PDLS General Principles of Disaster Care Pediatric Triage








- Slides: 41
PDLS©: General Principles of Disaster Care: Pediatric Triage Assessment, Stabilization, Resuscitation
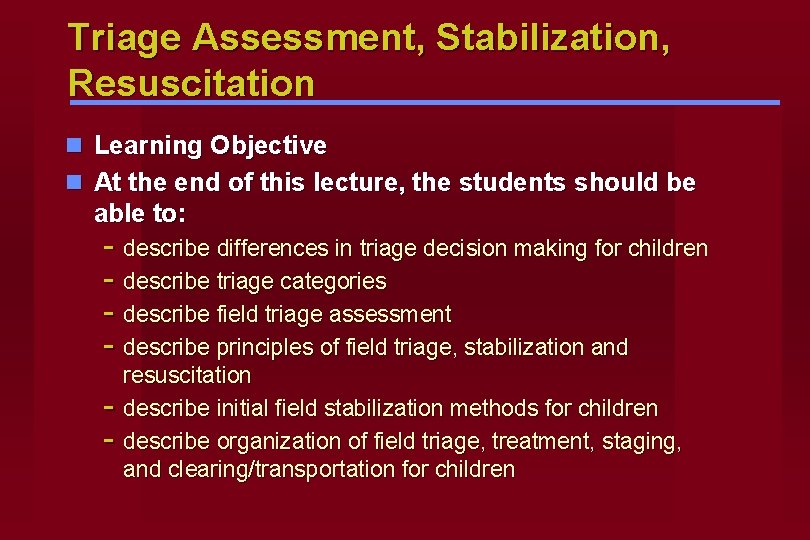
Triage Assessment, Stabilization, Resuscitation n Learning Objective n At the end of this lecture, the students should be able to: - describe differences in triage decision making for children - describe triage categories - describe field triage assessment - describe principles of field triage, stabilization and - resuscitation describe initial field stabilization methods for children describe organization of field triage, treatment, staging, and clearing/transportation for children
Oklahoma City – YMCA Day Care n The Scene: - Multiple injured kids - Delay in finding them - 4 Children: 2 not breathing, unresponsive 2 sitting, crying
General Principles of Disaster Care n Triage Assessment n Initial Stabilization n Resuscitation
Triage Assessment n Derived from the French “trier” meaning to sort, it describes a medical decision making process. n Appropriate performance crucial. n Dynamic process, re-triage / re-evaluate at several stages. n Determination of priority may effect the extent and quality of care the patient receives.
