Pediatric ARDS Understanding It and Managing It James
- Slides: 48
Pediatric ARDS: Understanding It and Managing It James D. Fortenberry, MD Medical Director, Pediatric and Adult ECMO Medical Director, Critical Care Medicine Children’s Healthcare of Atlanta at Egleston
New and Improved Adult Respiratory Distress Syndrome Acute Respiratory Distress Syndrome
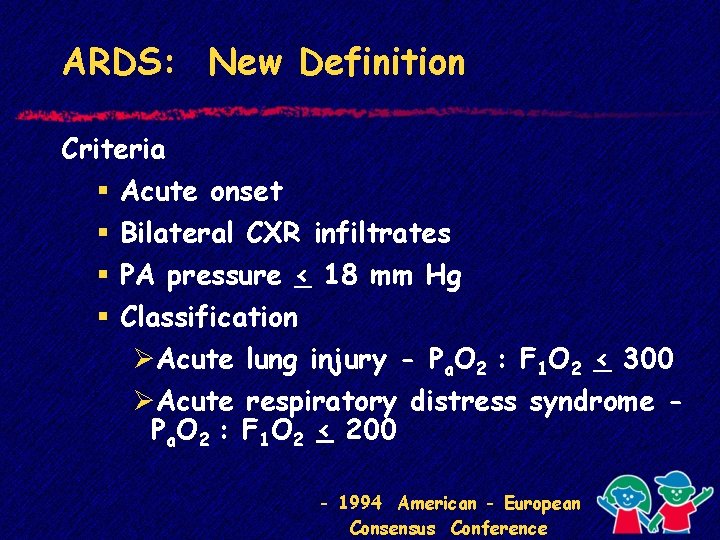
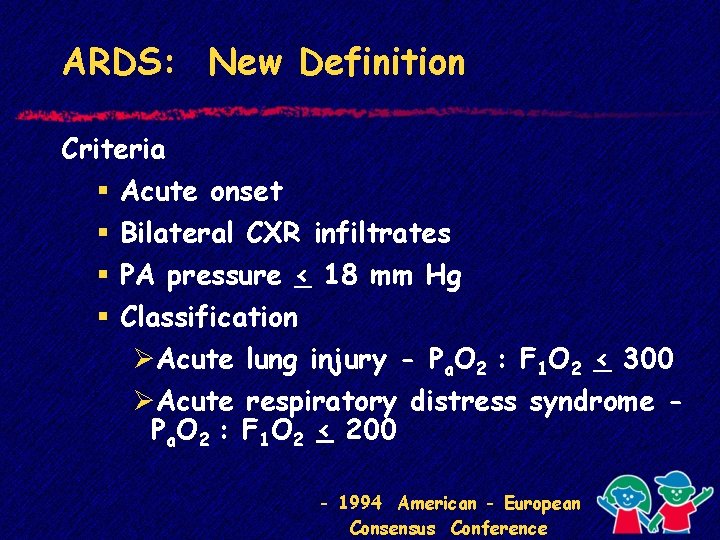
ARDS: New Definition Criteria § § Acute onset Bilateral CXR infiltrates PA pressure < 18 mm Hg Classification ØAcute lung injury - Pa. O 2 : F 1 O 2 < 300 ØAcute respiratory distress syndrome Pa. O 2 : F 1 O 2 < 200 - 1994 American - European Consensus Conference
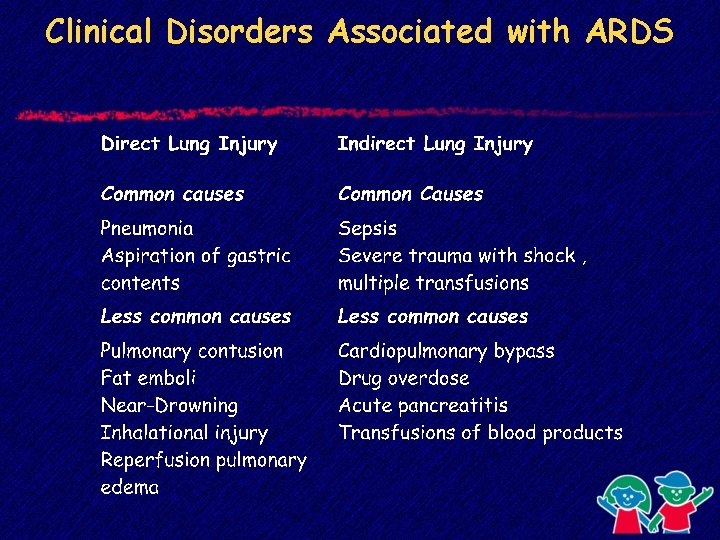
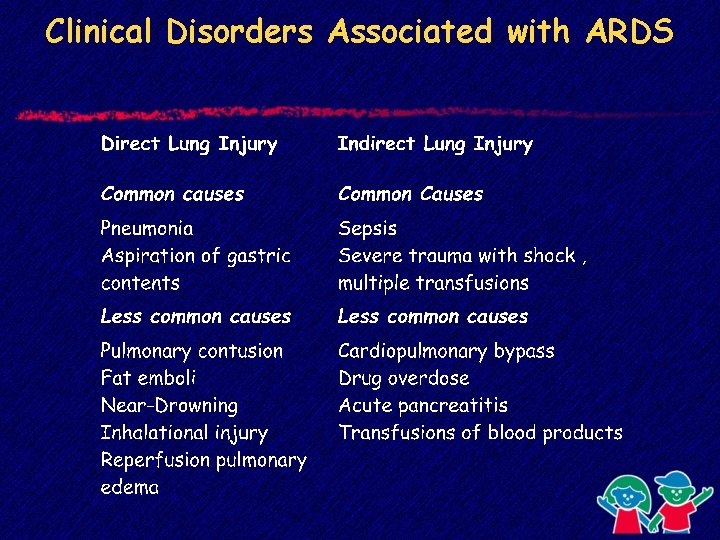
Clinical Disorders Associated with ARDS
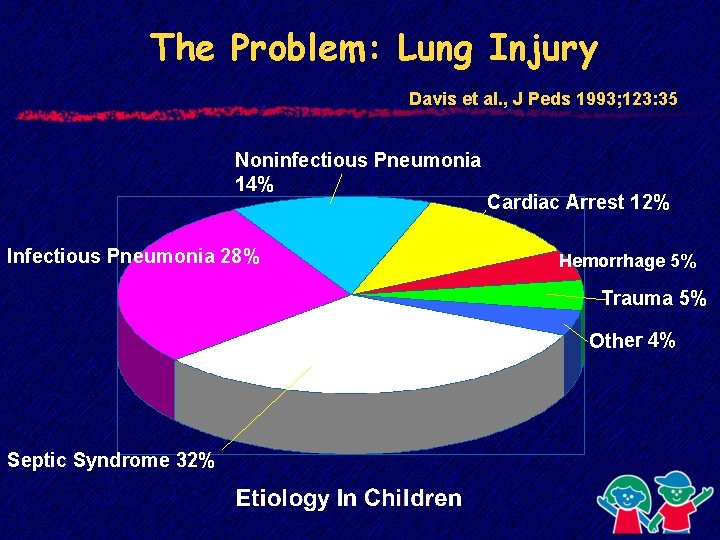
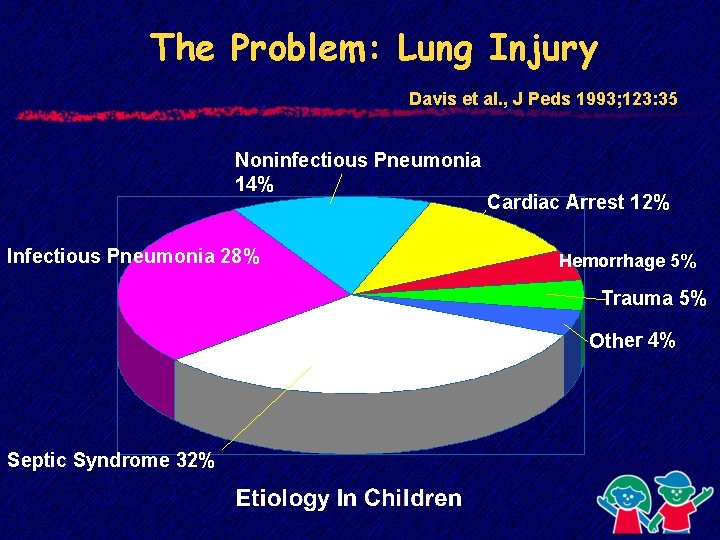
The Problem: Lung Injury Davis et al. , J Peds 1993; 123: 35 Noninfectious Pneumonia 14% Infectious Pneumonia 28% Cardiac Arrest 12% Hemorrhage 5% Trauma 5% Other 4% Septic Syndrome 32%
