Pediatric arrhythmias Conduction system of heart ECG waves


- Slides: 41
Pediatric arrhythmias
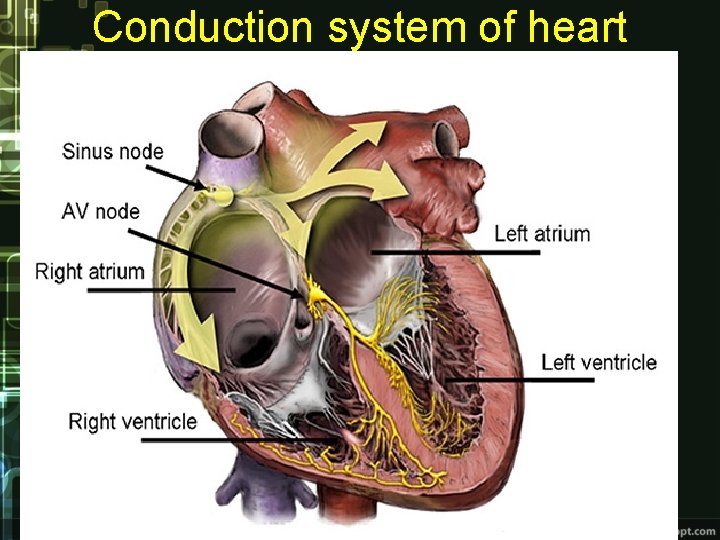
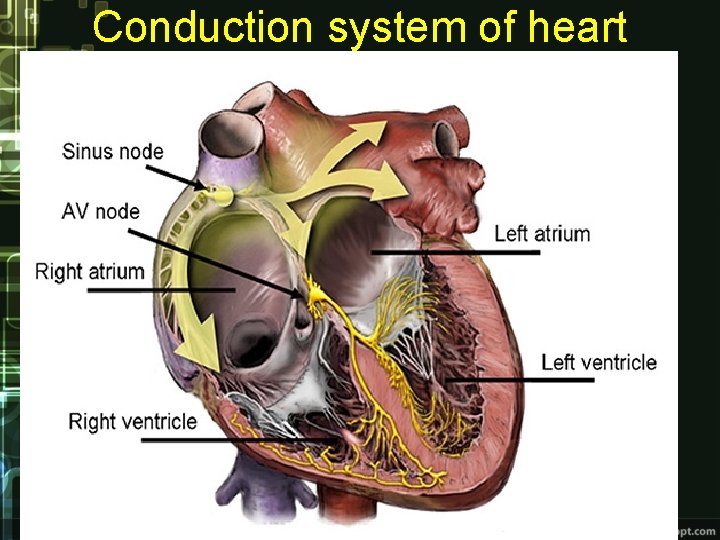
Conduction system of heart
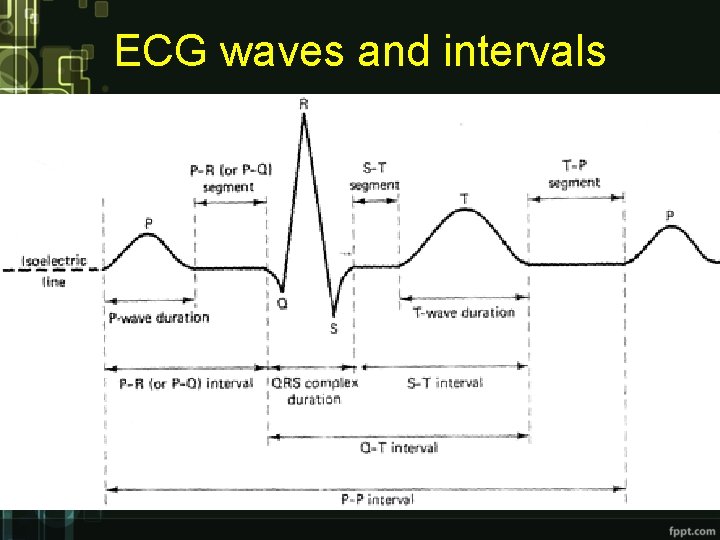
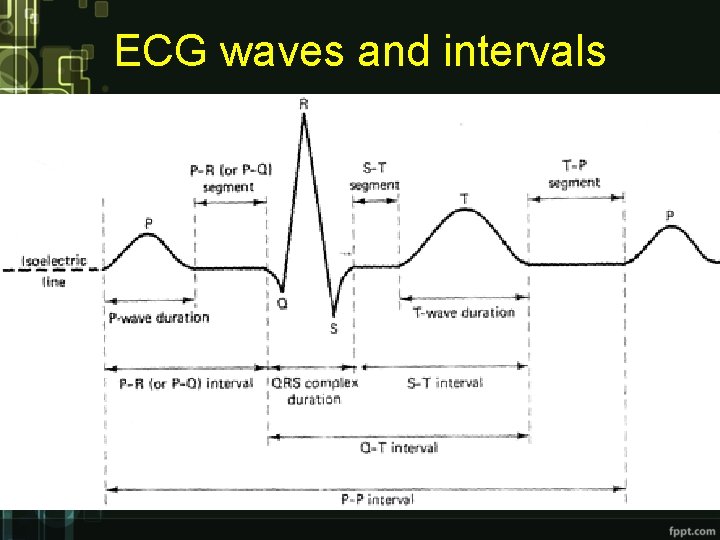
ECG waves and intervals
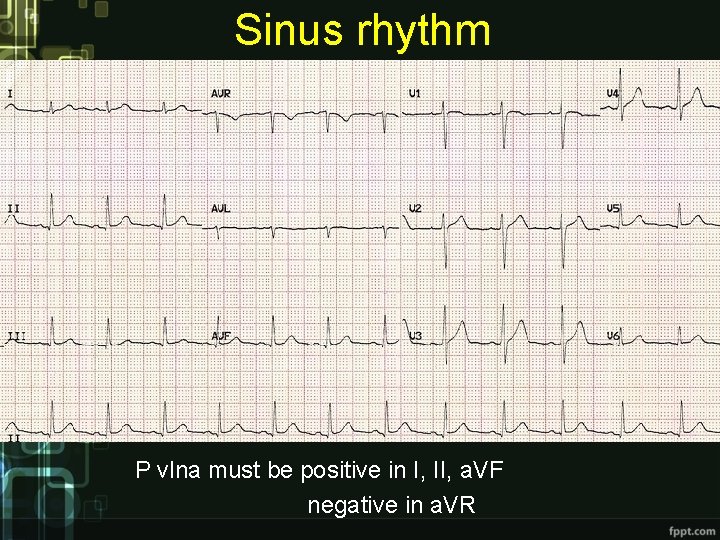
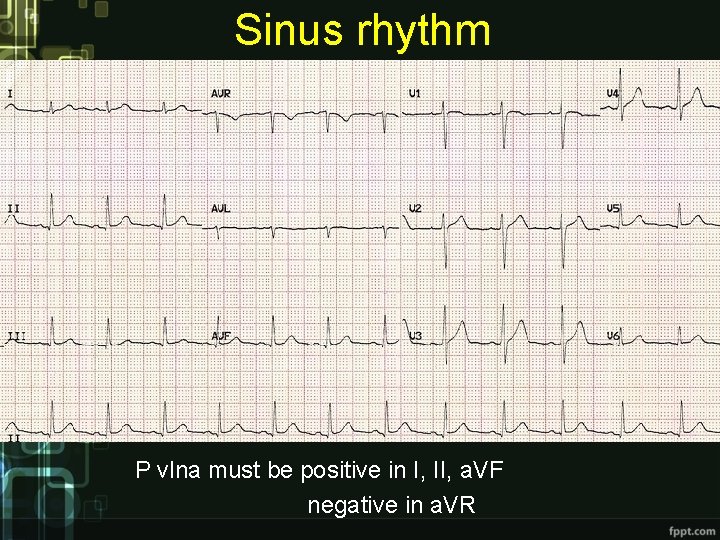
Sinus rhythm P vlna must be positive in I, II, a. VF negative in a. VR
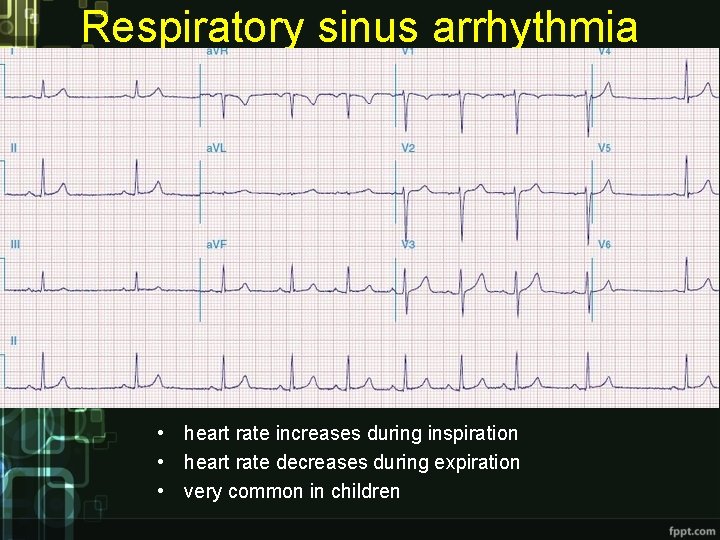
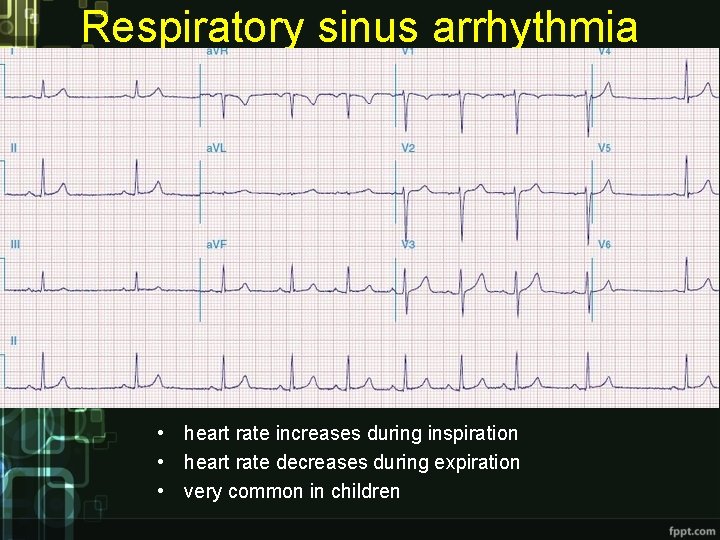
Respiratory sinus arrhythmia • heart rate increases during inspiration • heart rate decreases during expiration • very common in children
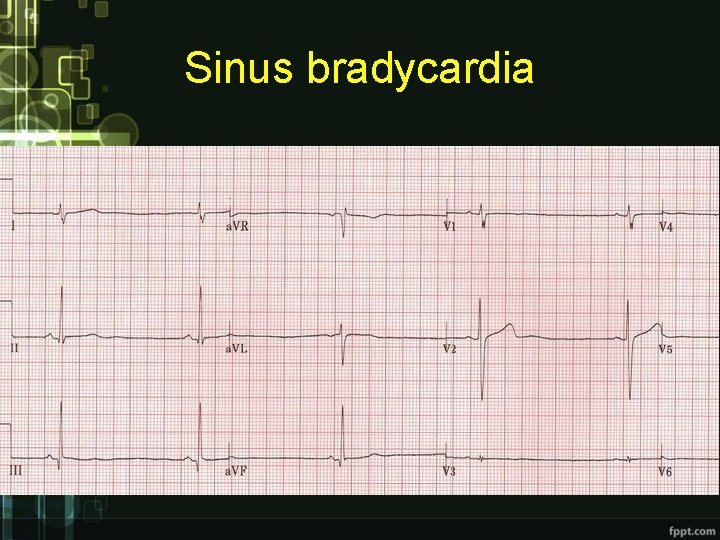
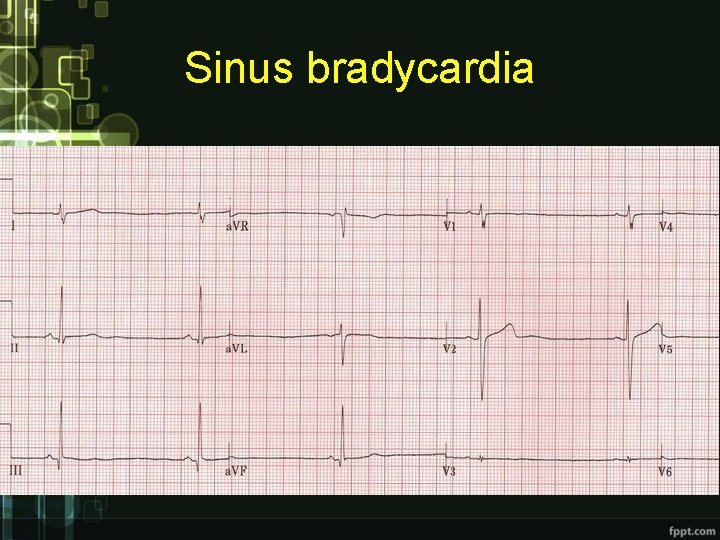
Sinus bradycardia
Causes of sinus bradycardia: Ø physiologic – sleeping, sportmen Ø pathologic – anorexia, hypothermia, hypothyroidism, intracranial hypertension, hypoxia Ø pharmacologic – betablockers, digoxin, calcium channel blockers threshold depends on age * newborn under 90 -100 b. p. m. * adolescent under 60 b. p. m.
