Pediatric Anxiety Disorders Diagnosis and Treatment Julie Lesser



























- Slides: 74
Pediatric Anxiety Disorders: Diagnosis and Treatment Julie Lesser, MD, and Sarah Frankfurt, LAMFT January 31, 2020
Objectives • Provide an overview of the epidemiology and diagnosis of anxiety disorders in children and adolescents. • Discuss treatment modalities including psychotherapy approaches, and brief overview of medication options • Cognitive Behavioral Therapy and Exposure Response Prevention • Review strategies for identifying and addressing anxiety in children in the school setting.
What is anxiety? • Anxiety is multidimensional… • Physical/somatic distress • Cognitive and subjective distress • Behavioral response and avoidance • ~8 -12% of children and adolescents ages 4 -20 suffer from ≥ 1 anxiety disorders.
Epidemiology of anxiety disorders • Most common psychiatric disorder in childhood • Seen in all socioeconomic levels • Median Age of Onset: 6 years old • Female-to-male ratio • Equal in preadolescent children • Females are increasingly represented in adolescent years (except OCD) • 80% of youth with a diagnosable anxiety disorder are not receiving treatment
Cross cultural perspective • White Americans shown in studies to endorse symptoms of anxiety disorders more than African Americans, Hispanic Americans and Asian Americans • Prevalence of OCD appears roughly consistent across ethnic groups in US • African and Caribbean Americans showed an OCD lifetime prevalence of 1. 6% • Epidemiologic studies in other countries find similar rates cross nationally (Weismann et al. , 1994)
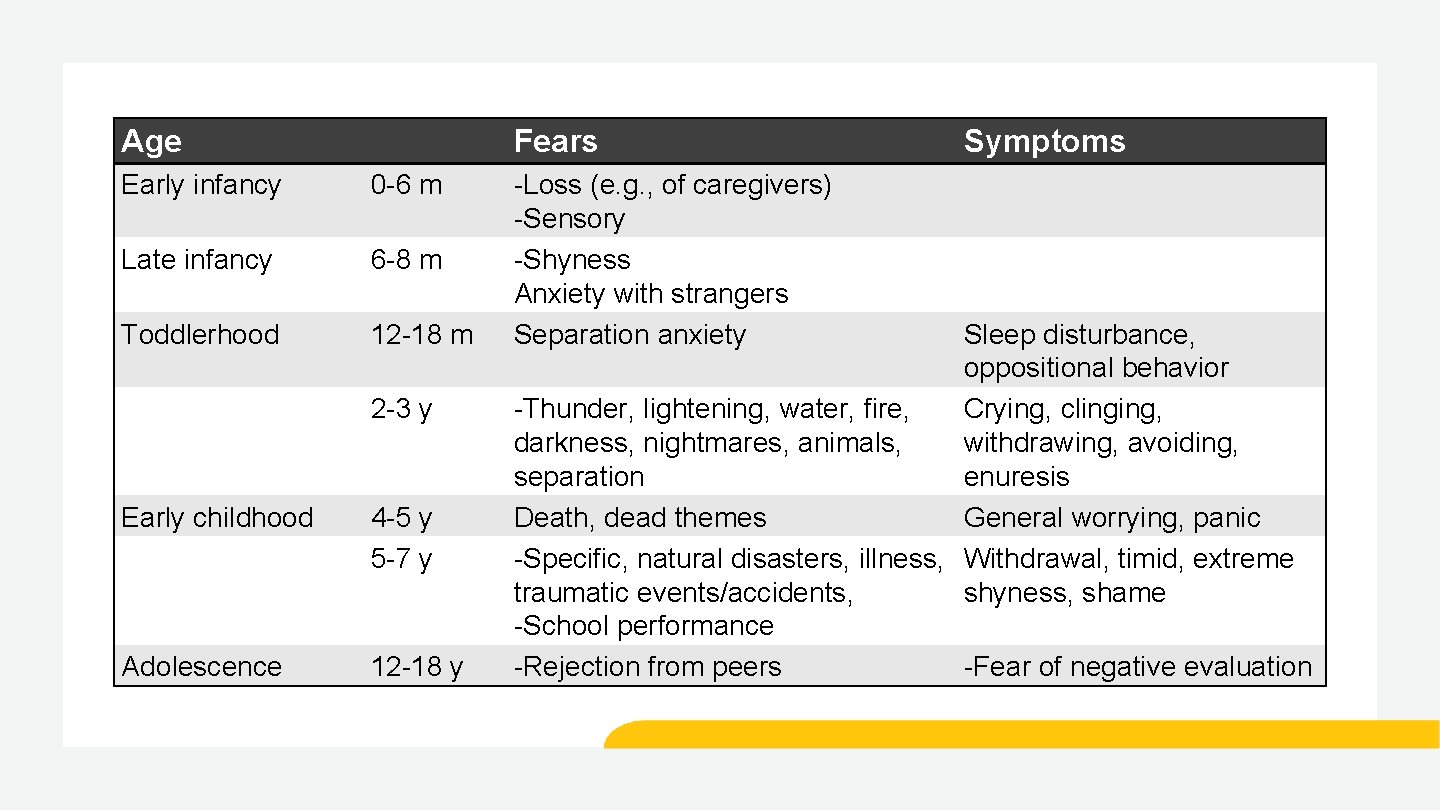
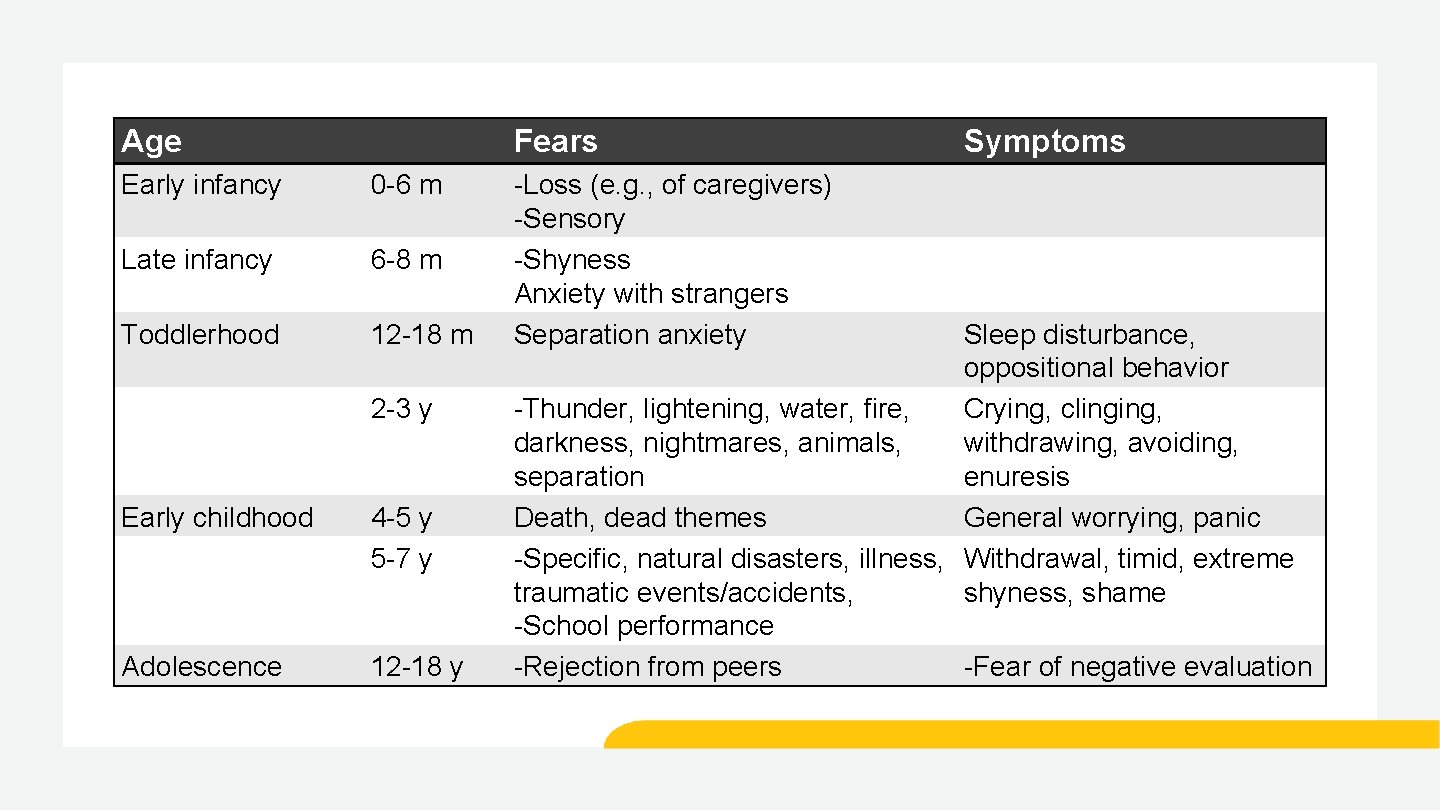
Age Fears Early infancy 0 -6 m Late infancy 6 -8 m Toddlerhood 12 -18 m 2 -3 y Early childhood 4 -5 y 5 -7 y Adolescence 12 -18 y -Loss (e. g. , of caregivers) -Sensory -Shyness Anxiety with strangers Separation anxiety Symptoms Sleep disturbance, oppositional behavior -Thunder, lightening, water, fire, Crying, clinging, darkness, nightmares, animals, withdrawing, avoiding, separation enuresis Death, dead themes General worrying, panic -Specific, natural disasters, illness, Withdrawal, timid, extreme traumatic events/accidents, shyness, shame -School performance -Rejection from peers -Fear of negative evaluation

When is fear/anxiety a problem? • Is it out of proportion to the situation? • Can it be explained or reasoned away? • Is the fear beyond voluntary control? • Unchanged? • Does fear lead to avoidance of the situation? • Is the fear appropriate for the child’s age or stage? • Does the fear interfere with functioning?

Risk factors • Genetic • Twin studies suggest heritability for phobias, GAD, and panic disorder • Environmental • Negative life events • Biology • Cognitive approaches • Overactive fear circuit • Inflammation • Neurotransmitters • Decreased functioning of serotonin and GABA • Increased norepinephrine activity

Signs and symptoms of anxiety in youth • Recurrent fears and worries • Difficulty falling asleep or nightmares • Hard to relax • Difficulty separating from parents • Scared about going to school • Irritability, crying, tantrums • Discomfort in social settings
Children with anxiety disorders • At risk for developing other types of anxiety disorders or psychiatric disorders • 75% of individuals with anxiety disorder meet the criteria for another psychiatric disorder • 60% meet criteria for major depression • Half of individuals with anxiety disorder meet criteria for another anxiety disorder • Subthreshold symptoms common
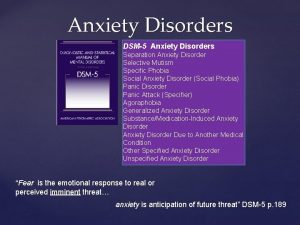
Anxiety disorders • Generalized Anxiety Disorder • Social Anxiety Disorder • Separation Anxiety Disorder • Specific Phobia • Selective Mutism • Panic Disorder • Obsessive-Compulsive Disorder *
Assessments • Assessments at the beginning and through out treatment • For social anxiety: Leibowitz Social Anxiety Scale (LSAS) • For panic disorder: Child Anxiety Sensitivity Index (CASI) • For GAD/worry: Penn State Worry Questionnaire, Child (PSWQC) • For Obsessive Compulsive Disorder: Children’s Yale-Brown Obsessive-Compulsive Disorder scale (CY-BOCs)
Generalized Anxiety Disorder (GAD) • Excessive, chronic worry about common events and activities occurring for at least 6 months. • Associated with at least 3 of following: – Restlessness or feeling on edge – Being easily fatigued – Difficulty concentrating or mind going blank – Irritability – Muscle tension – Sleep disturbance
GAD: Other features • Perfectionistic, excessively critical of themselves • Excessive self-consciousness • Frequent reassurance seeking • Worry about negative consequences • Somatic complaints – GI distress, headaches, frequent urination, sweating, tremor

Separation anxiety • Excessive anxiety focused on separating from home or parent figure • Worry about parent’s health and safety • Difficulty sleeping without parents • Difficulty being alone in another part of the house • Somatic complaints • May refuse to go to school or playdates

Separation anxiety • Most commonly diagnosed in pre-pubertal children • More common in 5 -7 and 11 -12 -year olds, with transition into elementary and middle school • Developmentally inappropriate • Typically occurs following a significant change or major life event

Social phobia • Excessive fear or discomfort in social situations or performance situations • Extreme fear of negative evaluation by others • Worry about doing something embarrassing in a variety of settings • Difficulty participating in class, working in groups, eating in front of others, making new friends, having pictures taken, talking on the phone • Often demonstrate diminished social skills, longer speech latency, fewer friends, school refusal
Selective mutism • Unable to speak in certain situations (school), despite being able to speak in other settings (home) • Difficulty speaking, laughing, reading aloud outside of family members • Speech/language development is most often normal • Often inadvertently reinforced by other individuals (i. e. , parents) in the child’s daily life (e. g. , speaking for the child, permitting the use of nonverbal communication) • Relationship between social phobia and selective mutism
Panic attacks • Sudden, discrete episodes of intense fear • Intense desire to escape • Feeling of doom • Activation of autonomic nervous system • Fight or flight • Symptoms – increased heart rate, sweating, fast shallow breathing • Duration 20 -30 minutes