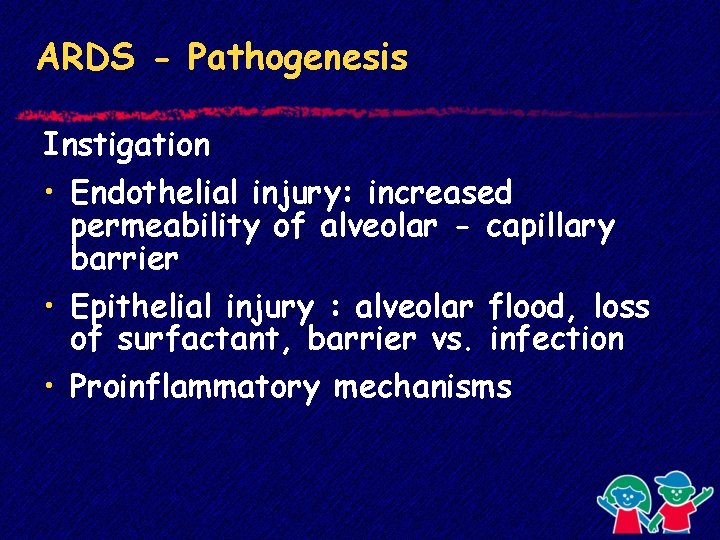
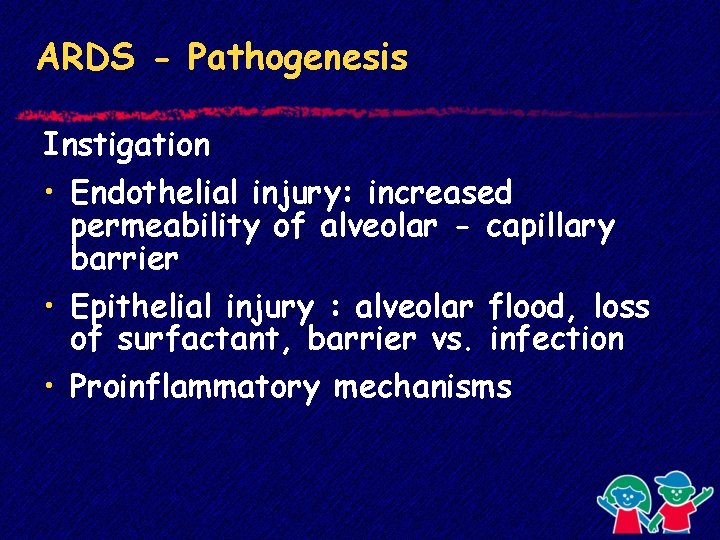
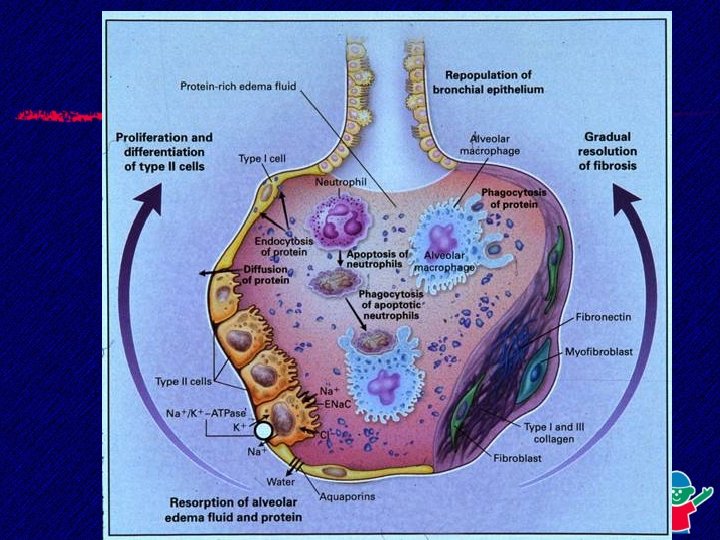
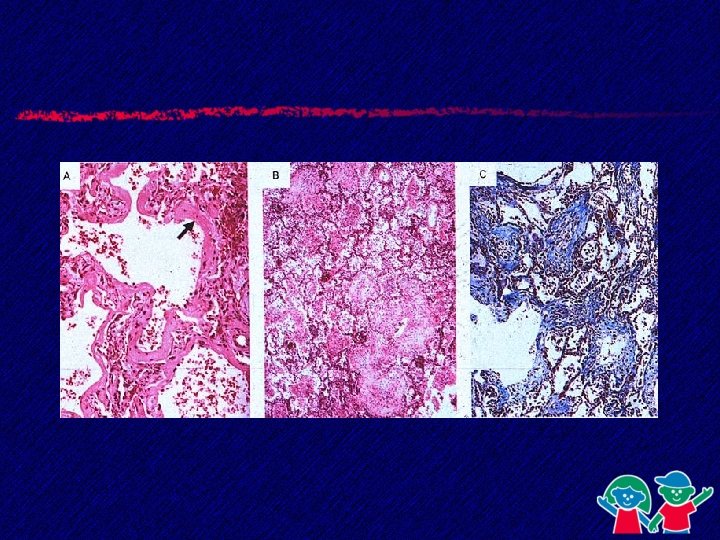
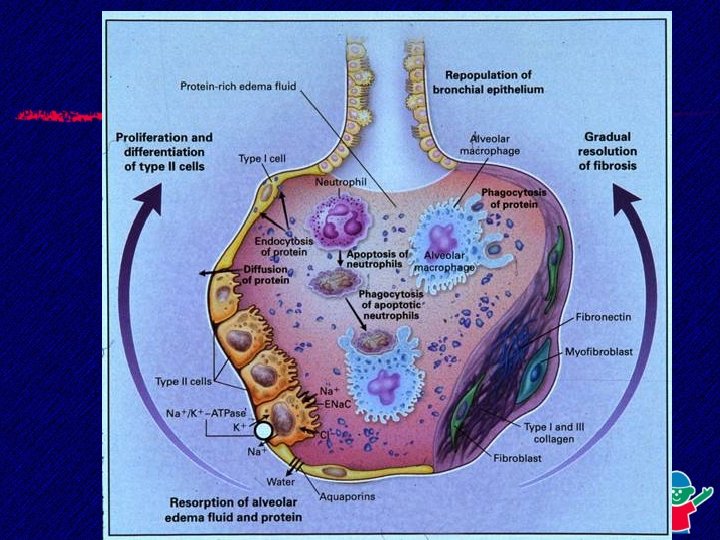
ARDS - Pathogenesis Instigation • Endothelial injury: increased permeability of alveolar - capillary barrier • Epithelial injury : alveolar flood, loss of surfactant, barrier vs. infection • Proinflammatory mechanisms
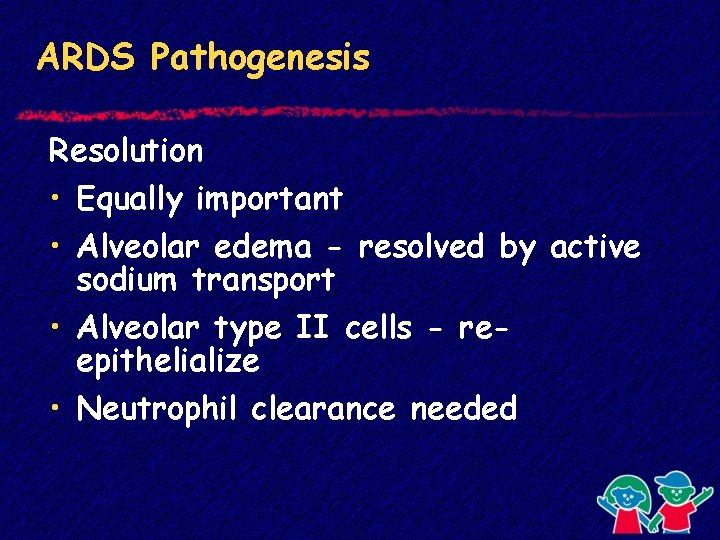
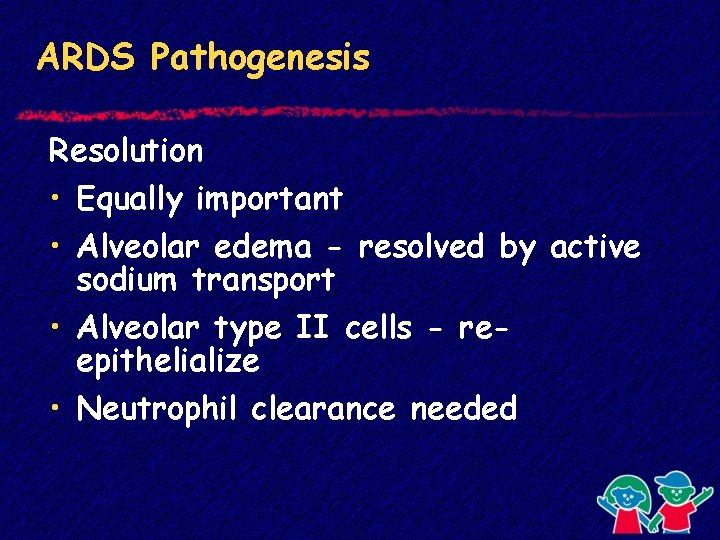
ARDS Pathogenesis Resolution • Equally important • Alveolar edema - resolved by active sodium transport • Alveolar type II cells - reepithelialize • Neutrophil clearance needed
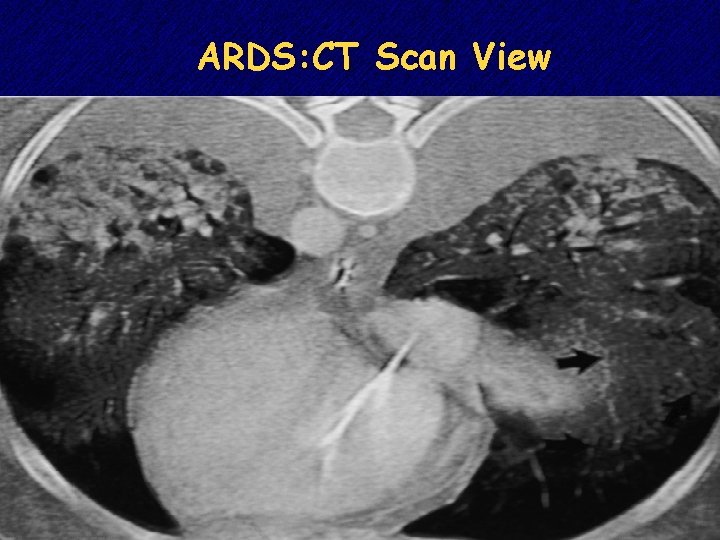
ARDS - Pathophysiology • Decreased compliance • Alveolar edema • Heterogenous • “Baby Lungs”
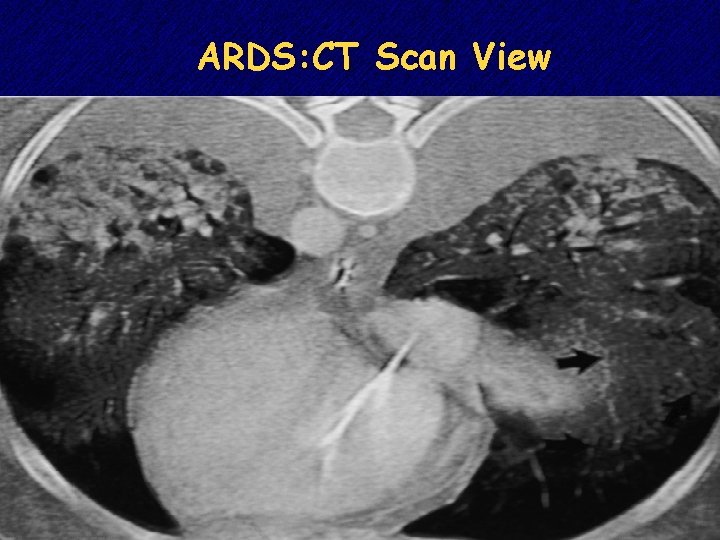
ARDS: CT Scan View
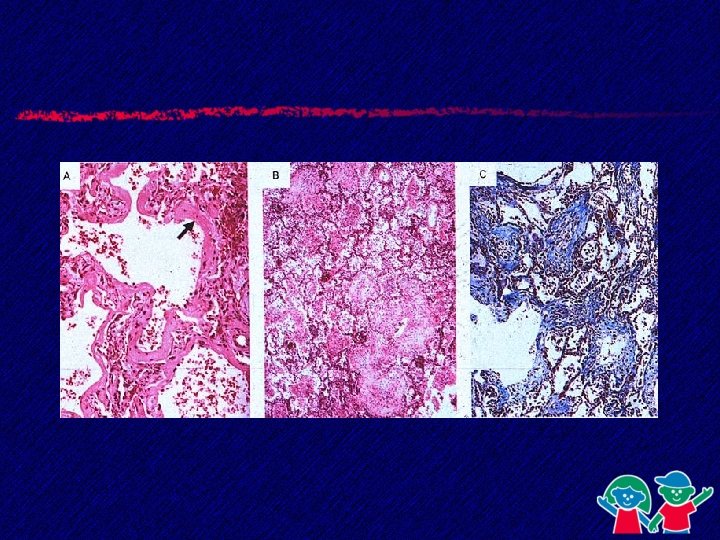