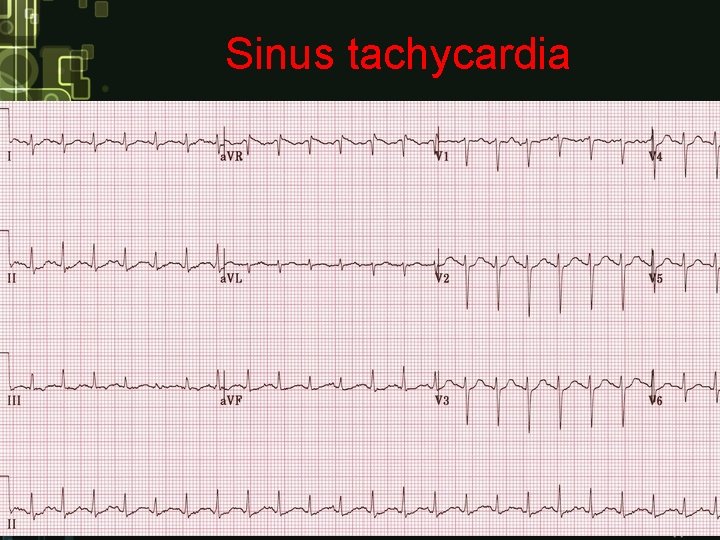
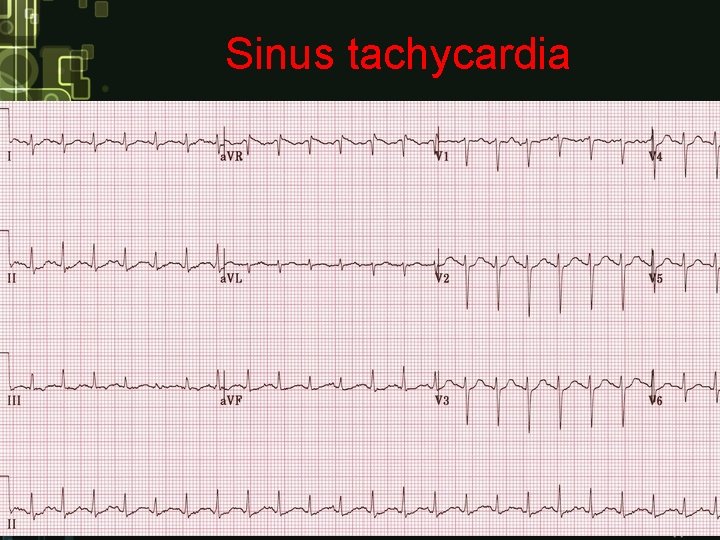
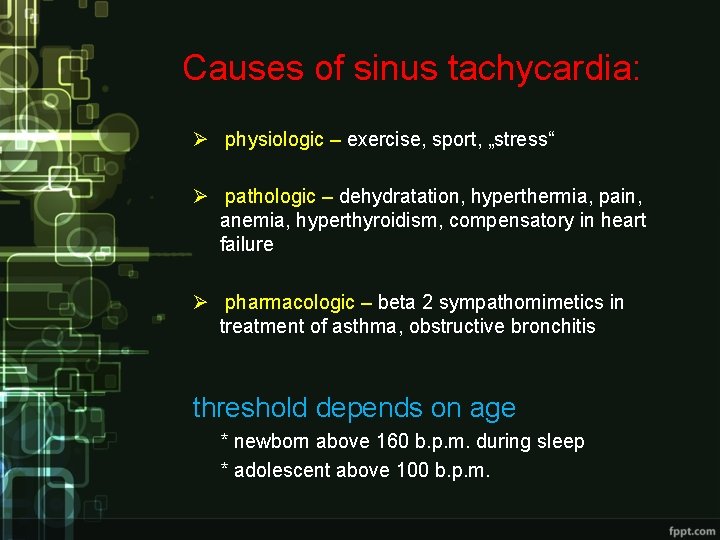
Sinus tachycardia
Causes of sinus tachycardia: Ø physiologic – exercise, sport, „stress“ Ø pathologic – dehydratation, hyperthermia, pain, anemia, hyperthyroidism, compensatory in heart failure Ø pharmacologic – beta 2 sympathomimetics in treatment of asthma, obstructive bronchitis threshold depends on age * newborn above 160 b. p. m. during sleep * adolescent above 100 b. p. m.
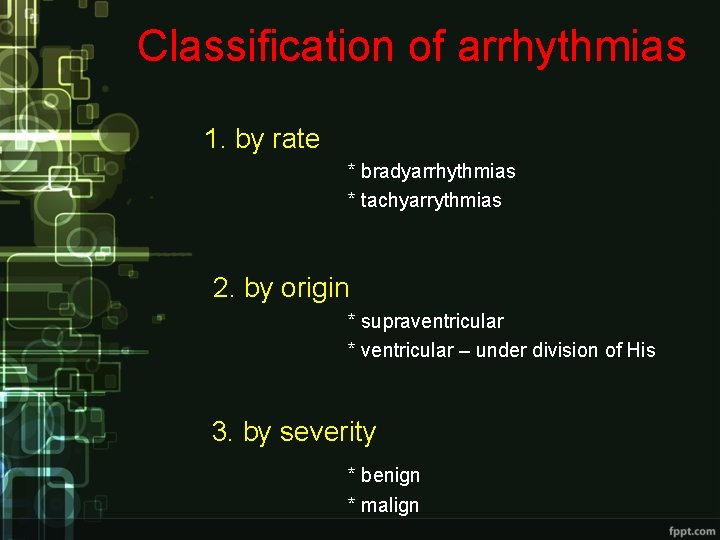
Classification of arrhythmias 1. by rate * bradyarrhythmias * tachyarrythmias 2. by origin * supraventricular * ventricular – under division of His 3. by severity * benign * malign
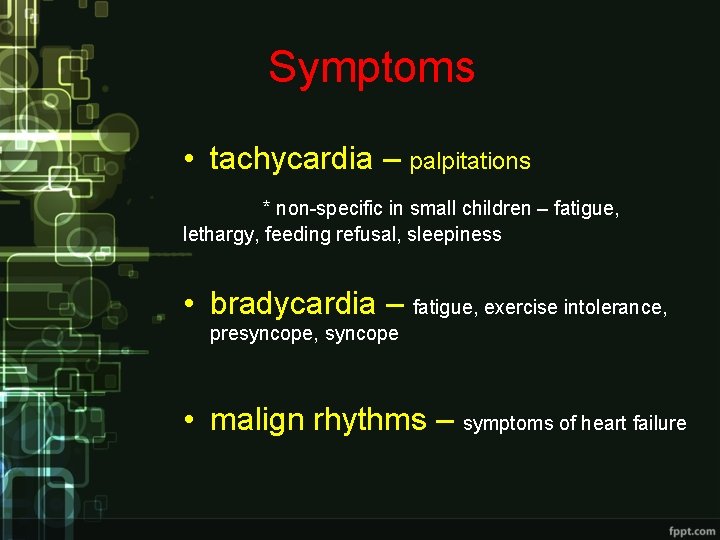
Symptoms • tachycardia – palpitations * non-specific in small children – fatigue, lethargy, feeding refusal, sleepiness • bradycardia – fatigue, exercise intolerance, presyncope, syncope • malign rhythms – symptoms of heart failure
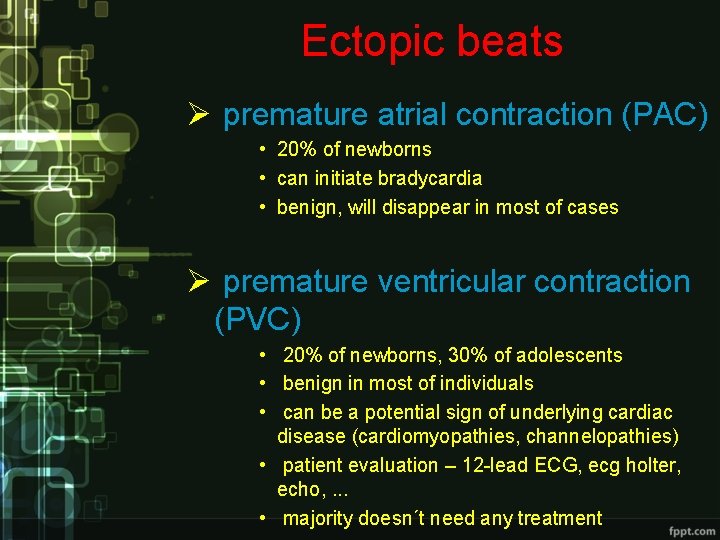
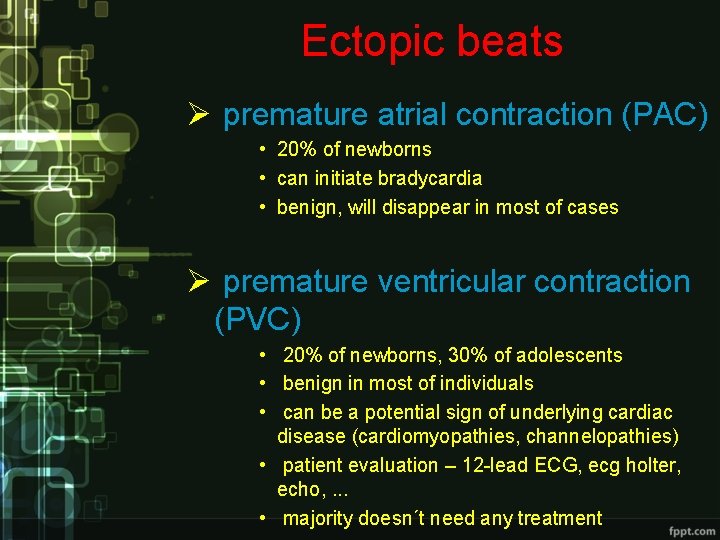
