Peak Expiratory Flow Dr anan esmail peak expiratory





- Slides: 49
Peak Expiratory Flow Dr. anan esmail
peak expiratory flow rate an effort-dependent assessment Of a patients ability To forcibly expel air from their lungs
peak expiratory flow rate take less than one minute to perform safe and inexpensive
peak expiratory flow rate It is measured with a small hand-held device that has a mouthpiece attached to one end
peak expiratory flow rate PEFR < Predicated PEFR Value Airways Obstruction
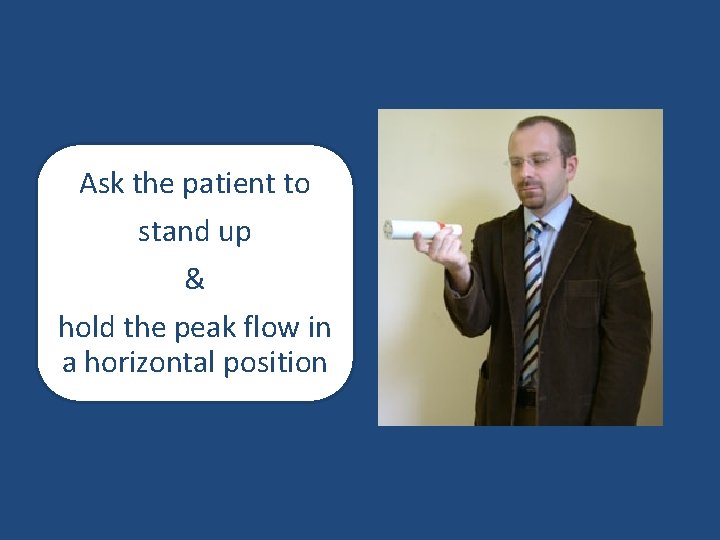
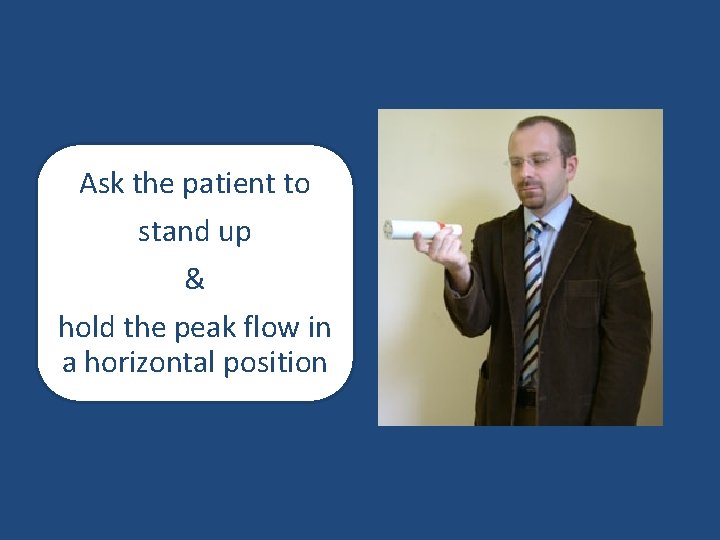
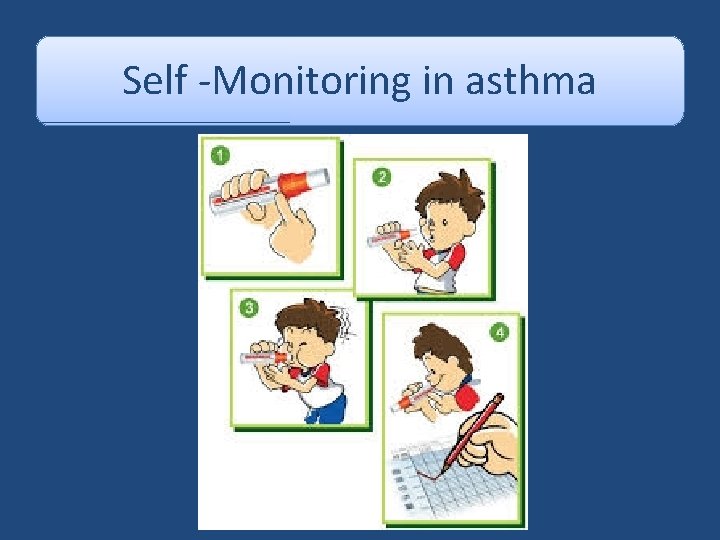
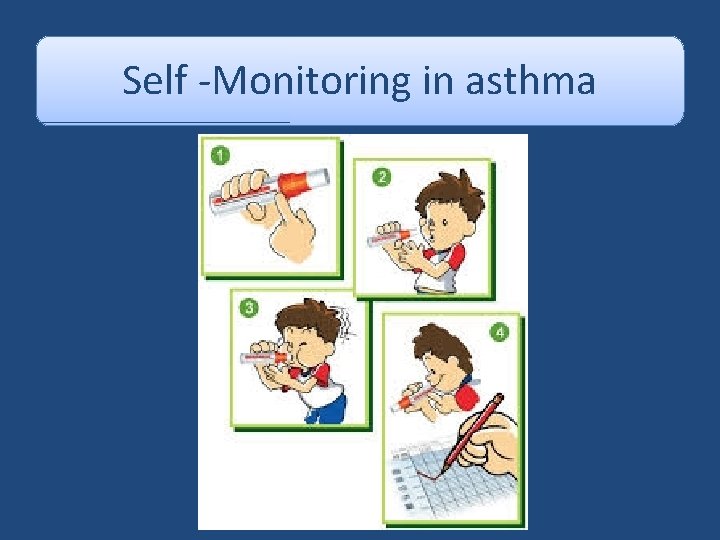
Ask the patient to stand up & hold the peak flow in a horizontal position

Take care not to place your fingers over the scale
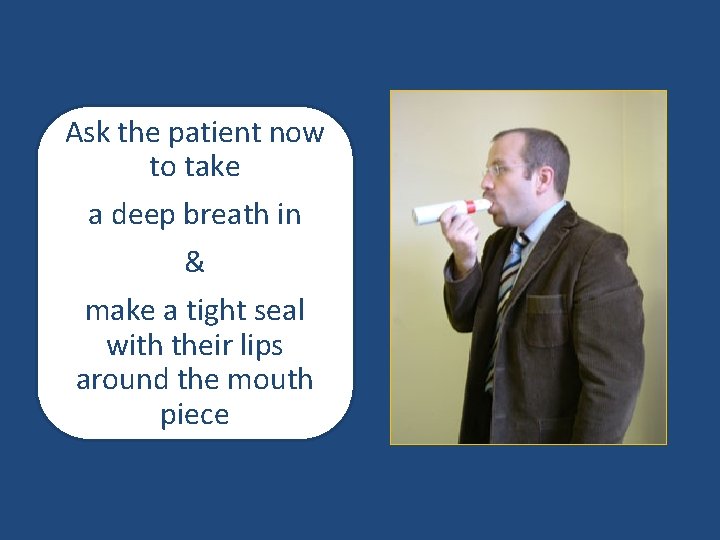
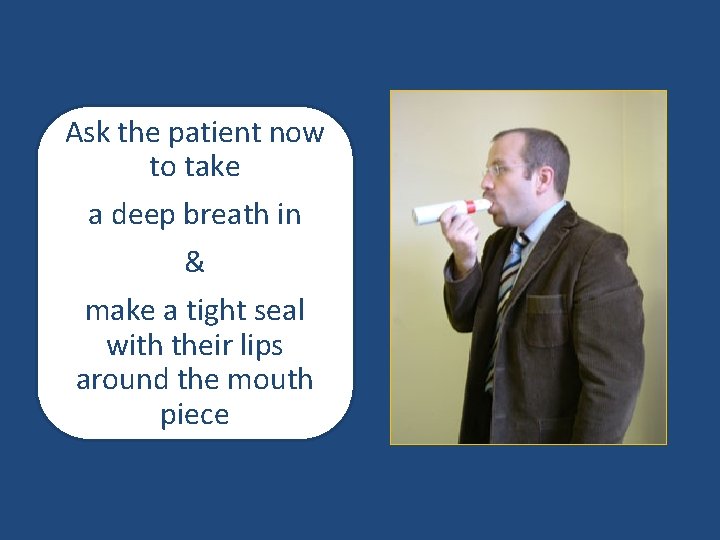
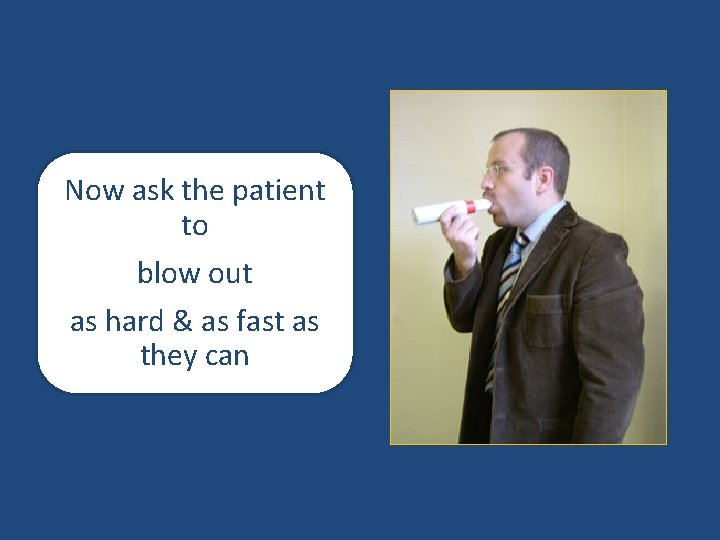
Ask the patient now to take a deep breath in & make a tight seal with their lips around the mouth piece