Phases of ARDS • Acute - exudative, inflammatory (0 - 3 days) • Subacute - proliferative (4 - 10 days) • Chronic - fibrosing alveolitis ( > 10 days)
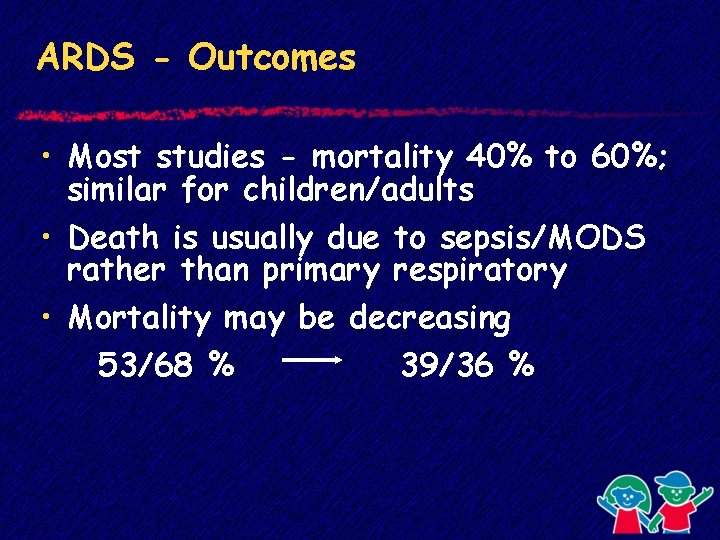
ARDS - Outcomes • Most studies - mortality 40% to 60%; similar for children/adults • Death is usually due to sepsis/MODS rather than primary respiratory • Mortality may be decreasing 53/68 % 39/36 %
ARDS - Principles of Therapy • Provide adequate gas exchange • Avoid secondary injury
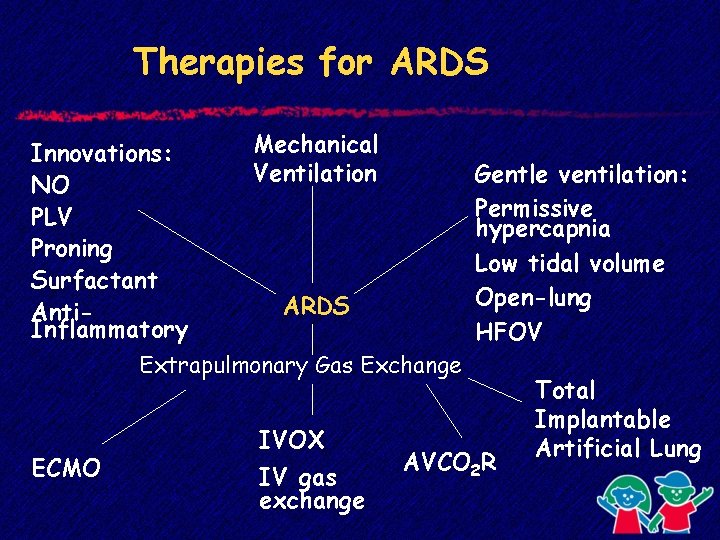
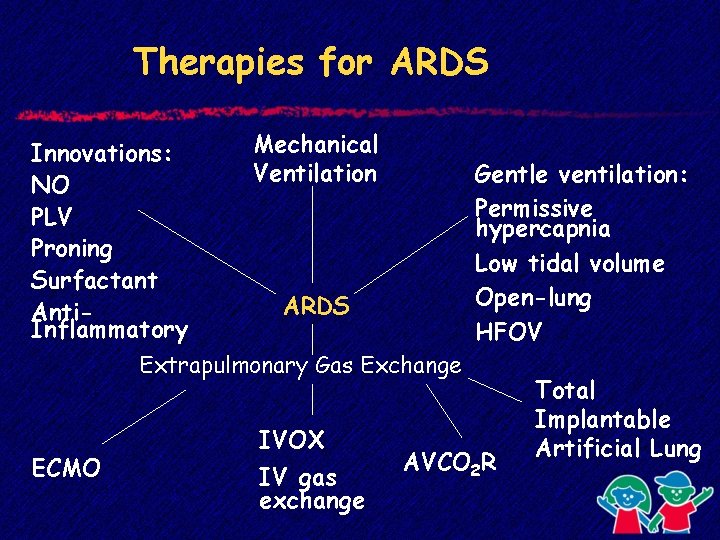
Therapies for ARDS Innovations: NO PLV Proning Surfactant Anti. Inflammatory Mechanical Ventilation Gentle ventilation: Permissive hypercapnia Low tidal volume Open-lung HFOV ARDS Extrapulmonary Gas Exchange ECMO IVOX IV gas exchange AVCO 2 R Total Implantable Artificial Lung
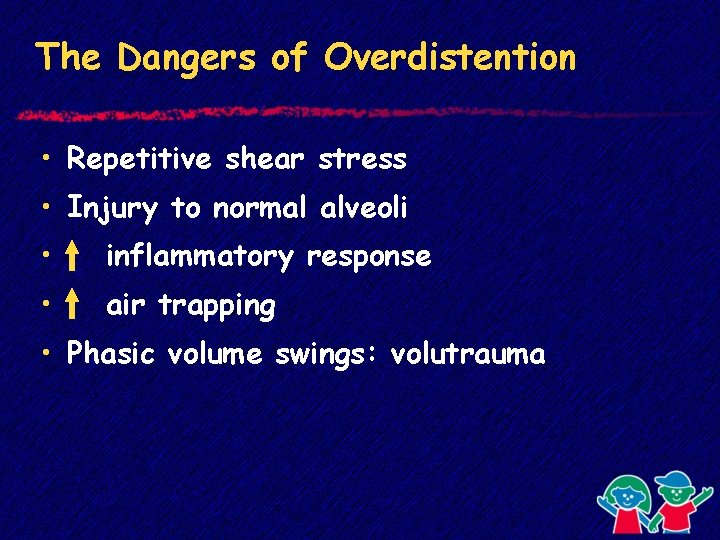
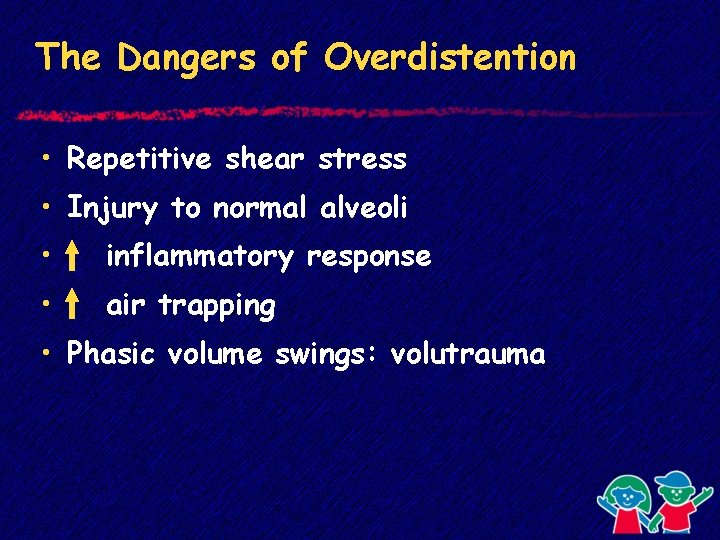
The Dangers of Overdistention • Repetitive shear stress • Injury to normal alveoli • inflammatory response • air trapping • Phasic volume swings: volutrauma
