PEDIATRIC AND ADOLESCENCE GYNECOLOGY SUPERVISOR PROF AYMAN SHAAMASH





![A. Mullerian agenesis (Mayer-von Rokitansky. Kauster-Hauser [MRKH] syndrome) 23 Group A A. Mullerian agenesis (Mayer-von Rokitansky. Kauster-Hauser [MRKH] syndrome) 23 Group A](https://slidetodoc.com/presentation_image_h2/09b84b77bbc46a3a08c877a58d4630af/image-23.jpg)




![Managment • First-line therapy is prostaglandin inhibitors (nonsteroidal anti-inflammatory drugs [NSAIDs] • If the Managment • First-line therapy is prostaglandin inhibitors (nonsteroidal anti-inflammatory drugs [NSAIDs] • If the](https://slidetodoc.com/presentation_image_h2/09b84b77bbc46a3a08c877a58d4630af/image-57.jpg)
- Slides: 61
PEDIATRIC AND ADOLESCENCE GYNECOLOGY SUPERVISOR : PROF. AYMAN SHAAMASH DONE BY : GROUP A 1 Group A

INTRODUCTION ▪ An awareness of the problems that are unique to pediatric and adolescent gynecology is invaluable for proper management of the young patient. Particular care is essential in addressing gynecologic concerns in emotional trauma this age group because both physical and may be inadvertently inflicted. 2 Group A
A. Normal findings in a pediatric patient. A mucoid vaginal discharge. An introitus that is located more anteriorly than normal and a clitoris that is more prominent than normal ( 1 to 2 cm ). A redundant hymen that may protrude on straining and that remains essentially the same size until 10 years of age. A vaginal epithelium that is uncornified and erythematous with an alkaline p. H. A small uterus ( 2. 5 to 3 cm ) in length. A cervical os that is covered with glandular epithelium and normally appears red ( ectropion ) 3 Group A
B. Normal findings in an adolescent patient . Intact hymen in those not sexually active. Postpubertal gynecologic examination in an adolescent is similar to an adult female. 4 Group A
C. Visualization of the vagina. Instruments for visualizing the vagina include the vaginoscope , the urethroscope , and the pediatric speculum. To determine the presence or absence of internal genitalia , ultrasound and MRI are helpful. D. Rectal examination is often more informative than a vaginal examination. 5 Group A
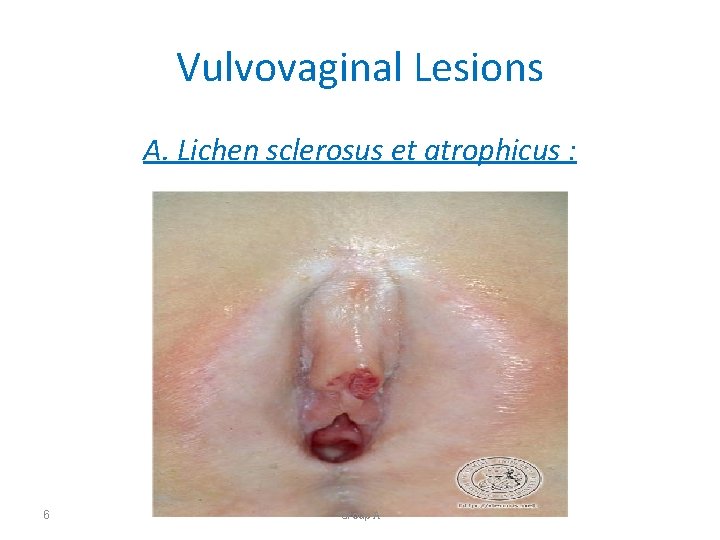
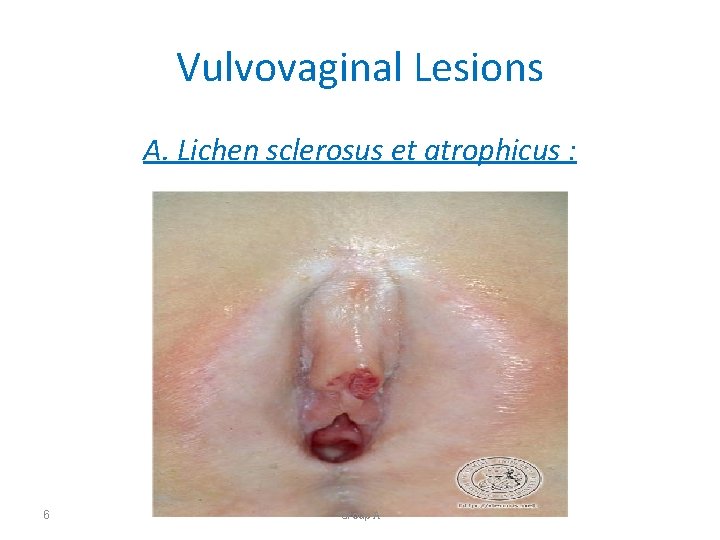
Vulvovaginal Lesions A. Lichen sclerosus et atrophicus : 6 Group A

A. Lichen sclerosus et atrophicus. Clinical picture : vulvar itching. A white , papular lesion resembling leukoplakia may cover the vulva and perianal regions. Etiology : Causes are unknown. . Diagnosis : Biopsy. Management : This condition is benign and can be Self-limiting. Improved hygiene is the first line of therapy. 7 Group A