Panic disorder • Recurrent panic attacks or intense fear • Inter-episode worry about having a panic attack which may lead to avoidant behaviors • Worry about implications and consequences • Changes in behavior • More common in adolescents
Specific phobia • Excessive fear of a particular object or situation • May avoid the feared object or situation • Anxiety may be expressed through crying, clinging, freezing • Common phobias: animals/insects, heights, storm, elevators, planes, costume characters, doctors, vomiting, choking

Obsessive-compulsive disorder (OCD) • Obsessions are unwanted and distressing so people try to resist them, get rid of them, or reduce their distress in some way: – avoidance of triggers – distraction – compulsive behaviors or thoughts • They are NOT excessive worries about real life problems • Differentiates from Generalized Anxiety Disorder • A compulsion is a behavior or mental act that a person feels driven to perform over and over again – to prevent or reduce anxiety, discomfort or distress – to “prevent” something bad from happening • Often performed in response to an obsession • Often performed according to rigid rules or until it feels “just right”

OCD: Putting it together Obsession Compulsion Fear of contamination Obsessive doubt/harm Need for symmetry Fear of losing things Need for certainty Intrusive image or thought Washing/Cleaning Checking Ordering/Arranging Hoarding Reassurance/”just right” Repeating/mental ritual
Manifestations of anxiety at school • Repeated approval seeking from teacher • Avoidance of school activities or peer activities • Not attending school • Excessive self-criticism • Poor transitioning from school to home • Poor test taking – especially timed tests • Inability to ask for help from others • Procrastination with schoolwork

OCD at school • Teachers may be first to observe child’s obsessions or compulsions • Compulsions can interfere with ability to complete homework, can be distracting, can upset sleep, and can increase absenteeism and tardiness • May increase risk for bullying as kids with OCD can be isolated or teased
Cognitive symptoms with anxiety • Memory impairment • Short-term memory • Impaired decision making • Inability to concentrate • Thought distortions • Poor judgment • Anxious or racing thoughts and constant worrying

Medication management of anxiety and OCD
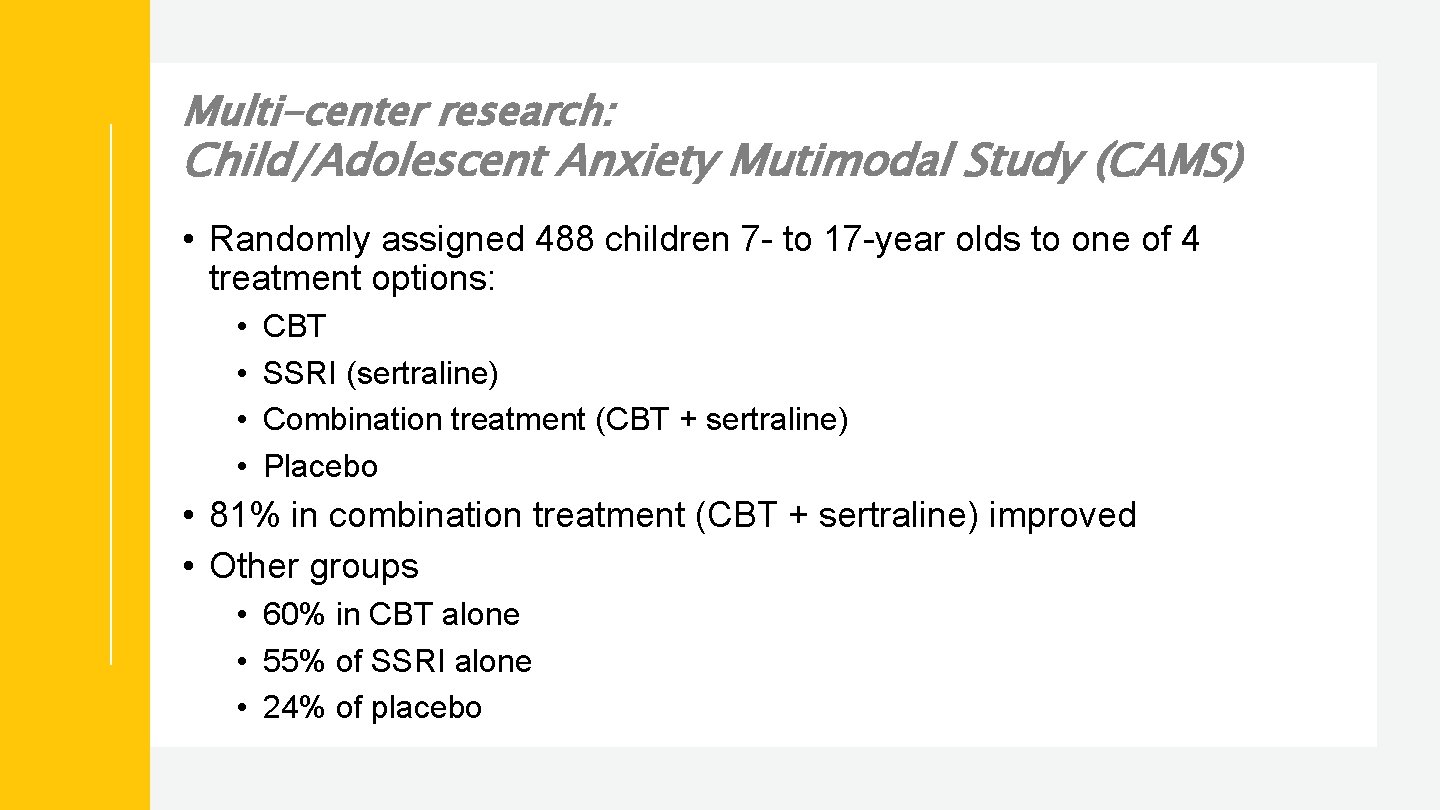
Multi-center research: Child/Adolescent Anxiety Mutimodal Study (CAMS) • Randomly assigned 488 children 7 - to 17 -year olds to one of 4 treatment options: • • CBT SSRI (sertraline) Combination treatment (CBT + sertraline) Placebo • 81% in combination treatment (CBT + sertraline) improved • Other groups • 60% in CBT alone • 55% of SSRI alone • 24% of placebo
Child/Adolescent Anxiety Multimodal Study (CAMS) PARS Remission rates in COMB (68%) > CBT (46%) and SRT (46%) > PBO (24%) (Walkup et al. , 2008, NEJM)
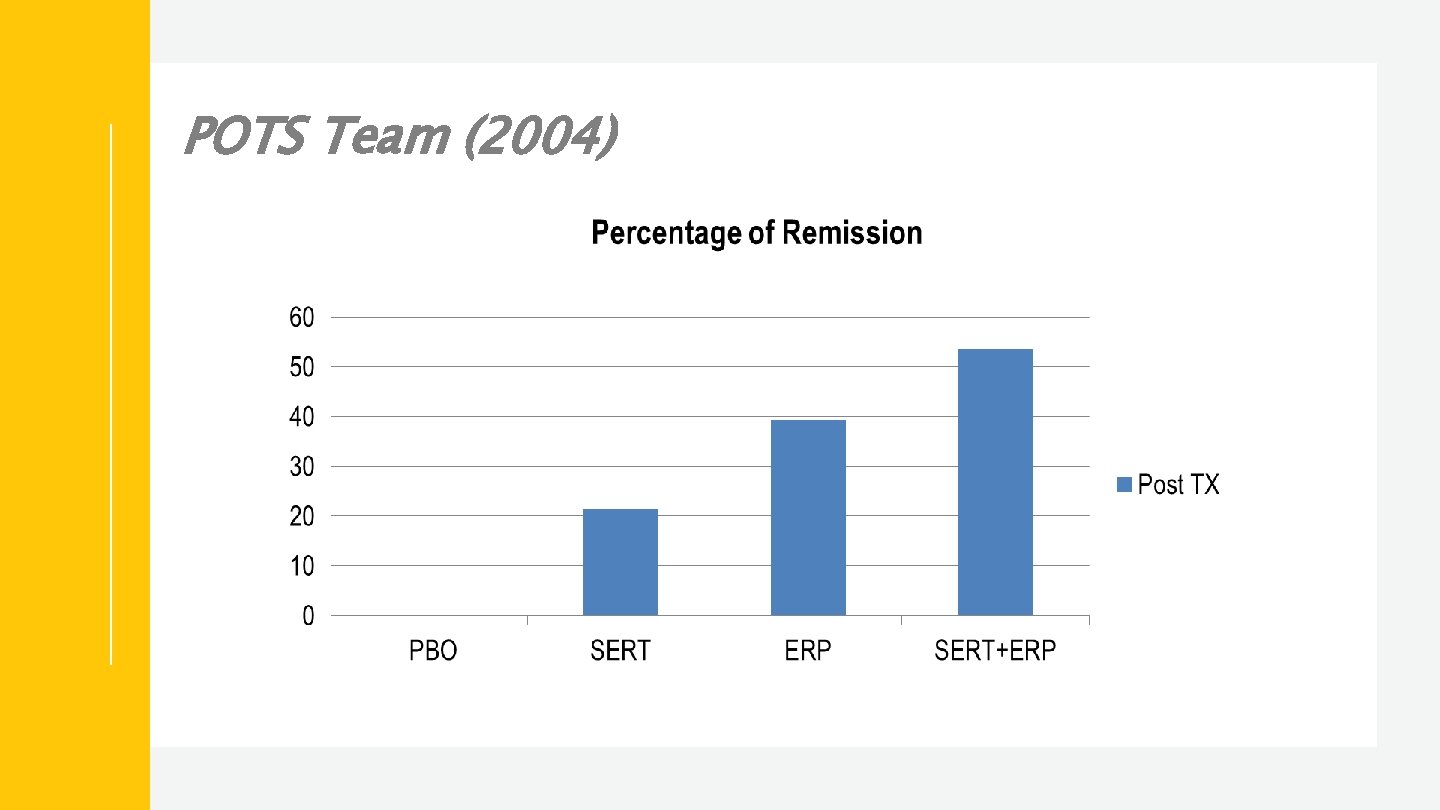
Multi-center research: Pediatric OCD Treatment Study (POTS) • N=112 (children 7 -17) • Randomized, placebo-controlled study • • 12 weeks of ERP Sertraline 12 weeks of ERP + sertraline (combined) Placebo • Looked at Clinical Remission rates (CYBOCS <10)
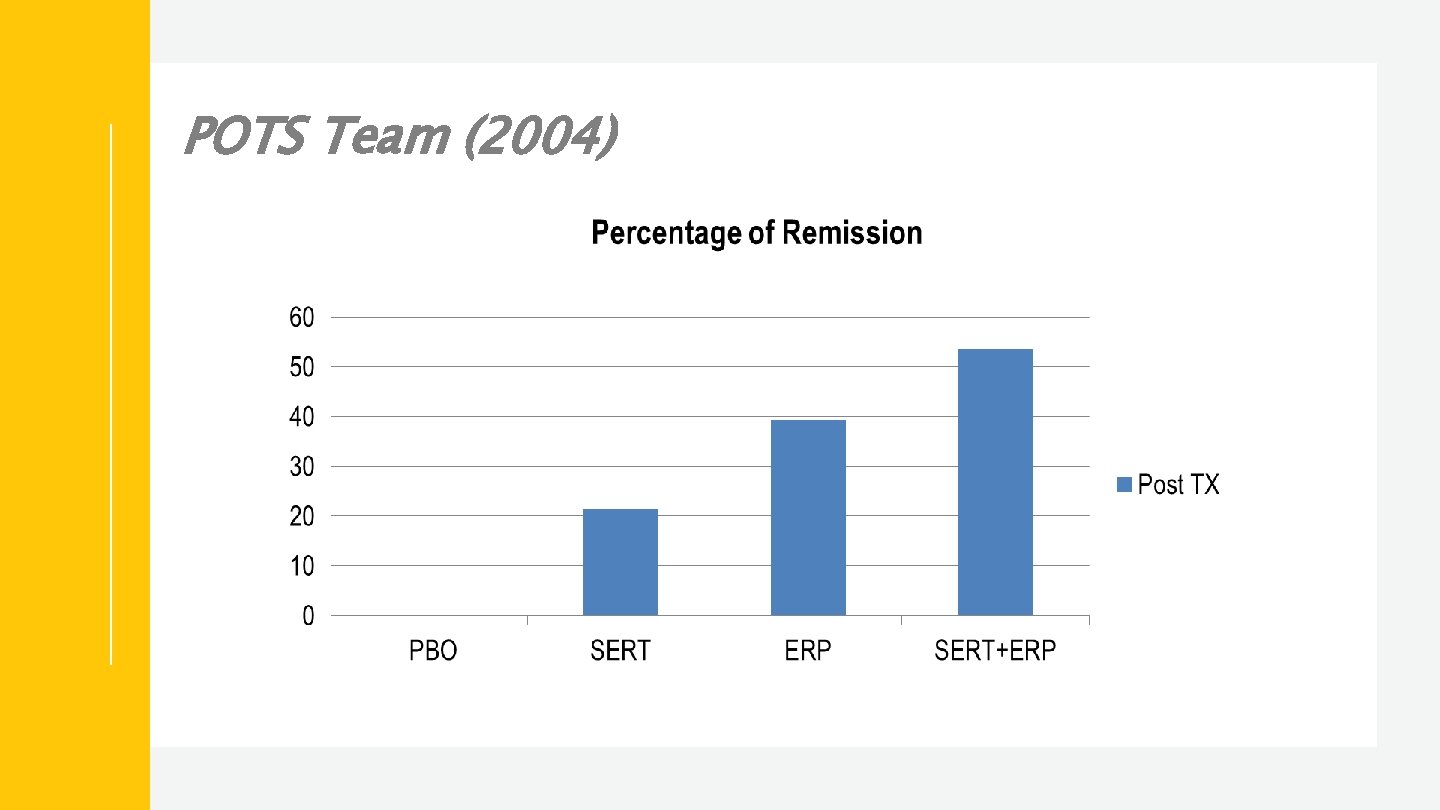
POTS Team (2004)
When to consider medication • Patient unable to participate in therapy due to severity of symptoms • Prominent daily impairment or avoidance • Co-occurring disorders • ADHD, depression, psychosis, bipolar disorder • Symptoms that do not respond to 6 - to 8 -week trial of CBT or ERP (with a family component) • Severe physiological symptoms of anxiety • Lack of availability of evidence-based therapy interventions