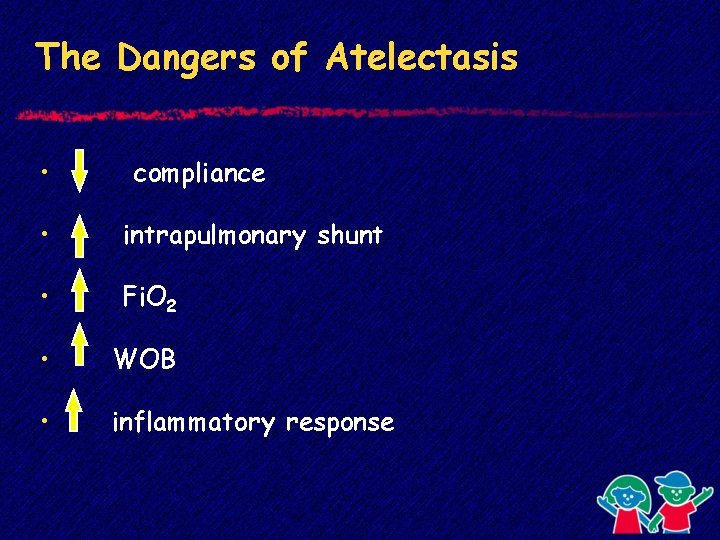
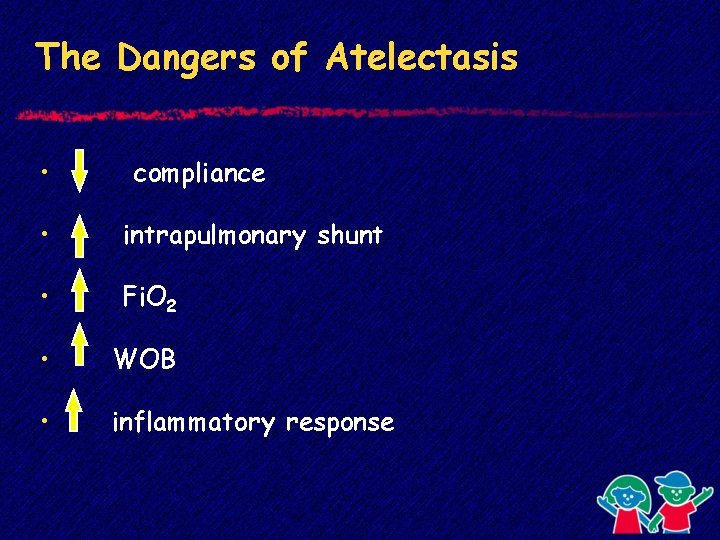
The Dangers of Atelectasis • compliance • intrapulmonary shunt • Fi. O 2 • WOB • inflammatory response
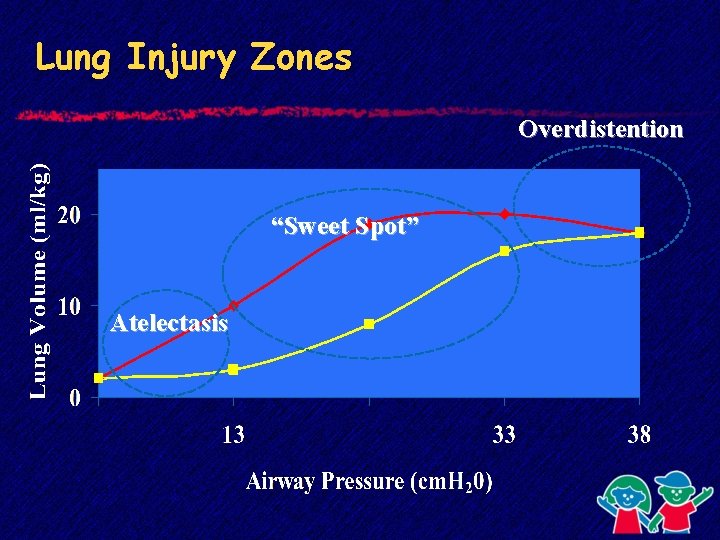
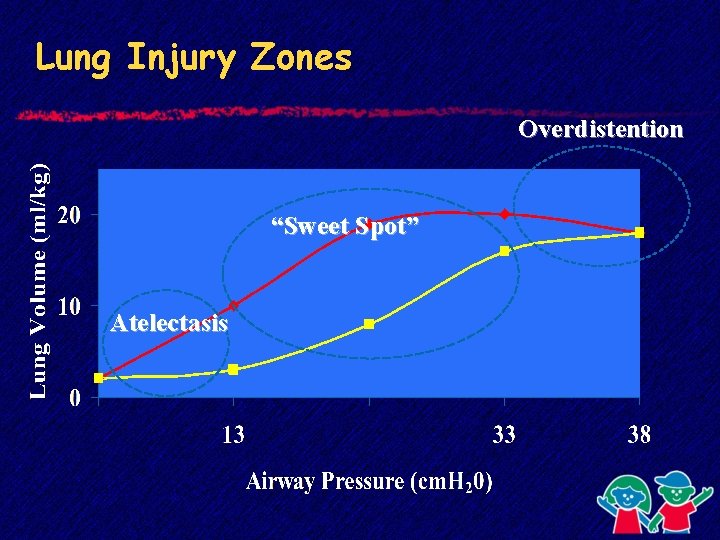
Lung Injury Zones Overdistention “Sweet Spot” Atelectasis
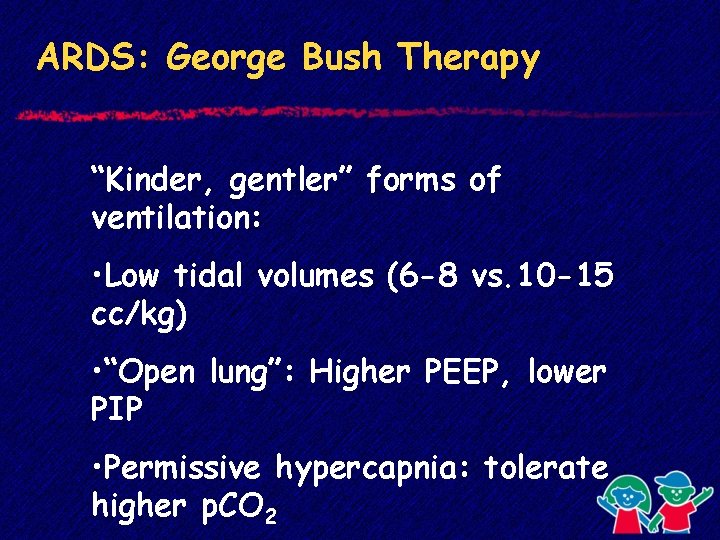
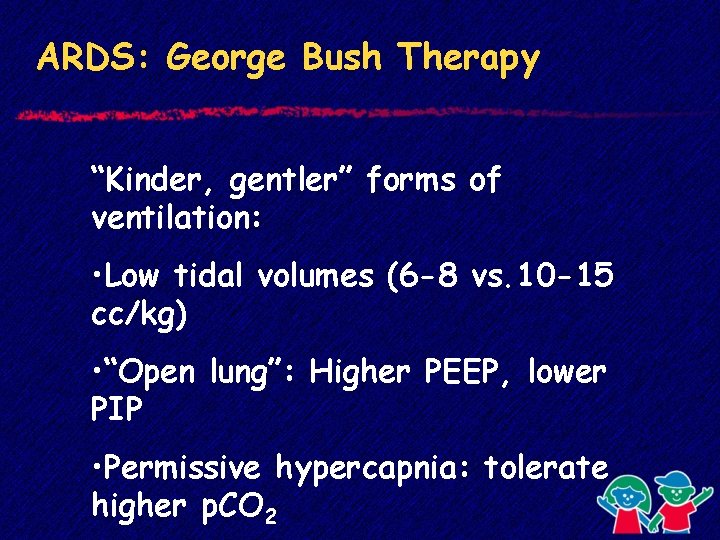
ARDS: George Bush Therapy “Kinder, gentler” forms of ventilation: • Low tidal volumes (6 -8 vs. 10 -15 cc/kg) • “Open lung”: Higher PEEP, lower PIP • Permissive hypercapnia: tolerate higher p. CO 2
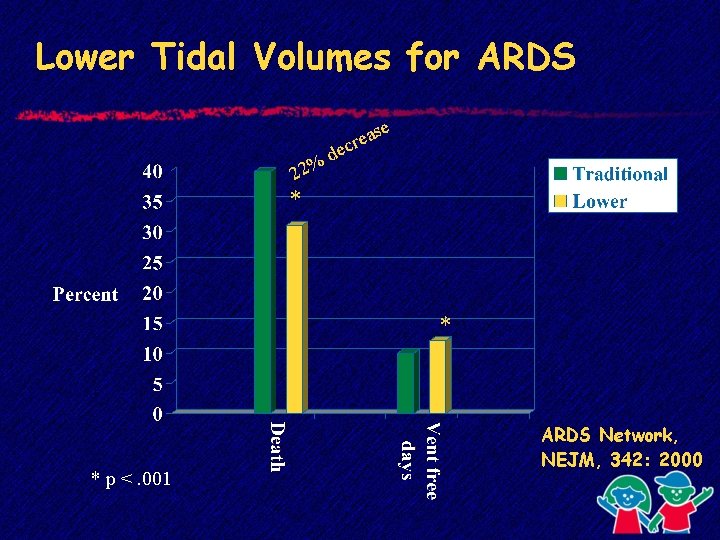
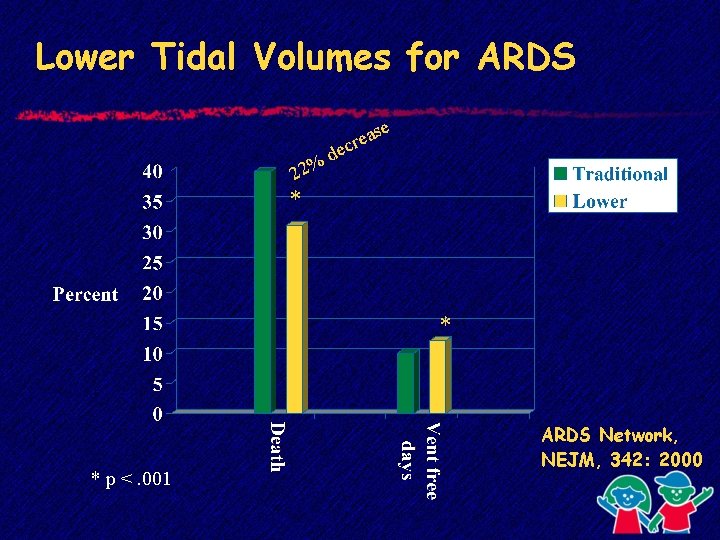
Lower Tidal Volumes for ARDS 22% se a e r dec * * * p <. 001 ARDS Network, NEJM, 342: 2000
Is turning the ARDS patient “prone” to be helpful?
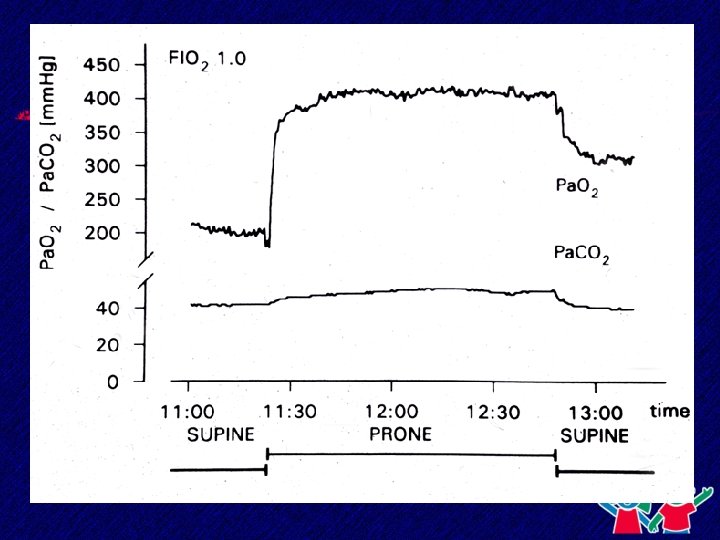
Prone Positioning in ARDS • Theory: let gravity improve matching perfusion to better ventilated areas • Improvement immediate • Uncertain effect on outcome