B. Trauma 8 Group A
B. Trauma. Clinical picture Tears , abrasions , ecchymoses , and hematomas are common in preadolescent girls. The incidence is highest in children between 4 and 12 years of age. The most common mechanism of injury are sexual abuse, straddle injuries , accidental penetration , sudden abduction of the extremities , and pelvic fractures. 9 Group A
Management. A vaginoscope is used to visualize the vagina to locate sources of bleeding. A large vaginal laceration may result in an expanding hematoma in the retroperitoneal space. Superficial abrasions and lacerations of the vulva , if not actively bleeding , can be cleaned and left alone. . Conservative therapy. . In sexual abuse , antibiotic therapy is advised as prophylaxis against sexually transmitted diseases. 10 Group A
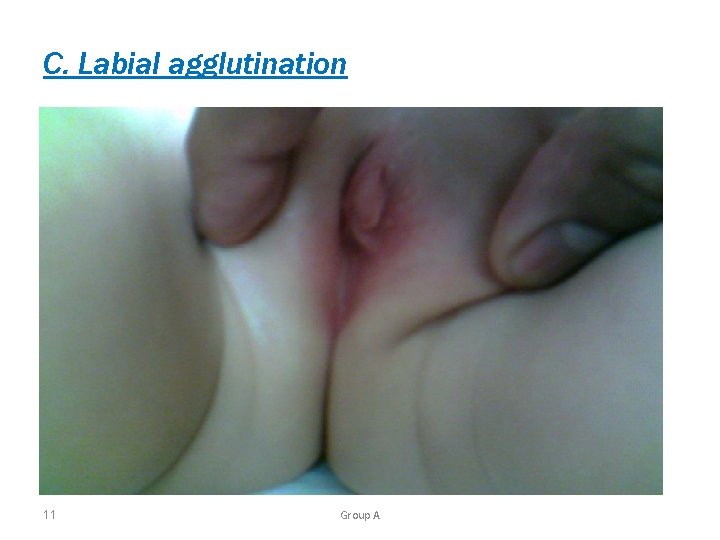
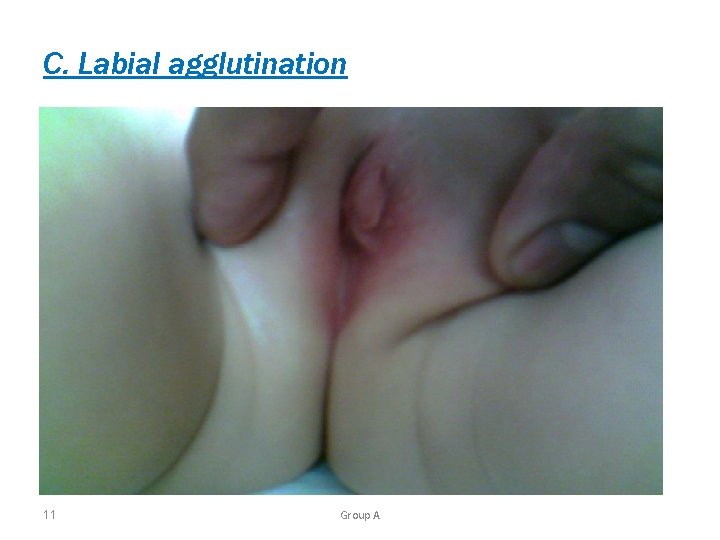
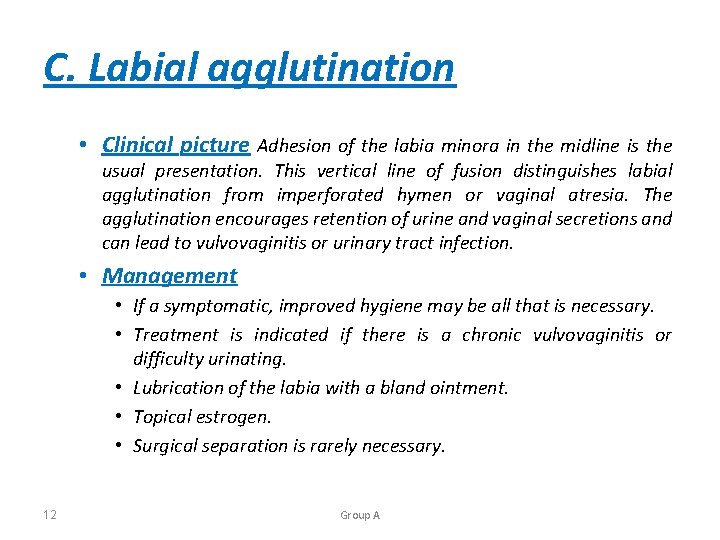
C. Labial agglutination 11 Group A
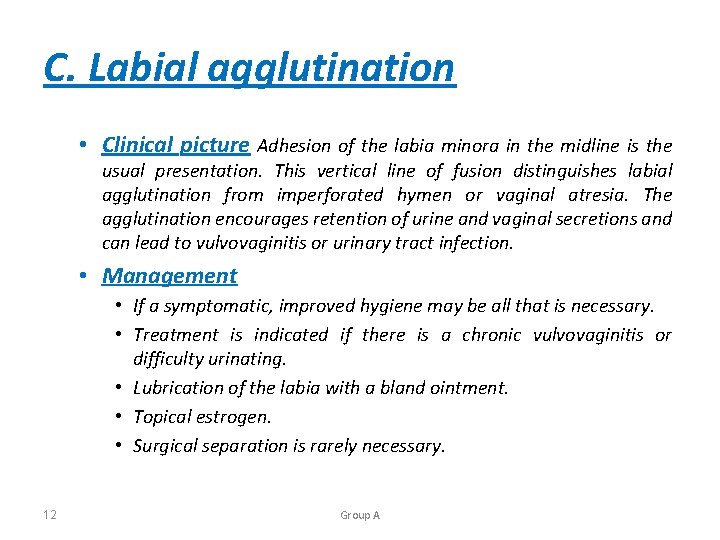
C. Labial agglutination • Clinical picture Adhesion of the labia minora in the midline is the usual presentation. This vertical line of fusion distinguishes labial agglutination from imperforated hymen or vaginal atresia. The agglutination encourages retention of urine and vaginal secretions and can lead to vulvovaginitis or urinary tract infection. • Management • If a symptomatic, improved hygiene may be all that is necessary. • Treatment is indicated if there is a chronic vulvovaginitis or difficulty urinating. • Lubrication of the labia with a bland ointment. • Topical estrogen. • Surgical separation is rarely necessary. 12 Group A
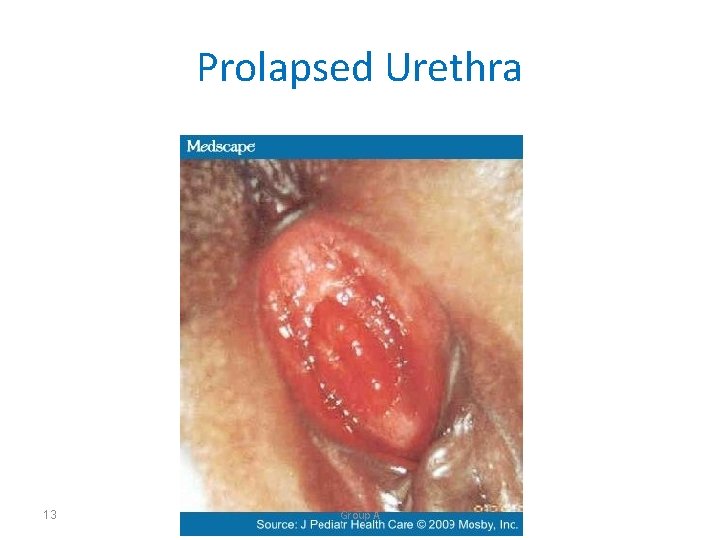
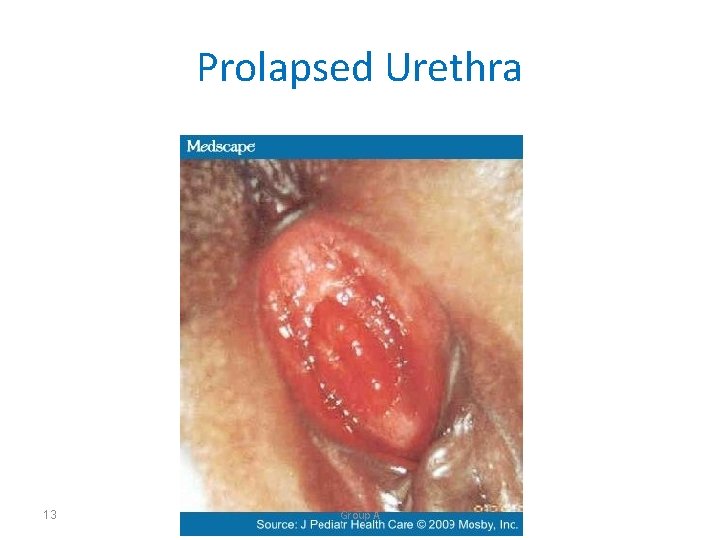
Prolapsed Urethra 13 Group A
14 • Clinical picture A small, hemorrhagic, friable mass surrounding the urethra is the most common presentation. • Management • If voiding is uninhibited, local therapy. • Topical estrogen and sitz bath are the mainstays of therapy. The prolapse usually resolves after 4 weeks of therapy. • If urinary tract retention or necrosis is present, surgical repair and catheterization are necessary. Group A
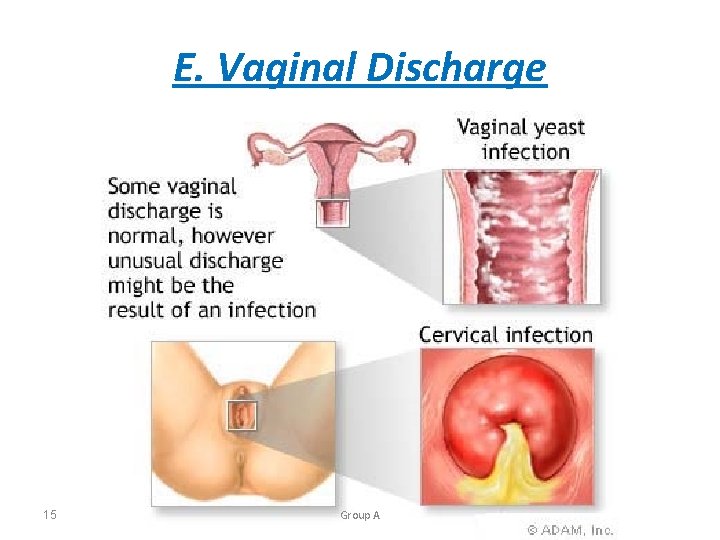
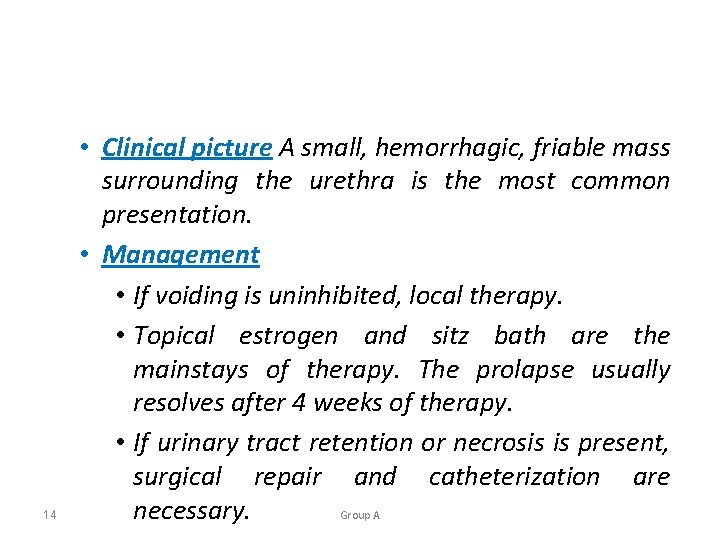
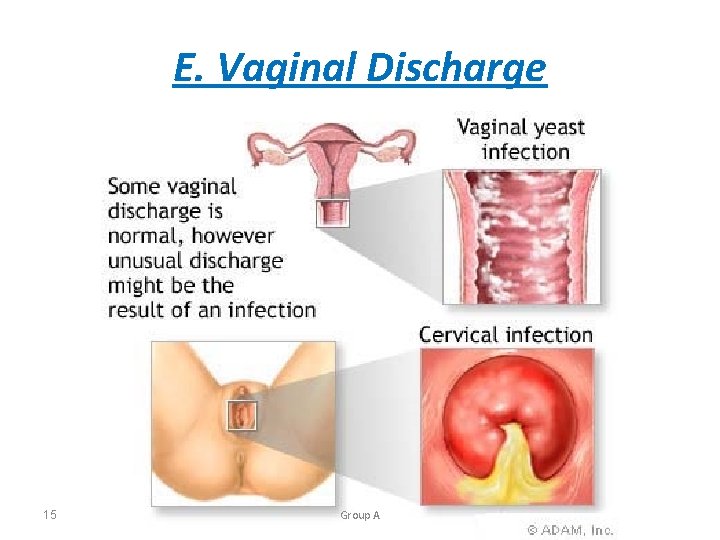
E. Vaginal Discharge 15 Group A
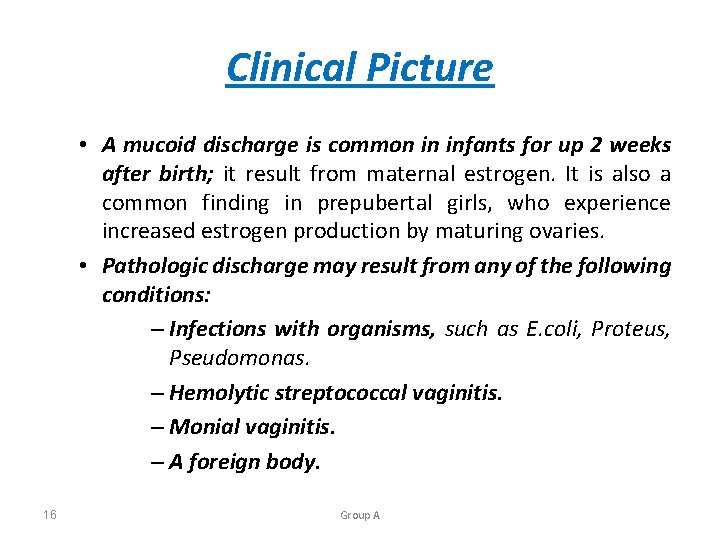
Clinical Picture • A mucoid discharge is common in infants for up 2 weeks after birth; it result from maternal estrogen. It is also a common finding in prepubertal girls, who experience increased estrogen production by maturing ovaries. • Pathologic discharge may result from any of the following conditions: – Infections with organisms, such as E. coli, Proteus, Pseudomonas. – Hemolytic streptococcal vaginitis. – Monial vaginitis. – A foreign body. 16 Group A