Selective Serotonin Reuptake Inhibitors (SSRIs) • First-line medication for pediatric anxiety • Safer side effect profile • Typically require higher doses for OCD as compared to patients with depression or other anxiety disorders • May take 10 -12 weeks in pediatric OCD to determine if medication is effective ─ SSRIs usually take 4 -6 weeks to determine effectiveness

Other medication strategies • Other antidepressants • Atypical Antipsychotics • B-blockers • Clonidine • Mood stabilizers/anti-seizure medications • Gaba-ergic Medications • Glutamate modulators
School role with medication • Part of treatment team • Observations of student during school invaluable • Dispense medication • Medication or side effects may impact behavior or learning • Impact on parent attitude toward medication

Cognitive behavioral therapy for anxiety disorders
Unmet need for anxiety treatment • Most people with anxiety never receive efficacious treatment • It is estimated that 84% of people with an anxiety disorder saw a health care provider but only 23% received appropriate treatment (Young et al. 2001) • Either with medication prescribed according to practice guidelines • < 4 sessions with a mental health specialist (11%) • Unmet need may be higher for children • Identification • Access • Cost

CBT for anxiety Ask for help in class = 8 Give speech to group of kids = 8 Psychoeducation Relaxation Cognitive restructuring/coping skills Problem solving Exposure Relapse prevention Talk to a new kid my age = 6 Talk to a new adult = 5 Trip in front of someone = 5 Drink water from a fountain and get some on my shirt = 4 Ask friend to come over to my house = 4 Ask security guard at school the time = 3 Answer the phone at home = 2

Psychoeducation • Psychoeducation about principles of CBT • Parent training to reduce accommodation of anxious behaviors, establish structure/routine, positive reinforcement and monitoring of symptoms • Co-therapist model with parents • Family-based CBT, has evidence of increased efficacy in school-age children • Coordinate treatment plan with school personnel
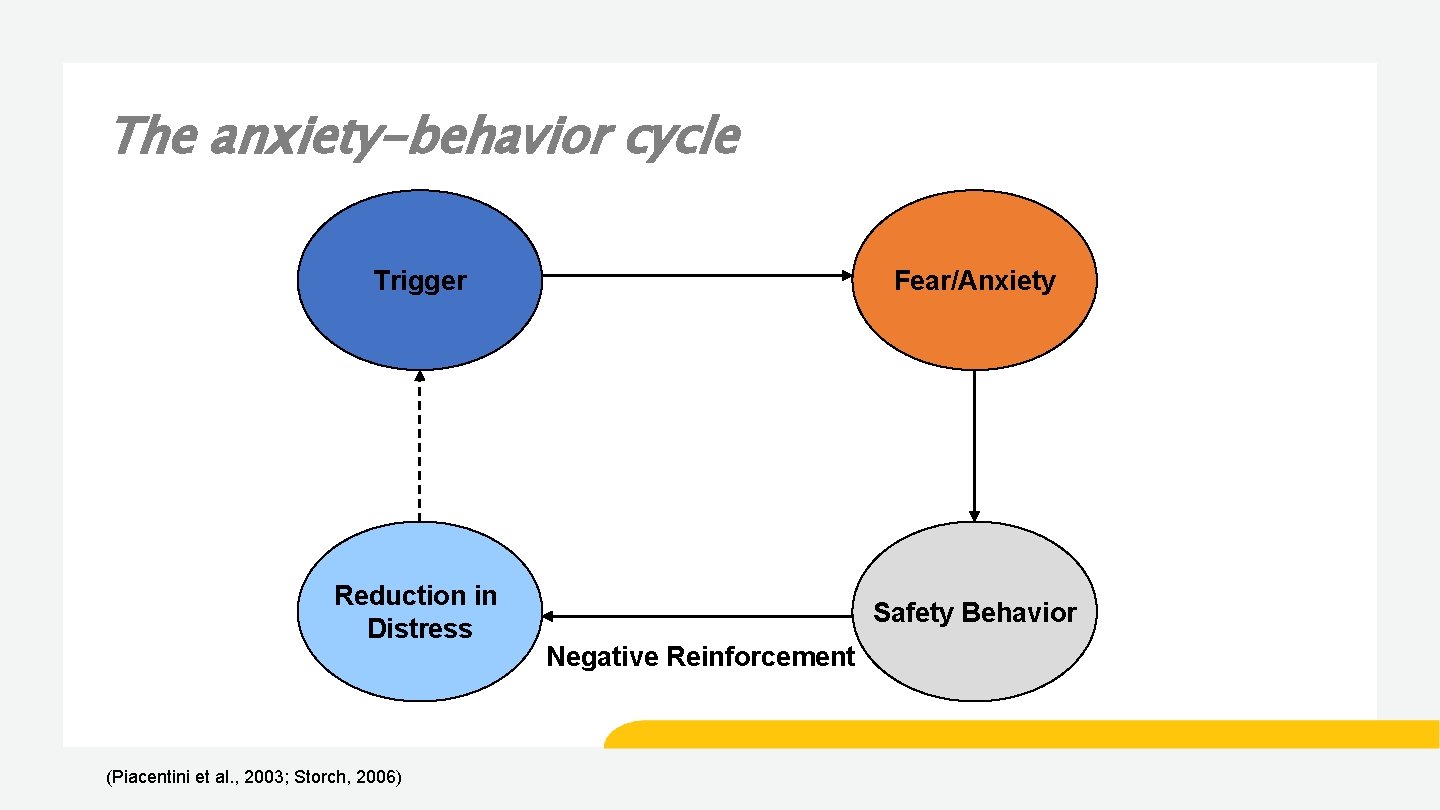
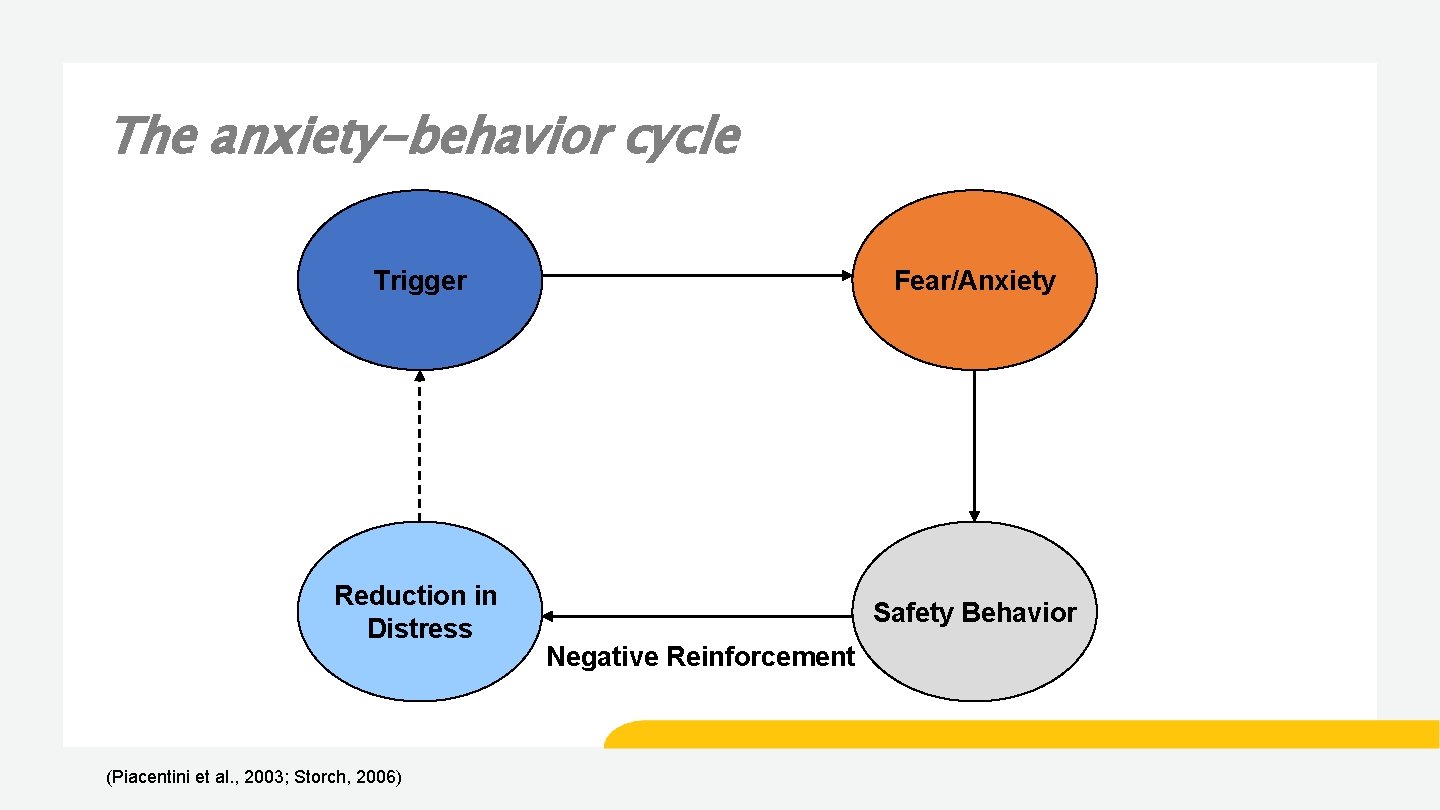
The anxiety-behavior cycle Trigger Fear/Anxiety Reduction in Distress Safety Behavior (Piacentini et al. , 2003; Storch, 2006) Negative Reinforcement
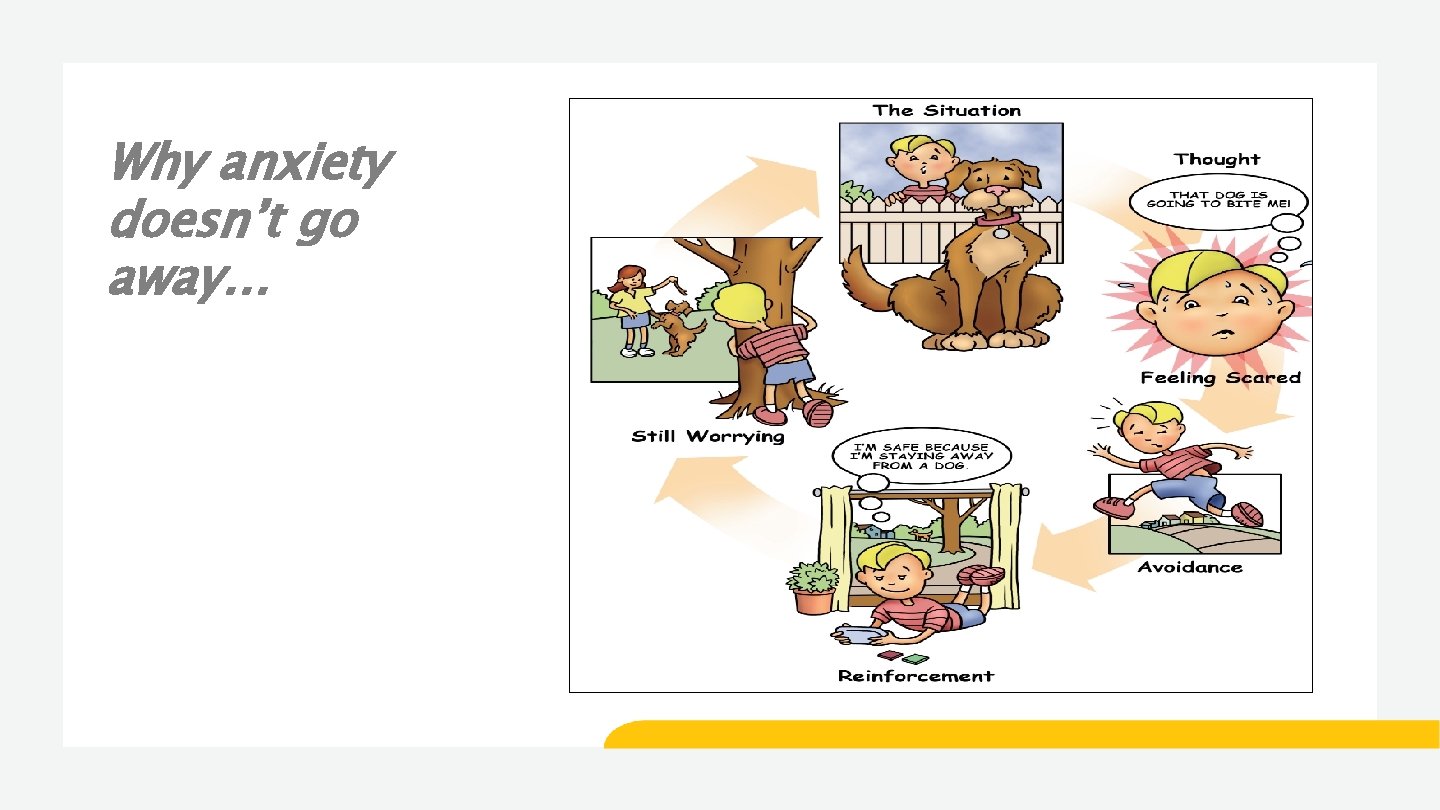
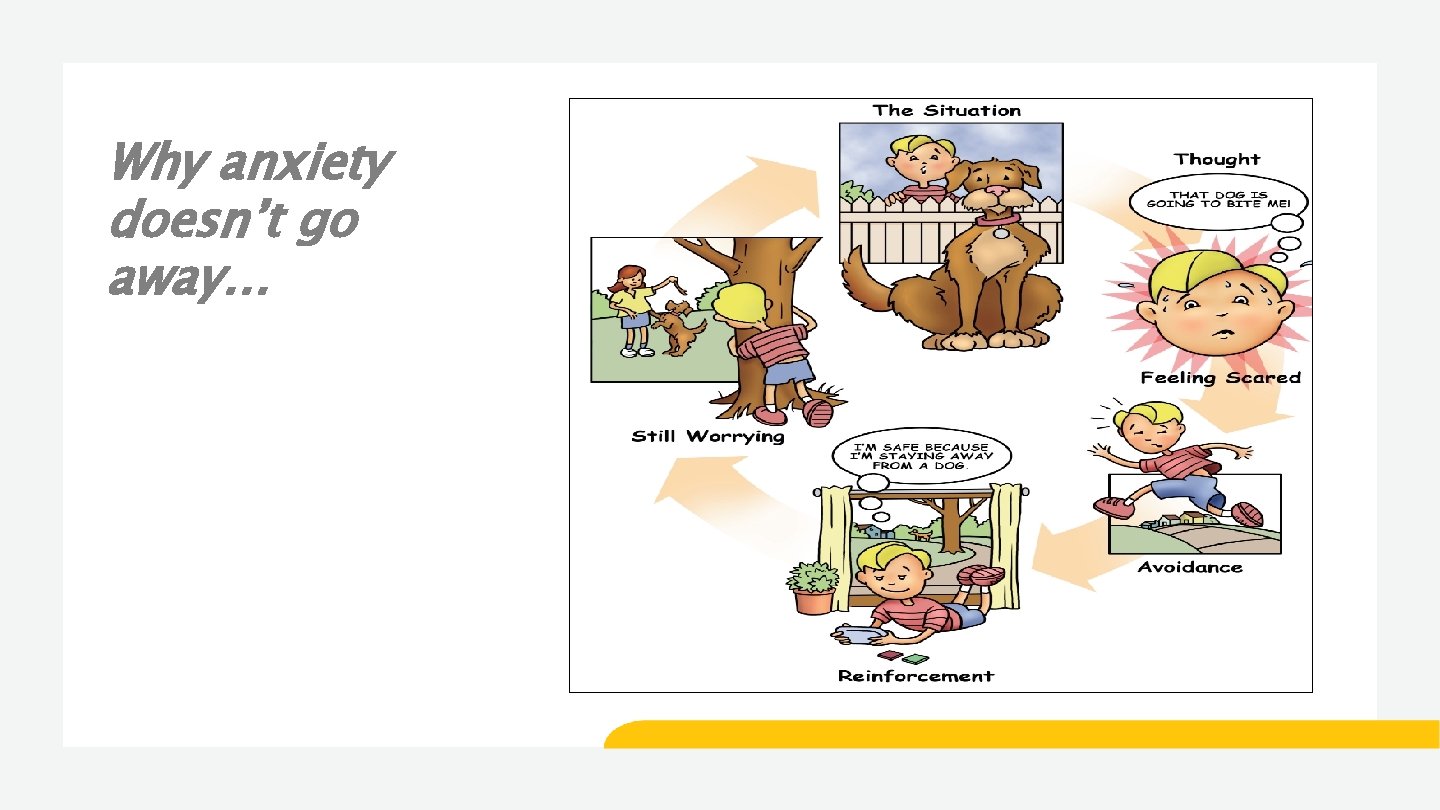
Why anxiety doesn’t go away…
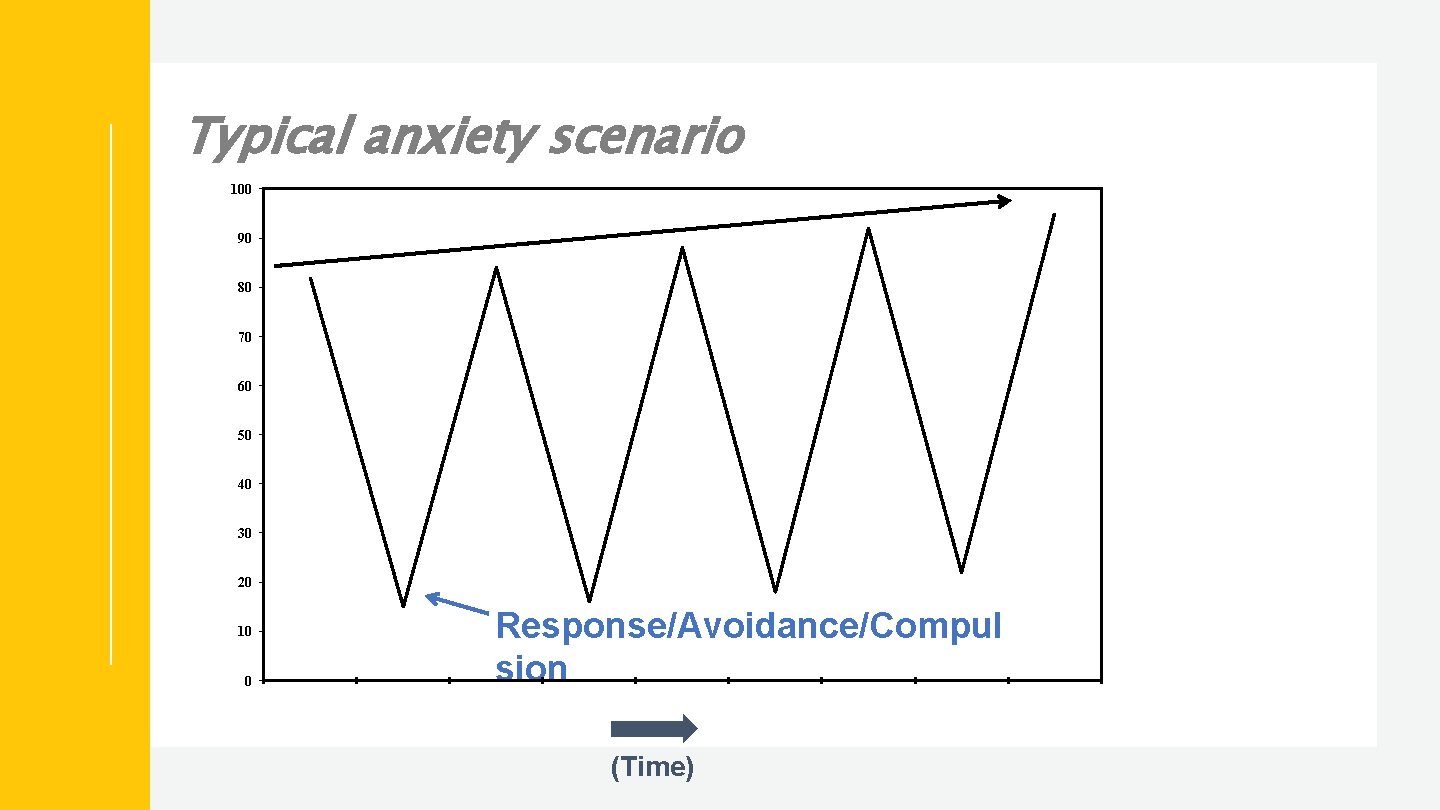
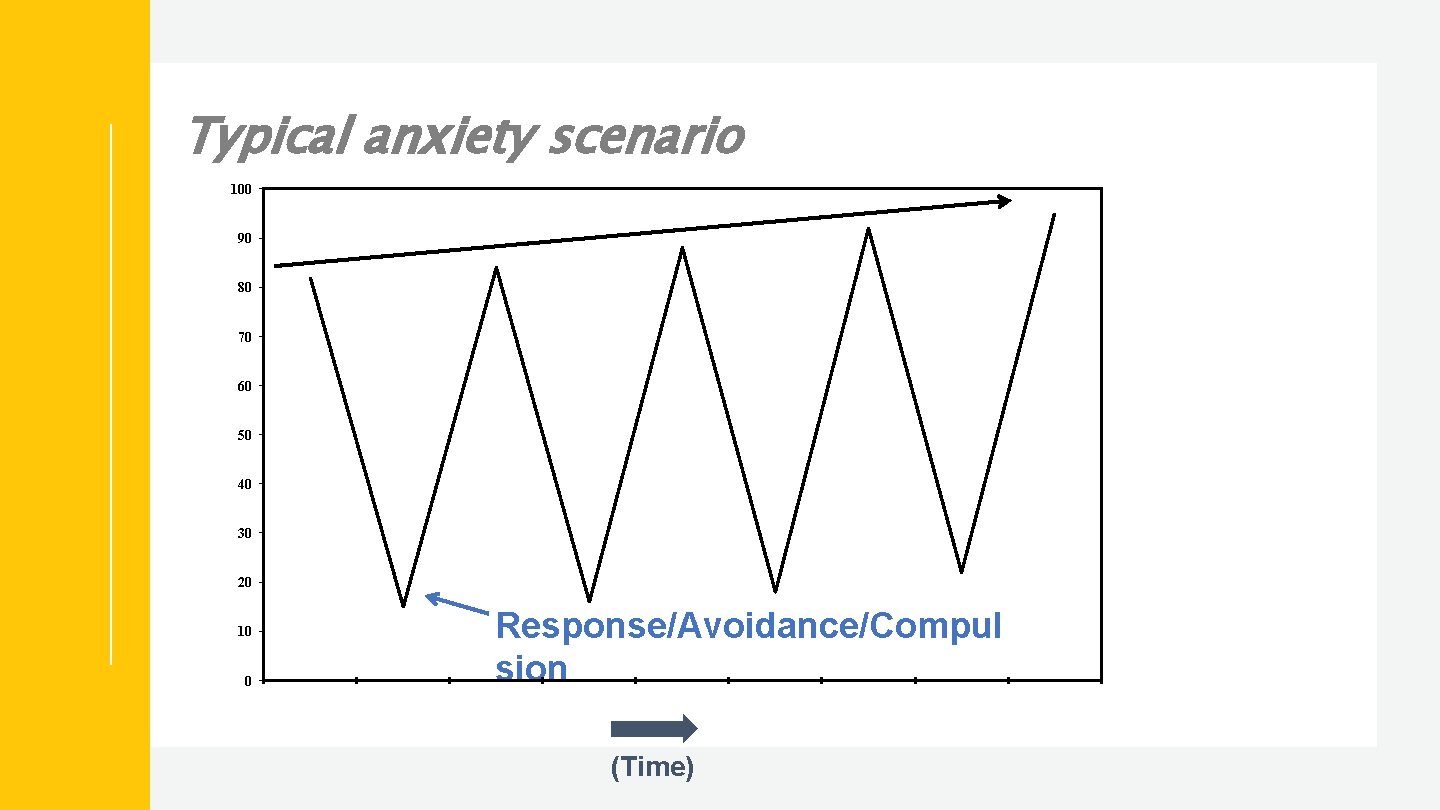
Typical anxiety scenario 100 90 80 70 60 50 40 30 20 10 0 Response/Avoidance/Compul sion (Time)

