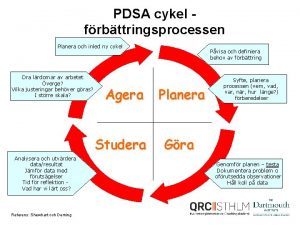
PDSA Training Agenda PDSA cycles How to run






![How do you collect your data? • Define starting point [ BASELINE] • Collecting How do you collect your data? • Define starting point [ BASELINE] • Collecting](https://slidetodoc.com/presentation_image_h2/b06379c47f186aa8bf7b3b738cec1334/image-31.jpg)




- Slides: 43

PDSA Training
Agenda • PDSA cycles • How to run a PDSA • Example Call Management and Dr Triage go live plan
Change Methodology for Improvement
The Thinking Part Three fundamental questions for improvement ( Nolan Questions )
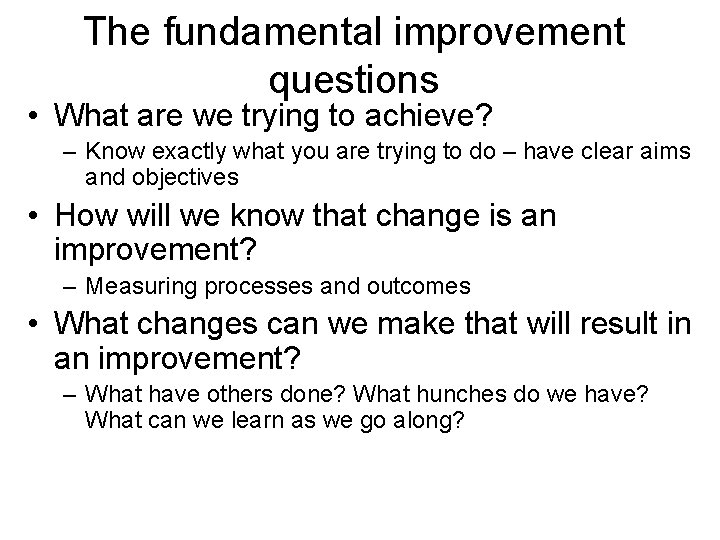
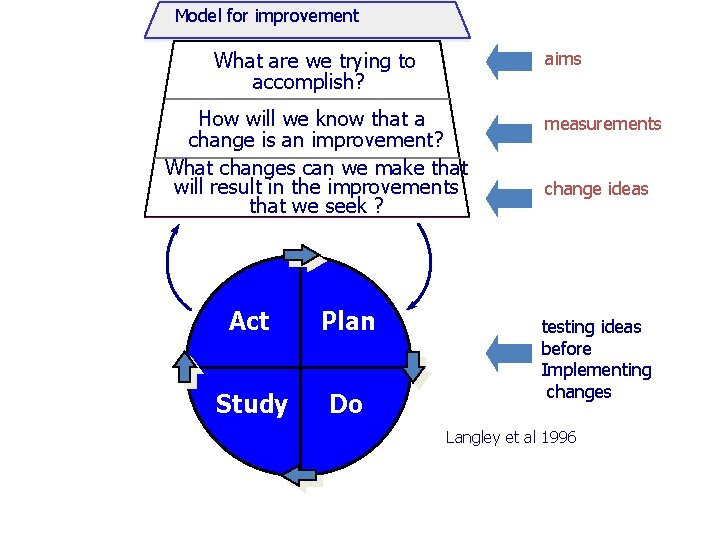
The fundamental improvement questions • What are we trying to achieve? – Know exactly what you are trying to do – have clear aims and objectives • How will we know that change is an improvement? – Measuring processes and outcomes • What changes can we make that will result in an improvement? – What have others done? What hunches do we have? What can we learn as we go along?
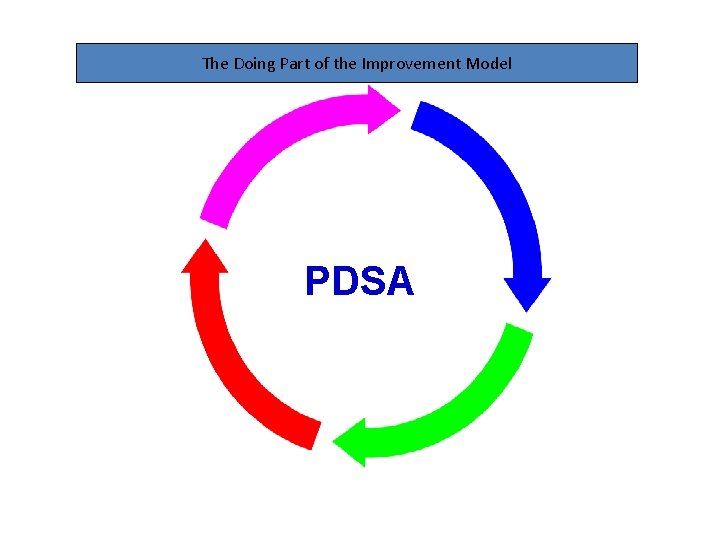
The Doing Part of the Improvement Model PDSA
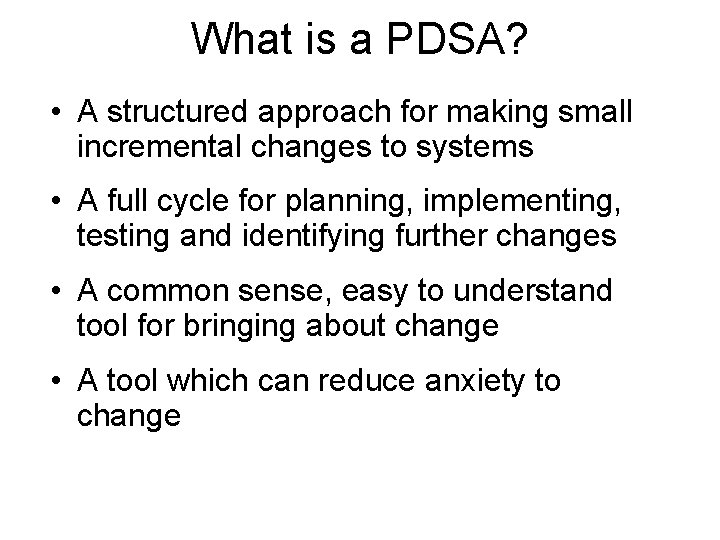
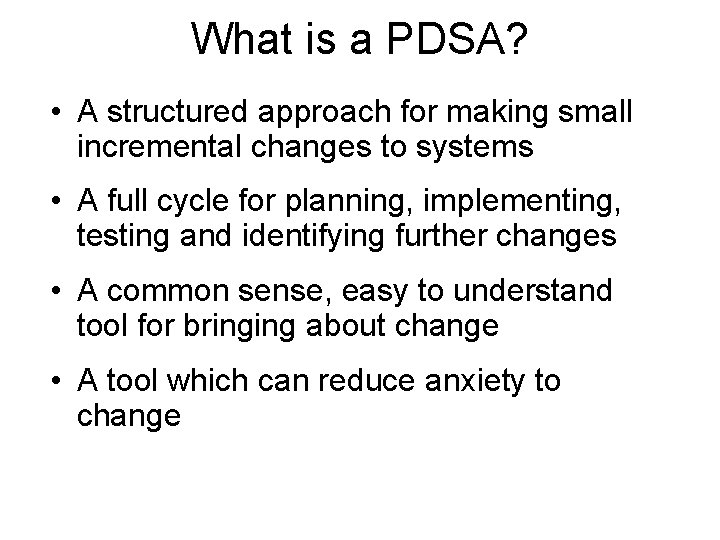
What is a PDSA? • A structured approach for making small incremental changes to systems • A full cycle for planning, implementing, testing and identifying further changes • A common sense, easy to understand tool for bringing about change • A tool which can reduce anxiety to change