Managment • Conservative management is advisable, as follows: Culture to identify causative organisms. Urinanalysis to rule out cystitis. Review proper hygiene. Perianal examination with transparent tape to test for pinworms. • In cases of persistent discharge, examination under anesthesia is indicated to rule out foreign body. • • 17 Group A

III. Neoplasms A. Tumors of the vagina 18 Group A
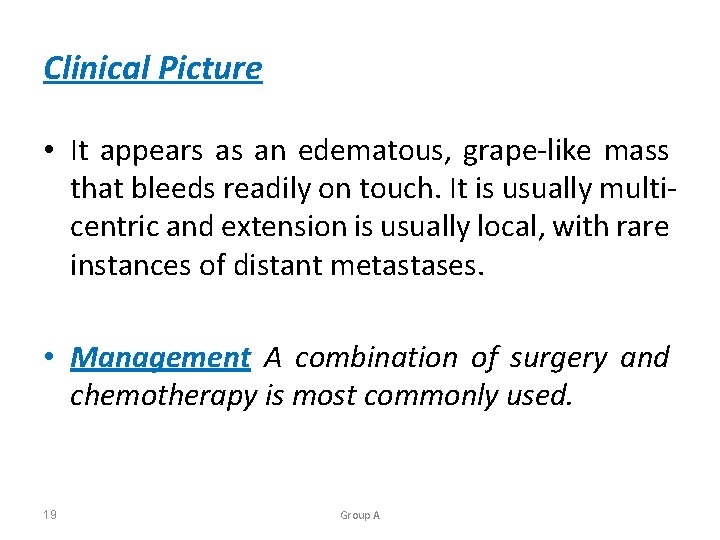
Clinical Picture • It appears as an edematous, grape-like mass that bleeds readily on touch. It is usually multicentric and extension is usually local, with rare instances of distant metastases. • Management A combination of surgery and chemotherapy is most commonly used. 19 Group A
B. Ovarian Tumors • Clinical Picture: • Non-germ cell origin • Lipoid cell tumors( estrogen producing) • Granules theca cell tumors(estrogen producing) • Germ cell origin Benign cystic teratomas. Benign cysts. Arrhenoblastomas (androgen producing). Dysgerminomas and gonadoblastomas ( tumors of dysgenetic gonads). • Endodermal carcinomas ( human chorionic gonadotropin [hcg]- secreting tumors). • Immature teratomas. • • 20 Group A

Managment • Treatment is surgical, alone or in combination with chemotherapy, depending on the tumor. Radiation is sometimes used to treat dysgerminomas. 21 Group A
Congenital Anomalies in the Pediatric Patient 22 Group A
![A Mullerian agenesis Mayervon Rokitansky KausterHauser MRKH syndrome 23 Group A A. Mullerian agenesis (Mayer-von Rokitansky. Kauster-Hauser [MRKH] syndrome) 23 Group A](https://slidetodoc.com/presentation_image_h2/09b84b77bbc46a3a08c877a58d4630af/image-23.jpg)
A. Mullerian agenesis (Mayer-von Rokitansky. Kauster-Hauser [MRKH] syndrome) 23 Group A
Clinical pictures Amenorrhea Ovarian development is normal The uterus is usually absent Vaginal agenesis(normal 46 xx karyotype) Management Surgical creation of neovagina 24 Group A
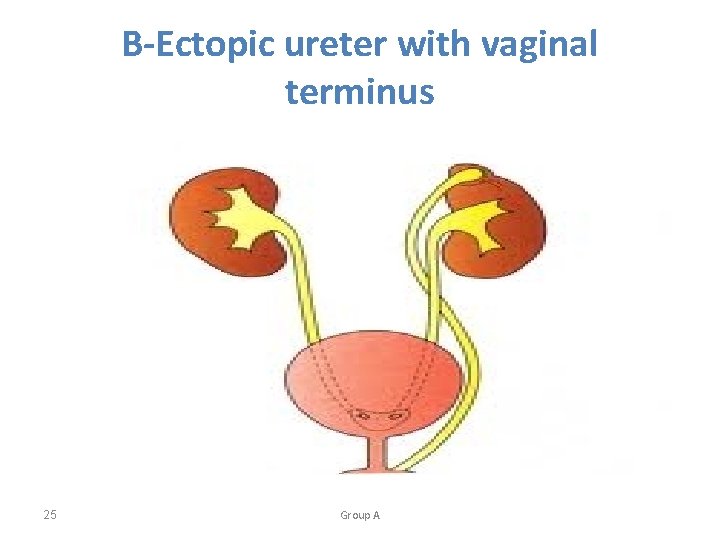
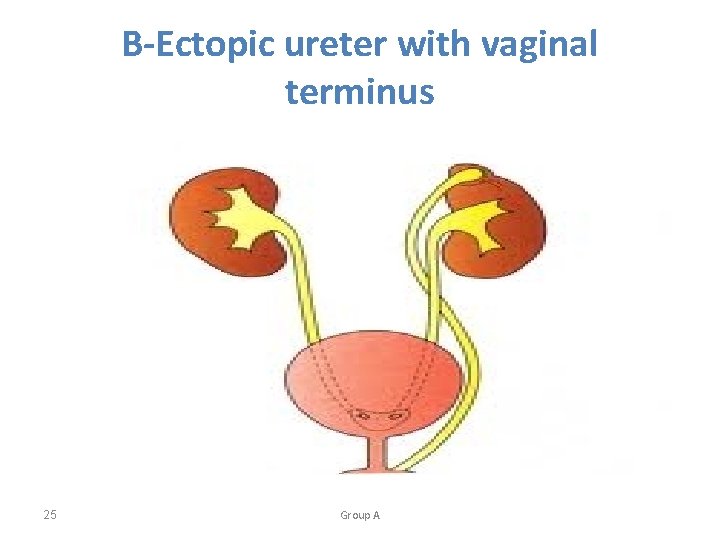
B-Ectopic ureter with vaginal terminus 25 Group A
Clinical pictures • Ectopic ureter, the most common cause of vaginal cysts in infants, presents as uretrocele, which appears as cystic mass protruding from the vagina. • Irritation • Vaginitis may be presenting signs • Hydroureter • Hydronephrosis 26 Group A
Diagnosis • Intravenous pyelography, which allows visualization of the entire urinary tract. Management • Resect the lowest portion of the ureter and implant it into the bladder. • Remove the ureter and associated portion of the kidney 27 Group A