Ectopic beats Ø premature atrial contraction (PAC) • 20% of newborns • can initiate bradycardia • benign, will disappear in most of cases Ø premature ventricular contraction (PVC) • 20% of newborns, 30% of adolescents • benign in most of individuals • can be a potential sign of underlying cardiac disease (cardiomyopathies, channelopathies) • patient evaluation – 12 -lead ECG, ecg holter, echo, . . . • majority doesn´t need any treatment
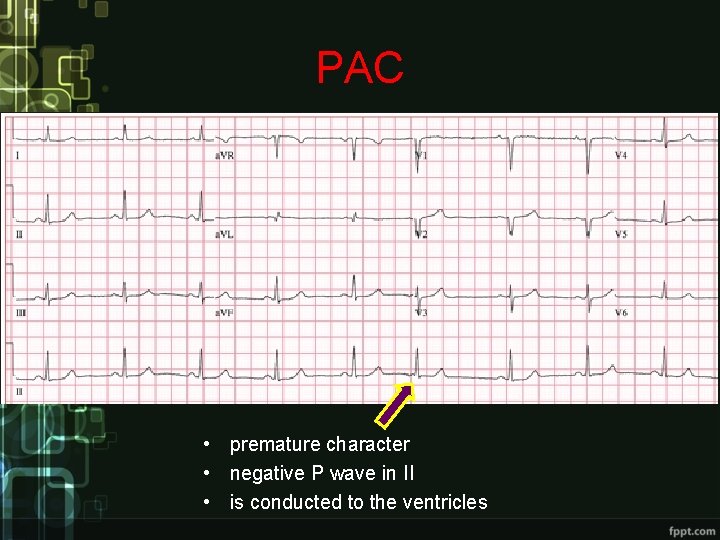
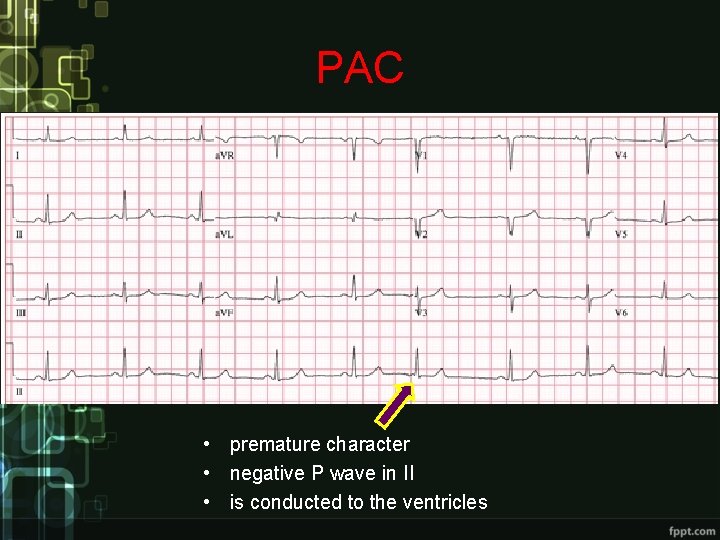
PAC • premature character • negative P wave in II • is conducted to the ventricles
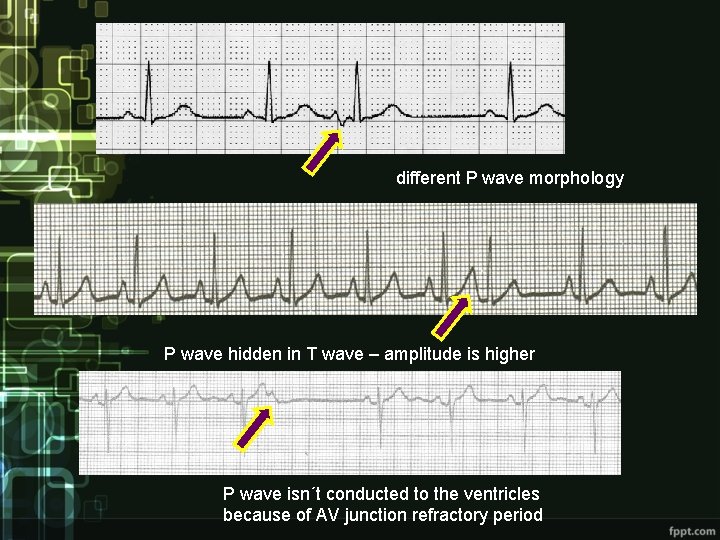
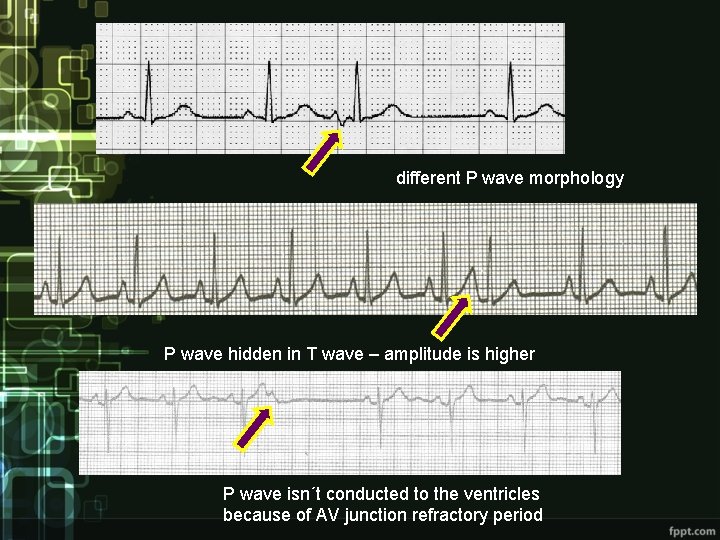
different P wave morphology P wave hidden in T wave – amplitude is higher P wave isn´t conducted to the ventricles because of AV junction refractory period
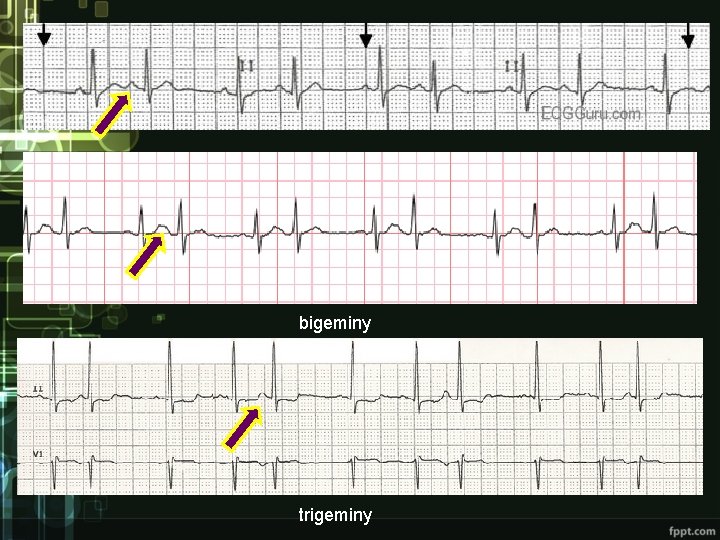
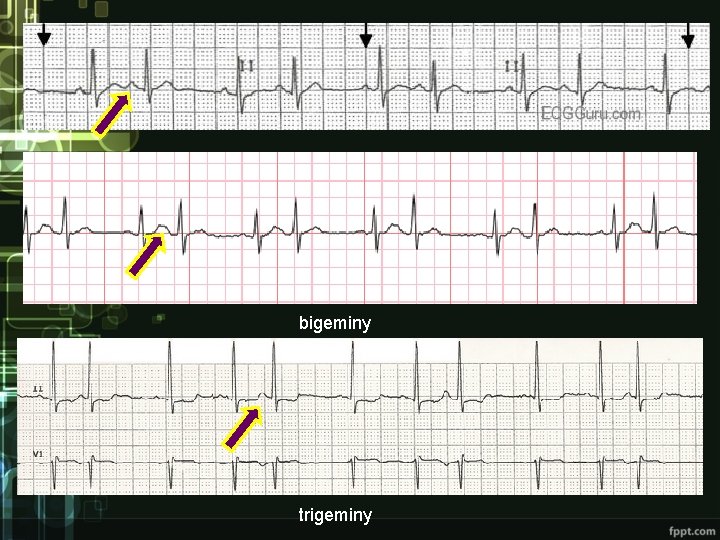
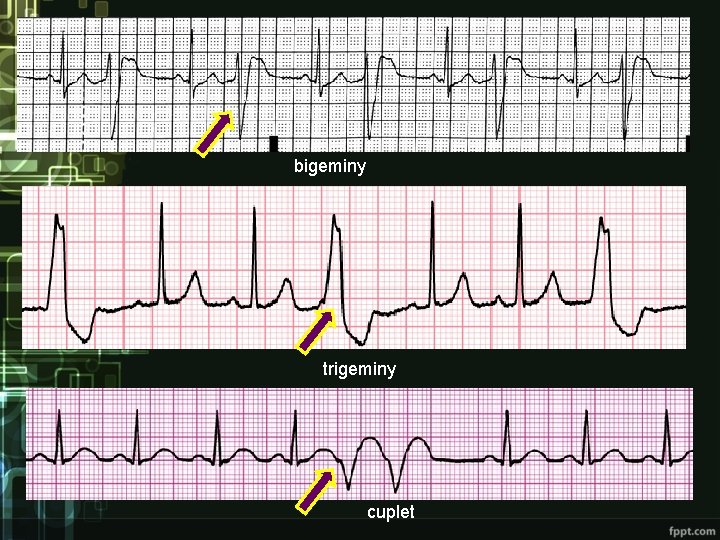
bigeminy trigeminy
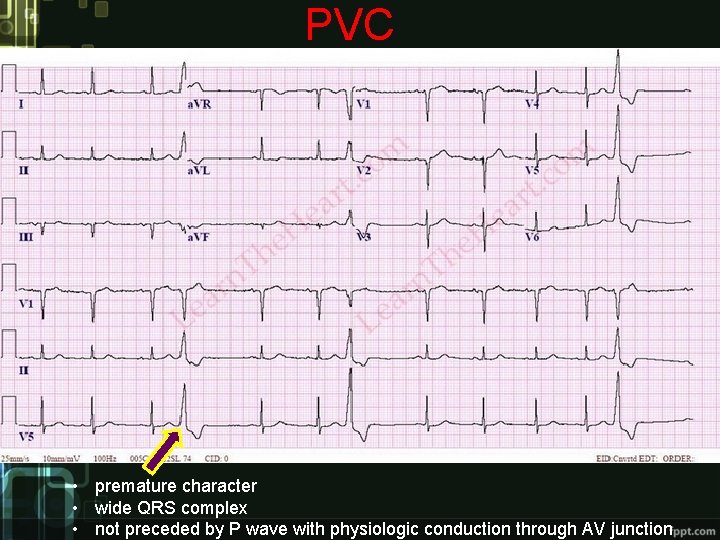
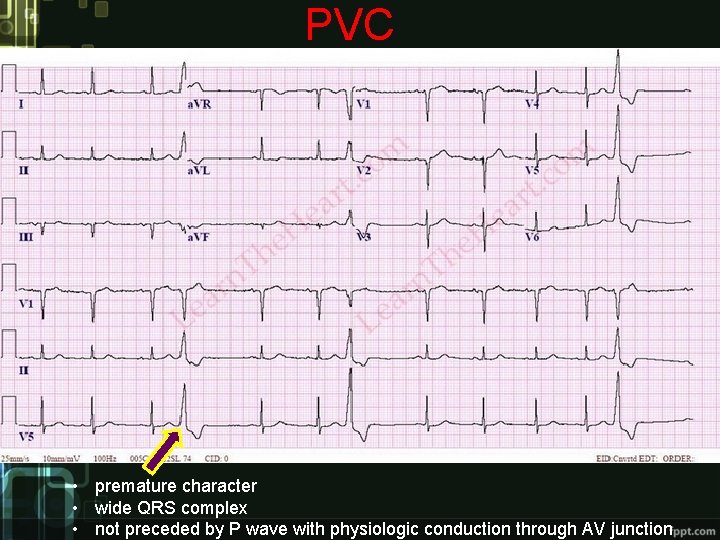
PVC • premature character • wide QRS complex • not preceded by P wave with physiologic conduction through AV junction