Why use PDSAs? • PDSA cycles have a long pedigree • They are ‘natural’ to Health Care • PDSAs are small in scope and build incrementally – small rapid cycles lead to improvement • They have methodological validity • They have been used and developed by Collaborative participants in the UK for 6 years and even longer across Scandinavia and America
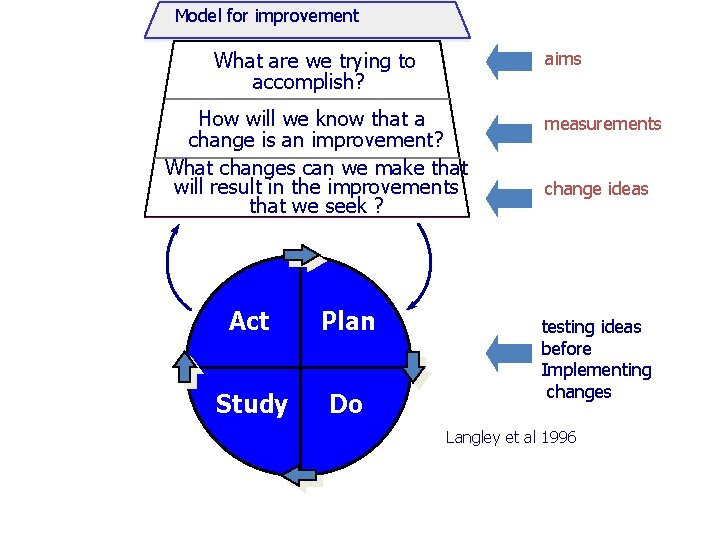
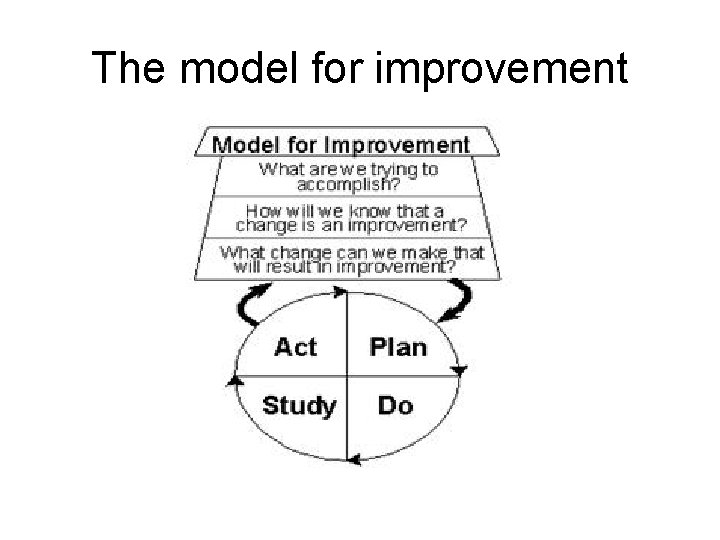
Model for improvement What are we trying to accomplish? aims How will we know that a change is an improvement? What changes can we make that will result in the improvements that we seek ? Act Plan Study Do measurements change ideas testing ideas before Implementing changes Langley et al 1996
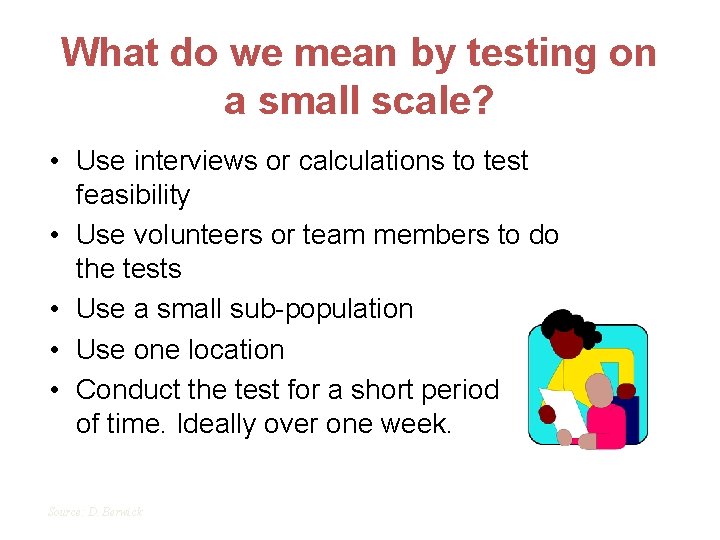
What do we mean by testing on a small scale? • Use interviews or calculations to test feasibility • Use volunteers or team members to do the tests • Use a small sub-population • Use one location • Conduct the test for a short period of time. Ideally over one week. Source: D. Berwick
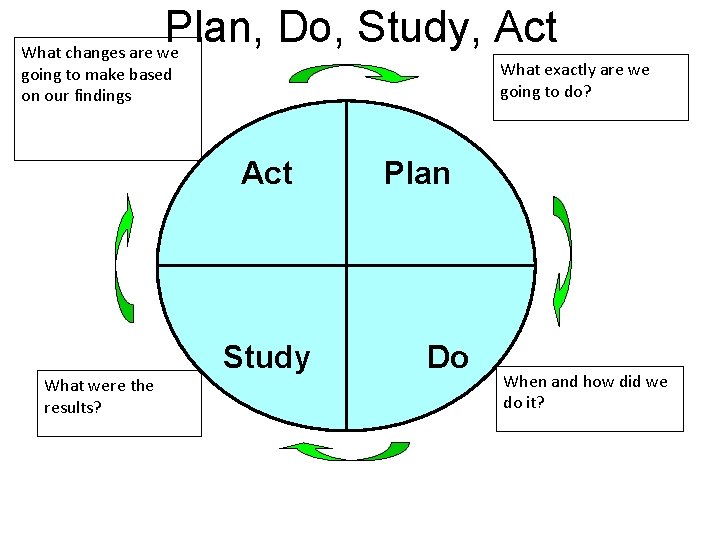
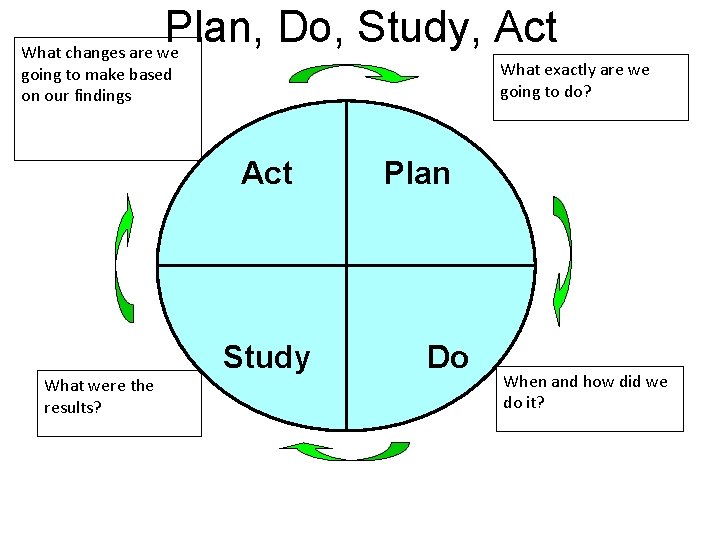
Plan, Do, Study, Act What changes are we What exactly are we going to do? going to make based on our findings Act What were the results? Study Plan Do When and how did we do it?
Objective (future tense) • Define the problem • What exactly are you trying to achieve • Refer to the Nolan questions (think)
