Pediatric Airway Management Dave French MD NREMTP Attending



- Slides: 76

Pediatric Airway Management Dave French, MD, NREMT-P Attending ED Physician, Albany Medical Center Medical Director, Albany & Schenectady Fire Departments
Goals Decision-making l Basics l Intubation l Rescue devices l Medications l Ventilators l Broselow l
Decision-making What do I need to accomplish (why ETT)? l How aggressive should I be (BLS vs. ALS)? l What is my back-up plan? l What is the long-term picture? l
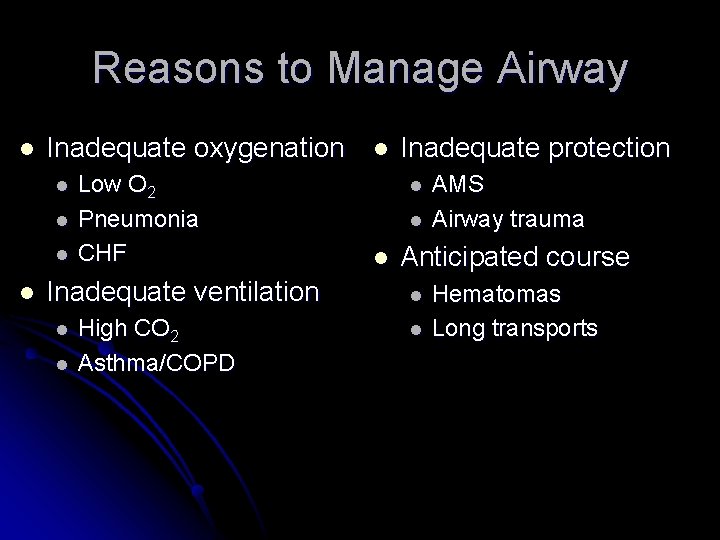
Reasons to Manage Airway l Inadequate oxygenation l l Low O 2 Pneumonia CHF Inadequate ventilation l l High CO 2 Asthma/COPD l Inadequate protection l l l AMS Airway trauma Anticipated course l l Hematomas Long transports
BLS vs. ALS We think intubation is easy l We are not good at it l l Prehospital success rate as low as 70% We can manage many patients with BLS l RSI can kill people l
Who Should Be Intubated? l AHA recommends prehospital intubation l l AAP developed PEPP course l l De-emphasized under new ACLS/PALS guidelines Teaches intubation but not the focus What does the literature say?
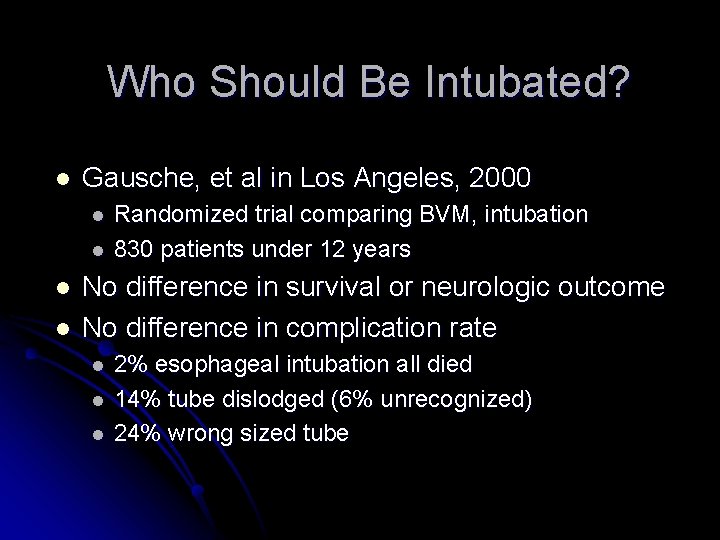
Who Should Be Intubated? l Gausche, et al in Los Angeles, 2000 l l Randomized trial comparing BVM, intubation 830 patients under 12 years No difference in survival or neurologic outcome No difference in complication rate l l l 2% esophageal intubation all died 14% tube dislodged (6% unrecognized) 24% wrong sized tube
Should we be intubating ANY pediatric patients? !? ! Jury is still out, but some states already forbid it.
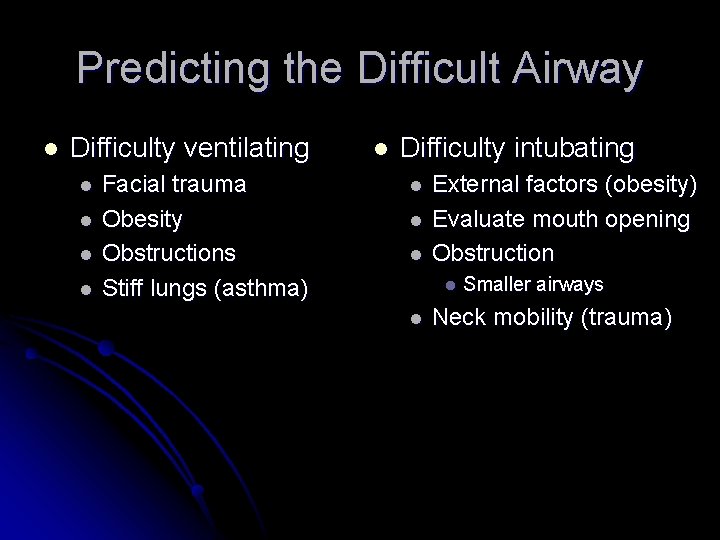
Predicting the Difficult Airway l Difficulty ventilating l l Facial trauma Obesity Obstructions Stiff lungs (asthma) l Difficulty intubating l l l External factors (obesity) Evaluate mouth opening Obstruction l l Smaller airways Neck mobility (trauma)
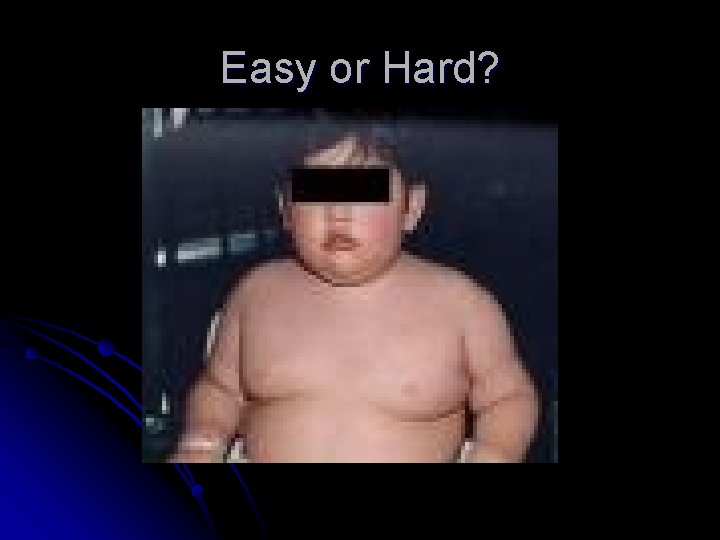
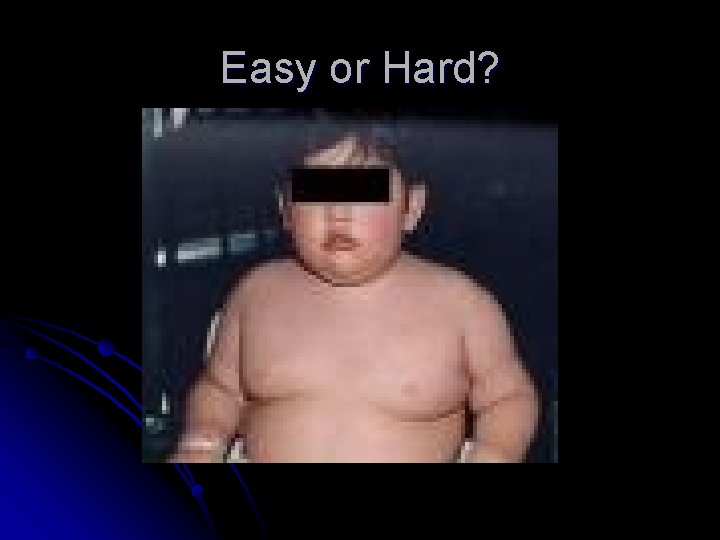
Easy or Hard?
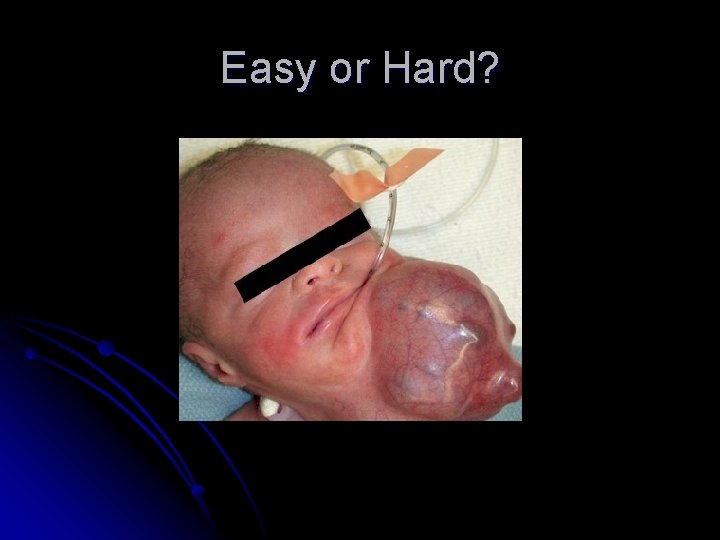
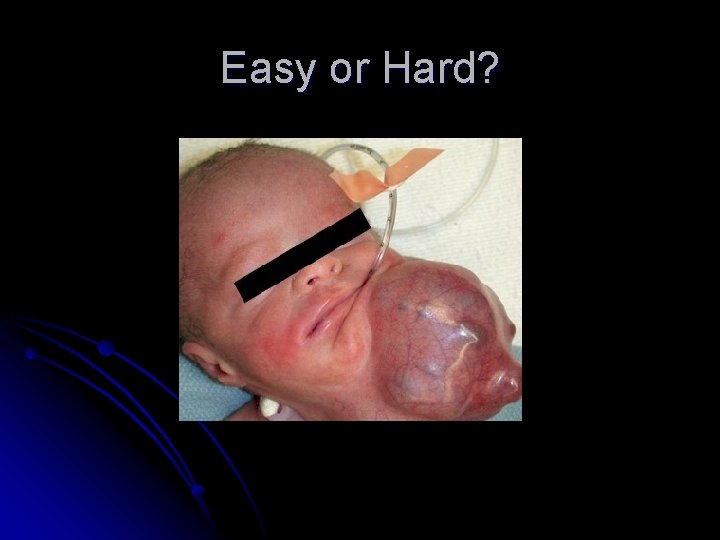
Easy or Hard?