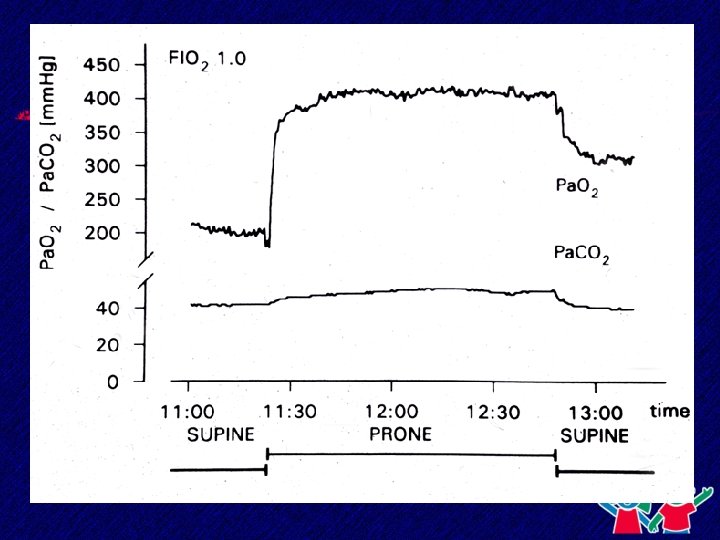
Prone Positioning in Pediatric ARDS: Longer May Be Better • Compared 6 -10 hrs PP vs. 18 -24 hrs PP • Overall ARDS survival 79% in 40 pts. ØRelvas et al. , Chest 2003
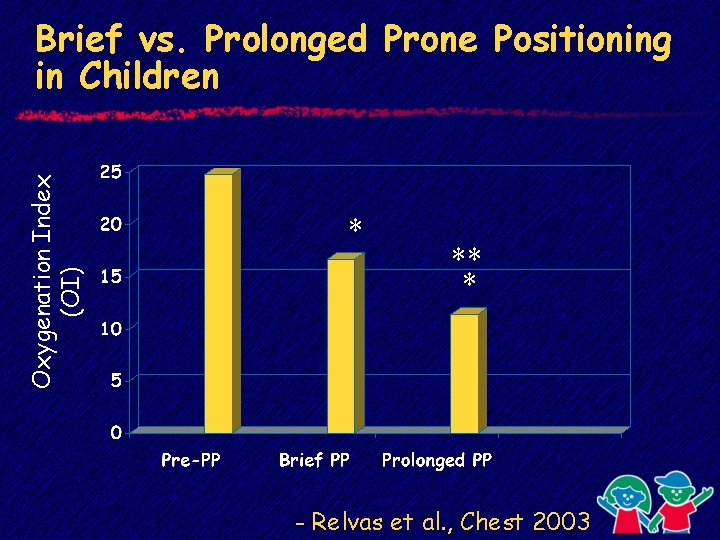
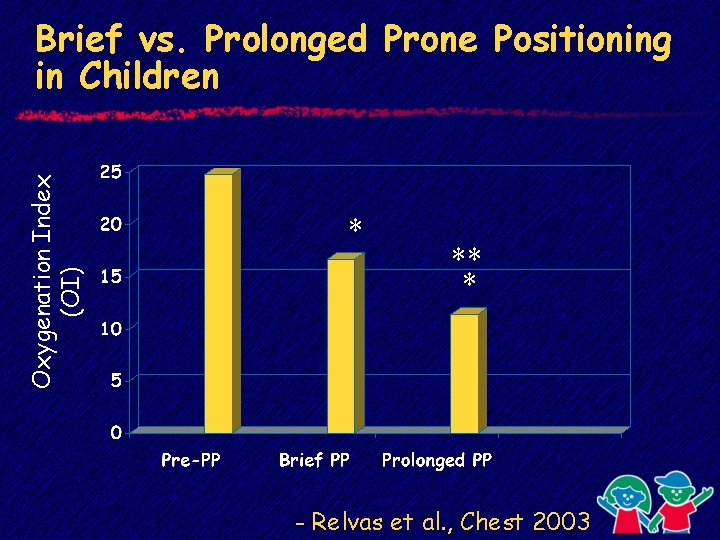
Oxygenation Index (OI) Brief vs. Prolonged Prone Positioning in Children * ** * - Relvas et al. , Chest 2003
High Frequency Oscillation: A Whole Lotta Shakin’ Goin’ On
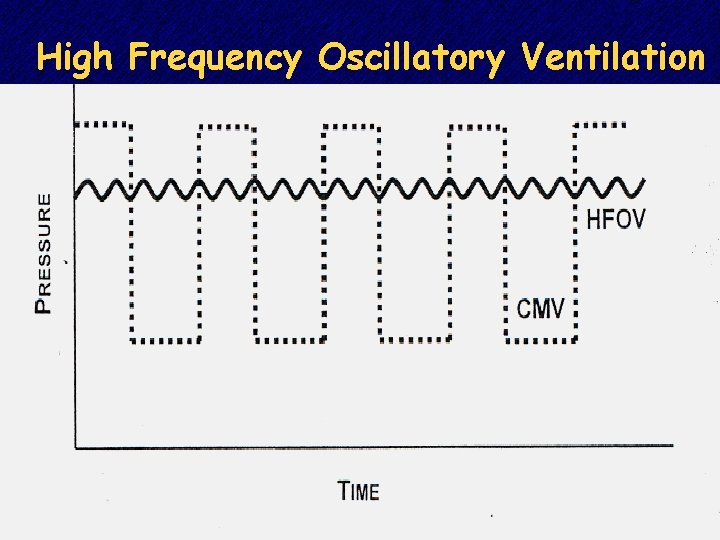
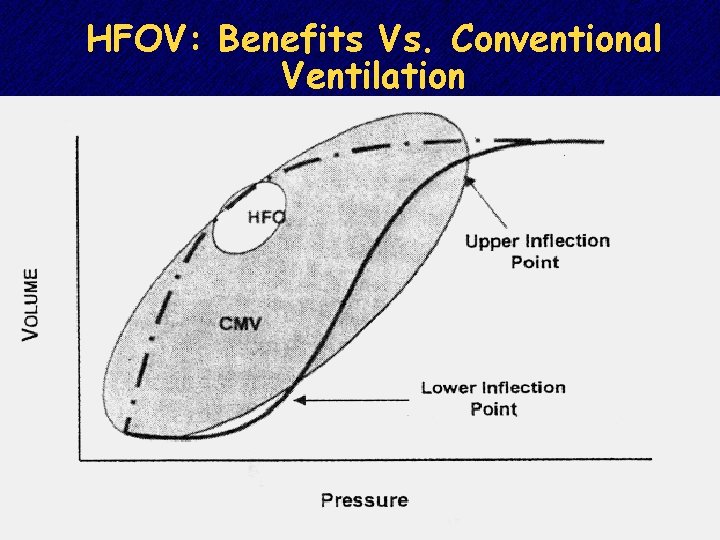
It’s not absolute pressure, but volume or pressure swings that promote lung injury or atelectasis. - Reese Clark
High Frequency Ventilation • Rapid rate • Low tidal volume • Maintain open lung • Minimal volume swings
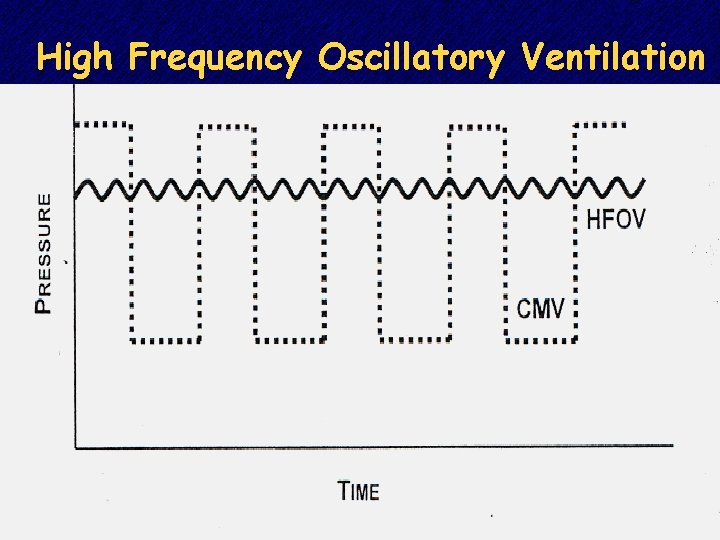
High Frequency Oscillatory Ventilation
HFOV is the easiest way to find the ventilation “sweet spot”
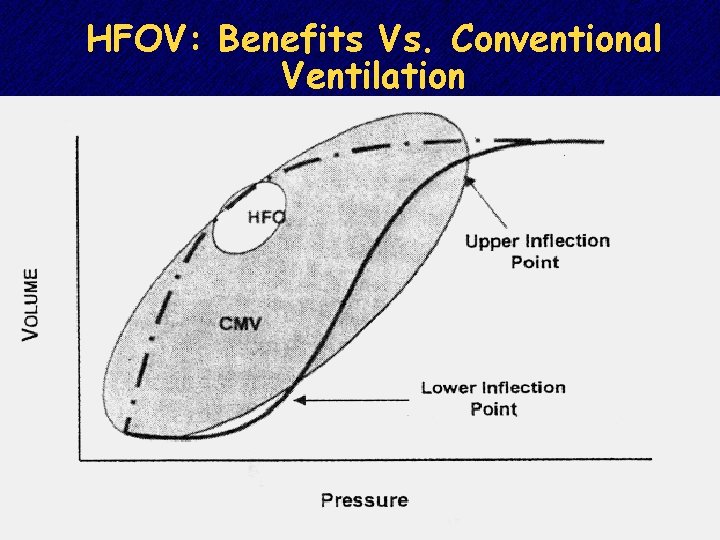
HFOV: Benefits Vs. Conventional Ventilation
