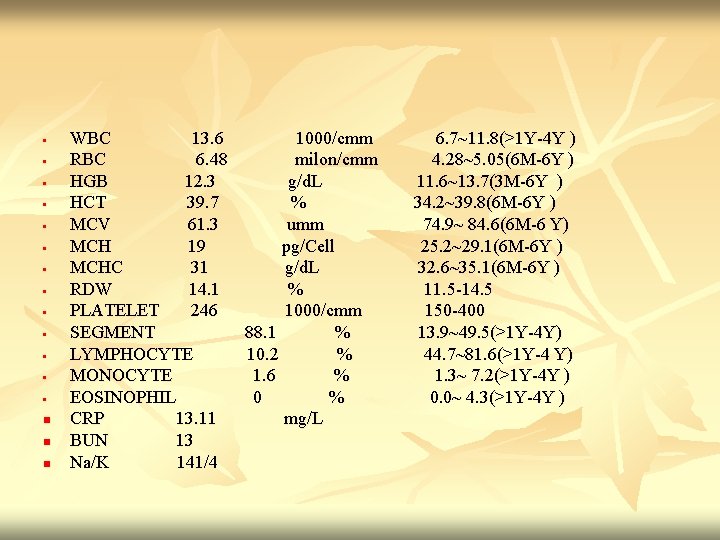
• • • • n n n WBC 13. 6 1000/cmm RBC 6. 48 milon/cmm HGB 12. 3 g/d. L HCT 39. 7 % MCV 61. 3 umm MCH 19 pg/Cell MCHC 31 g/d. L RDW 14. 1 % PLATELET 246 1000/cmm SEGMENT 88. 1 % LYMPHOCYTE 10. 2 % MONOCYTE 1. 6 % EOSINOPHIL 0 % CRP 13. 11 mg/L BUN 13 Na/K 141/4 6. 7~11. 8(>1 Y-4 Y ) 4. 28~5. 05(6 M-6 Y ) 11. 6~13. 7(3 M-6 Y ) 34. 2~39. 8(6 M-6 Y ) 74. 9~ 84. 6(6 M-6 Y) 25. 2~29. 1(6 M-6 Y ) 32. 6~35. 1(6 M-6 Y ) 11. 5 -14. 5 150 -400 13. 9~49. 5(>1 Y-4 Y) 44. 7~81. 6(>1 Y-4 Y) 1. 3~ 7. 2(>1 Y-4 Y ) 0. 0~ 4. 3(>1 Y-4 Y )
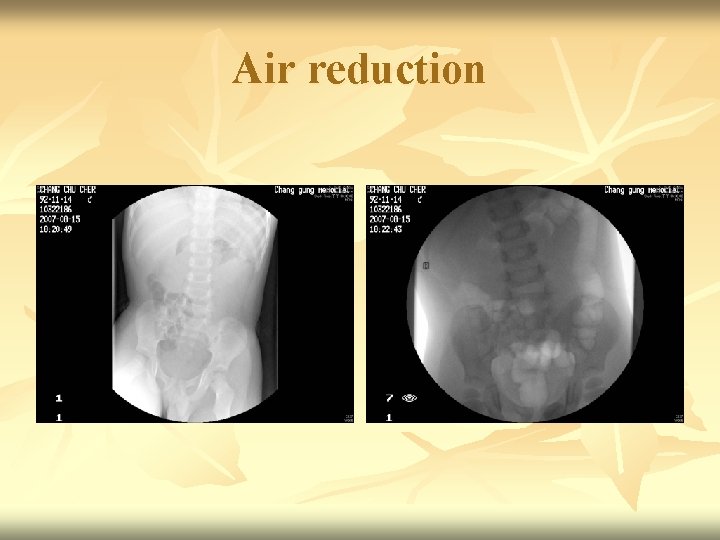