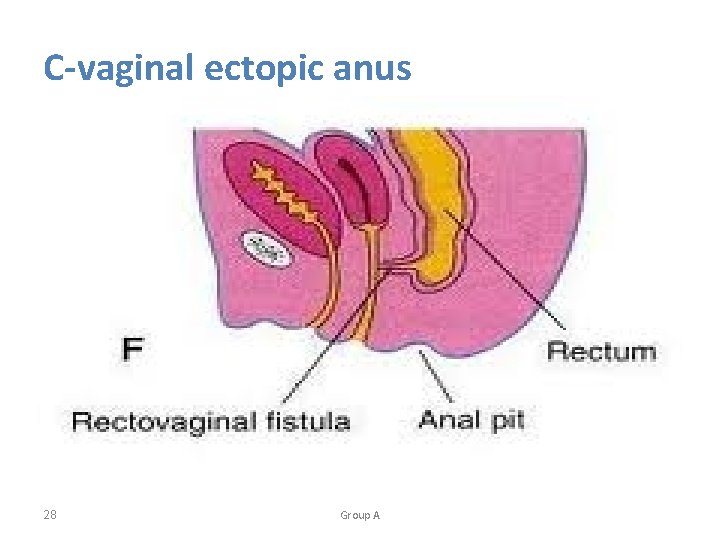
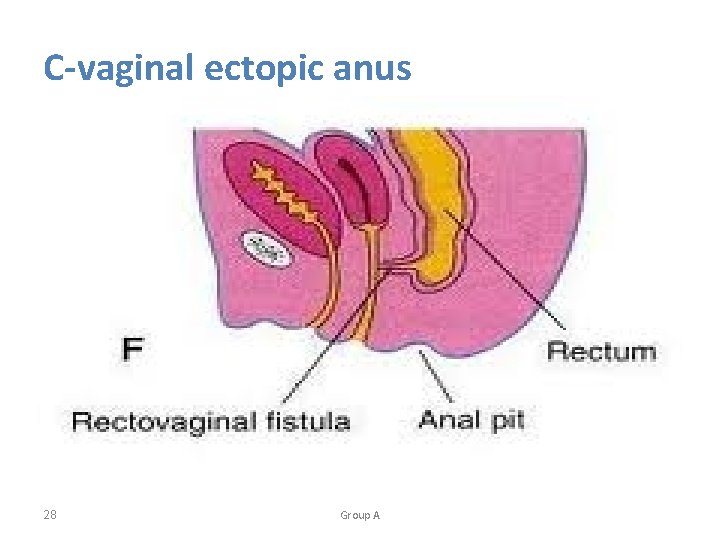
C-vaginal ectopic anus 28 Group A
Clinical picture • Imperforate anus associated with rectovaginal communication Management • Surgical correction is indicated 29 Group A
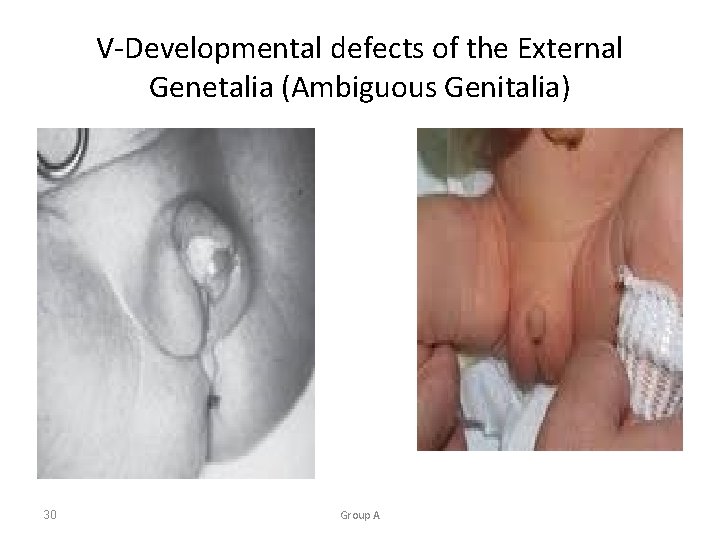
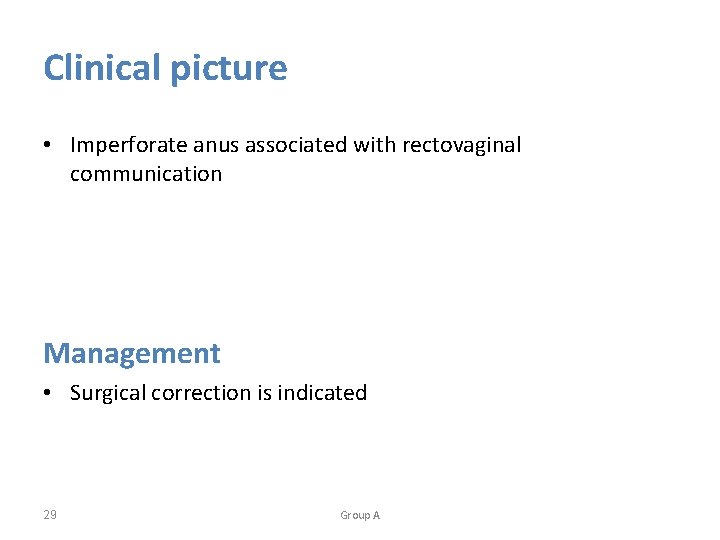
V-Developmental defects of the External Genetalia (Ambiguous Genitalia) 30 Group A
• Ambiguous genitalia results when hormones with androgenic activity are present during development of female fetus, or androgens or androgen activity are absent during development of male fetus. 31 Group A
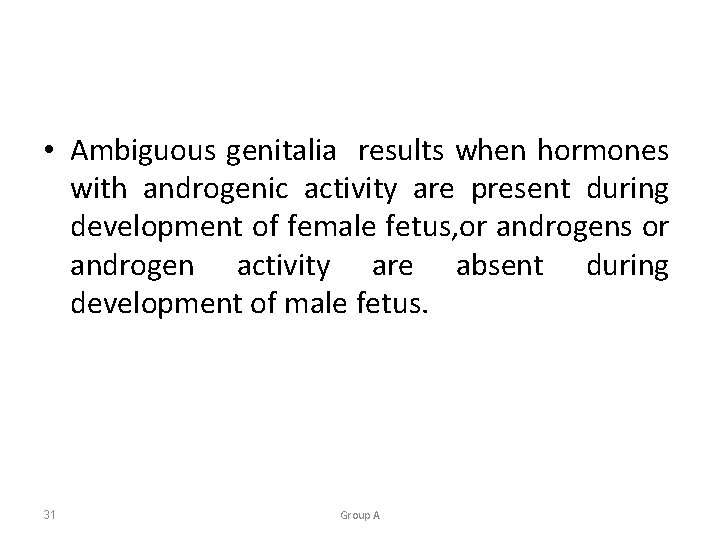
A-Congenital adrenal hyperplasia (CAH) • Cortisol and aldosterone pathways are impaired. • The 21 -hydroxylase defect is the most common cuse of distinct virilization of the female newborn. • Its incidence is 1 in 5000 births, and it accounts for 95% of all cases of congenital adrenal hyperplasia, which is inherited as an autosomal recessive trait. 32 Group A
Clinical picture • The chromosomes, gonads, and internal genitalia are female, but the external genitalia are virilized to varying degrees. • Urogenital orifice closed. • Clitoral enlargement and accentuation of labial folds are characteristic. 33 Group A
Diagnosis • Serum 17 -hydroxyprogestrone and dehydroepiandrosterone (DHEA) obtained after 24 hours of life are both elevated. • A blood karyotype • Serum electrolytes should be followed because salt wasting. Management • Hydrocortisone. 34 Group A
B-Adrenal tumors • These tumors, which may cause virilization of the external genitalia after infancy, should be suspected in children with high levels of dehydroepiandrosterone sulfate (DHEAS). 35 Group A
C-maternal ingestion of androgenic substances • This condition can result in masculinization of the female fetus. Causal agents identified include androgens, danazol, any synthetic progestins(in doses much higher than in oral contraceptive pills). 36 Group A
Clinical picture • The clitoris is enlarged and the labia may be fused, but the vagina, tubes, and uterus are normal. • Growth and development are normal, and progressive viritization does not occur. Diagnosis • The condition can be diagnosed based on positive history and on exclusion. Management • Clitoral reduction and surgical correction of the fused labia maybe necessary. 37 Group A
D-childhood ingestion of androgens • This condition usually involves preparations that have androgenic activity. 38 Group A