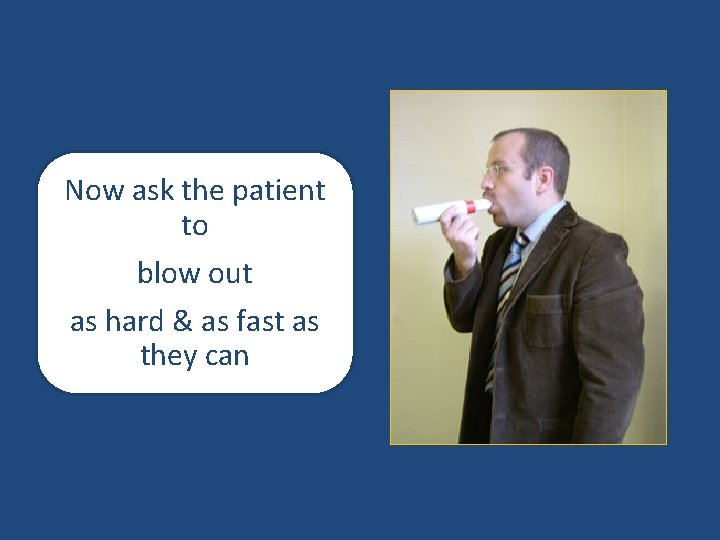
Now ask the patient to blow out as hard & as fast as they can
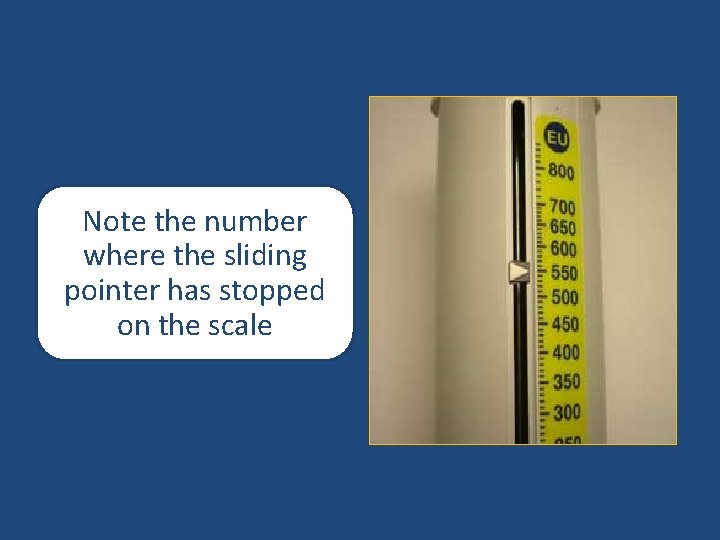
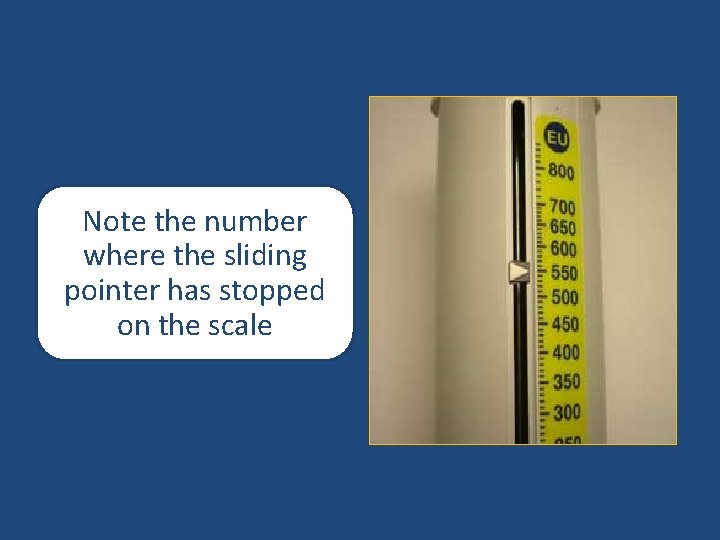
Note the number where the sliding pointer has stopped on the scale
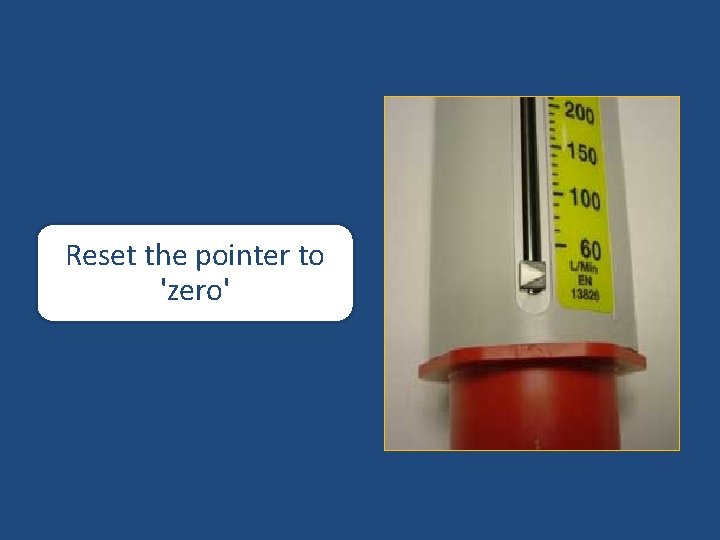
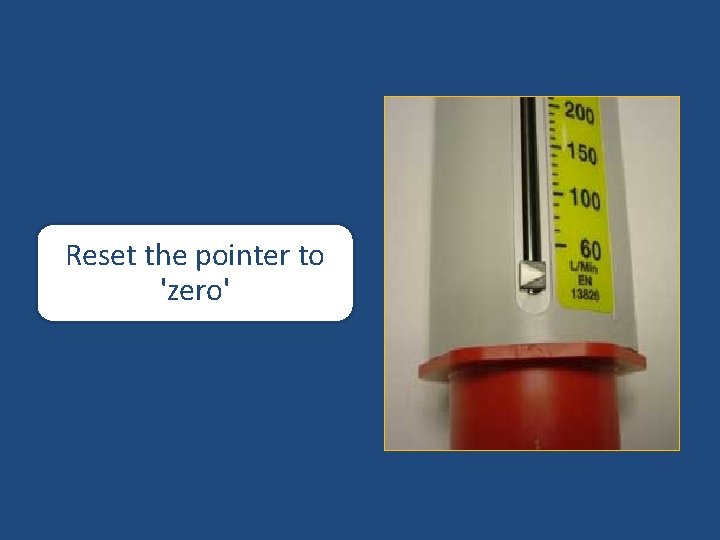
Reset the pointer to 'zero'
ASTHMA DIAGNOSIS
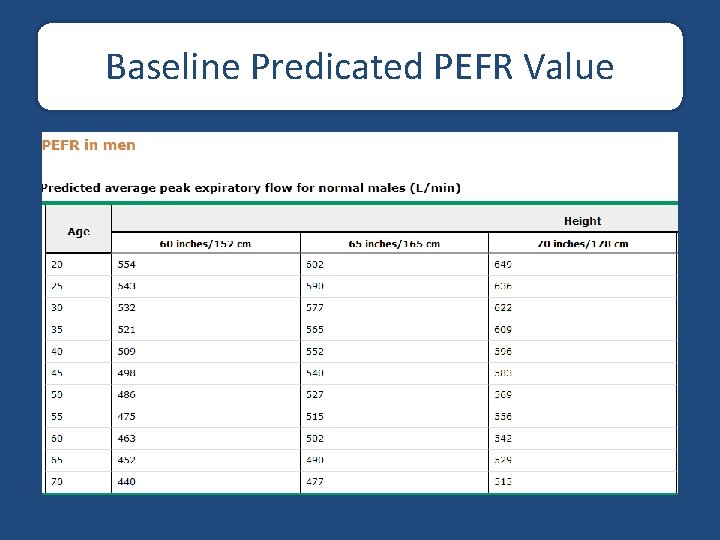
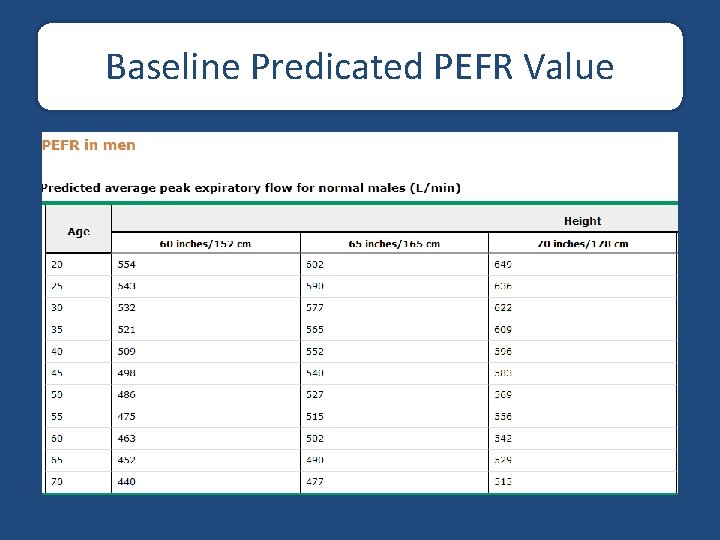
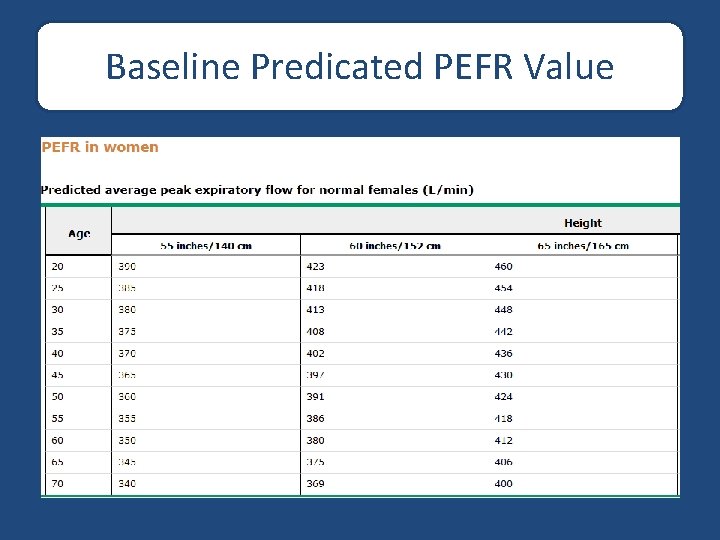
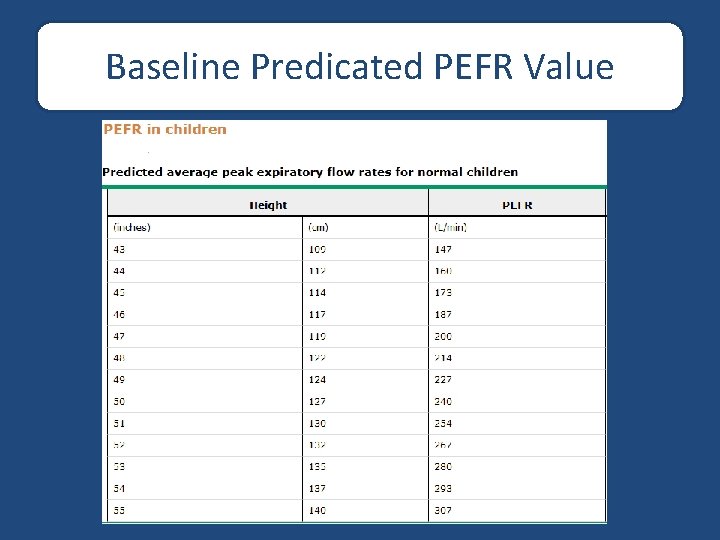
Baseline Predicated PEFR Value
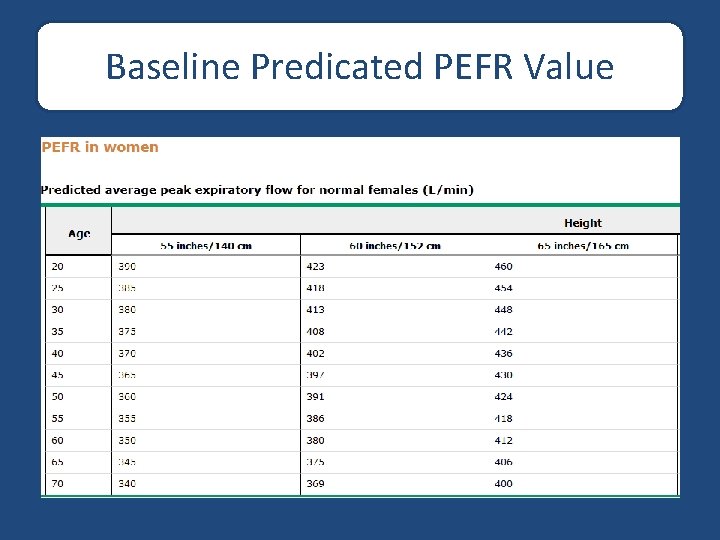
Baseline Predicated PEFR Value
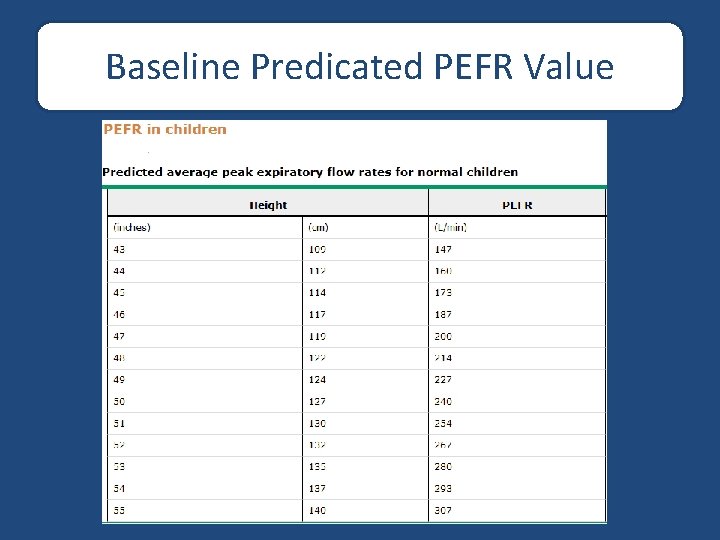
Baseline Predicated PEFR Value
Baseline Predicated PEFR Value Tall – 80 X 5 = Prv PEFR Example: 150 – 80 x 5 = 350 L/min
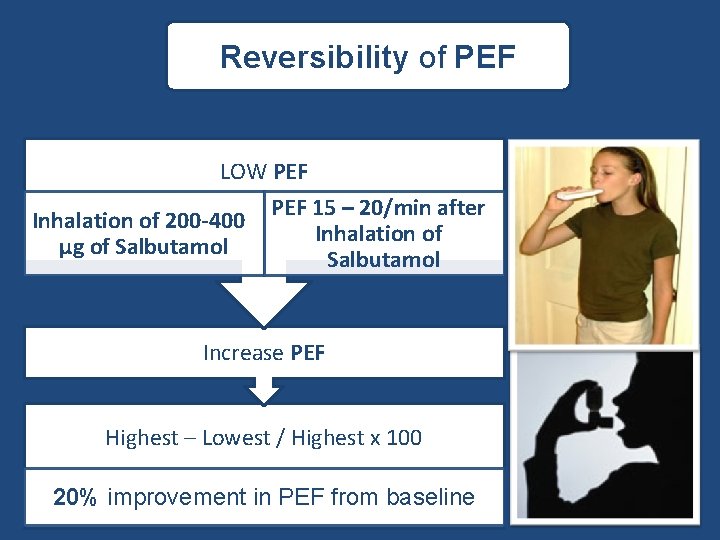
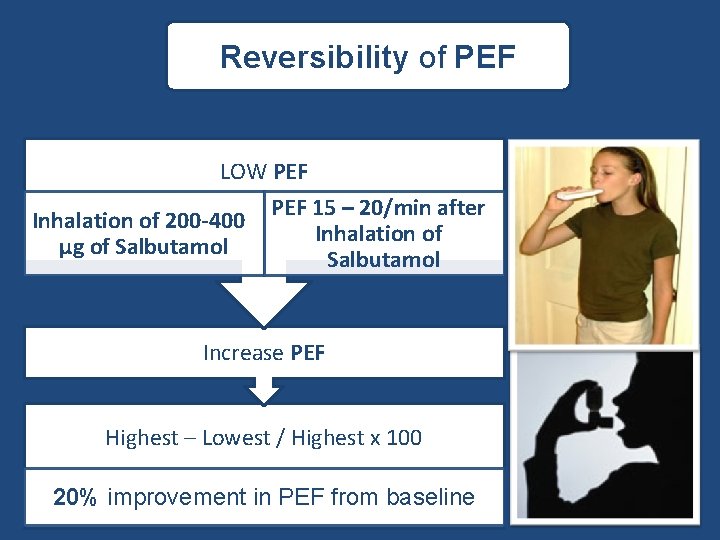