Triage n Triage in disaster setting may be very difficult n Pediatric population unique challenge

Problems of Under / Over-Triage
Triage in Prehospital Setting n ICS (Incident Command System) - Medical Branch n Gain Control of Scene n Triage Officer: Initial Brief Assessment
Initial Evaluation n Ensure scene safety n Establish that disaster exists n Estimate number of victims: adults/children
Initial Evaluation n Notification to medical control: regional communications, local emergency management / disaster authority - type of event - initial casualty estimate n Make initial request for additional resources Then begin triage assessment of individual patients

Initial Brief Assessment n Open airway n Control major hemorrhage n Categorize
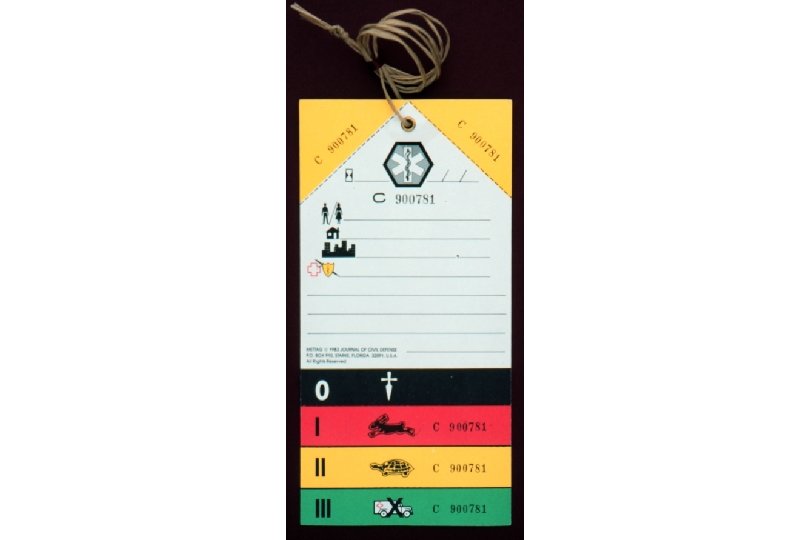
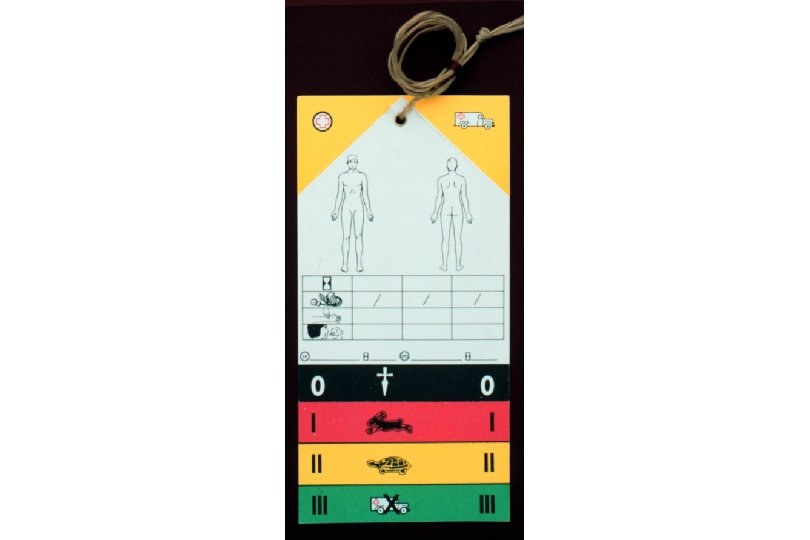
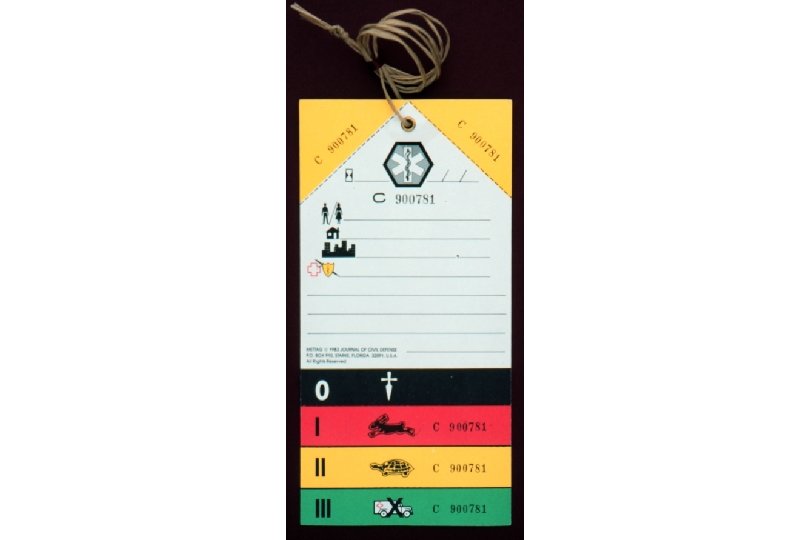
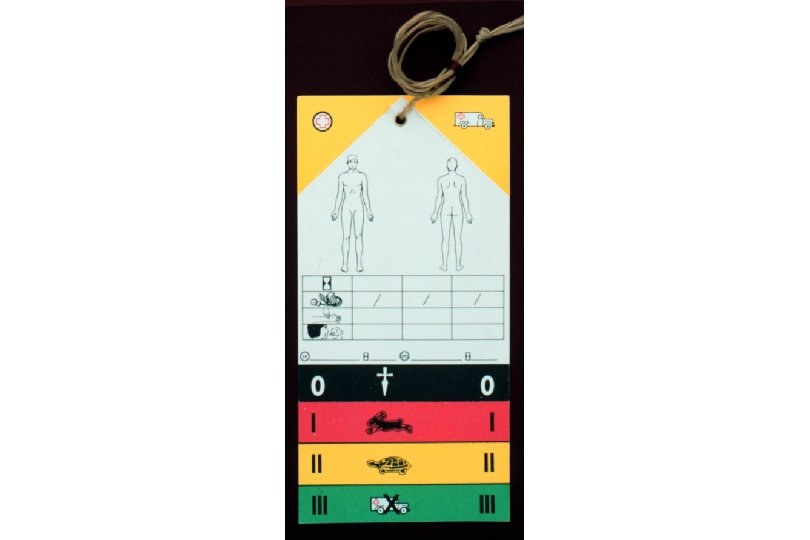
Triage Categories n Red / Immediate / Emergency n Yellow / Urgent n Green / Non-Urgent / Walking Wounded n Black / Blue