Clinical picture • Clinical manifestations are the same as those resulting from maternal ingestion of androgenic substances (i. e. , masculinization). Management • Therapy involves clitoral reduction and surgical correction of the fused labia , if necessary. 39 Group A

E-Androgen insensitivity syndrome (testicular feminization) 40 Group A
Clinical picture • A 46 xx genotype is present, but a female phenotype develops. • Androgens are produced by the testes (which develop in the presence of y chromosome) and by adrenal glands. • External genitalia are feminized • No uterine, cervical, upper vaginal, or fallopian tube development. • A short vagina. • Labia, may contain testes. • An incomplete form (reifenstein syndrome) occurs in which external genitalia appear virilized. 41 Group A
Diagnosis • Primary amenorrhea. • A blind or absent vagina. • Lack of pubic and axillary hair development. Breast development does occur because estrogen concentration is high due to conversion of testosterone produced after puberty. • A karyotype. • This syndrome is distinguished from MRKH by absent axillary and pubic hair development and high testosterone level. 42 Group A
Management • The gonads should be removed because of an incresed risk of malignancy (3% to 4% before 25 years of age ) 43 Group A
F. True hermaphroditism Clinical picture • The genotype is 46 xx • The external genitalia may appear male, female, or ambiguous. • Both male and female internal genitalia may be present. Management • The genitlia that are inconsistent with sex assignment should be surgically removed or modified. 44 Group A
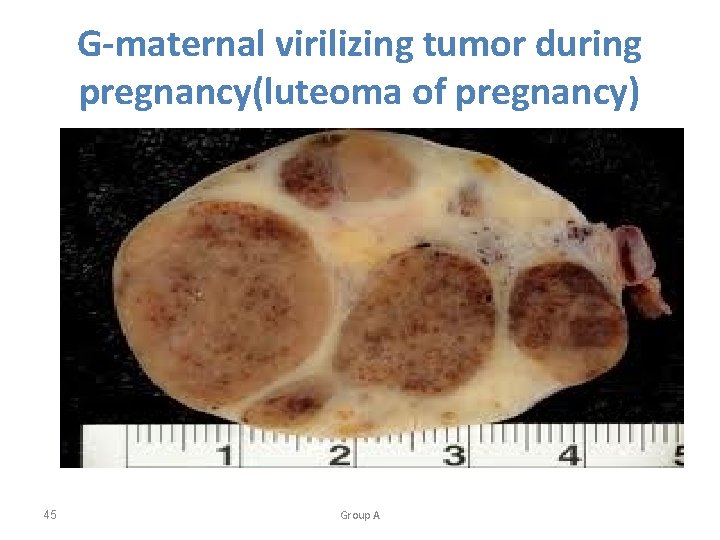
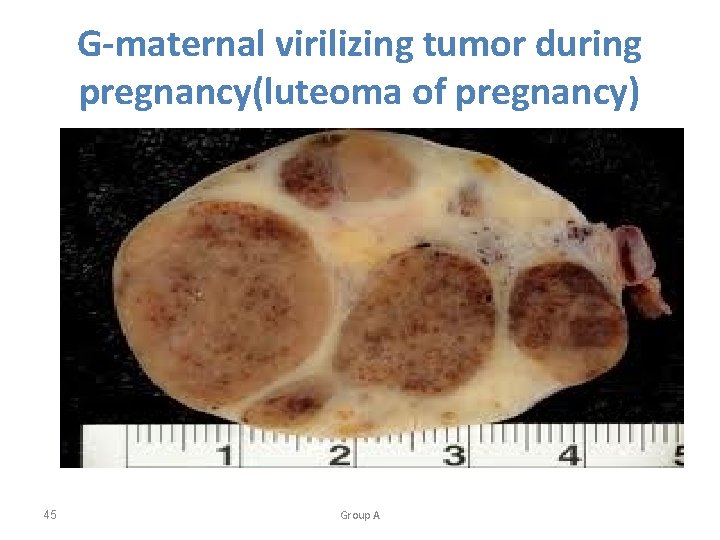
G-maternal virilizing tumor during pregnancy(luteoma of pregnancy) 45 Group A
• This condition may result in masculinization of the female fetus. The clinical picture and therapy are similar to those for the maternal ingestion of androgenic substances. • Psychological development and mental capacity are consistent with choronologic age. Reproductive potential is not adversely affected, and the patient can become pregnant. 46 Group A
Normal Pubertal Development • Increased production of lutenizing hormone and folliclestimulating hormone, as other factors(such as leptin), is responsible for the irritiation of the pubertal process. • Growth spurt. begins before the onset of other signs of the puberty. Usually 1 year before menarch. • Thelarche. The onset of breast development usually begins between 9 and 11 years of age. It is a sign of ovarian estrogen production. Tanner stages describe the normal changes in the transition from the pubertal to the mature breast contour. 47 Group A