Easy or Hard?
The Debate on Prehospital Pediatric Intubation Continues…
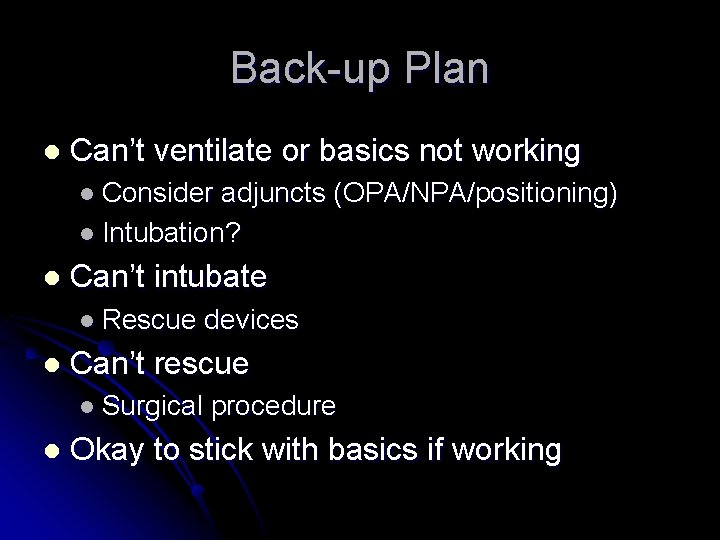
Back-up Plan l Can’t ventilate or basics not working l Consider adjuncts (OPA/NPA/positioning) l Intubation? l Can’t intubate l Rescue l Can’t rescue l Surgical l devices procedure Okay to stick with basics if working
It’s Not Okay to Continue with Failed Techniques
Long-Term Issues l Securing the tube l Tape vs. ties l Commercial devices l Restraints
Long-Term Issues l Sedation l Agent and administration (drip vs. bolus) l Paralytics? Ventilator management l What if the tube comes out? l
Basics Positioning l Adjuncts l l OPA - good choice if tolerated l NPA - easy to tear mucosa l Effective BVM use is most important skill l Get a good seal (two person better) l Don’t over ventilate l Don’t forget the suction
Intubation Preparation l Preoxygenate l Monitors - ECG, pulse ox l Sellick’s l Good l basics Equipment selection l Miller vs. Mac l Cuffed vs. uncuffed l ETT size l Positioning
Airway Equipment l Straight blade to age 4? l Better able to control epiglottis? l Choose for comfort l Smaller tubes l Less stability l More resistance l Uncuffed tubes < 8 years of age
Airway Equipment Suction l Magill forceps l Stylet l Tube check and securing devices l
Tube Size l ETT size (Age in years/4) + 4 l Diameter of nare l Diameter of pinky l Broselow tape l Have one size smaller and larger l
Tube Placement l ETT depth – use the black line (Age in years/2) + 12 l ETT internal diameter x 3 l
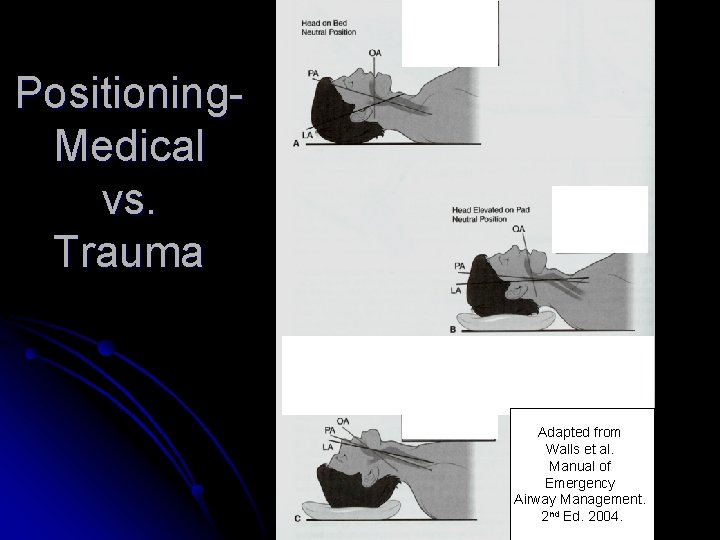
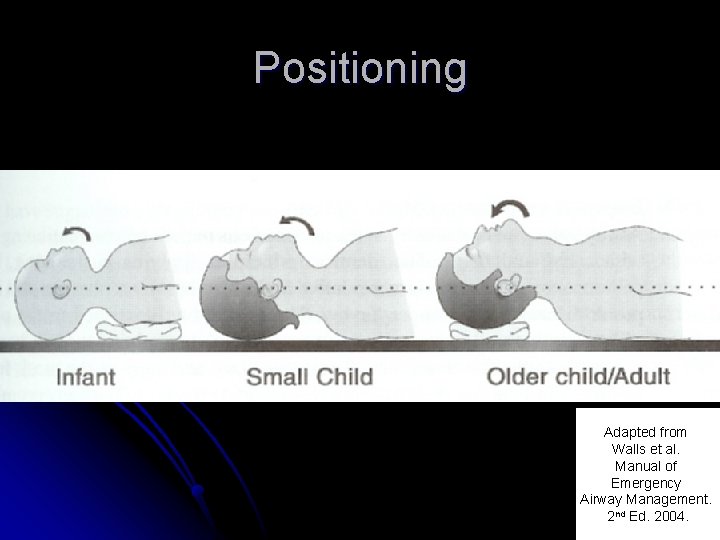
Intubation Positioning l Goal is to align three axes l OA/PA/LA l Medical positioning l Head tilt chin lift l Towels (older = head, younger = shoulders) l Trauma positioning l Manual in-line stabilization
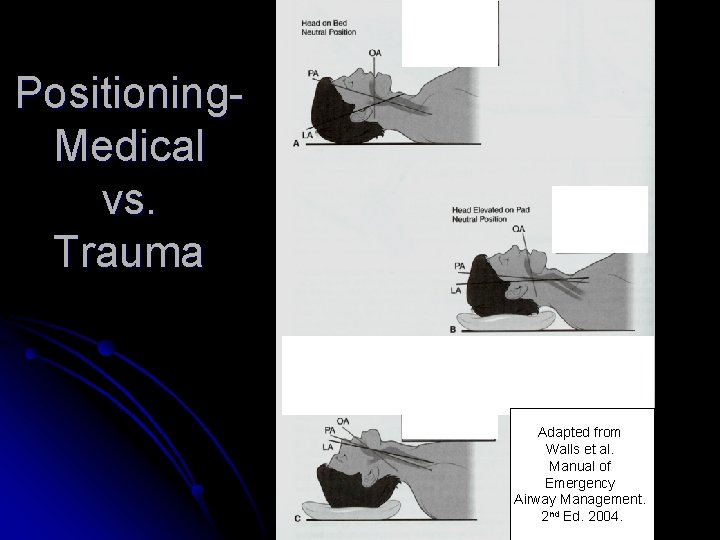
Positioning. Medical vs. Trauma Adapted from Walls et al. Manual of Emergency Airway Management. 2 nd Ed. 2004.
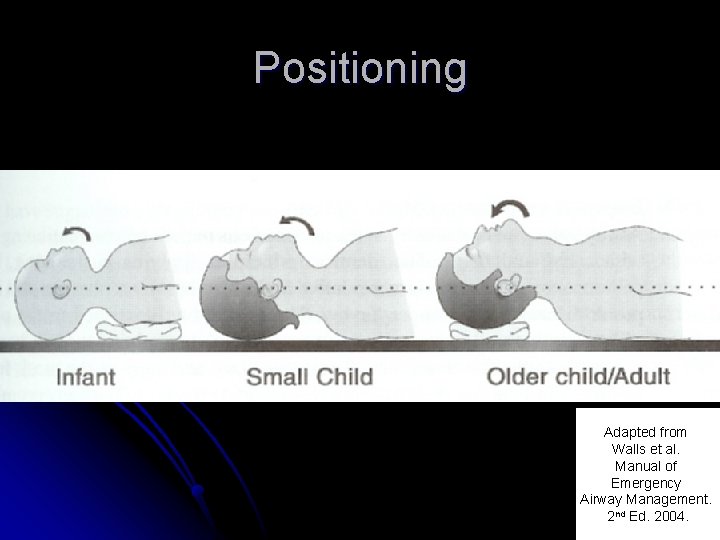
Positioning Adapted from Walls et al. Manual of Emergency Airway Management. 2 nd Ed. 2004.