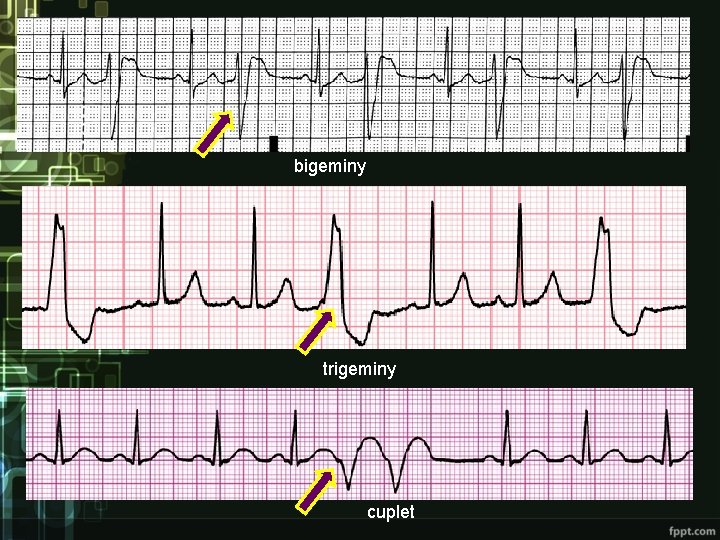
bigeminy trigeminy cuplet
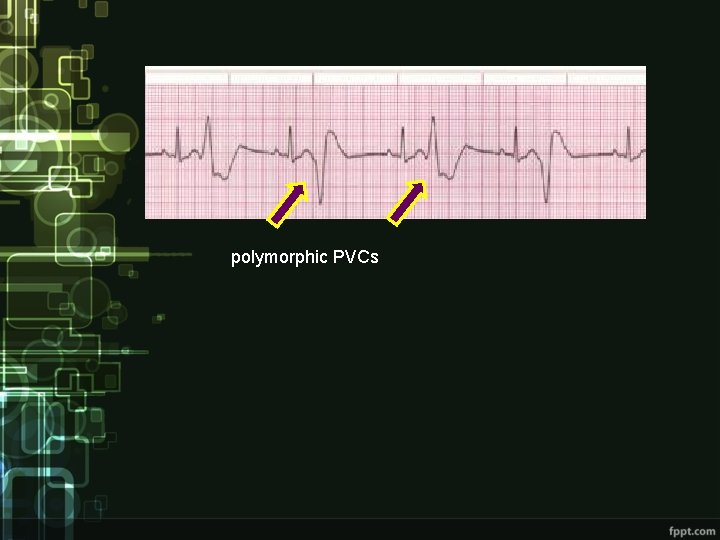
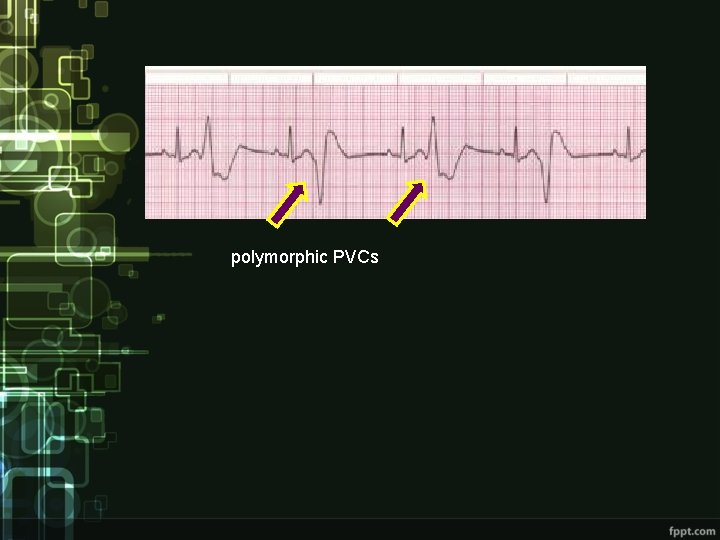
polymorphic PVCs
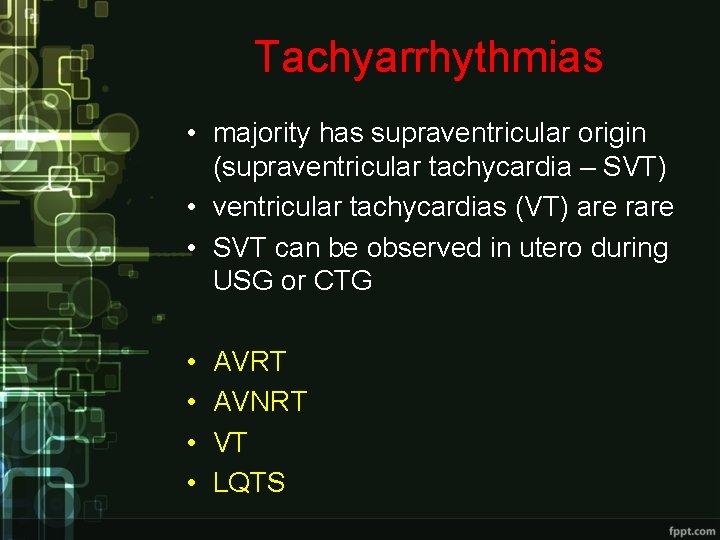
Tachyarrhythmias • majority has supraventricular origin (supraventricular tachycardia – SVT) • ventricular tachycardias (VT) are rare • SVT can be observed in utero during USG or CTG • • AVRT AVNRT VT LQTS

SVT
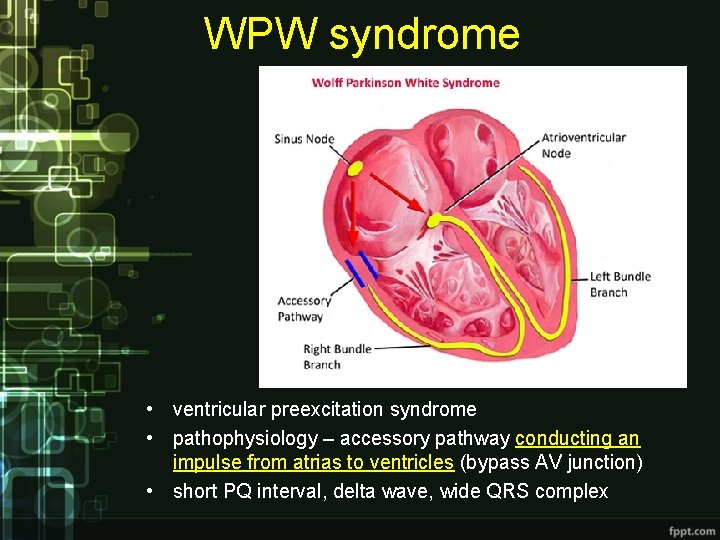
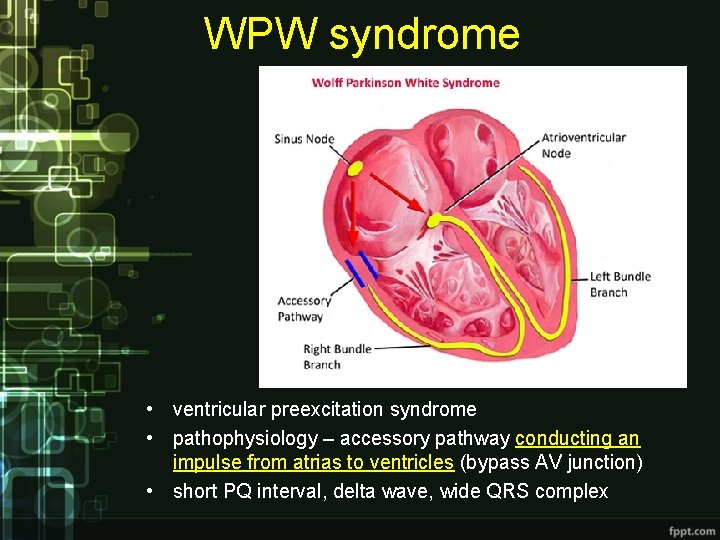
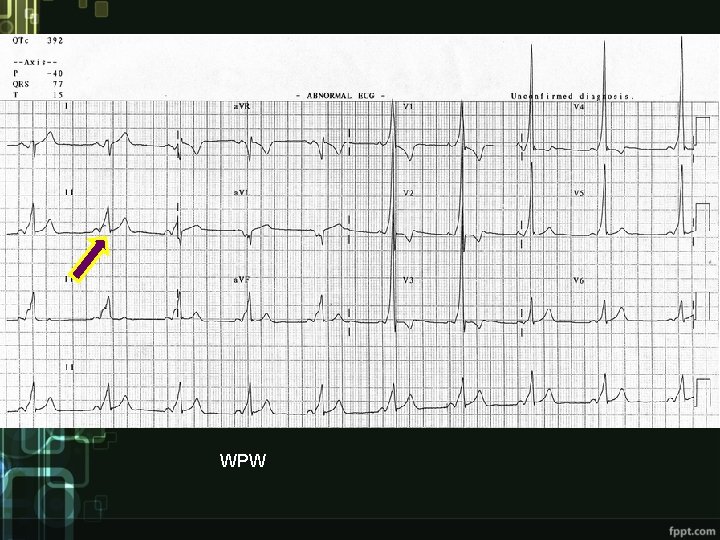
WPW syndrome • ventricular preexcitation syndrome • pathophysiology – accessory pathway conducting an impulse from atrias to ventricles (bypass AV junction) • short PQ interval, delta wave, wide QRS complex
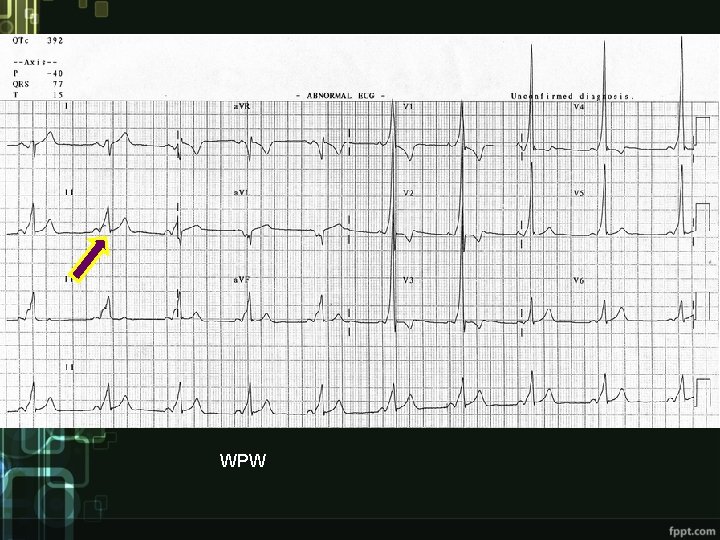
WPW
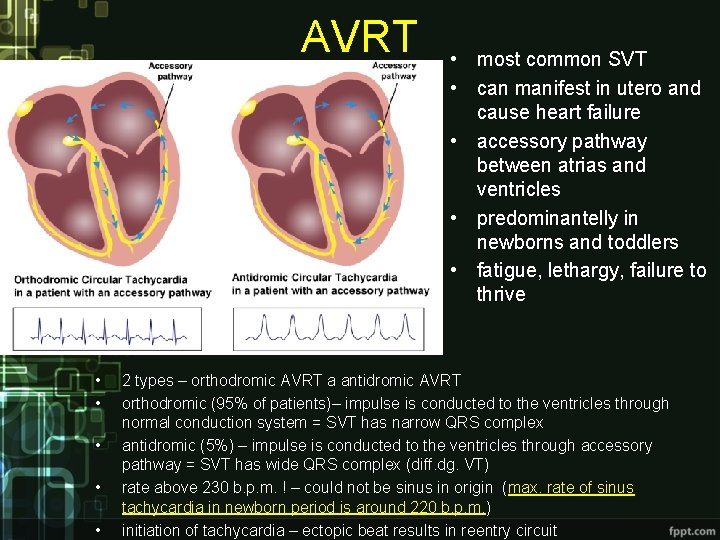
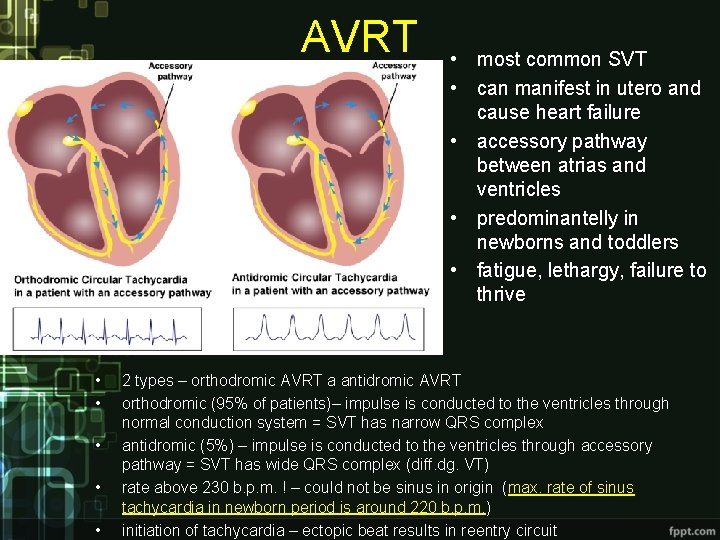
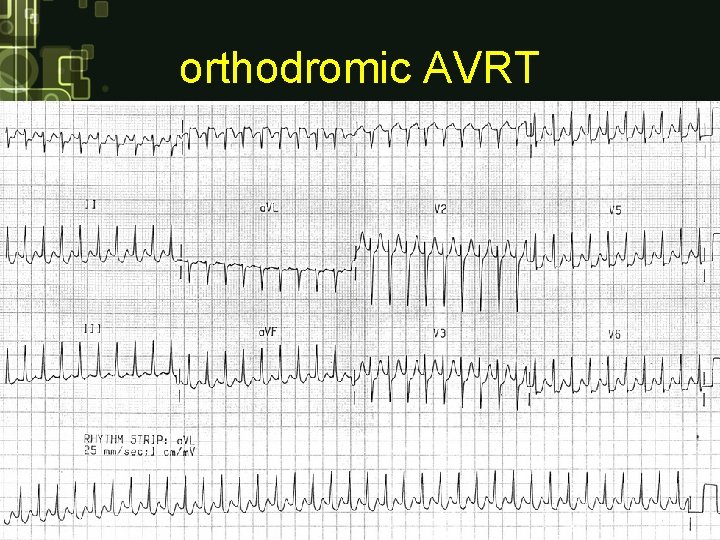
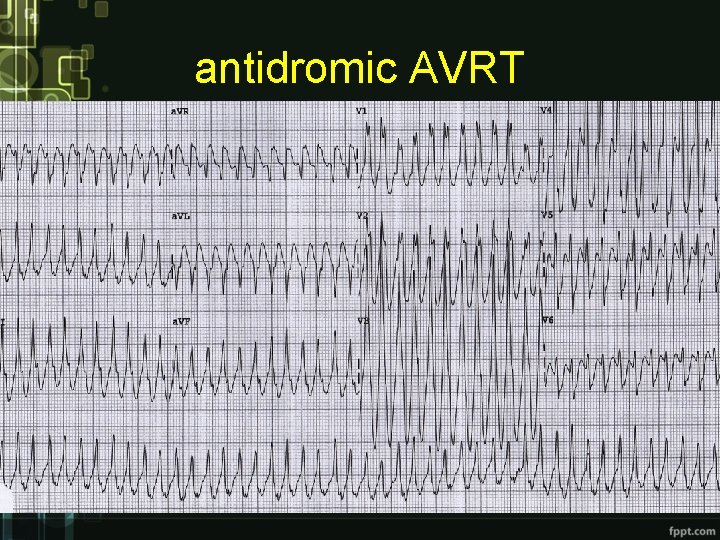