Reversibility of PEF LOW PEF Inhalation of 200 -400 µg of Salbutamol PEF 15 – 20/min after Inhalation of Salbutamol Increase PEF Highest – Lowest / Highest x 100 20% improvement in PEF from baseline

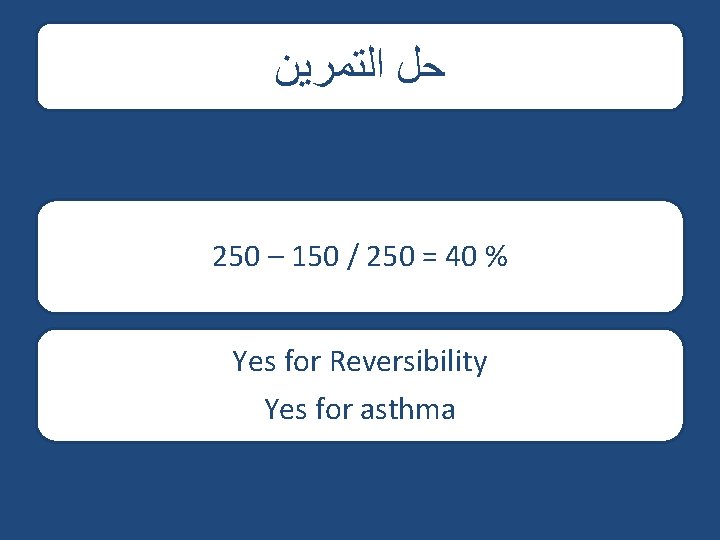
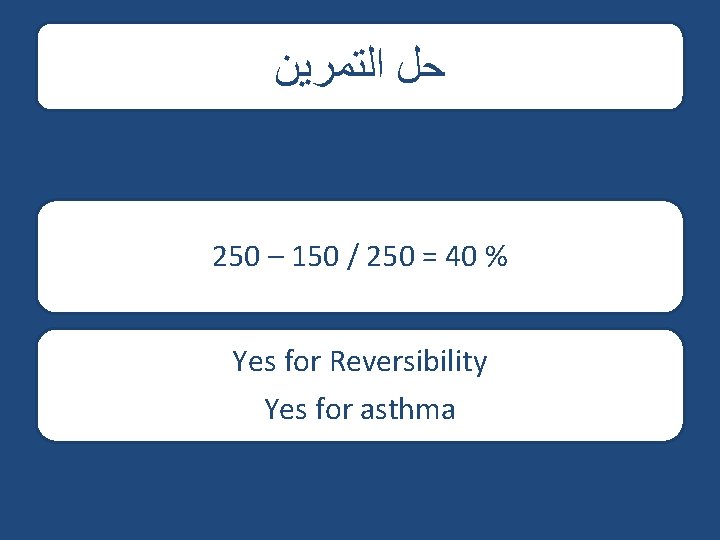
ﺣﻞ ﺍﻟﺘﻤﺮﻳﻦ 250 – 150 / 250 = 40 % Yes for Reversibility Yes for asthma
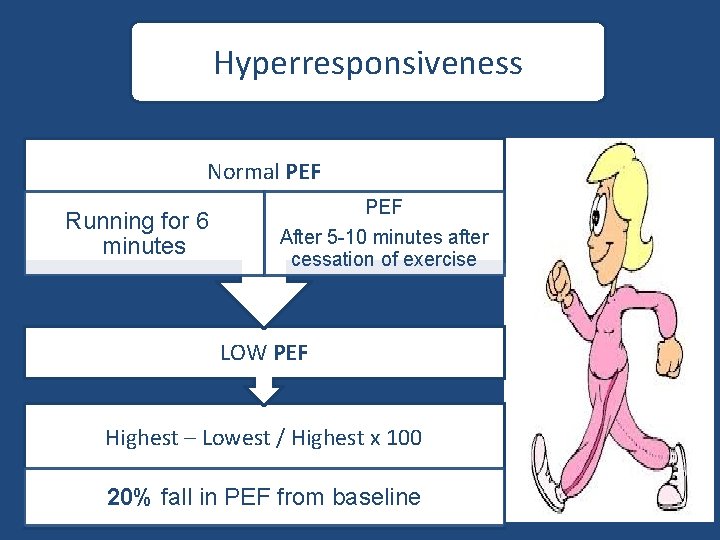
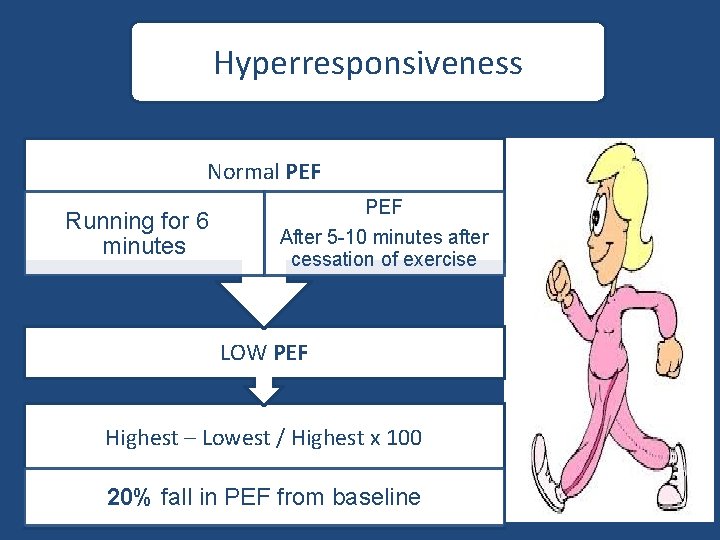
Hyperresponsiveness Normal PEF Running for 6 minutes PEF After 5 -10 minutes after cessation of exercise LOW PEF Highest – Lowest / Highest x 100 20% fall in PEF from baseline

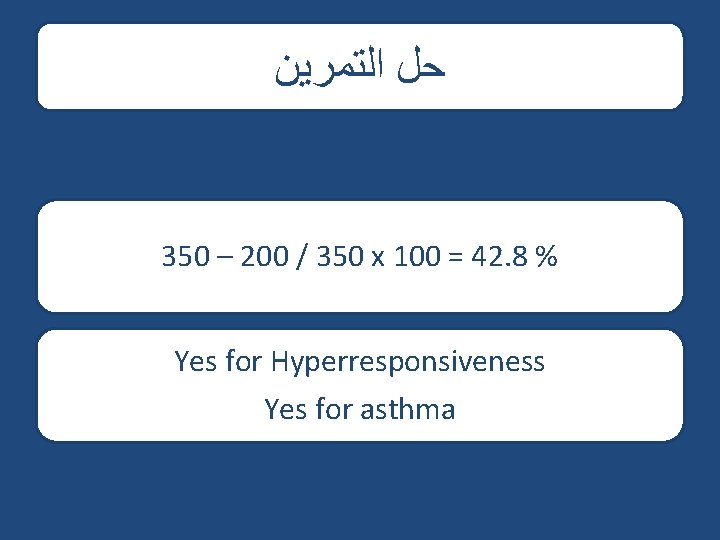
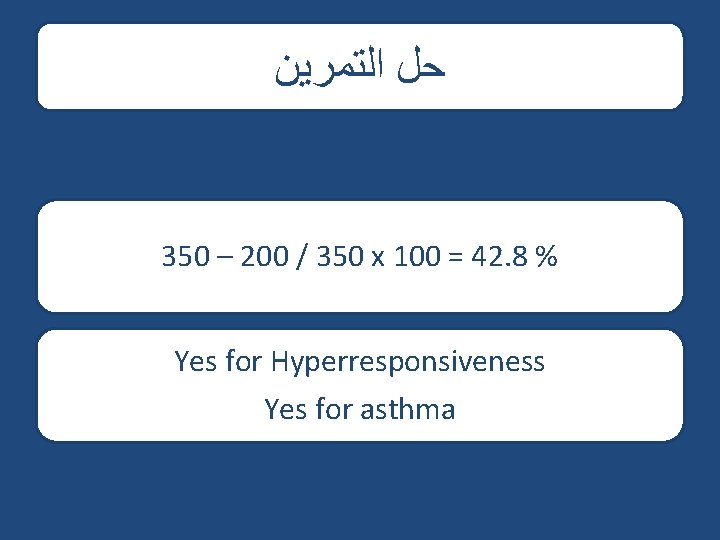
ﺣﻞ ﺍﻟﺘﻤﺮﻳﻦ 350 – 200 / 350 x 100 = 42. 8 % Yes for Hyperresponsiveness Yes for asthma
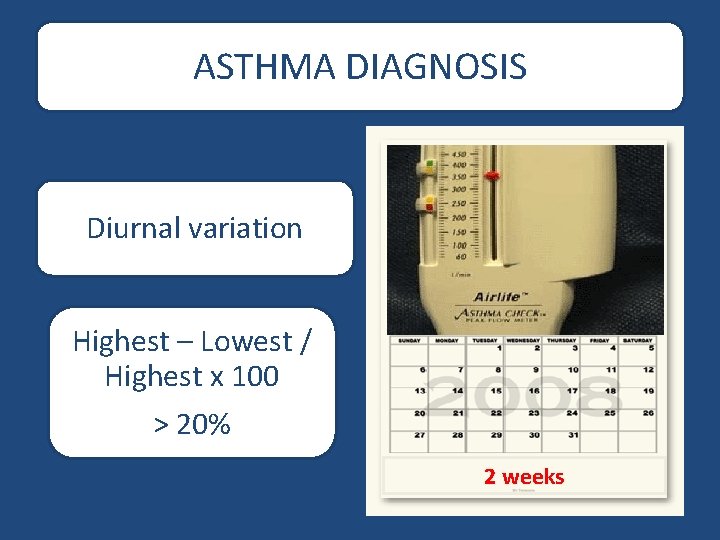
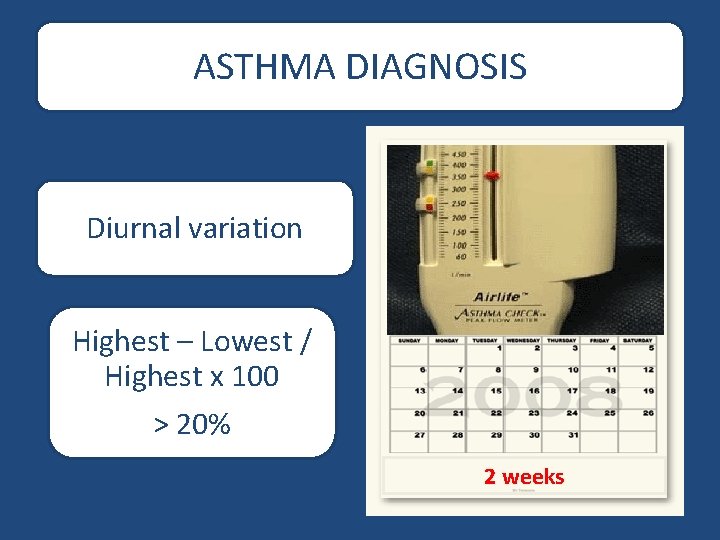
ASTHMA DIAGNOSIS Diurnal variation Highest – Lowest / Highest x 100 > 20% 2 weeks
CLASSIFY SEVERITY OF ASTHMA