Plan (future tense) • • • Who? What? Where? When? How? What are you going to measure?
Do (past tense) • Just do it! Note any variation from the plan, such as a change from the plan due to complexity, lack of staff etc.
Study (past tense - outcome) • Study the outcome of your measures What worked? Do you need to carry out another PDSA? Do you need to involve more people? Do you need to generate more ideas? • What didn’t work and why? Do you need to change the plan? Do you need to tweak the original pdsa?

Act (present / future tense) • What changes are you going to make based on your findings? • This will inform your next PDSA cycle • Document the change you are going to make and identify future plans
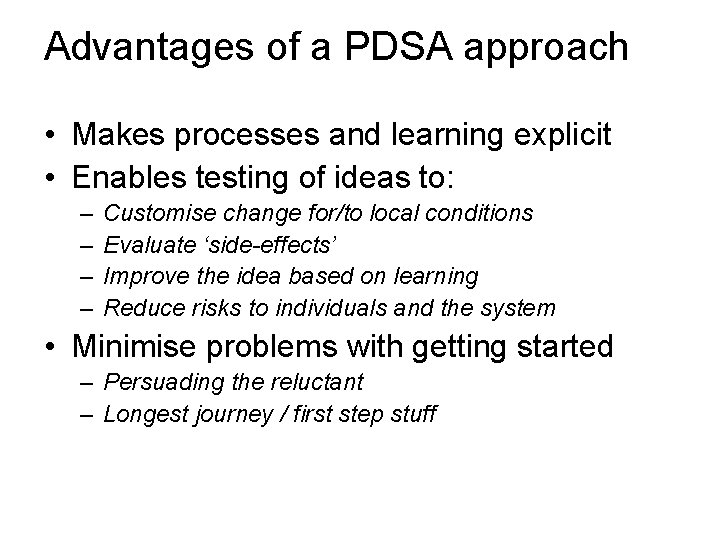
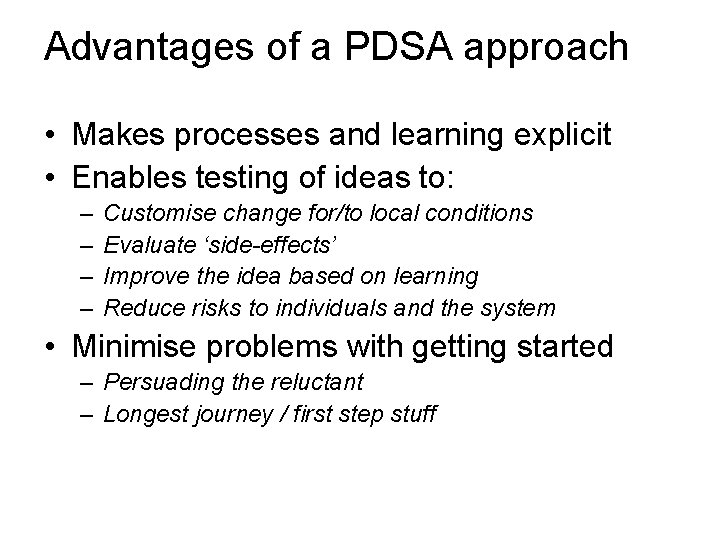
Advantages of a PDSA approach • Makes processes and learning explicit • Enables testing of ideas to: – – Customise change for/to local conditions Evaluate ‘side-effects’ Improve the idea based on learning Reduce risks to individuals and the system • Minimise problems with getting started – Persuading the reluctant – Longest journey / first step stuff
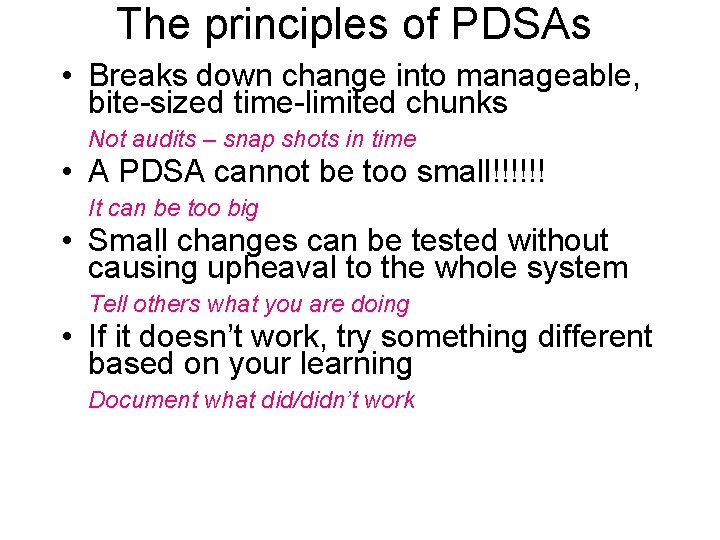
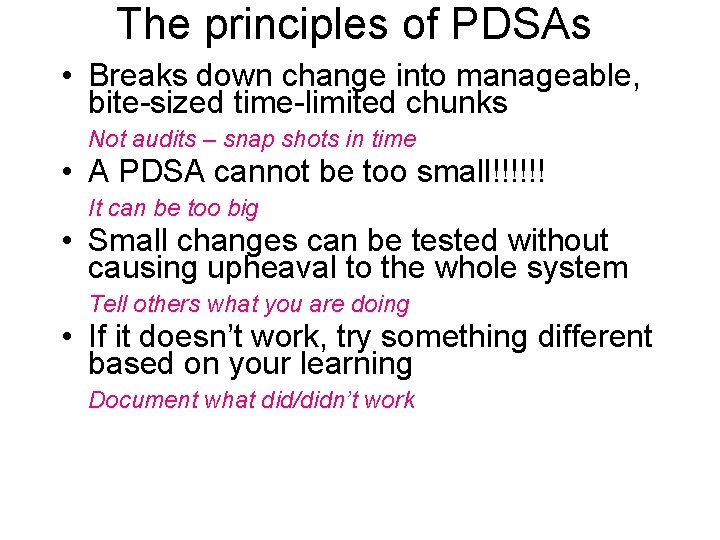
The principles of PDSAs • Breaks down change into manageable, bite-sized time-limited chunks Not audits – snap shots in time • A PDSA cannot be too small!!!!!! It can be too big • Small changes can be tested without causing upheaval to the whole system Tell others what you are doing • If it doesn’t work, try something different based on your learning Document what did/didn’t work