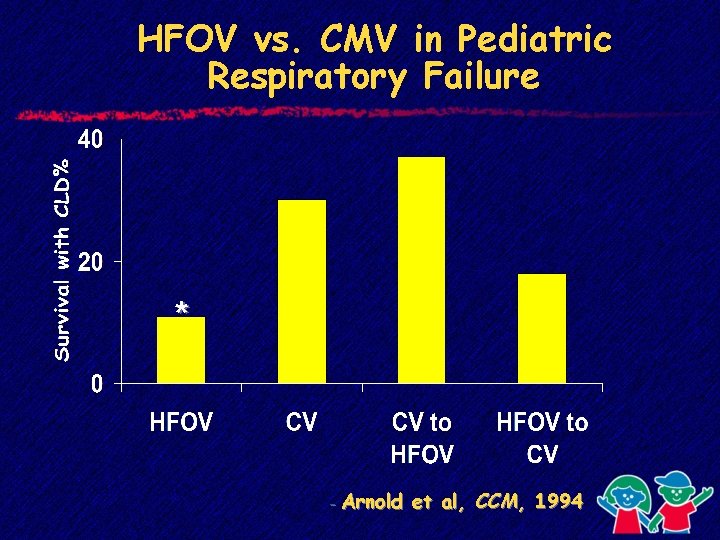
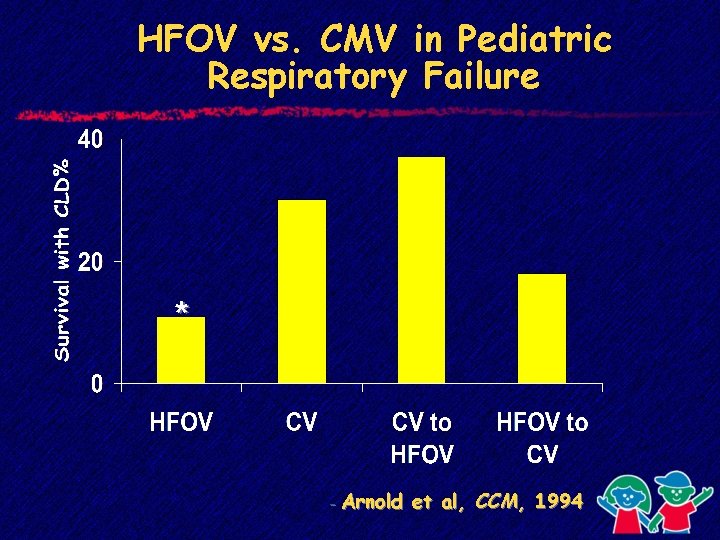
HFOV vs. CMV in Pediatric Respiratory Failure * - Arnold et al, CCM, 1994
Surfactant in ARDS • ARDS: § surfactant deficiency § surfactant present is dysfunctional • Surfactant replacement improves physiologic function
Surfactant in Pediatric ARDS • Current randomized multi-center trial • Placebo vs calf lung surfactant (Infasurf) • Children’s at Egleston is a participating center-study closed, await results
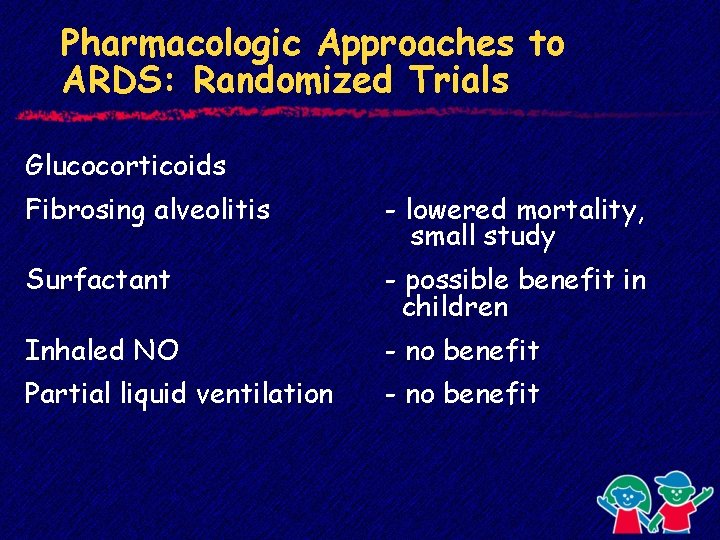
Steroids in Unresolving ARDS • Randomized, double-blind, placebocontrolled trial • Adult ARDS ventilated for > 7 days without improvement • Randomized: § Placebo § Methylprednisolone 2 mg/kg/day x 4 days, tapered over 1 month Meduri et al, JAMA 280: 159, 1998
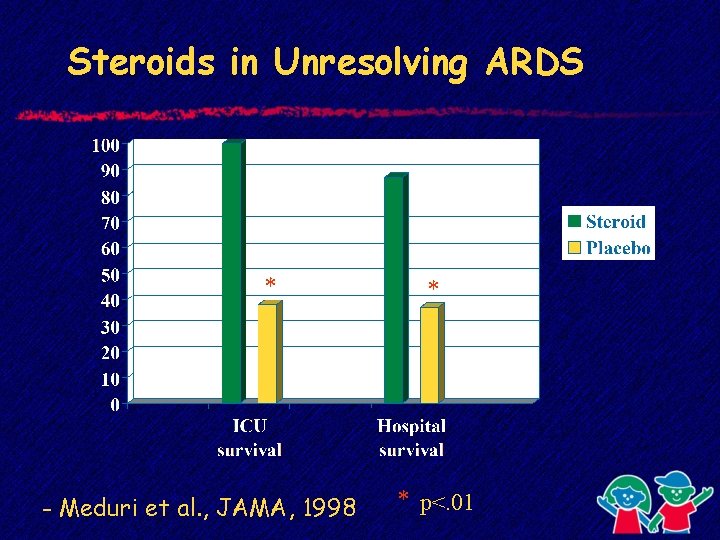
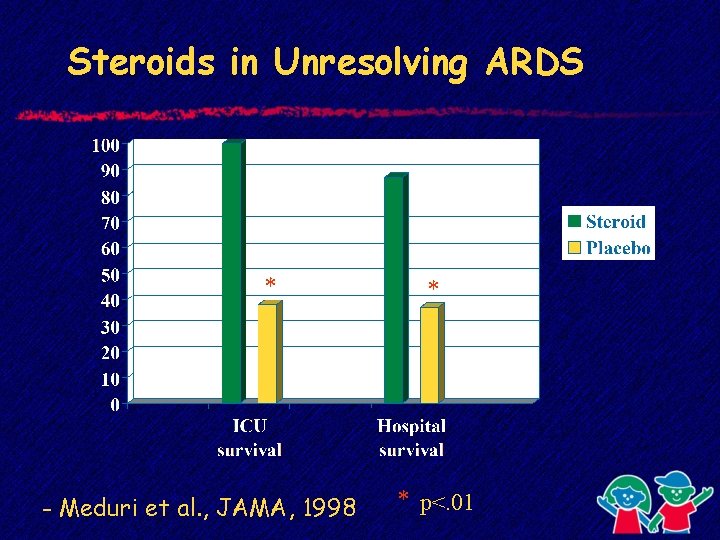
Steroids in Unresolving ARDS * - Meduri et al. , JAMA, 1998 * * p<. 01