Cognitive behavioral model of anxiety Physical Feelings/Emotions e. g. , tummy ache, headache, racing heart Behaviors e. g. , clinging, avoidance Thoughts e. g. , I can’t handle being away from my mom

Somatic management skills training • Respiratory control/diaphragmatic breathing • Muscle relaxation • Imagery/meditation
Cognition and anxiety disorders • People with anxiety disorders have biased information processing • Heightened level of attention to potential threat • View situations as being unrealistically dangerous or likely to cause harm • Underestimate ability to manage or cope with feared situations

Identifying and challenging anxious thoughts • Do I know for sure this is going to happen? • Has this happened before? • How many times? • Has this happened to anyone I know? • What else could happen instead? • What am I missing out on due to worry? I’m going to fail this test and then I won’t be able to go to college and get a good job!
Problem solving as a way to detour worrying (worry as the “default” setting) “That must be tough, what are you going to do about it? ” Elements: 1. Problem identification 2. Possible solutions-all ideas are fair game 3. Assess all solutions and choose one (chance to take a risk) 4. Assess effectiveness of solution – continue or pick another
What is exposure therapy?

Exposure therapy • Placing an individual in feared situations without response engagement • Needs to be prolonged enough to lead to within trial habituation (at least 50% reduction in anxiety) • Needs to be repetitive enough to lead to between trial habituation (until causes minimal to no anxiety) • Needs to be graduated (increases compliance)
Exposure • CBT for anxiety is unique in that it requires a client to experience increased anxiety in order for new learning to take place • Exposure is the key active ingredient (Peris et al. , 2014) Yet… • some view exposure-based treatments as demanding, challenging, and perhaps even mean (Olatunji et al. , 2009) • therapists may fear damaging their clients with exposure procedures (Rosqvist, 2005) • may be even more of a problem for therapists who work with children

Typical Phobic Scenario High Trigger (Anxiety) Low 60 sec 10 min (Time)

Typical Phobic Scenario High Response/Compulsion (Anxiety) Low 60 sec 10 min (Time)
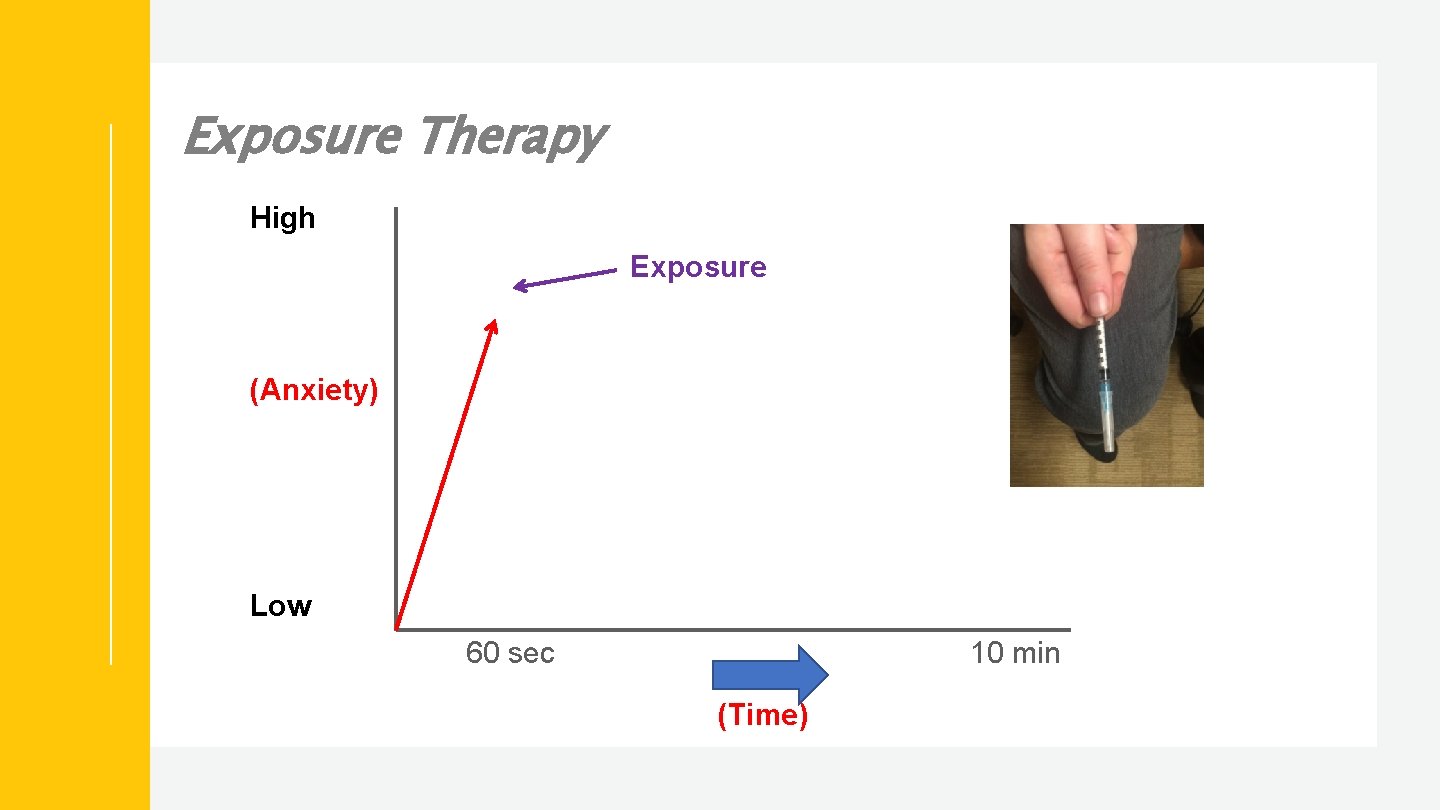
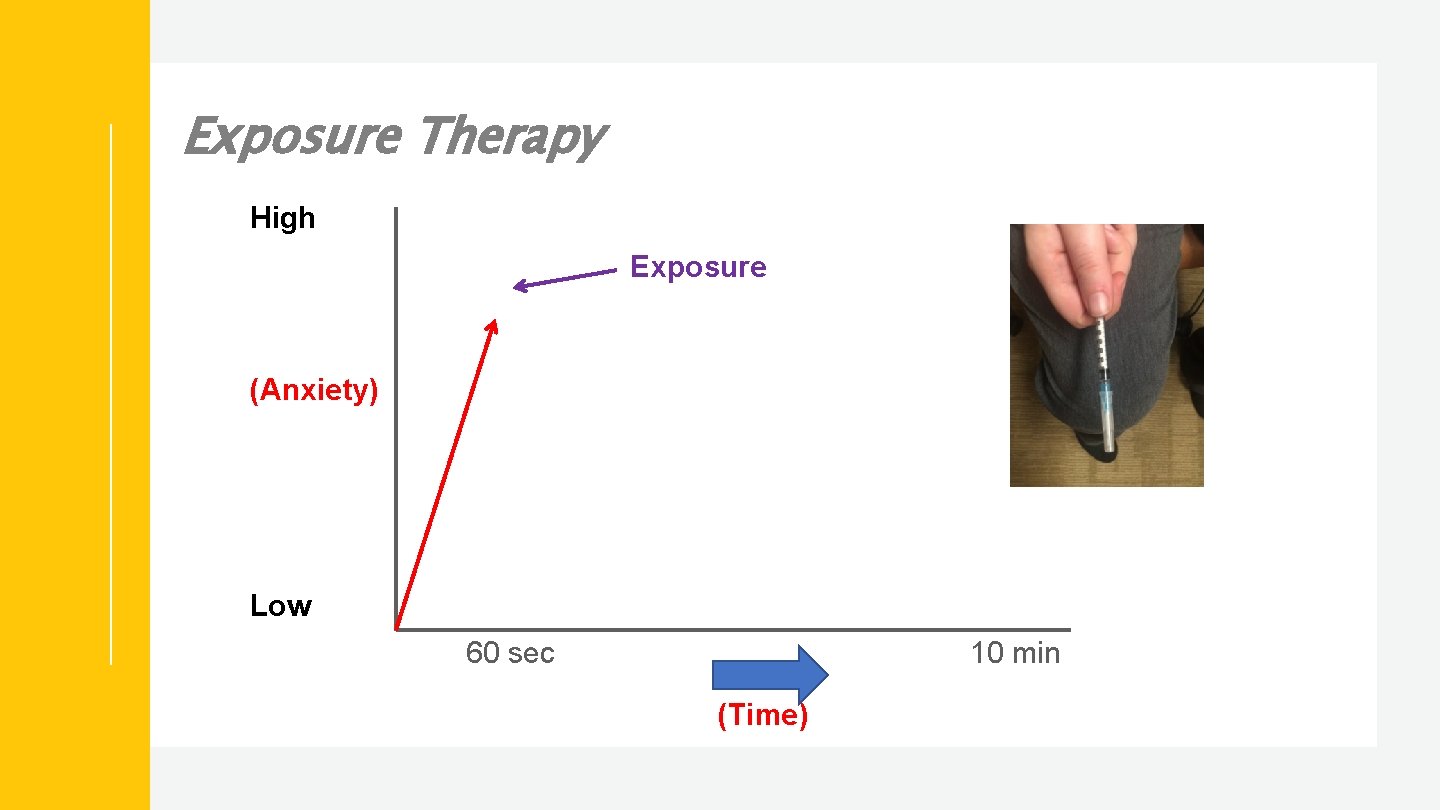
Exposure Therapy High Exposure (Anxiety) Low 60 sec 10 min (Time)

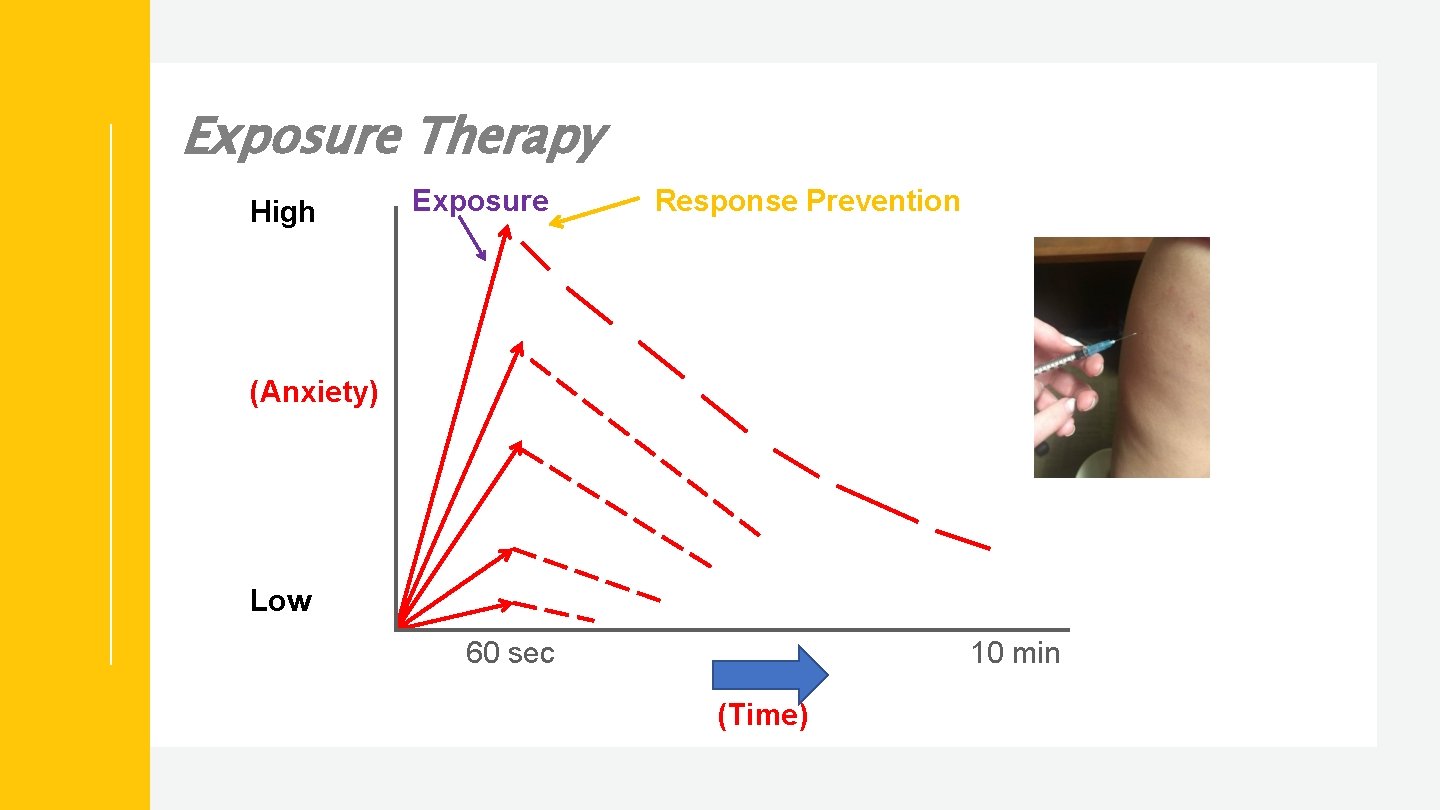
Exposure Therapy High Exposure Response Prevention (Anxiety) Habituation Low 60 sec 10 min (Time)
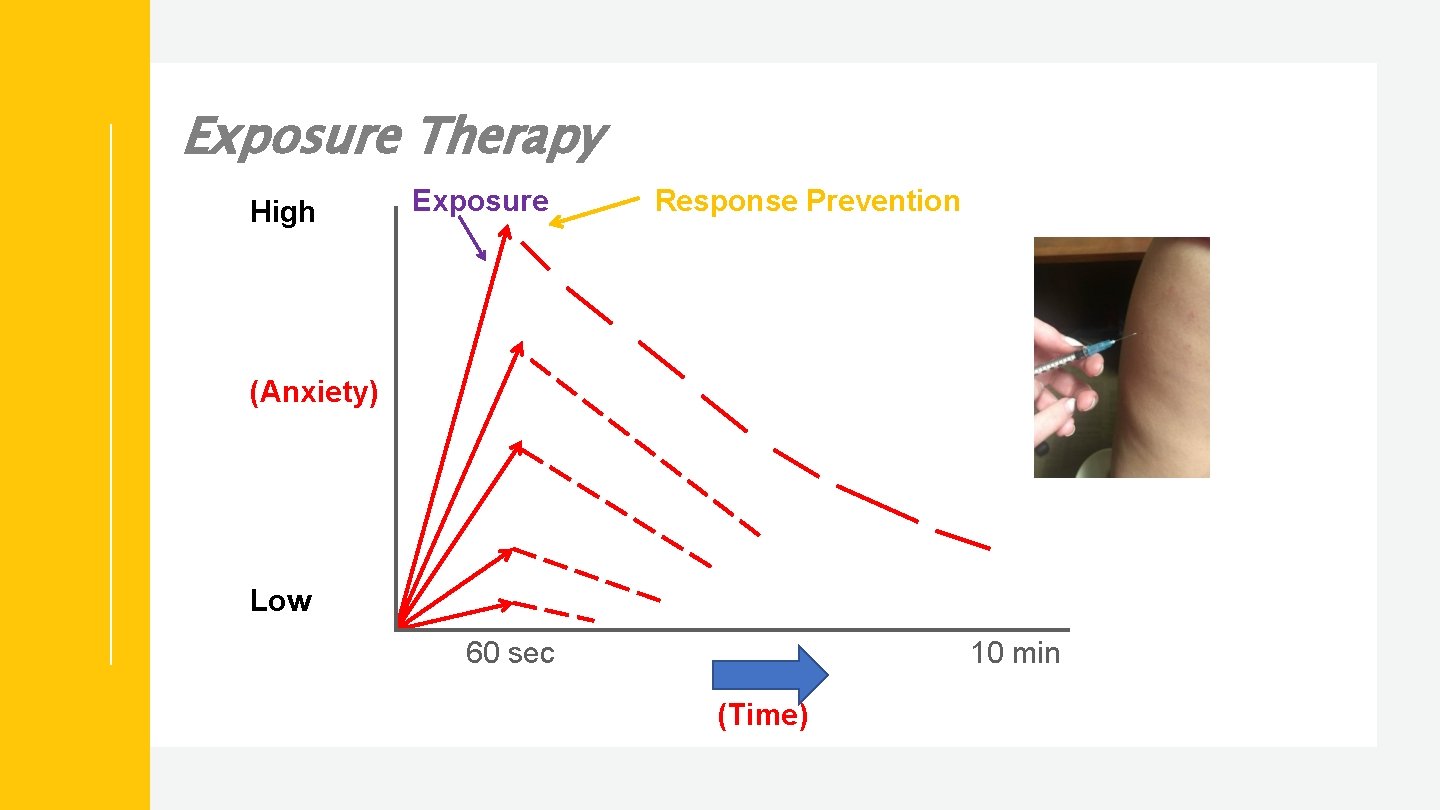
Exposure Therapy High Exposure Response Prevention (Anxiety) Low 60 sec 10 min (Time)
Exposure and response prevention How does it work? • Create a list of events that cause rituals/responses • Easiest to hardest • Be creative and ‘intense’ • Identify subtle changes in SUDS ratings • Incorporate reductions in family accommodation • Progress up the list slowly where the person does not engage in rituals/responses • First exposures should have high likelihood of success