Triage Classifications n Simple Triage And Rapid Treatment S. T. A. R. T. n Jump. START Tool for Rapid Pediatric Multicasualty Field Triage (children from 1 - 8 years of age)
Triage Classifications and Examples n Red - tension pneumothorax, rib fractures, upper airway obstruction, hemorrhage, femur fracture, asthmatic n Yellow - humerus fracture, scalp lacerations, shoulder dislocation n Green - ankle sprain, simple laceration, orphaned child, subluxed radial head n Black/Blue - cardiopulmonary arrest, severe open head injury
Triage Classifications n Consider pediatric anatomy / physiology / age / development when categorizing child n Familiarity with - level of expertise of personnel - numbers and type of transport available - equipment supplies - appropriate destination for definitive care
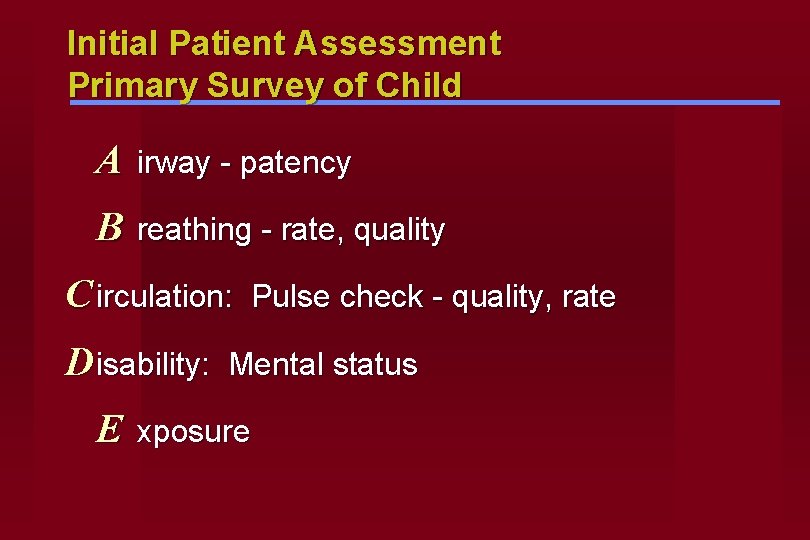
Initial Patient Assessment Primary Survey of Child A irway - patency B reathing - rate, quality C irculation: D isability: E Pulse check - quality, rate Mental status xposure
Airway n First priority even more so than in an adult. Hypoxia main factor leading to organ dysfunction, ischemia, and cardiopulmonary arrest. n Consider need for endotracheal intubation in child with GCS<8, significant maxillofacial trauma, aspiration, or respiratory distress. Remember - - Oropharyngeal airway ET size/uncuffed ET route for delivery of medication (LANE)