AVRT • • • most common SVT • can manifest in utero and cause heart failure • accessory pathway between atrias and ventricles • predominantelly in newborns and toddlers • fatigue, lethargy, failure to thrive 2 types – orthodromic AVRT a antidromic AVRT orthodromic (95% of patients)– impulse is conducted to the ventricles through normal conduction system = SVT has narrow QRS complex antidromic (5%) – impulse is conducted to the ventricles through accessory pathway = SVT has wide QRS complex (diff. dg. VT) rate above 230 b. p. m. ! – could not be sinus in origin (max. rate of sinus tachycardia in newborn period is around 220 b. p. m. ) initiation of tachycardia – ectopic beat results in reentry circuit
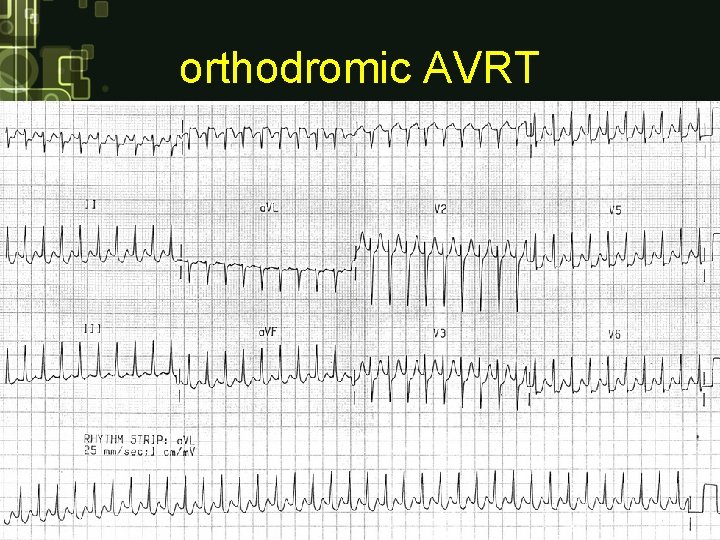
orthodromic AVRT
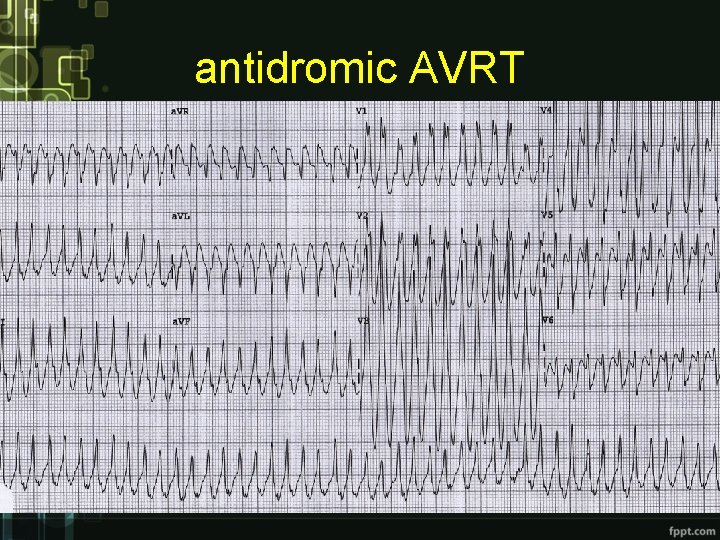
antidromic AVRT
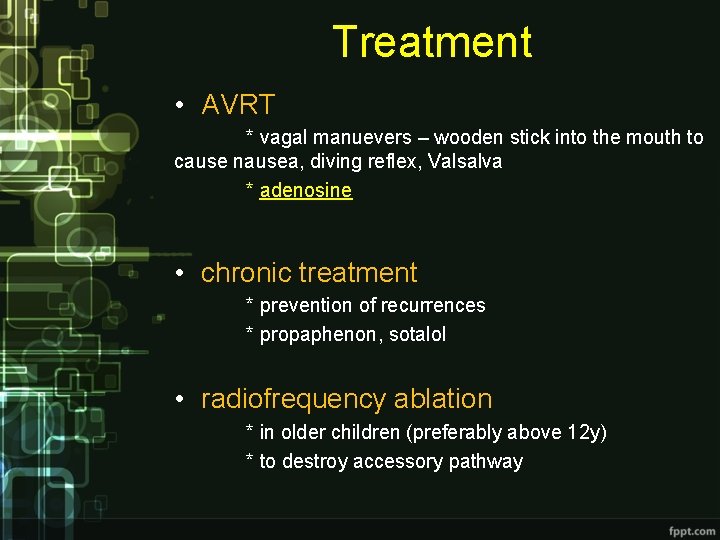
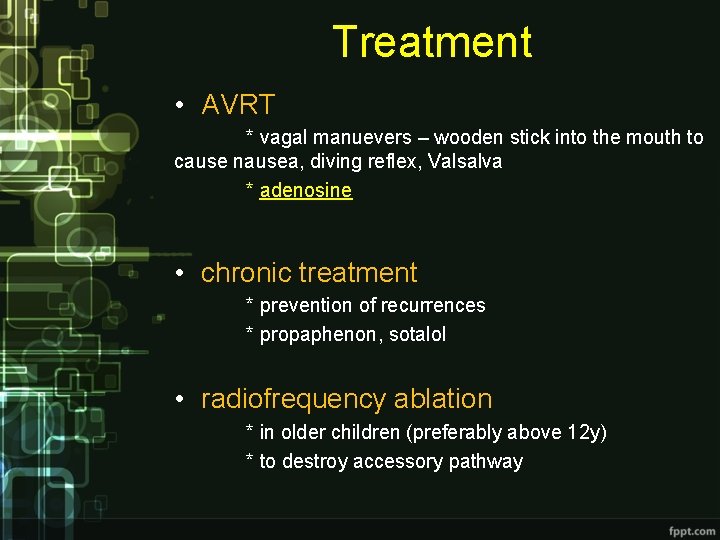
Treatment • AVRT * vagal manuevers – wooden stick into the mouth to cause nausea, diving reflex, Valsalva * adenosine • chronic treatment * prevention of recurrences * propaphenon, sotalol • radiofrequency ablation * in older children (preferably above 12 y) * to destroy accessory pathway
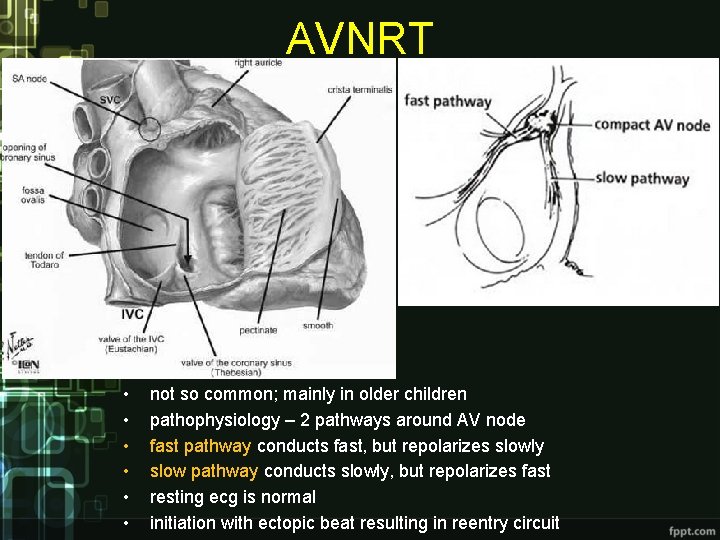
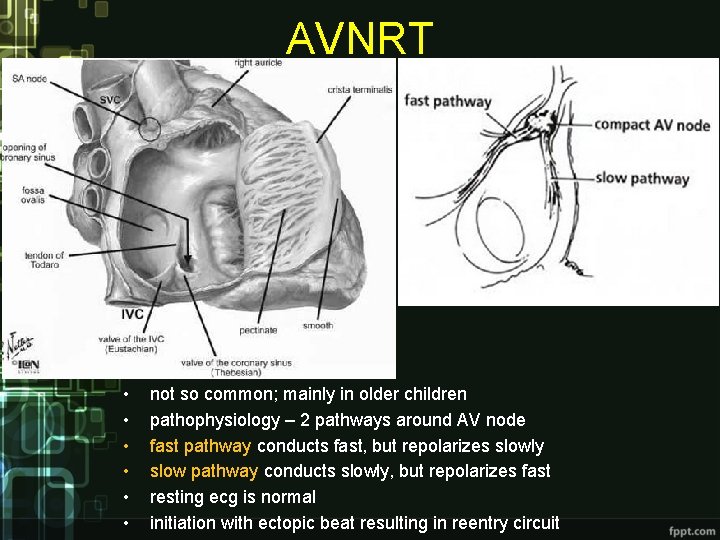