Exposure and response prevention How does it work? (continued) • Tackle things one at a time • Give child choices • Therapist should model exposure • In vivo works best (but can do it through imagination) • Don’t leave the situation until anxiety drops
Some FALSE assumptions about exposure • Exposure is difficult to control with clients • Conducting exposure increases risk of client dropout • Exposure cannot be conducted with children or adolescents
General strategies to help kids with anxiety at home and at school

Teaching a child about anxiety • Anxiety is normal • Everyone experiences anxiety at times • Anxiety is not dangerous • Although anxiety may feel uncomfortable; it does not last long and will eventually decrease • Anxiety is adaptive • Anxiety helps us prepare for real danger. We perform our best at moderate levels of arousal (Yerkes-Dodson curve) • Advantages of the “fight or flight” response • Anxiety can become a problem when our bodies react to normal situations as if they were real dangers
Active ignoring • Active reinforcement of positive behaviors • Active ignoring of unwanted behaviors to extinguish (complaining, crying, somatic complaints) • Temporary increases in problem behaviors are expected • Helps children learn to try coping skills and problem solve
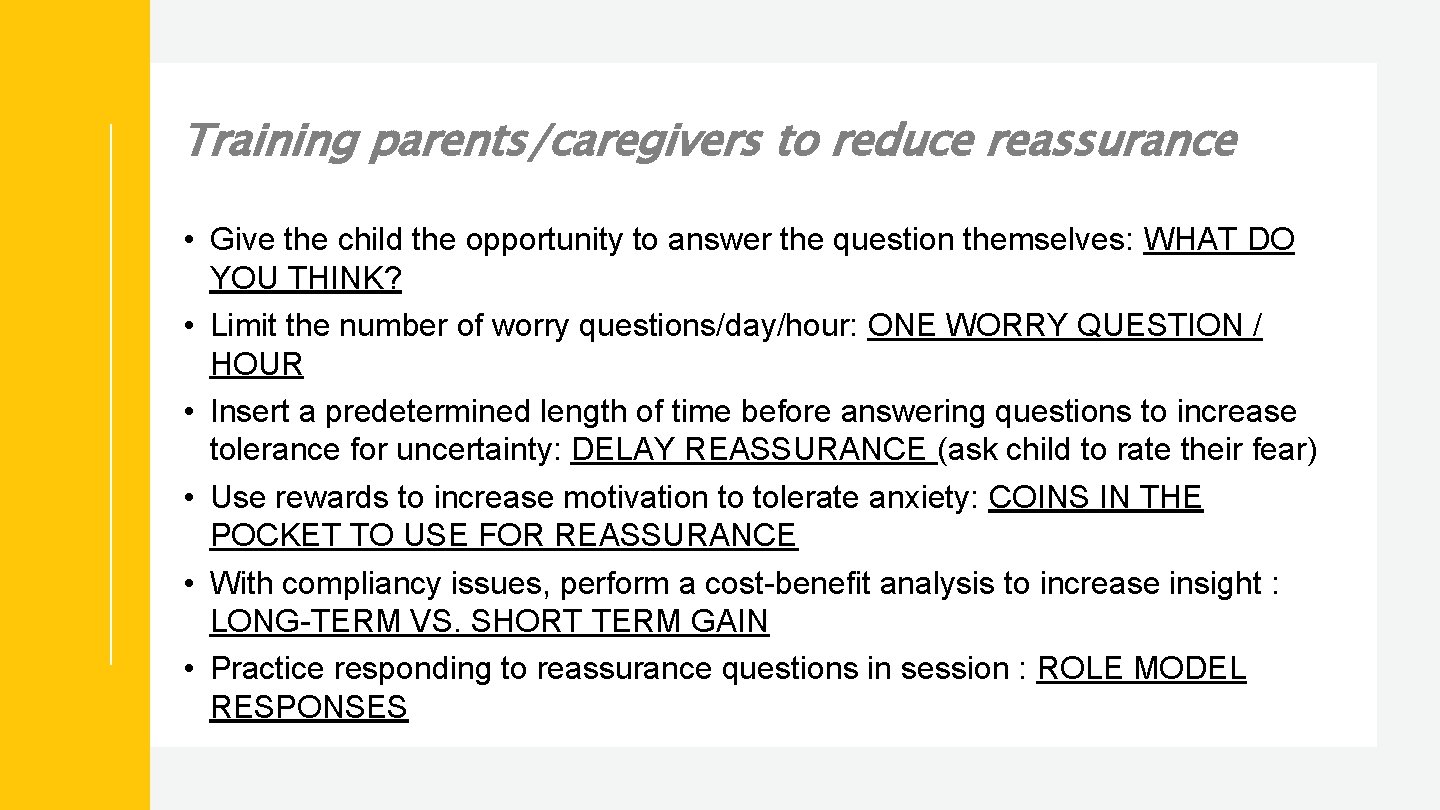
Training parents/caregivers to reduce reassurance • Give the child the opportunity to answer the question themselves: WHAT DO YOU THINK? • Limit the number of worry questions/day/hour: ONE WORRY QUESTION / HOUR • Insert a predetermined length of time before answering questions to increase tolerance for uncertainty: DELAY REASSURANCE (ask child to rate their fear) • Use rewards to increase motivation to tolerate anxiety: COINS IN THE POCKET TO USE FOR REASSURANCE • With compliancy issues, perform a cost-benefit analysis to increase insight : LONG-TERM VS. SHORT TERM GAIN • Practice responding to reassurance questions in session : ROLE MODEL RESPONSES

Coping cards • Reminder that physical symptoms of anxiety are normal • Reminder that anxiety may feel dangerous, but is not • Identify a name your child can give anxiety (e. g. , Mr. Meany, pest, monster) • Realistic thought challenges (e. g. , How many times have I worried about this and it has turned out fine? What would I tell a friend to do in this exact situation? ) • Use of coping skills (e. g. , respiratory control, deep muscle relaxation, reading, talking to a friend, etc. )
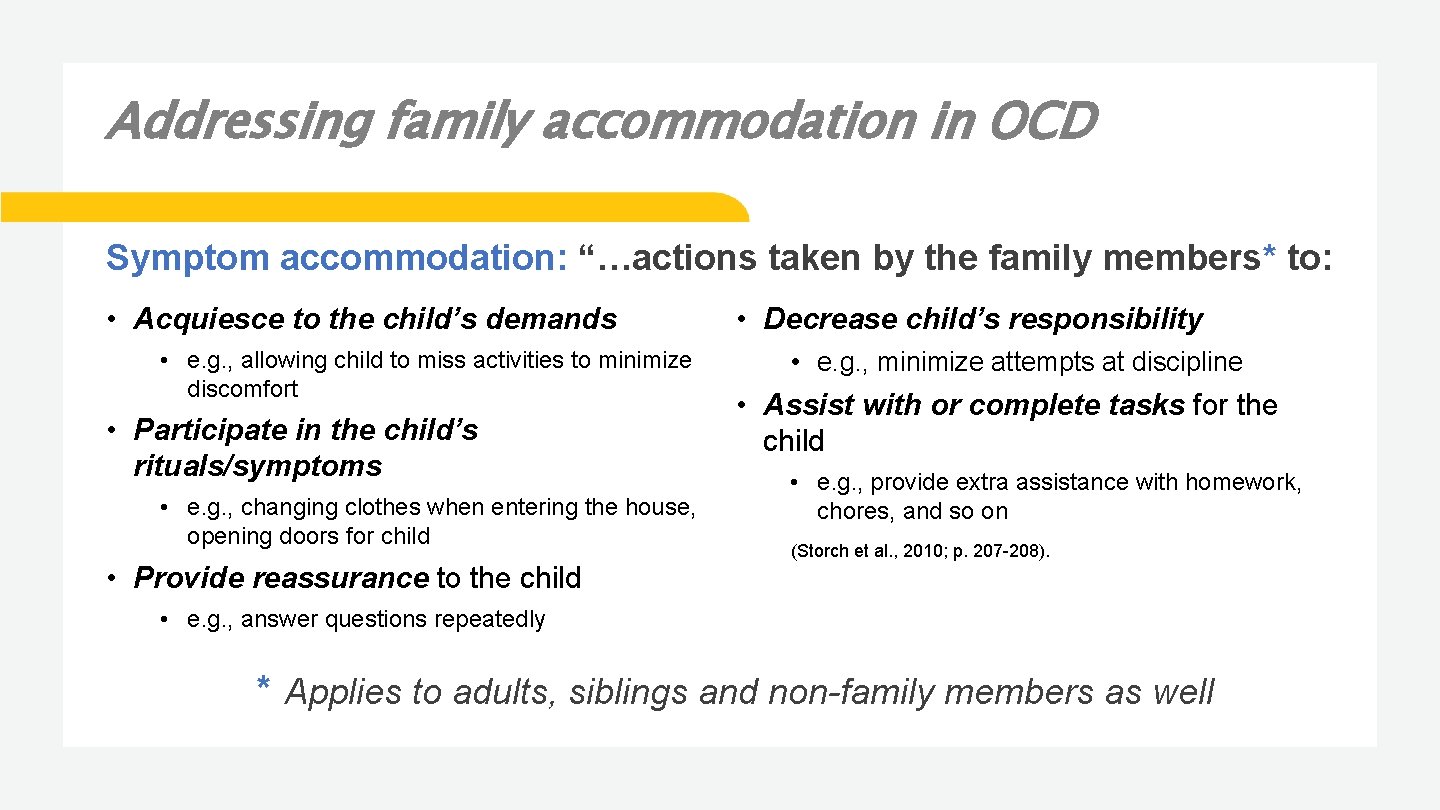
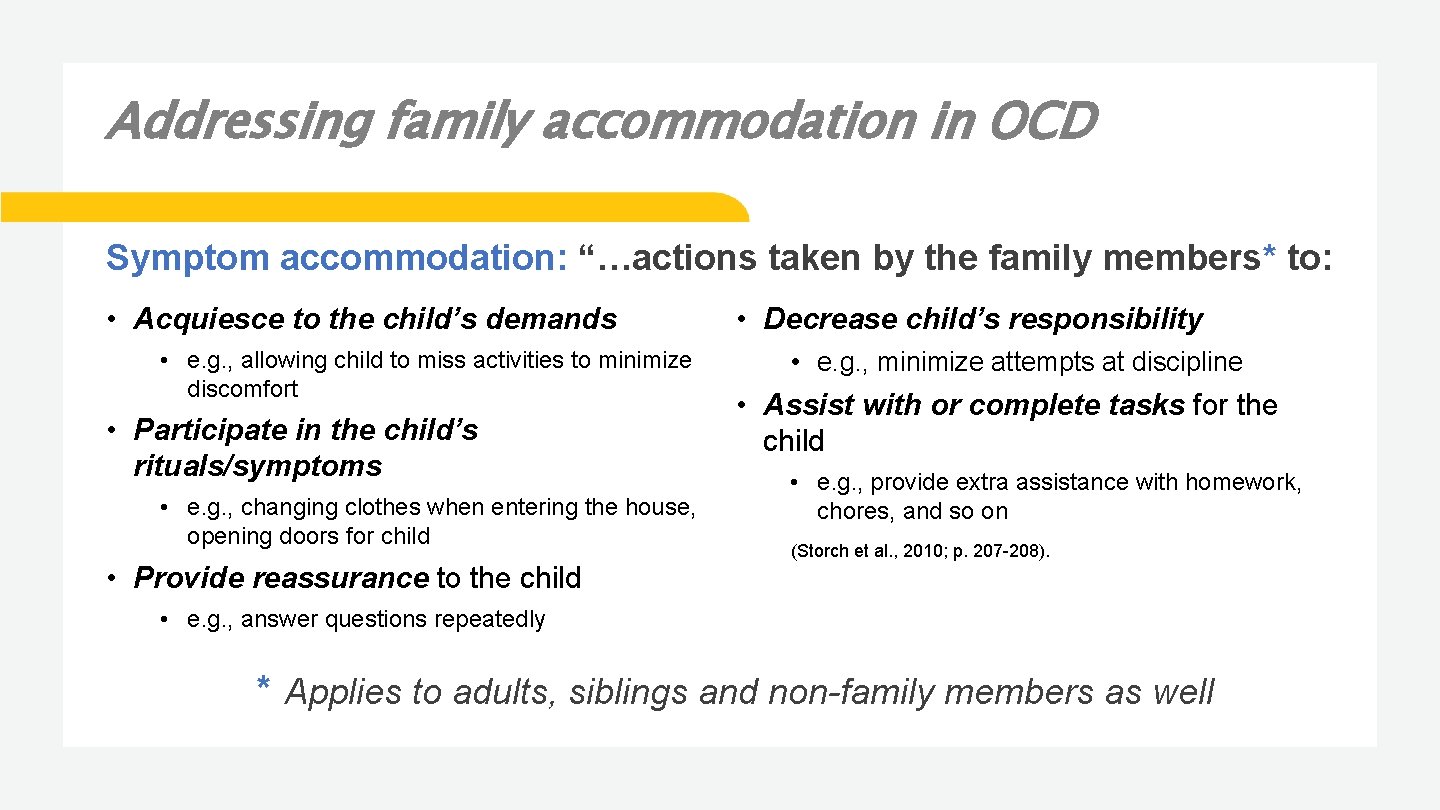
Addressing family accommodation in OCD Symptom accommodation: “…actions taken by the family members* to: • Acquiesce to the child’s demands • e. g. , allowing child to miss activities to minimize discomfort • Participate in the child’s rituals/symptoms • e. g. , changing clothes when entering the house, opening doors for child • Provide reassurance to the child • Decrease child’s responsibility • e. g. , minimize attempts at discipline • Assist with or complete tasks for the child • e. g. , provide extra assistance with homework, chores, and so on (Storch et al. , 2010; p. 207 -208). • e. g. , answer questions repeatedly * Applies to adults, siblings and non-family members as well