Why test? • To learn whether the change will result in an improvement • To predict the amount of improvement possible • To learn how to adapt the change to different environments • To understand the costs and impact of change • To reduce resistance
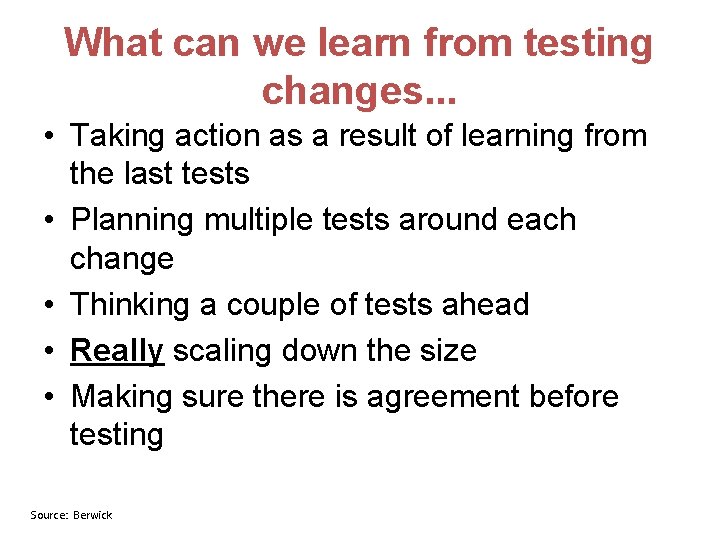
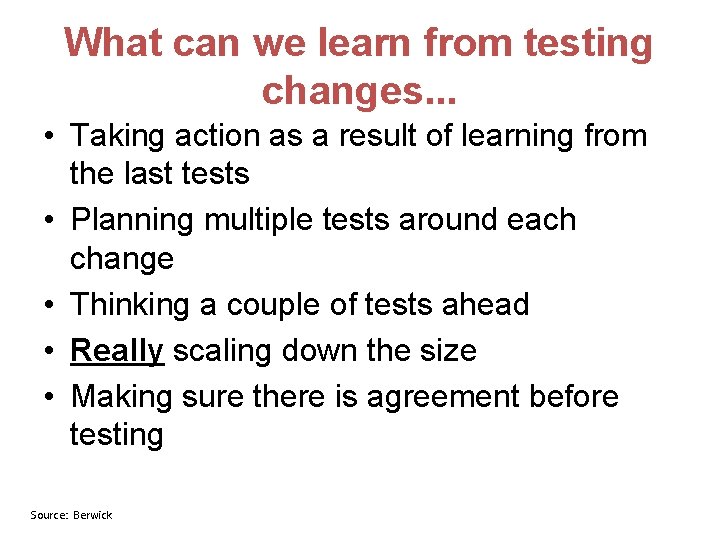
What can we learn from testing changes. . . • Taking action as a result of learning from the last tests • Planning multiple tests around each change • Thinking a couple of tests ahead • Really scaling down the size • Making sure there is agreement before testing Source: Berwick
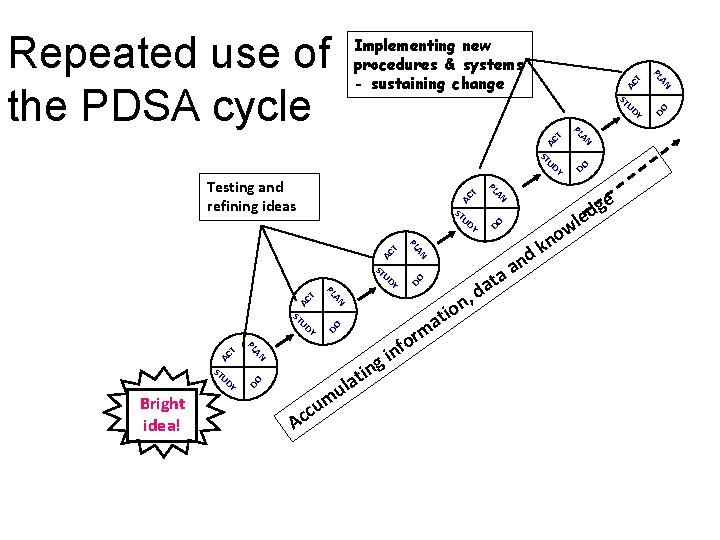
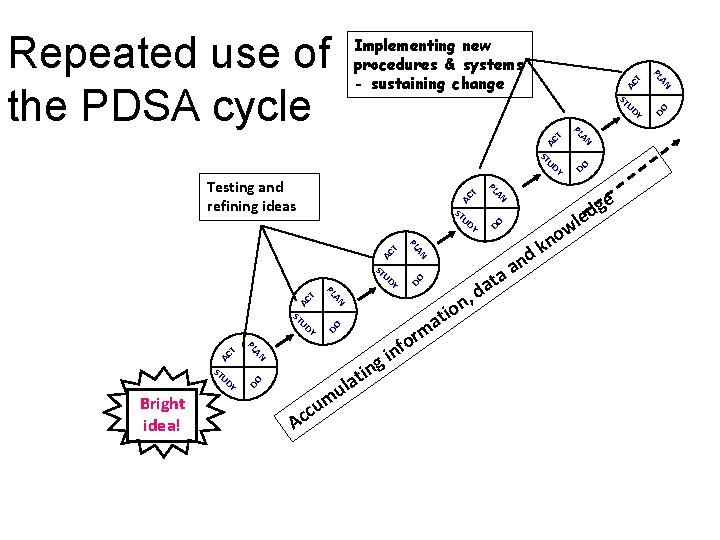
r o f in m n, o i at AC T DO ge d le w o n DO AC T DO A u m ccu g DO AC T n i t la DO AC T AN PL Bright idea! AN PL ST UD Y AN PL Testing and refining ideas ST UD Y d ata a k d n AC T AN PL ST UD Y DO Repeated use of the PDSA cycle Implementing new procedures & systems - sustaining change
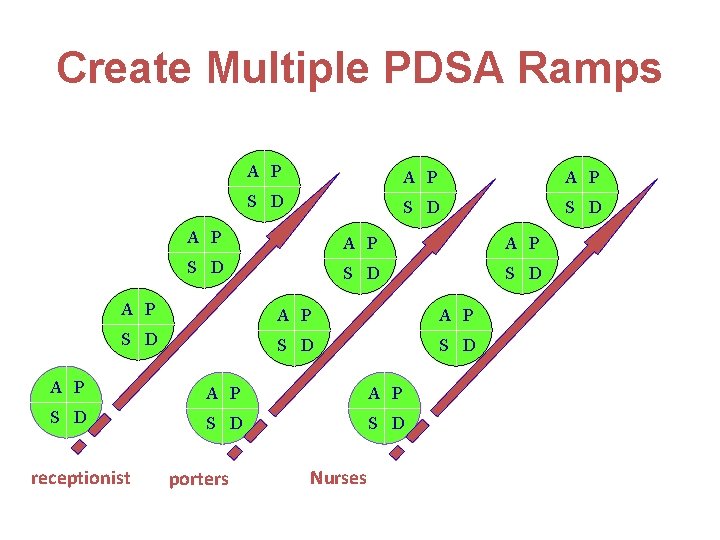
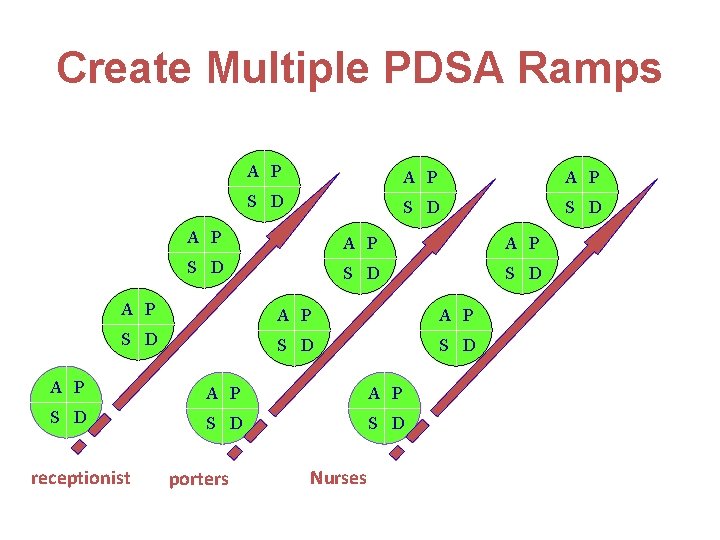
Create Multiple PDSA Ramps A P A P A P S D S D S D receptionist porters Nurses
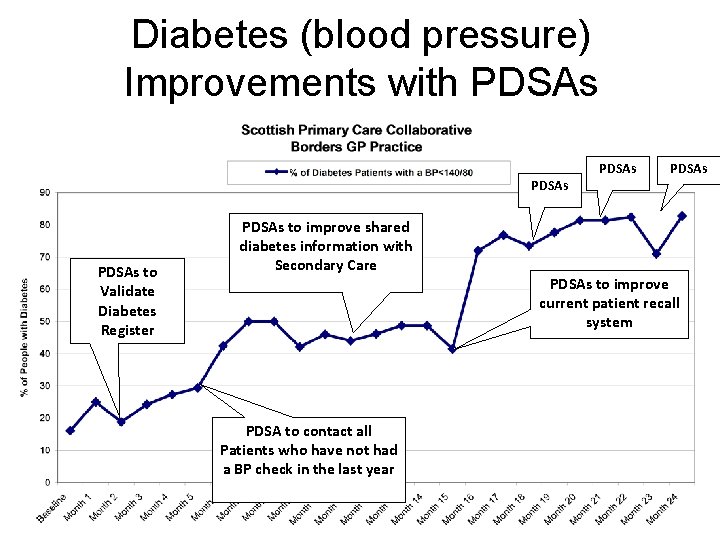
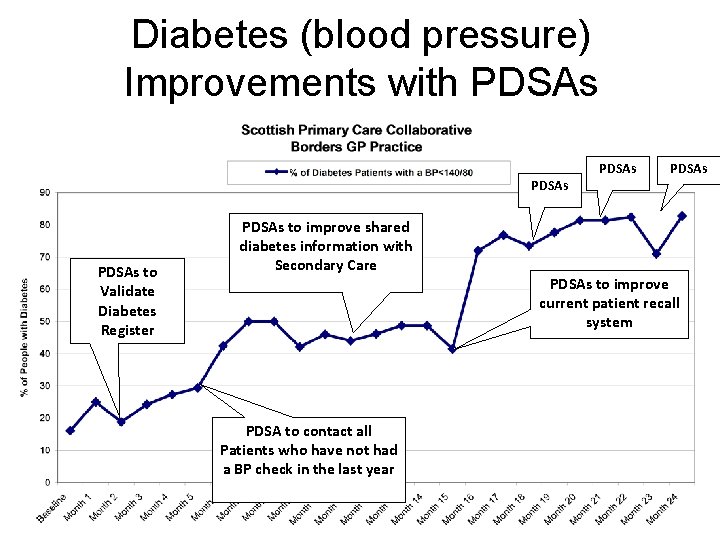