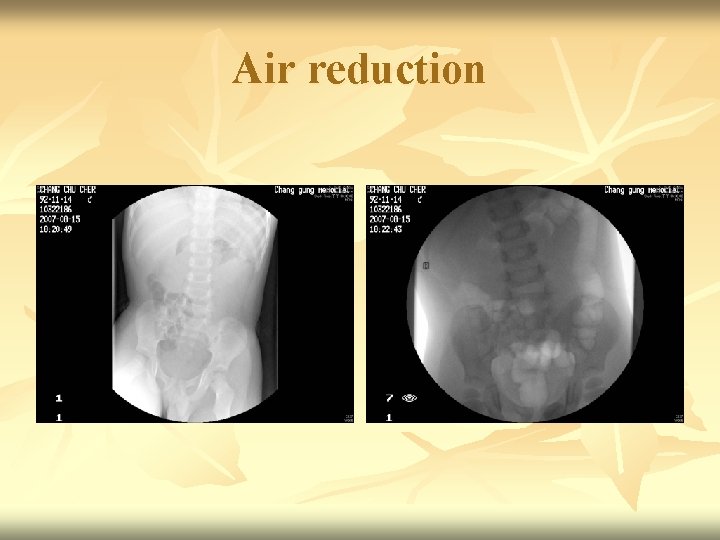
Air reduction



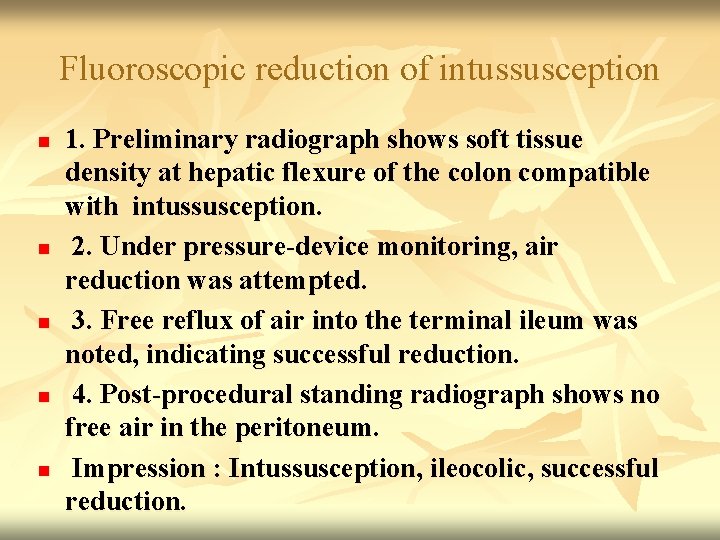
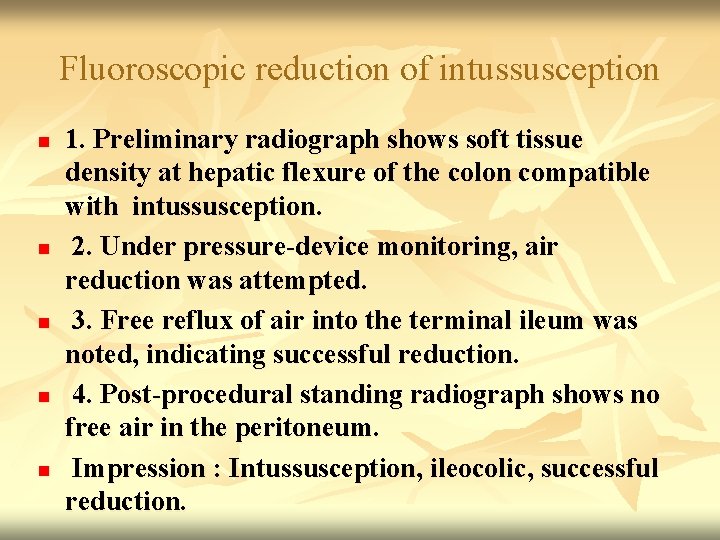
Fluoroscopic reduction of intussusception n n 1. Preliminary radiograph shows soft tissue density at hepatic flexure of the colon compatible with intussusception. 2. Under pressure-device monitoring, air reduction was attempted. 3. Free reflux of air into the terminal ileum was noted, indicating successful reduction. 4. Post-procedural standing radiograph shows no free air in the peritoneum. Impression : Intussusception, ileocolic, successful reduction.