Examples of accommodation • Physically assisting a child to hand wash • Opening doors or turning on light switches • Having an uncontaminated place for a child to turn in schoolwork • Providing reassurance • Repeating phrases or actions • Avoiding having a child participate in activities or being around others (social anxiety or contamination concerns)
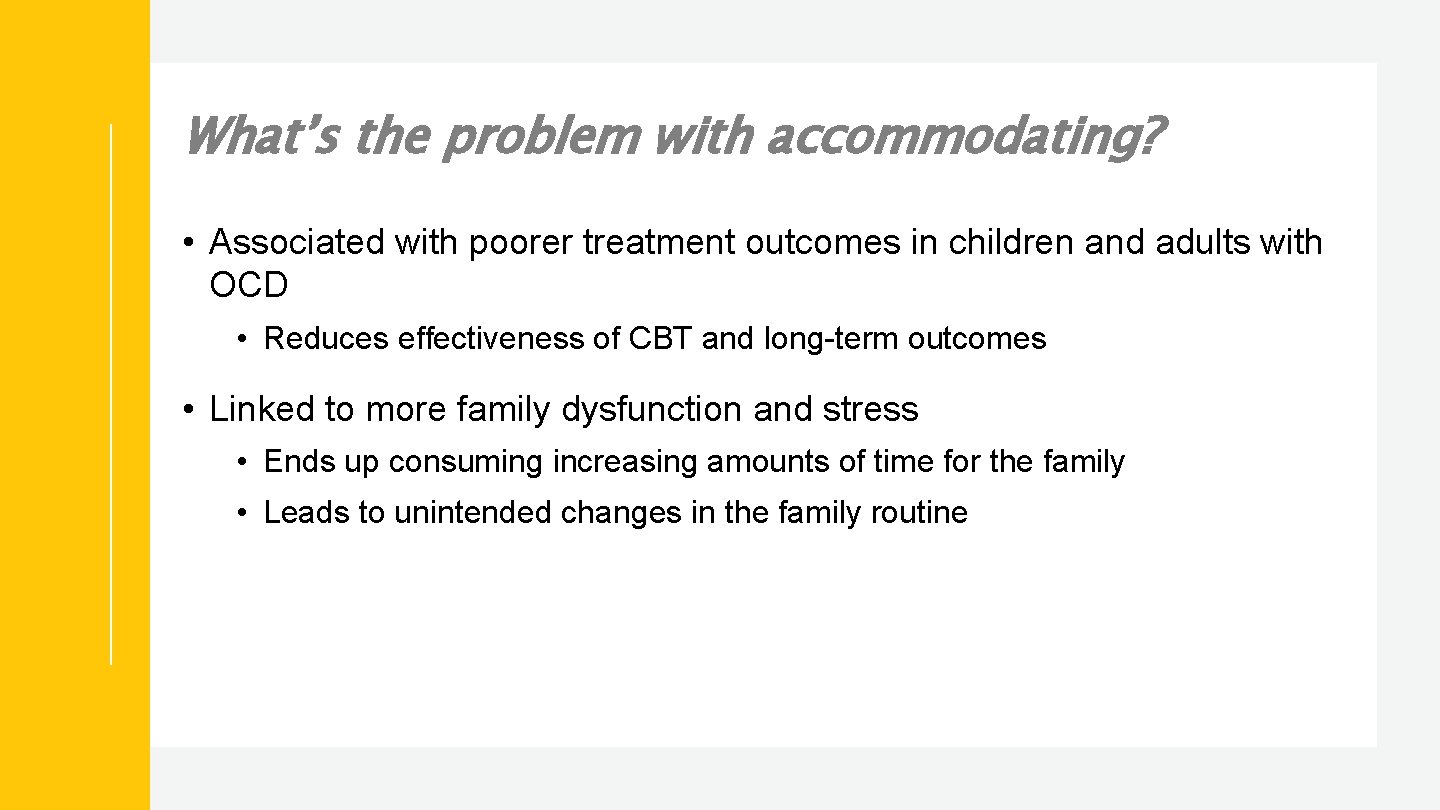
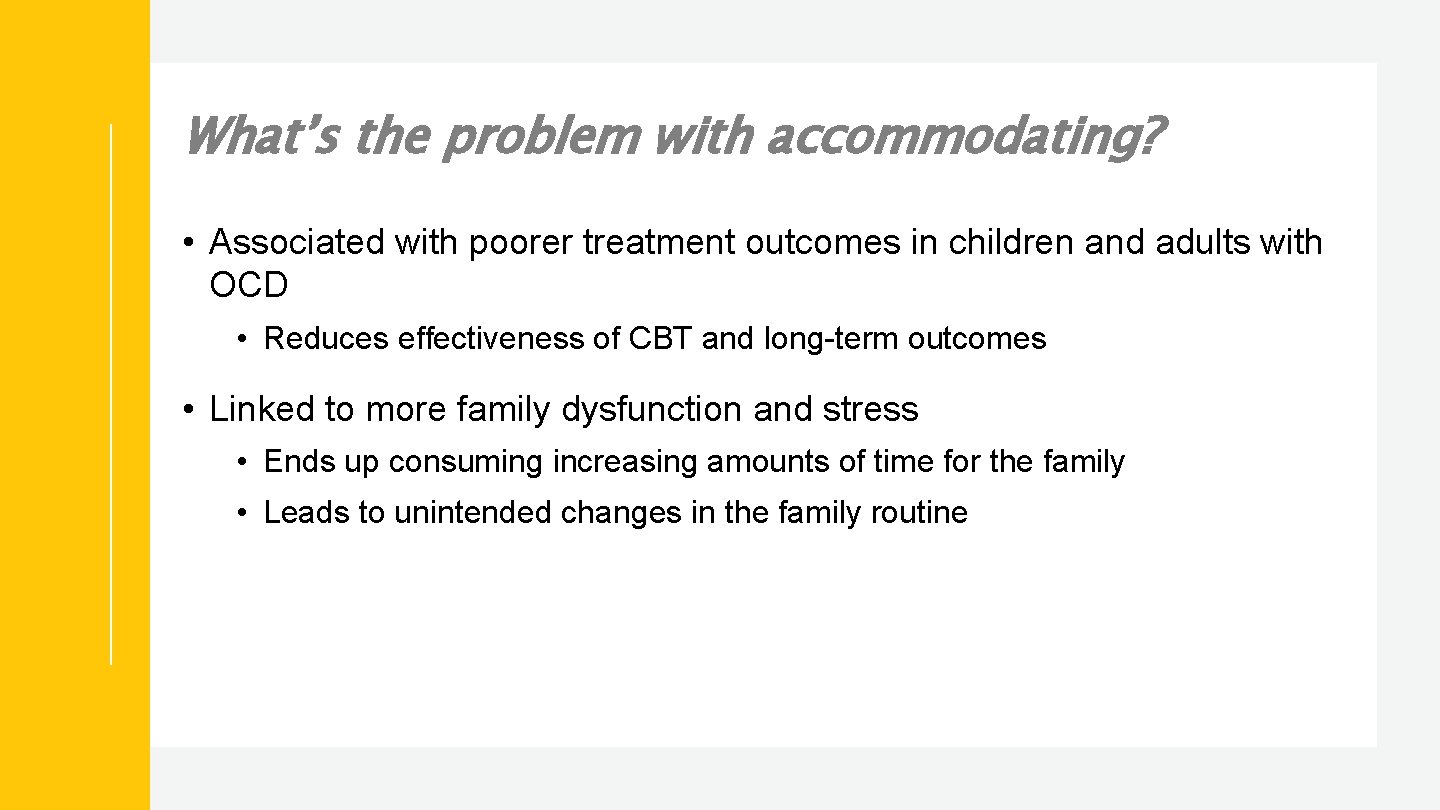
What’s the problem with accommodating? • Associated with poorer treatment outcomes in children and adults with OCD • Reduces effectiveness of CBT and long-term outcomes • Linked to more family dysfunction and stress • Ends up consuming increasing amounts of time for the family • Leads to unintended changes in the family routine
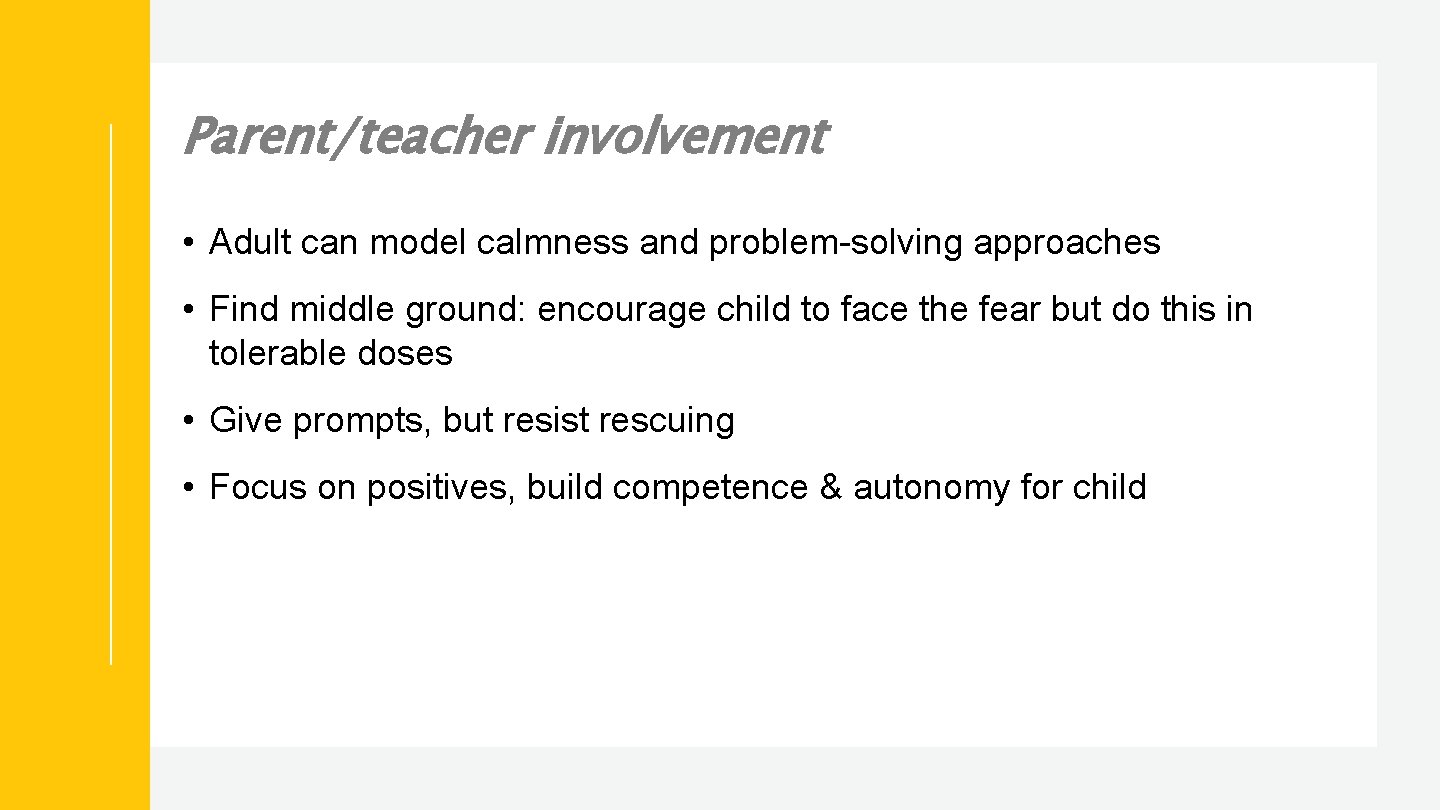
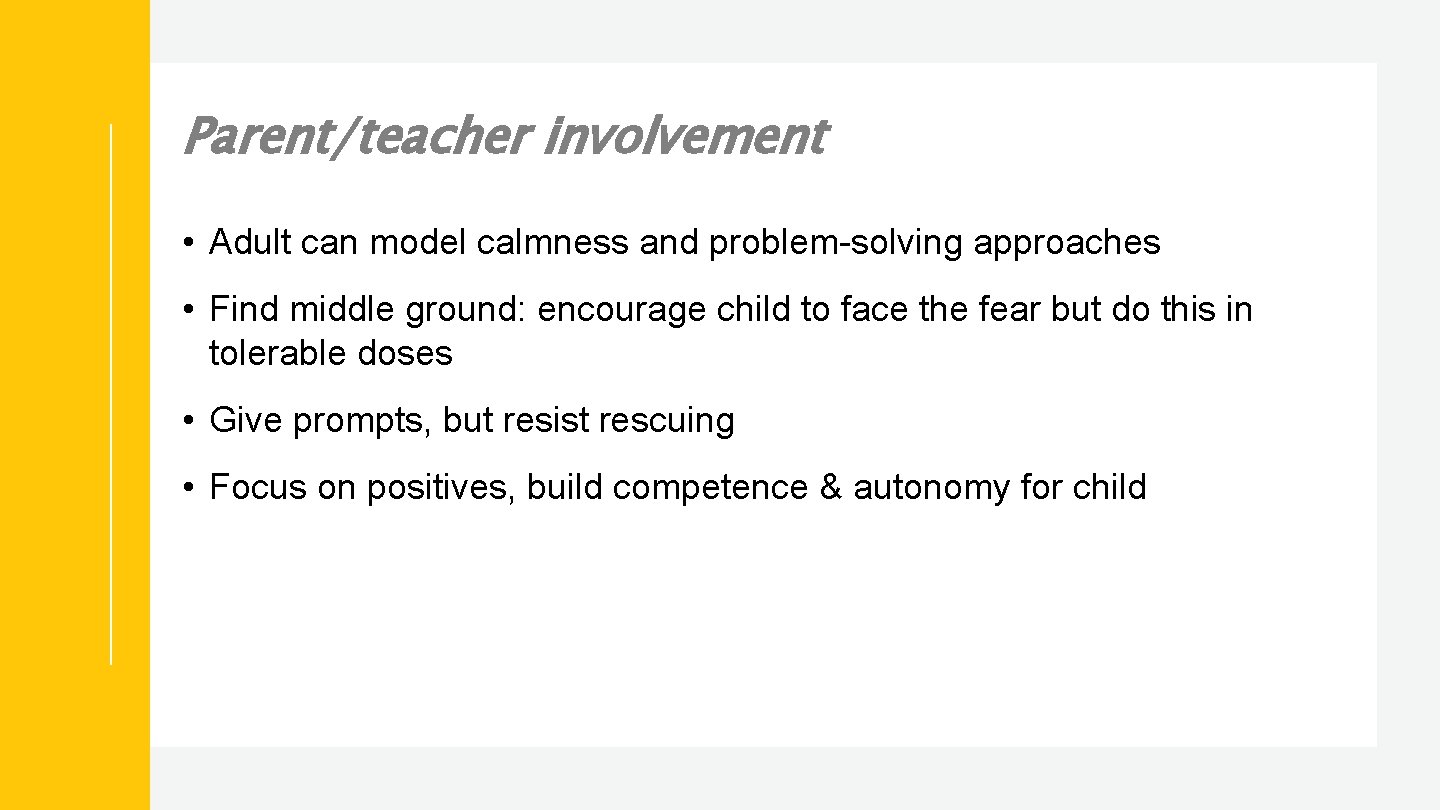
Parent/teacher involvement • Adult can model calmness and problem-solving approaches • Find middle ground: encourage child to face the fear but do this in tolerable doses • Give prompts, but resist rescuing • Focus on positives, build competence & autonomy for child
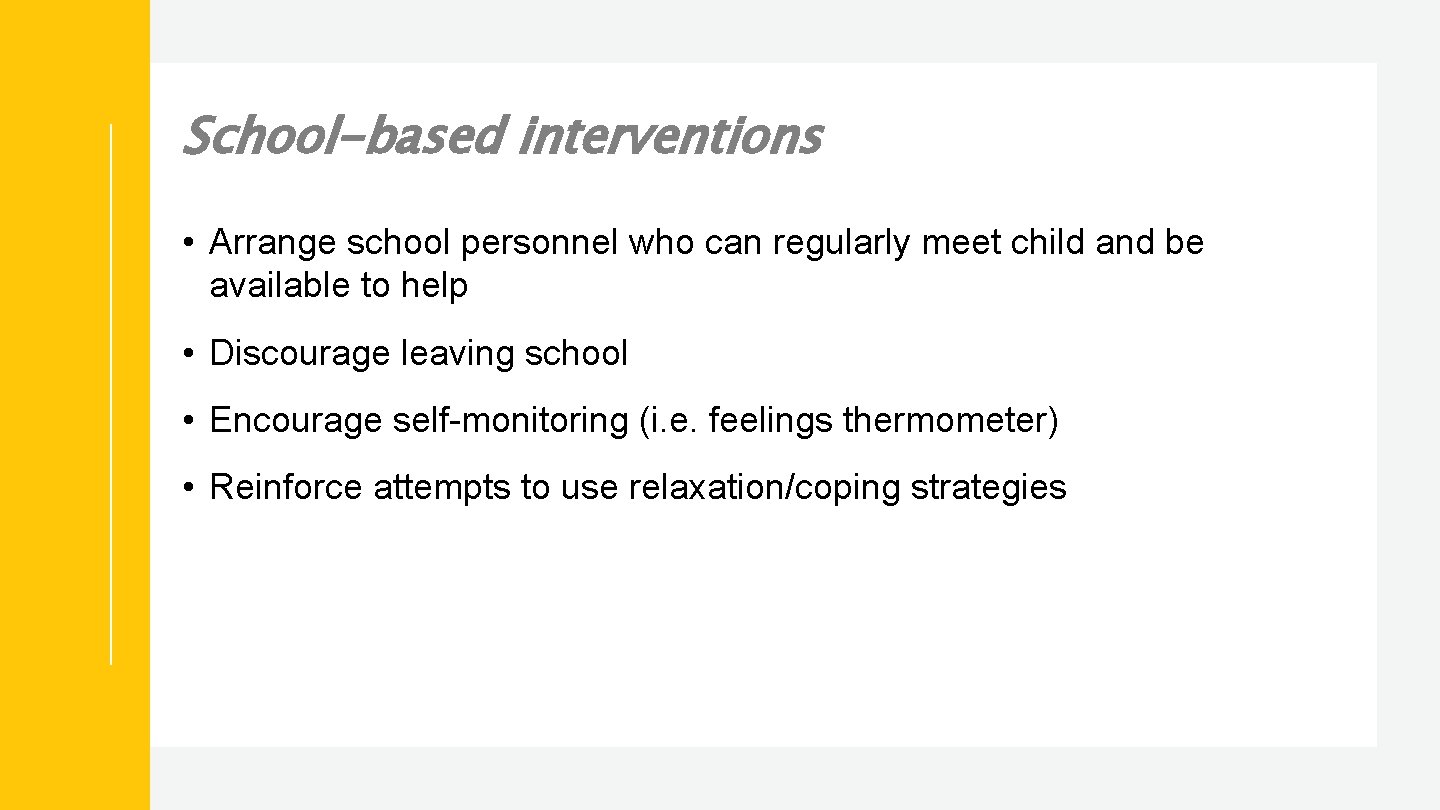
School-based interventions • Arrange school personnel who can regularly meet child and be available to help • Discourage leaving school • Encourage self-monitoring (i. e. feelings thermometer) • Reinforce attempts to use relaxation/coping strategies
School-based interventions • Accommodate late arrivals • Modify assignments • Shorter school days to transition children with separation anxiety • Testing in private • Allow extra time for transitions • Have a “safe” place if child develops increased anxiety or panic attacks
Internet resources American Academy of Child and Adolescent Psychiatry (aacap. org) “Facts for Families” handouts on many topics Latest news on hot topics Parents. Med. Guide. org Question and answer material about depression, suicide and black box warning Links for parents and physicians Up-to-date, well-organized, English-Spanish
Resources Anxiety Disorders Association of America (ADAA): ADAA. org Anxiety Disorders Association of British Columbia: anxietybc. com International OCD Foundation (IOCDF): ocfoundation. org Massachusetts General Hospital: School Psychiatry Program: www 2. massgeneral. org/schoolpsychiatry/
Thank you! Rogers Behavioral Health has two clinic locations in the Twin Cities area: Call us 844 -599 -8959 6442 City West Parkway Suite 200 Eden Prairie, MN 55344 Call or visit: 800 -767 -4411 rogersbh. org 576 Bielenberg Drive, Suite 180 Woodbury, MN 55125
 Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Anxiety disorders def
Anxiety disorders def Icd x anxiety disorders
Icd x anxiety disorders Multipath model of anxiety disorders
Multipath model of anxiety disorders Grief nursing diagnosis
Grief nursing diagnosis Nursing diagnosis of retinal detachment slideshare
Nursing diagnosis of retinal detachment slideshare What are the nursing process
What are the nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing diagnosis three parts
Nursing diagnosis three parts Nursing process objectives
Nursing process objectives Charting exercise chapter 28