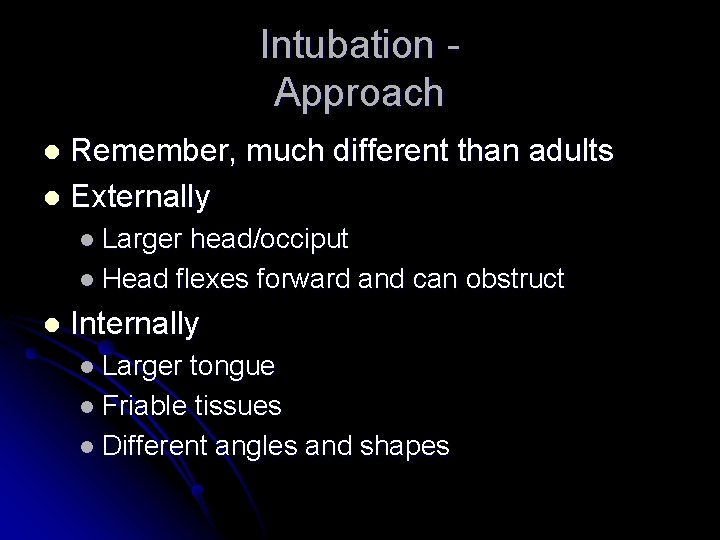
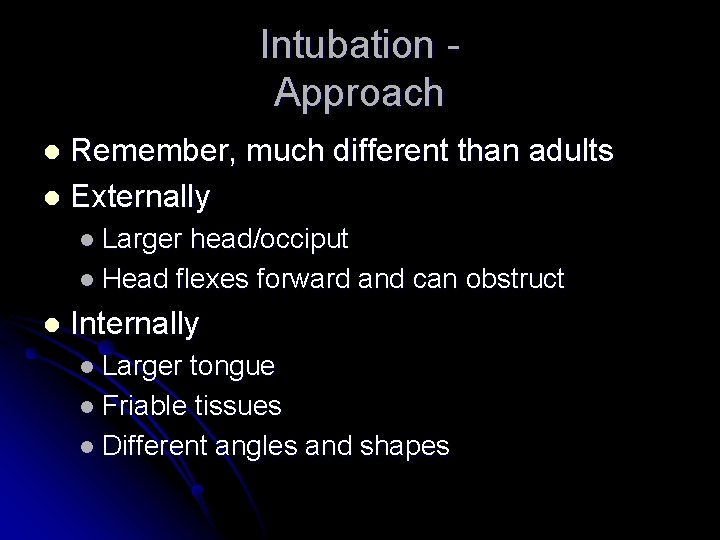
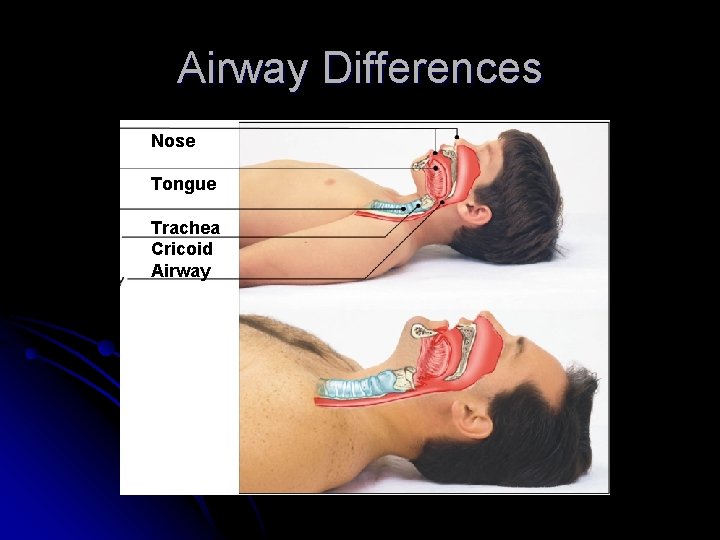
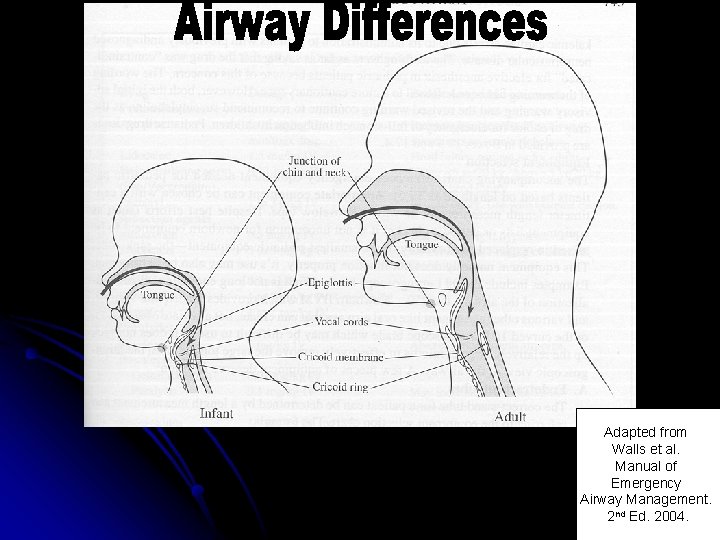
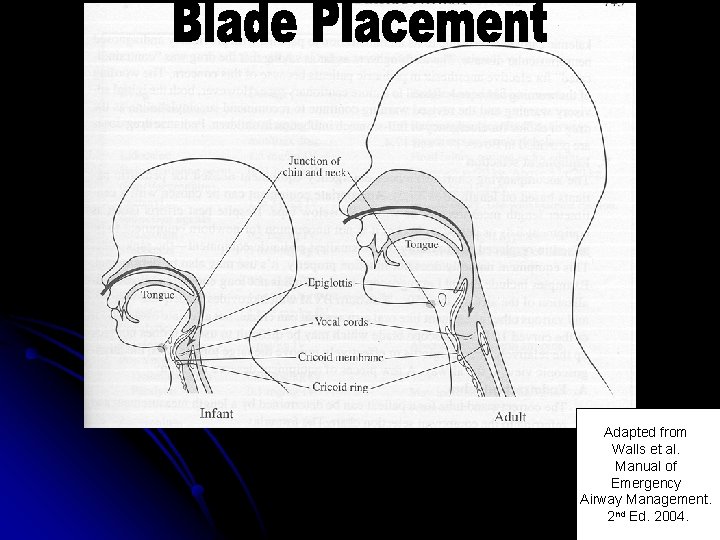
Intubation Approach Remember, much different than adults l Externally l l Larger head/occiput l Head flexes forward and can obstruct l Internally l Larger tongue l Friable tissues l Different angles and shapes
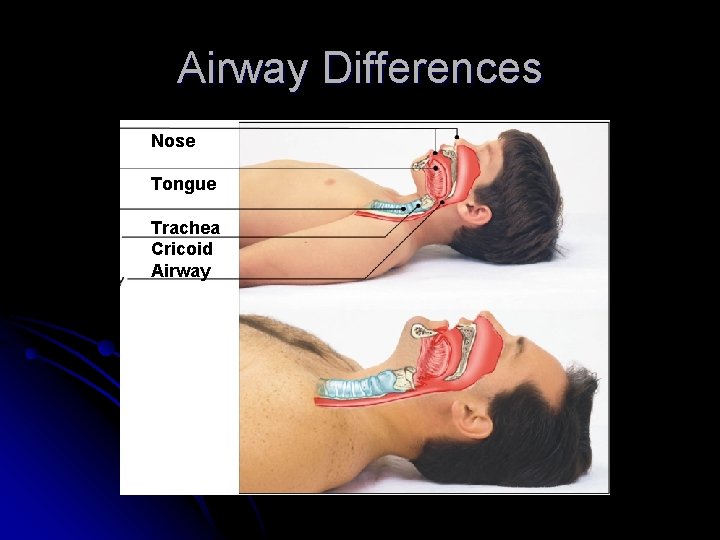
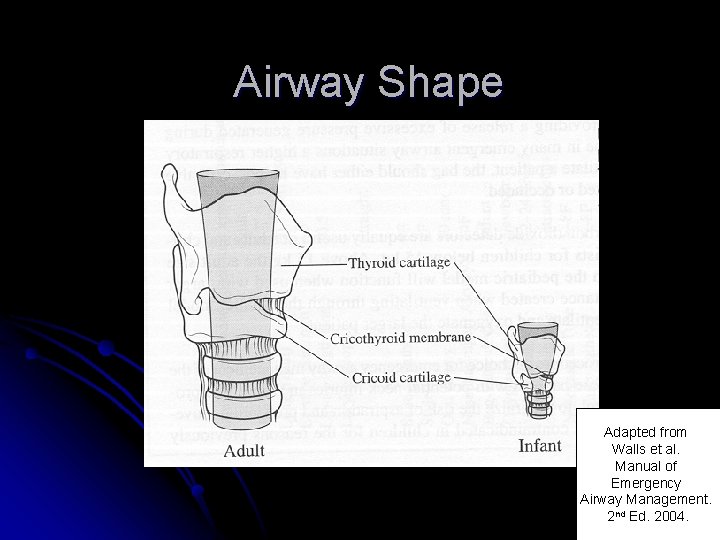
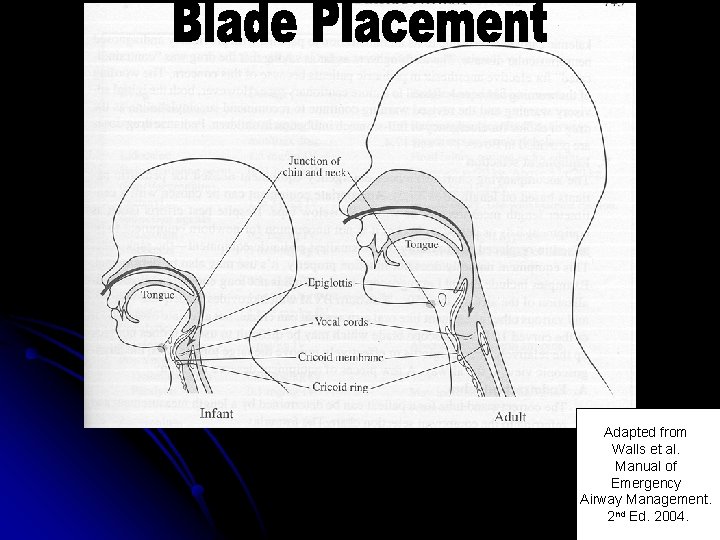
Airway Differences Nose Tongue Trachea Cricoid Airway
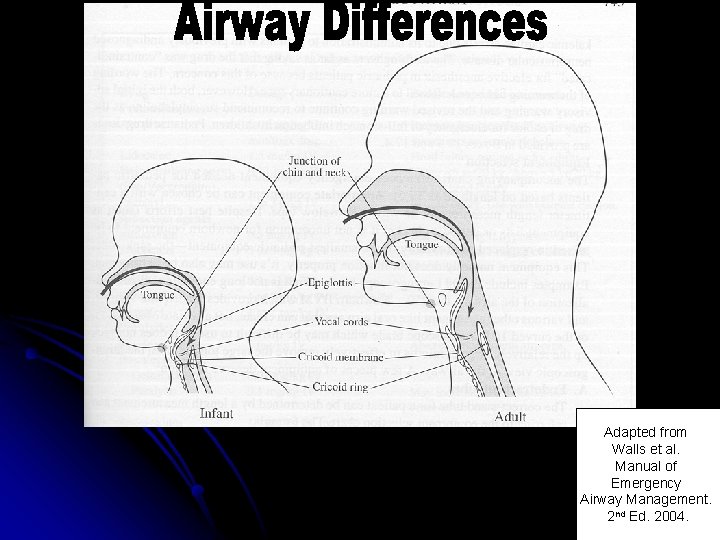
Adapted from Walls et al. Manual of Emergency Airway Management. 2 nd Ed. 2004.