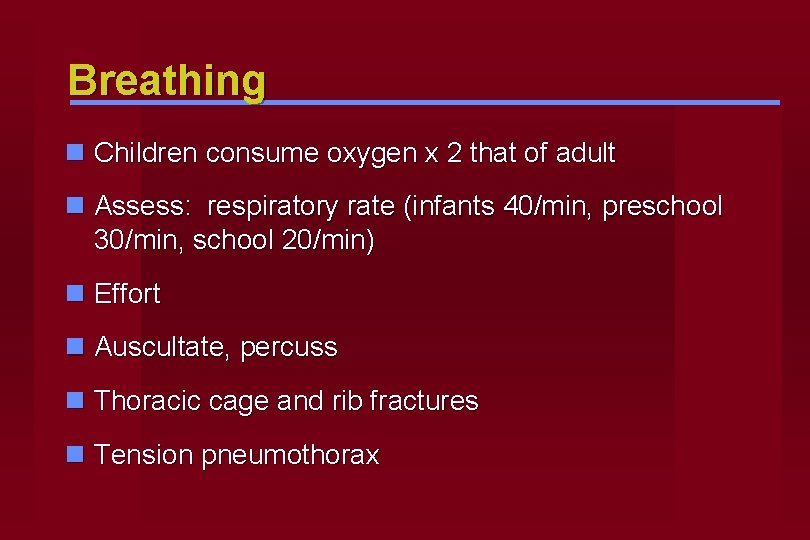
Breathing n Children consume oxygen x 2 that of adult n Assess: respiratory rate (infants 40/min, preschool 30/min, school 20/min) n Effort n Auscultate, percuss n Thoracic cage and rib fractures n Tension pneumothorax


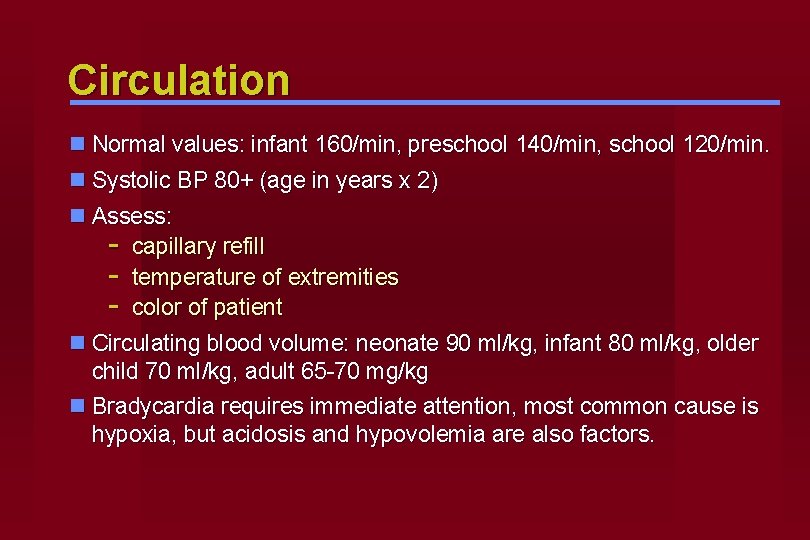
Circulation n Normal values: infant 160/min, preschool 140/min, school 120/min. n Systolic BP 80+ (age in years x 2) n Assess: - capillary refill - temperature of extremities - color of patient n Circulating blood volume: neonate 90 ml/kg, infant 80 ml/kg, older child 70 ml/kg, adult 65 -70 mg/kg n Bradycardia requires immediate attention, most common cause is hypoxia, but acidosis and hypovolemia are also factors.
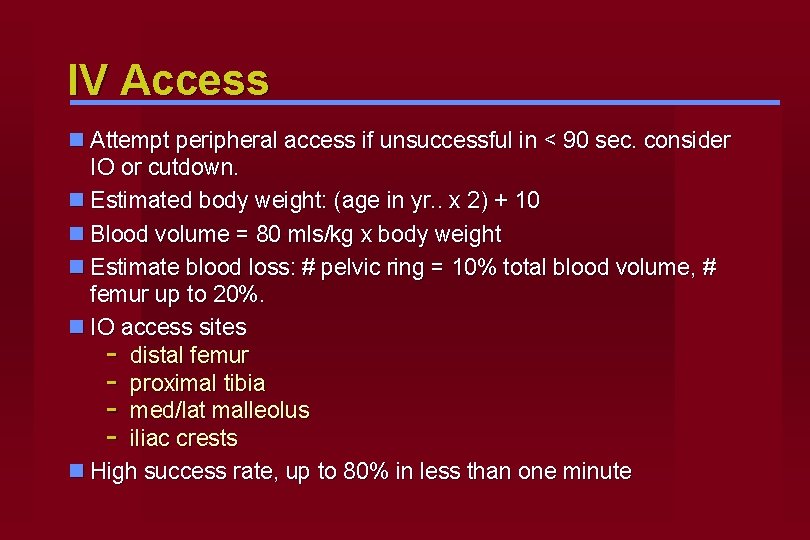
IV Access n Attempt peripheral access if unsuccessful in < 90 sec. consider IO or cutdown. n Estimated body weight: (age in yr. . x 2) + 10 n Blood volume = 80 mls/kg x body weight n Estimate blood loss: # pelvic ring = 10% total blood volume, # femur up to 20%. n IO access sites - distal femur - proximal tibia - med/lat malleolus - iliac crests n High success rate, up to 80% in less than one minute