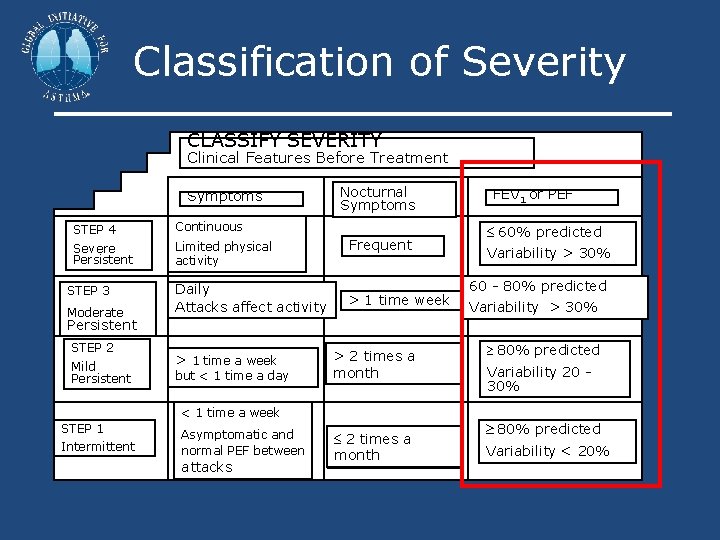
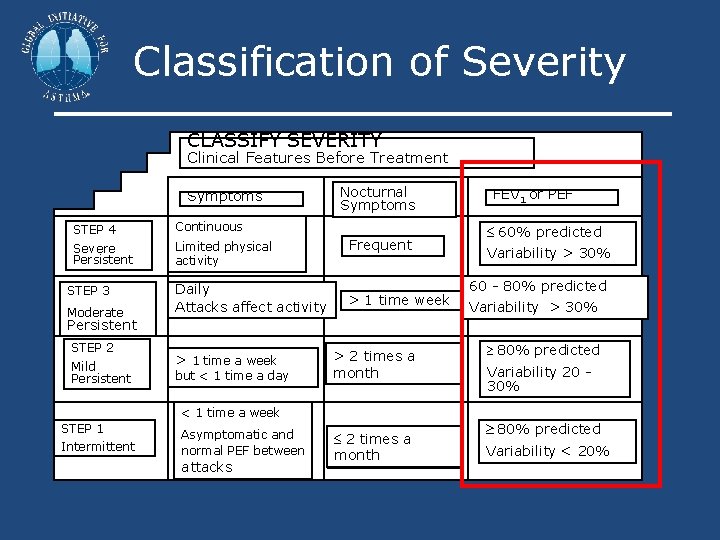
Classification of Severity CLASSIFY SEVERITY Clinical Features Before Treatment Symptoms STEP 4 Continuous Severe Persistent Limited physical activity STEP 3 Moderate Daily Attacks affect activity Nocturnal Symptoms Frequent > 1 time week FEV 1 or PEF 60% predicted Variability > 30% 60 - 80% predicted Variability > 30% Persistent STEP 2 Mild Persistent > 1 time a week but < 1 time a day > 2 times a month 80% predicted Variability 20 30% < 1 time a week STEP 1 Intermittent Asymptomatic and normal PEF between attacks 2 times a month 80% predicted Variability < 20%
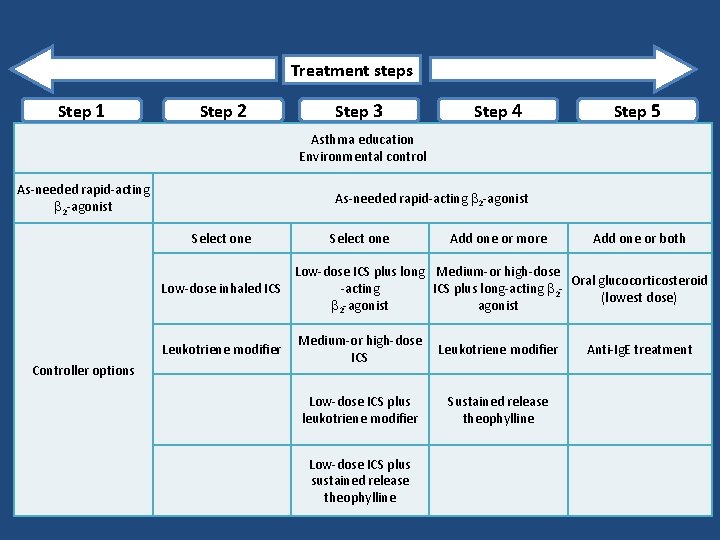
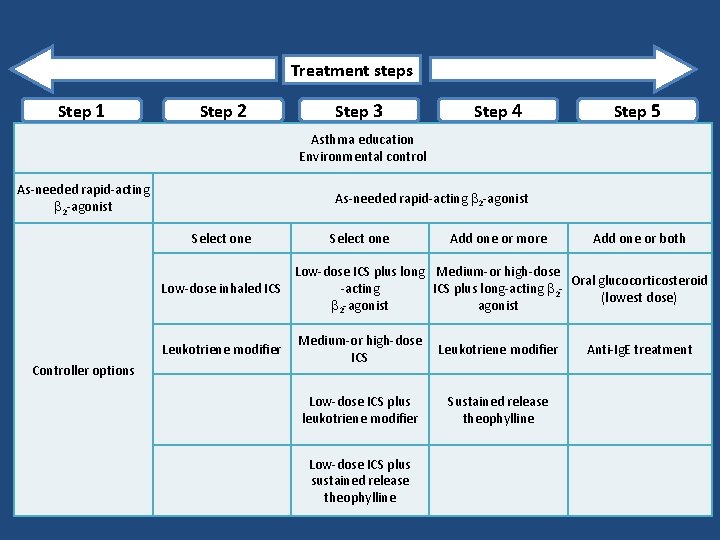
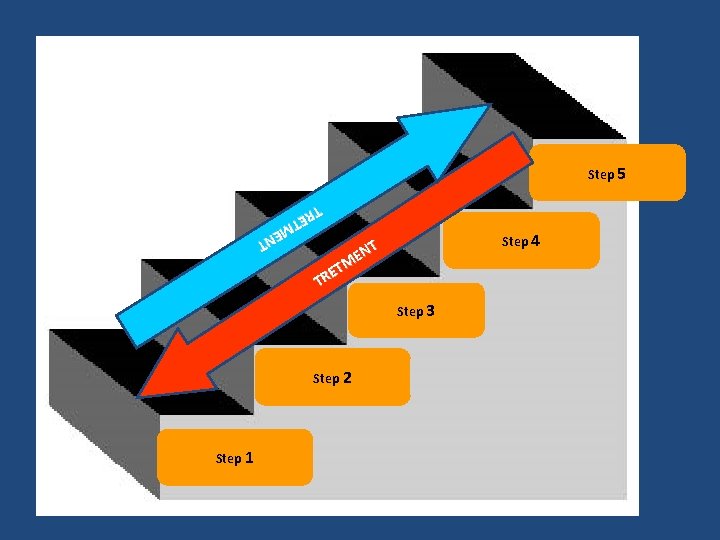
REDUCE INCREASE Treatment steps Step 1 Step 2 Step 3 Step 4 Step 5 Asthma education Environmental control As-needed rapid-acting 2 -agonist Select one Add one or more Add one or both Low-dose ICS plus long