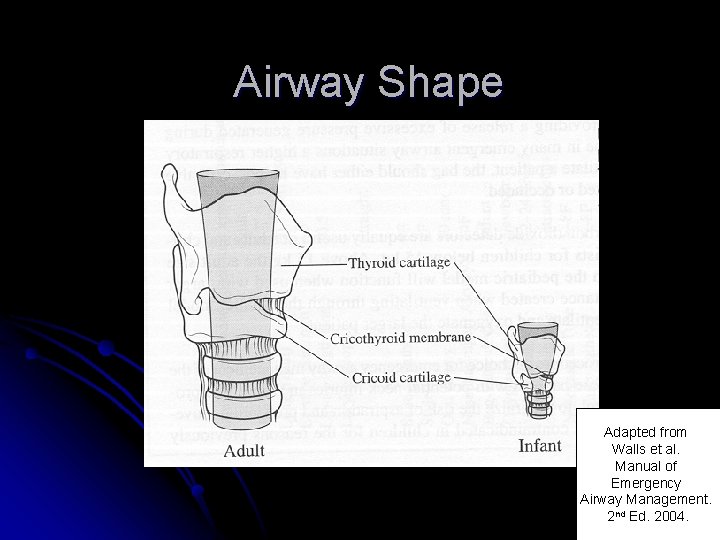
Airway Shape Adapted from Walls et al. Manual of Emergency Airway Management. 2 nd Ed. 2004.
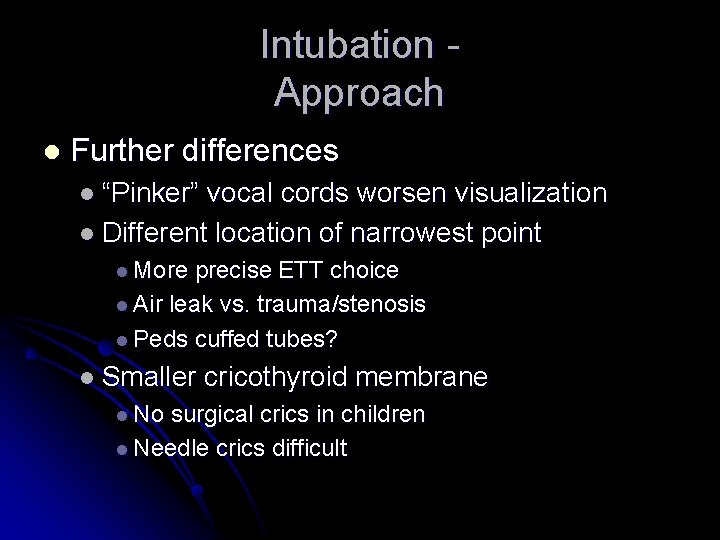
Intubation Approach l Further differences l “Pinker” vocal cords worsen visualization l Different location of narrowest point l More precise ETT choice l Air leak vs. trauma/stenosis l Peds cuffed tubes? l Smaller l No cricothyroid membrane surgical crics in children l Needle crics difficult
Other Considerations More gastric insufflation with BVM l Different oxygenation abilities l l Higher basal usage l Less residual lung capacity l Quicker desats during intubation l 10 l kg to 90% in <4 minutes (vs. 8 for adult) More likely to have vagal response
Intubation Techniques Always enter from the right corner l Tongue control is critical l Lift the epiglottis with the Miller l Slide the Mac into the vallecula l l Can lift the epiglottis if needed
Adapted from Walls et al. Manual of Emergency Airway Management. 2 nd Ed. 2004.
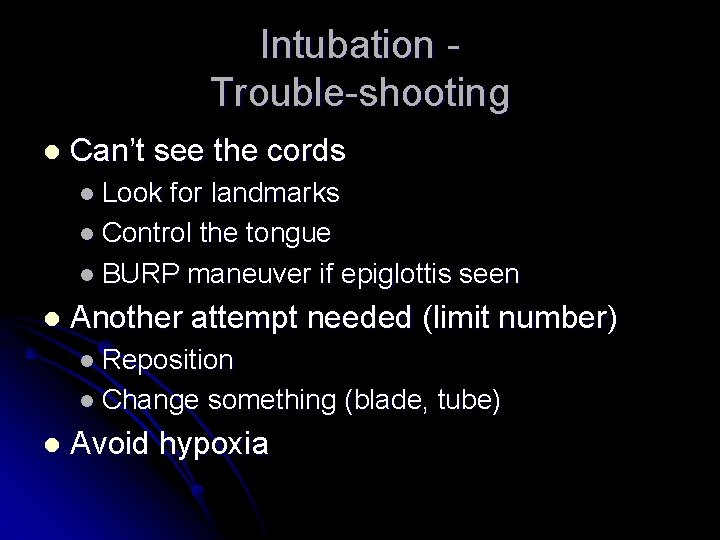
Intubation Trouble-shooting l Can’t see the cords l Look for landmarks l Control the tongue l BURP maneuver if epiglottis seen l Another attempt needed (limit number) l Reposition l Change l something (blade, tube) Avoid hypoxia
Blind Techniques Exist but need practice for proficiency l Digital intubation l l Small l work area Blind nasotracheal intubation l Tough angles for tube placement l Remember anatomic differences l Contraindicated until >10 years old
In general, blind techniques not useful in children
Intubation Confirmation Visualize tube passing through cords l Breath sounds and epigastric sounds l End Tidal CO 2 (ETCO 2) l Commercial devices l l Not effective on uncuffed tubes l Be careful if used in children
REMINDER: It’s Not Okay to Continue with Failed Techniques
Rescue Devices LMAs (laryngeal mask airway) l I-LMAs (intubating LMA) l Combitube l Bougie l Pick one or two and practice l l Need to be comfortable before crisis
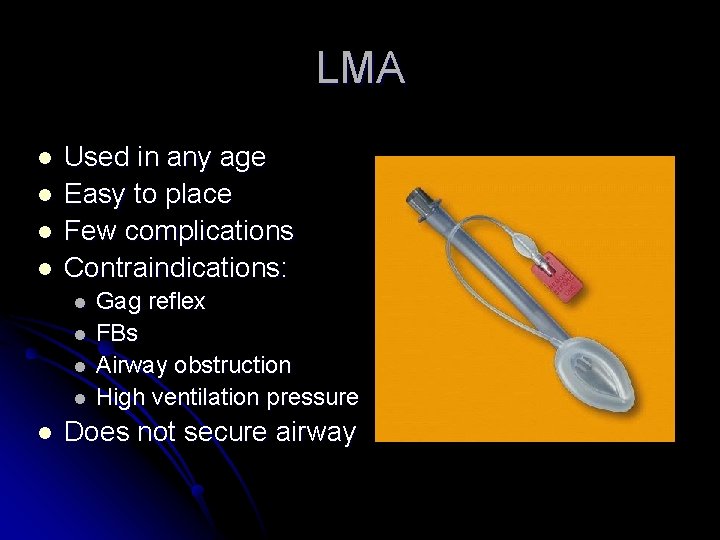
LMA l l Used in any age Easy to place Few complications Contraindications: l l l Gag reflex FBs Airway obstruction High ventilation pressure Does not secure airway
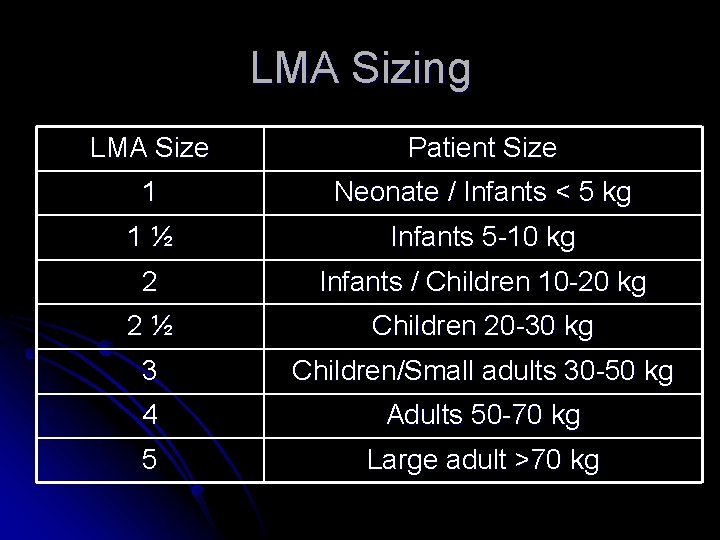
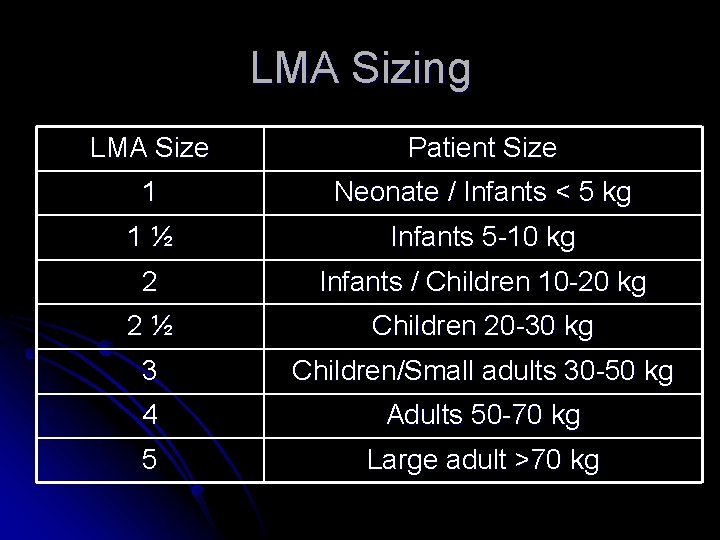