Diabetes (blood pressure) Improvements with PDSAs to Validate Diabetes Register PDSAs to improve shared diabetes information with Secondary Care PDSA to contact all Patients who have not had a BP check in the last year PDSAs to improve current patient recall system
SCENARIO • What are we trying to achieve? – know exactly what you are trying to do – have clear aims and objectives • What changes can we make that will result in an improvement? – What have others done? – What hunches do we have? – What can we learn as we go along?

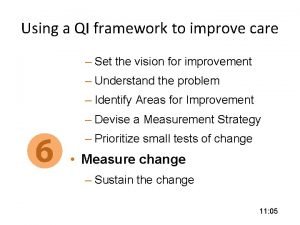
Measurement for Improvement
Measurement for Improvement • • • What is measurement for improvement Why measure anything? What should you measure? How do you collect your data? How do you present and share your data?

What is measurement for improvement? IMPROVEMENT Purpose Data Duration Understanding of Process Evaluation of change To discover new knowledge ACCOUNTABILITY Comparison Reassurance RESEARCH To bring new knowledge into daily practice Gather just enough data to learn and complete another cycle Large amounts of data Gather as much data as possible ‘just in case’ ‘Small tests of significant change’ accelerates the rate of improvement Short & current Long periods of time Long & past Can take long periods of time to obtain results Long & past
Why measure? • Critical part of testing and implementing change. • Allows us to know if change resulted in an improvement. • Allows us to determine further impact of the change. • To evidence improvements.