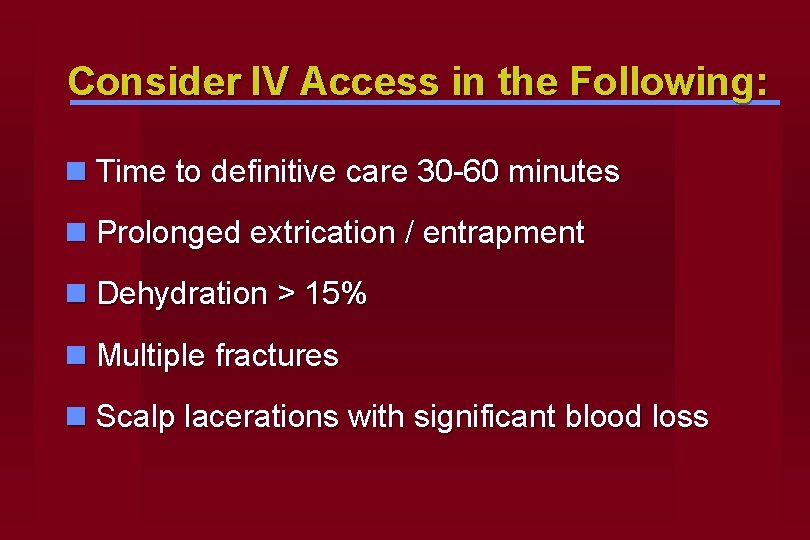
Consider IV Access in the Following: n Time to definitive care 30 -60 minutes n Prolonged extrication / entrapment n Dehydration > 15% n Multiple fractures n Scalp lacerations with significant blood loss
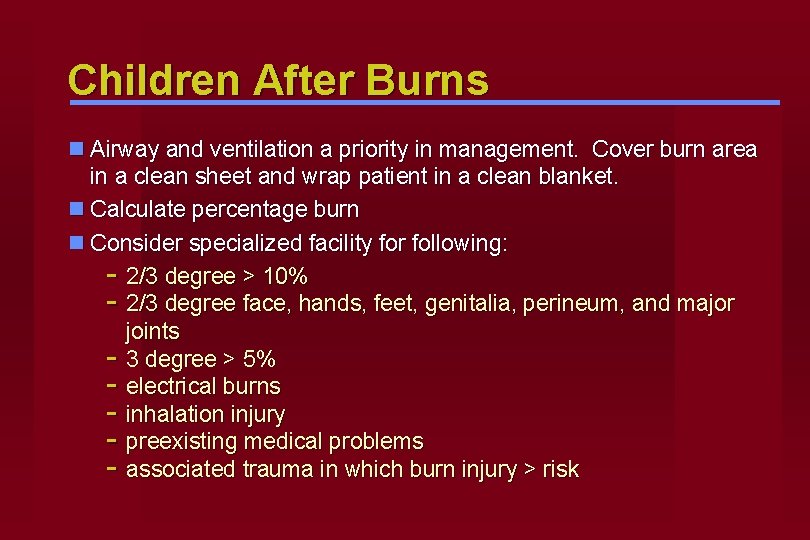
Children After Burns n Airway and ventilation a priority in management. Cover burn area in a clean sheet and wrap patient in a clean blanket. n Calculate percentage burn n Consider specialized facility for following: - 2/3 degree > 10% - 2/3 degree face, hands, feet, genitalia, perineum, and major joints - 3 degree > 5% - electrical burns - inhalation injury - preexisting medical problems - associated trauma in which burn injury > risk

Disability n GCS useful in children > 1 yr
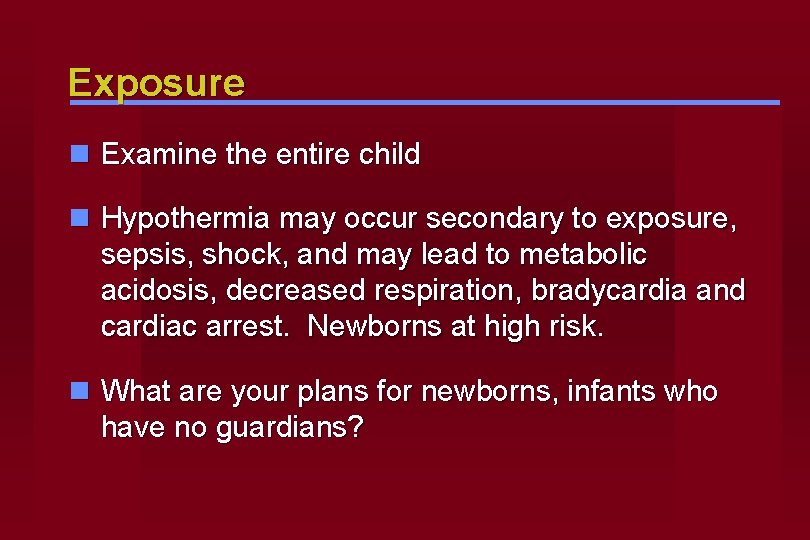
Exposure n Examine the entire child n Hypothermia may occur secondary to exposure, sepsis, shock, and may lead to metabolic acidosis, decreased respiration, bradycardia and cardiac arrest. Newborns at high risk. n What are your plans for newborns, infants who have no guardians?