Medium-or high-dose Oral glucocorticosteroid Low-dose inhaled ICS -acting ICS plus long-acting 2(lowest dose) 2 -agonist Leukotriene modifier Controller options Medium-or high-dose ICS Leukotriene modifier Low-dose ICS plus leukotriene modifier Sustained release theophylline Low-dose ICS plus sustained release theophylline Anti-Ig. E treatment
Self -Monitoring in asthma
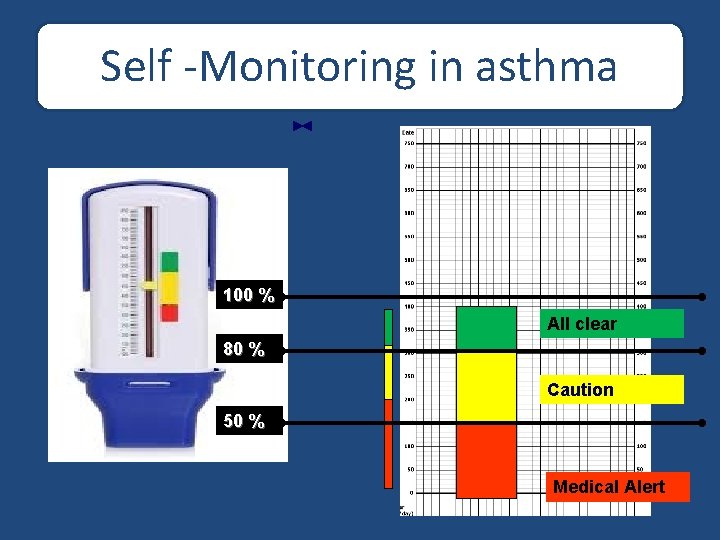
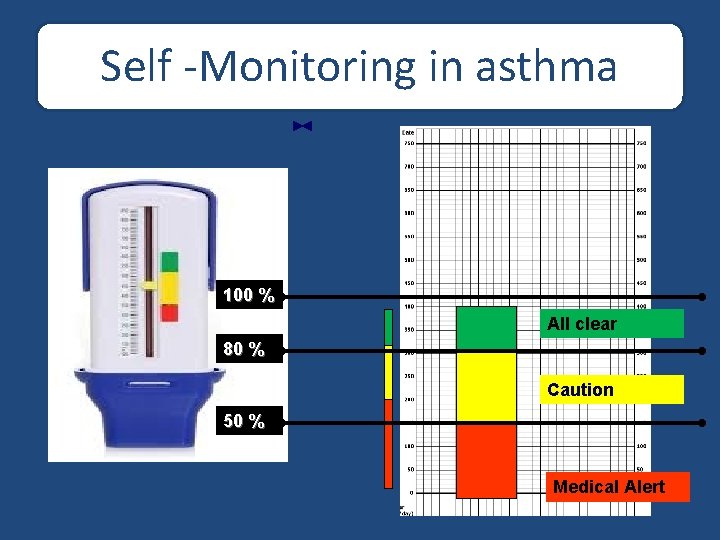
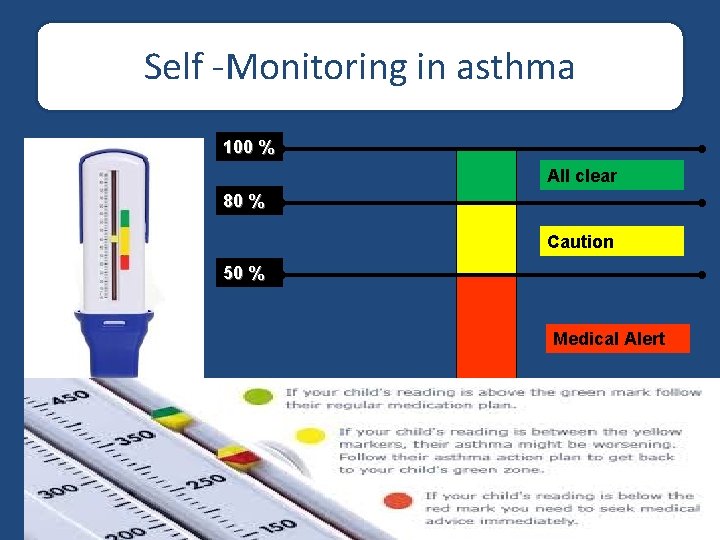
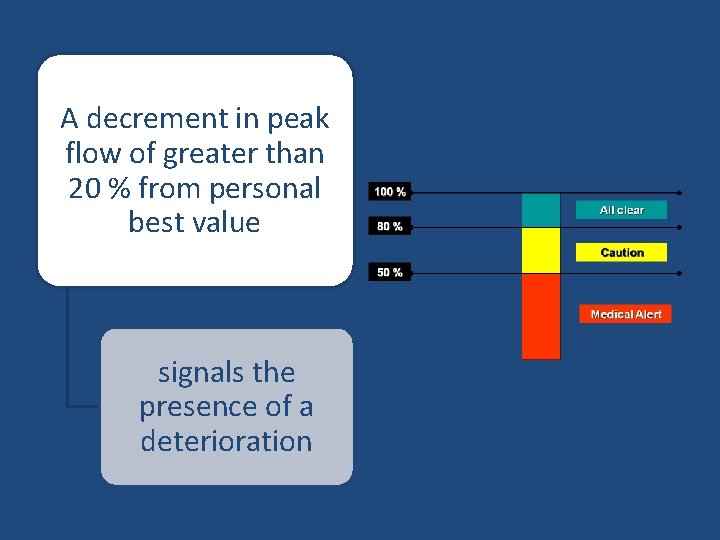
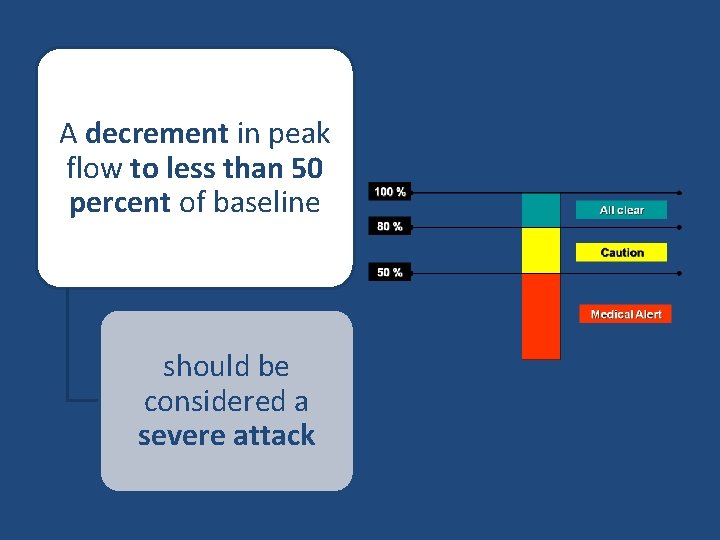
Self -Monitoring in asthma 100 % All clear 80 % Caution 50 % Medical Alert
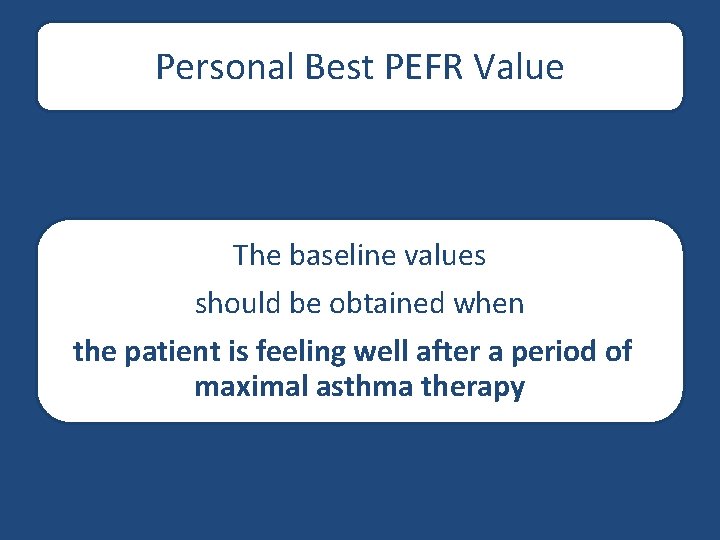
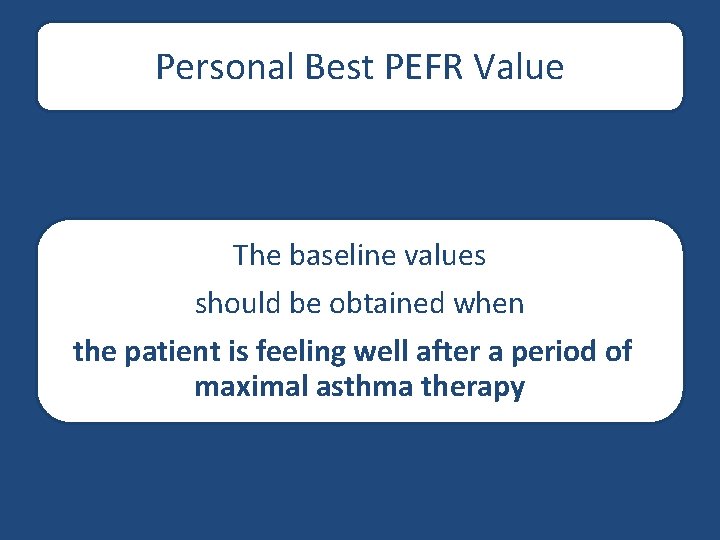
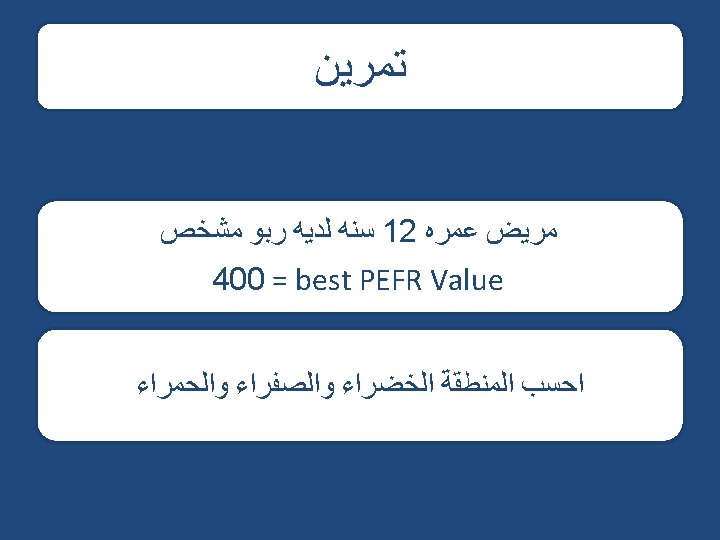
Personal Best PEFR Value The baseline values should be obtained when the patient is feeling well after a period of maximal asthma therapy
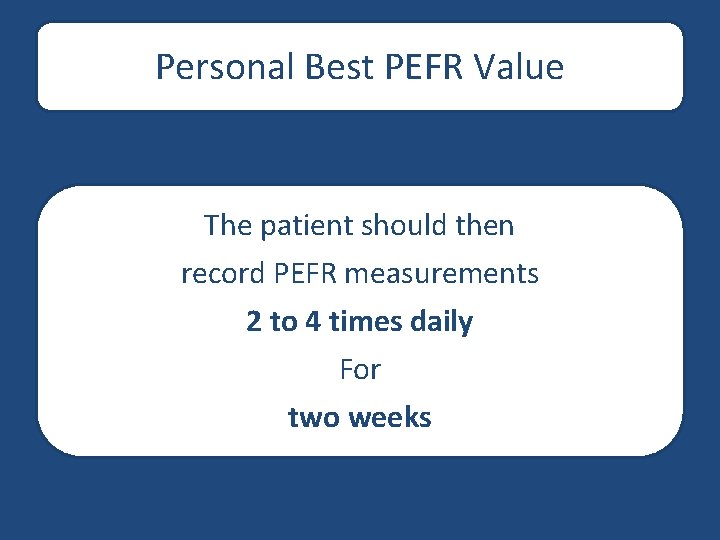