LMA Sizing LMA Size Patient Size 1 Neonate / Infants < 5 kg 1½ Infants 5 -10 kg 2 Infants / Children 10 -20 kg 2½ Children 20 -30 kg 3 Children/Small adults 30 -50 kg 4 Adults 50 -70 kg 5 Large adult >70 kg

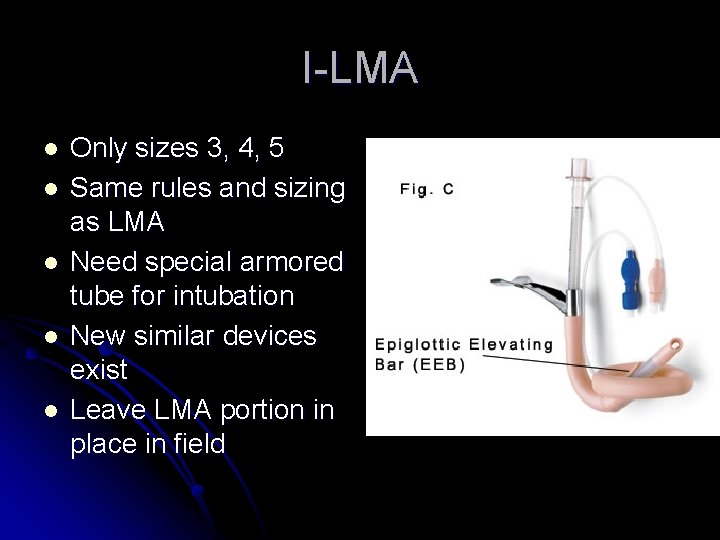
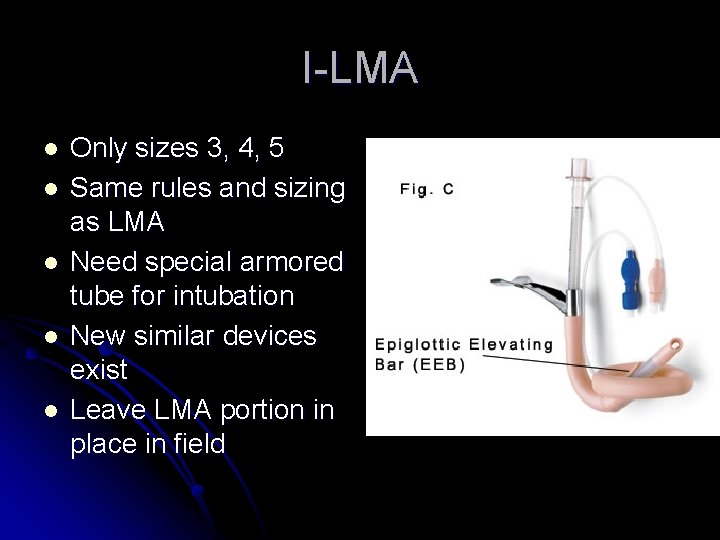
I-LMA l l l Only sizes 3, 4, 5 Same rules and sizing as LMA Need special armored tube for intubation New similar devices exist Leave LMA portion in place in field
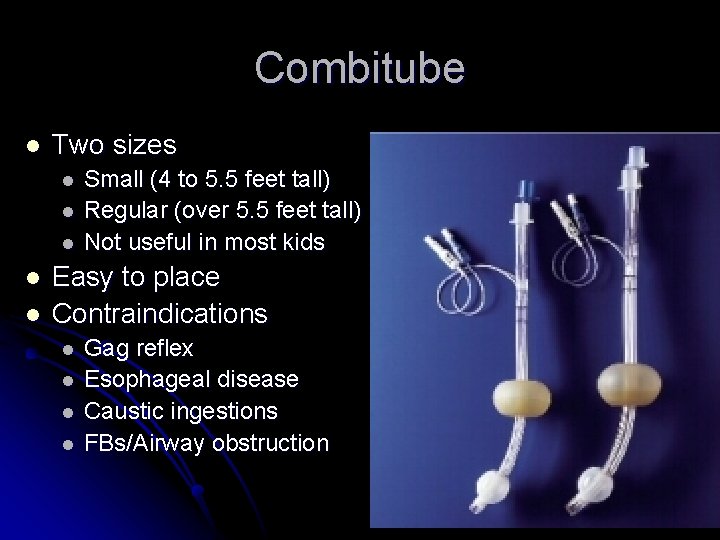
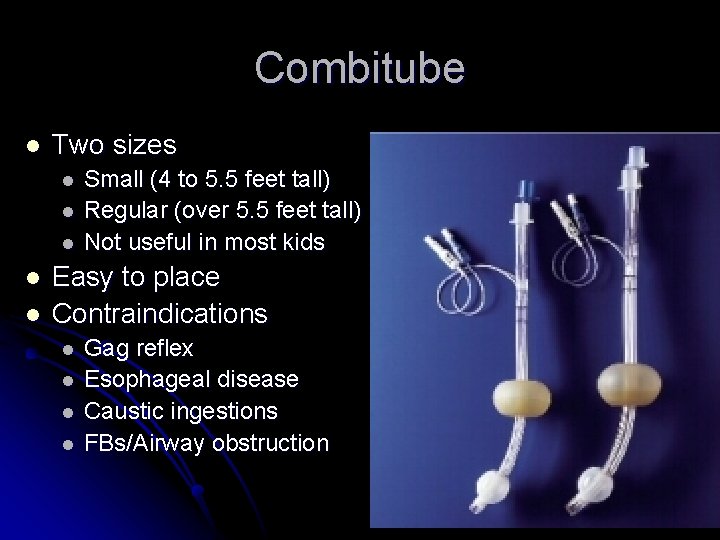
Combitube l Two sizes l l l Small (4 to 5. 5 feet tall) Regular (over 5. 5 feet tall) Not useful in most kids Easy to place Contraindications l l Gag reflex Esophageal disease Caustic ingestions FBs/Airway obstruction
Bougie l l Replaces stylet Able to use with poor view l l l Intubate over it l l l Feel tracheal rings Feel carina Keep blade in place Two person technique Need to practice
Other Toys l l l Lighted stylet Flexible fiberoptic scopes Rigid fiberoptic scopes l l l Bullard Shikani Video laryngoscopy
Surgical Airways Cricothyrotomy l Indications (only if >10 years old) l Failed airway l Failed ventilation l Predictors of difficulty l Previous neck surgery l Obesity l Hematoma or infection
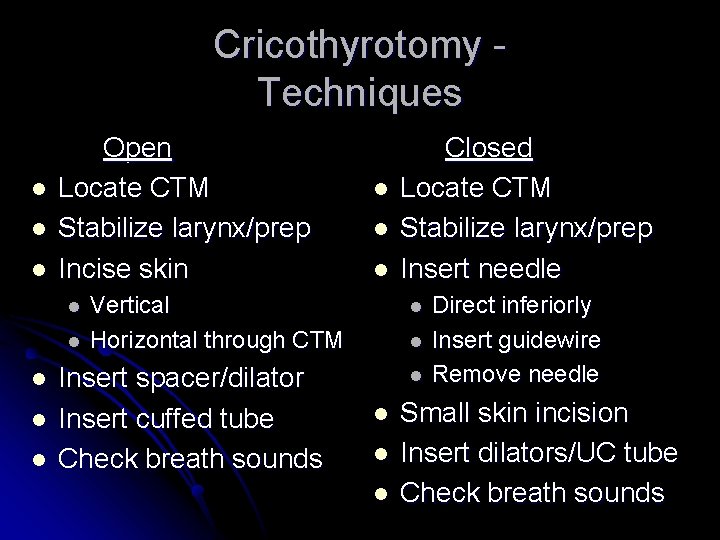
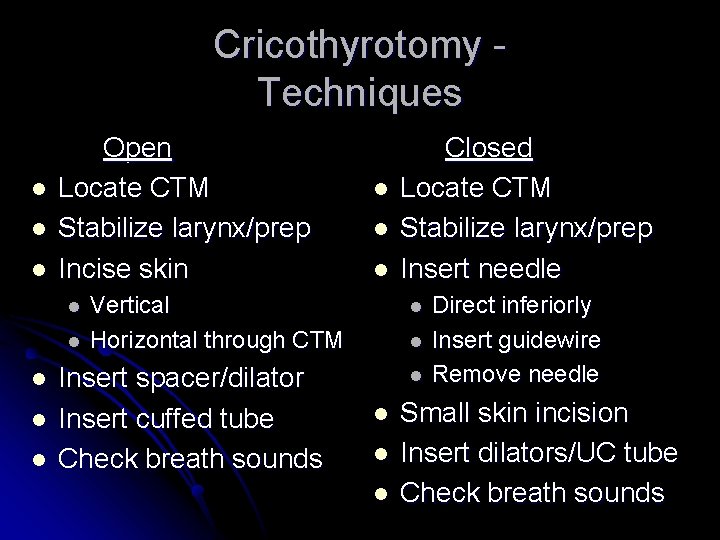
Cricothyrotomy Techniques l l l Open Locate CTM Stabilize larynx/prep Incise skin l l l l Vertical Horizontal through CTM Insert spacer/dilator Insert cuffed tube Check breath sounds Closed Locate CTM Stabilize larynx/prep Insert needle l l l Direct inferiorly Insert guidewire Remove needle Small skin incision Insert dilators/UC tube Check breath sounds
Cricothyrotomy Complications Bleeding l Laryngeal or tracheal injury l Infection l Pneumomediastinum l Subglottic stenosis l
Surgical Airways Needle Cric Same indications (all ages, tougher if young) l Must use with TTJV (jet ventilator) l l Cannot l use with superior airway obstruction Similarly difficult patients
Needle Cricothyrotomy Procedure Identify CTM and stabilize/prep larynx l Insert needle on syringe, direct inferiorly l l Large bore needle (12 -16 gauge) l Catheter over needle Advance catheter l Connect to TTJV (BVM for infants - 3. 0 ETT) l l Oxygen pressure (20 -30 psi) l 1 second on/2 -3 seconds off
Needle Cricothyrotomy Complications l Similar complications to other crics l Pneumothorax/subcutaneous l Barotrauma l Esophageal l Obstruction injury emphysema

TTJV
What About RSI?