What should you measure? • Develop aims before measures. • Design measures around aims. • Make measures easy to collect by staff. • Should not take longer than one week
• How will we know that change is an improvement? – Measuring processes and outcomes
![How do you collect your data Define starting point BASELINE Collecting How do you collect your data? • Define starting point [ BASELINE] • Collecting](https://slidetodoc.com/presentation_image_h2/b06379c47f186aa8bf7b3b738cec1334/image-31.jpg)
How do you collect your data? • Define starting point [ BASELINE] • Collecting data: Tick box sheets, Excel spreadsheet Existing information. Patient & Staff Questionnaires • Build measurement into work • RIGHT person to capture the RIGHT data at the RIGHT time
How do you present and share your data? • Define Improvements in raw numbers and as % improvement. • Use newsletters, intranet, posters, patient and professional groups, journals etc. ,

• fundamental questions for improvement • results from using the PDSA cycle • effective use of data • testing changes Source: D. Berwick
The elevator to success is out of order. You’ll have to use the stairs …… One step at a time
Useful links • Institute of Healthcare Improvement www. ihi. org A Guide to Service Improvement www. scotland. gov. uk • Improvement & Support Team Toolkit http: //member. goodpractice. net/Continuous. Impr ovement. Toolkit/Welcome. gp • Improvement Leaders Guides www. modern. nhs. uk/improvementguides