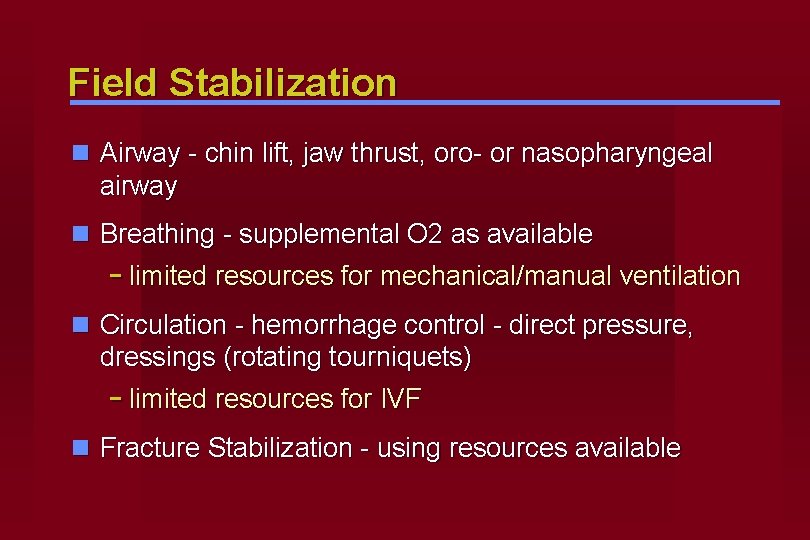
Field Stabilization n Airway - chin lift, jaw thrust, oro- or nasopharyngeal airway n Breathing - supplemental O 2 as available - limited resources for mechanical/manual ventilation n Circulation - hemorrhage control - direct pressure, dressings (rotating tourniquets) - limited resources for IVF n Fracture Stabilization - using resources available
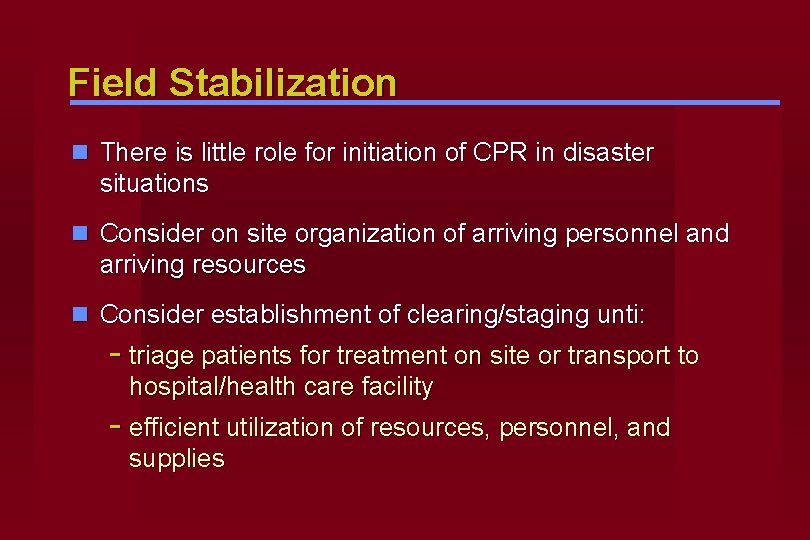
Field Stabilization n There is little role for initiation of CPR in disaster situations n Consider on site organization of arriving personnel and arriving resources n Consider establishment of clearing/staging unti: - triage patients for treatment on site or transport to hospital/health care facility - efficient utilization of resources, personnel, and supplies
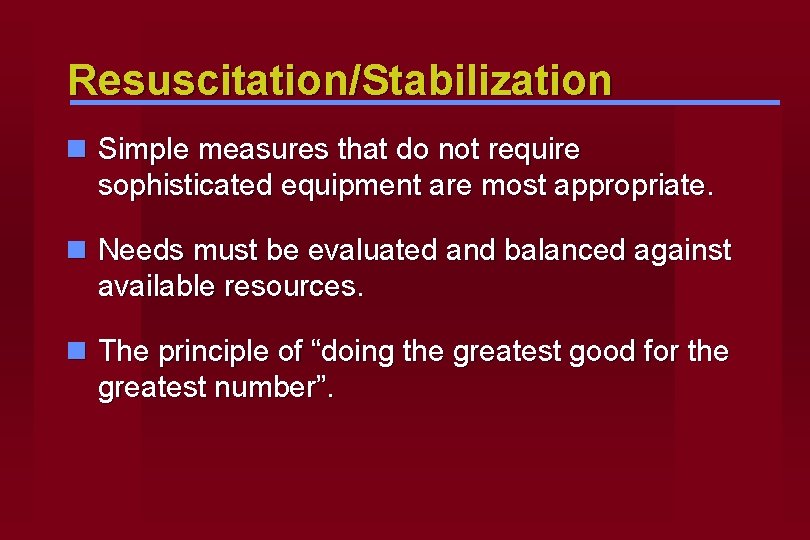