Rapid Sequence Intubation Does increase intubation success l You stop intrinsic breathing l l You l can kill them Little place for peds in prehospital setting
RSI Medications l Same as adults l Lidocaine l Etomidate l Succinylcholine l Vecuronium Remember atropine l Consider ketamine l
Pretreatment Lidocaine Mechanism: Decrease ICP, bronchospasm l Indications: Asthma, head injury l Contraindications: Allergy l Dosage: 1. 5 mg/kg 3 minutes before ETT l
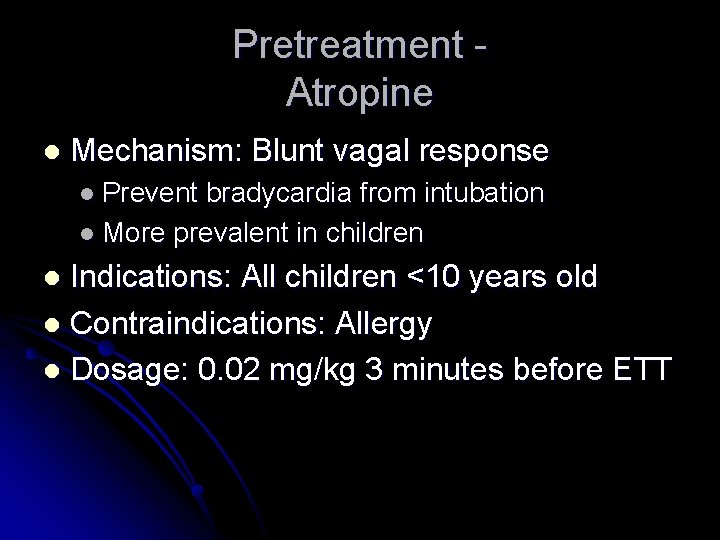
Pretreatment Atropine l Mechanism: Blunt vagal response l Prevent bradycardia from intubation l More prevalent in children Indications: All children <10 years old l Contraindications: Allergy l Dosage: 0. 02 mg/kg 3 minutes before ETT l
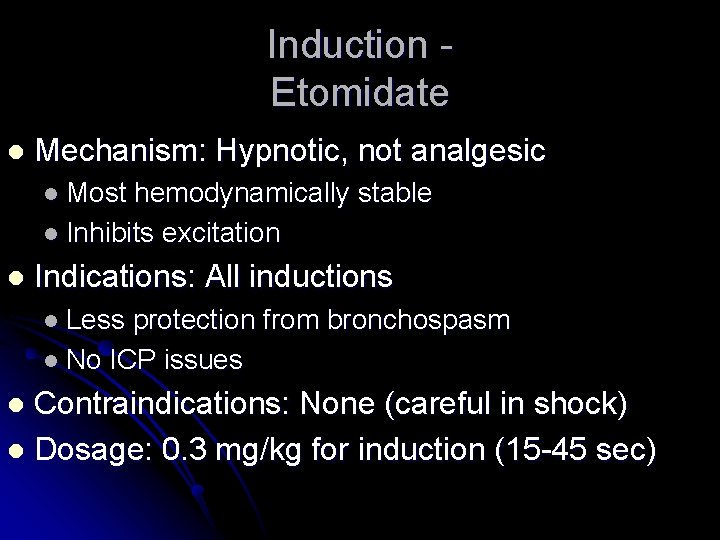
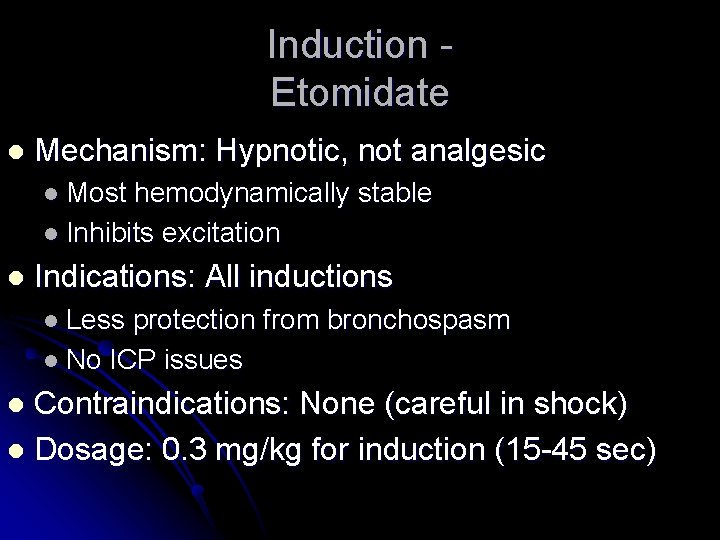
Induction Etomidate l Mechanism: Hypnotic, not analgesic l Most hemodynamically stable l Inhibits excitation l Indications: All inductions l Less protection from bronchospasm l No ICP issues Contraindications: None (careful in shock) l Dosage: 0. 3 mg/kg for induction (15 -45 sec) l
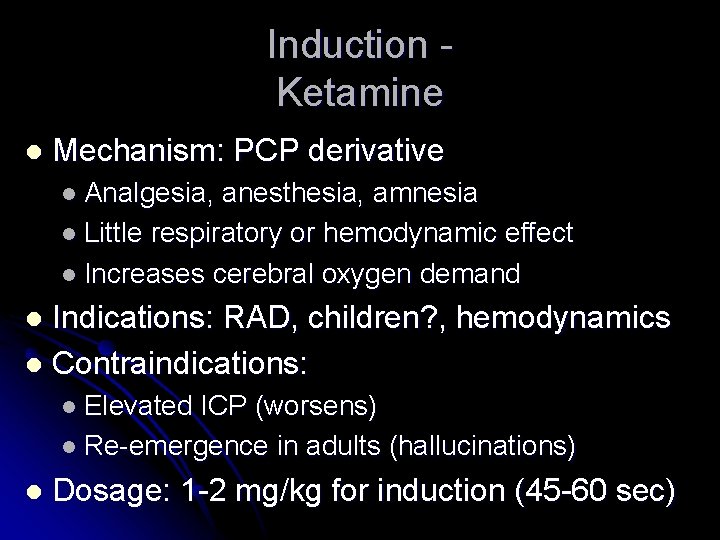
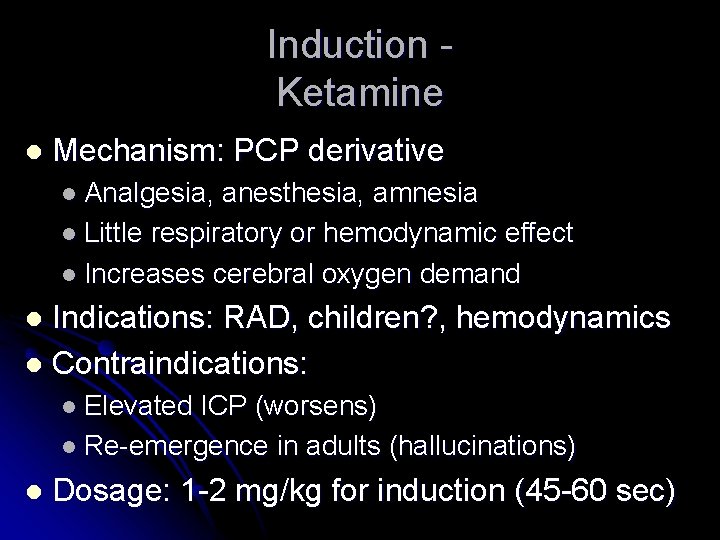
Induction Ketamine l Mechanism: PCP derivative l Analgesia, anesthesia, amnesia l Little respiratory or hemodynamic effect l Increases cerebral oxygen demand Indications: RAD, children? , hemodynamics l Contraindications: l l Elevated ICP (worsens) l Re-emergence in adults (hallucinations) l Dosage: 1 -2 mg/kg for induction (45 -60 sec)
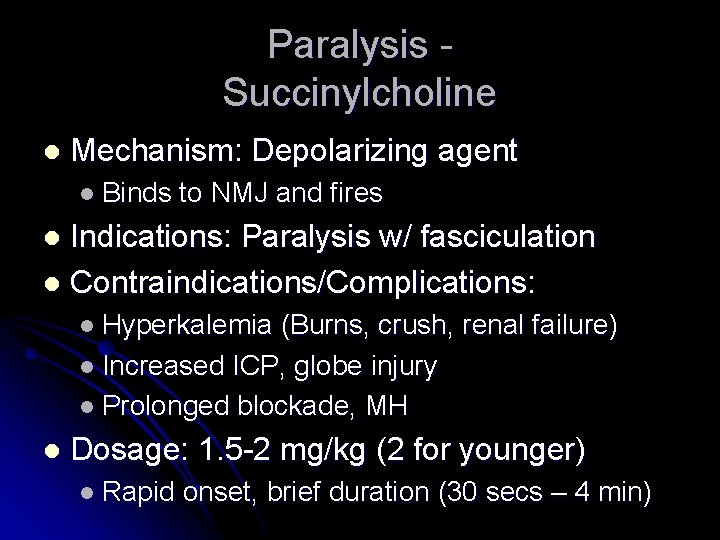
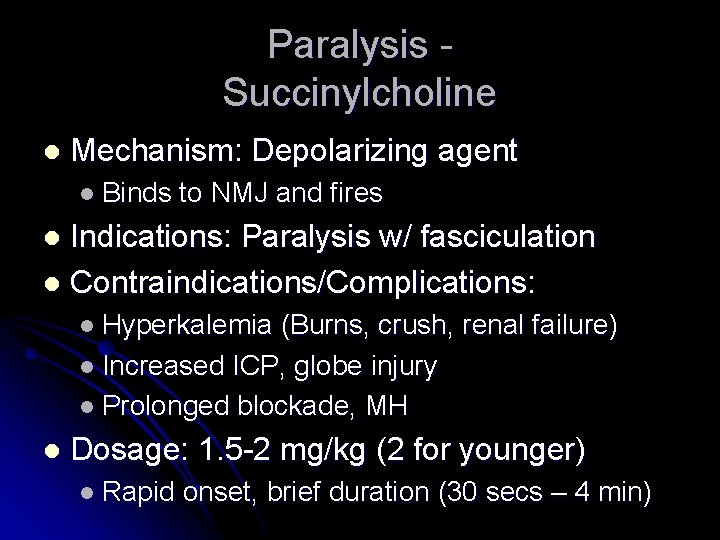
Paralysis Succinylcholine l Mechanism: Depolarizing agent l Binds to NMJ and fires Indications: Paralysis w/ fasciculation l Contraindications/Complications: l l Hyperkalemia (Burns, crush, renal failure) l Increased ICP, globe injury l Prolonged blockade, MH l Dosage: 1. 5 -2 mg/kg (2 for younger) l Rapid onset, brief duration (30 secs – 4 min)