AVNRT • • • not so common; mainly in older children pathophysiology – 2 pathways around AV node fast pathway conducts fast, but repolarizes slowly slow pathway conducts slowly, but repolarizes fast resting ecg is normal initiation with ectopic beat resulting in reentry circuit
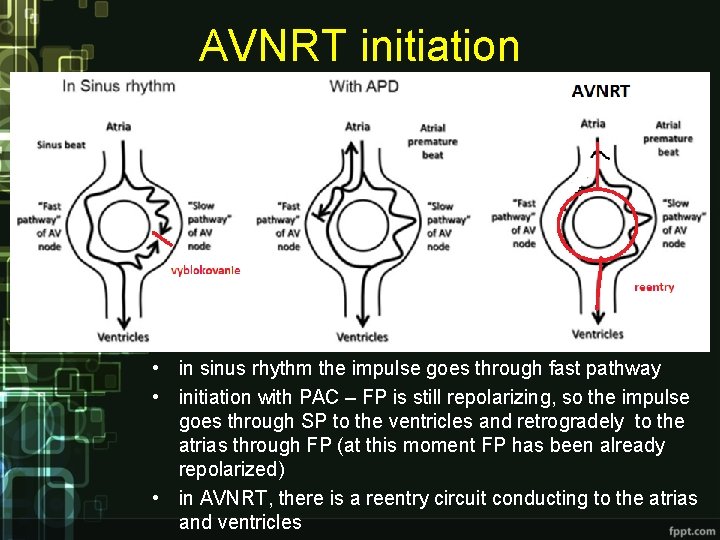
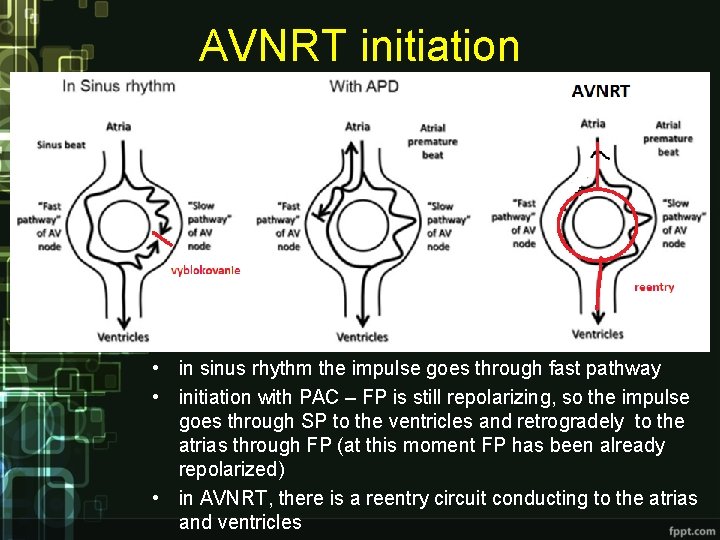
AVNRT initiation • in sinus rhythm the impulse goes through fast pathway • initiation with PAC – FP is still repolarizing, so the impulse goes through SP to the ventricles and retrogradely to the atrias through FP (at this moment FP has been already repolarized) • in AVNRT, there is a reentry circuit conducting to the atrias and ventricles
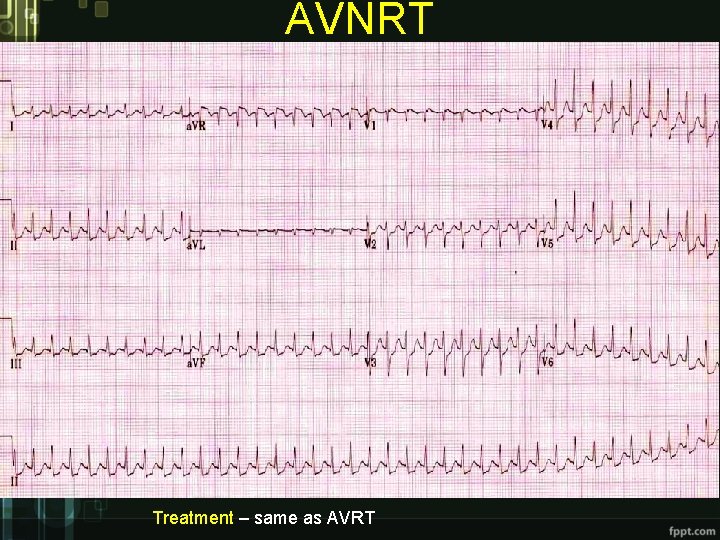
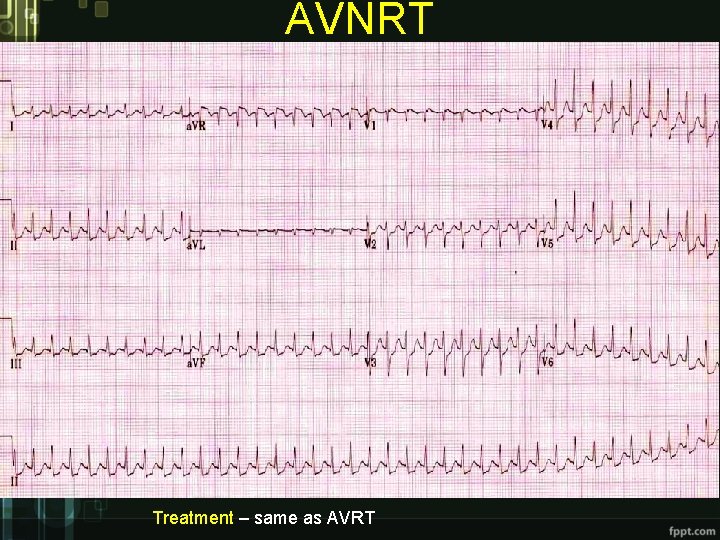
AVNRT Treatment – same as AVRT
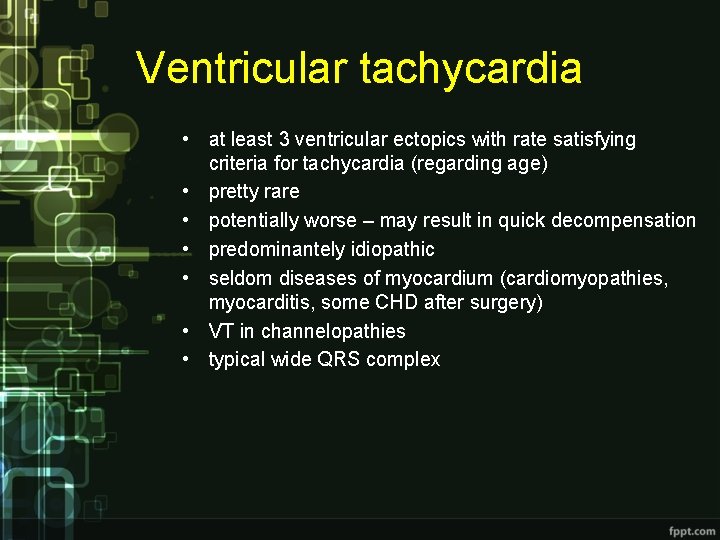
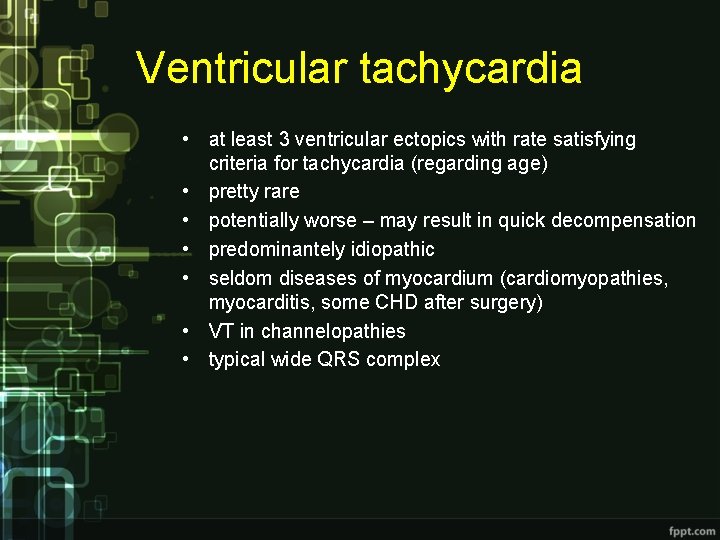
Ventricular tachycardia • at least 3 ventricular ectopics with rate satisfying criteria for tachycardia (regarding age) • pretty rare • potentially worse – may result in quick decompensation • predominantely idiopathic • seldom diseases of myocardium (cardiomyopathies, myocarditis, some CHD after surgery) • VT in channelopathies • typical wide QRS complex