Resuscitation/Stabilization n Simple measures that do not require sophisticated equipment are most appropriate. n Needs must be evaluated and balanced against available resources. n The principle of “doing the greatest good for the greatest number”.
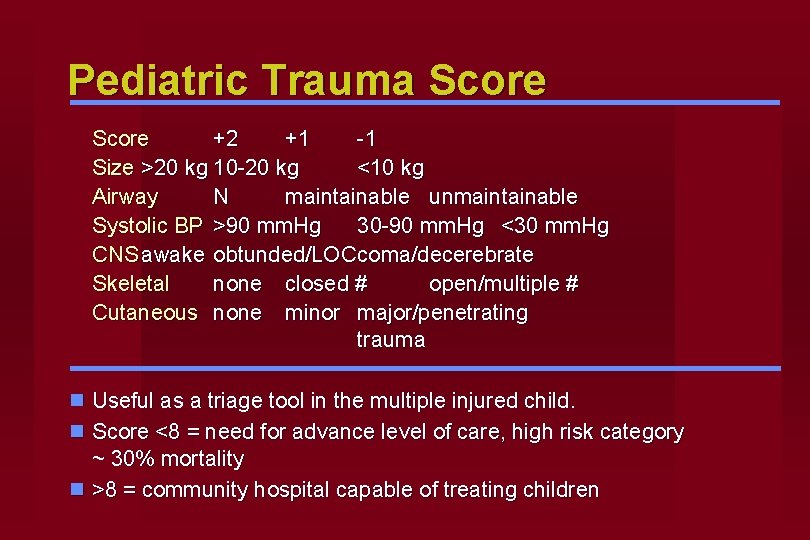
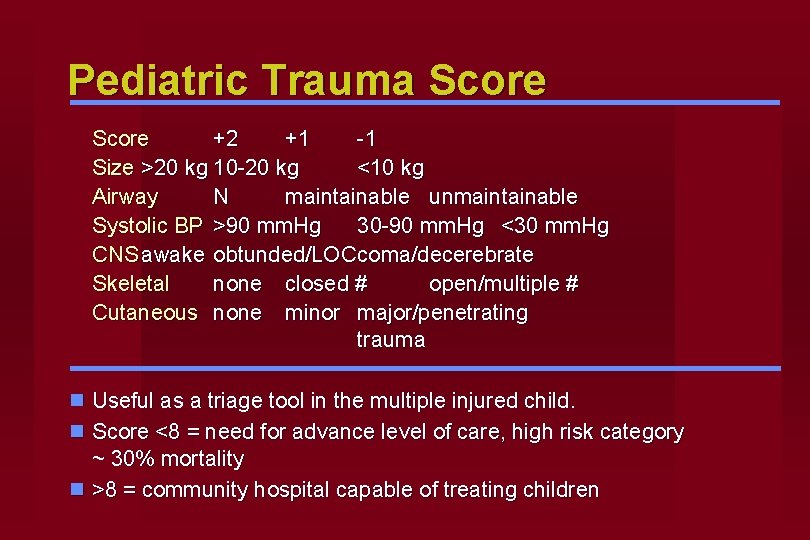
Pediatric Trauma Score +2 +1 -1 Size >20 kg 10 -20 kg <10 kg Airway N maintainable unmaintainable Systolic BP >90 mm. Hg 30 -90 mm. Hg <30 mm. Hg CNS awake obtunded/LOC coma/decerebrate Skeletal none closed # open/multiple # Cutaneous none minor major/penetrating trauma n Useful as a triage tool in the multiple injured child. n Score <8 = need for advance level of care, high risk category ~ 30% mortality n >8 = community hospital capable of treating children
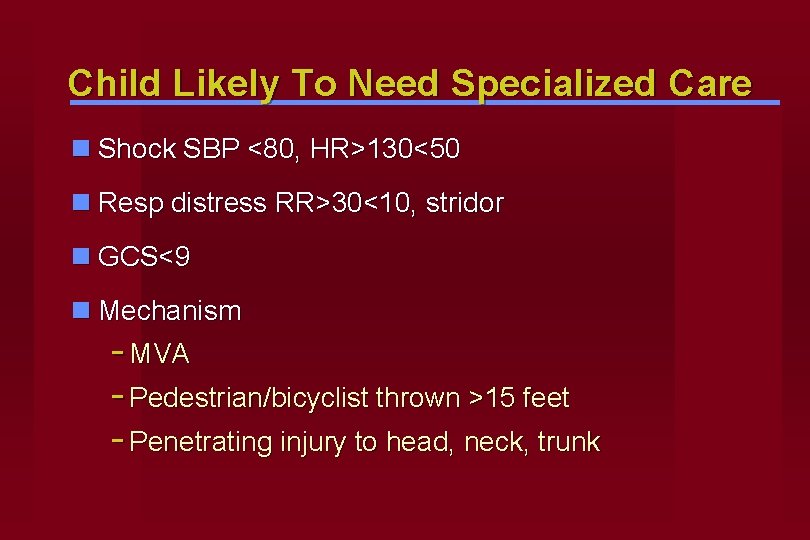
Child Likely To Need Specialized Care n Shock SBP <80, HR>130<50 n Resp distress RR>30<10, stridor n GCS<9 n Mechanism - MVA - Pedestrian/bicyclist thrown >15 feet - Penetrating injury to head, neck, trunk