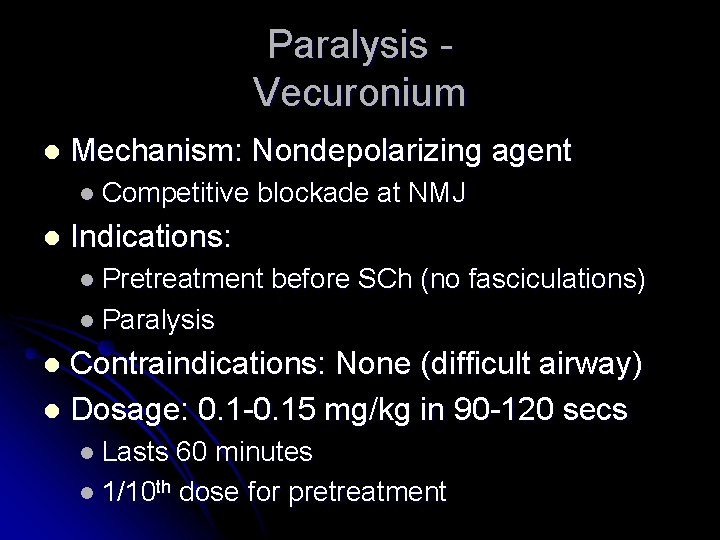
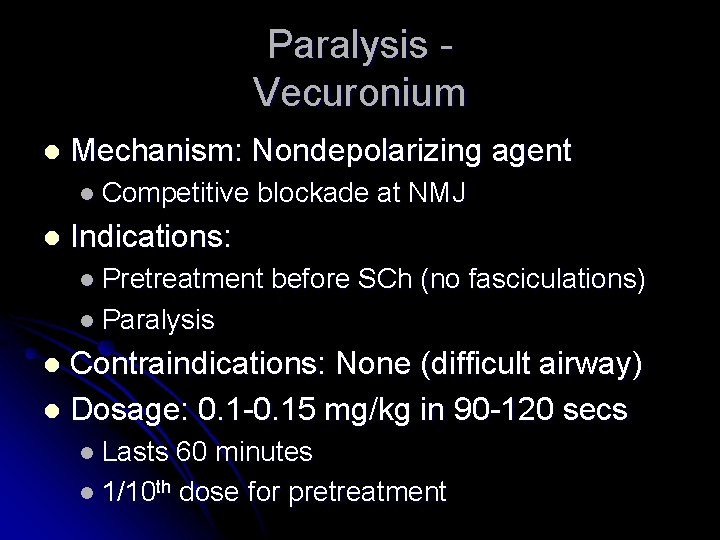
Paralysis Vecuronium l Mechanism: Nondepolarizing agent l Competitive l blockade at NMJ Indications: l Pretreatment before SCh (no fasciculations) l Paralysis Contraindications: None (difficult airway) l Dosage: 0. 1 -0. 15 mg/kg in 90 -120 secs l l Lasts 60 minutes l 1/10 th dose for pretreatment
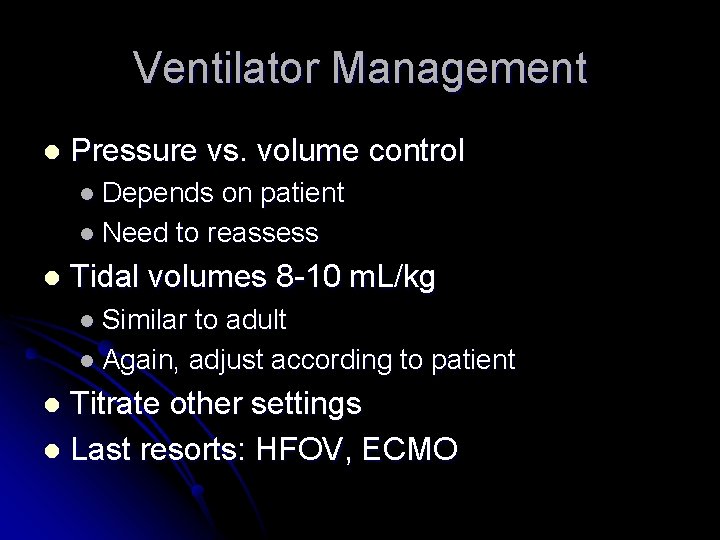
Ventilator Management l Pressure vs. volume control l Depends on patient l Need to reassess l Tidal volumes 8 -10 m. L/kg l Similar to adult l Again, adjust according to patient Titrate other settings l Last resorts: HFOV, ECMO l
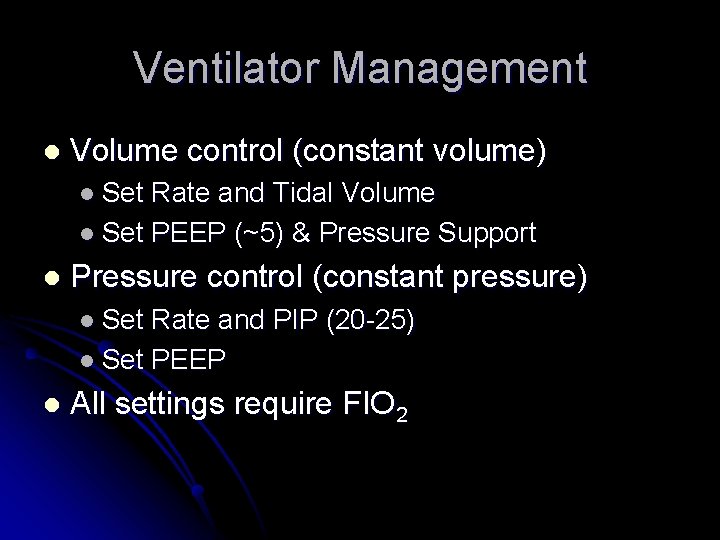
Ventilator Management l Volume control (constant volume) l Set Rate and Tidal Volume l Set PEEP (~5) & Pressure Support l Pressure control (constant pressure) l Set Rate and PIP (20 -25) l Set PEEP l All settings require FIO 2
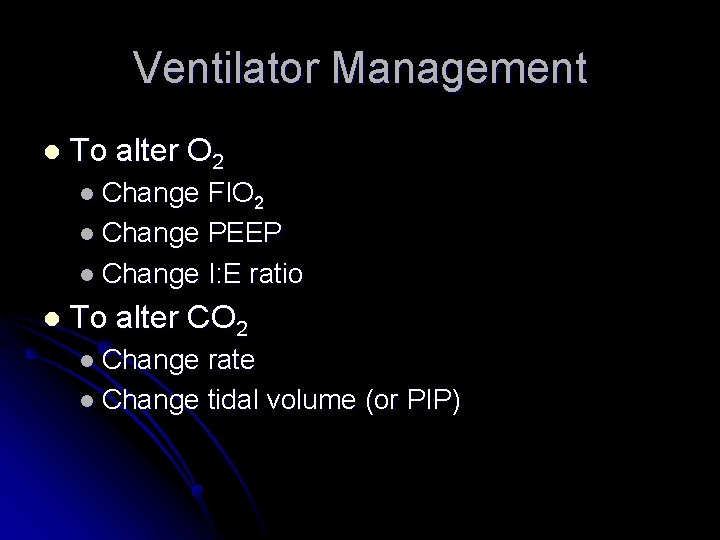
Ventilator Management l To alter O 2 l Change FIO 2 l Change PEEP l Change I: E ratio l To alter CO 2 l Change rate l Change tidal volume (or PIP)
Ventilator Management l CPAP and Bi. PAP l Not much use in younger children l Need to be able to comply with treatment l Good modalities in some settings l Rarely (if ever) useful in prehospital setting
Last but not least…
Broselow Tape l l Lubitz, et al. (1998) Most accurate 3. 5 - 25 kg More accurate than RN or MD 94% vs 63%
Broselow Tape l l Rowe, et al. (1998) Calculation error rate 3% Recheck increases to 10% Under stress, up to 25%
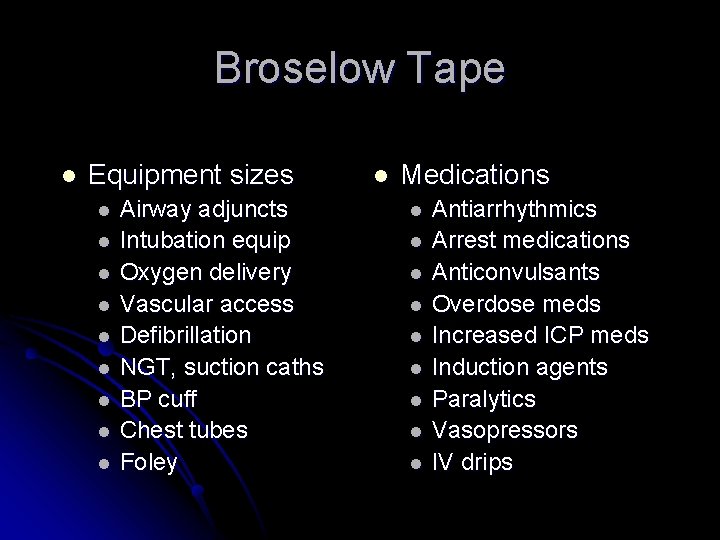
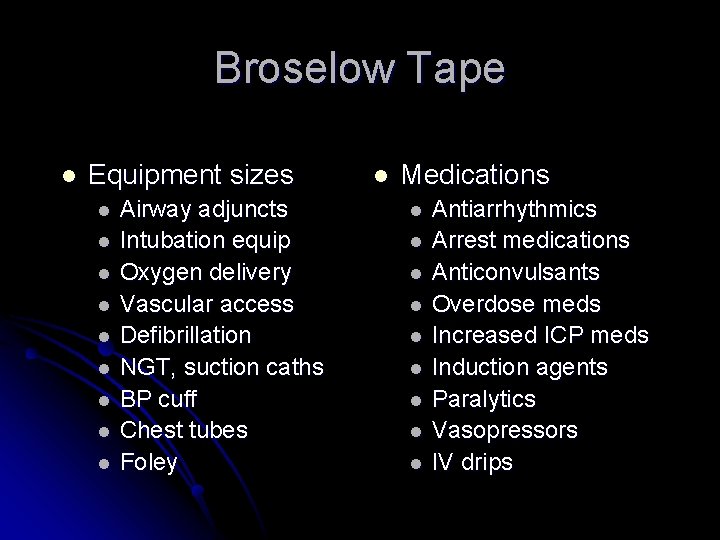