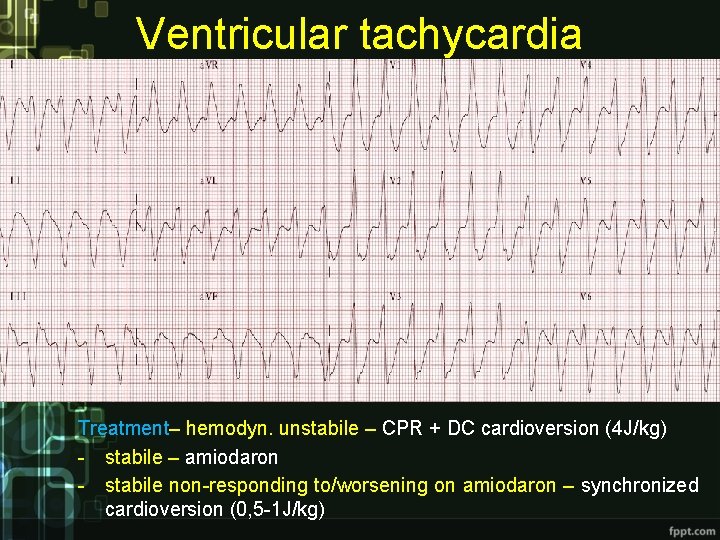
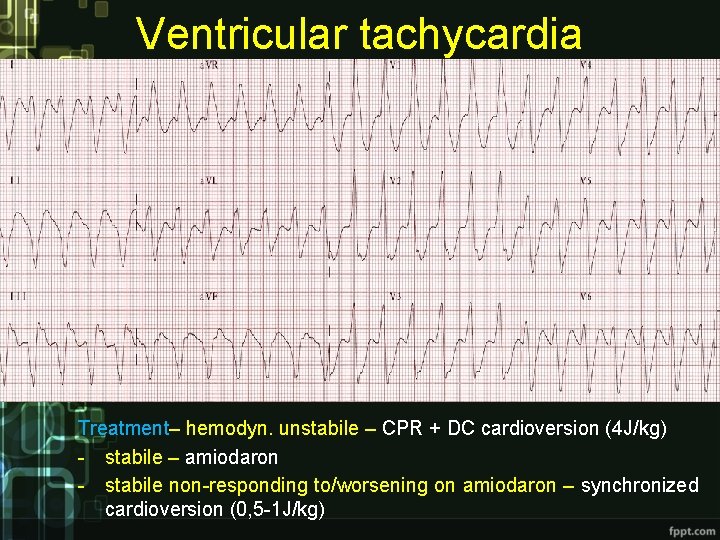
Ventricular tachycardia Treatment– hemodyn. unstabile – CPR + DC cardioversion (4 J/kg) - stabile – amiodaron - stabile non-responding to/worsening on amiodaron – synchronized cardioversion (0, 5 -1 J/kg)
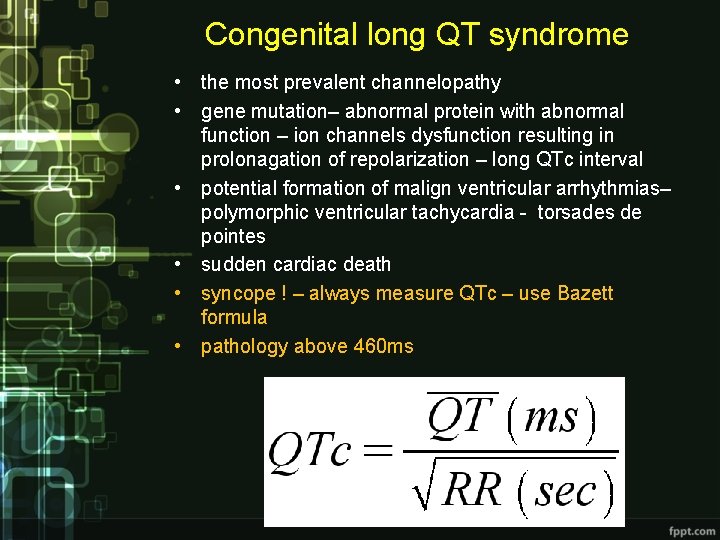
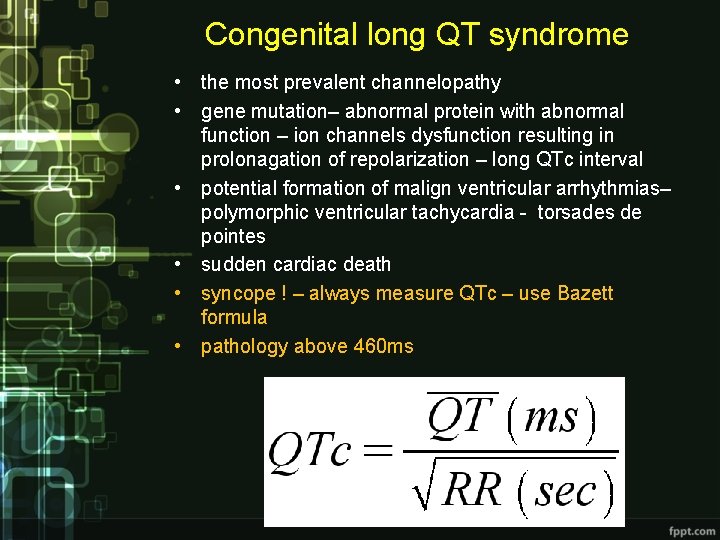
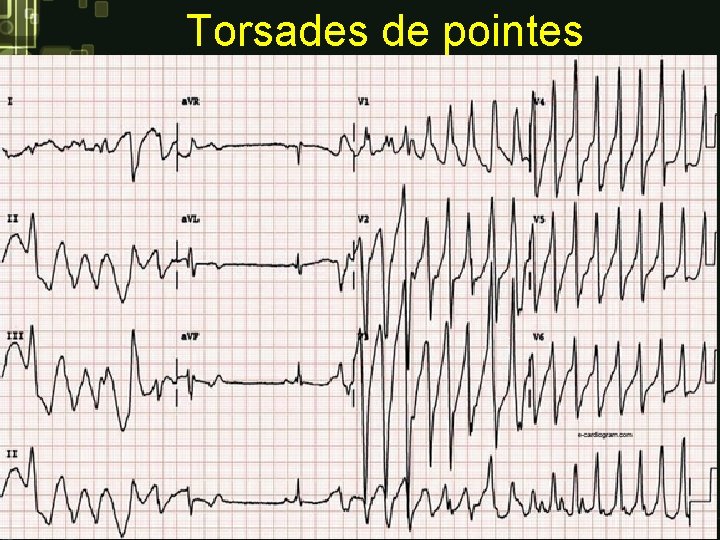
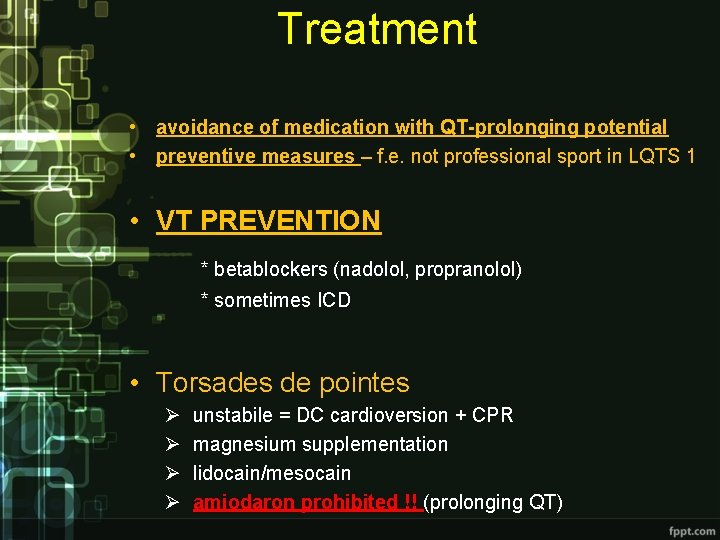
Congenital long QT syndrome • the most prevalent channelopathy • gene mutation– abnormal protein with abnormal function – ion channels dysfunction resulting in prolonagation of repolarization – long QTc interval • potential formation of malign ventricular arrhythmias– polymorphic ventricular tachycardia - torsades de pointes • sudden cardiac death • syncope ! – always measure QTc – use Bazett formula • pathology above 460 ms
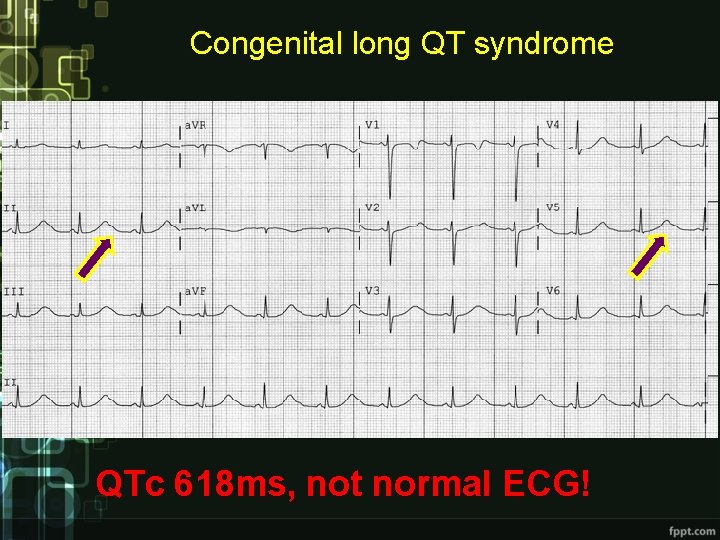
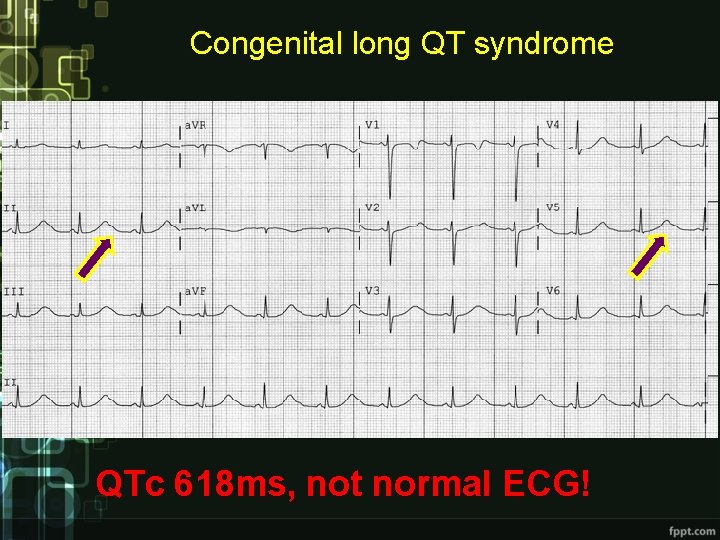
Congenital long QT syndrome QTc 618 ms, not normal ECG!