Charting exercise chapter 28 Neil's lateral throat form classification
Neil's lateral throat form classification Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Chapter 28 oral diagnosis and treatment planning
Chapter 28 oral diagnosis and treatment planning Perbedaan diagnosis gizi dan diagnosis medis
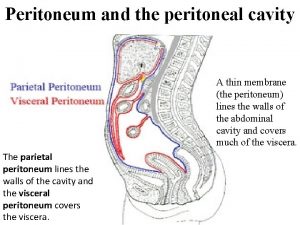
Perbedaan diagnosis gizi dan diagnosis medis What is peritoneal cavity
What is peritoneal cavity Fold of peritoneum
Fold of peritoneum Surgical neck
Surgical neck Omental (epiploic) foramen
Omental (epiploic) foramen Gastrocolic ligament
Gastrocolic ligament Epiploic foramen boundaries
Epiploic foramen boundaries Lesser palatine canal
Lesser palatine canal Peritoneum lecture
Peritoneum lecture Greater ve lesser oksipital sinir bloğu
Greater ve lesser oksipital sinir bloğu Card stacking advertising
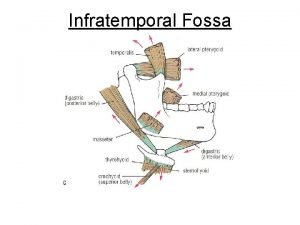
Card stacking advertising Temporal and infratemporal fossa
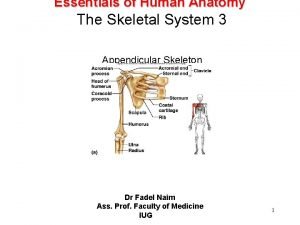
Temporal and infratemporal fossa Greater tubercle of humerus
Greater tubercle of humerus Extremity
Extremity Sighkee
Sighkee Slash and burn agriculture
Slash and burn agriculture Spoke wheel pattern in gastric ulcer
Spoke wheel pattern in gastric ulcer Tristram lesser
Tristram lesser Lesser roman gods
Lesser roman gods Lesser tubercle
Lesser tubercle Rickets
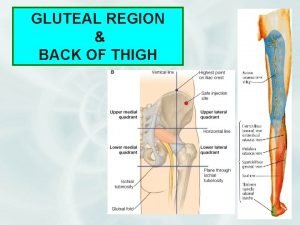
Rickets Nerve supply of gluteus maximus
Nerve supply of gluteus maximus Lesser omentum
Lesser omentum Lymphatic drainage of lower limb
Lymphatic drainage of lower limb Jeff lesser
Jeff lesser Palatin
Palatin Lindley wall md
Lindley wall md Chapter 8 managing stress and anxiety
Chapter 8 managing stress and anxiety Frustration anxiety and tension
Frustration anxiety and tension Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Cpi defensive behavior
Cpi defensive behavior Anxiety symptoms
Anxiety symptoms Igor areh
Igor areh Relaxation techniques test anxiety
Relaxation techniques test anxiety Anxiety symptoms
Anxiety symptoms I'm a perfect example of someone who has math anxiety
I'm a perfect example of someone who has math anxiety Neurotic behavior
Neurotic behavior Neurotic definition
Neurotic definition Examples of generalized anxiety disorder
Examples of generalized anxiety disorder Free floating anxiety
Free floating anxiety Ocd ego syntonic
Ocd ego syntonic Uw integrative medicine
Uw integrative medicine Astrid zamora
Astrid zamora Mecbal
Mecbal Generalized anxiety disorder dsm 5
Generalized anxiety disorder dsm 5 Define neurotic
Define neurotic Neurotic anxiety example
Neurotic anxiety example Pie nursing examples
Pie nursing examples Test anxiety essay
Test anxiety essay Chapter 18 managing anxiety
Chapter 18 managing anxiety Caregiver anxiety
Caregiver anxiety Levels of anxiety nursing
Levels of anxiety nursing Sucheta connolly md
Sucheta connolly md Ocd behaviors
Ocd behaviors Hildegard peplau levels of anxiety
Hildegard peplau levels of anxiety Anxiety vs apprehension
Anxiety vs apprehension Agoraphobia vs social anxiety
Agoraphobia vs social anxiety Agoraphobia vs social phobia
Agoraphobia vs social phobia Snri social anxiety
Snri social anxiety Amy drahota
Amy drahota