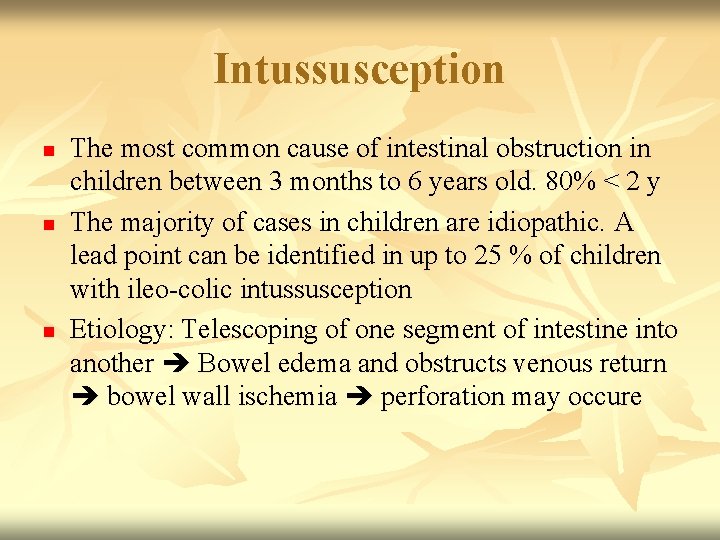
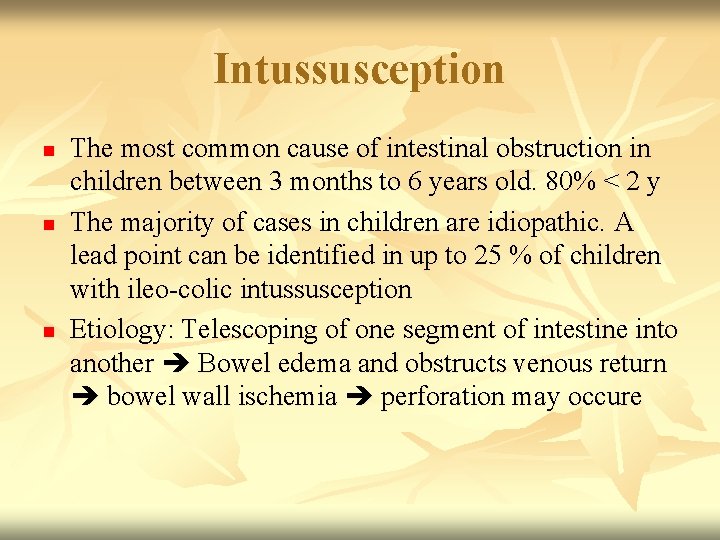
Intussusception n The most common cause of intestinal obstruction in children between 3 months to 6 years old. 80% < 2 y The majority of cases in children are idiopathic. A lead point can be identified in up to 25 % of children with ileo-colic intussusception Etiology: Telescoping of one segment of intestine into another Bowel edema and obstructs venous return bowel wall ischemia perforation may occure
Leading point n n < 5 years old: Enlarged peyer’s patches secondary to a recent viral infection > 5 years old: Underlying lesion is found in 75% of cases: Henoch-Schonlein purpura, Meckel’s diverticulum, Lymphoma, polyps, cystic fibrosis
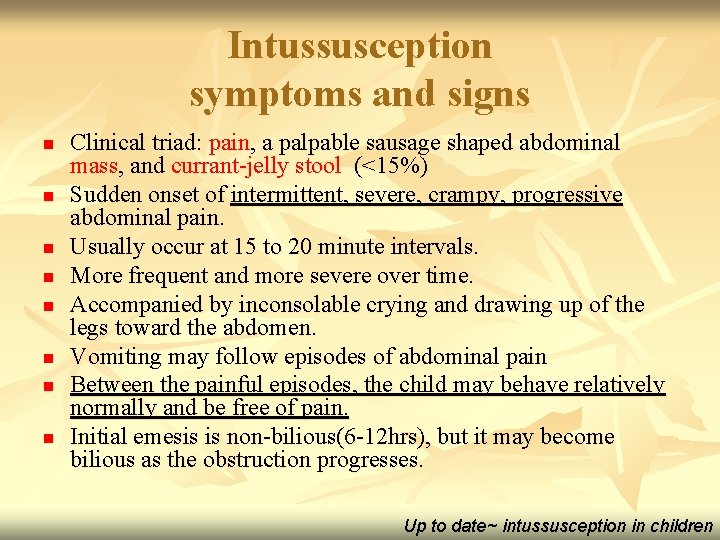
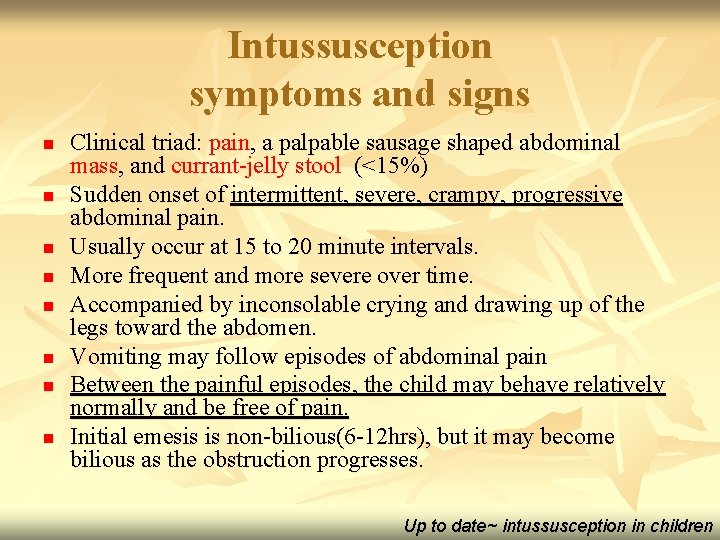
Intussusception symptoms and signs n n n n Clinical triad: pain, a palpable sausage shaped abdominal mass, and currant-jelly stool (<15%) Sudden onset of intermittent, severe, crampy, progressive abdominal pain. Usually occur at 15 to 20 minute intervals. More frequent and more severe over time. Accompanied by inconsolable crying and drawing