Resources
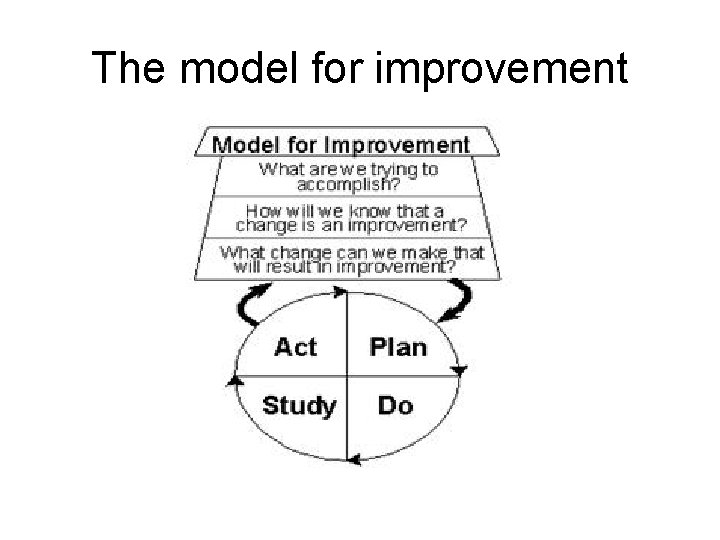
The model for improvement



PDSA Ramping Improved Practice a t a D Cycle 1 d Cycle 1 c Cycle 1 b Cycle 1 a Specific Changes e. g. Dr Triage
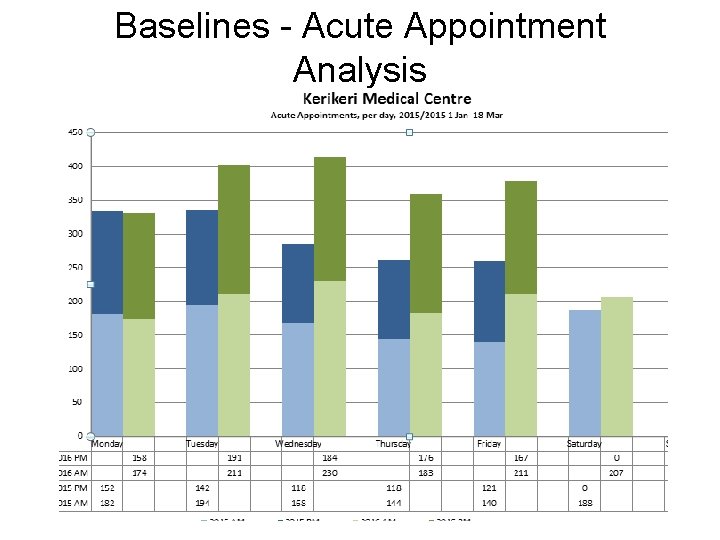
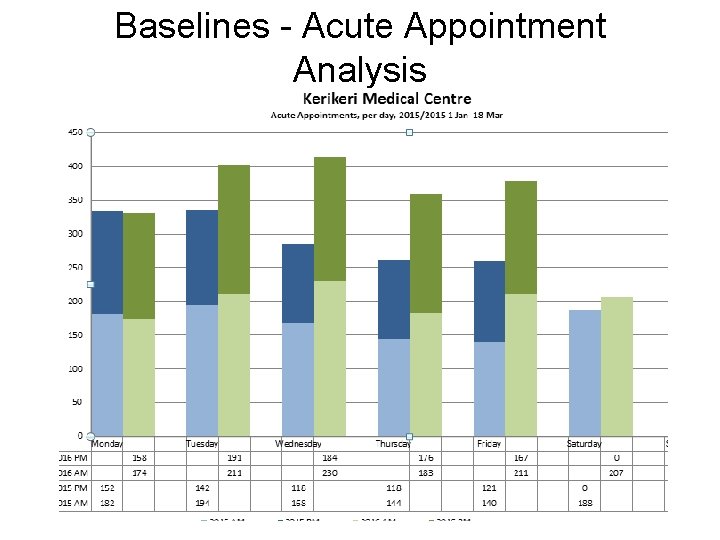
Baselines - Acute Appointment Analysis
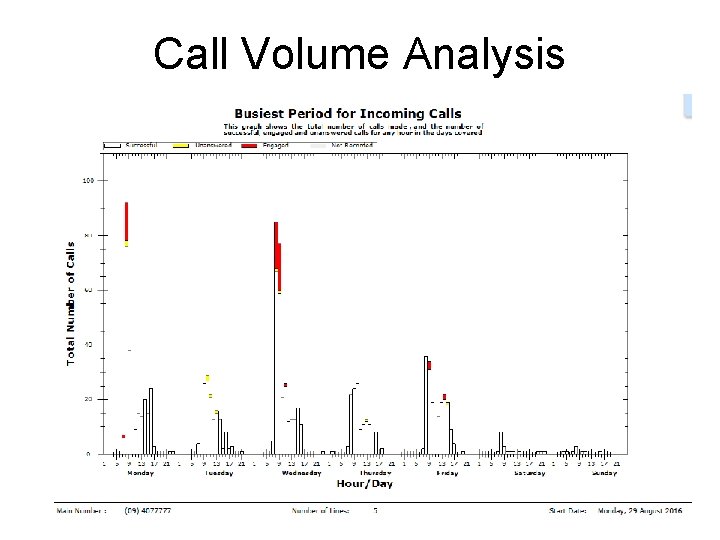
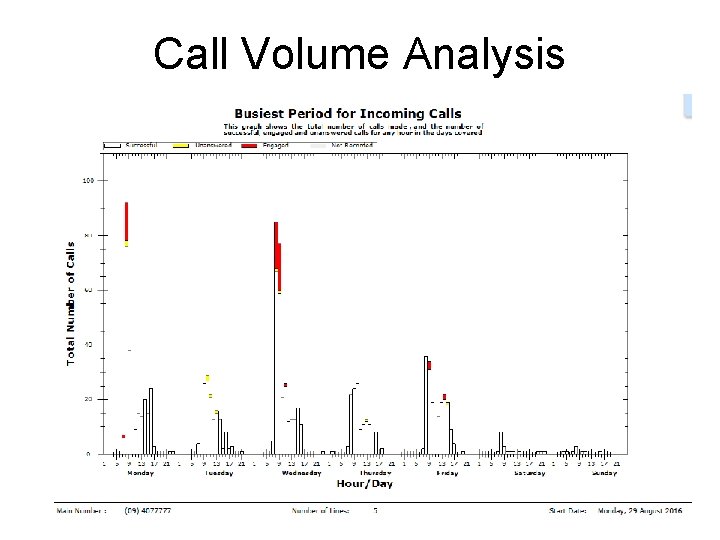
Call Volume Analysis
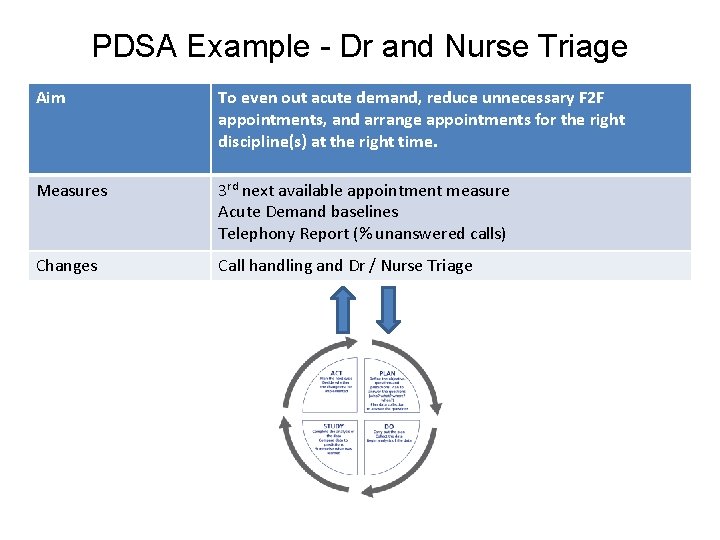
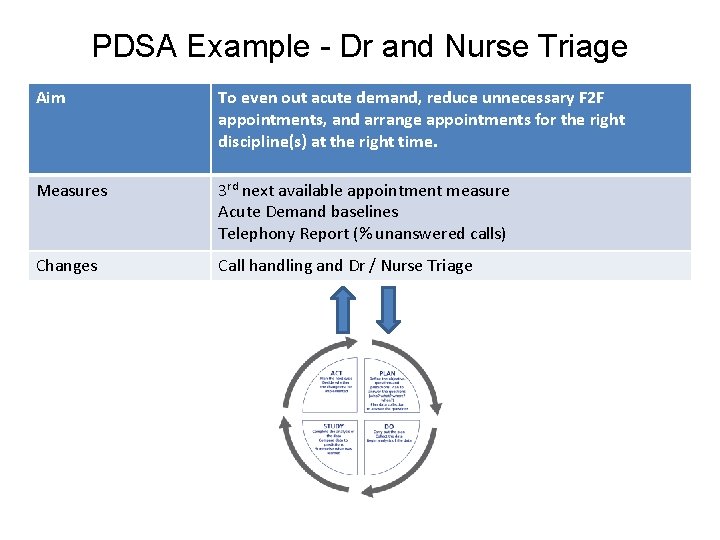
PDSA Example - Dr and Nurse Triage Aim To even out acute demand, reduce unnecessary F 2 F appointments, and arrange appointments for the right discipline(s) at the right time. Measures 3 rd next available appointment measure Acute Demand baselines Telephony Report (% unanswered calls) Changes Call handling and Dr / Nurse Triage
 Model for improvement
Model for improvement Gambar tersebut merupakan
Gambar tersebut merupakan Agenda sistemica y agenda institucional
Agenda sistemica y agenda institucional Long run supply curve
Long run supply curve Themes in run lola run
Themes in run lola run Run lola run editing techniques
Run lola run editing techniques Short run vs long run economics
Short run vs long run economics Within run and across run meaning
Within run and across run meaning Long run market supply curve
Long run market supply curve Brigitta olsen
Brigitta olsen Run lola run wiki
Run lola run wiki Pdsa worksheet
Pdsa worksheet Rampa de pdsa