• Adrenarche and pubarche. Adrenarche refers to the production of androgens from the adrenal gland, and pubarche is the development of axillary and pubic hair that results from the adrenal and gonadal androgens. Pubarche usually follows thelarche in the pubertal. • Menarche. In menarche, vaginal bleeding occurs in response to hormonal changes , specifically production of estrogen by the ovary, for the first time. The average of the first menses is 12 to 13 years. 48 Group A

Abnormal pubertal development • Delayed puberty: is characterized by the absence of breast development by age 13 years or the absence of menses by age 16 years 49 Group A
• Hypergonadotropic hypogonadism : this layed condition affects almost 50 % of all patients with delayed puberty. It includes conditions in which the ovaries or gon ads are not functioning and are unable to respond to gonadotropins as a result gonadotropin levels are high. 50 Group A

• Hypogonadotropic hypogonadism : This condition accounts for 10% to 15% of patients with pubertal delay. The ovary is normal , however, there is a lack of production of hormonal stimulation from the hypothalamus. hypogonadotropic hypogonadism includes Kallmann syndrom (isolated Gn. RH deficiency ) 51 Group A
• Eugonadotropic: constitutional delay accounts for 10% to 20% of cases. These patients have normal progression of the stages of puberty The initiation of the process is simply delayed 52 Group A
Managment • Treatment is based on the etiology of the delay. In cases of gonadal dysgenesis when a Y chromosome or fragment of a Y chromosome is present , the gonads should be removed at diagnosis because of the risk of neoplastic degeneration. Otherwise , hormone replacement with estrogen and subsequently both estrogen and progesterone , is required to promote sexual development and menarache. 53 Group A
Special problems of the adolescent • A. Dysmenorrhea : Dysmenorrhea is defined as cramp –like pain in the lower abdomen associated with menstrual flow. 54 Group A
Etiology • Primary dysmenorrhea accounts for most cases and is attributed to increased prostaglandin production with menses in the presence of normal anatomy. • Secondary dysmenorrhea results from conditions such as endometriosis and anomalies with obstruction in a portion of the outflow tract which leads to pain in the obstructed segment but menstrual flow is not affected. • Examples include obstructed hemiuterus and uterus didelphys with obstructed hemivagina 55 Group A

Clinical picture • Sever , cyclic , cramp-like pain located in the lower abdomen and pelvis is associated with menses • Pain may radiate to the thighs and back and be accompanied by nausea , vomiting , and diarrhea 56 Group A