up of the legs toward the abdomen. Vomiting may follow episodes of abdominal pain Between the painful episodes, the child may behave relatively normally and be free of pain. Initial emesis is non-bilious(6 -12 hrs), but it may become bilious as the obstruction progresses. Up to date~ intussusception in children
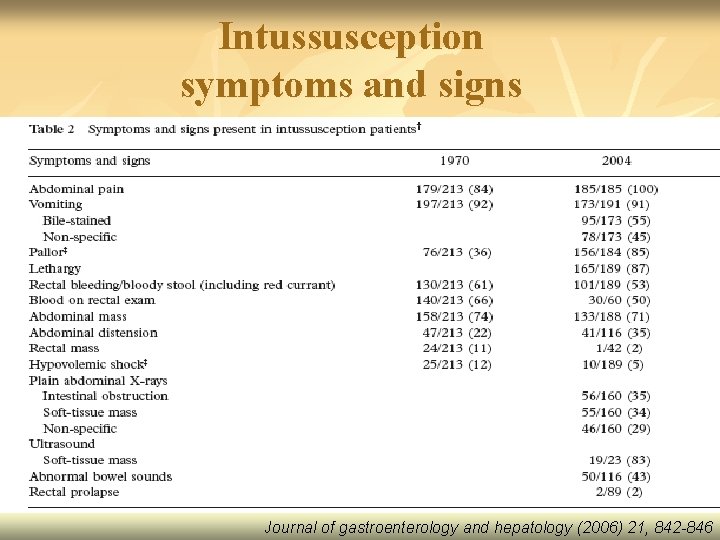
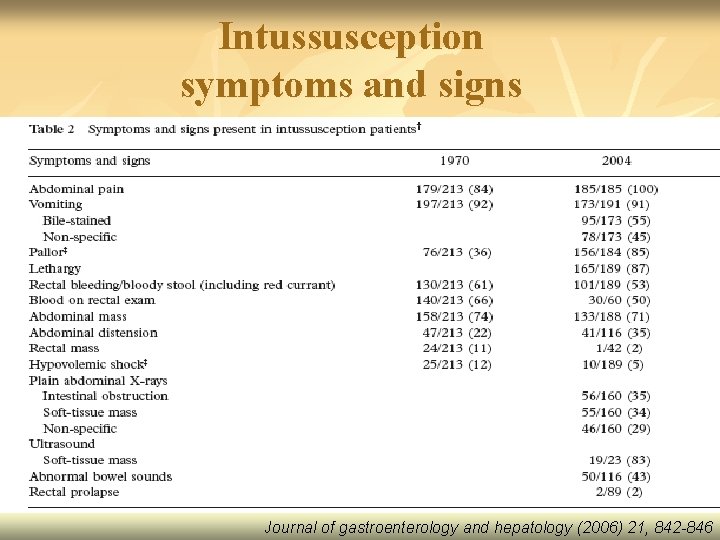
Intussusception symptoms and signs Journal of gastroenterology and hepatology (2006) 21, 842 -846
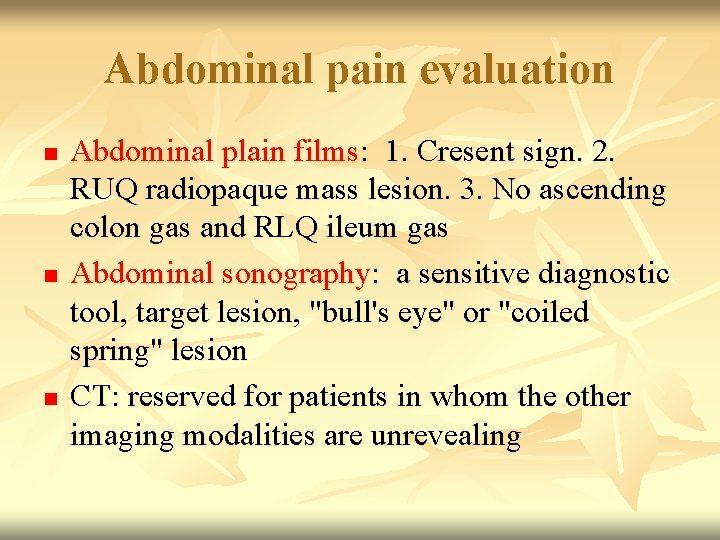
Abdominal pain evaluation n Abdominal plain films: 1. Cresent sign. 2. RUQ radiopaque mass lesion. 3. No ascending colon gas and RLQ ileum gas Abdominal sonography: a sensitive diagnostic tool, target lesion, "bull's eye" or "coiled spring" lesion CT: reserved for patients in whom the other imaging modalities are unrevealing
Evaluation and Management Fluoroscopic reduction n n 1. 2. n The standard procedure for diagnosis and treatment of ileocolonic intussusception is a contrast (air favored) enema. Greatest risk of perforation in: (<1%) infants younger than six months of age who have had symptoms for three days or longer. patients with evidence of small bowel obstruction Reduction should not be attempted in patients with prolonged symptoms or any signs of peritoneal irritation or free peritoneal air
Fluoroscopic reduction n Observation policy differed between countries and settings, with a minimum observation period of 12 -36 hrs after conservative treatment. (The pediatric infectious disease journal. Vol. 25, NO 1, Jan. 2006 review article) n n Recurrence after successful nonoperative reduction is approximately 10%. Recurrence is not necessarily an indication for surgery.
Surgery n 1. 2. 3. n Indications: nonoperative reduction is incomplete persistent filling defect signs of peritoneal irritation or free peritoneal air Manual reduction (recurrence : 1%)& resection with primary anastomosis
Key points n n Abdominal pain: child’s age, fever, ex/abdominal, obstructive, local or systemic Bilious vomiting is always indicative of a serious process. Diarrhea should be evaluated for blood. Chest and abdominal radiographs can be useful for pneumonia and obstruction or ileus. Abdominal sonography can be helpful in ER for differential diagnosis.