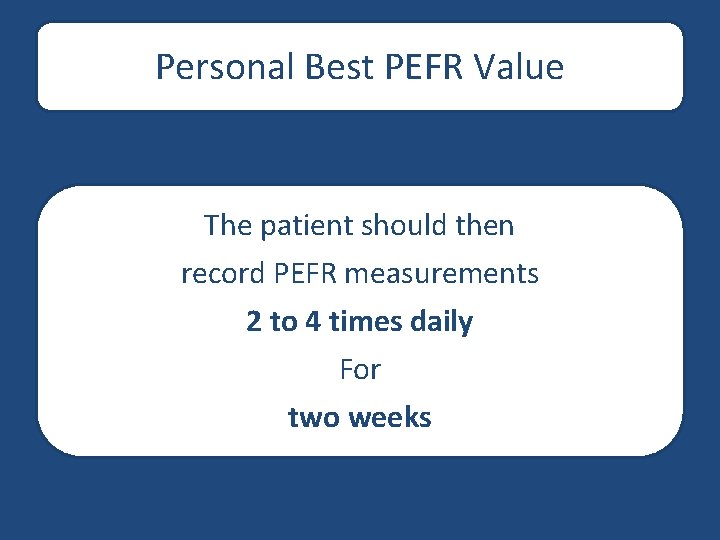
Personal Best PEFR Value The patient should then record PEFR measurements 2 to 4 times daily For two weeks

Personal Best PEFR Value The personal best PEFR Value Is the highest PEFR measurement achieved during this post-treatment monitoring period
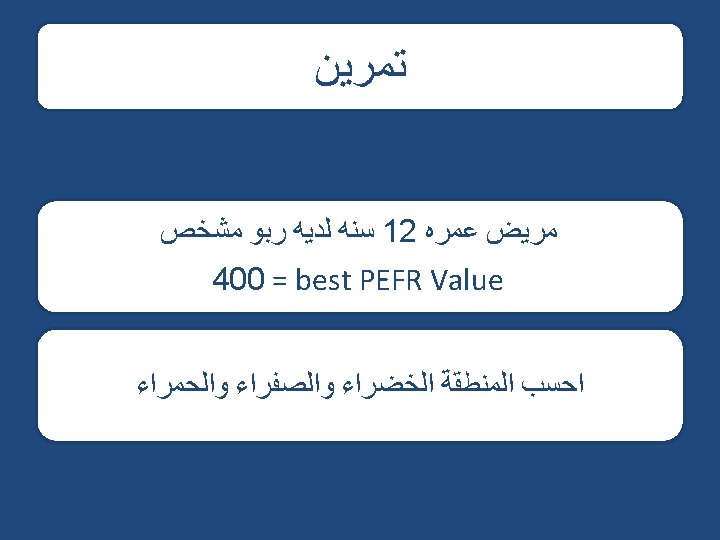
Self -Monitoring in asthma The patient's normal PEFR range is defined as 80 and 100 percent of the patient's personal best
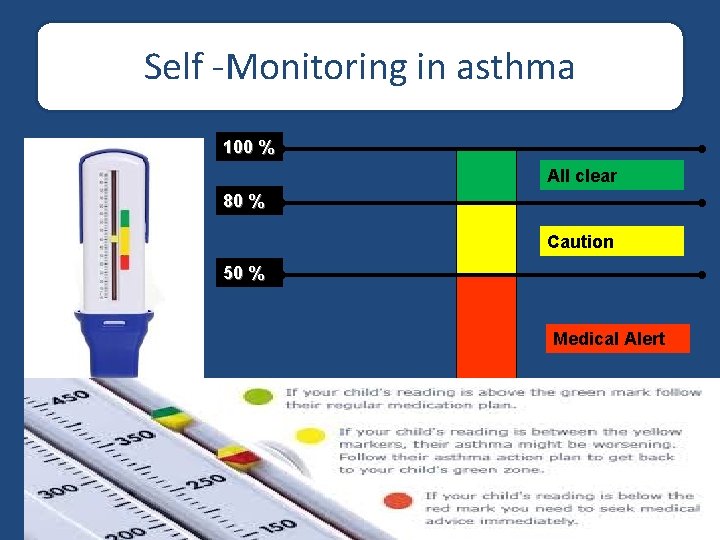
Self -Monitoring in asthma 100 % All clear 80 % Caution 50 % Medical Alert
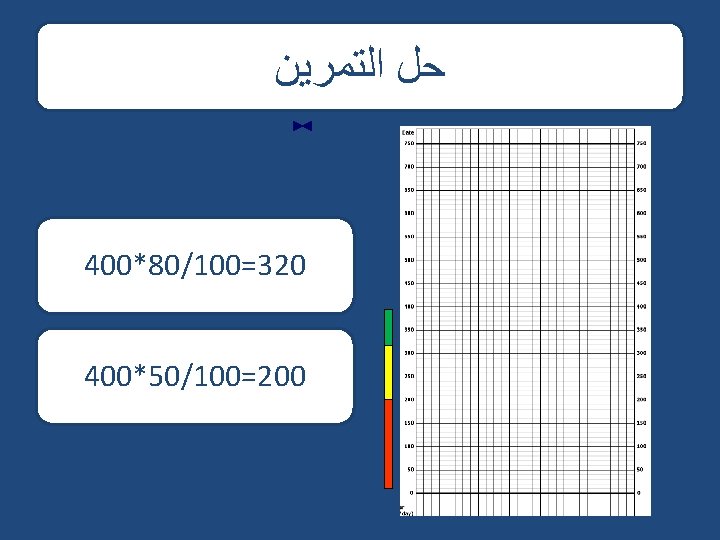
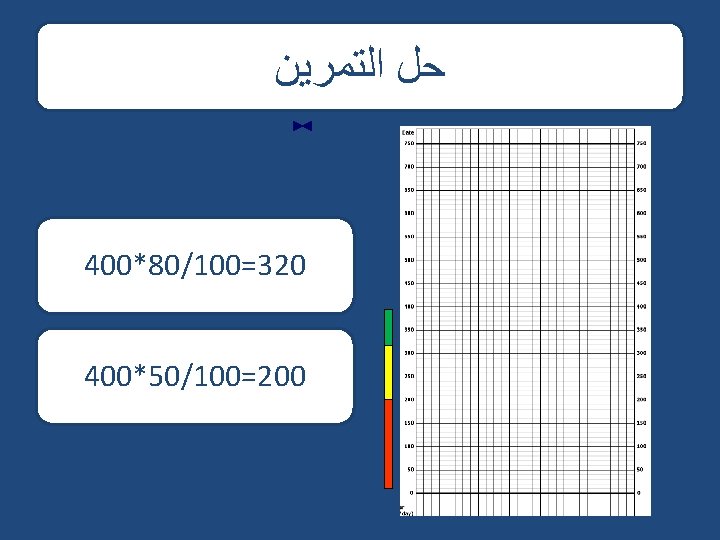
ﺣﻞ ﺍﻟﺘﻤﺮﻳﻦ 400*80/100=320 400*50/100=200
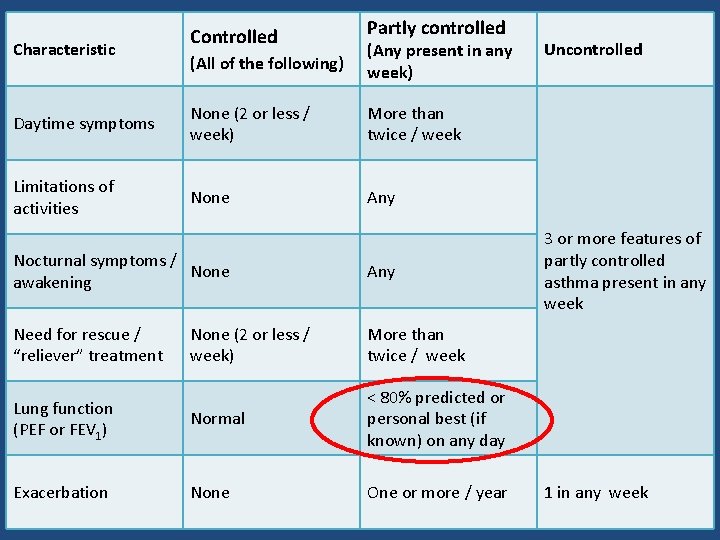
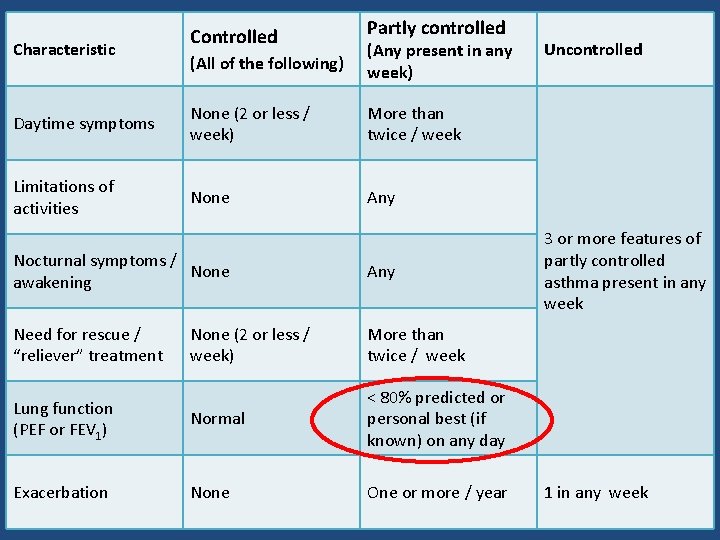
Characteristic Controlled Partly controlled (All of the following) (Any present in any week) Daytime symptoms None (2 or less / week) More than twice / week Limitations of activities None Any Nocturnal