Child Likely To Need Specialized Care Specific injuries n skull # n pneumothorax, flail chest n abd trauma with peritoneal signs n amputation / degloving n vascular injury n burn with inhalation n FB aspiration / ingestion
Preplanning n Needs assessment of community n Commitment on part of institutions and key personnel to treating injured children n Consider children with special needs n Consider evacuation process for NICU/PICU/SCU for newborns n Lack of supervision n Requirement of children in shelters


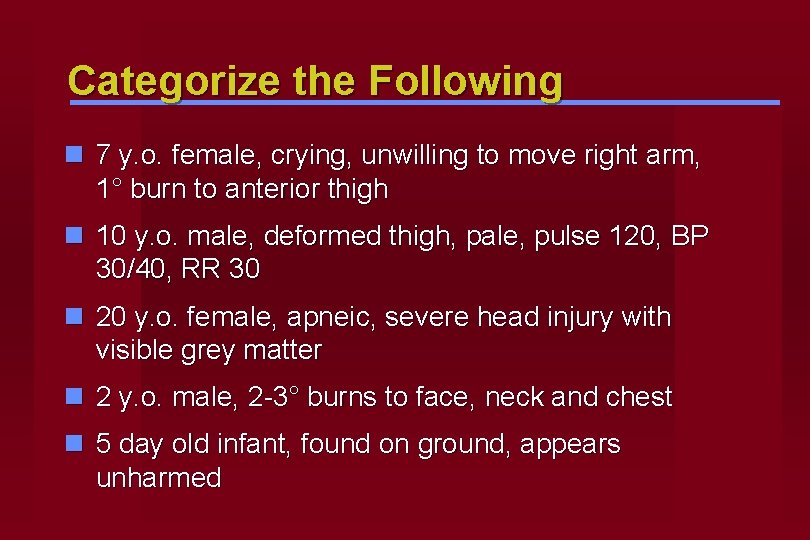
Categorize the Following n 7 y. o. female, crying, unwilling to move right arm, 1° burn to anterior thigh n 10 y. o. male, deformed thigh, pale, pulse 120, BP 30/40, RR 30 n 20 y. o. female, apneic, severe head injury with visible grey matter n 2 y. o. male, 2 -3° burns to face, neck and chest n 5 day old infant, found on ground, appears unharmed