Steroids in Unresolving ARDS • Randomized, double-blind, placebocontrolled trial • ARDSNetwork-180 adults • Randomized: § Placebo § Methylprednisolone § No mortality difference § Decreased ventilator-free days but only if started 7 -14 days Steinberg, NEJM, 354: 1671, 2006
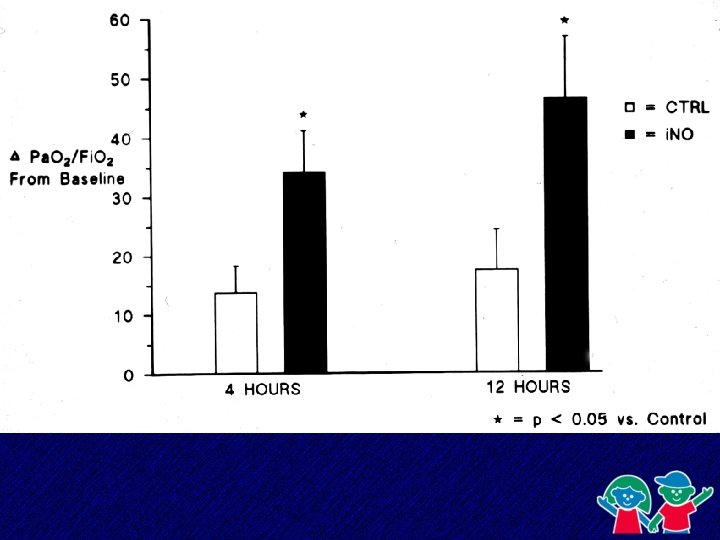
Inhaled Nitric Oxide in Respiratory Failure Neonates § Beneficial in term neonates with PPHN § Decreased need for ECMO Adults/Pediatrics § Benefits - lowers PA pressures, improves gas exchange § Randomized trials: No difference in mortality or days of ventilation
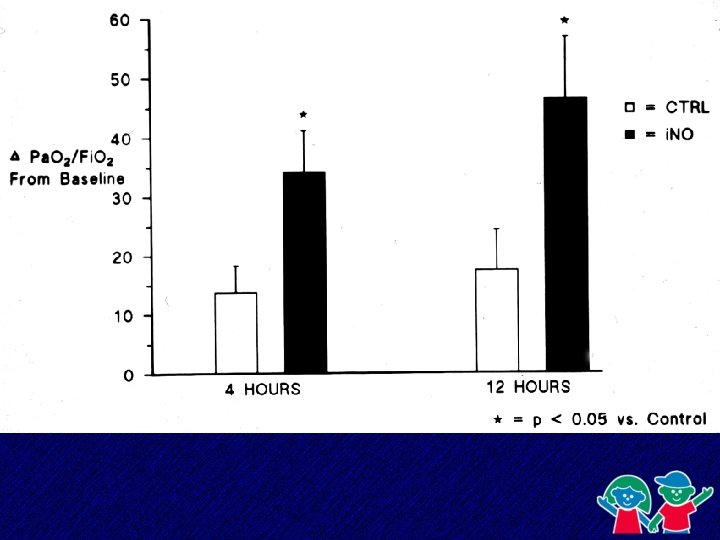
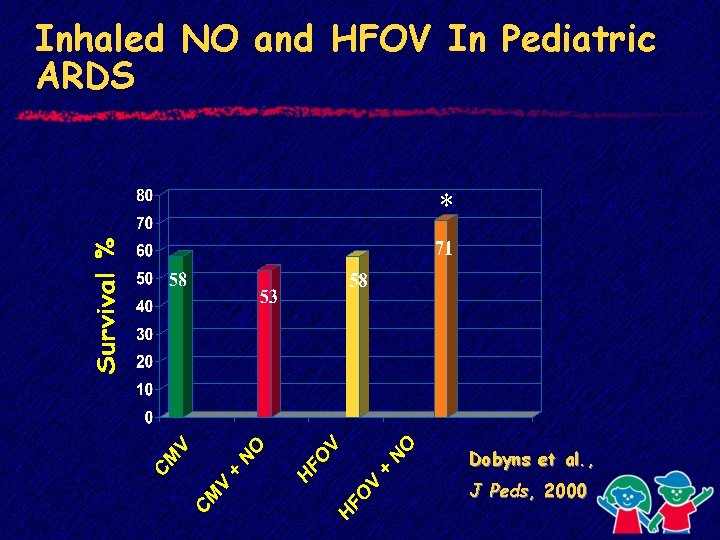
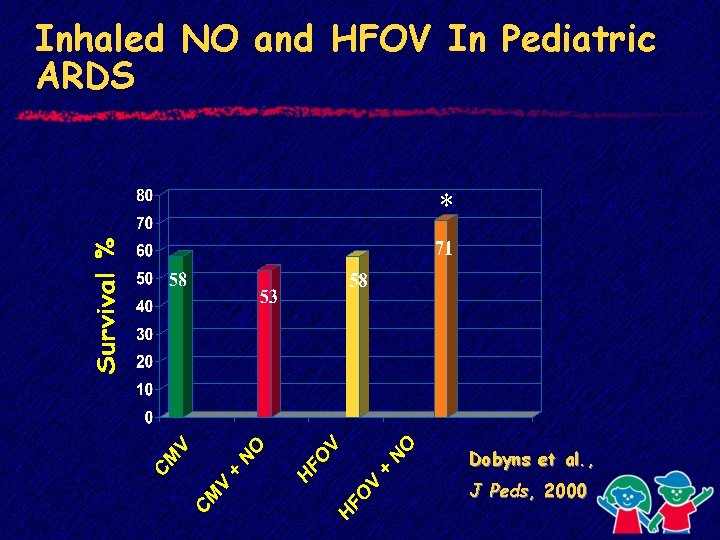
Inhaled NO and HFOV In Pediatric ARDS * Dobyns et al. , J Peds, 2000
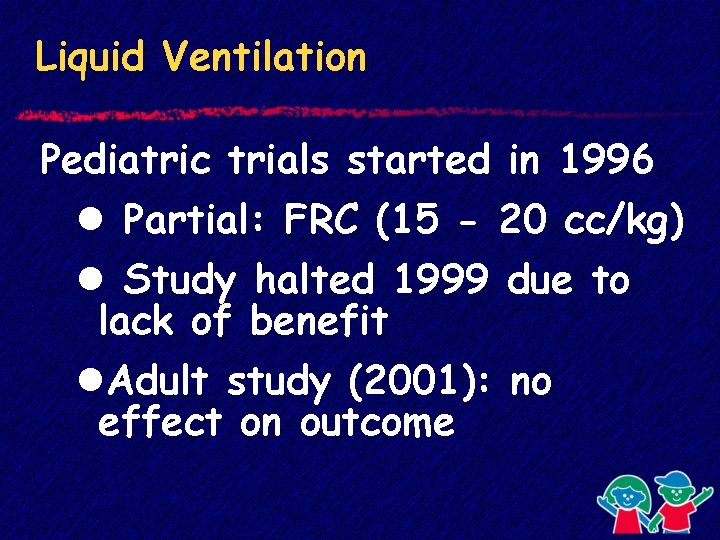
Partial Liquid Ventilation
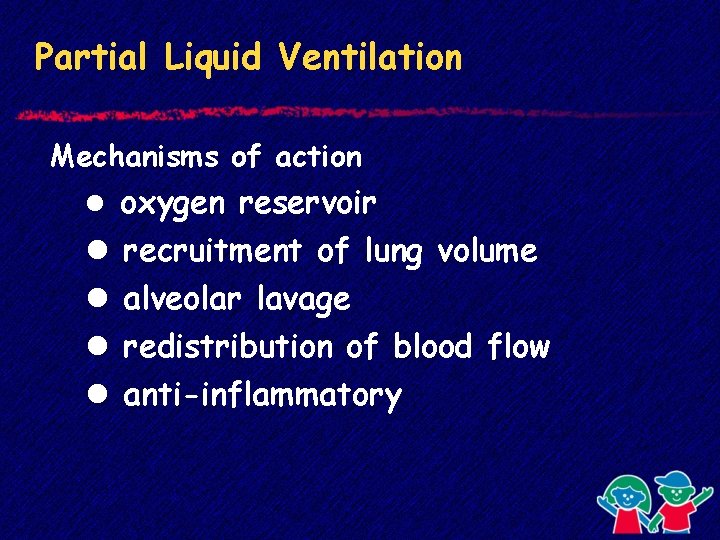
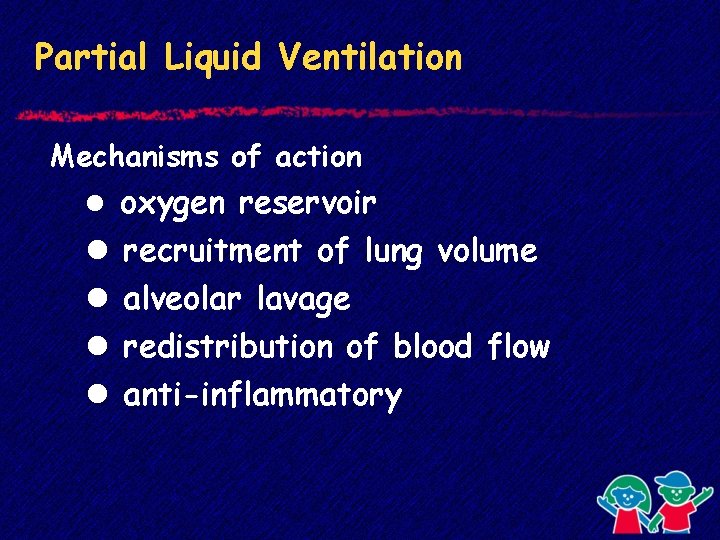
Partial Liquid Ventilation Mechanisms of action l oxygen reservoir l l recruitment of lung volume alveolar lavage redistribution of blood flow anti-inflammatory