![Managment Firstline therapy is prostaglandin inhibitors nonsteroidal antiinflammatory drugs NSAIDs If the Managment • First-line therapy is prostaglandin inhibitors (nonsteroidal anti-inflammatory drugs [NSAIDs] • If the](https://slidetodoc.com/presentation_image_h2/09b84b77bbc46a3a08c877a58d4630af/image-57.jpg)
Managment • First-line therapy is prostaglandin inhibitors (nonsteroidal anti-inflammatory drugs [NSAIDs] • If the symptoms are not adequately : start oral contraceptives or obtain a pelvic ultrasound to evaluate for abnormal anatomy depending on the loction, progression, andseverityofthesymptoms • Laparoscopyisrecommended if medical treatment fails to control the symptoms. 57 Group A
B. Dysfunctional uterine bleeding • DUB is defined as excessive , prolonged , or irregular bleeding not associated with an anatomic lesion. • Most adolescent girls have anovulatory menstrual periods for the first 2 to 3 years following menarche. 58 Group A
Etiology • The cause of DUBin 75% of cases is an immature hypothalamic –pitutary axis resulting in anovulation • Other cases include psychogenic factors , juvenile hypothyrodism and coagulation disorders (von willebrand disease ) 59 Group A
Clinical picture • Menometrorrhagia ( irregular , heavy bleeding) is the most characteristic symptom. • Bleeding can be prolonged and heavy in some cases leadng to sever anemia. • The condition is usually self – limited • Management Cyclic hormonal manipulation with progestins or comined oral contrceptive pills. 60 Group A
Thank You 61 Group A
 Supervisor qualification herbalife
Supervisor qualification herbalife Shoroug ayman
Shoroug ayman Ayman bukhari
Ayman bukhari Introduction to obstetrics
Introduction to obstetrics Obstetrics and gynecology lecture notes ppt
Obstetrics and gynecology lecture notes ppt Ninewells hospital outpatients area 3
Ninewells hospital outpatients area 3 Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Colp medical term
Colp medical term Gynecology
Gynecology Adolescent egocentrism
Adolescent egocentrism Example of fast mapping
Example of fast mapping Challenge of middle and late adolescence
Challenge of middle and late adolescence Eating a balanced diet during childhood and adolescence
Eating a balanced diet during childhood and adolescence The developing person through childhood and adolescence
The developing person through childhood and adolescence Middle childhood and adolescence
Middle childhood and adolescence Jeffrey arnett emerging adulthood theory
Jeffrey arnett emerging adulthood theory The developing person through childhood and adolescence