Rampa de pdsa Pdsa template
Pdsa template Pdsa-cykeln
Pdsa-cykeln Pdsa cirkler
Pdsa cirkler Pdsa model nhs
Pdsa model nhs Pdsa model nhs
Pdsa model nhs Pdsa sirkel
Pdsa sirkel Pdsa exemplo
Pdsa exemplo Pdsa cycle in healthcare
Pdsa cycle in healthcare Pdsa sirkel
Pdsa sirkel Pdsa
Pdsa Pdsa falkirk
Pdsa falkirk Pdsa
Pdsa Ucf pdsa
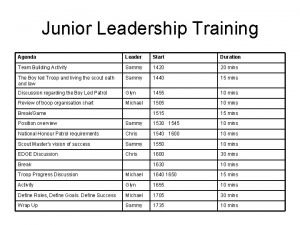
Ucf pdsa Leadership training agenda
Leadership training agenda Mandarin cycles
Mandarin cycles Alliteration words for cycle
Alliteration words for cycle Importance of water cycle
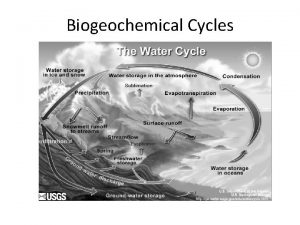
Importance of water cycle Precession milankovitch cycles
Precession milankovitch cycles Correct order
Correct order Relationship between transaction cycles
Relationship between transaction cycles Cpi cycles per instruction
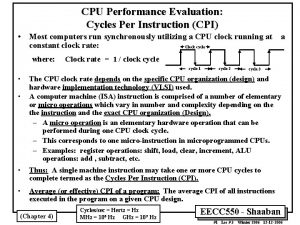
Cpi cycles per instruction Biogeochemical cycles performance task
Biogeochemical cycles performance task Apes cycles
Apes cycles What is the major abiotic reservoir for phosphorus
What is the major abiotic reservoir for phosphorus Biogeochemical cycles quiz
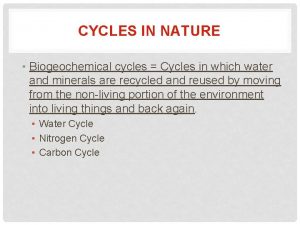
Biogeochemical cycles quiz Cycles in nature
Cycles in nature Joke cycles
Joke cycles Joke cycles
Joke cycles Biogeochemical cycles class 9 ppt
Biogeochemical cycles class 9 ppt Fatigue risk assessment matrix
Fatigue risk assessment matrix Biogeochemical cycles foldable
Biogeochemical cycles foldable