symptoms / None awakening Any Need for rescue / “reliever” treatment None (2 or less / week) More than twice / week Lung function (PEF or FEV 1) Normal < 80% predicted or personal best (if known) on any day Exacerbation None One or more / year Uncontrolled 3 or more features of partly controlled asthma present in any week 1 in any week
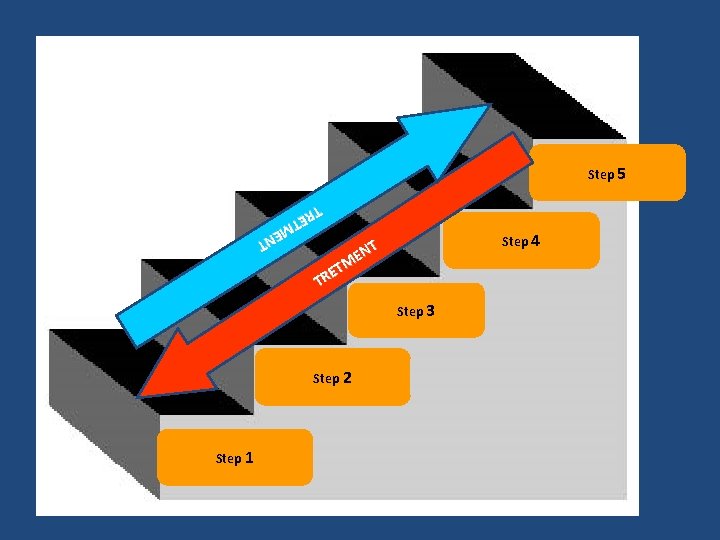
Step 5 NT ME ET TR Step 4 NT E M ET R T Step 3 Step 2 Step 1
Detecting the onset of asthma exacerbation
Some patients are very sensitive to increased asthma symptoms while others perceive reduced airflow only when it becomes marked decrease in peak expiratory flow may be the first sign that asthma control is deteriorating
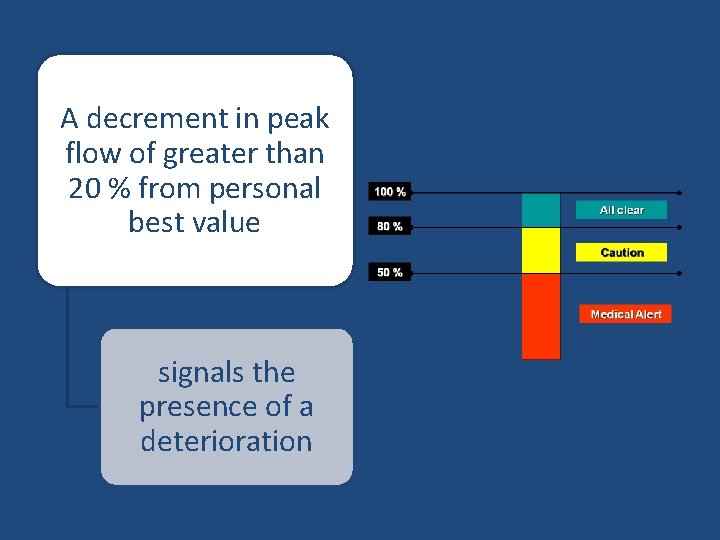
A decrement in peak flow of greater than 20 % from personal best value signals the presence of a deterioration
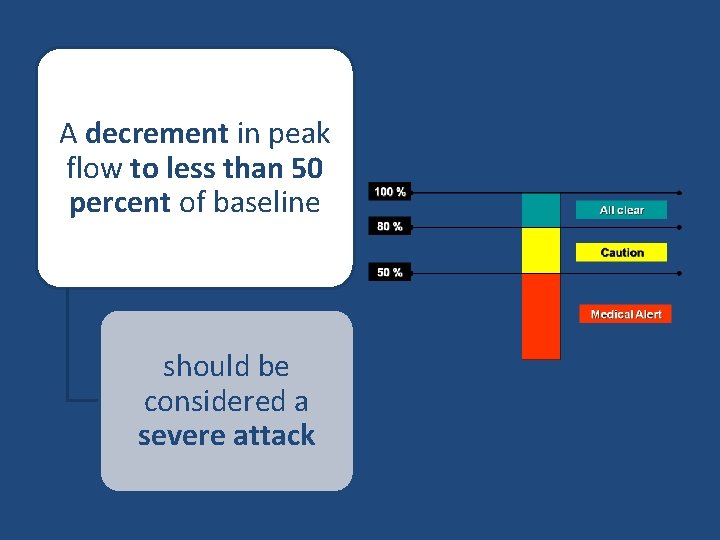
A decrement in peak flow to less than 50 percent of baseline should be considered a severe attack