The developing person through childhood and adolescence Managersafety u.com
Managersafety u.com Practice assessor and practice supervisor
Practice assessor and practice supervisor Dating serves several important functions that include:
Dating serves several important functions that include: Adolescence vocabulary
Adolescence vocabulary Chapter 6 the adolescent in society
Chapter 6 the adolescent in society Adolescence
Adolescence Brain development adolescence
Brain development adolescence Dominant values
Dominant values Moral development in adolescence
Moral development in adolescence Middle adolescence physical development
Middle adolescence physical development Objectives of adolescence education
Objectives of adolescence education Industry versus inferiority
Industry versus inferiority Adolescense period
Adolescense period Suicide cuts across all social categories
Suicide cuts across all social categories Adolescence in our society
Adolescence in our society Psychosocial development in adolescence
Psychosocial development in adolescence Physical development
Physical development Erikson's stage of adolescence
Erikson's stage of adolescence Adolescence sociology definition
Adolescence sociology definition ________ is a self-portrait composed of many pieces.
________ is a self-portrait composed of many pieces. Personal fable ap psychology
Personal fable ap psychology Adolescence
Adolescence Les avantages de l'adolescence
Les avantages de l'adolescence Vocabulary activity 4-2 personal development
Vocabulary activity 4-2 personal development Social changes in adolescence
Social changes in adolescence Chapter 4 adolescence psychology
Chapter 4 adolescence psychology Caloub
Caloub Infancy childhood adolescence adulthood old age
Infancy childhood adolescence adulthood old age Critical thinking in adolescence
Critical thinking in adolescence Adolescence
Adolescence Youtube youtube
Youtube youtube Needs of adolescence
Needs of adolescence Moral development in adolescence
Moral development in adolescence Emotional development in adolescence
Emotional development in adolescence 5 characteristics of adolescence
5 characteristics of adolescence Chapter 4 adolescence psychology
Chapter 4 adolescence psychology Herbalife 90 day plan
Herbalife 90 day plan Housekeeping feladata
Housekeeping feladata Principle of supervision
Principle of supervision Memorandum to supervisor
Memorandum to supervisor Penn performance management
Penn performance management What is the liaison role of a manager
What is the liaison role of a manager Taiwan water corporation
Taiwan water corporation Supervisor activo herbalife
Supervisor activo herbalife