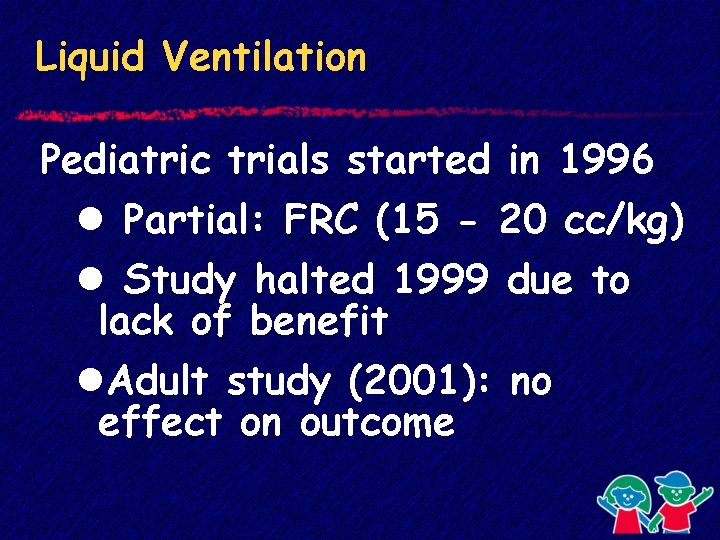
Liquid Ventilation Pediatric trials started in 1996 l Partial: FRC (15 - 20 cc/kg) l Study halted 1999 due to lack of benefit l. Adult study (2001): no effect on outcome
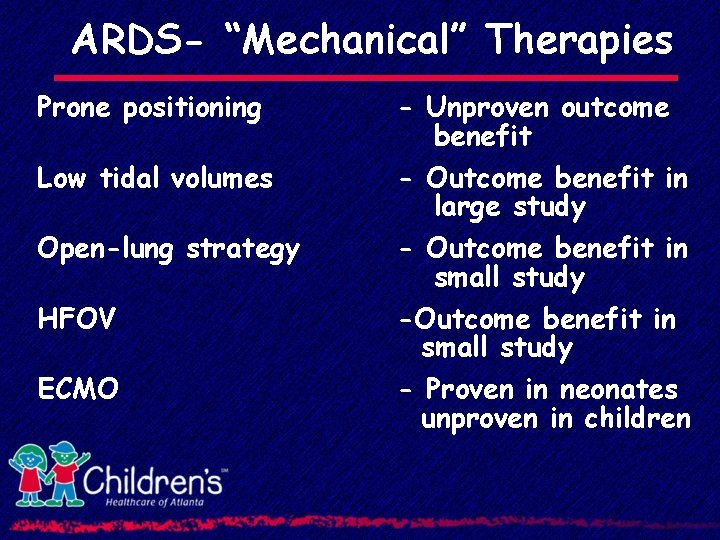
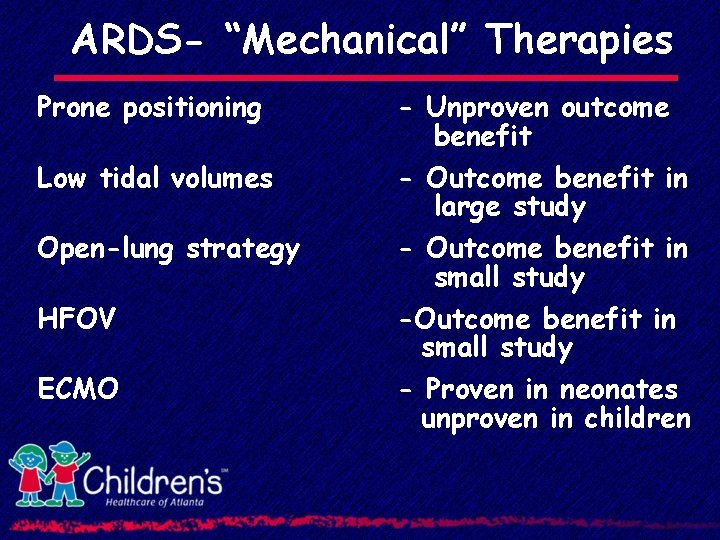
ARDS- “Mechanical” Therapies Prone positioning - Unproven outcome benefit Low tidal volumes - Outcome benefit in large study - Outcome benefit in small study - Proven in neonates unproven in children Open-lung strategy HFOV ECMO
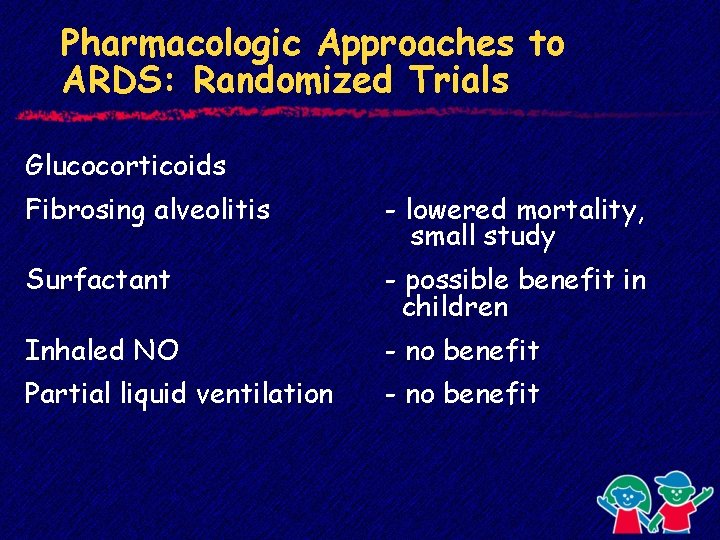
Pharmacologic Approaches to ARDS: Randomized Trials Glucocorticoids Fibrosing alveolitis - lowered mortality, small study Surfactant - possible benefit in children Inhaled NO - no benefit Partial liquid ventilation - no benefit
“…We must discard the old approach and continue to search for ways to improve mechanical ventilation. In the meantime, there is no substitute for the clinician standing by the ventilator…” - Martin J. Tobin, MD