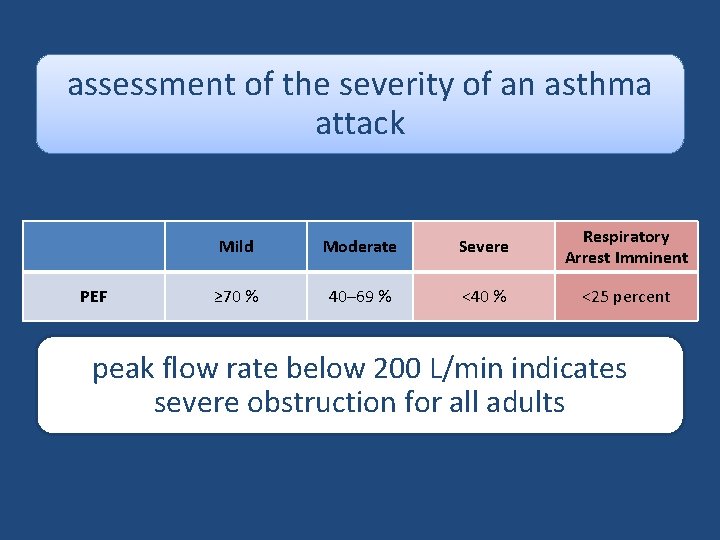
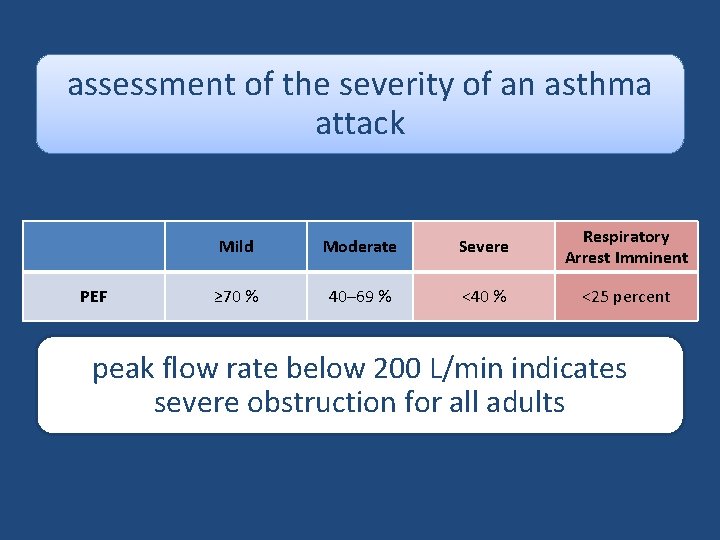
assessment of the severity of an asthma attack PEF Mild Moderate Severe Respiratory Arrest Imminent ≥ 70 % 40– 69 % <40 % <25 percent peak flow rate below 200 L/min indicates severe obstruction for all adults
monitor a patient's response to treatment of asthma exacerbation
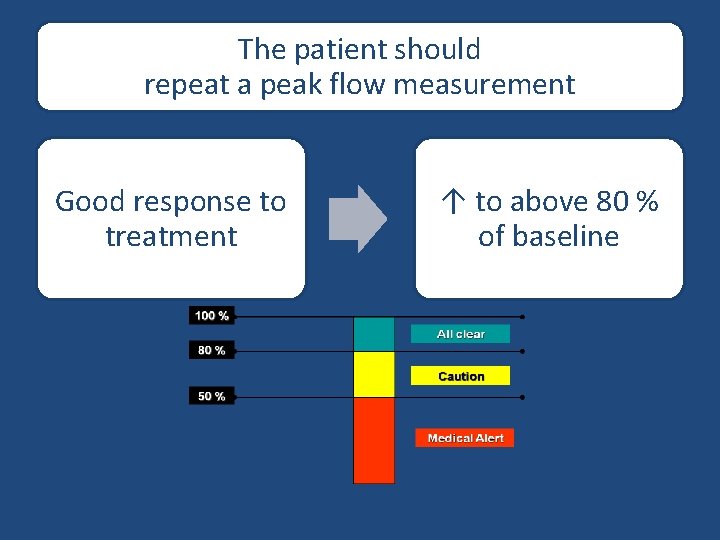
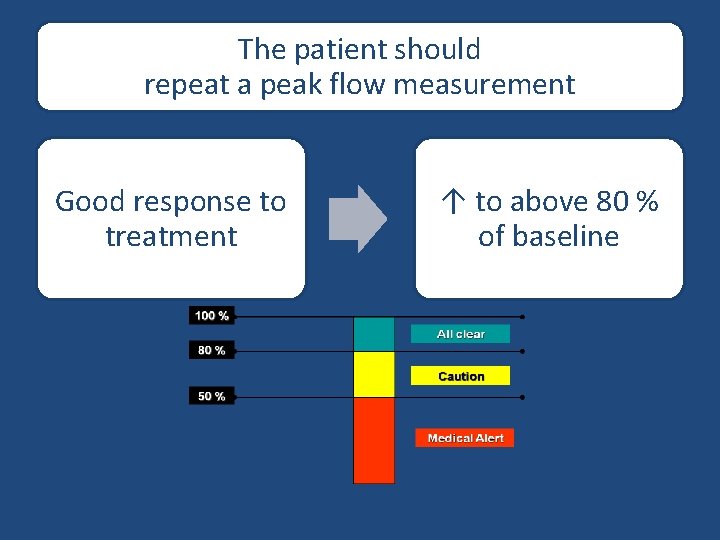
The patient should repeat a peak flow measurement Good response to treatment ↑ to above 80 % of baseline
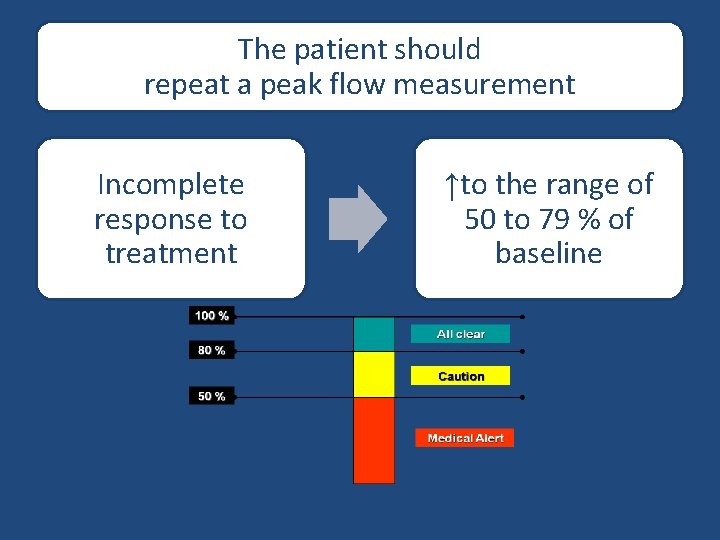
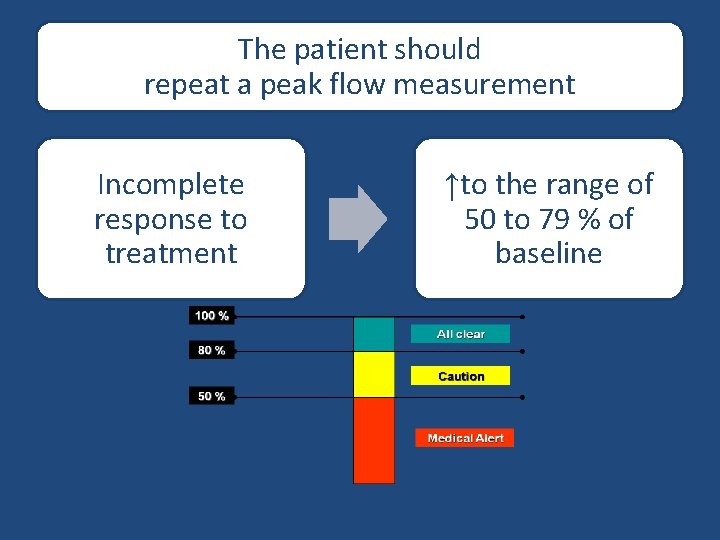
The patient should repeat a peak flow measurement Incomplete response to treatment ↑to the range of 50 to 79 % of baseline
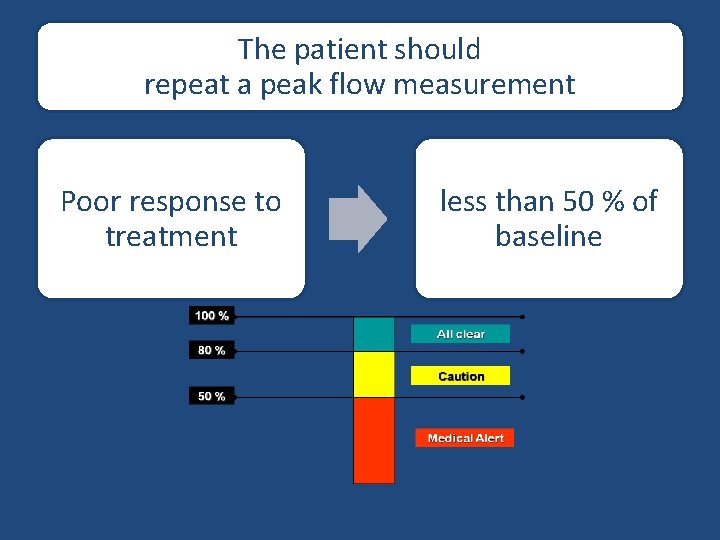
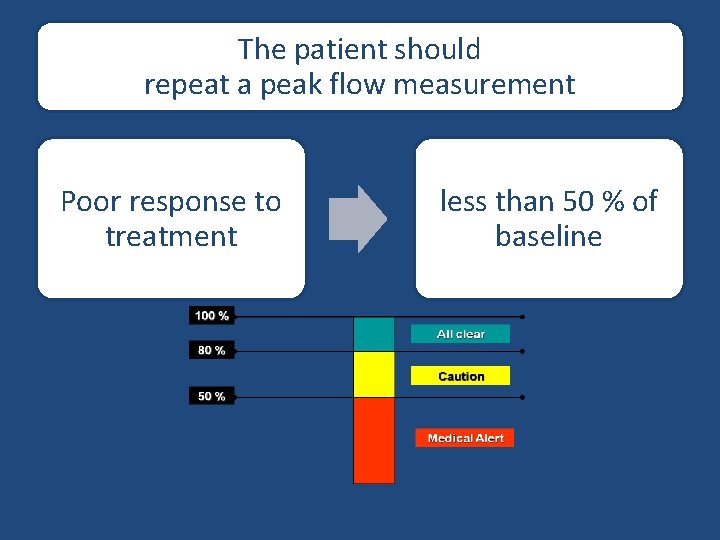
The patient should repeat a peak flow measurement Poor response to treatment less than 50 % of baseline