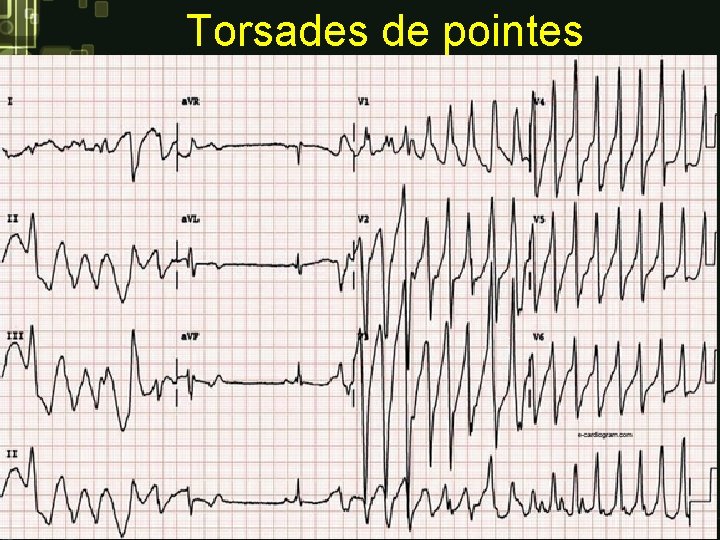
Torsades de pointes
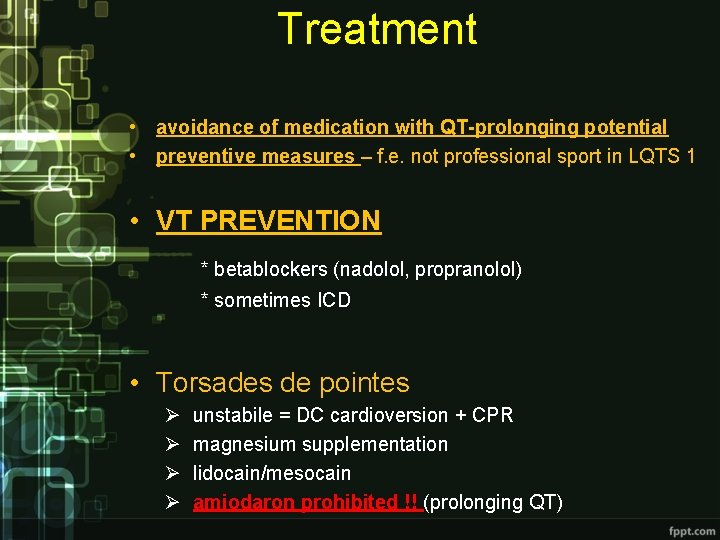
Treatment • avoidance of medication with QT-prolonging potential • preventive measures – f. e. not professional sport in LQTS 1 • VT PREVENTION * betablockers (nadolol, propranolol) * sometimes ICD • Torsades de pointes Ø Ø unstabile = DC cardioversion + CPR magnesium supplementation lidocain/mesocain amiodaron prohibited !! (prolonging QT)
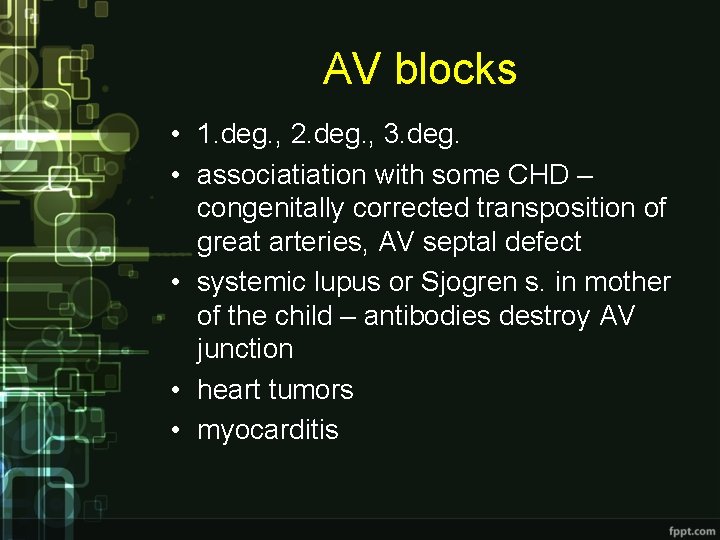
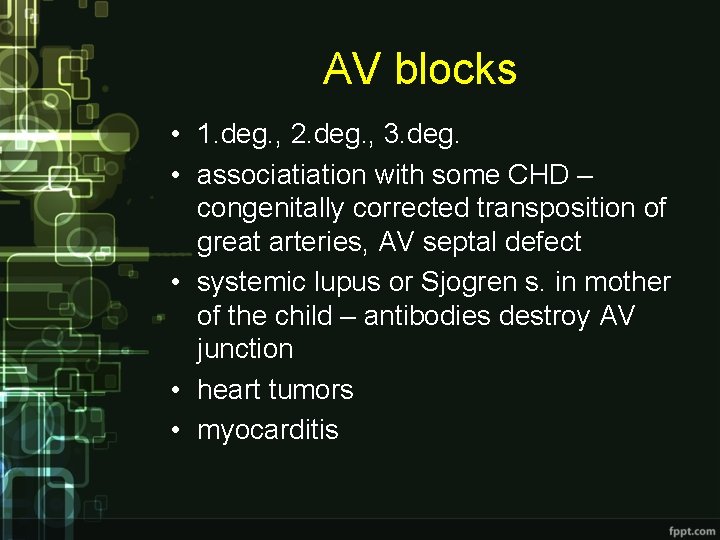
AV blocks • 1. deg. , 2. deg. , 3. deg. • associatiation with some CHD – congenitally corrected transposition of great arteries, AV septal defect • systemic lupus or Sjogren s. in mother of the child – antibodies destroy AV junction • heart tumors • myocarditis
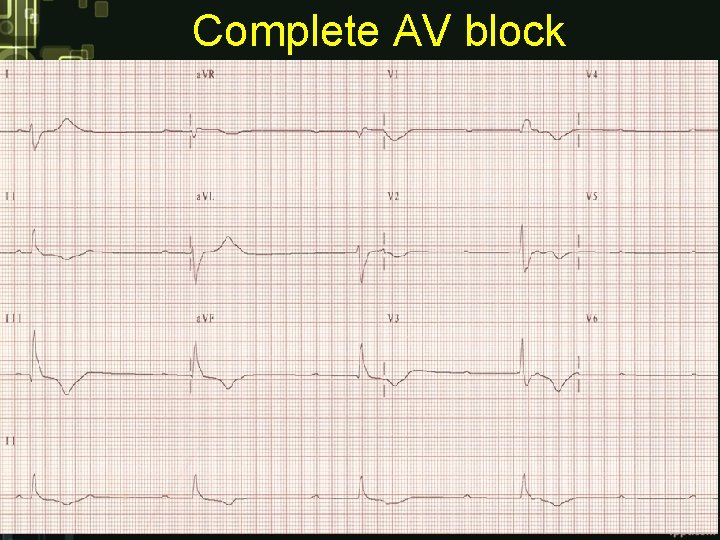
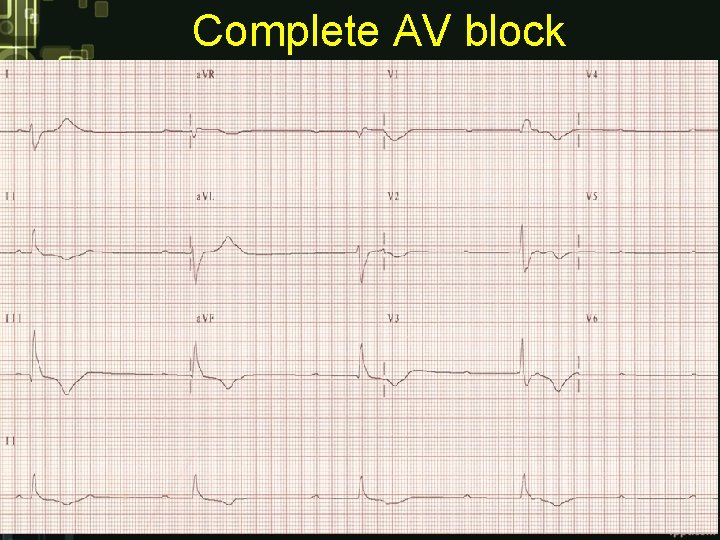
Complete AV block
Treatment • pharmacological - euphyllin • pacemaker

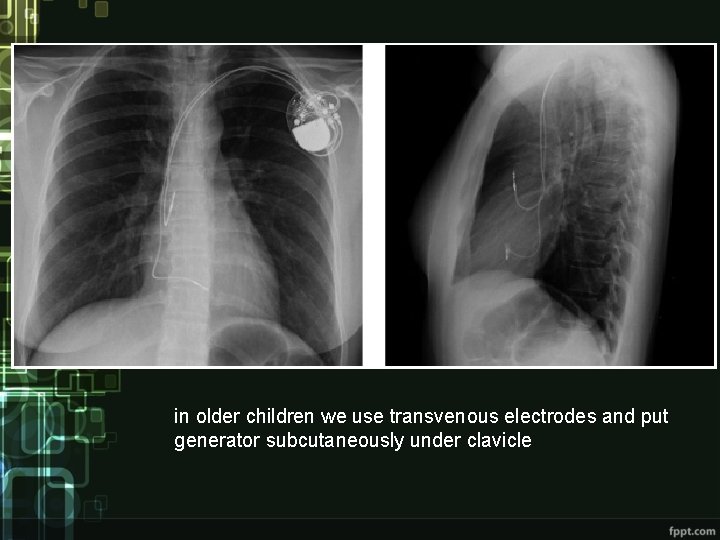
in small children we implant epicardial electrodes and put generator into the belly
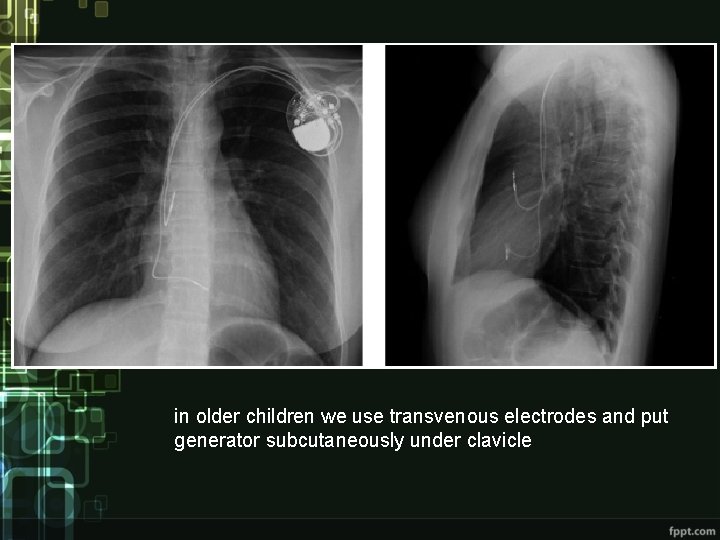
in older children we use transvenous electrodes and put generator subcutaneously under clavicle
Questions 1. How would characterize sinus rhythm and sinus respiratory arrhythmia? Causes of sinus tachycardia and bradycardia. 2. What is WPW syndrome and how does it look on ECG? Define AVRT – pathophysiology, occurence, types, heart rate, initiation, clinical condition and treatment. 3. Define ventricular tachycardiu, occurence, causes and treatment. 4. Congenital long QT syndrome – cause, basic pathophysiology, ECG, Bazett formula, clinical condition, treatment. Why are those patients at risk? 5. AV blocks – types, ECG characteristics, causes, treatment.