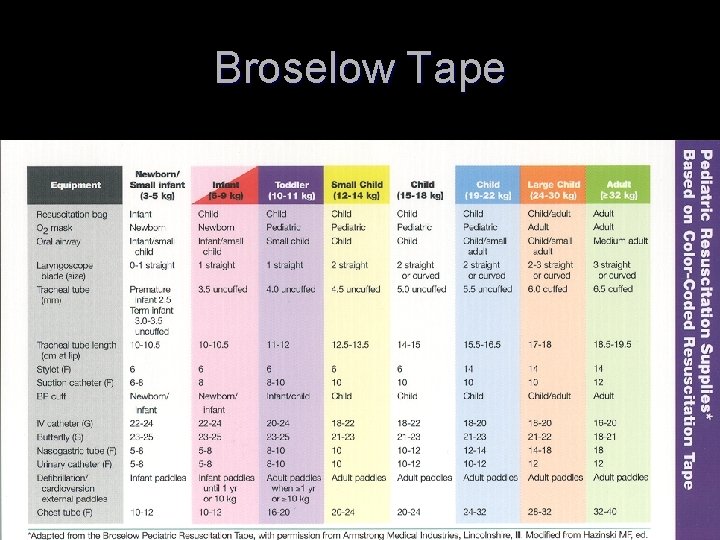
Broselow Tape l Equipment sizes l l l l l Airway adjuncts Intubation equip Oxygen delivery Vascular access Defibrillation NGT, suction caths BP cuff Chest tubes Foley l Medications l l l l l Antiarrhythmics Arrest medications Anticonvulsants Overdose meds Increased ICP meds Induction agents Paralytics Vasopressors IV drips
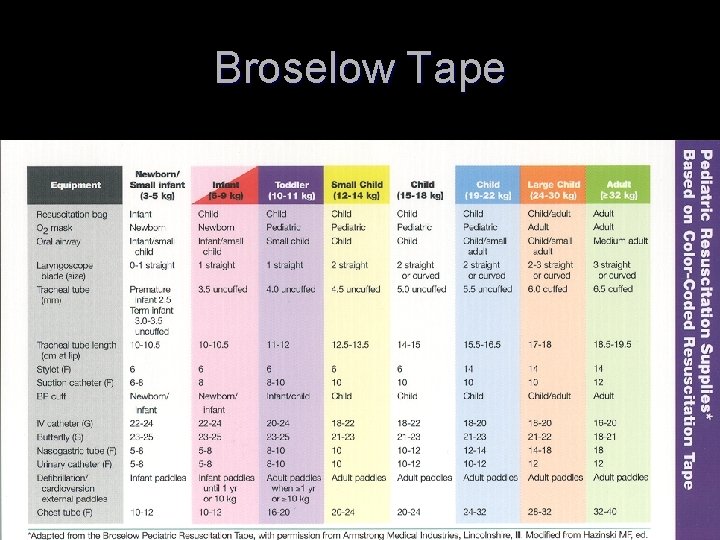
Broselow Tape
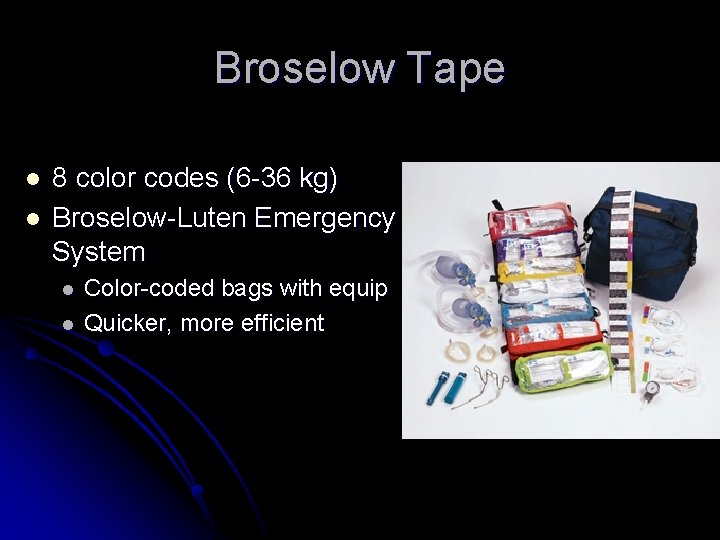
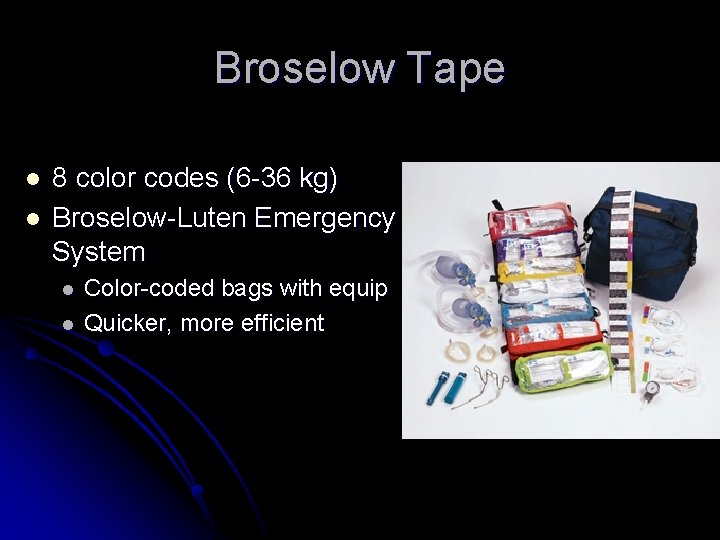
Broselow Tape l l 8 color codes (6 -36 kg) Broselow-Luten Emergency System l l Color-coded bags with equip Quicker, more efficient
Summary Think carefully about your goals l Assess your options l Good BLS is the most important skill l Intubate or not? l Have a back-up plan l Use your Broselow l
Questions?
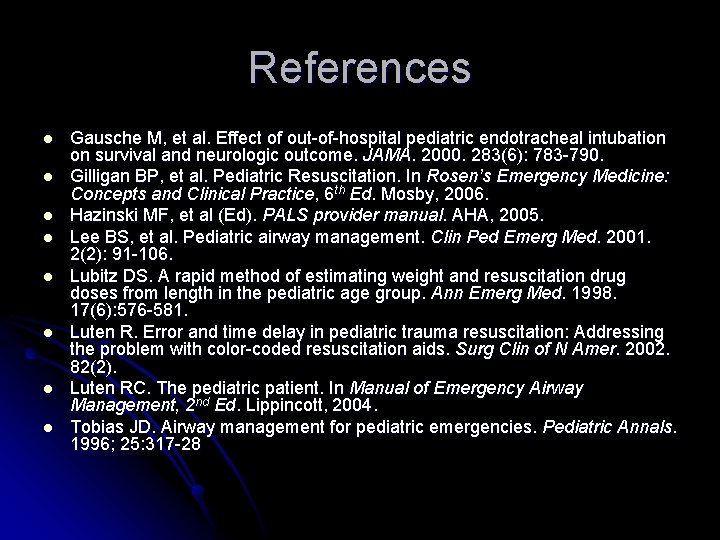
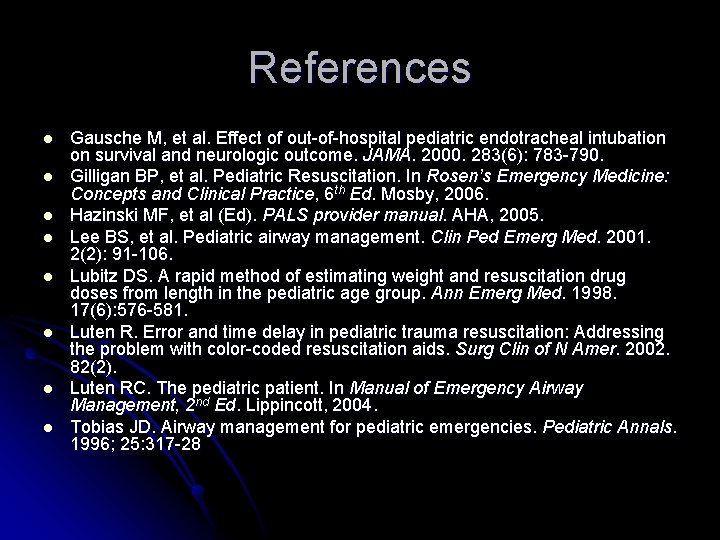
References l l l l Gausche M, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurologic outcome. JAMA. 2000. 283(6): 783 -790. Gilligan BP, et al. Pediatric Resuscitation. In Rosen’s Emergency Medicine: Concepts and Clinical Practice, 6 th Ed. Mosby, 2006. Hazinski MF, et al (Ed). PALS provider manual. AHA, 2005. Lee BS, et al. Pediatric airway management. Clin Ped Emerg Med. 2001. 2(2): 91 -106. Lubitz DS. A rapid method of estimating weight and resuscitation drug doses from length in the pediatric age group. Ann Emerg Med. 1998. 17(6): 576 -581. Luten R. Error and time delay in pediatric trauma resuscitation: Addressing the problem with color-coded resuscitation aids. Surg Clin of N Amer. 2002. 82(2). Luten RC. The pediatric patient. In Manual of Emergency Airway Management, 2 nd Ed. Lippincott, 2004. Tobias JD. Airway management for pediatric emergencies. Pediatric Annals. 1996; 25: 317 -28